Abstract
[Purpose] This study was conducted to investigate the effects of ankle control balance training (ACBT) on postural balance and gait ability in community-dwelling older adults. [Subjects and Methods] Fifty-four subjects were randomly divided into two groups, with 27 subjects in the ACBT group and 27 subjects in the control group. Subjects in the ACBT group received ACBT for 60 minutes, twice per week for 4 weeks, and all subjects had undergone fall prevention education for 60 minutes, once per week for 4 weeks. The main outcome measures, including the Berg balance scale; the functional reach test and one leg stance test for postural balance; and the timed up-and-go test and 10-meter walking test for gait ability, were assessed at baseline and after 4 weeks of training. [Results] The postural balance and gait ability in the ACBT group improved significantly compared to those in the control group, except BBS. [Conclusion] The results of this study showed improved postural balance and gait abilities after ACBT and that ACBT is a feasible method for improving postural balance and gait ability in community-dwelling older adults.
Keywords: Postural balance, Gait, Elderly
INTRODUCTION
Gait patterns, which go through changes as aging process prolongs, deliver significant impacts on the quality of life for the elderly1). It has been reported that the causes for fall, a major issue for the elderly, arise from various aspects, including low vision, cognitive impairment, postural hypotension, environmental problems and deterioration of gait and mobility2). From the above, since the fall during the gait is reported to consist 45% of all falls, it is considered as the significant risk factor for a fall while further closely associated with the aging process3,4,5). Ten to 15% of those who experienced falls also suffer substantial deterioration to their quality of life due to fractures or critical damages6). Hence, normal gait can be deemed vital to the life of the elderly.
Gait patterns of the elderly exhibit several characteristics, such as decreasing stride length, decline of stride time, decreasing gait velocity, declining cadence, decreasing time ratio of stand phase, increasing double limb stance and elevating step due to extended proximal surface7).
A major cause for falls during the gait is reported to be the tripping8). According to the study analyzing the tripping motions, the motions can be divided into forward movements of the leg for recovery after getting tripped and motions of supporting foot in order to sustain the body; advancing recovery limb is to prevent from falling by fully stretching the limb forward9) while the support limb is to enable holding the position by appropriately advancing the recovery limb through plantar flexion, knee extension and hip extension10, 11). Therefore, it was revealed that the muscle strength of lower limb is closely associated with the tripping motion, which led to an assertion where the muscle strength of lower limb needs to be enhanced to prevent such tripping motion; and the control of ankle centered on plantar flexion was particularly stressed12, 13). During gait cycle, ankle joint is involved with shock absorption and momentum. Shock absorption is controlled through eccentric contraction of tibialis anterior, and the momentum is generated by push-off motion and achieved by plantar flexor. Ankle strategy, an important means to postural balance, is deeply involved with the control of ankle joint14). The proper function of ankle joint is required for the entire body to safely move forward during the gait15, 16). However, since flexibility and muscle strength of ankle joint continuously deteriorates as aging process keeps progressing, it becomes more difficult to walk safely17, 18). Degradation of muscles surrounding the ankle and range of motion increase of ankle joint stiffness and causes unstable gait patterns19,20,21,22,23). These causes are bound to increase the risks of fall for the elderly16, 24). Especially, when postural balance of the entire body is disrupted such as an occasion of slipping, plantar flexor muscles plays a pivotal role of controlling center-of-mass25). Thus, degradation of muscle strength of the muscles surrounding ankles due to aging process may hinder the ability to maintain balance and increase the possibilities of fall. In conclusion, ankle control is indispensable to prevent a fall.
Consequently, this study aims to ascertain the effects on balance and gait by applying ankle control balance training (ACBT) to community-dwelling old adults to prevent a fall.
SUBJECTS AND METHODS
Community-dwelling older adults were recruited by the principal author through advertisements in senior welfare centre, senior sports clubs, and senior society organizations in South Korea.
The following inclusion criteria were applied: age ≥65 years, either two or more falls during the previous 12 months or one fall. Participants were excluded if they had any musculoskeletal impairment, neurological impairment, vision impairment, or vestibular disease, or dementia (Mini-Mental State Examination score <24/30).
Participants whose training participation rate was below 80% were excluded from the final analyses. The goals and procedures of the study were explained to all subjects. Only those who signed the study participation consent form voluntarily were selected as subjects and the study was approved by the Institutional Review Board of Sahmyook University.
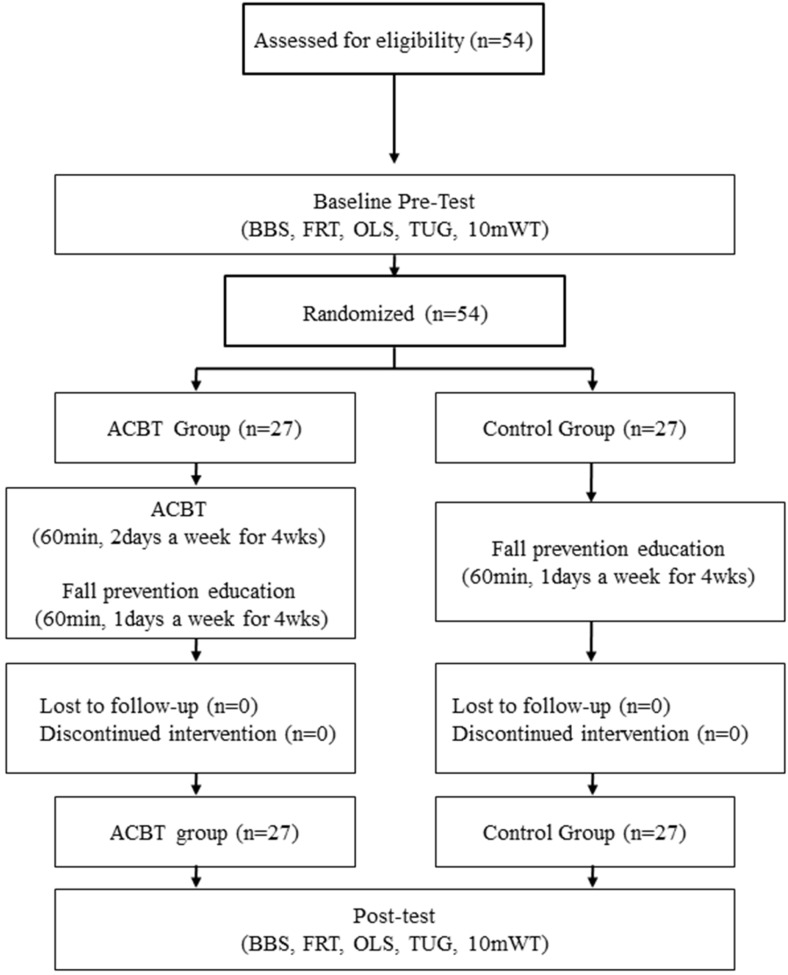
Fifty-four subjects who met the inclusion criteria were randomly divided into two groups, an ACBT group (n=27) and a control group (n=27) using Random Allocation Software (version 1.0) (Saghaei, 2004). No significant differences were observed among the three groups for gender, age, height, weight, experience of falls (Table 1, Fig. 1).
Table 1. General characteristics of subject (N=54).
| ACBT group n=27 |
Control group n=27 |
|
|---|---|---|
| Age (years) | 71.6 ± 3.6 | 72.7 ± 5.2 |
| Height (cm) | 164.3 ± 7.0 | 161.6 ± 10.0 |
| Weight (kg) | 62.0 ± 7.8 | 60.9 ± 9.2 |
| BMI (point) | 22.9 ± 2.3 | 23.2 ± 1.9 |
| MMSE-K | 25.8 ± 1.3 | 25.8 ± 0.9 |
| Gender (male/female) | 17/10 | 16/11 |
BMI: body mass index; MMSE-K: mini mental state examination-Korean. Values are expressed as mean ± standard deviation.
Fig. 1.
Flow diagram of ths study
This study used a randomized, single-blinded design. To determine the sample size, the G-Power 3.19 software was used (Faul, Erdfelder, Lang, & Buchner, 2007). To calculate the sample size, the probability of alpha error and power were set at 0.05 and 0.8, respectively. In addition, the effect size was set at 0.8, based on Cohen’s methods (Cohen, 1977). Therefore, a sample size of 26 patients per group was necessary. By estimating a drop-out rate of about 10%, 27 participants per group needed to be recruited for randomization.
The training was composed of 3 minutes of stretching, 5 minutes of warm-up exercise including 2 minutes of slow walking, 40 minutes of main exercise, and 10 minutes of cool-down exercise, totalling 60 minutes. The training was conducted under the supervision of four therapists, for the safety of the subjects. The subjects wore shoes but did not use walking aids.
The ACBT was designed based on exercises previously shown to improve ankle control and balance26, 27).
Warm-up included gentle stretching, forward, backward, and sideways step-ups on foam and massage with a sensory ball, all performed to light smoothing music. This warm-up was performed to increase muscle flexibility.
The ACBT consisted of three parts. The exercise interventions were performed on a high-elasticity balance-training mat. Static exercise on a training mat comprised heel and toe raises, one-legged stance for each limb, weight shifting forward, backward, sideward and diagonally, and turning the head to the left and then to the right keeping the feet together. This exercise comprised two 10-min sessions each, with eyes opened and eyes closed, respectively. While performing the second set of exercises, patients were paired for safety reasons and they performed in turns. Dynamic exercise on the training mat involved walking, step-ups, and bipedal jumps for 10 min. Progressive balance exercises on the training mat involved narrow walking, walking backward, walking sideward, stepping over obstacles, stepping on obstacles, passing balls arranged on the training mat in a circle, and throwing and catching a ball on the training mat for 10 min.
Following balance training, cool-down exercises were performed to prevent muscle fatigue, to relax tensed muscles, and to help return the heart and respiratory rates to normal. These exercises included deep breathing, abdominal breathing, and static back extensor exercises in a reclined position.
Identical training products were used for all participants (high-elasticity balance training mat (StimUp, Alfoots, Korea): 46 × 496 × 6 cm; polyurethane foam ball (Polyurethan soft ball; EDUFOAM, Korea): diameter, 17 cm; yellow Theraband (Thera-band; Hygenic Corporation, USA): length, 40 cm and resistance, 1 kg).
The both groups received health education on fall prevention. The educational topics included cause of falling, fall risk factor, home safety evaluation, necessary of fall prevention exercise, and environment problems.
Postural balance was measured by the one-leg-standing (OLS) test, the Berg Balance Scale (BBS), and Functional reach test (FRT). The OLS test is used to assess postural stability. Participants were instructed to balance on the non-dominant leg with eyes opened and arms spread for as long as possible. The time elapsed before the contralateral foot touched the ground was measured in seconds using a stopwatch. This test was performed twice, and the highest score was recorded. The BBS has been used to evaluate functional balance in a wide range of subjects, including elderly individuals with a high risk of falling and patients with acute and chronic diseases. It consists of 14 items common to daily activities; each item is rated on a 5-point scale from 0 to 4, with higher scores indicating better balance. The FRT evaluates the limits of physical stability, and measures dynamic balance and flexibility as subjects perform functional tasks. The FRT measures the maximum distance that subjects can reach forward as far as possible their own arm’s length while maintaining a fixed base of support in the standing position. The distance was measured in centimeters using a Laser Range Finder (DLE50, BOSCH, Germany). Results represent the average of 3 consecutive measurements.
Gait ability was measured by the timed up-and-go (TUG) test and 10-meter walking test (10MWT). TUG test is used to predict fall risk by examining balance ability and functional mobility. 36 It measures the time it takes a subject to stand up from an armchair (46 cm height), walk a distance of 3 meters, and then turn around, walk back to the chair, and sit down again. The total time taken to complete the circuit was measured in seconds with a stopwatch. The 10MWT is a standard test used to investigate the extent of gait ability. The test was repeated 3 times, and the results were averaged.
Descriptive statistics were used to summarize baseline characteristics data. The Shapiro-Wilk test was used to test variables for normality. Comparisons of baseline characteristics between the ACBT group and control group were analysed using a χ2 test. The independent t-test was used to compare changes in postural balance and gait ability between the ACBT group and control group. Comparisons between pre-and post-treatment data within each group were analysed using a paired t-test. SPSS version 18.0 for Windows was used to perform all analyses, and p values <0.05 were regarded as significant.
RESULTS
Regarding changes in postural balance, FRT and OLS were significantly improved except BBS in the ACBT group (p<0.05). However, the control group displayed no significant differences for any of these variables following the intervention. In addition, FRT and OLS were significantly lower in the ACBT group than the control group (p<0.05) (Table 2).
Table 2. The changes of postural balance (N=54).
| ACBT group (n=27) |
Control group (n=27) |
||
|---|---|---|---|
| BBS | Pre | 54.4 ± 2.4 | 54.1 ± 2.6 |
| (point) | Post | 54.7 ± 2.6 | 54.1 ± 2.3 |
| Pre-Post | 0.3 ± 0.9* | 0.0 ± 0.8 | |
| FRT | Pre | 36.3 ± 3.6 | 35.4 ± 4.2 |
| (cm) | Post | 37.4 ± 4.2 | 35.5 ± 4.3 |
| Pre-Post | 1.1 ± 1.4*† | 0.1 ± 1.4 | |
| OLST | Pre | 29.1 ± 6.7 | 32.3 ± 10.2 |
| (sec) | Post | 39.6 ± 11.1 | 30.8 ± 12.9 |
| Pre-Post | 10.5 ± 7.1*† | –1.5 ± 18.5 | |
BBS: Berg balance scale; FRT: functional reach test; OLST: one leg stance test. Values are expressed as mean ± standard deviation (SD). *Significant difference within group. †Significant difference between groups.
Regarding changes in gait ability, TUG test, and 10MWT were significantly improved in the ACBT group (p<0.05). However, the control group displayed no significant differences for any of these variables following the intervention. In addition, TUG test, and 10MWT were significantly lower in the ACBT group than the control group (p<0.05) (Table 3).
Table 3. The changes of gait ability (N=54).
| ACBT group (n=27) |
Control group (n=27) |
||
|---|---|---|---|
| TUG | Pre | 10.5 ± 3.5 | 9.9 ± 2.3 |
| (sec) | Post | 9.4 ± 2.9 | 9.7 ± 2.5 |
| Pre-Post | –1.1 ± 1.4*† | –0.2 ± 0.9 | |
| 10mWT | Pre | 10.6 ± 3.3 | 9.9 ± 1.4 |
| (sec) | Post | 9.5 ± 3.9 | 9.4 ± 1.8 |
| Pre-Post | –1.1 ± 1.3*† | –0.5 ± 1.2 | |
TUG: timed up and go test; 10mWT: 10 m walk test. Values are expressed as mean ± standard deviation (SD). *Significant difference within group. †Significant difference between groups.
DISCUSSION
The aim of this study was to investigate the effects of ACBT for balance and gait ability associated with the elderly fall. There was a significant improvement in balance and gait ability after ACBT which means may reduce the risk of fall.
The balance is a pivotal index to forecast a fall; and it was evaluated through numerous studies by using BBS, FRT and OLS28,29,30,31). Also in this study, BBS showed 0.1% improvement by assessing BBS, FRT and OLS, where FRT and OLS displayed 3% and 36% improvements respectively.
BBS scores by the subjects of this study delivered high initial scores (54 points), but it did not show significant changes following the intervention due to ceiling effect. Other studies also report that the changes in BBS following the intervention fail to show statistically significant differences10, 29). It is also believed to be caused by the distinction of BBS tools.
FRS test is designed to evaluate the limits of stability. FRT presented an average of 34 cm for male adults between the age of 70 and 87 and 27 cm for females from the same age group. Lower than 15.20 through 17.78 cm of the FRT is treated as limitation of functional balance. Since the elderly of this study exhibited the 31 cm, the study demonstrated the initial value similar with previous studies when considering the genders32), and it presented 7% improvement of static balance following the intervention.
OLS may be quite simple yet has been used as quite a useful tool to evaluate the risk of fall33, 34). Despite its usefulness, there have been quite a few studies asserting that it is not associated with a fall. Considering other studies on interventions to prevent falls of the elderly, one leg stance with eyes open delivered rather a wide range of results with 3 to 40 seconds35, 36). Previous studies reported the time of OLS based on the age. Old adults, especially in their 80s, showed results of OLS with a significantly wide range, which made difficult direct comparison37). However, because this study was frequently involved with muscles participating in ankle strategy or hip strategy, where interventional motions are deeply involved with balance, it is believed that OLS was improved. The motion of one leg stance is responsible for 40% of all gait motions, and it also enables the swing of the other limb. Hence, OLS test is closely related to balance ability and mobility including gait34, 38). Through the findings from the balance-related indexes, it is believed that the gait training based on the ACBT is effective in improving the balance, a key index to the risk of a fall.
In this study, gait was assessed through TUG and 10MWT. TUG time of the control group was significantly reduced from 10.48 seconds to 9.42 seconds which means reduced 10% compared with initial value (p<0.05). The investigation provided 8 to 13.1 seconds for normal male adults in their 60s39), and it reported that the chance of a fall is high when it takes 14 seconds or longer40). The study by Desai et al.41) also reported that TUG time was significantly increased from the group who have not previously experienced a fall amongst the elderly. TUG time of the subjects of this study is within the normal range; however, it is believed that it reduced the risk for the subjects with high risks of falling as they showed 10% decrease following the intervention. The fact that TUG time is reduced suggests that the functional mobility has improved since the gait ability and dynamic balance ability were increased. Improving dynamic balance ability is considered as the foundation to improve mobility while preventing falls42).
15% of the adults who are 60 years old or older showed anomaly in their gait, while postural imbalance and gait disturbance leads to the risk of falling. With unstable balance, a subject is prone to widen their stance to compensate the imbalance, lower the center of gravity by bending the knees and somewhat widen and bend the arms to take a posture preparing for the risks. Therefore, they walk slowly with short step and maintaining bent position43). Subsequently, it slows down the gait speed as well as reduces the length of step, which leads to the reduced cadence. It is originated from an attempt to adapt the body to the discreet gait pattern to enhance gait stability and reduce the risks of falling44). At the same time, preceding studies17, 18) pointed out that the strength of ankle plays a key role to walk across geographical features or to safely move the body forward. During gait, it appeared that elderly is not capable of proving proper strength to the ankle compared to young people17, 18). Because degradation of senses and motor skills as a part of natural aging process affects mobility, especially the gait requiring complex movements, most of fall incidents of the elderly occur during the gait, and the reduced gait ability becomes a risk factor for falls45).
Based on the findings of this study, 10MWT was significantly improved by 10% from 10.59 sec to 9.46 sec.
The study by Trombetti et al.46) also reported that gait speed was increased by 5.5 cm/s from 104.2 cm/s to 109.7 cm/s after having the old adults at an average age of 75 to exercise. Cadence was increased by 2.9 from 108.1 to 111 but not significant. But the number of falls after intervention was decreased, and the risk of a fall was also reduced; and it delivered a reducing effect to a fall at 54%.
Gait required balance ability, and there is a significant correlation between gait speed and balance38). Thus, this study suggests that the improvement of postural balance improves gait ability as they bring the increase gait speed.
The present study verified the beneficial effects of ACBT which are considered an effective intervention for fall prevention and improving fall-related parameters in community-dwelling older adults.
REFERENCES
- 1.Stolze H, Klebe S, Zechlin C, et al. : Falls in frequent neurological diseases—prevalence, risk factors and aetiology. J Neurol, 2004, 251: 79–84. [DOI] [PubMed] [Google Scholar]
- 2.Moylan KC, Binder EF: Falls in older adults: risk assessment, management and prevention. Am J Med, 2007, 120: 493.e1–493.e6. [DOI] [PubMed] [Google Scholar]
- 3.Lopopolo RB, Greco M, Sullivan D, et al. : Effect of therapeutic exercise on gait speed in community-dwelling elderly people: a meta-analysis. Phys Ther, 2006, 86: 520–540. [PubMed] [Google Scholar]
- 4.Hausdorff JM, Edelberg HK, Mitchell SL, et al. : Increased gait unsteadiness in community-dwelling elderly fallers. Arch Phys Med Rehabil, 1997, 78: 278–283. [DOI] [PubMed] [Google Scholar]
- 5.Maki BE: Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc, 1997, 45: 313–320. [DOI] [PubMed] [Google Scholar]
- 6.Rubenstein LZ, Powers CM, MacLean CH: Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders. Ann Intern Med, 2001, 135: 686–693. [DOI] [PubMed] [Google Scholar]
- 7.Kirtley C: Clinical gait analysis: theory and practice. New York: Churchill Livingstone, 2006. [Google Scholar]
- 8.Blake AJ, Morgan K, Bendall MJ, et al. : Falls by elderly people at home: prevalence and associated factors. Age Ageing, 1988, 17: 365–372. [DOI] [PubMed] [Google Scholar]
- 9.Grabiner MD, Koh TJ, Lundin TM, et al. : Kinematics of recovery from a stumble. J Gerontol, 1993, 48: M97–M102. [DOI] [PubMed] [Google Scholar]
- 10.Owings TM, Pavol MJ, Grabiner MD: Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin Biomech (Bristol, Avon), 2001, 16: 813–819. [DOI] [PubMed] [Google Scholar]
- 11.Pavol MJ, Owings TM, Foley KT, et al. : Influence of lower extremity strength of healthy older adults on the outcome of an induced trip. J Am Geriatr Soc, 2002, 50: 256–262. [DOI] [PubMed] [Google Scholar]
- 12.Pijnappels M, Bobbert MF, van Dieën JH: Push-off reactions in recovery after tripping discriminate young subjects, older non-fallers and older fallers. Gait Posture, 2005, 21: 388–394. [DOI] [PubMed] [Google Scholar]
- 13.Pijnappels M, van der Burg PJ, Reeves ND, et al. : Identification of elderly fallers by muscle strength measures. Eur J Appl Physiol, 2008, 102: 585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carrier DR, Heglund NC, Earls KD: Variable gearing during locomotion in the human musculoskeletal system. Science, 1994, 265: 651–653. [DOI] [PubMed] [Google Scholar]
- 15.Lark SD, Buckley JG, Bennett S, et al. : Joint torques and dynamic joint stiffness in elderly and young men during stepping down. Clin Biomech (Bristol, Avon), 2003, 18: 848–855. [DOI] [PubMed] [Google Scholar]
- 16.Gehlsen GM, Whaley MH: Falls in the elderly: Part II, Balance, strength, and flexibility. Arch Phys Med Rehabil, 1990, 71: 739–741. [PubMed] [Google Scholar]
- 17.Chen IH, Andriacchi TP: The influence of walking speed on mechanical joint power during gait. Gait Posture, 1997, 6: 171–176. [Google Scholar]
- 18.Mickelborough J, van der Linden ML, Tallis RC, et al. : Muscle activity during gait initiation in normal elderly people. Gait Posture, 2004, 19: 50–57. [DOI] [PubMed] [Google Scholar]
- 19.Ho CY, Bendrups AP: Ankle reflex stiffness during unperceived perturbation of standing in elderly subjects. J Gerontol A Biol Sci Med Sci, 2002, 57: B344–B350. [DOI] [PubMed] [Google Scholar]
- 20.Vandervoort AA, Chesworth BM, Cunningham DA, et al. : Age and sex effects on mobility of the human ankle. J Gerontol, 1992, 47: M17–M21. [DOI] [PubMed] [Google Scholar]
- 21.Buzzi UH, Stergiou N, Kurz MJ, et al. : Nonlinear dynamics indicates aging affects variability during gait. Clin Biomech (Bristol, Avon), 2003, 18: 435–443. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Lockhart TE: Age-related joint moment characteristics during normal gait and successful reactive-recovery from unexpected slip perturbations. Gait Posture, 2009, 30: 276–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lockhart TE, Woldstad JC, Smith JL: Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics, 2003, 46: 1136–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whipple RH, Wolfson LI, Amerman PM: The relationship of knee and ankle weakness to falls in nursing home residents: an isokinetic study. J Am Geriatr Soc, 1987, 35: 13–20. [DOI] [PubMed] [Google Scholar]
- 25.Gatev P, Thomas S, Kepple T, et al. : Feedforward ankle strategy of balance during quiet stance in adults. J Physiol, 1999, 514: 915–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee K, Lee S, Song C: Whole-body vibration training improves balance, muscle strength and glycosylated hemoglobin in elderly patients with diabetic neuropathy. Tohoku J Exp Med, 2013, 231: 305–314. [DOI] [PubMed] [Google Scholar]
- 27.Song CH, Petrofsky JS, Lee SW, et al. : Effects of an exercise program on balance and trunk proprioception in older adults with diabetic neuropathies. Diabetes Technol Ther, 2011, 13: 803–811. [DOI] [PubMed] [Google Scholar]
- 28.Cakar E, Dincer U, Kiralp MZ, et al. : Jumping combined exercise programs reduce fall risk and improve balance and life quality of elderly people who live in a long-term care facility. Eur J Phys Rehabil Med, 2010, 46: 59–67. [PubMed] [Google Scholar]
- 29.Helbostad JL, Moe-Nilssen R: The effect of gait speed on lateral balance control during walking in healthy elderly. Gait Posture, 2003, 18: 27–36. [DOI] [PubMed] [Google Scholar]
- 30.Persch LN, Ugrinowitsch C, Pereira G, et al. : Strength training improves fall-related gait kinematics in the elderly: a randomized controlled trial. Clin Biomech (Bristol, Avon), 2009, 24: 819–825. [DOI] [PubMed] [Google Scholar]
- 31.Stevenson TJ, Connelly DM, Murray JM, et al. : Threshold Berg balance scale scores for gait-aid use in elderly subjects: a secondary analysis. Physiother Can, 2010, 62: 133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duncan PW, Weiner DK, Chandler J, et al. : Functional reach: a new clinical measure of balance. J Gerontol, 1990, 45: M192–M197. [DOI] [PubMed] [Google Scholar]
- 33.Englund U, Littbrand H, Sondell A, et al. : A 1-year combined weight-bearing training program is beneficial for bone mineral density and neuromuscular function in older women. Osteoporos Int, 2005, 16: 1117–1123. [DOI] [PubMed] [Google Scholar]
- 34.Persad CC, Cook S, Giordani B: Assessing falls in the elderly: should we use simple screening tests or a comprehensive fall risk evaluation? Eur J Phys Rehabil Med, 2010, 46: 249–259. [PubMed] [Google Scholar]
- 35.Jonsson E, Seiger A, Hirschfeld H: One-leg stance in healthy young and elderly adults: a measure of postural steadiness? Clin Biomech (Bristol, Avon), 2004, 19: 688–694. [DOI] [PubMed] [Google Scholar]
- 36.Mao DW, Li JX, Hong Y: The duration and plantar pressure distribution during one-leg stance in Tai Chi exercise. Clin Biomech (Bristol, Avon), 2006, 21: 640–645. [DOI] [PubMed] [Google Scholar]
- 37.Bohannon RW, Larkin PA, Cook AC, et al. : Decrease in timed balance test scores with aging. Phys Ther, 1984, 64: 1067–1070. [DOI] [PubMed] [Google Scholar]
- 38.Jacquelin Perry JB: Gait analysis: normal and pathological function. New Jersey: Slack, 2010. [Google Scholar]
- 39.Steffen TM, Hacker TA, Mollinger L: Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther, 2002, 82: 128–137. [DOI] [PubMed] [Google Scholar]
- 40.Shumway-Cook A, Brauer S, Woollacott M: Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther, 2000, 80: 896–903. [PubMed] [Google Scholar]
- 41.Desai A, Goodman V, Kapadia N, et al. : Relationship between dynamic balance measures and functional performance in community-dwelling elderly people. Phys Ther, 2010, 90: 748–760. [DOI] [PubMed] [Google Scholar]
- 42.Howe TE, Rochester L, Jackson A, et al. : Exercise for improving balance in older people. Cochrane Database Syst Rev, 2007, (4): CD004963. [DOI] [PubMed] [Google Scholar]
- 43.Morris JN, Howard EP, Steel K, et al. : Strategies to reduce the risk of falling: cohort study analysis with 1-year follow-up in community dwelling older adults. BMC Geriatr, 2016, 16: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lamoth CJ, van Deudekom FJ, van Campen JP, et al. : Gait stability and variability measures show effects of impaired cognition and dual tasking in frail people. J Neuroeng Rehabil, 2011, 8: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Bruin ED, Schoene D, Pichierri G, et al. : Use of virtual reality technique for the training of motor control in the elderly. Some theoretical considerations. Z Gerontol Geriatr, 2010, 43: 229–234. [DOI] [PubMed] [Google Scholar]
- 46.Trombetti A, Hars M, Herrmann FR, et al. : Effect of music-based multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Arch Intern Med, 2011, 171: 525–533. [DOI] [PubMed] [Google Scholar]