Abstract
Background
Double-bundle anterior cruciate ligament (ACL) reconstruction has demonstrated improved biomechanical properties and moderately better objective outcomes compared with single-bundle reconstructions. This could make an impact on the rerupture rate and reduce the risk of revisions in patients undergoing double-bundle ACL reconstruction compared with patients reconstructed with a traditional single-bundle technique. The National Knee Ligament Registers in Scandinavia provide information that can be used to evaluate the revision outcome after ACL reconstructions.
Questions/purposes
The purposes of the study were (1) to compare the risk of revision between double-bundle and single-bundle reconstructions, reconstructed with autologous hamstring tendon grafts; (2) to compare the risk of revision between double-bundle hamstring tendon and single-bundle bone-patellar tendon-bone autografts; and (3) to compare the hazard ratios for the same two research questions after Cox regression analysis was performed.
Methods
Data collection of primary ACL reconstructions from the National Knee Ligament Registers in Denmark, Norway, and Sweden from July 1, 2005, to December 31, 2014, was retrospectively analyzed. A total of 60,775 patients were included in the study; 994 patients were reconstructed with double-bundle hamstring tendon grafts, 51,991 with single-bundle hamstring tendon grafts, and 7790 with single-bundle bone-patellar tendon-bone grafts. The double-bundle ACL-reconstructed patients were compared with the two other groups. The risk of revision for each research question was detected by the risk ratio, hazard ratio, and the corresponding 95% confidence intervals. Kaplan-Meier analysis was used to estimate survival at 1, 2, and 5 years for the three different groups. Furthermore, a Cox proportional hazard regression model was applied and the hazard ratios were adjusted for country, age, sex, meniscal or chondral injury, and utilized fixation devices on the femoral and tibial sides.
Results
There were no differences in the crude risk of revision between the patients undergoing the double-bundle technique and the two other groups. A total of 3.7% patients were revised in the double-bundle group (37 of 994 patients) versus 3.8% in the single-bundle hamstring tendon group (1952 of 51,991; risk ratio, 1.01; 95% confidence interval (CI), 0.73–1.39; p = 0.96), and 2.8% of the patients were revised in the bone-patellar tendon-bone group (219 of the 7790 bone-patellar tendon-bone patients; risk ratio, 0.76; 95% CI, 0.54–1.06; p = 0.11). Cox regression analysis with adjustment for country, age, sex, menisci or cartilage injury, and utilized fixation device on the femoral and tibial sides, did not reveal any further difference in the risk of revision between the single-bundle hamstring tendon and double-bundle hamstring tendon groups (hazard ratio, 1.18; 95% CI, 0.85–1.62; p = 0.33), but the adjusted hazard ratio showed a lower risk of revision in the single-bundle bone-patellar tendon-bone group compared with the double-bundle group (hazard ratio, 0.62; 95% CI, 0.43–0.90; p = 0.01). Comparisons of the graft revision rates reported separately for each country revealed that double-bundle hamstring tendon reconstructions in Sweden had a lower hazard ratio compared with the single-bundle hamstring tendon reconstructions (hazard ratio, 1.00 versus 1.89; 95% CI, 1.09–3.29; p = 0.02). Survival at 5 years after index surgery was 96.0% for the double-bundle group, 95.4% for the single-bundle hamstring tendon group, and 97.0% for the single-bundle bone-patellar tendon-bone group.
Conclusions
Based on the data from all three national registers, the risk of revision was not influenced by the reconstruction technique in terms of using single- or double-bundle hamstring tendons, although national differences in survival existed. Using bone-patellar tendon-bone grafts lowered the risk of revision compared with double-bundle hamstring tendon grafts. These findings should be considered when deciding what reconstruction technique to use in ACL-deficient knees. Future studies identifying the reasons for graft rerupture in single- and double-bundle reconstructions would be of interest to understand the findings of the present study.
Level of Evidence
Level III, therapeutic study.
Introduction
The purpose of double-bundle reconstruction is to better restore the anterior cruciate ligament (ACL) anatomy with regard to its two bundles, the anteromedial and the posterolateral bundles [9, 36]. It has been proposed that this reconstruction technique achieves higher coverage of the native ACL footprints and improves the rotational stability of the knee compared with the single-bundle reconstruction technique, although the technique is performed with higher costs and technical demands [22, 25, 30, 34]. Additionally, biomechanical studies have revealed higher ultimate failure loads and lower elongation in double-bundle compared with single-bundle grafts [18].
Several studies have published moderately better objective knee stability after double-bundle ACL reconstructions [10, 16, 29, 31]. Whether these improvements could prevent rerupturing of the graft and subsequently reduce the risk of revision is difficult to detect through a randomized controlled study approach. Previous studies looking at the rerupture rate of double-bundle compared with single-bundle reconstructions are influenced by inaccurate reporting, risk of bias, and small numbers from which to make inferences [23]. One systematic review of meta-analysis could not find any difference in graft reruptures between the two techniques, although other studies again have proclaimed that the double-bundle technique was associated with a lower incidence of graft reruptures and a lower risk of revision [20, 32, 33]. The double-bundle procedure has been performed in less than 2% of all ACL reconstructions in Scandinavia [12], but with the data from the three National Knee Ligament Registers in Scandinavia, the outcome of almost 1000 double-bundle reconstructions can be evaluated.
The purposes of the study were (1) to compare the risk of revision between double-bundle and single-bundle reconstructions, reconstructed with autologous hamstring tendon grafts; (2) to compare the risk of revision between double-bundle hamstring tendon grafts and single-bundle bone-patellar tendon-bone autografts; and (3) to compare the hazard ratios for the same two research questions after Cox regression analysis was performed.
Patients and Methods
The study included primary ACL-reconstructed patients registered in the National Knee Ligament Registers of Norway, Denmark, and Sweden. The inclusion period was from July 1, 2005, until December 31, 2014. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement was used as guidance when reporting the results [17]. Patients were excluded if they were reconstructed before or after the inclusion period or if they were younger than 15 years or older than 59 years. Patients undergoing other techniques than single- or double-bundle reconstruction were excluded. Also, patients reconstructed with other graft types than autologous hamstring and bone-patellar tendon-bone autografts were excluded. If reconstruction of the posterior cruciate ligament, lateral collateral ligament, medial collateral ligament, or of the posterolateral corner was performed in the same knee, the patients were excluded. Patients with contralateral ACL reconstruction were not excluded (Table 1). No censoring was done because of emigration or death. The National Knee Ligament Registers in Norway, Denmark, and Sweden are nationwide and cover more than 20 million people. Approximately 86% to 90% of the primary ACL reconstruction procedures performed in these three countries are recorded in those registers [1, 13, 28]. The registration form and data collection process have been described in detail in previous publications [1, 14, 19]. Any revision, defined as insertion of a new graft in a former primary ACL-reconstructed knee, was regarded as the final endpoint. This endpoint was followed continuously both for patients undergoing the single-bundle technique and those undergoing the double-bundle technique from index operation until revision or December 31, 2014, whichever came first. The revisions were reported to the register by the revising surgeon. In Denmark and Sweden, the double-bundle procedure has been registered since 2005; in Norway, the procedure has been registered since 2008. The single-bundle reconstructed patients were further stratified into two groups: autologous hamstring tendon and autologous bone-patellar tendon-bone groups. The reason for this was because the primary aim of the study was to compare the survival of two different reconstruction techniques, and the different graft types could further bias the outcome [12, 24, 27].
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria |
| Primary anterior cruciate ligament reconstruction |
| 15-59 years |
| Single- or double-bundle technique |
| Autologous HT or BPTB graft |
| Index and contralateral knee |
| Exclusion criteria |
| Concomitant PCL, LCL, PLC, or MCL reconstructions |
| Allografts or quadriceps grafts |
| Direct sutures |
HT = hamstring tendon; BPTB = bone-patellar tendon-bone; PCL = posterior cruciate ligament; LCL = lateral collateral ligament; PLC = posterolateral corner; MCL = medial collateral ligament.
Possible confounding factors were selected considering previous studies and data obtained from the registration forms. The selected variables were sex, age, the presence of meniscal or chondral injury at index operation, and the utilized fixation devices on the femoral and tibial sides [2, 3, 6]. Each fixation device was categorized into one of four different categories: “metal screw,” “biodegradable screw,” “button fixation” (extracortical suspensory device), and “other” fixation devices. The same categories were used for both the femoral and tibial sides. The categories were defined after their fixation level (aperture or extracortical) and material (biodegradable or metal) because these properties have been correlated with different biomechanical properties and also with a difference in the risk of revisions [8, 11, 21]. Age was classified as a categorical variable with four different age categories: 15 to 19 years, 20 to 24 years, 25 to 29 years, and 30 years and older, because the incidence of revision is known to be different in the younger age groups. Details about the meniscal injuries and their treatment were not further differentiated. Correspondingly, details about the reported chondral injuries and treatment were also not taken into account in the final analysis.
More than 98% of the primary ACL reconstructions performed in Scandinavia are done with autologous hamstring or bone-patellar tendon-bone grafts and the coverage and completeness of the data collection are known to be high [1, 12, 26, 35]. There are no competing national registers from other healthcare systems in those countries, both public and private health institutions deliver data to the same register. Transfer bias resulting from loss to follow-up, emigration, or death of the participants could lead to both under- and overestimation of the revision risk. Selection bias could also potentially affect the results because only 1% to 2% of all patients were registered as double-bundle-reconstructed patients. To diminish this sort of bias, the most important confounders were detected and implemented in multivariate regression analysis. The main reason for revision surgery should be a nonfunctional graft, but graft revisions in knees with a functional graft could have been performed and would consequently bias the results. Also, information bias from the reporting surgeon could exist and lead to underestimating of the true revision rate.
Only 1% to 2% of all patients have received a double-bundle reconstruction during the study period. Power calculation was performed, and found in order to detect a decrease in the revision rate from 0.06% to 0.04% with a double-bundle reconstruction, 1000 double-bundle patients and 52,000 control patients, would be needed to be able to reject the null hypothesis with a power of 0.80 and a Type I error probability of 0.05. An uncorrected chi square statistic was used for this power calculation.
A total of 68,636 patients underwent a primary reconstruction of their ACL during the study period, and 60,775 of these patients met the inclusion criteria: 994 double-bundle grafts, 51,991 single-bundles with hamstring tendon autografts, and 7790 single bundles with bone-patellar tendon-bone autografts (Fig. 1). The three groups were differently distributed within each country: Sweden had a higher incidence of double-bundle reconstructions and Norway had a higher incidence of bone-patellar tendon-bone graft reconstructions than the other countries during the study period (Fig. 2). Patient characteristics and baseline data were compared within the three groups. The double-bundle group consisted of a higher percentage of men (63.9% compared with 58.2%; p < .001) and a higher proportion of patients with reported chondral injuries compared with the single-bundle hamstring tendon group (27.7% versus 21.6%; p < .001). Compared with the bone-patellar tendon-bone group, the double-bundle group were younger, and had a higher percentage of patients with reported chondral injuries (27.7% versus 20.0%; p < .001) (Table 2).
Fig. 1.
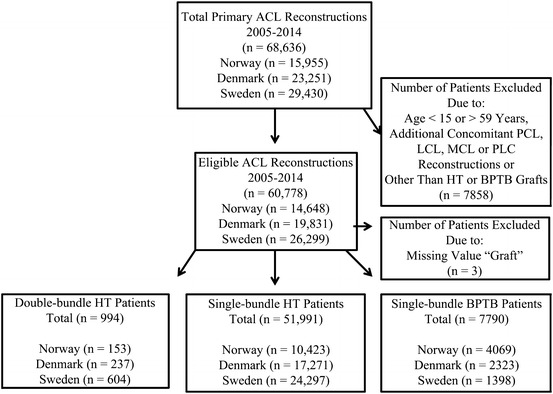
A flowchart of all primary ACL reconstructions recorded in the National Knee Ligament Registers of Norway, Denmark, and Sweden is shown. PCL = posterior cruciate ligament; LCL = lateral collateral ligament; MCL = medial collateral ligament; PLC = posterolateral corner; HT = hamstring tendon; BPTB = bone-patellar tendon-bone.
Fig. 2.
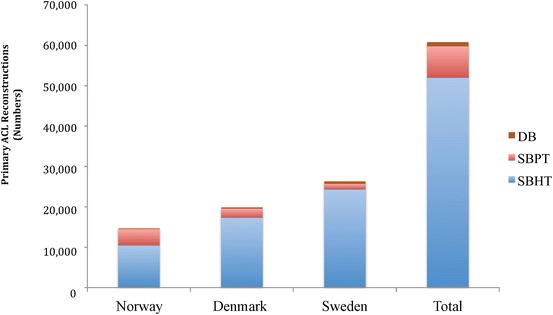
The frequency of primary ACL reconstructions in the three Scandinavian countries is shown. DB = double-bundle hamstring tendon graft; SBPT = single-bundle bone-patellar tendon-bone graft; SBHT = single-bundle hamstring tendon graft.
Table 2.
Baseline demographics and surgical characteristics of the study groups: double-bundle (DB) hamstring tendon (HT), single-bundle HT (SBHT), and single-bundle bone-pateller tendon-bone (BPTB) group
| Demographics and surgical characteristics | Double-bundle HT (n = 994) | Single-bundle HT (n = 51,991) | p value (DB versus SBHT) | Single-bundle BPTB (n = 7790) | p value (DB versus SBPT) |
|---|---|---|---|---|---|
| Age (years), number (%) | |||||
| 15–19 | 232 (23.3) | 12,751 (24.5) | 1748 (22.4) | ||
| 20–24 | 222 (22.3) | 10,891 (20.9) | 1532 (19.7) | ||
| 25–29 | 154 (15.5) | 7895(15.2) | 1231 (15.8) | ||
| 30+ | 386 (38.8) | 20,454 (39.3) | 3279 (42.1) | ||
| Mean age (years) ± SD | 28.0 ± 9.59 | 28.2 ± 10.07 | 0.45† | 28.8 ± 10.06 | 0.02 † |
| Sex, number (% male) | 635 (63.9) | 30,257 (58.2) | <0.001 * | 4866 (62.5) | 0.38* |
| Side, number (% right) | 519 (52.2) | 26,628 (51.2) | 0.54* | 4019 (51.6) | 0.71* |
| Meniscal injury, number (% yes) | 478 (48.1) | 23,166 (44.6) | 0.27* | 3549 (45.6) | 0.13* |
| Chondral injury, number (% yes) | 275 (27.7) | 11,252 (21.6) | <0.001 * | 1561 (20.0) | <0.001 * |
| Time from surgery to revision (months) | |||||
| Mean ± SD | 31.75 ± 17.95 | 27.62 ± 18.83 | <0.001 † | 35.02 ± 21.14 | <0.001 † |
| Median | 27 | 22 | 30 | ||
| Fixation femur, number (%) (n = 60,515, missing n = 263) | |||||
| Metal screw (n = 9788) | 220 (22.1) | 3118 (6.0) | 6450 (82.8) | ||
| Bioscrew (n = 766) | 15 (1.5) | 570 (1.1) | 181 (2.3) | ||
| Button (n = 24,872) | 357 (35.9) | 24,306 (46.8) | 209 (2.7) | ||
| Other (n = 25,089) | 399 (40.1) | 23,759 (45.7) | 931 (12.0) | ||
| Fixation tibia, number (%) (n = 60,331, missing n = 447) | |||||
| Metal screw (n = 17,564) | 258 (26.0) | 11,122 (21.4) | 6184 (79.4) | ||
| Bioscrew (n = 10,859) | 400 (40.2) | 10,206 (19.6) | 253 (3.2) | ||
| Button (n = 1035) | 9 (0.9) | 1025 (2.0) | 1 (0.0) | ||
| Other (n = 30,873) | 306 (30.8) | 29,233 (56.2) | 1334 (17.1) | ||
Bold values indicate statistical significance (p < 0.05)
*Pearson’s chi-square test; † independent samples t-test; NS = nonsignificant.
In Denmark, Danish law assured that ACL-reconstructed patients are registered without the need for additional consent forms. For participants in Norway and Sweden, registration is voluntary. Approval for the utilization of the register data was applied for through the Regional Committees for Medical Research Ethics-South East Norway (Norwegian RIB No. 2015/922). Also, the respective boards of the Knee Ligament Registers in Denmark, Norway, and Sweden were informed and approved for the study to be done.
Statistical Analysis
A combined file of the data sets from all three countries was obtained and processed into an SPSS Statistics (IBM® SPSS® Inc, New York, NY, USA) software program. The risk of revision in the single-bundle hamstring and single-bundle bone-patellar tendon-bone reconstructions were compared with the double-bundle-reconstructed group. The survival estimates at 1, 2, and 5 years and the cumulative survival were detected in each group using a Kaplan-Meier survival table. Cox regression analysis was performed and the outcome was expressed with hazard ratios and their 95% confidence intervals and the respective p value with adjustment for possible confounding. Furthermore, the interaction term was introduced between country and graft in the Cox regression model and comparisons of the revision rates of the grafts could be reported separately within each country. Demographic and baseline data between the groups were reported. The categorical data in each group were calculated in counts and percentages and their proportions compared by Pearson’s chi-square test. For continuous data, means ± standard deviations (SD) were presented and the independent samples t-test was used for comparison of the groups. Probability values < 0.05 were considered significant.
Results
There were no difference in the crude risk of revision between the double-bundle and single-bundle hamstring tendon groups (3.7% of the patients in the double-bundle group (37 of 994) versus 3.8% in the single-bundle hamstring tendon group (1952 of 51,991); risk ratio, 1.01; 95% confidence interval (CI), 0.73–1.39; p = 0.96). Multivariate analyses adjusted for country, age, gender, menisci or cartilage injury, and utilized fixation devices did not reveal any further difference in risk of revision between the two groups (hazard ratio, 1.18; 95% CI, 0.85–1.62; p = 0.33 unadjusted; hazard ratio, 1.24; 95% CI, 0.89–1.72; p = 0.20 after adjustment) (Table 3; Fig. 3). Although comparisons of the graft revision rates reported separately for each country revealed that double-bundle hamstring tendon reconstructions in Sweden had a lower hazard ratio compared with the single-bundle hamstring tendon reconstructions in Sweden (hazard ratio, 1.00 versus 1.89; 95% CI, 1.09-3.29; p = 0.02) (Fig. 4A–C; Table 4).
Table 3.
Cox regression analysis with crude and adjusted hazard ratios of double-bundle (DB), single-bundle hamstring tendon (SBHT), and single-bundle bone patellar tendon-bone (SB BPTB) grafts and other covariates
| Covariate | Number | Revisions (%) | HR (crude) | CI | p value | HR (adjusted) | CI | p value |
|---|---|---|---|---|---|---|---|---|
| Graft | ||||||||
| DB | 994 | 37 (3.7) | 1 | 1 | ||||
| SBHT | 51,991 | 1952 (3.8) | 1.18 | 0.85–1.62 | 0.33 | 1.24 | 0.89–1.72 | 0.20 |
| SB BPTB | 7790 | 219 (2.8) | 0.77 | 0.55–1.10 | 0.15 | 0.62 | 0.43–0.90 | 0.01 |
| Missing | 3 | |||||||
| Sex | ||||||||
| Male | 35,759 | 1223 (3.4) | 1 | |||||
| Female | 25,019 | 985 (3.9) | 0.95 | 0.87–1.04 | 0.27 | |||
| Age group (years) | ||||||||
| 14–19 | 14,733 | 985 (6.7) | 1 | |||||
| 20–24 | 12,645 | 568 (4.5) | 0.69 | 0.62–0.77 | <0.001 | |||
| 25–29 | 9280 | 252 (2.7) | 0.39 | 0.34–0.45 | <0.001 | |||
| 30–60 | 24,120 | 403 (1.7) | 0.23 | 0.21–0.26 | <0.001 | |||
| Country | ||||||||
| Norway | 14,648 | 613 (4.2) | 1 | |||||
| Denmark | 19,831 | 727 (3.7) | 0.94 | 0.84–1.06 | 0.32 | |||
| Sweden | 26,299 | 868 (3.3) | 0.69 | 0.62–0.77 | <0.001 | |||
| Meniscal injury | ||||||||
| No | 33,584 | 1257 (3.7) | 1 | |||||
| Yes | 27,194 | 951 (3.5) | 0.97 | 0.89–1.06 | 0.53 | |||
| Cartilage injury | ||||||||
| No | 47,689 | 1866 (3.9) | 1 | |||||
| Yes | 13,089 | 342 (2.6) | 0.94 | 0.83–1.06 | 0.29 | |||
| Fixation femur | ||||||||
| Metal screw | 9788 | 357 (3.6) | 1 | |||||
| Bioscrew | 766 | 33 (4.3) | 0.80 | 0.55–1.17 | 0.26 | |||
| Button | 24,872 | 906 (3.6) | 0.81 | 0.68–0.96 | 0.01 | |||
| Other | 25,089 | 902 (3.6) | 0.59 | 0.50–0.71 | <0.001 | |||
| Missing | 263 | |||||||
| Fixation tibia | ||||||||
| Metal screw | 17,564 | 609 (3.5) | 1 | |||||
| Bioscrew | 10,859 | 399 (3.7) | 1.18 | 1.03–1.36 | 0.02 | |||
| Button | 1035 | 13 (1.3) | 1.57 | 0.90–2.74 | 0.11 | |||
| Other | 30,873 | 1171 (3.8) | 1.13 | 1.00–1.27 | 0.04 | |||
| Missing | 447 |
Bold values indicate statistical significance (p < 0.05)
HR = hazard ratio; CI = confidence interval.
Fig. 3.
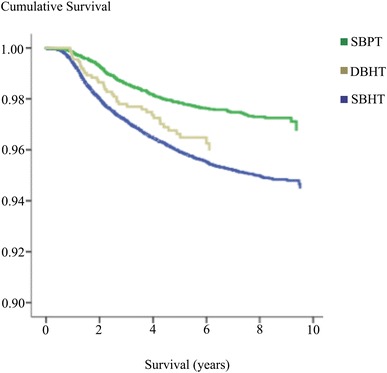
A Kaplan–Meier survival plot shows the cumulative risk of revision for single- and double-bundle ACL reconstructions in Scandinavia, 2005–2014.
Fig. 4A–C.
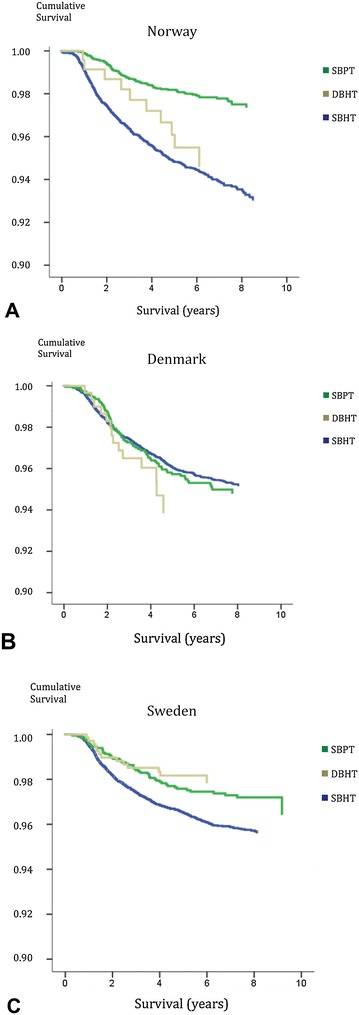
(A) The cumulative survival function at a mean of covariates in Norway. (B) The cumulative survival function at a mean of covariates in Denmark. (C) The cumulative survival function at a mean of covariates in Sweden.
Table 4.
Cox regression model reported separately for each country
| Graft | Norway | Denmark | Sweden | ||||||
|---|---|---|---|---|---|---|---|---|---|
| HR (adjusted with interaction) | CI | p value | HR (adjusted with interaction) | CI | p value | HR (adjusted with interaction) | CI | p value | |
| DB | 1 | 1 | 1 | ||||||
| SBHT | 1.15 | 0.61–2.15 | 0.67 | 0.71 | 0.42–1.20 | 0.20 | 1.89 | 1.09–3.29 | 0.02 |
| SBPT | 0.42 | 0.21–0.81 | 0.01 | 0.42 | 0.24–0.76 | 0.004 | 1.33 | 0.72–2.46 | 0.37 |
Bold values indicate statistical significance (p < 0.05)
HR = hazard ratio; CI = confidence interval; DB = double-bundle hamstring tendon grafts; SBHT = single-bundle hamstring tendon graft; SBPT = single-bundle bone-patellar tendon-bone graft.
A total of 3.7% patients were revised in the double-bundle group (37 of 994) versus 2.8% of the patients in the bone-patellar tendon-bone group (219 of 7790; risk ratio, 0.76; 95% CI, 0.54–1.06; p = 0.11). The applied Cox regression analysis revealed a decreased risk of revision between the bone-patellar tendon-bone group and the double-bundle group (hazard ratio, 0.62; 95% CI, 0.43–0.90; p = 0.01) (Table 3).
Survival at 5 years after index surgery was 96.0% for the double-bundle group, 95.4% for the single-bundle hamstring tendon group, and 97.0% for the single-bundle bone-patellar tendon-bone group (Table 5).
Table 5.
Graft survival 1, 2, and 5 years after index surgery for double-bundle (DB), single-bundle hamstring tendon (SBHT), and single-bundle bone-patellar tendon-bone (BPTB) graft reconstruction
| Graft | 1 year | 2 years | 5 years |
|---|---|---|---|
| DB | 99.6% | 98.4% | 96.0% |
| SBHT | 99.3% | 97.7% | 95.4% |
| SBPT | 99.8% | 99.0% | 97.0% |
Discussion
There has been debate whether the introduction of the double-bundle ACL reconstruction technique, could decrease the amount of patients needing revision surgery. The risk of revision within this subgroup has been difficult to detect without large cohort studies. With this study the authors were able to compare the risk for revision between the single- and double-bundle reconstruction techniques in a cohort of more than 60,000 patients. The most important finding of this study was that the risk of revision was not influenced by the reconstruction technique in terms of using the single- or double-bundle technique, whereas the use of the bone-patellar tendon-bone technique seemed to decrease the risk in future revision surgery compared with both hamstring tendon groups.
There are some limitations to consider when conducting a study on register information. First, the double-bundle cohort could potentially be affected by selection bias because only 1% to 2% of all the recorded patients received this operation. To perform regression analysis would help to prevent such bias, but not all of the underlying factors that were involved when selecting the patients are known. If the surgeons use this method only for a selected group of patients, this could further lead to a closer follow-up and earlier detection of graft reruptures. On the contrary, a higher threshold to recommend revision surgery in double-bundle-reconstructed patients could exist because of the extent of bone loss at both sides of the joint. Also, the reported revision rate is the “best case scenario” and the real incidence of graft rerupturing is thought to be higher because not all patients with a nonfunctioning graft would go further and do a revision procedure. Of the eligible population, 86% to 90% were recorded in the national registers during the last years, although this coverage was lower during the first years after initiation of the registers [26]. This could potentially underestimate the revision rates in both groups. Also, the fact that there was no censoring for emigrated or dead participants could affect the results and underestimate the true risk of revision in the target population. Finally, not all variables that could influence the outcome after ACL reconstruction are registered through the Knee Ligament Registers. The preoperative level of activity, quality of the postoperative physical rehabilitation, psychologic aspects of the patients, and clinical and radiographic findings are not detected, but are still important factors concerning ACL outcome and graft survival [4, 15]. Other factors known to affect the revision outcome such as body mass index and the use of nicotine were not included in the final analysis due to the high rate of nonresponders for this outcome [2, 3, 12].
Previous research comparing the revision outcome of single-bundle versus the double-bundle technique have been inconclusive. Two systematic reviews proclaimed that double-bundle reconstruction protected against repeated graft rupture [7, 33]. On the contrary, one study found an increased number of graft reruptures in double-bundle-reconstructed knees detected by second-look arthroscopy and a meta-analysis of 15 systematic review papers could not find any difference in graft rerupture rates between the anatomic single- and anatomic double-bundle reconstructions [5, 10]. The findings from this meta-analysis are consistent with the results in this study. Further, a recent study from the Swedish Knee Ligament Register revealed a lower risk of revision in double-bundle-reconstructed knees compared with other reconstruction techniques in Sweden [32]. In this study the same national differences were detected and the lower risk of revision in double-bundle grafts in Sweden still existed after multivariate regression analysis was performed. As this study design could only be hypothesis-generating and not explanatory for this outcome, the reasons for these geographic differences should be looked at in future studies. In the present study, patients reconstructed with single-bundle bone-patellar tendon-bone grafts revealed a decreased risk of revision compared with patients in the hamstring tendon groups. Previous research has proclaimed a similar tendency towards improved survival in bone-patellar tendon-bone reconstructions [12, 23, 24, 27].
In conclusion, based on the data from three national registers, the risk of revision was not influenced by the reconstruction technique in terms of using single- or double-bundle hamstring tendons, although national differences existed. Using bone-patellar tendon-bone grafts lowered the risk of revision compared with double-bundle hamstring tendon grafts. These findings should be considered when deciding what reconstruction technique to use in ACL-deficient knees. Future studies identifying the reasons for graft rerupturing in single- and double-bundle reconstructions would be of interest to understand the findings of the present study.
Acknowledgments
We would like to thank the staff of the Norwegian, Swedish, and Danish Knee Ligament Registers for their contributions with the data for this study.
Footnotes
One of the authors (CA) has received a grant from the Norwegian authorities (Health South-Eastern Norway).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Martina Hansens Hospital, Bærum, Norway.
References
- 1.Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230–2235. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 2.Andernord D, Bjornsson H, Petzold M, Eriksson BI, Forssblad M, Karlsson J, Samuelsson K. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42:1574–1582. doi: 10.1177/0363546514531396. [DOI] [PubMed] [Google Scholar]
- 3.Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43:121–127. doi: 10.1177/0363546514552788. [DOI] [PubMed] [Google Scholar]
- 4.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 5.Asagumo H, Kimura M, Kobayashi Y, Taki M, Takagishi K. Anatomic reconstruction of the anterior cruciate ligament using double-bundle hamstring tendons: surgical techniques, clinical outcomes, and complications. Arthroscopy. 2007;23:602–609. doi: 10.1016/j.arthro.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Bjornsson H, Andernord D, Desai N, Norrby O, Forssblad M, Petzold M, Karlsson J, Samuelsson K. No difference in revision rates between single- and double-bundle anterior cruciate ligament reconstruction: a comparative study of 16,791 patients from the Swedish national knee ligament register. Arthroscopy. 2015;31:659–664. doi: 10.1016/j.arthro.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 7.Bjornsson H, Desai N, Musahl V, Alentorn-Geli E, Bhandari M, Fu F, Samuelsson K. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:696–739. doi: 10.1007/s00167-013-2666-x. [DOI] [PubMed] [Google Scholar]
- 8.Brand J, Jr, Weiler A, Caborn DN, Brown CH, Jr, Johnson DL. Graft fixation in cruciate ligament reconstruction. Am J Sports Med. 2000;28:761–774. doi: 10.1177/03635465000280052501. [DOI] [PubMed] [Google Scholar]
- 9.Cha PS, Brucker PU, West RV, Zelle BA, Yagi M, Kurosaka M, Fu FH. Arthroscopic double-bundle anterior cruciate ligament reconstruction: an anatomic approach. Arthroscopy. 2005;21:1275. doi: 10.1016/j.arthro.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 10.Desai N, Bjornsson H, Musahl V, Bhandari M, Petzold M, Fu FH, Samuelsson K. Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:1009–1023. doi: 10.1007/s00167-013-2811-6. [DOI] [PubMed] [Google Scholar]
- 11.Fauno P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy. 2005;21:1337–1341. doi: 10.1016/j.arthro.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42:2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 13.Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008;36:308–315. doi: 10.1177/0363546507308939. [DOI] [PubMed] [Google Scholar]
- 14.Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop. 2009;80:563–567. doi: 10.3109/17453670903350107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grindem H, Granan LP, Risberg MA, Engebretsen L, Snyder-Mackler L, Eitzen I. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2015;49:385–389. doi: 10.1136/bjsports-2014-093891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40:512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 17.Knottnerus A, Tugwell P. STROBE–a checklist to Strengthen the Reporting of Observational Studies in Epidemiology. J Clin Epidemiol. 2008;61:323. doi: 10.1016/j.jclinepi.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Lehmann AK, Osada N, Zantop T, Raschke MJ, Petersen W. Femoral bridge stability in double-bundle ACL reconstruction: impact of bridge width and different fixation techniques on the structural properties of the graft/femur complex. Arch Orthop Trauma Surg. 2009;129:1127–1132. doi: 10.1007/s00402-009-0869-x. [DOI] [PubMed] [Google Scholar]
- 19.Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40:1551–1557. doi: 10.1177/0363546512446000. [DOI] [PubMed] [Google Scholar]
- 20.Mascarenhas R, Cvetanovich GL, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, Bach BR., Jr Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:1185–1196. doi: 10.1016/j.arthro.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 21.Mascarenhas R, Saltzman BM, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, Bach BR., Jr Bioabsorbable versus metallic interference screws in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:561–568. doi: 10.1016/j.arthro.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 22.Middleton KK, Muller B, Araujo PH, Fujimaki Y, Rabuck SJ, Irrgang JJ, Tashman S, Fu FH. Is the native ACL insertion site ‘completely restored’ using an individualized approach to single-bundle ACL-R? Knee Surg Sports Traumatol Arthrosc. 2015;23:2145–2150. doi: 10.1007/s00167-014-3043-0. [DOI] [PubMed] [Google Scholar]
- 23.Mohtadi N, Chan D, Barber R, Paolucci EO. Reruptures, reinjuries, and revisions at a minimum 2-year follow-up: a randomized clinical trial comparing 3 graft types for ACL reconstruction. Clin J Sports Med. 2016;26:96–107. doi: 10.1097/JSM.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 24.Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM, Fevang JM. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med. 2014;42:285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 25.Petersen W, Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2007;454:35–47. doi: 10.1097/BLO.0b013e31802b4a59. [DOI] [PubMed] [Google Scholar]
- 26.Rahr-Wagner L, Lind M. The Danish Knee Ligament Reconstruction Registry. Clin Epidemiol. 2016;8:531–535. doi: 10.2147/CLEP.S100670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish Registry of Knee Ligament Reconstruction. Am J Sports Med. 2014;42:278–284. doi: 10.1177/0363546513509220. [DOI] [PubMed] [Google Scholar]
- 28.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013;29:98–105. doi: 10.1016/j.arthro.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 29.Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:137–145. doi: 10.1016/j.arthro.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 30.Siebold R, Schuhmacher P. Restoration of the tibial ACL footprint area and geometry using the Modified Insertion Site Table. Knee Surg Sports Traumatol Arthrosc. 2012;20:1845–1849. doi: 10.1007/s00167-012-1899-4. [DOI] [PubMed] [Google Scholar]
- 31.Suomalainen P, Kannus P, Jarvela T. Double-bundle anterior cruciate ligament reconstruction: a review of literature. Int Orthop. 2013;37:227–232. doi: 10.1007/s00264-012-1680-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Svantesson E, Sundemo D, Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu FH, Desai N, Stalman A, Samuelsson K. Double-bundle anterior cruciate ligament reconstruction is superior to single-bundle reconstruction in terms of revision frequency: a study of 22,460 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2016 Nov 23. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 33.Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. [DOI] [PMC free article] [PubMed]
- 34.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 35.Ytterstad K, Granan LP, Ytterstad B, Steindal K, Fjeldsgaard KA, Furnes O, Engebretsen L. Registration rate in the Norwegian Cruciate Ligament Register: large-volume hospitals perform better. Acta Orthop. 2012;83:174–178. doi: 10.3109/17453674.2012.678800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35:223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]


