Summary
Background
Hepatitis D virus (also known as hepatitis delta virus) can establish a persistent infection in people with chronic hepatitis B, leading to accelerated progression of liver disease. In sub-Saharan Africa, where HBsAg prevalence is higher than 8%, hepatitis D virus might represent an important additive cause of chronic liver disease. We aimed to establish the prevalence of hepatitis D virus among HBsAg-positive populations in sub-Saharan Africa.
Methods
We systematically reviewed studies of hepatitis D virus prevalence among HBsAg-positive populations in sub-Saharan Africa. We searched PubMed, Embase, and Scopus for papers published between Jan 1, 1995, and Aug 30, 2016, in which patient selection criteria and geographical setting were described. Search strings included sub-Saharan Africa, the countries therein, and permutations of hepatitis D virus. Cohort data were also added from HIV-positive populations in Malawi and Ghana. Populations undergoing assessment in liver disease clinics and those sampled from other populations (defined as general populations) were analysed. We did a meta-analysis with a DerSimonian-Laird random-effects model to calculate a pooled estimate of hepatitis D virus seroprevalence.
Findings
Of 374 studies identified by our search, 30 were included in our study, only eight of which included detection of hepatitis D virus RNA among anti-hepatitis D virus seropositive participants. In west Africa, the pooled seroprevalence of hepatitis D virus was 7·33% (95% CI 3·55–12·20) in general populations and 9·57% (2·31–20·43) in liver-disease populations. In central Africa, seroprevalence was 25·64% (12·09–42·00) in general populations and 37·77% (12·13–67·54) in liver-disease populations. In east and southern Africa, seroprevalence was 0·05% (0·00–1·78) in general populations. The odds ratio for anti-hepatitis D virus detection among HBsAg-positive patients with liver fibrosis or hepatocellular carcinoma was 5·24 (95% CI 2·74–10·01; p<0·0001) relative to asymptomatic controls.
Interpretation
Findings suggest localised clusters of hepatitis D virus endemicity across sub-Saharan Africa. Epidemiological data are needed from southern and east Africa, and from patients with established liver disease. Further studies should aim to define the reliability of hepatitis D virus testing methods, identify risk factors for transmission, and characterise the natural history of the infection in the region.
Funding
Wellcome Trust, Royal Society.
Introduction
Liver cirrhosis and hepatocellular carcinoma accounted for more than 3% of adult deaths in sub-Saharan Africa in 2013, and this proportion is rising.1 Chronic infection with hepatitis B virus, which has an estimated population prevalence of 8·8%, is the main cause.2 Hepatitis D virus (also known as hepatitis delta virus) is a small satellite sub-virus that requires the presence of HBsAg to propagate.3 Hepatitis B and D virus infections can occur simultaneously, which frequently results in clearance of both viruses, or as superinfection in chronic hepatitis B virus carriers, which often leads to persistence of hepatitis D virus.4 Individuals concomitantly infected with hepatitis B and D viruses can mount transient serological responses before clearance; thus, screening for hepatitis-D-virus-specific antibody reliably identifies cases of chronic super-infection but is less accurate for ascertainment of overall rates of exposure.4
Chronic hepatitis B and D virus co-infection is associated with expedited progression to cirrhosis, and has been characterised as the most severe form of viral hepatitis.5 In sub-Saharan Africa, where 4·8% of adults are living with HIV, hepatitis B virus infection and HIV often coexist, albeit with geographical variations.6, 7 Co-infection with HIV, hepatitis B virus, and hepatitis D virus could be an important specific cause of liver-related morbidity and mortality.8, 9 The only treatment for hepatitis D virus is pegylated interferon-α, and less than 30% attain sustained virological responses. Novel drug classes, including prenylation and entry inhibitors, are in development.4, 10, 11
Despite widely held assumptions of hyper-endemicity, no previous systematic analyses have been done of the epidemiology of hepatitis D virus in sub-Saharan Africa. Routine testing for hepatitis D virus is rare in clinical practice, and because of low rates of case ascertainment, the overall contribution of the virus to the burden of liver disease in the region is unknown.5 We aimed to define the available evidence on the prevalence of hepatitis D virus in sub-Saharan Africa and identify research needs.
Research in context.
Evidence before this study
We searched PubMed, Embase, and Scopus with the terms “hepatitis delta” and “sub-Saharan Africa” and the countries therein for studies published in any language between Jan 1, 1995, and Aug 30, 2016 (appendix). We identified no systematic reviews of hepatitis D virus seroprevalence in the region. In narrative reviews, cited studies predominantly done in west Africa suggested a seroprevalence of between 12% and 67% from diverse populations in Gabon, Cameroon, and Nigeria. We identified no studies in which risk factors for hepatitis D virus infection or a possible association between hepatitis D virus infection and HIV status were analysed.
Added value of this study
In our analysis, we systematically compiled available data for hepatitis D virus epidemiology in sub-Saharan Africa, added novel cohort data from Malawi and Ghana, and provided pooled estimates of seroprevalence by region and population group. Our findings suggest substantial geographical variability, with pockets of hyperendemicity in central Africa and low seroprevalence in southern Africa. Overall, hepatitis D virus seroprevalence among HBsAg-positive populations in west and central Africa exceeds the estimated global seroprevalence. Published data do not allow firm conclusions to be drawn about risk factors for hepatitis D virus infection, including any possible association with HIV status. In most studies, detection of anti-hepatitis D virus was not confirmed with a second assay, and hepatitis D virus RNA detection was reported in only a few studies.
Implications of all the available evidence
Hepatitis D virus infection makes a potentially important contribution to the burden of liver disease in sub-Saharan Africa, particularly in west and central Africa, but important gaps in knowledge remain and more research is needed. Epidemiological data for east and southern Africa are insufficient. The natural history of infection with genotypes 5–8, which are endemic to Africa, remains to be characterised, including ascertainment of prevalence among patients with well characterised liver disease. Methods of detection of hepatitis D virus RNA need to be standardised, and the reliability of hepatitis D virus antibody and RNA testing in African settings should be investigated. Studies are needed to identify specific risk factors for hepatitis D virus infection, and guide the formulation of prevention and management policies.
Methods
Search strategy and selection criteria
We did a systematic review and meta-analysis of studies of the prevalence of hepatitis D virus in sub-Saharan Africa, including added data for anti-hepatitis D virus and hepatitis D virus RNA prevalence from two HIV-positive cohorts in Ghana and Malawi, where scarce data were previously available. AJS searched PubMed, Embase, and Scopus for studies published in any language between Jan 1, 1995, and Aug 30, 2016, in which the prevalence of anti-hepatitis D virus antibody or hepatitis D virus RNA was reported. Search strings included sub-Saharan Africa, the countries therein, and permutations of hepatitis D virus (appendix). MC and AJS independently assessed articles for inclusion; disagreements were resolved by consensus. Hepatitis D virus seroprevalence was defined as reported detection of anti-hepatitis D virus by enzyme immunoassay in HBsAg-positive patients. To be included in our review, hepatitis D virus seroprevalence, patient selection methods, and the geographical and clinical setting had to be reported in the study.12 Data for infants or children whose age was not described were excluded to avoid confounding from potential maternal antibody transfer. Populations undergoing assessment in liver disease clinics and those sampled from other populations (defined as general populations) were analysed separately. We contacted study authors for clarification as required. Genotypic data were compiled from studies in which hepatitis D virus RNA was sequenced. We also searched the public sequence databases European Nucleotide Archive and GenBank with the same search strategy used in our initial search (appendix). We excluded genotypic data from studies of immigrants from sub-Saharan Africa who now reside outside the region. Our study was done in accordance with PRISMA recommendations.13
Statistical analysis
AJS extracted seroprevalence data. Duplicate data from the same locations were excluded. Confidence intervals (CIs) were computed by the Wilson method and pooled seroprevalence was calculated with the DerSimonian-Laird random-effects model with Freeman-Tukey double arcsine transformation.14, 15 We chose a random-effects model a priori because we anticipated heterogeneity arising from variation in study geography and populations. To avoid small sample bias in the random-effects model, we excluded studies in which fewer than ten patients underwent RNA testing, for our calculation of the pooled estimate of hepatitis D virus RNA positivity in patients seropositive for hepatitis D virus. Between-study heterogeneity was assessed with the I2 statistic. Seroprevalence in patients with liver disease compared with that in those without liver disease were pooled with a DerSimonian-Laird random-effects model.14 Meta-regression was done with a residual maximum-likelihood model to examine for sources of heterogeneity related to study location, rural versus urban setting, and the effect of HIV infection by comparison with data from cohorts in which the HIV status of recruited participants was known. We did sensitivity analyses to investigate the effect of population source and of using potentially unrepresentative samples. Risk of bias was independently assessed by AJS and MC with a prevalence critical appraisal tool.16 Publication bias was assessed by inspection of a funnel plot and Egger's test.17 Analyses were done with metan, metaprop, and metareg packages in Stata (version 14.2).
Role of the funding source
The study funder had no role in study design; data collection, analysis, or interpretation; or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
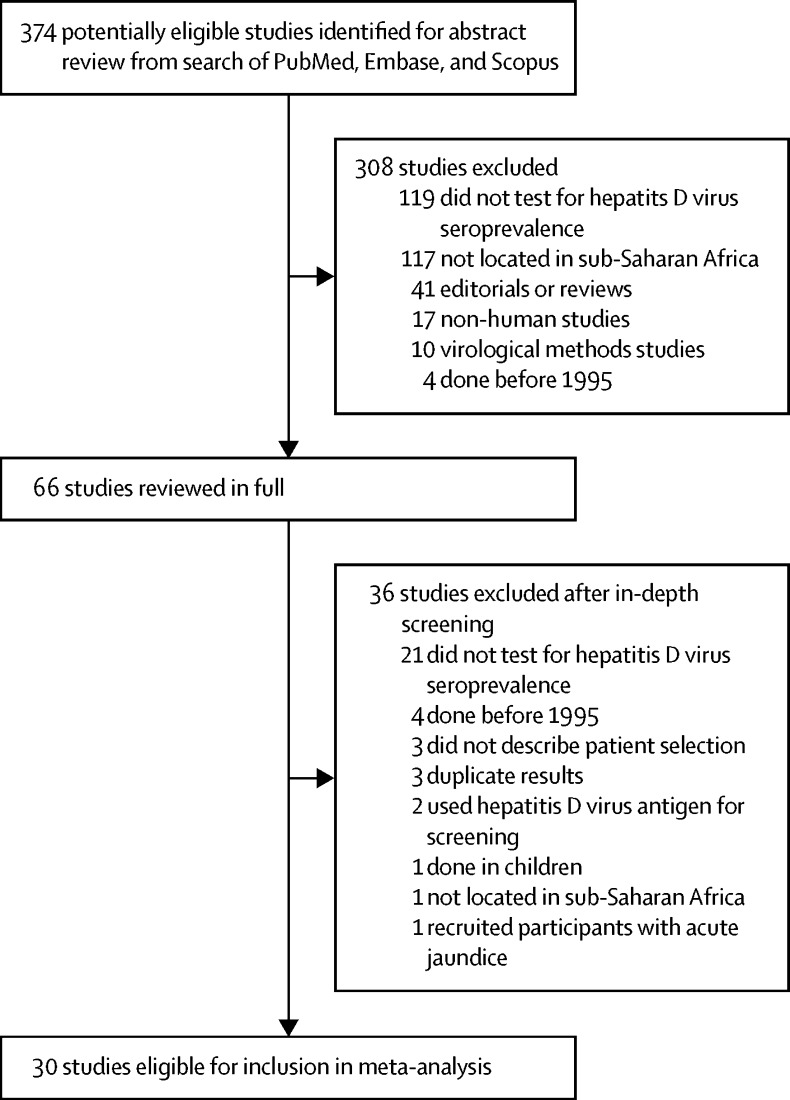
Our search returned 374 records, 30 of which met the inclusion criteria (figure 1). The 30 studies described 40 populations from 15 countries: 23 cohorts from eight west African countries (Benin, Burkina Faso, The Gambia, Ghana, Guinea-Bissau, Mauritania, Nigeria, and Senegal),18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 ten cohorts from three central African countries (Cameroon, Central African Republic, and Gabon),18, 35, 36, 37, 38, 39, 40, 41, 42, 43 and seven cohorts from four east or southern African countries (Botswana, Mozambique, South Africa, and Tanzania; figure 2; table).19, 44, 45, 46 We added data from previously characterised cohorts co-infected with HIV and hepatitis B virus infection in Malawi and Ghana (appendix).48, 49 Eight studies included populations21, 33, 34, 36, 37, 40, 43, 46 from rural settings; the rest were done in urban or mixed populations. Seven commercial enzyme immunoassays were used in studies to test for total anti-hepatitis D virus; in four studies28, 35, 36, 42 the test manufacturer was not stated (appendix). Patients were recruited in various settings: through community surveys,33, 34, 40 via blood donation,25, 30, 31, 34, 45 in antenatal care,19, 21, 37, 39, 44 during testing of health-care workers,36 at HIV clinics,18, 22, 23, 41, 44, 46 and at general medical clinics (patients did not have known liver disease).25, 32 Eight cohorts comprised exclusively HIV-positive participants.18, 22, 23, 41, 44, 46 HIV testing was done in 13 other cohorts: people with HIV were excluded from seven cohorts,24, 25, 30, 36, 43, 44 whereas the remaining six cohorts19, 21, 31, 34, 37, 45 had a HIV prevalence of 0·6–13·8%. HIV status was not reported in 19 cohorts.18, 20, 24, 26, 27, 28, 29, 32, 33, 34, 35, 38, 39, 40, 42, 47 In one study,31 HIV prevalence was compared according to hepatitis D virus serostatus, but it lacked statistical power because only six participants seropositive for hepatitis D virus were included.
Figure 1.
Selection of studies of hepatitis D virus epidemiology in sub-Saharan Africa, 1995–2016, for inclusion in meta-analysis
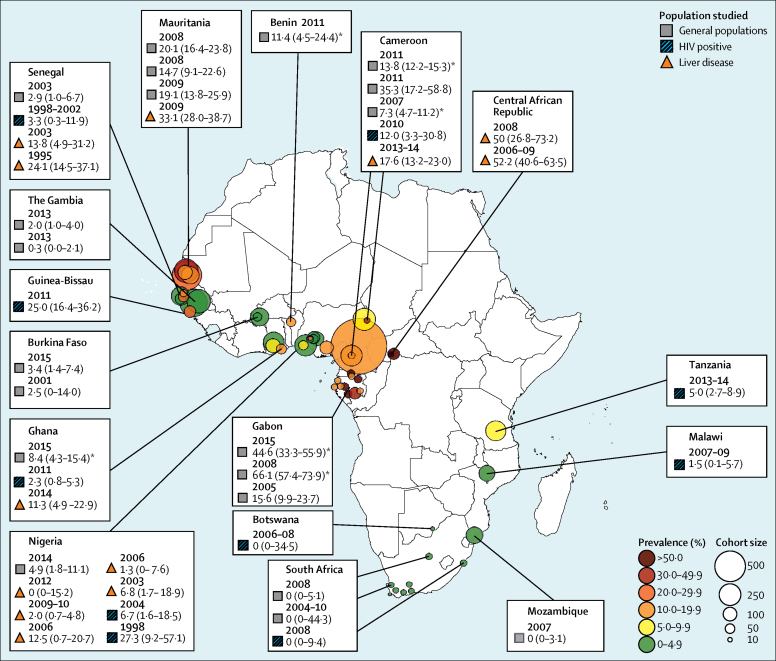
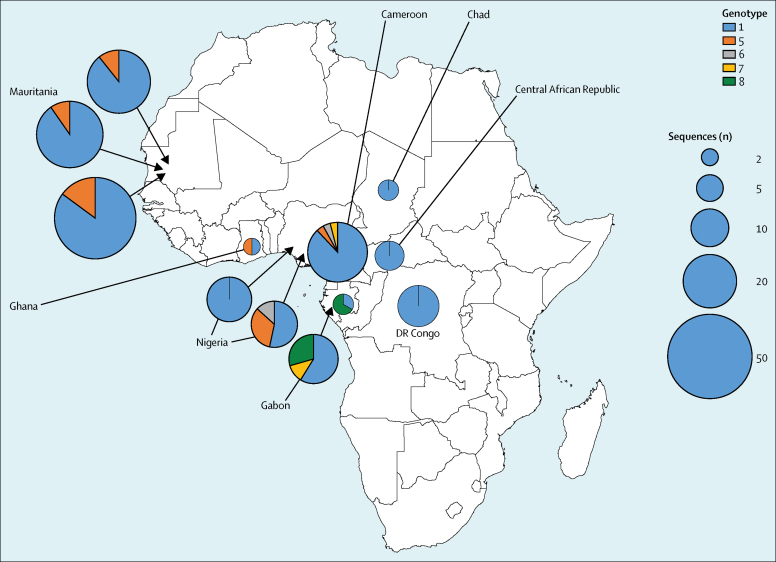
Figure 2.
Seroprevalence of hepatitis D virus among HBsAg carriers in sub-Saharan Africa in published studies, 1995–2016
Data in parentheses are 95% CIs. Colour and size of bubble plots show prevalence and cohort size, respectively. *Data obtained in rural settings.
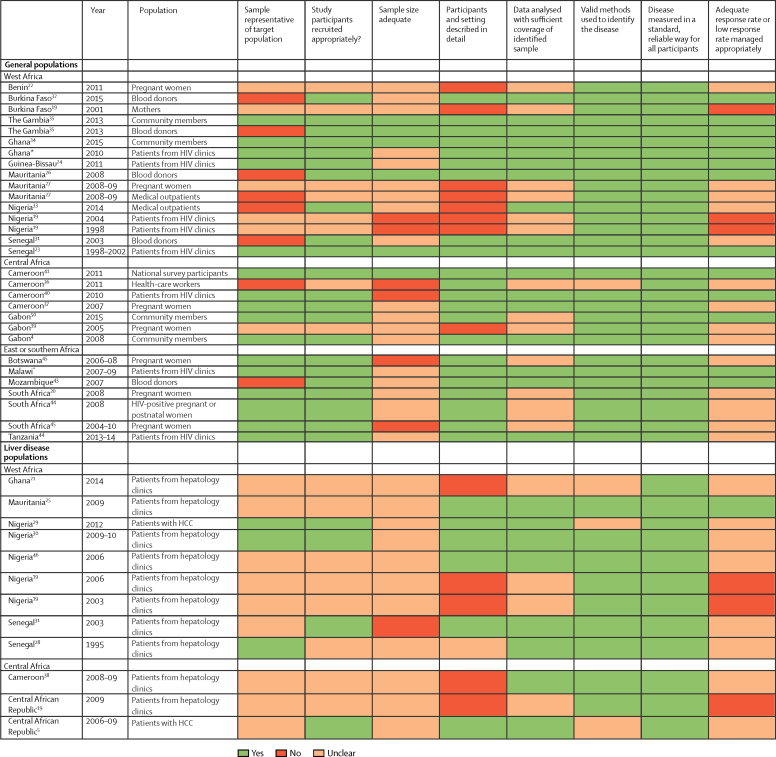
Table.
Prevalence of anti-hepatitis D virus and hepatitis D virus RNA in HBsAg-positive general populations and liver disease populations in sub-Saharan Africa, 1995–2015
| Year | Population | Tested (n) |
Anti-hepatitis D virus positive |
Hepatitis D virus RNA positive* |
||||
|---|---|---|---|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | |||||
| General populations | ||||||||
| West Africa | ||||||||
| Benin21 | 2011 | Pregnant women† | 44 | 5 (11%) | 5–24 | ·· | ·· | |
| Burkina Faso31 | 2015 | Blood donors | 177 | 6 (3%) | 1–7 | ·· | ·· | |
| Burkina Faso18 | 2001 | Mothers | 40 | 1 (3%) | 0–14 | 0 (0) | 0–83 | |
| The Gambia34 | 2013 | Community members† | 394 | 8 (2%) | 1–4 | ·· | ·· | |
| The Gambia34 | 2013 | Blood donors | 292 | 1 (<1%) | 0–2 | ·· | ·· | |
| Ghana33 | 2015 | Community members† | 107 | 9 (8%) | 4–15 | ·· | ·· | |
| Ghana‡ | 2010 | Patients from HIV clinics | 222 | 5 (2%) | 1–5 | 2 (40%) | 12–77 | |
| Guinea-Bissau23 | 2011 | Patients from HIV clinics | 72 | 18 (25%) | 16–36 | 4 (44%)§ | 19–73 | |
| Mauritania25 | 2008 | Blood donors | 447 | 90 (20%) | 17–24 | 56 (62%) | 52–72 | |
| Mauritania26 | 2008–09 | Pregnant women | 109 | 16 (15%) | 9–23 | 11 (69%) | 44–86 | |
| Mauritania26 | 2008–09 | Medical outpatients¶ | 162 | 31 (19%) | 14–26 | 21 (68%) | 50–82 | |
| Nigeria32 | 2014 | Medical outpatients¶ | 103 | 5 (5%) | 2–11 | ·· | ·· | |
| Nigeria18 | 2004 | Patients from HIV clinics | 45 | 3 (7%) | 2–19 | 2 (67%) | 20–94 | |
| Nigeria18 | 1998 | Patients from HIV clinics | 11 | 3 (27%) | 9–57 | 0 (0) | 0–62 | |
| Senegal30 | 2003 | Blood donors | 175 | 5 (3%) | 1–7 | ·· | ·· | |
| Senegal22 | 1998–2002 | Patients from HIV clinics | 61 | 2 (3%) | 0–12 | ·· | ·· | |
| Central Africa | ||||||||
| Cameroon42 | 2011 | National survey participants | 1627 | 225 (14%) | 12–15 | ·· | ·· | |
| Cameroon36 | 2011 | Health-care workers† | 17 | 6 (35%) | 17–59 | ·· | ·· | |
| Cameroon41 | 2010 | Patients from HIV clinics | 25 | 3 (12%) | 3–31 | 1 (33%) | 6–80 | |
| Cameroon37 | 2007 | Pregnant women† | 259 | 19 (7%) | 5–11 | ·· | ·· | |
| Gabon43 | 2015 | Community members†|| | 74 | 33 (45%) | 33–56 | ·· | ·· | |
| Gabon39 | 2005 | Pregnant women | 109 | 17 (16%) | 10–24 | ·· | ·· | |
| Gabon40 | 2008 | Community members†|| | 124 | 82 (66%) | 57–74 | ·· | ·· | |
| East or southern Africa | ||||||||
| Botswana44 | 2006–08 | Pregnant women | 9 | 0 (0) | 0–35 | ·· | ·· | |
| Malawi‡ | 2007–09 | Patients from HIV clinics | 133 | 2 (2%) | 0–6 | 0 (0) | 0–71 | |
| Mozambique45 | 2007 | Blood donors | 146 | 0 (0) | 0–3 | ·· | ·· | |
| South Africa19 | 2008 | Pregnant women | 87 | 0 (0) | 0–5 | ·· | ·· | |
| South Africa44 | 2008 | HIV-positive pregnant or postnatal women | 45 | 0 (0) | 0–9 | ·· | ·· | |
| South Africa44 | 2004–10 | Pregnant women | 6 | 0 (0) | 0–44 | ·· | ·· | |
| Tanzania46 | 2013–14 | Patients from HIV clinics† | 219 | 11 (5%) | 3–9 | 0 (0) | 0–30 | |
| Liver disease populations | ||||||||
| West Africa | ||||||||
| Ghana20 | 2014 | Patients from hepatology clinics | 53 | 6 (11%) | 5–23 | ·· | ·· | |
| Mauritania24 | 2009 | Patients from hepatology clinics | 296 | 98 (33%) | 28–39 | 61 (62%) | 52–71 | |
| Nigeria28 | 2012 | Patients with HCC | 26 | 0 (0) | 0–15 | ·· | ·· | |
| Nigeria29 | 2009–10 | Patients from hepatology clinics (15% had cirrhosis, 3% had HCC) | 245 | 5 (2%) | 1–5 | ·· | ·· | |
| Nigeria47 | 2006 | Patients from hepatology clinics (22% had cirrhosis, 51% had HCC) | 96 | 12 (13%) | 1–21 | ·· | ·· | |
| Nigeria18 | 2006 | Patients from hepatology clinics | 78 | 1 (1%) | 0–8 | 1 (100%) | 17–100 | |
| Nigeria18 | 2003 | Patients from hepatology clinics | 44 | 3 (7%) | 2–19 | 0 (0) | 0–62 | |
| Senegal30 | 2003 | Patients from hepatology clinics | 29 | 4 (14%) | 5–31 | ·· | ·· | |
| Senegal27 | 1995 | Patients from hepatology clinics (39% had cirrhosis, 57% had HCC) | 54 | 13 (24%) | 15–37 | ·· | ·· | |
| Central Africa | ||||||||
| Cameroon38 | 2008–09 | Patients from hepatology clinics | 233 | 41 (18%) | 13–23 | 25 (61%) | 42–74 | |
| Central African Republic18 | 2009 | Patients from hepatology clinics | 14 | 7 (50%) | 27–73 | 5 (71%) | 35–92 | |
| Central African Republic35 | 2006–09 | Patients with HCC | 69 | 36 (52%) | 41–64 | ·· | ·· | |
HCC=hepatocellular carcinoma.
Percentages are calculated in the group of patients who are anti-hepatitis D virus positive.
Study was done in a rural setting.
Data are from the present study.
Only nine of 18 samples were tested for hepatitis D virus RNA.
The study population was attendees at a general (non-hepatology) medical clinic without known liver disease.
Cluster-sampling community survey.
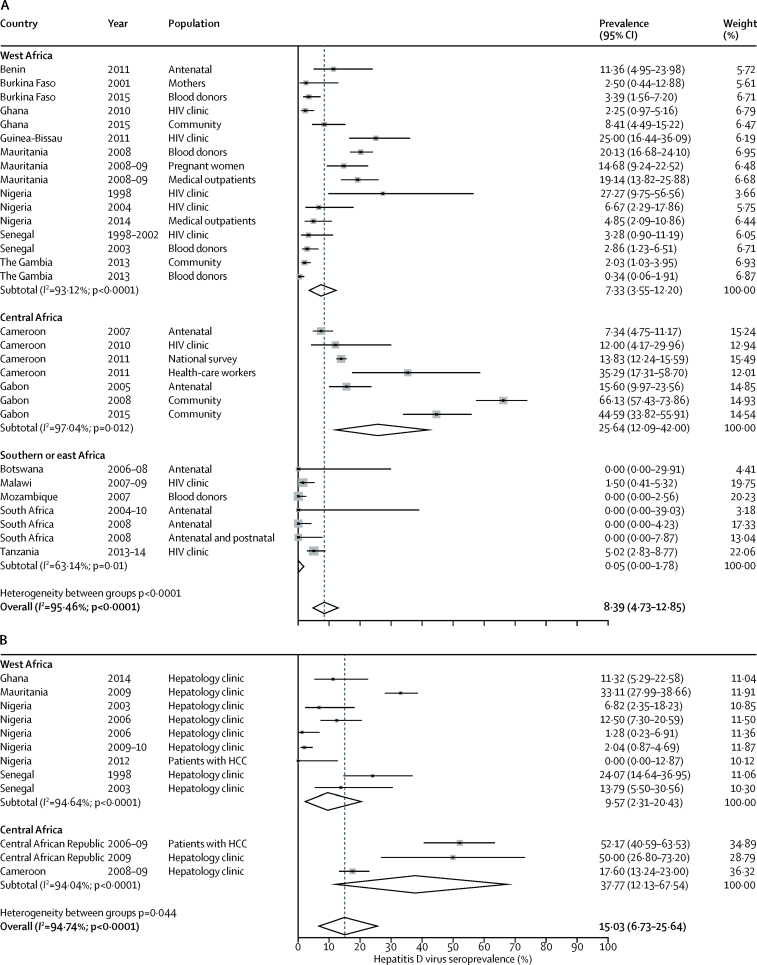
Among general populations with HBsAg, hepatitis D virus seroprevalence varied widely within geographical regions, from 0·34% to 27·27% in adults in west Africa,18, 21, 25, 26, 30, 31, 32 7·34% to 66·13% in central Africa,36, 37, 39, 40, 43 and 0·00% to 5·02% in east and southern Africa19, 44, 45, 46 (figure 3A; table). One cluster-sampling survey40 done in a rural area in northern Gabon was an extreme outlier, with a seroprevalence of 66·13%. Pooled overall seroprevalence of hepatitis D virus was 8·39% (95% CI 4·73–12·85; figure 3A). Seroprevalence was 7·33% in west Africa (95% CI 3·55-12·20), 25·64% in central Africa (95% CI 12·09–42·00), and 0·05% (95% CI 0·00–1·78%) in east and southern Africa; study region was significantly associated with seroprevalence (p=0·01). According to meta-regression analysis, relative to the reference category of west Africa, seroprevalence was significantly higher in central Africa (coefficient 0·17 [95% CI 0·04–0·30]; p=0·012), but was not significantly different in east or southern Africa (coefficient −0·07 [95% CI −0·21 to 0·07]; p=0·31). The seroprevalence of hepatitis D virus was significantly higher in studies in rural areas than in those in urban areas, but not after adjustment for confounding by African region (coefficient for rural dwelling 0·10 [95% CI −0·03 to 0·24]; p=0·13). Among the 21 studies in which HIV status was reported, seroprevalence of hepatitis D virus did not differ according to HIV prevalence, after adjustment for African region (coefficient per 10% increase in HIV prevalence −0·0002 [95% CI −0·01 to 0·01]; p=0·97).
Figure 3.
Forest plots of hepatitis D virus seroprevalence among HBsAg-positive patients in sub-Saharan Africa 1995–2016 in general populations (A) and liver-disease populations (B)
Data are from a random-effects model. HCC=hepatocellular carcinoma.
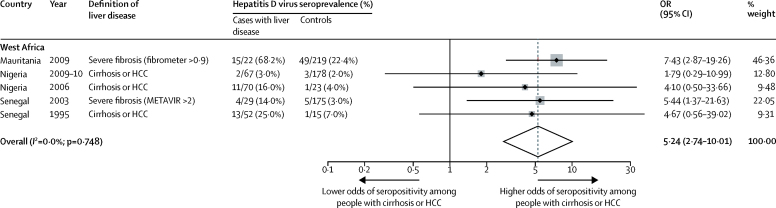
Among HBsAg-positive patients recruited from hepatology clinics, seroprevalence ranged from 0·00% to 33·11% among nine cohorts in Ghana, Mauritania, Nigeria, and Senegal,18, 20, 24, 27, 28, 29, 30, 47 with a pooled estimated seroprevalence of 9·57% (95% CI 2·31–20·43) in west Africa (figure 3B). In central Africa, the pooled prevalence from three studies18, 35, 38 from Cameroon and Central African Republic was 37·77% (95% CI 12·13–67·54). We noted significant heterogeneity between west and central Africa (p=0·04; figure 3B; table). In the five studies24, 27, 29, 30, 47 from Mauritania, Nigeria, and Senegal in which patients with evidence of liver disease (severe fibrosis, cirrhosis, or hepatocellular carcinoma) were directly compared with asymptomatic controls without evidence of liver disease drawn from the same population, the pooled odds ratio of the presence of anti-hepatitis D virus among HBsAg-positive patients with liver disease was 5·24 (95% CI 2·74–10·01; p<0·0001; figure 4).
Figure 4.
Forest plot of hepatitis D virus seroprevalence among patients with liver disease compared with asymptomatic controls in sub-Saharan Africa
Data are from a random-effects model. METAVIR is a histological scoring system based on liver biopsy. OR=odds ratio. HCC=hepatocellular carcinoma.
Testing for hepatitis D virus RNA by qualitative PCR in patients seropositive for hepatitis D virus was done in 324 patients (174 from general populations and 150 from liver-disease populations) in 16 populations.18, 22, 23, 24, 25, 26, 41, 44, 46 RNA positivity ranged from 0% to 69% in general populations, and from 0% to 71% in liver-disease populations (table), but some studies had very small patient numbers. Three studies25, 26 in blood donors, pregnant women, and medical inpatients from a site in Mauritania were included, in which the prevalence of RNA detected ranged from 62% to 69%, with a pooled estimate of 64% (95% CI 56–73). In a study46 done in Tanzania, no hepatitis D virus RNA was detected in 11 participants with HIV who were positive for anti-hepatitis D virus. In two studies in patients with liver disease from Mauritania and Central African Republic, RNA detection rates were 62% and 61% respectively, with a pooled estimate of 62% (95% CI 54–70).24, 38
Hepatitis D virus genotype data were included in seven studies.18, 24, 25, 26, 38, 39, 40 We identified two additional studies by searching public sequence databases. Of the 203 sequences available, genotype 1 was the most prevalent (median 88% [IQR 57–100]; figure 5; appendix).
Figure 5.
Distribution of hepatitis D virus genotypes in sub-Saharan Africa
Genotype data were derived from included studies and publicly available sequences deposited in Genbank and the European Nucleotide Archive database. Each bubble represents an individual study.
In our quality assessment, we identified recurrent issues with respect to incomplete description of study populations and sampling methods (figure 6). Testing methods did not commonly include confirmation of anti-hepatitis D virus seropositivity by either retesting or hepatitis D virus RNA detection. In most studies, hepatitis D virus epidemiology was not a primary outcome (data not shown), and none of the studies included sample size calculations or estimates of the completeness of the data, including the proportion of eligible people who participated in the study. In several studies, populations were selected that might have not been representative of the general population, including blood donors, health-care workers, and medical outpatients (figure 6). In a sensitivity analysis, exclusion of these studies did not affect estimates of overall prevalence of hepatitis D virus infection (p=0·92). Furthermore, in studies done in the general population, the type of patient recruited or location of recruitment (eg, blood donors, perinatal care, community, health-care workers, medical outpatients, HIV clinics) was not significantly associated with hepatitis D virus seroprevalence (p=0·30). No evidence of publication bias was evident in the funnel plot (appendix) or by the Egger's test (p=0·78).
Figure 6.
Quality assessment of included studies
HCC=hepatocellular carcinoma. *Data are from the present study.
Discussion
Epidemiological data for the prevalence of hepatitis D virus are needed to inform drug development and guide the formulation of policy on prevention, diagnosis, and management of the infection in sub-Saharan Africa, in agreement with recommendations from WHO.51 In this systematic review and meta-analysis, the estimated prevalence of anti-hepatitis D virus among general HBsAg-positive populations in sub-Saharan Africa was 8·39% (95% CI 4·73–12·85), which exceeded the estimated global prevalence of 5%.5 Relating these findings to the prevalence of hepatitis B virus infection would provide an estimated population prevalence of hepatitis B virus and D virus co-infection in sub-Saharan Africa of 0·7%, corresponding to around 7 million people.
Enzyme immunoassay, the method of screening for hepatitis D virus that was used in the included studies, provides case ascertainment of superinfection with hepatitis D virus in carriers of hepatitis B virus, but is thought to be less reliable for the detection of simultaneous hepatitis B virus and D virus co-infection because of high rates of virus clearance and subsequent disappearance of anti-hepatitis D virus.5, 52 Hepatitis D virus RNA was measured in participants positive for anti-hepatitis D virus in only 16 cohorts, only ten of which tested more than ten participants. In Mauritania, prevalence of RNA detection was consistent across populations, including pregnant women, blood donors, medical outpatients, and attendees at hepatology clinics, at around 62–69%. RNA was detected at a similar frequency in patients with liver disease in central Africa. Available data overall suggest persistent active hepatitis D virus replication in most patients positive for anti-hepatitis D virus, at least in settings with high seroprevalence. In settings with low seroprevalence, RNA was tested for in too few participants to draw firm conclusions about the prevalence of RNA positivity, and the resulting wide CIs overlap with those for estimates of RNA positivity in high-prevalence settings.
Hepatitis D virus seroprevalence was highest among HBsAg-positive populations in central Africa, and lowest in east and southern Africa, although more data are needed from the latter two regions to confirm these findings. Even across similar populations from close geographical regions, seroprevalence was notably heterogeneous. Consistent testing methods (ie, seven commercial assays) were used in all published studies, and thus available data suggest localised clusters of endemicity across sub-Saharan Africa. We did not identify an association between HIV status and hepatitis D virus seroprevalence, although HIV-positive and HIV-negative people in the same population were directly compared in only one study. Furthermore, HIV status was not ascertained in almost half the included studies. Thus, the absence of an association with HIV status should be interpreted with caution, and this finding contrasts with those from the USA and Taiwan, where increasing age, hepatitis C virus co-infection, and intravenous drug use were additonal risk factors for hepatitis D virus seropositivity.53, 54 Risk factors for hepatitis D virus infection in sub-Saharan Africa have not been established so far. Rural versus urban dwelling was not a risk factor after adjustment for confounding by geographical region in our analysis.
Hepatitis D virus infection is associated with accelerated progression to cirrhosis and increased incidence of hepatocellular carcinoma in carriers of hepatitis B virus, and cross-sectional assessments of hepatitis D virus seroprevalence can therefore be affected by survivorship bias.5, 52 In European populations, 15% of patients with chronic hepatitis D virus infection progress to cirrhosis within 1–2 years, and 70–80% progress within 5–10 years.55 Natural history data have not been reported in African populations or for hepatitis D virus genotypes 5–8, which are specific to the continent. Studies in which convenience sampling of hepatology units was done are helpful to capture the burden of hepatitis D virus among patients with severe liver disease, and our analysis suggests an increased likelihood of seropositivity among HBsAg-positive people with liver disease compared with asymptomatic controls without liver disease in sub-Saharan Africa. However, data are insufficient to derive an estimation of the burden of liver disease attributable to hepatitis D virus in sub-Saharan Africa, because liver disease was incompletely characterised as a result of the poor availability of validated measures of liver fibrosis.56
Our analysis has several limitations, which point to important research needs. First, we grouped various populations to facilitate summarising of the data. Published studies were few, addressed populations in various settings, and often had small sample sizes. Convenience sampling often included potentially unrepresentative populations, such as medical outpatients or health-care workers, although exclusion of these studies in sensitivity analyses did not affect estimates of hepatitis D virus seroprevalence in general populations. Substantial resources are needed to provide reliable prevalence estimates—sample sizes are large if drawn from unbiased community sampling, and have to be adjusted by the population prevalence of hepatitis B virus infection. Second, selection and method of ascertainment of the underlying hepatitis B virus infection are likely to affect hepatitis D virus estimates, and were frequently poorly described in the included studies. Third, serological results should ideally be substantiated with measurement of hepatitis D virus RNA to show active replication, but such confirmation was infrequently reported in included studies, raising the possibility of insufficient specificity of seroprevalence data even when commercial assays were used.57 RNA testing is not without problems, however. Evidence from an international external quality-control assessment suggested frequent false-negative results among 28 participating laboratories in 17 countries, particularly with the Africa-specific genotypes 5–8; thus, RNA detection might not provide adequate confirmation without rigorous standardisation.58 Finally, our regional pooled estimates of hepatitis D virus seroprevalence have wide CIs, reflecting the substantial heterogeneity of the available data.59 We adopted a random-effects model a priori to account for anticipated heterogeneity.12
In summary, our analysis provides a preliminary estimate of the epidemiology of hepatitis D virus infection in sub-Saharan Africa, and points to several important gaps in knowledge and directions for future research. Results suggest that co-infection with hepatitis B and D viruses could represent an important cause of liver disease in some regions and populations. Improved and systematically collected epidemiology data are needed, particularly for east and southern Africa, as is identification of risk factors for hepatitis D virus transmission. A clinical characterisation of hepatitis D virus infection is needed, particularly for the genotypes 5–8. A focus on patients with established liver disease is required to ascertain the burden of adverse hepatic outcomes attributable to hepatitis D virus. Future research initiatives should be accompanied by an assessment of the reliability of testing methods in the African setting.
Hepatitis B virus infection remains endemic across sub-Saharan Africa60 and improved implementation of measures to prevent hepatitis B virus infection—including vaccination, prevention of needle reuse in health care, quality-assured transfusion screening, and expansion of diagnosis and treatment services—is required to reduce the burden of both infections.50 Mathematical modelling suggests that maintaining infant hepatitis B virus vaccination coverage above 80% and improving birth-dose vaccination coverage for children born to HBsAg-positive mothers (presently less than 10% in sub-Saharan Africa), represents an effective strategy for the eradication of both hepatitis B and D virus infection.61, 62
Acknowledgments
Acknowledgments
AJS is supported by a Wellcome Trust Clinical PhD Fellowship, grant 205157/Z/16/Z.
Contributors
AJS did the literature search, appraised study quality, extracted, analysed, and interpreted data, did laboratory work, and wrote and revised the Article. MC developed the study, assessed studies for inclusion, appraised study quality, and reviewed the Article. AB did phylogenetic analysis of hepatitis D virus sequences and reviewed the Article. ROP developed the study and reviewed the Article. PCM provided input into data interpretation and reviewed the Article. AP and SK did laboratory work. LB provided statistical support. AMG designed the study, interpreted data, and wrote and revised the Article.
Declaration of interests
AMG reports consultancy and speaker fees from Abbott, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, and ViiV. The University of Liverpool is the recipient of research funds from Bristol-Myers Squibb, Gilead, Janssen, and ViiV for studies of which AMG is the principal investigator. AMG is employed as an expert scientist by Roche Pharma Research and Early Discovery. All other authors declare no competing interests.
Supplementary Material
References
- 1.Global Burden of Disease Study 2013 Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015;386:1546–1555. doi: 10.1016/S0140-6736(15)61412-X. [DOI] [PubMed] [Google Scholar]
- 3.Hughes SA, Wedemeyer H, Harrison PM. Hepatitis delta virus. Lancet. 2011;378:73–85. doi: 10.1016/S0140-6736(10)61931-9. [DOI] [PubMed] [Google Scholar]
- 4.Rizzetto M. Hepatitis D virus: introduction and epidemiology. Cold Spring Harb Perspect Med. 2015;5:a021576. doi: 10.1101/cshperspect.a021576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lempp FA, Ni Y, Urban S. Hepatitis delta virus: insights into a peculiar pathogen and novel treatment options. Nat Rev Gastroenterol Hepatol. 2016;13:580–589. doi: 10.1038/nrgastro.2016.126. [DOI] [PubMed] [Google Scholar]
- 6.Matthews PC, Geretti AM, Goulder PJ, Klenerman P. Epidemiology and impact of HIV coinfection with hepatitis B and hepatitis C viruses in Sub-Saharan Africa. J Clin Virol. 2014;61:20–33. doi: 10.1016/j.jcv.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 7.UNAIDS HIV/AIDS estimates: core epidemiological slides. 2014. http://www.unaids.org/sites/default/files/media_asset/20150714_epi_core_en.pdf (accessed March 25, 2017).
- 8.Lacombe K, Rockstroh J. HIV and viral hepatitis coinfections: advances and challenges. Gut. 2012;61(suppl 1):i47–i58. doi: 10.1136/gutjnl-2012-302062. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez-Montero JV, Vispo E, Barreiro P. Hepatitis delta is a major determinant of liver decompensation events and death in hiv-infected patients. Clin Infect Dis. 2014;58:1549–1645. doi: 10.1093/cid/ciu167. [DOI] [PubMed] [Google Scholar]
- 10.Koh C, Canini L, Dahari H. Oral prenylation inhibition with lonafarnib in chronic hepatitis D infection: a proof-of-concept randomised, double-blind, placebo-controlled phase 2A trial. Lancet Infect Dis. 2015;15:1167–1174. doi: 10.1016/S1473-3099(15)00074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bogomolov P, Alexandrov A, Voronkova N. Treatment of chronic hepatitis D with the entry inhibitor myrcludex B: First results of a phase Ib/IIa study. J Hepatol. 2016;65:490–498. doi: 10.1016/j.jhep.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A. 2009;172:137–159. doi: 10.1111/j.1467-985X.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 15.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21:607–611. [Google Scholar]
- 16.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 17.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andernach IE, Leiss LV, Tarnagda ZS. Characterization of hepatitis delta virus in sub-Saharan Africa. J Clin Microbiol. 2014;52:1629–1636. doi: 10.1128/JCM.02297-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersson MI, Maponga TG, Ijaz S. The epidemiology of hepatitis B virus infection in HIV-infected and HIV-uninfected pregnant women in the Western Cape, South Africa. Vaccine. 2013;31:5579–5584. doi: 10.1016/j.vaccine.2013.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asmah RH, Boamah I, Afodzinu M. Prevalence of hepatitis D infection in patients with hepatitis B virus-related liver diseases in Accra, Ghana. West Afr J Med. 2014;33:32–36. [PubMed] [Google Scholar]
- 21.De Paschale M, Ceriani C, Cerulli T. Prevalence of HBV, HDV, HCV, and HIV infection during pregnancy in northern Benin. J Med Virol. 2014;86:1281–1287. doi: 10.1002/jmv.23951. [DOI] [PubMed] [Google Scholar]
- 22.Diop-Ndiaye H, Toure-Kane C, Etard JF. Hepatitis B, C seroprevalence and delta viruses in HIV-1 Senegalese patients at HAART initiation (retrospective study) J Med Virol. 2008;80:1332–1336. doi: 10.1002/jmv.21236. [DOI] [PubMed] [Google Scholar]
- 23.Langhoff Hønge B, Jespersen S, Medina C. Hepatitis B and delta virus are prevalent but often subclinical co-infections among HIV infected patients in Guinea-Bissau, West Africa: a cross-sectional study. PLoS One. 2014;9:e99971. doi: 10.1371/journal.pone.0099971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lunel-Fabiani F, Mansour W, Amar AO. Impact of hepatitis B and delta virus co-infection on liver disease in Mauritania: a cross sectional study. J Infect. 2013;67:448–457. doi: 10.1016/j.jinf.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Mansour W, Bollahi MA, Hamed CT. Virological and epidemiological features of hepatitis delta infection among blood donors in Nouakchott, Mauritania. J Clin Virol. 2012;55:12–16. doi: 10.1016/j.jcv.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Mansour W, Malick FZ, Sidiya A. Prevalence, risk factors, and molecular epidemiology of hepatitis B and hepatitis delta virus in pregnant women and in patients in Mauritania. J Med Virol. 2012;84:1186–1198. doi: 10.1002/jmv.23336. [DOI] [PubMed] [Google Scholar]
- 27.Mbaye PS, Renaudineau Y, Diallo A. Hepatitis C virus and chronic hepatopathies in Dakar: case-control study. Med Trop (Mars) 2000;60:47–52. (in French). [PubMed] [Google Scholar]
- 28.Olal SO, Akere A, Otegbayo JA. Are patients with primary hepatocellular carcinoma infectious of hepatitis B, C and D viruses? Afr J Med Med Sci. 2012;41(suppl):187–191. [PubMed] [Google Scholar]
- 29.Onyekwere CA, Audu RA, Duro-Emmanuel F, Ige FA. Hepatitis D infection in Nigeria. Indian J Gastroenterol. 2012;31:34–35. doi: 10.1007/s12664-011-0158-9. [DOI] [PubMed] [Google Scholar]
- 30.Vray M, Debonne JM, Sire JM. Molecular epidemiology of hepatitis B virus in Dakar, Sénégal. J Med Virol. 2006;78:329–334. doi: 10.1002/jmv.20544. [DOI] [PubMed] [Google Scholar]
- 31.Sawadogo A, Ouédraogo AS, Poda A. Seroprevalence of hepatitis D virus among blood donors with antigene HBs at Bobo-Dioulasso regional transfusion center, Burkina Faso. J Afr Hepato Gastroenterol. 2016;10:31–33. [Google Scholar]
- 32.Opaleye OO, Japhet OM, Adewumi OM. Molecular epidemiology of hepatitis D virus circulating in Southwestern Nigeria. Virol J. 2016;13:61. doi: 10.1186/s12985-016-0514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ampah KA, Pinho-Nascimento CA, Kerber S. Limited genetic diversity of hepatitis B virus in the general population of the Offin River Valley in Ghana. PLoS One. 2016;11:e0156864. doi: 10.1371/journal.pone.0156864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lemoine M, Shimakawa Y, Njie R, on behalf of the PROLIFICA investigators Acceptability and feasibility of a screen-and-treat programme for hepatitis B virus infection in The Gambia: the Prevention of Liver Fibrosis and Cancer in Africa (PROLIFICA) study. Lancet Glob Health. 2016;4:e559–e567. doi: 10.1016/S2214-109X(16)30130-9. [DOI] [PubMed] [Google Scholar]
- 35.Bekondi C, Mobima T, Ouavene JO. Etiopathological factors of hepatocellular carcinoma in Bangui, Central African Republic: clinical, biological characteristics and virological aspects of patients. Pathol Biol (Paris) 2010;58:152–155. doi: 10.1016/j.patbio.2009.07.027. (in French). [DOI] [PubMed] [Google Scholar]
- 36.Birguel J, Ndong JG, Akhavan S. Viral markers of hepatitis B, C and D and HB vaccination status of a health care team in a rural district of Cameroon. Med Trop (Mars) 2011;71:201–202. (in French). [PubMed] [Google Scholar]
- 37.Ducancelle A, Abgueguen P, Birguel J. High endemicity and low molecular diversity of hepatitis B virus infections in pregnant women in a rural district of North Cameroon. PLoS One. 2013;8:e80346. doi: 10.1371/journal.pone.0080346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foupouapouognigni Y, Noah DN, Sartre MT, Njouom R. High prevalence and predominance of hepatitis delta virus genotype 1 infection in Cameroon. J Clin Microbiol. 2011;49:1162–1164. doi: 10.1128/JCM.01822-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Makuwa M, Caron M, Souquiere S, Malonga-Mouelet G, Mahe A, Kazanji M. Prevalence and genetic diversity of hepatitis B and delta viruses in pregnant women in Gabon: molecular evidence that hepatitis delta virus clade 8 originates from and is endemic in central Africa. J Clin Microbiol. 2008;46:754–756. doi: 10.1128/JCM.02142-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Makuwa M, Mintsa-Ndong A, Souquiere S, Nkoghe D, Leroy EM, Kazanji M. Prevalence and molecular diversity of hepatitis B virus and hepatitis delta virus in urban and rural populations in northern Gabon in central Africa. J Clin Microbiol. 2009;47:2265–2268. doi: 10.1128/JCM.02012-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salpini R, Fokam J, Ceccarelli L. High burden of HBV-infection and atypical HBV strains among HIV-infected Cameroonians. Curr HIV Res. 2016;14:165–171. doi: 10.2174/1570162x13666150930114742. [DOI] [PubMed] [Google Scholar]
- 42.Njouom R, Tejiokem MC, Texier G, Fontanet A. Prevalence of hepatitis B, hepatitis C and hepatitis D virus infections in Cameroon: results from a national population based survey (the ANRS 12289 project) J Viral Hepat. 2015;22:1–2. [Google Scholar]
- 43.Francois-Souquiere S, Makuwa M, Bisvigou U, Kazanji M. Epidemiological and molecular features of hepatitis B and hepatitis delta virus transmission in a remote rural community in central Africa. Infect Genet Evol. 2016;39:12–21. doi: 10.1016/j.meegid.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 44.Matthews PC, Beloukas A, Malik A. Prevalence and characteristics of hepatitis B virus (HBV) coinfection among HIV-positive women in South Africa and Botswana. PLoS One. 2015;10:e0134037. doi: 10.1371/journal.pone.0134037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cunha L, Plouzeau C, Ingrand P. Use of replacement blood donors to study the epidemiology of major blood-borne viruses in the general population of Maputo, Mozambique. J Med Virol. 2007;79:1832–1840. doi: 10.1002/jmv.21010. [DOI] [PubMed] [Google Scholar]
- 46.Winter A, Letang E, Vedastus Kalinjuma A. Absence of hepatitis delta infection in a large rural HIV cohort in Tanzania. Int J Infect Dis. 2016;46:8–10. doi: 10.1016/j.ijid.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 47.Nwokediuko SC, Ijeoma U. Seroprevalence of antibody to HDV in Nigerians with hepatitis B virus-related liver diseases. Niger J Clin Pract. 2009;12:439–442. [PubMed] [Google Scholar]
- 48.Aoudjane S, Chaponda M, Gonzalez Del Castillo AA. Hepatitis B virus sub-genotype A1 infection is characterized by high replication levels and rapid emergence of drug resistance in HIV-positive adults receiving first-line antiretroviral therapy in Malawi. Clin Infect Dis. 2014;59:1618–1626. doi: 10.1093/cid/ciu630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stockdale AJ, Phillips RO, Beloukas A. Liver fibrosis by transient elastography and virologic outcomes after introduction of tenofovir in lamivudine-experienced adults with HIV and hepatitis B virus coinfection in Ghana. Clin Infect Dis. 2015;61:883–891. doi: 10.1093/cid/civ421. [DOI] [PubMed] [Google Scholar]
- 50.Lemoine M, Thursz MR. Battlefield against hepatitis B infection and HCC in Africa. J Hepatol. 2017;66:645–654. doi: 10.1016/j.jhep.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 51.WHO . Combating hepatitis B and C to reach elimination by 2030. World Health Organization; Geneva: 2016. [Google Scholar]
- 52.Alfaiate D, Dény P, Durantel D. Hepatitis delta virus: From biological and medical aspects to current and investigational therapeutic options. Antiviral Research. 2015;122:112–129. doi: 10.1016/j.antiviral.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 53.Kushner T, Serper M, Kaplan DE. Delta hepatitis within the Veterans Affairs medical system in the United States: prevalence, risk factors, and outcomes. J Hepatol. 2015;63:586–592. doi: 10.1016/j.jhep.2015.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lin HH, Lee SS, Yu ML. Changing hepatitis D virus epidemiology in a hepatitis B virus endemic area with a national vaccination program. Hepatology. 2015;61:1870–1879. doi: 10.1002/hep.27742. [DOI] [PubMed] [Google Scholar]
- 55.Sureau C, Negro F. The hepatitis delta virus: replication and pathogenesis. J Hepatol. 2016;64(suppl):S102–S116. doi: 10.1016/j.jhep.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Lemoine M, Eholie S, Lacombe K. Reducing the neglected burden of viral hepatitis in Africa: strategies for a global approach. J Hepatol. 2015;62:469–476. doi: 10.1016/j.jhep.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 57.King S, Adjei-Asante K, Appiah L. Antibody screening tests variably overestimate the prevalence of hepatitis C virus infection among HIV-infected adults in Ghana. J Viral Hepat. 2015;22:461–468. doi: 10.1111/jvh.12354. [DOI] [PubMed] [Google Scholar]
- 58.Le Gal F, Brichler S, Sahli R, Chevret S, Gordien E. First international external quality assessment for hepatitis delta virus RNA quantification in plasma. Hepatology. 2016;64:1483–1494. doi: 10.1002/hep.28772. [DOI] [PubMed] [Google Scholar]
- 59.Greenland S. Can meta-analysis be salvaged? Am J Epidemiol. 1994;140:783–787. doi: 10.1093/oxfordjournals.aje.a117326. [DOI] [PubMed] [Google Scholar]
- 60.Lozano R, Naghavi M, Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goyal A, Murray JM. The impact of vaccination and antiviral therapy on hepatitis B and hepatitis D epidemiology. PLoS One. 2014;9:e110143. doi: 10.1371/journal.pone.0110143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Subaiya S, Dumolard L, Lydon P, Gacic-Dobo M, Eggers R, Conklin L. Global routine vaccination coverage, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:1252–1255. doi: 10.15585/mmwr.mm6444a5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.