Abstract
[Purpose] Locomotive syndrome (LS) is a condition by which older people may require care service because of problems with locomotive organs. This study examined whether the loco-check, a 7-item questionnaire, is useful for quantitatively assessing the severity of LS. [Subjects and Methods] Seventy-one community dwelling Japanese females aged 64–96 years (81.7 ± 8.0 years) participated in this study. The associations of the loco-check with thigh muscle mass measured by X-ray CT, physical performance, nutritional status, and quality of life (QOL) were investigated. [Results] The results showed that the number of times that “yes” was selected in the loco-check was significantly correlated with thigh muscle mass, major measures of physical performance, nutritional status, and QOL. This number was also significantly larger in the participants experiencing falling, fracture, and lumbar pain than in those without these episodes. [Conclusion] These results suggest that the loco-check might be useful for quantitatively evaluating LS.
Keywords: Locomotive syndrome, Loco-check, Quantitative evaluation of frailty
INTRODUCTION
The number of people aged 65 and over has been increasing for the past 20 years in Japan, and the pace of aging is the highest among other countries in the world1). Many older people are suffering from musculoskeletal disorders for which they are likely to soon require care services. Locomotive syndrome (LS), which is caused by functional deterioration of the musculoskeletal system, was proposed by the Japanese Orthopedic Association in 2007 to prevent the progression of frailty, reduce nursing care needs, and prolong healthy life expectancy2, 3). The prevalence of the LS increases with aging and has reached 50% in men and 70% in women over the age of 80 years old in the Japanese general population4).
LS is screened by the loco-check3), which consists of a 7-item questionnaire to assess locomotive disability based on the activities of daily living (ADL). The examinee is suspected to have LS if at least one of the items in the loco-check is positive. However, the loco-check has not yet been fully validated, and the association between the loco-check and individual physical function, nutritional status, and QOL remains to be explored. Recently, a quantitative diagnostic tool for LS, the 25-question Geriatric Locomotive Function Scale (GLF-25), was developed to evaluate the extent of LS, and its validity and reliability have been confirmed5). However, the GLF-25 is complex and time-consuming, and it is difficult for elderly people to precisely complete all questions.
Six out of the 7 items in the loco-check are included as the same or similar questions in the GLF-25. Thus, the loco-check may be considered as a shortened version of the GLF-25. If the number of items with an answer of “yes” on the loco-check can be evaluated quantitatively, the screening and staging of LS can be sometime easily carried out. A previous study has shown that a larger number of items with an answer of “yes” on the loco-check was significantly associated with reduced health-related quality of life (HRQoL) assessed by the EuroQoL-5 dimensions (EQ-5D) and EuroQoL-visual analog scale (EQ-VAS)6). Furthermore, the number of times that “yes” was selected on the loco-check has been found to be significantly correlated with the experience of falling in the previous year7).
The present study was conducted to clarify the association between the results of loco-check and physical function, muscle volume, nutritional status, or the physical factor of the 36-item Short-Form Health Survey (SF-36) in community dwelling older Japanese females.
SUBJECTS AND METHODS
Participants, who were older than 60 years of age, could independently read and answer questionnaires, and assented to our projects, were recruited from outpatients in a local hospital (Shizuoka, Japan). Exclusion criteria were as follows: individuals who were unable to walk without assistance; those who had systemic neuromuscular diseases, acute infection, cancer, severe cardiovascular diseases, pulmonary failure, and renal failure; those who had mental illness; those who could not take food by mouth. A final total of 20 males and 71 females participated in this study. However, the analysis was performed only in females (age 81.7 ± 8.0 yrs, range 64−96 yrs) because of the small number of males. Six out of these 71 females (8.5%) were receiving various home care services based on public Long-term Care Insurance (LTCI). Their care-needs levels included one patient requiring support level 1, two patients requiring support level 2, and three patients requiring care level 2 of 7 grade levels (support levels 1–2 and care levels 1–5). All procedures were performed in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of the University of Shizuoka (No. 21-22). All participants gave their informed consent to participate in this study.
The loco-check self-completed questionnaire consists of the following 7 statements: 1) You cannot put on a pair of socks while standing on one leg; 2) You stumble or slip in your house; 3) You need to use a handrail when going upstairs; 4) You cannot get across the road at a crossing before the traffic light changes; 5) You have difficulty walking continuously for 15 min; 6) You find it difficult to walk home carrying a shopping bag weighing about 2 kg; and 7) You find it difficult to do housework requiring physical strength3). Participants who check one or more statements are usually defined as having LS. Additionally, we calculated the cumulative number of times that “yes” was selected and investigated the association of this number with other variables in this study.
Weight and height were measured to calculate body mass index (BMI, kg/m2). Weight (kg) was measured with a portable digital scale, and height (m) was measured by a portable stadiometer. The maximal body weight throughout the entire lifetime was obtained from the history of each participant, and the percentage of weight reduction was calculated as follows.
Weight reduction (%)=(maximal body weight-current body weight)/maximal body weight ×100
A blood sample was taken at the regular health checkup, and serum albumin was measured.
The geriatric nutritional risk index (GNRI) is a very simple and objective method for screening the nutritional status of elderly individuals8). It can be calculated using a simple equation, in which only 3 nutritional variables, namely serum albumin, actual body weight, and ideal body weight (IBW), are used. The IBW was determined to be IBW (kg)=22 (kg/m2) × height (m)2. We used the following GNRI formula:
| GNRI = [1.489 × albumin (g/l)] + [41.7 × (weight/IBW)] |
In this formula, the weight/IBW was set to 1, when the weight exceeded the IBW. From these GNRI values, 4 grades of nutritional level were defined in the present study as the same as in the original classification: level 1, no risk of malnutrition (GNRI, >98); level 2, low risk of malnutrition (GNRI, 92 to ≤98); level 3, moderate risk of malnutrition (GNRI, 82 to <92); level 4, major risk of malnutrition (GNRI, <82).
Intake of all food, drinks, and dietary supplements were recorded for 3 days by participants or their relatives. Assessment days were consecutive and concurrent with physical activity measurement. Participants recorded all of the food and drinks they consumed, and estimated the portion size of each item. Portion weights were then approximated by a registered dietitian. The data were transferred into a nutrient calculation program, Excel Eiyo-kun version 6.0 (Kenpaku-sha, Tokyo, Japan), which is based on the Japanese Food Composition Database 2010 (Ministry of Education, Culture, Sports, Science, and Technology, Tokyo, Japan). The average intake of energy and protein for each participant was also calculated.
An axial CT image of the thigh was obtained at the midpoint of a line extending from the superior border of the patella to the greater trochanter of the femur. Each patient was examined in the supine position with the thigh muscles relaxed. The slice thickness was 10 mm. The radiographic image was digitally scanned for analysis by a personal computer. The whole thigh area (TA), adipose-tissue-free thigh muscle area (TMA), and thigh subcutaneous fat area (TSFA) were quantified using Image-J, a public-domain planimetry program (developed by Wayne Rasband, US National Institutes of Health). The ratio of TMA divided by height was used as the thigh muscle mass index, which was independent of body size9).
Maximal hand grip strength, maximal knee extensor strength, 10-meter maximum walking speed, timed up-and-go and one-leg standing time with eyes open were assessed for examining physical performance functions. Maximal hand grip strength was measured with the Smedley handgrip dynamometer (Hata Sporting Goods, Osaka, Japan). The larger value of two trials with the preferred hand was used for analysis. Maximal knee extensor strength was determined by a dynamometer (Molten, Hiroshima, Japan) fixed to the rigid leg of a bench. The subject sat on the bench in a vertical position with the knee bent at 90°, and a shin pad connected to the dynamometer was worn on the dominant lower leg. Three-second maximal isometric knee extension strength was measured. Each subject performed twice, and the larger value was used for analysis. Ten-meter maximal walking speed was measured once on a 10-m straight walking course. Timed up-and-go was the time taken by the subject to rise from a chair, walk a distance of 3 m, turn around, walk back to the chair, and sit down10). Each subject performed the test twice, and the shorter value was used for analysis. One-leg standing time with eyes open was measured to examine the static balance function11). The subject looked straight ahead at a dot 1 m in front of them and stood on the preferred leg with their eyes open and hands down alongside the trunk. The time until the raised leg was put down on the floor (or a maximum of 30 seconds) was recorded. The longer value of two trials was used in the analysis. Some participants could not complete all of the physical performance examinations. The number of participants who completed each physical examination is shown in Fig. 1.
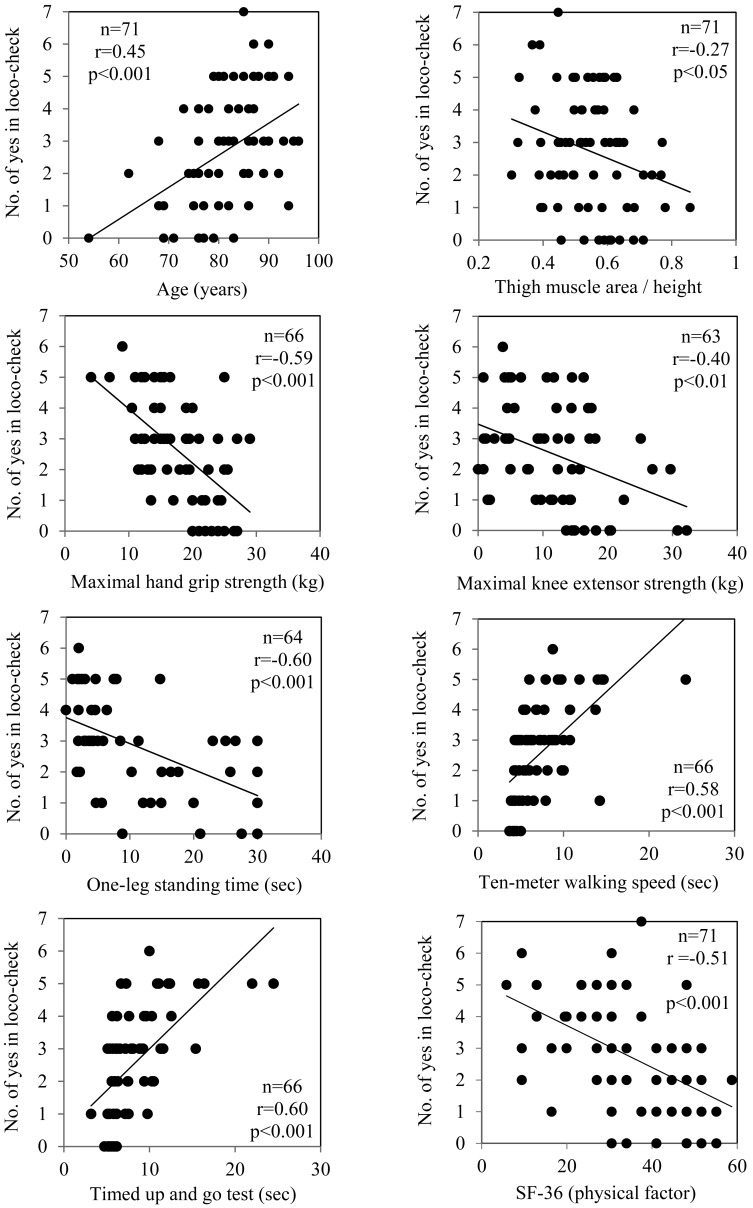
Fig. 1.
Associations between the number of “yes” for the loco-check and age, thigh muscle area, physical functions or SF-36 (physical factor) in older Japanese females
HRQoL was assessed using the SF-36 Health Survey ver. 2 (Medical Outcome Trust, Quality Metric, Kyoto, Japan)12). This is a reliable and valid generic health questionnaire that includes 36 questions to measure 8 categories of HRQoL: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health13). The HRQoL was assessed on a 4-week recall. Each category is scored 1–100, with higher scores indicating better QOL in each category. A transformation to norm-based scoring (NBS) was performed to compare each scale to the values of the normal population irrespective of gender and age dependent differences.
A fall was defined as “an unintentional change in position resulting in coming to rest at a lower level or on the ground”14). The number of falls within 2 years, the experience of fractures after the age of 65 years, or the presence of continuous lumbar pain or knee pain for more than 3 months were recorded. The association between experiences of these symptoms and loco-check was investigated.
Each variable was presented as mean ± SD. Differences between groups were determined by Student’s t-test. Simple or multiple regression analysis was performed to examine the association between the number of “yes” answers on the loco-check and age, nutritional status, physical function, or HRQoL. The multiple regression analysis was performed with the forward stepwise method to determine the final model. A p-value of less than 0.05 was considered statistically significant. All statistical analyses were performed by JMP ver. 6 software (SAS Institute, Tokyo, Japan).
RESULTS
Characteristics of the participants are shown in Table 1. While more than half of the participants were older than 80 years, nutritional indices such as BMI, serum albumin, GNRI, dietary energy intake, and protein intake were almost average values in elderly Japanese individuals with similar ages. The values of the hand grip strength, 10-meter maximum walking speed, timed up-and-go, and one-leg standing time with eyes open tests in our participants were similar to the values in Japanese females with LS reported in the previous study15). The number of participants who answered “yes” for each statement in the loco-check is shown in Table 2. Sixty two-subjects (87.3%) out of 71 participants answered “yes” to at least 1 item of the loco-check questionnaire, and thus, these participants were classified into LS. The number of times that “yes” was chosen in the loco-check was principally distributed around 1 to 5 in these participants (Table 3), and it is significantly correlated with age (Fig. 1).
Table 1. Participant characteristics.
| Variables | Mean ± SD | |||
|---|---|---|---|---|
| Age (years) | 81.7 ± 8.0 | |||
| Height (cm) | 147.4 ± 6.5 | |||
| Weight (kg) | 45.8 ± 9.2 | |||
| Body mass index (kg/m2) | 21.0 ± 3.5 | |||
| Weight reduction (%) | 14.0 ± 9.9 | |||
| Serum albumin (g/dl) | 4.0 ± 0.3 | |||
| GNRI | 97.9 ± 6.5 | |||
| X-ray computed tomography | ||||
| Thigh | ||||
| Whole area (cm2) | 142.0 ± 38.3 | |||
| Muscle area (cm2) | 81.1 ± 19.0 | |||
| Subcutaneous fat area (cm2) | 47.8 ± 22.5 | |||
| Muscle area/height | 0.55 ± 0.12 | |||
| Physical function | ||||
| Hand grip strength (kg) | 17.9 ± 5.5 | |||
| Knee extensor strength (kg) | 11.6 ± 7.7 | |||
| Ten-meter maximum walking speed (sec) | 7.3 ± 3.6 | |||
| Timed up-and-go (sec) | 8.3 ± 3.9 | |||
| One-leg standing time with eyes open (sec) | 16.1 ± 11.5 | |||
| SF-36v2 scores (NBS) | ||||
| Physical function | 34.9 ± 13.6 | |||
| Role physical | 40.5 ± 14.9 | |||
| Bodily pain | 45.8 ± 9.5 | |||
| General health perception | 45.7 ± 9.5 | |||
| Vitality | 48.9 ± 9.7 | |||
| Social function | 48.9 ± 11.9 | |||
| Role emotional | 42.9 ± 15.4 | |||
| Mental health | 50.7 ± 10.7 | |||
| Dietary intake | ||||
| Energy | (kcal/day) | 1,486 ± 249 | ||
| (kcal/kg/day) | 33.6 ± 7.9 | |||
| Protein | (g/day) | 61.3 ± 11.8 | ||
| (g/kg/day) | 1.38 ± 0.33 | |||
| Loco-check (number of “yes”) | 2.7 ± 1.7 | |||
GNRI: geriatric nutritional risk index; NBS: norm-based scoring
Table 2. The number of participants who answered “yes” for each statement in the loco-check.
| Statements in the loco-check | Number of participants, n (%) |
|---|---|
| You cannot put on a pair of socks while standing on one leg | 54 (76.1) |
| You stumble or slip in your house | 30 (43.7) |
| You need to use a handrail when going upstairs | 65 (91.5) |
| You cannot get across the road at a crossing before the traffic light changes | 16 (22.5) |
| You have difficulty walking continuously for 15 min | 22 (40.0) |
| You find it difficult to walk home carrying a shopping bag weighing about 2 kg | 43 (60.6) |
| You find it difficult to do housework requiring physical strength | 41 (57.7) |
Table 3. Distribution of the number of participants with various number of “yes” answers in the loco-check.
| Number of “yes” answers in the loco-check |
Number of participants n (%) |
|---|---|
| 0 | 9 (12.7) |
| 1 | 10 (14.1) |
| 2 | 12 (16.9) |
| 3 | 18 (25.3) |
| 4 | 8 (11.3) |
| 5 | 11 (15.5) |
| 6 | 2 (2.8) |
| 7 | 1 (1.4) |
The number of “yes” answers in the loco-check was significantly associated with the thigh muscle mass and physical performance measured with the hand grip strength, maximal knee extensor strength, one-leg standing time with eyes open, 10-m maximum walking speed, and timed up-and–go test in the simple regression analysis (Fig. 1). Furthermore, the number of times that “yes” was selected in the loco-check showed a significant negative correlation with SF-36 physical factor.
The number of “yes” answers in the loco-check was also significantly associated with various nutritional indices, namely weight reduction, serum albumin and GNRI, dietary energy, and protein intakes (Table 4).
Table 4. Association between the number of “yes” in loco-check and nutritional indices or dietary intake.
| Nutritional or dietary variables | r | ||
|---|---|---|---|
| Body mass index | –0.15 | ||
| Weight reduction | 0.32** | ||
| Serum albumin | –0.41** | ||
| GNRI | –0.41** | ||
| Dietary intake | |||
| Energy | (kcal) | –0.28* | |
| (kcal/kg) | –0.16 | ||
| Protein | (g) | –0.33** | |
| (g/kg) | –0.19 | ||
*p<0.05, **p<0.01. GNRI: geriatric nutritional risk index
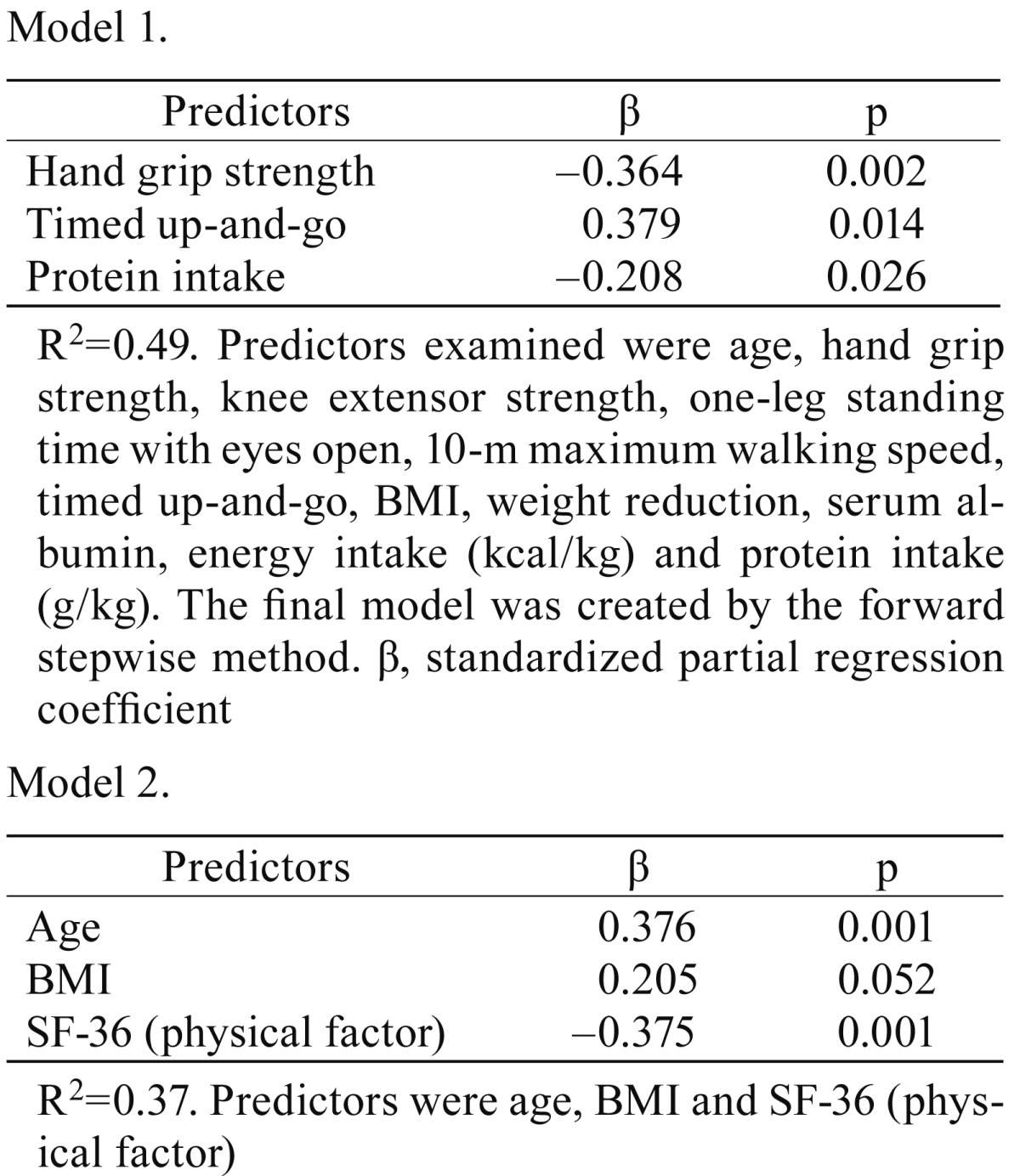
Since many measures of physical performance and nutritional indices were significantly correlated with the number of “yes” answers in the loco-check in the simple regression analysis, we tried to determine which were important LS predictors using multiple regression analysis. The potential predictors of higher numbers of “yes” answers in the loco-check were chosen as follows: age, hand grip strength, knee extensor strength, one-leg standing time with eyes open, 10-m maximum walking speed, timed up-and-go, BMI, weight reduction, serum albumin, energy intake (kcal/kg), and protein intake (g/kg). The final model, which consisted of hand grip strength, timed up-and-go, and protein intake, was created by the forward stepwise multiple regression analysis (Table 5 ). The final model revealed that these three factors were significantly associated with the number of “yes” answers in the loco-check. Furthermore, since the EuroQol was reported to be associated with the loco-check in the previous study6), we also examined the association between the physical factor in SF-36 and the number of “yes” answers in the loco-check by the multiple regression analysis. The result showed that the age and the physical factor in SF-36 independently correlated with the number of “yes” answers in the loco-check.
Table 5. Multiple regression analysis for the number of “yes” answers in the loco-check.
Finally, the number of “yes” answers in the loco-check was compared between participants with and without histories of falling and fracture and the symptoms of lumbar and knee pain. The number of “yes” answers in the loco-check was significantly larger in the participants who have experienced falling, fracture, and lumbar pain than in those without these experiences (Table 6).
Table 6. The number of “yes” answers in the loco-check in participants with or without falling, fracture, lumber pain and knee pain.
| Number of “yes” (mean ± SD) | p | ||
|---|---|---|---|
| With | Without | ||
| Falling | 3.6 ± 1.2 (n=11) | 2.5 ± 1.8 (n=59) | 0.05 |
| Fracture | 3.6 ± 1.1 (n=19) | 2.4 ± 1.8 (n=51) | <0.01 |
| Lumbar pain | 3.5 ± 1.6 (n=25) | 2.3 ± 1.7 (n=45) | <0.01 |
| Knee pain | 3.3 ± 1.7 (n=17) | 2.5 ± 1.7 (n=53) | NS |
One participant did not answer the question for these incidences and symptoms.
DISCUSSION
Preventive and therapeutic strategies against weakness in older people have attracted attention for prolonging their healthy life in the aging society. New concepts such as sarcopenia, frailty, and LS have been developed in the past two decades to represent the condition of weakness in the elderly. Among them, LS is particularly defined as moving ability disorders due to functional disturbances of locomotive organs such as bones, joints, nerves and muscles3).
Early detection and assessment of LS is essential for preventing and treating LS. Two screening tools, the loco-check and the GLFS-25, have been developed since the concept of LS was established in Japan. The loco-check was developed as a self-assessment checklist of LS in 2007. By the original criteria, an individual answering in the affirmative to one or more items of the 7 statements in this checklist is considered to have LS. However, this checklist has not yet been quantitatively validated as a reliable questionnaire, while the GLFS-25 has been shown to be a valid and reliable tool for evaluating the progression of LS.
The present study demonstrated that the number of “yes” answers in the loco-check was significantly associated with muscle mass, the physical performance evaluated by the hand grip strength, maximal knee extensor strength, one-leg standing time with eyes open, 10-m maximum walking speed, and timed up-and-go test, and the SF-36 physical factor. The multiple regression analysis confirmed that the hand grip strength, the timed up-and-go test, and the SF-36 physical factor were significant predictors for the number of “yes” answers in the loco-check. These results suggested that the loco-check might be useful for quantitatively evaluating LS. Such an approach is in line with previous studies. For example, Iizuka et al. showed by simple and multiple regression analyses that age, gender and EQ-5D utility value or EQ-VAS scores were independently correlated with the number of items with a “yes” answer on the loco-check in 442 community bound Japanese individuals, with age 66.1 ± 10.9 years6). Akahane et al. also showed by a logistic regression analysis that persons with larger number of “yes” answers in the loco-check appeared to be at higher risk for falling in 624 persons aged between 30 and 90 years7). Furthermore, a recent study demonstrated that the loco-check was statistically associated with GLF-25; the Spearman’s rank coefficient between them was r=0.452, and the receiver operating characteristic (ROC) curve analysis between them revealed that the area under the curve (AUC) was 0.81816).
While most physical function tests performed in the present study were significantly correlated with the number of “yes” answers in the loco-check by the simple regression analysis, only 2 physical function tests, the hand grip strength and the timed up-and-go test, were found to be significant by the multiple regression analysis. This may be because other physical function tests had similar trends to either of these 2 positive tests; for example, the result of the 10-m walking speed test was similar to the result of the timed up-and-go test in these participants.
It is noteworthy that the number of “yes” answers in the loco-check was also significantly associated with nutritional and dietary variables, including weight reduction, serum albumin, GNRI, energy intake, and protein intake. The protein intake was confirmed to be an independent predictor for loco-check in the multiple regression analysis. This association is similar to the finding that frailty was associated with malnutrition17, 18). However, BMI was not an independent predictor of LS in this study. Although the exact reason for this phenomenon remains unknown, it may be due to the presence of sarcopenic obesity in some participants19).
The participants who had histories of falling, fracture, or low back pain had a higher number of “yes” answers in the loco-check than those without these histories. This result strengthened our hypothesis that the loco-check can be quantitatively assessed.
LS is very common in elderly females over 80 years of age. Actually, the 87.3% of participants diagnosed with LS in the present study was similar to the result of a larger study conducted in Japan3). For such population, it seems more important to evaluate the severity or progression of LS than to screen and detect individuals with LS to provide appropriate care services. Compared with GLF-25, the loco-check is a simpler tool for evaluating the severity of LS, and thus can be easily applied to elderly at the home-care setting. The number of participants who answered “yes” to each statement in the loco-check ranged from 22.5% to 91.5% (Table 2), suggesting that they encountered varying levels of difficulty when performing each of the seven tasks described in the loco-check questionnaire. The loco-check results may be more useful if the number of “yes” responses is similar across all seven questionnaires.
There are some limitations in this study. First, the sample size was small, and thus, our results have a limited external validity. However, the association between the number of “yes” answers in the loco-check and physical performance was definite in this study. Second, since the number of participants with LS reached 87.3% in all participants in this study group, the difference between LS and non LS could not be compared. Third, since so few males participated in the present study, the analysis was carried out using females only. Ideally, a similar study might be carried out on males to confirm the validity of the present study.
In conclusion, the loco-check seems to be useful for quantitatively assessing the severity of LS in the elderly. Further studies are necessary to evaluate the association between the number of “yes” answers in the loco-check and the outcome of participants to establish the value of the loco-check.
REFERENCES
- 1.Government of Japan: Cabinet office. Annual report on the aging society FY 2014. http://www8.cao.go.jp/kourei/english/annualreport/2014/2014pdf_e.html
- 2.Nakamura K: A “super-aged” society and the “locomotive syndrome”. J Orthop Sci, 2008, 13: 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakamura K: The concept and treatment of locomotive syndrome: its acceptance and spread in Japan. J Orthop Sci, 2011, 16: 489–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sasaki E, Ishibashi Y, Tsuda E, et al. : Evaluation of locomotive disability using loco-check: a cross-sectional study in the Japanese general population. J Orthop Sci, 2013, 18: 121–129. [DOI] [PubMed] [Google Scholar]
- 5.Seichi A, Hoshino Y, Doi T, et al. : Development of a screening tool for risk of locomotive syndrome in the elderly: the 25-question Geriatric Locomotive Function Scale. J Orthop Sci, 2012, 17: 163–172. [DOI] [PubMed] [Google Scholar]
- 6.Iizuka Y, Iizuka H, Mieda T, et al. : Association between “loco-check” and EuroQol, a comprehensive instrument for assessing health-related quality of life: a study of the Japanese general population. J Orthop Sci, 2014, 19: 786–791. [DOI] [PubMed] [Google Scholar]
- 7.Akahane M, Maeyashiki A, Yoshihara S, et al. : Relationship between difficulties in daily activities and falling: loco-check as a self-assessment of fall risk. Interact J Med Res, 2016, 5: e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouillanne O, Morineau G, Dupont C, et al. : Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr, 2005, 82: 777–783. [DOI] [PubMed] [Google Scholar]
- 9.Abrahamsen B, Hansen TB, Høgsberg IM, et al. : Impact of hemodialysis on dual X-ray absorptiometry, bioelectrical impedance measurements, and anthropometry. Am J Clin Nutr, 1996, 63: 80–86. [DOI] [PubMed] [Google Scholar]
- 10.Podsiadlo D, Richardson S: The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc, 1991, 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 11.Bohannon RW, Larkin PA, Cook AC, et al. : Decrease in timed balance test scores with aging. Phys Ther, 1984, 64: 1067–1070. [DOI] [PubMed] [Google Scholar]
- 12.Fukuhara S, Bito S, Green J, et al. : Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol, 1998, 51: 1037–1044. [DOI] [PubMed] [Google Scholar]
- 13.Hawthorne G, Osborne RH, Taylor A, et al. : The SF36 Version 2: critical analyses of population weights, scoring algorithms and population norms. Qual Life Res, 2007, 16: 661–673. [DOI] [PubMed] [Google Scholar]
- 14.The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull, 1987, 34: 1–24. [PubMed] [Google Scholar]
- 15.Muramoto A, Imagama S, Ito Z, et al. : Threshold values of physical performance tests for locomotive syndrome. J Orthop Sci, 2013, 18: 618–626. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y, Suehara Y, Ishii M, et al. : A comparative study of 2 screening tools for locomotive syndrome (The “Loco-check” and the “GLFS-25”): an orthopedic outpatient-based survey. Br J Med Med Res, 2016, 17: 1–13. [Google Scholar]
- 17.Boulos C, Salameh P, Barberger-Gateau P: Malnutrition and frailty in community dwelling older adults living in a rural setting. Clin Nutr, 2016, 35: 138–143. [DOI] [PubMed] [Google Scholar]
- 18.Dorner TE, Luger E, Tschinderle J, et al. : Association between nutritional status (MNA®-SF) and frailty (SHARE-FI) in acute hospitalised elderly patients. J Nutr Health Aging, 2014, 18: 264–269. [DOI] [PubMed] [Google Scholar]
- 19.Deutz NE, Bauer JM, Barazzoni R, et al. : Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr, 2014, 33: 929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]