Abstract
Background
Failure of hip preservation to alleviate symptoms potentially subjects the patient to reoperation or conversion surgery to THA, adding recovery time, risk, and cost. A risk calculator using an algorithm that can predict the likelihood that a patient who undergoes arthroscopic hip surgery will undergo THA within 2 years would be helpful, but to our knowledge, no such tool exists.
Questions
(1) Are there preoperative and intraoperative variables at the time of hip arthroscopy associated with subsequent conversion to THA? (2) Can these variables be used to develop a predictive tool for conversion to THA?
Materials and Methods
All patients undergoing arthroscopy from January 2009 through December 2011 were registered in our longitudinal database. Inclusion criteria for the study group were patients undergoing hip arthroscopy for a labral tear, who eventually had conversion surgery to THA. Patients were compared with a control group of patients who underwent hip arthroscopy for a labral tear but who did not undergo conversion surgery to THA during the same study period. Of the 893 who underwent surgery during that time, 792 (88.7%) were available for followup at a minimum of 2 years (mean, 31.1 ± 8.1 years) and so were considered in this analysis. Multivariate regression analyses of 41 preoperative and intraoperative variables were performed. Using the results of the multivariate regression, we developed a simplified calculator that may be helpful in counseling a patient regarding the risk of conversion to THA after hip arthroscopy.
Results
Variables simultaneously associated with conversion to THA in this model were older age (rate ratio, 1.06; 95% CI, 1.03–1.08; p < 0.0001), lower preoperative modified Harris hip score (rate ratio [RR], 0.98; 95% CI, 0.96–0.99; p = 0.0003), decreased femoral anteversion (RR, 0.97; 95% CI, 0.94–0.99; p = 0.0111), revision surgery (RR, 2.4; 95% CI, 1.15–5.01; p = 0.0193), femoral Outerbridge Grades II to IV (Grade II: RR, 2.23 [95% CI, 1.11–4.46], p = 0.023; Grade III: RR, 2.17, [95% CI, 1.11–4.23], p = 0.024; Grade IV: RR, 2.96 [95% CI, 1.34–6.52], p = 0.007), performance of acetabuloplasty (RR, 1.83; 95% CI, 1.03–3.24; p = 0.038), and lack of performance of femoral osteoplasty (RR, 0.62; 95% CI, 0.36–1.06; p = 0.081). Using the results of the multivariate regression, we developed a simplified calculator that may be helpful in counseling a patient regarding the risk of conversion surgery to THA after hip arthroscopy.
Conclusion
Multiple risk factors have been identified as possible risk factors for conversion to THA after hip arthroscopy. A weighted calculator based on our data is presented here and may be useful for predicting failure after hip arthroscopy for labral treatment. Determining the best candidates for hip preservation remains challenging; careful attention to long-term followup and identifying characteristics associated with successful outcomes should be the focus of further study.
Level of Evidence
Level III, therapeutic study.
Introduction
Arthroscopic treatment of hip conditions is a rapidly expanding field in sports medicine and adult reconstruction. Currently, the most-common indications for hip arthroscopy are the treatment of femoroacetabular impingement and symptomatic labral tear [4]. The goals of hip arthroscopy are to address soft tissue injuries and correct abnormal bony morphologic features. Ideally, in doing so, arthroscopic hip surgery has the potential to prevent patients from progressing to the development of symptomatic degenerative joint disease. The number of hip arthroscopies performed by board applicants increased 600% from 2006 to 2010 [4]. As the number of arthroscopic hip procedures increases, so will complications and reoperations. The most-common reason for reoperation after arthroscopic hip surgery is conversion to THA [8]. Failure of hip preservation to alleviate symptoms potentially subjects the patient to reoperation, leading to a prolonged and frustrating recovery for the patient and wasting economic resources. These patients are often young, which also has potential implications for revision arthroplasty during their lifetime [7, 9]. When THA is required after hip arthroscopy, it often is performed within 4 years from arthroscopy [2], indicating failed joint preservation and raising the question of which factors might predict early conversion to THA.
The risk of early conversion to THA after hip arthroscopy, which we generally would define as within 2 years, appears to be highly dependent on the degree of preoperative arthrosis with some studies documenting a high reoperation rate in patients with chondral damage [10, 17]. Radiographic joint space narrowing and other markers of degenerative joint disease may portend a poor prognosis; however, even patients with sufficient joint space may have attempts at joint preservation fail [1, 11, 12, 14–17, 20]. Acetabular chondral delamination also has been considered a potential risk factor for poor outcomes after hip preservation and may be difficult to diagnose preoperatively, even with high-quality MRI arthrograms [1]. In our practice, we noted many patients with no or minimal degenerative changes seen on preoperative radiographs who subsequently had symptomatic degenerative joint disease. We therefore hoped to establish prognostic factors which might aid in identifying patients at risk.
We therefore asked: (1) Are there preoperative and intraoperative variables at the time of hip arthroscopy associated with subsequent conversion to THA? (2) Can these variables be used to develop a predictive model for conversion to THA?
Materials and Methods
Patient Inclusion and Data Collection
After obtaining institutional review board approval, we used our longitudinally maintained institutional database to evaluate all patients treated with hip arthroscopy for labral tears between January 2009 and December 2011. The study group included all patients with adequate followup who underwent hip arthroscopy for labral treatment and then required conversion surgery to THA. The control group included all patients with adequate followup who underwent hip arthroscopy for labral treatment but who did not have conversion surgery to THA. Inclusion criteria were all patients undergoing primary or revision hip arthroscopy for a symptomatic labral tear. Exclusion criteria were patients with previous hip conditions such as Legg-Calvé-Perthes disease, slipped capital femoral epiphysis, pigmented villonodular synovitis, ankylosing spondylitis, and avascular necrosis. The database includes demographics, clinical history, patient-reported outcomes scores, and radiographic data.
We collected 41 preoperative and intraoperative variables on patients during the study period. These variables were based on the following characteristics: (1) demographics; (2) scoring instruments used; (3) radiographic factors; and (4) intraoperative findings.
These individual variables based on the four characteristics included: age, sex, BMI, workers compensation status, revision surgery status, history of back pain, previous back surgery, months of symptoms, modified Harris hip score, nonarthritic hip score, hip outcome score-activities of daily living, hip outcome score-sport-specific subscale, VAS, femoral anteversion, Tönnis grade, lateral center-edge angle (LCEA), anterior center-edge angle (ACEA), acetabular inclination, alpha angle, joint space measurements, and crossover sign percentage. Intraoperative variables included: Seldes labral tear grade, labral tear size, acetabular labrum articular disruption (ALAD) grade, acetabular chondral defect size, acetabular Outerbridge grade, femoral chondral defect size, femoral Outerbridge grade, ligamentum teres tear grade, labral treatment (repair versus débridement), traction time, number of labral anchors, capsular treatment (release versus repair), acetabuloplasty, femoral osteoplasty, iliopsoas release, notchplasty, microfracture, and loose body removal. The type and grade of chondral lesion for the acetabulum and femoral head were recorded using the Outerbridge classification. Peripheral acetabular labral-articular disruption lesions were classified according to the ALAD classification: softening of cartilage adjacent to the labrum (ALAD1), early peel back of the cartilage (ALAD2), large chondral flap (ALAD3), or complete loss of cartilage (ALAD4).
Demographics and Followup
Of the 893 patients who underwent hip arthroscopy and who met study inclusion criteria, 792 (89%) were available for followup. Seventy-two patients (9%) who underwent conversion surgery to THA during the followup period constituted the study group, and 720 patients (91%) who did not undergo conversion surgery to THA during the followup period constituted the control group. One hundred one patients were lost to followup. Mean time to conversion to THA for the study group was 19 ± 12 months (range, 0.9–52 months), and the average time to followup for the control group was 31 ± 8.months (range, 20–62 months). The entire patient population had an average age of 38 ± 14 years (range, 13–76 years) and an average BMI of 25 ± 4.8 kg/m2 (range, 16–48 kg/m2). There were 293 (37%) men and 499 (63%) women. Four hundred twenty-four (54%) underwent right hip surgery, and 368 (46%) underwent left hip surgery. The proportion of right and left hip procedures was not different between groups. Seventy-eight (9.8%) procedures involved a workers’ compensation claim, and 81 (10%) procedures were revision hip arthroscopy.
Radiographic Review
At our institution preoperative and postoperative radiographic data on all patients undergoing hip arthroscopy are recorded by hip preservation fellows once the patient reaches the 2-year followup. The measurements were taken by multiple readers, however previous interobserver reliability has been shown from our group [8], but was not tested for the current study. Using the supine AP pelvis radiograph, the LCEA, acetabular inclination, acetabular crossover, and Tönnis grade were measured [6]. When a crossover sign was present we estimated the percent of crossover by dividing distance from the superior acetabulum to the point of intersection of the anterior and posterior wall by the entire length of the posterior wall. This was done to gauge the amount of acetabular retroversion. A 45°-Dunn view was used to measure the alpha angle. A false profile view was used to measure the ACEA. The joint space is measured in three places on an AP pelvic radiograph: the medial and the lateral edges of the sourcil and the central aspect of the sourcil. Femoral anteversion was collected from preoperative MR images when performed at our center.
Indications for Hip Arthroscopy
Clinically all patients had signs and symptoms of a labral tear and did not respond to 3 months of nonoperative treatment. Patients had groin pain, or pain surrounding their hip, with positive impingement maneuvers for a minimum of 3 months. Nonoperative treatment included a minimum of 6 weeks of physical therapy and a trial of antiinflammatory medication. During the preoperative workup patients underwent plain radiographs as detailed above. Patients also underwent MRI or an MRI arthrogram to confirm labral disorders.
Surgical Technique
All surgeries were performed by the senior author (BGD), with the patient in the modified supine position, using a minimum of two portals. After establishment of portals and capsulotomy, a diagnostic arthroscopy of the hip was performed to evaluate for loose bodies, chondral defects, labral tears, ligamentum teres tears, and other intraarticular disorders. An intraoperative data sheet was collected on all patients at the time of diagnostic arthroscopy. Labra were repaired when possible. If labral tissue quality was unable to be repaired, patients were treated with débridement or reconstruction. The acetabular rim was resected when features of pincer impingement were present. After addressing lesions in the central compartment, the peripheral compartment was exposed and femoral osteoplasty performed for cam lesions. Surgical treatments were recorded in our database.
Intraoperative Data Recording
At our institution a detailed intraoperative data sheet is recorded for all patients undergoing hip arthroscopy. At the time of surgery labral tear size was documented for all patients using traditional acetabular clock-face nomenclature to determine size and location of the tear. Labral tears were described using the classification of Seldes et al. [19], with Type I tears being separation at the chondrolabral junction and Type II tears being intrasubstance damage. To describe the position of the labral tear, the acetabulum is divided into 12 sectors corresponding to a clock face. Labral tear size was documented by recording the number of sectors involved in the tear. An arthroscopic probe is used to measure chondral damage on the femoral head and acetabulum in square centimeters.
Rehabilitation
The postoperative rehabilitation was patient-specific depending on concomitant procedures. In general, patients were advised to use partial, 20-pound weightbearing for 2 to 6 weeks.
Patients wore a hip abduction brace for 2 weeks postoperatively. Hip ROM was limited to 90° flexion, neutral internal rotation, 30° external rotation, and 30° abduction for 3 to 6 weeks. When the patient was full weightbearing, therapy was advanced to achieve full strength and activity by 3 to 4 months.
Statistical Analysis
Multivariate Analysis
Up to 41 potential predictors were assessed simultaneously using a multivariate (multivariable), backward, stepwise Cox proportional hazard model regression using the 41 potential candidate predictors. A liberal probability less than 0.10 variable retention criterion was used. This probability was used, rather than 0.05, to ensure potentially important variables were not eliminated. The rate ratio (RR) for the simultaneously significant variables is reported along with the corresponding 95% confidence bounds and p values. For a continuous variable such as age, the RR is for a one-unit increase in the variable. For example, if the RR for age is 1.06, this is 1.06 per year. That is, for a 1-year increase in age, the event rate is 6% larger. For a K-unit increase the, RR is RRK. So, for a K = 5-year increase in age, the RR in this example is 1.065 × 5 = 1.34, implying that a 5-year age increase is associated with a 34% increase in the total hip replacement rate.
The accuracy of the Cox model was assessed using the Harrell C statistic [21]. The linear relation between the log hazard versus continuous variables such as age was confirmed by fitting cubic splines. For example, to see that there was a linear relation between the log hazard and age, age and the cubic spline of age were fit. If the relationship is linear, only age, not the spline of age, should be statistically significant.
To use all 792 cases in the multivariate Cox model, missing values were first imputed using Markov chain Monte Carlo methods [5]. Results were similar to those using only complete cases.
Risk Calculator
Using the results of the multivariate regression, we developed a simplified calculator that may be helpful in counseling a patient regarding the risk of conversion surgery to THA after hip arthroscopy. Variables chosen were based on the results of the multivariate analysis. Points for certain values of variables were assigned based on hazard ratios. We then weighted the variable to develop a 100-point scale. These points can be added and the sum used to predict the risk of conversion to THA at 27 months followup based on the hazard ratios.
Results
Are there preoperative and intraoperative variables at the time of hip arthroscopy associated with subsequent conversion to THA?
Several preoperative and intraoperative variables were associated with conversion to THA (Table 1). Variables simultaneously associated with conversion to THA in this model were older age (RR, 1.06; 95% CI, 1.03–1.08; p < 0.0001), lower preoperative modified Harris hip score (RR, 0.98; 95% CI, 0.96–0.99; p = 0.0003), decreased femoral anteversion (RR, 0.97; 95% CI, 0.94–0.99; p = 0.011), revision surgery (RR, 2.4; 95% CI, 1.15–5.01; p = 0.019), femoral Outerbridge Grades II to IV (Grade II: RR, 2.23 [95% CI, 1.11–4.46], p = 0.023; Grade III: RR, 2.17 [95% CI, 1.11–4.23], p = 0.024; Grade IV: RR, 2.96 [95% CI, 1.34–6.52], p = 0.007), performance of acetabuloplasty (RR, 1.83; 95% CI, 1.03–3.24; p = 0.038), and lack of performance of femoral osteoplasty (RR, 0.62; 95% CI, 0.36–1.06; p = 0.081). Higher acetabular Outerbridge grade was not associated with conversion (p < 0.115) (Table 1). LCEA has a quadratic effect, u-shaped, unlike other variables. In other words the RR increases at low and high angles. Using these eight variables a Harrell C statistic of 0.832 was obtained. An incidence curve was generated using the Kaplan-Meier method (Fig. 1).
Table 1.
Multivariate Cox model for conversion to THA
| Variable | Unit | Rate ratio | Lower confidence interval | Upper confidence interval | p Value | Log rate ratio | SE |
|---|---|---|---|---|---|---|---|
| Age | Per year | 1.06 | 1.03 | 1.08 | 0 | 0.055 | 0.012 |
| Preoperative modified Harris hip score | Per unit | 0.98 | 0.96 | 0.99 | < 0.001 | −0.025 | 0.007 |
| Femoral anteversion | Per unit | 0.97 | 0.94 | 0.99 | 0.0111 | −0.034 | 0.014 |
| Lateral center-edge angle | Per degree | 0.93 | 0.89 | 0.97 | < 0.001 | −0.074 | 0.02 |
| Revision surgery | Yes vs no | 2.4 | 1.15 | 5.01 | 0.0193 | 0.877 | 0.375 |
| Acetabular cartilage damage grade | 1 vs 0 | 0.29 | 0.06 | 1.35 | 0.115 | −1.22 | 0.77 |
| Acetabular cartilage damage grade | 2 vs 0 | 0.87 | 0.24 | 3.11 | 0.831 | −0.14 | 0.65 |
| Acetabular cartilage damage grade | 3 vs 0 | 1.8 | 0.5 | 6.47 | 0.368 | 0.59 | 0.65 |
| Acetabular cartilage damage grade | 4 vs 0 | 1.95 | 0.54 | 7.04 | 0.311 | 0.67 | 0.66 |
| Femoral cartilage damage grade | 1 vs 0 | 0.59 | 0.08 | 4.42 | 0.606 | −0.53 | 1.03 |
| Femoral cartilage damage grade | 2 vs 0 | 2.23 | 1.11 | 4.46 | 0.023 | 0.8 | 0.35 |
| Femoral cartilage damage grade | 3 vs 0 | 2.17 | 1.11 | 4.23 | 0.024 | 0.77 | 0.34 |
| Femoral cartilage damage grade | 4 vs 0 | 2.96 | 1.34 | 6.52 | 0.007 | 1.09 | 0.4 |
| Acetabuloplasty | Yes vs no | 1.83 | 1.03 | 3.24 | 0.038 | 0.604 | 0.291 |
| Femoral osteoplasty | Yes vs no | 0.62 | 0.36 | 1.06 | 0.0809 | −0.484 | 0.277 |
| Harrell C statistic | 0.832 |
SE = standard error.
Fig. 1.
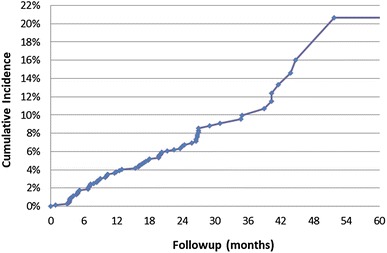
The cumulative incidence curve for THA after hip arthroscopy for labral treatment is shown.
Can these variables be used in a predictive model for conversion to THA?
To estimate a patient’s risk of conversion surgery to THA by 27 months after hip arthroscopy for a labral tear, the clinician may use our risk calculator by plugging in select variables, which result in a total point value, which is converted to a percent risk (Fig. 2). For example, a 45-year-old patient undergoing primary hip arthroscopy for a labral tear with a preoperative LCEA of 30°, acetabular Outerbridge Grade 0, and femoral Outerbridge Grade I would have a point total of 29 (14 points for age 45 years, 0 points for primary hip surgery, 14 points for LCEA of 30°, 9 points for acetabular Outerbridge Grade 0, 0 points for femoral Outerbridge Grade I) and would be estimated to have less than a 1% chance of undergoing THA within 27 months after hip arthroscopy. However, a 60-year-old patient undergoing revision hip arthroscopy for a labral tear with a preoperative LCEA of 15°, acetabular Outerbridge Grade II, and femoral Outerbridge Grade III would have a point total of 68 (20 points for age 60 years, 8 points for revision surgery, 21 points for LCEA of 15°, 9 points for acetabular Outerbridge Grade II, and 10 points for femoral Outerbridge Grade III) and would be estimated to have a 10% chance of undergoing THA within 27 months after hip arthroscopy.
Fig. 2.
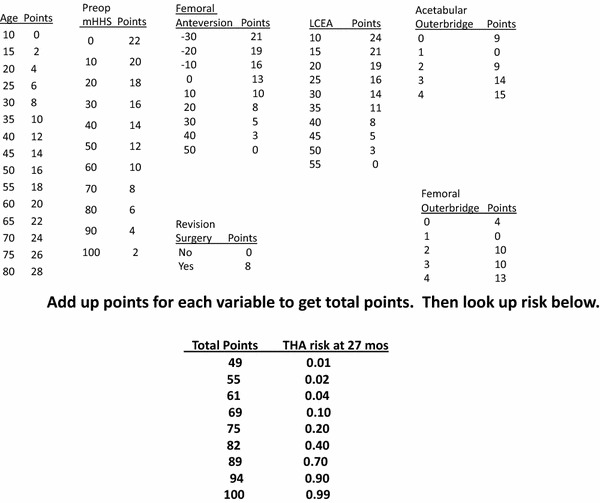
Our risk factor calculator for predicting THA after labral treatment is presented. mHHS = modified Harris hip score; LCEA = lateral center-edge angle.
Discussion
Hip arthroscopy is generally effective for patients with symptomatic labral tears resulting from femoroacetabular impingement or borderline hip dysplasia [6, 11, 13, 18, 20]. However, early conversion to THA after hip arthroscopy for labral tears is a frustrating and potentially preventable problem. Previous studies have shown chondral damage and radiographic joint space narrowing portend a poor prognosis [1, 10, 15, 17, 20]. Although chondral damage has been identified as a predictor of conversion to THA, we sought to identify preoperative and intraoperative clinical and radiographic risk factors for conversion after hip arthroscopy. In the current study we found patient age, functional scores, femoral version, LCEA, femoral and acetabular chondral damage, acetabuloplasty, femoral osteoplasty, and revision status were predictors of early conversion to THA.
This study had several major limitations. First, there was a low number of events (72 conversions to THA) per variable (41 variables) used in our multivariate analysis, which may make our model unreliable owing to the risk of overfitting. In addition, our study might be underpowered to detect truly significant variables, such as joint space narrowing. We believe our findings add to what is known on risk factors for hip arthroscopy failure, but should be used with caution, and in the context of previously suggested risk factors. In addition, our risk calculator includes intraoperative data such as Outerbridge classification, making it less beneficial to the surgeon and patient before surgery. It also has not been validated or tested as it is merely an extension of our multivariate analysis, so it should be used with caution and with sound clinical judgement. In addition, the patient cohort includes patients with multiple underlying deformities such as femoroacetabular impingement, dysplasia, and ligamentous laxity that contribute to labral tears; therefore the results may apply only to patients having surgery for those indications. The radiographic parameters evaluated were measured by several different hip preservation fellows during a period of time, and interobserver reliability could introduce bias in the sample that we are unable to detect; however previous interobserver reliability has been shown from our group [8], but it was not tested for the current study. The followup in this study is relatively short, but important information regarding early THA conversion can be gathered from the results. As longer-term data become available the risk calculator may need to be refined.
This study has several other limitations. First, we had a lost-to-followup rate of 11.3% in the setting of a conversion to THA rate of 9.1%. It is possible that the patients who were lost to followup had a conversion to THA rate significantly out of proportion to our findings among those with followup. If this were the case, our findings may not reflect the true conversion to THA and risk factors leading to conversion. However, we feel that a lost-to-followup rate of 11.3% for a large followup outcomes study such as the current one reflects the reality of clinical practice, and that the utility of our risk calculator would not change appreciably with the patients included who were lost to followup. It is possible that if all patients lost to followup underwent THA the calculator would underestimate the risk of early conversion to THA. In addition, some patients who underwent conversion surgery to THA underwent the THA at an outside institution, meaning we cannot reliably comment on explicit criteria or indications for conversion to arthroplasty in this study. In addition, because many patients underwent THA at outside institutions, we were not able to assess progression of osteoarthritis in those who underwent conversion surgery to THA. Additionally, some potential factors were not included owing to unreliable data such as trauma or mechanism of injury. Finally, this is a single-center, single-surgeon study, which limits the generalizability of the findings.
McCarthy et al. [15] identified age, acetabular Outerbridge grade, and femoral head Outerbridge grade as risk factors for conversion to THA. Our study differs in some respects. McCarthy et al. [15] treated patients with intraarticular lesions with labral débridement and chondroplasty, while more-recent arthroscopic procedures such as labral repair, femoroplasty, and acetabuloplasty were used as treatment modalities in our study patients We also considered 41 variables, compared with the five studied by McCarthy et al. [15]. In addition, we identified age and femoral chondral injury to be associated with risk of conversion to THA. We did not find that labral repair or acetabular cartilage grade were associated with a decreased risk of conversion to THA in the short term. However, the followup period for the current study is shorter, and our findings may reflect that.
Larson and Giveans [13] found that joint space narrowing, MRI findings of chondral damage, and duration of symptoms predicted failure, defined as conversion to THA or a Harris hip score less than 70. We did not identify joint space narrowing as a predictor, although we defined failure differently, and included patients with dysplasia, which Larson and Giveans did not. We also did not evaluate chondral injury at the time of MRI or the duration of preoperative symptoms.
Advanced age at the time of hip arthroscopy predicts conversion to THA. Two studies specifically evaluated patients older than 50 years undergoing hip arthroscopy. Philippon et al. [18] evaluated 153 patients older than 50 years undergoing hip arthroscopy for femoroacetabular impingement and found a 20% conversion to THA at a mean of 1.6 years after surgery. Ben Tov et al. [3] evaluated 22 patients older than 50 years after hip arthroscopy with labral repair at a mean followup of 22 months. One patient underwent conversion surgery to THA in their cohort and one patient was unable to be followed up. The remaining 20 patients had satisfactory results, as defined by the authors. Our study thus corroborates previous findings regarding patient age.
Joint space narrowing and signs of osteoarthritis have been shown to be associated with conversion to THA. Skendzel et al. [20] reported mid-term outcomes after hip arthroscopy for femoroacetabular impingement in 559 patients by performing a subgroup analysis of 383 patients with less than and more than 2 mm joint space narrowing. Fifty-four of the 63 patients (86%) with narrowed joint space had conversion surgery to THA within 5 years compared with 63 of the 383 patients (16%) without a narrowed joint space. A couple studies have identified arthritic features as a risk for failure [1, 11]. In our study, joint space narrowing was not associated with conversion to THA in the multivariate regression analyses. This may be attributable to a relatively small number of patients with joint space narrowing undergoing hip arthroscopy, or patients with joint space narrowing were counseled regarding expectations. Although we did not specifically identify joint space narrowing as a risk factor, we believe it should be a relative contraindication to hip arthroscopy based on the above studies.
Multiple risk factors have been identified as possible risk factors for conversion to THA after hip arthroscopy. A weighted calculator based on our data is presented here and may be useful for predicting failure after hip arthroscopy for labral treatment. Determining the best candidates for hip preservation remains challenging; careful attention to long-term followup and identifying characteristics associated with successful outcomes should be the focus of further study.
Footnotes
The institution of one or more of the authors (BGD) has received, during the study period, funding from Arthrex Inc, ATI Physical Therapy, Breg Inc, Pacira Pharmaceuticals Inc, and Stryker Corporation.
One of the authors certifies that he (BGD), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Amplitude Technologies (Evry, France) an amount of USD 10,000–USD 100,000 from Arthrex Inc (Naples, FL, USA); an amount of less than USD 10,000 from DJO Global Inc (Vista, CA, USA); an amount of less than USD 10,000 from Medacta International (Chicago, IL, USA); an amount of less than USD 10,000 from Orthomerica Products Inc (Orlando, FL, USA); an amount of less than USD 10,000 from Pacira Pharmaceuticals Inc (Parsippany-Troy Hills, NJ, USA); and an amount of less than USD 10,000 from Stryker Corporation (Kalamazoo, MI, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the American Hip Institute, Westmont, IL, USA.
References
- 1.Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement: risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91:305–313. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 2.Bedard NA, Pugely AJ, Duchman KR, Westermann RW, Gao Y, Callaghan JJ. When hip scopes fail, they do so quickly. J Arthroplasty. 2016;31:1183–1187. doi: 10.1016/j.arth.2015.12.024. [DOI] [PubMed] [Google Scholar]
- 3.Ben Tov T, Amar E, Shapira A, Steinberg E, Atoun E, Rath E. Clinical and functional outcome after acetabular labral repair in patients aged older than 50 years. Arthroscopy. 2014;30:305–310. doi: 10.1016/j.arthro.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Chan V, Valone FH, 3rd, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8 suppl):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 5.Chib S, Nardari F, Shephard N. Markov chain Monte Carlo methods for stochastic volatility models. J Economics. 2002;108:281–316. doi: 10.1016/S0304-4076(01)00137-3. [DOI] [Google Scholar]
- 6.Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 7.Girard J, Glorion C, Bonnomet F, Fron D, Migaud H. Risk factors for revision of hip arthroplasties in patients younger than 30 years. Clin Orthop Relat Res. 2011;469:1141–1147. doi: 10.1007/s11999-010-1669-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris JD, McCormick FM, Abrams GD, Gupta AK, Ellis TJ, Bach BR, Jr, Bush-Joseph CA, Nho SJ. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Haviv B, O’Donnell J. The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients. SportsMed Arthrosc Rehabil Ther Technol. 2010;2:18. doi: 10.1186/1758-2555-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010;26:623–629. doi: 10.1016/j.arthro.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Jerosch J, Schunck J, Khoja A. Arthroscopic treatment of the hip in early and midstage degenerative joint disease. Knee Surg Sports Traumatol Arthrosc. 2006;14:641–645. doi: 10.1007/s00167-005-0009-2. [DOI] [PubMed] [Google Scholar]
- 12.Kim KC, Hwang DS, Lee CH, Kwon ST. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007;456:128–132. doi: 10.1097/01.blo.0000246542.49574.2c. [DOI] [PubMed] [Google Scholar]
- 13.Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy JC. Hip arthroscopy: when it is and when it is not indicated. Instr Course Lect. 2004;53:615–621. [PubMed] [Google Scholar]
- 15.McCarthy JC, Jarrett BT, Ojeifo O, Lee JA, Bragdon CR. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res. 2011;469:362–371. doi: 10.1007/s11999-010-1559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013;471:2492–2496. doi: 10.1007/s11999-012-2779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 18.Philippon MJ. Schroder e Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28:59–65. doi: 10.1016/j.arthro.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232–240. doi: 10.1097/00003086-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 20.Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42:1127–1133. doi: 10.1177/0363546514526357. [DOI] [PubMed] [Google Scholar]
- 21.Uno H, Cai T, Pencina MJ, D’Agostino RB, Wei LJ. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med. 2011;30:1105–1117. doi: 10.1002/sim.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]


