Abstract
Background
Movement asymmetries during walking are common after anterior cruciate ligament (ACL) injury and reconstruction and may influence the early development of posttraumatic osteoarthritis. Preoperative neuromuscular training (like perturbation training, which is neuromuscular training requiring selective muscle activation in response to surface perturbations) improves gait asymmetries and functional outcomes among people who are ACL-deficient, but the effect of postoperative perturbation training on gait mechanics after ACL reconstruction is unknown.
Questions/purposes
Among men undergoing ACL reconstruction, we sought to compare strength, agility, and secondary prevention (SAP) treatment with SAP plus perturbation training (SAP+PERT) with respect to (1) gait mechanics; and (2) elimination of gait asymmetries 1 and 2 years after ACL reconstruction.
Methods
Forty men were randomized into a SAP group or a SAP+PERT group after ACL reconstruction and before returning to preinjury activities. Participants were required to achieve ≥ 80% quadriceps muscle strength symmetry, minimal knee effusion, full ROM, no reports of pain, and completion of a running progression (all between 3 and 9 months postoperatively) before enrollment. Of 94 potentially eligible athletic male patients evaluated < 9 months after ACL reconstruction, 54 were excluded for prespecified reasons. Participants underwent motion analysis during overground walking at 1 and 2 years postoperatively. Variables of interest included (1) sagittal and frontal plane hip and knee angles and moments at peak knee flexion angle; (2) sagittal plane hip and knee angles and moments at peak knee extension angle; (3) sagittal plane hip and knee excursion during weight acceptance; and (4) sagittal plane hip and knee excursion during midstance. We also calculated the proportion of athletes in each group who walked with clinically meaningful interlimb asymmetry in sagittal plane hip and knee variables and compared these proportions using odds ratios. There was no differential loss to followup between groups.
Results
There were no differences between the SAP or SAP+PERT groups for the biomechanical gait variables. The involved limb’s knee excursion during midstance for the SAP (mean ± SD: 1 year: 15° ± 5°; 2 years: 16° ± 5°) and SAP+PERT (1 year: 16° ± 5°; 2 years: 15° ± 4°) athletes was not different between groups at 1 year (mean difference: −1°; 95% confidence interval [CI], −5° to 2°; p = 0.49) or 2 years (mean difference: 1°; 95% CI, −2° to 4°; p = 0.54). There were no differences between SAP and SAP+PERT athletes regarding the elimination of gait asymmetries, and gait asymmetries persisted to a large degree in both groups 1 and 2 years postoperatively. At 1 year, 11 of 18 SAP and 11 of 20 SAP+PERT athletes walked with truncated knee excursions during weight acceptance (odds ratio: 0.8, p = 0.70) and midstance (SAP 12 of 18, SAP+PERT 12 of 20; odds ratio: 0.8, p = 0.67), whereas at 2 years postoperatively, truncated knee excursions during weight acceptance (SAP seven of 17, SAP+PERT eight of 19; odds ratio: 1.0, p = 0.96) and midstance (SAP five of 17, SAP+PERT 11 of 19; odds ratio: 3.3, p = 0.09) remained prevalent.
Conclusions
We found that a comprehensive, progressive return-to-sport training program with or without perturbation was not effective at restoring interlimb symmetry among men 1 or 2 years after ACL reconstruction. Although gait asymmetries improved from 1 to 2 years postoperatively, meaningful asymmetries persisted in both groups. To restore gait symmetry after ACL reconstruction, additional interventions likely are necessary.
Level of Evidence
Level II, therapeutic study.
Keywords: Anterior Cruciate Ligament, Anterior Cruciate Ligament Reconstruction, Anterior Cruciate Ligament Injury, Minimal Clinically Important Difference, Knee Flexion Angle
Introduction
After anterior cruciate ligament (ACL) injury, many individuals undergo reconstructive surgery to restore knee stability and function [30, 38], yet despite ACL reconstruction (ACLR), movement asymmetries exist at least 6 months to 1 year after ACLR [12, 16, 19, 20, 36, 41, 43] and may persist longer [36]. Movement asymmetries during gait are associated with the development of early osteoarthritis [4, 41]; thus, developing strategies to mitigate these asymmetries is an important area of research.
To improve movement asymmetries in individuals after ACL injuries, neuromuscular training programs have been suggested. One type of neuromuscular training is perturbation training [8, 13, 15, 25, 42], which consists of external perturbations applied by a therapist while the participant stands on an unstable surface (such as a roller board or rocker board) [8, 15, 25, 42]. Perturbation training, when applied preoperatively, improves gait asymmetries [8, 13, 20]. Moreover, an extended preoperative physical therapy program including perturbation training results in higher success rates and longer maintained functional status compared with control subjects with extended physical therapy but no perturbation training [15]. Unfortunately, improvements in gait asymmetry that occur from preoperative perturbation training are not retained postoperatively [16, 36]. Postoperative interventions beyond traditional physical therapy are likely needed to restore gait symmetry after ACLR given the prevalence of movement abnormalities that persist [6, 16, 27, 28, 36, 37, 40, 41].
Although previous studies show promise for the efficacy of perturbation training, the effect of postoperative perturbation training on movement patterns is unknown. To address this gap, we developed the Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports training protocol (ACL-SPORTS) [42] for athletes after ACLR and traditional physical therapy. The ACL-SPORTS training protocol consists of 10 progressive sessions of comprehensive strengthening, agility, and secondary prevention exercises (SAP) or this SAP protocol with the addition of perturbation training (SAP+PERT).
The purpose of this study was to evaluate the effect of two versions of the ACL-SPORTS training protocol on hip and knee gait mechanics in men 1 and 2 years after ACLR. Specifically, among men undergoing ACLR, we sought to compare SAP treatment with SAP+PERT with respect to (1) gait mechanics; and (2) elimination of gait asymmetries 1 and 2 years after ACLR.
Patients and Methods
A detailed description of the patients and methodology for this study may be found in Cummer et al. [1]. Briefly, we enrolled and randomized 40 male athletes (mean age ± SD at surgery: 23 ± 7 years) after unilateral ACLR (autograft = 27, allograft = 13) when they met the following criteria for enrollment: ≥ 12 weeks after ACLR, ≥ 80% quadriceps femoris muscle strength symmetry, minimal knee effusion, full ROM, no reports of pain, and completion of a running progression [3]. Participants were randomized to two treatment groups: SAP group (n = 20) and SAP+PERT group (n = 20) (Fig. 1). The SAP group received 10 training sessions (twice per week) of ACL injury prevention exercises, agility drills, and plyometric exercises, whereas the SAP+PERT group received 10 training sessions (twice per week) consisting of all these exercises plus perturbation training (ie, neuromuscular training requiring selective muscle activation in response to surface perturbations applied by a physical therapist) [15]. After completing training and achieving objective return-to-sports criteria [3, 18, 42] (≥ 90% quadriceps strength index, ≥ 90% limb symmetry on four single-leg hop tests [34], and ≥ 90% score on the Knee Outcome Survey-Activities of Daily Living Scale [26]), participants were cleared to begin a gradual, patient-specific return-to-sport progression; rehabilitation after this time was not standardized.
Fig. 1.
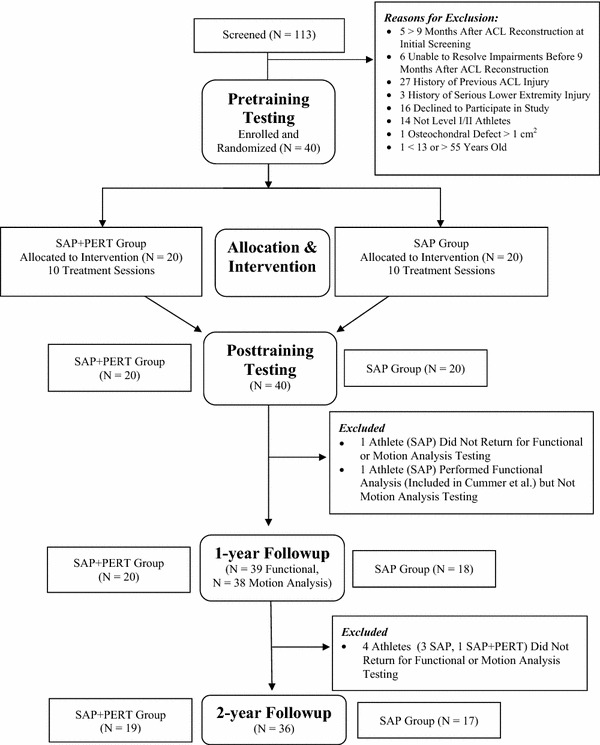
The CONSORT flow diagram outlines enrollment, allocation and intervention, testing time points, and followup.
We analyzed participants’ walking patterns 1 and 2 years postoperatively using an eight-camera motion capture system (VICON, Oxford, UK) and embedded force platform (Bertec Corporation, Columbus, OH, USA). Thirty-nine retroreflective markers were placed on the bilateral lower extremities and pelvis before motion analysis testing. Participants then walked overground at a self-selected gait speed maintained to ± 5% across trials and time points. Kinematic data were captured at 120 Hz, whereas kinetic data were captured at 1080 Hz. Data were processed using commercial software (Visual3D; C-Motion, Germantown, MD, USA) and normalized to 100% of stance phase. Joint moments were calculated through inverse dynamics and normalized to body weight and height (Nm/Kg*m) to allow comparisons between participants [32].
Variables of interest included (1) sagittal and frontal plane hip and knee angles and moments at peak knee flexion angle (pKFA); (2) sagittal plane hip and knee angles and moments at peak knee extension angle (pKExtA); (3) sagittal plane hip and knee excursion during weight acceptance (ie, pKFA – initial contact); and (4) sagittal plane hip and knee excursion during midstance (ie, pKExtA – pKFA). Sagittal plane joint excursions during weight acceptance and midstance are of particular interest after ACLR given the role of the quadriceps muscle in eccentrically and concentrically controlling knee motion during these phases of the gait cycle.
Statistical Analyses
To compare the demographic characteristics of participants in each group (SAP versus SAP+PERT), we used Student’s t-tests and Pearson chi-square tests of proportions and odds ratios (Table 1). To compare gait biomechanical variables, we used 2 × 2 × 2 analysis of variance with three factors: (1) time (1 versus 2 years postoperatively); (2) group (SAP versus SAP+PERT); and (3) limb (uninvolved [UN] versus involved [INV]). Alpha was set at 0.05 a priori for all comparisons. We conducted post hoc t-tests and calculated mean differences (with 95% confidence intervals).
Table 1.
Demographics and anthropometrics were similar for subjects in the SAP and SAP+PERT groups
| Demographics/anthropometrics | SAP (mean ± SD) |
SAP+PERT (mean ± SD) | Mean difference (95% confidence interval) | p value |
|---|---|---|---|---|
| Age at surgery (years) | 24 ± 9 | 23 ± 6 | 0 (−4 to 5) | 0.39 |
| Height (cm) | 179 ± 7 | 177 ± 7 | 2 (−2 to 6) | 0.98 |
| Weight (kg) | 86 ± 13 | 86 ± 10 | 0 (−7 to 7) | 0.44 |
| Graft type | Autograft = 14 Allograft = 6 | Autograft = 13 Allograft = 7 | Odds ratio 0.8 (0.2–3.0) | 1.00 |
| Mechanism of injury | Contact 9 Noncontact 11 |
Contact 9 Noncontact 11 |
Odds ratio 1.0 (0.3–3.5) | 1.00 |
| Weeks from surgery to enrollment in ACL-SPORTS training protocol | 23 ± 8 | 22 ± 7 | 1 (−4, 5) | 0.73 |
SAP = strength, agility, and secondary prevention treatment group; SAP+PERT = SAP + perturbation training group; ACL-SPORTS = ACL-Specialized Post-Operative Return-to-Sports.
We also compared interlimb differences (UN – INV) with previously established minimal clinically important difference (MCID) [13] values to assess for meaningful interlimb asymmetries. MCID values are 3° for sagittal plane hip and knee kinematics during weight acceptance and 0.06 Nm/Kg*m and 0.04 Nm/Kg*m for sagittal plane hip and knee kinetics, respectively, at peak knee flexion angle [13]. Clinically meaningful interlimb asymmetry was defined as an absolute difference that met or exceeded the MCID [13] for hip angles, moments, and excursions and knee moments. Only smaller [13] involved (versus uninvolved) limb knee angles and excursions were deemed clinically meaningful given the prevalence of reduced knee flexion angles and excursions after ACLR. We computed the proportion of SAP and SAP+PERT athletes who walked with clinically meaningful interlimb asymmetry in sagittal plane hip and knee variables and compared these proportions using odds ratios.
Post Hoc Power Analysis
We conducted a post hoc power analysis on our primary outcome (ie, knee flexion angle) using the observed SDs (for peak knee flexion angle) and number of subjects per group. With 80% power and an α of 0.05, we could have detected a group difference of 3.5° for knee flexion angle. The previously established MCID for peak knee is 3° [13], which is only marginally smaller than what we were powered to detect. Moreover, none of our group differences for knee flexion angles or excursions at 1 or 2 years postoperatively exceeded 2.0°: the largest measured group difference for knee flexion angles/excursions in the involved limb was 1.8° (95% confidence interval [CI], −2.2° to 5.7°; p = 0.37) for pKFA 2 years postoperatively; the largest measured group difference for knee flexion angles/excursions in the uninvolved limb was −2.0° (95% CI, −5.0° to 1.0°; p = 0.18) for knee excursion during midstance 1 year postoperatively.
Results
Gait Mechanics
There were no differences between the SAP or SAP+PERT groups for the biomechanical gait variables. Athletes walked with similar sagittal plane hip and knee angles at both 1 and 2 years postoperatively in both their involved and uninvolved limbs (Table 2). Likewise, hip and knee excursions were similar across groups at both time points. Notably, the involved limb’s knee excursion during midstance for the SAP (mean ± SD: 1 year: 15° ± 5°; 2 years: 16° ± 5°) and SAP+PERT (1 year: 16° ± 5°; 2 years: 15° ± 4°) groups was similar between groups at both 1 year (mean difference: −1°; 95% CI, −5° to 2°; p = 0.49) and 2 years (mean difference: 1°; 95% CI, −2° to 4°; p = 0.54) postoperatively. Hip extension moments at peak knee flexion angle decreased from 1 year to 2 years postoperatively but did not differ between groups.
Table 2.
Sagittal plane hip and knee angles at peak knee flexion angle did not differ between SAP and SAP+PERT groups for the involved or uninvolved limbs at 1 or 2 years after ACLR
| Involved limb | ||||
|---|---|---|---|---|
| Variable | SAP | SAP+PERT | Mean difference | p value |
| KFA (°) at 1 year | 20 (6) | 20 (5) | 0 (−3 to 4) | 0.92 |
| KFA (°) at 2 years | 20 (7) | 18 (4) | 2 (−2 to 6) | 0.37 |
| HFA (°) at 1 year | 17 (6) | 18 (5) | −1 (−4 to 2) | 0.55 |
| HFA (°) at 2 years | 18 (8) | 17 (6) | 1 (−4 to 6) | 0.63 |
| Uninvolved limb | ||||
|---|---|---|---|---|
| Variable | SAP | SAP+PERT | Mean difference | p value |
| KFA (°) at 1 year | 22 (6) | 24 (5) | −2 (−5 to 2) | 0.27 |
| KFA (°) at 2 years | 22 (6) | 20 (6) | 2 (−2 to 6) | 0.34 |
| HFA (°) at 1 year | 17 (5) | 20 (5) | −2 (−6 to 1) | 0.19 |
| HFA (°) at 2 years | 19 (7) | 17 (6) | 1 (−3 to 6) | 0.48 |
Values are mean (SD) and mean group differences (95% confidence interval); SAP = strength, agility, and secondary prevention treatment group; SAP+PERT = SAP + perturbation training group; ACLR = anterior cruciate ligament reconstruction; KFA = knee flexion angle; HFA = hip flexion angle.
Gait Asymmetries
There were no differences between SAP and SAP+PERT training regarding the elimination of gait asymmetries 1 or 2 years after ACLR, and gait asymmetries persisted to a large degree in both groups at both time points. The majority of both SAP and SAP+PERT athletes walked with meaningful interlimb asymmetries for sagittal plane hip and knee moments at pKFA, knee excursions during weight acceptance and midstance, and hip excursion during midstance at 1 year postoperatively, but these proportions did not differ between groups (Table 3). Likewise, the proportion of athletes who walked with clinically meaningful hip and knee angles, moments, and excursions did not differ at 2 years after ACLR (Table 3).
Table 3.
This table displays the proportions of SAP and SAP+PERT athletes who walked with clinically meaningful interlimb asymmetries for sagittal plane hip and knee angles and moments at 1- 2-years followup
| 1 year | ||||
|---|---|---|---|---|
| Variable | SAP (N = 18) | SAP+PERT (N = 20) | Odds ratio (95% CI) | p value |
| HFA at pKFA | 5 | 9 | 2.1 (0.5–8.3) | 0.27 |
| KFA at pKFA | 9 | 12 | 1.5 (0.4–5.4) | 0.54 |
| HFM at pKFA | 13 | 13 | 0.7 (0.2–2.8) | 0.63 |
| KFM at pKFA | 13 | 18 | 3.5 (0.6–20.7) | 0.16 |
| Knee excursion during WA | 11 | 11 | 0.8 (0.2–2.8) | 0.70 |
| Hip excursion during WA | 7 | 5 | 0.5 (0.1–2.1) | 0.36 |
| Knee excursion during MS | 12 | 12 | 0.8 (0.2–2.8) | 0.67 |
| Hip excursion during MS | 13 | 14 | 0.9 (0.2–3.7) | 0.88 |
| 2 years | ||||
|---|---|---|---|---|
| Variable | SAP (N = 17) | SAP+PERT (N = 19) | Odds ratio (95% CI) | p value |
| HFA at pKFA | 7 | 4 | 0.4 (0.1–1.7) | 0.19 |
| KFA at pKFA | 4 | 9 | 2.9 (0.7–12.3) | 0.14 |
| HFM at pKFA | 8 | 9 | 1.0 (0.3–3.8) | 0.99 |
| KFM at pKFA | 14 | 16 | 1.1 (0.2–6.6) | 0.88 |
| Knee excursion during WA | 7 | 8 | 1.0 (0.3–3.9) | 0.96 |
| Hip excursion during WA | 5 | 5 | 0.9 (0.2–3.7) | 0.84 |
| Knee excursion during MS | 5 | 11 | 3.3 (0.8–13.2) | 0.09 |
| Hip excursion during MS | 9 | 12 | 1.5 (0.4–5.8) | 0.54 |
Odds ratios (with 95% confidence interval) represent the relative odds that clinically meaningful asymmetries existed in the SAP+PERT group compared with the SAP group; SAP = strength, agility, and secondary prevention treatment group; SAP+PERT = SAP + perturbation training group; CI = confidence interval; HFA = hip flexion angle; pKFA = peak knee flexion angle; KFA = knee flexion angle; HFM = hip flexion moment; KFM = knee flexion moment; WA = weight acceptance (ie, pKFA – initial contact); MS = midstance (ie, peak knee extension angle – pKFA).
When comparing the interlimb difference in mean UN and INV limbs within each group, gait asymmetries existed in both SAP and SAP+PERT groups, but were more prevalent at 1 year versus 2 years postoperatively regardless of group (Table 4). Both groups walked with similar hip (Fig. 2A–B) but smaller knee excursions (Fig. 2C–D) during weight acceptance and clinically smaller hip (Fig. 3A–B) and smaller knee (Fig. 3C–D) excursions during midstance in the involved versus uninvolved limb. Post hoc t-tests revealed meaningful [13] interlimb mean differences at 1 year postoperatively for knee excursions during weight acceptance (SAP: UN 18° ± 3° versus INV 14° ± 4°, mean interlimb difference [95% CI]: 4° [1° to 7°], p = 0.004; SAP+PERT: UN 18° ± 3° versus INV 15° ± 4°, mean interlimb difference [95% CI]: 3° [1° to 5°], p = 0.007) and midstance (SAP: UN 19° ± 5° versus INV 15° ± 5°, mean interlimb difference [95% CI]: 4° [1° to 8°], p = 0.019; SAP+PERT: UN 21° ± 4° versus INV 16° ± 5°, mean interlimb difference [95% CI]: 5° [2° to 8°], p = 0.002). At 1 year postoperatively, SAP athletes walked with smaller hip excursion during midstance (SAP: UN 34° ± 6° versus INV 30° ± 6°, mean interlimb difference [95% CI]: 5° [0° to 9°], p = 0.031), whereas SAP+PERT athletes tended to walk with clinically smaller hip excursions during midstance (SAP+PERT: UN 34° ± 5° versus INV 31° ± 5°, mean interlimb difference [95% CI]: 3° [0° to 6°], p = 0.065). At 2 years followup, hip and knee excursions were clinically asymmetrical for only the SAP group’s hip (UN 33° ± 6° versus INV 29° ± 5°; mean interlimb difference: 3°; 95% CI, 0° to 7°; p = 0.083) and the SAP+PERT group’s knee (UN 18° ± 4° versus INV 15° ± 4°; mean interlimb difference: 3°; 95% CI, 0° to 6°; p = 0.024) during midstance. Pooling across groups, athletes walked with smaller peak knee flexion angles in their involved versus uninvolved limbs; they also walked with smaller sagittal plane hip and knee moments in their involved versus uninvolved limbs at peak knee extension angle.
Table 4.
Sagittal plane interlimb asymmetries (determined by the difference in the mean values of the uninvolved and involved limbs for each group) exceeding MCID values [31] existed across both groups, as indicated by the check marks (√)*
| Variable | One year | Two years | |||
|---|---|---|---|---|---|
| SAP | SAP+PERT | SAP | SAP+PERT | ||
| pKFA | Hip flexion angle | ||||
| Hip extension moment | |||||
| Knee flexion angle | √ | ||||
| Knee extension moment | √ | ||||
| Hip excursion: weight acceptance | |||||
| Knee excursion: weight acceptance | √ | √ | |||
| Hip excursion: midstance | √ | √ | √ | ||
| Knee excursion: midstance | √ | √ | √ | ||
*Note the larger number of asymmetries that was present at 1 versus 2 years postoperatively; MCID = minimal clinically important difference; SAP = strength, agility, and secondary prevention treatment group; SAP+PERT = SAP + perturbation training group; pKFA = peak knee flexion angle.
Fig. 2A–D.
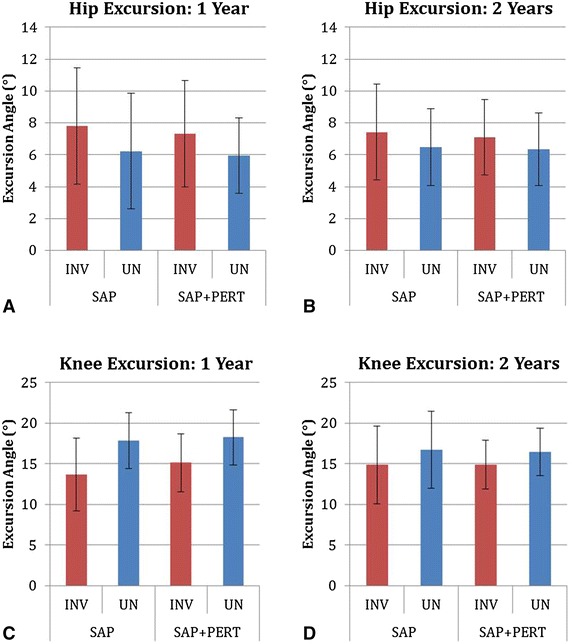
These figures display the mean sagittal plane hip (A–B) and knee (C–D) excursions during weight acceptance at 1 (A, C) and 2 (B, D) years postoperatively (whiskers are SDs). Both SAP and SAP+PERT athletes walked with meaningfully smaller knee excursions during weight acceptance at 1 year postoperatively.
Fig. 3A–D.

These figures display the mean sagittal plane hip (A–B) and knee (C–D) excursions during midstance at 1 (A, C) and 2 (B, D) years postoperatively (whiskers are SDs). Both SAP and SAP+PERT athletes walked with meaningfully smaller hip and knee excursions during midstance at 1 year postoperatively; however, at 2 years, only SAP athletes walked with meaningfully smaller hip excursions and only SAP+PERT athletes walked with meaningfully smaller knee excursions when comparing differences in mean values.
Discussion
Movement asymmetries during walking are prevalent after ACL injury and reconstruction and may increase the risk of posttraumatic osteoarthritis (OA) early after ACLR [6, 41]. Previous research has found that a specialized type of neuromuscular training (ie, perturbation training) improves gait asymmetries and functional outcomes when applied to ACL-deficient patients [8, 10, 13, 15, 20]. However, movement asymmetries exist after ACLR even in individuals who had preoperative perturbation training and postoperative physical therapy [10, 20, 36]. Thus, additional training is likely needed to restore movement symmetry during gait. However, the effect of postoperative perturbation training on gait mechanics is previously unknown. Therefore, we conducted a randomized controlled trial to compare SAP with SAP+PERT training. We found no difference between SAP and SAP+PERT training on the gait mechanics or resolution of gait asymmetries in men after ACLR, and both groups walked with meaningful gait asymmetries 1 and 2 years postoperatively.
There are several limitations to consider when interpreting the results of our study. The primary limitation of this study is that we only included men in this analysis; thus, the effect of SAP and SAP+PERT training on the gait mechanics of women is unknown. We are currently recruiting our final female participants for this study and plan to analyze and report these outcomes once enrollment and testing are complete. We also did not include the pretraining and posttraining data from our male participants; thus, we do not know what their gait mechanics were before and immediately after SAP or SAP+PERT training, and the present study is unable to quantify the pre- to post-changes or immediate effects of SAP versus SAP+PERT training on gait mechanics. We will analyze the pretraining and posttraining time points for both men and women once all women have completed training. Additionally, all participants were Level I/II (that is, jumping, cutting, and pivoting) [9, 22] athletes; thus, it is unknown whether our findings are applicable to less athletic populations. However, the majority of individuals who tear their ACL do so in Level I/II [9, 22] sports. Our findings also may not apply to individuals with severe concomitant injuries (eg, large osteochondral defects, multiple ligament injury, previous ACL injury) given our exclusion criteria; by excluding these patients, however, we created a more homogenous cohort for randomization and analysis. We did not standardize surgical method (performed by 21 different surgeons); thus, we do not know what effect surgical technique may have had on our findings. However, because we randomized our subjects to treatment group, the findings should be more generalizable across surgical intervention. Finally, we did not analyze electromyographic data or use musculoskeletal modeling [5, 29] to estimate joint contact forces, which have implications for the development of OA [27, 41]. Further analysis is warranted.
Our findings suggest that SAP+PERT training does not alter gait mechanics in men 1 or 2 years after ACLR compared with SAP training alone. Although the authors are unaware of any prior study investigating the effect of postoperative SAP versus SAP+PERT training on gait mechanics after ACLR, previous studies have investigated preoperative perturbation training on gait mechanics [8, 13, 15, 20, 25]. In these prior studies, changes in gait from pre- to post-intervention occurred; however, these changes were more prevalent among women, who, as compared with men and healthy control subjects, demonstrated a more impaired gait strategy (including smaller knee flexion angles [8] and muscle activation imbalances [25]) before training [8, 13, 20, 25]. In contrast to the changes seen among ACL-deficient women, ACL-deficient men walked with similar gait patterns before and after preoperative perturbation training [13]. Moreover, men who received preoperative strength training and physical therapy with or without perturbation training walked with stable and persistent truncated knee excursions pre- and post-intervention (before surgery) and 6 months after ACLR [10]. Similarly, in another study by Risberg et al. [35], lower extremity biomechanics in ACL-injured patients were largely unchanged even after 20 rehabilitation sessions including neuromuscular and strength training: smaller knee excursions persisted in both walking and hopping despite improvements in functional outcomes. Current rehabilitation programs may not be effective at changing gait, which is an automatic activity that may be resistant to change [10, 14, 35]. Future work should investigate the pre- to post-intervention effects of SAP versus SAP+PERT training, these programs on the gait mechanics of women, and novel paradigms to improve gait mechanics after ACLR.
There were no differences between SAP and SAP+PERT groups regarding the elimination of gait asymmetries at 1 or 2 years postoperatively, and clinically meaningful asymmetries existed to a large degree in both groups at both time points. The presence of gait asymmetries among individuals after ACLR is consistent with previous work [12, 16, 19, 20, 36, 41, 43]. Previous work has shown that limb asymmetries are prevalent in the short and medium term after ACLR [12, 16, 19, 20, 36, 41, 43], persist in both ACL-injured and ACL-reconstructed athletes despite rehabilitation programs including preoperative perturbation training [10, 13] and postoperative strengthening and neuromuscular rehabilitation [35], and may continue up to 2 years postoperatively [36]. The present study corroborates these findings and underscores that limb asymmetries remain present 2 years postoperatively even among individuals who are well rehabilitated after ACLR and have returned to sports [1]. The present study adds to a growing body of rehabilitation paradigms that have not succeeded in restoring gait symmetry [10, 21, 35]. Notably, gait asymmetries (including smaller INV versus UN limb knee flexion angles) persisted among patients after ACLR even when towing a sled or wearing a weighted vest [21]. Interestingly, previous studies have typically evaluated gait mechanics in the short and medium term by comparing group means rather than the proportion of individuals who walk with clinically meaningful asymmetries, as was done in the present study. By comparing the proportions of individual athletes who walked asymmetrically (Table 3) with the presence of meaningful asymmetries in group means (Table 4), it is apparent that many athletes in both the SAP and SAP+PERT groups walked asymmetrically despite generally symmetric means when pooling limb data across groups. These findings suggest that meaningful asymmetries may be even more present than once thought, even among participants who were functioning at a high level. Further development of rehabilitation paradigms is likely necessary to restore gait symmetry after ACLR, but further investigation to identify an effective program is needed.
Our findings suggest that a postoperative strength, agility, and secondary prevention training program with or without perturbation training is not effective at ameliorating gait asymmetries in men 1 or 2 years after ACLR. Moreover, regardless of treatment group, meaningful interlimb asymmetries persisted during gait at both 1 and 2 years after ACLR. Interestingly, by comparing the proportion of athletes who walked with interlimb asymmetries as well as each group’s mean, our findings suggest that interlimb asymmetries may be even more ubiquitous when comparing individuals versus group means. Although impaired gait patterns may be more prevalent among those with poorer functional and clinical performance [2, 12, 17, 41, 43], gait impairments may be present even in the absence of functional or clinical deficits [24, 43]. Therefore, although neither of the rehabilitation paradigms tested in the present study (SAP or SAP+PERT) restored gait symmetry or altered gait mechanics 1 or 2 years after ACLR, there may be other benefits to these programs. Previous work suggests neuromuscular training programs may be efficacious in improving functional performance and patient-reported outcomes [7, 31, 33, 35, 39] and facilitating return to sport while lowering second injury risk [11, 23, 44]. Future work should not only further investigate the functional, clinical, and biomechanical outcomes of SAP versus SAP+PERT training and compare them with outcomes of other programs and no additional training, but also explore new interventions to improve gait mechanics and ameliorate gait asymmetry in athletes after ACLR.
Acknowledgments
The authors thank Angela Hutchinson Smith PT, DPT, OCS, SCS, ATC, Martha Callahan, and the Delaware Rehabilitation Institute Research Core for their assistance with participant recruitment and retention; Celeste Dix for her assistance with data processing; Ashutosh Khandha PhD, for his assistance with figure preparation; the University of Delaware Physical Therapy Clinic; and the National Institutes of Health.
Footnotes
This project was funded by the following National Institutes of Health grants: R01-AR048212, P30-GM103333, U54-GM104941 (LS-M), and T32-HD00749 (JJC). In addition, one of the author’s (AA) work was supported in part by a Promotion of Doctoral Studies (PODS)–Level I Scholarship from the Foundation for Physical Therapy. ClinicalTrials.gov Identifier: NCT01773317.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Delaware, Newark, DE, USA.
References
- 1.Arundale AJH, Cummer K, Capin JJ, Zarzycki R, Snyder-Mackler L. Report of the Clinical and Functional Primary Outcomes in Men of the ACL-SPORTS Trial: Similar Outcomes in Men Receiving Secondary Prevention With and Without Perturbation Training 1 and 2 Years After ACL Reconstruction. Clin Orthop Relat Res. 2017; February. DOI 10.1007/s11999-017-5280-2. [DOI] [PMC free article] [PubMed]
- 2.Abourezk MN, Ithurburn MP, McNally MP, Thoma LM, Briggs MS, Hewett TE, Spindler KP, Kaeding CC, Schmitt LC. Hamstring strength asymmetry at 3 years after anterior cruciate ligament reconstruction alters knee mechanics during gait and jogging. Am J Sports Med. 2017;45:97–105. doi: 10.1177/0363546516664705. [DOI] [PubMed] [Google Scholar]
- 3.Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009;91:95–101. doi: 10.2106/JBJS.H.01408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buchanan TS, Lloyd DG, Manal K, Besier TF. Neuromusculoskeletal modeling: estimation of muscle forces and joint moments and movements from measurements of neural command. J Appl Biomech. 2004;20:367–395. doi: 10.1123/jab.20.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler RJ, Minick KI, Ferber R, Underwood F. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43:366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 7.Chappell JD, Limpisvasti O. Effect of a neuromuscular training program on the kinetics and kinematics of jumping tasks. Am J Sports Med. 2008;36:1081–1086. doi: 10.1177/0363546508314425. [DOI] [PubMed] [Google Scholar]
- 8.Chmielewski TL, Hurd WJ, Rudolph KS, Axe MJ, Snyder-Mackler L. Perturbation training improves knee kinematics and reduces muscle co-contraction after complete unilateral anterior cruciate ligament rupture. Phys Ther. 2005;85:740–754. [PubMed] [Google Scholar]
- 9.Daniel DM, Stone M. Lou, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 10.Di Stasi S, Hartigan EH, Snyder-Mackler L. Sex-specific gait adaptations prior to and up to 6 months after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45:207–214. doi: 10.2519/jospt.2015.5062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43:777–792. doi: 10.2519/jospt.2013.4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41:1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Stasi SL, Snyder-Mackler L. The effects of neuromuscular training on the gait patterns of ACL-deficient men and women. Clin Biomech. 2012;27:360–365. doi: 10.1016/j.clinbiomech.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eitzen I, Fernandes L, Nordsletten L, Risberg MA. No effects of a 12-week supervised exercise therapy program on gait in patients with mild to moderate osteoarthritis: a secondary analysis of a randomized trial. J Negat Results Biomed. 2015;14:1–11. doi: 10.1186/s12952-015-0023-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Phys Ther. 2000;80:128–140. [PubMed] [Google Scholar]
- 16.Gardinier ES, Di Stasi S, Manal K, Buchanan TS, Snyder-Mackler L. Knee contact force asymmetries in patients who failed return-to-sport readiness criteria 6 months after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:2917–2925. doi: 10.1177/0363546514552184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gardinier ES, Manal K, Buchanan TS, Snyder-Mackler L. Clinically-relevant measures associated with altered contact forces in patients with anterior cruciate ligament deficiency. Clin Biomech. 2014;29:531–536. doi: 10.1016/j.clinbiomech.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hart JM, Ko JW, Konold T, Pietrosimone B. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech. 2010;25:277–283. doi: 10.1016/j.clinbiomech.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27:724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hartigan E, Lawrence M, Murray T, Shaw B, Collins E, Powers K, Townsend J. Biomechanical profiles when towing a sled and wearing a weighted vest once cleared for sports post-ACL reconstruction. Sports Health. 2016;8:456–464. doi: 10.1177/1941738116659855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 23.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:216–224. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 25.Hurd WJ, Chmielewski TL, Snyder-Mackler L. Perturbation-enhanced neuromuscular training alters muscle activity in female athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:60–69. doi: 10.1007/s00167-005-0624-y. [DOI] [PubMed] [Google Scholar]
- 26.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Khandha A, Manal K, Wellsandt E, Capin J, Snyder-Mackler L, Buchanan TS. A comparison of knee gait mechanics in subjects with and without medial compartment knee osteoarthritis five years after anterior cruciate ligament reconstruction. J Orthop Res. 2016 Apr 15. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 28.Labanca L, Laudani L, Menotti F, Rocchi J, Mariani PP, Giombini A, Pigozzi F, Macaluso A. Asymmetrical lower extremity loading early after anterior cruciate ligament reconstruction is a significant predictor of asymmetrical loading at the time of return to sport. Am J Phys Med Rehabil. 2016;95:248–255. doi: 10.1097/PHM.0000000000000369. [DOI] [PubMed] [Google Scholar]
- 29.Manal K, Buchanan TS. An electromyogram-driven musculoskeletal model of the knee to predict in vivo joint contact forces during normal and novel gait patterns. J Biomed Eng. 2013;135:021014. doi: 10.1115/1.4023457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mather RC, 3rd, Koenig L, Kocher MS, Dall TM, Gallo P, Scott DJ, Bach BR., Jr Spindler KP; MOON Knee Group. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95:1751–1759. doi: 10.2106/JBJS.L.01705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meierbachtol A, Rohman E, Paur E, Bottoms J, Tompkins M. Quantitative improvements in hop test scores after a 6-week neuromuscular training program. Sports Health. 2016 Sep 12. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 32.Moisio KC, Sumner DR, Shott S, Hurwitz DE. Normalization of joint moments during gait: a comparison of two techniques. J Biomech. 2003;36:599–603. doi: 10.1016/S0021-9290(02)00433-5. [DOI] [PubMed] [Google Scholar]
- 33.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 34.Noyes F, Barber S, Mangine R. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 35.Risberg M, Moksnes H, Storevold A, Holm I, Snyder-Mackler L. Rehabilitation after anterior cruciate ligament injury influences joint loading during walking but not hopping. Br J Sports Med. 2009;43:423–428. doi: 10.1136/bjsm.2008.056846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44:1948–1953. doi: 10.1016/j.jbiomech.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saxby DJ, Bryant AL, Modenese L, Gerus P, Killen BA, Konrath J, Fortin K, Wrigley TV, Bennell KL, Cicuttini FM, Vertullo C, Feller JA, Whitehead T, Gallie P, Lloyd DG. Tibiofemoral contact forces in the anterior cruciate ligament-reconstructed knee. Med Sci Sports Exerc. 2016;48:2195–2206. doi: 10.1249/MSS.0000000000001021. [DOI] [PubMed] [Google Scholar]
- 38.Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Melick N, van Cingel REH, Brooijmans F, Neeter C, van Tienen T, Hullegie W, Nijhuis-van der Sanden MW. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506–1515. [DOI] [PubMed]
- 40.Webster KE, Feller JA. Alterations in joint kinematics during walking following hamstring and patellar tendon anterior cruciate ligament reconstruction surgery. Clin Biomech. 2011;26:175–180. doi: 10.1016/j.clinbiomech.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 41.Wellsandt E, Gardinier ES, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L. Decreased knee joint loading associated with early knee osteoarthritis after anterior cruciate ligament injury. Am J Sports Med. 2016;44:143–151. doi: 10.1177/0363546515608475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.White K, Di Stasi SL, Smith AH, Snyder-Mackler L. Anterior cruciate ligament-specialized post-operative return-to-sports (ACL-SPORTS) training: a randomized control trial. BMC Musculoskelet Disord. 2013;14:108. doi: 10.1186/1471-2474-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.White K, Logerstedt D, Snyder-Mackler L. Gait asymmetries persist 1 year after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2013;1:1–7. doi: 10.1177/2325967113496967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]


