Abstract
[Purpose] The aim was to evaluate the effect of therapeutic ultrasound on the pain, joint mobility, muscle strength, physical function, and quality of life of people with knee OA. [Subjects and Methods] One-site, one-arm, before-after study that included people with Grade II or III tibiofemoral osteoarthritis. Ten therapeutic ultrasound sessions (duty cycle=20%, ERA=10 cm2, BNR=6:1, SATP=2.2 W/cm2, SATA=0.44 W/cm2, frequency=1 MHz, time=4 minutes) were applied. Assessments of primary outcome variables: pain intensity and function, and secondary variables: joint mobility, muscle strength and quality of life, were performed at onset and end of therapy; an additional intermediate evaluation was included for the primary variables. [Results] Means of repeated measurements of pain intensity (pain at rest, pain on palpation and pain after functional activities) and function showed significant differences. There was a significant reduction in pain intensity at the end of functional activities as well as a significant increase in function and in quadriceps muscle strength. [Conclusion] Therapeutic ultrasound applied in accordance with the parameters used, could be recommended during the treatment of individuals with knee osteoarthritis, because it significantly decreased the intensity of pain after the 5th session, and this reduction was maintained until the end of the intervention.
Keywords: Pain, Ultrasound therapy, Muscle strength
INTRODUCTION
Osteoarthritis (OA) is a chronic and degenerative disorder, characterized by joint cartilage wear. Its main symptoms include pain and reduction of joint mobility and muscle strength. It is one of the conditions with the greatest impact on function and quality of life of the elderly in developed countries1).
In the United States of America (USA), OA affects 12.1% of the adult population, particularly females (RR=1.79)2). In Colombia, the Ministry of Social Protection reported that healthy life-years (HLY, an epidemiological indicator) lost prematurely due to disability and death were similar to HLY lost due to prostate and cervix cancer and leukemia3). The support joint with the highest incidence of OA is the knee with an incidence of 240 new cases per 100,000 person-years compared to hip OA with an incidence of 88 new cases per 100,000 person-years4).
Pain, the main symptom, is present in 38–68% of people with OA and it is associated with insomnia, depression and impairment of participation in social activities3). Moreover, pain has a negative impact on muscle strength and joint Range of Motion (ROM), favoring the progressive decline of function and therefore of the quality of life of these people3).
Therapeutic ultrasound (TUS) is one of the most-used physical modalities of physiotherapy for treatment of knee and hip OA5); however, its application has not shown conclusive effects due to methodological limitations such as small sample size, confounding biases and the lack of clarity about the application parameters, the way ultrasound is generated and the recommended dose for this pathology6).
Few studies7, 8) have been applied the TUS as the only modality of intervention and evaluated its short-term effects of TUS. These authors did not report significant differences in the variables evaluated possibly due to the application of continuous TUS and by methodological limitations such as selection bias, mainly. Regarding the use of pulsed TUS, only a controlled clinical trial included this form of generation in patients with knee OA. Huang et al.9) Reported a significant increase in the ROM of the knee, and decreased pain intensity, however, these authors did not evaluate the short-term effect of TUS.
Therefore, considering the high prevalence of OA in the elderly population and the daily use of TUS in clinical practice, the aim of the present study was to evaluate the effect of TUS applied to the medial and lateral compartments of the knee on pain intensity, joint ROM, muscle strength, function and quality of life of the participants. This study was proposed with the hypothesis that relief of pain might increase knee ROM and the strength of the quadriceps and ischiotibial muscles, and hence give rise to a positive change in the function and quality of life of the participants.
SUBJECTS AND METHODS
This A quasi-experimental study with pre and post-intervention analysis included a population of individuals (40–75 years old) with a diagnosis of grade II or III knee (tibiofemoral joint) OA, in accordance with the Kellgren-Lawrence radiographic grading scale, taking into account that in these degrees of severity the ultrasound could be effective9). The severity of disease was radiologically evaluated by an orthopedic knee specialist with 23 years of clinical experience.
Individuals were excluded from the study in accordance with the following criteria: if they had received an intra-articular injection of hyaluronic acid or corticoids during the six months prior to the study, or if they had a clinical history of orthopedic knee surgery, a skin disorder, acute-phase respiratory conditions, cardiovascular diseases, such as acute myocardial infarction, during the previous month, or uncontrolled arterial hypertension, or if they had been receiving another kind of physiotherapeutic treatment.
Sample size was calculated considering a power of 80%, a 20% adjustment for follow-up losses, and assuming a significance level of 5%. It was determined that a final sample size of 17 participants would be appropriate for establishing the proposed differences.
The project was approved by the Scientific Research Ethics Committee of the School of Health of Universidad Industrial de Santander with code 7083, and it was carried out in accordance with Good Clinical Practice rules and the Ethics Principles for Medical Research Involving Human Beings that are defined in the latest revision of the Declaration of Helsinki. Written informed consent was obtained from all participants prior to the study.
The number of therapeutic ultrasound sessions (0, 5 or 10) was the explanatory variable of this study. Accordingly, the phases of the evaluation process were defined as initial: at the onset (baseline) of trial (T0); intermediate: at the end of the fifth session (T1); and final: a day after the tenth session of therapeutic ultrasound (T2).
The primary outcome variables were function, intensity of pain at rest (PAR), intensity of pain on palpation (POP), and intensity of pain at the end of a functional activity, specifically the Six-Minute Walk Test (6MWT). This variables were assessed in the T0, T1 and T2 phases. The secondary outcome variables were joint mobility, muscle strength and quality of life of the participants, which were evaluated in the T0 and T2 phases.
Anthropometric and socio-demographic variables, analgesic ingestion, type of analgesic used, level of physical activity, unilateral or bilateral OA, and disease severity score were considered as covariates in the present study.
Before the first session, participants were involved in a process to familiarize them with the instruments and the evaluation tests. During the first session, the initial baseline (T0) assessment was made in the following sequence: First, completion of self-reporting instruments for measuring quality of life (Outcome Osteoathritis Knee Hip Quality of Life/OOAKHQOL10), PAR, and POP). Then, evaluation of knee flexion and extension ROM, quadriceps and ischiotibial muscles strengths, and performance of the 6MWT were measured. Immediately after the initial evaluation, the first TUS session was applied.
With the aim of ensuring the precision of the measurements, all the instruments and tests used for evaluation were subjected to intra-evaluator and test-retest reproducibility analyses during a previous pilot trial. The intraclass correlation coefficients (ICC) were between 0.93 and 0.97 for intra-evaluator reproducibility of goniometry and hand-held dynamometry, and between 0.82 and 0.97 for a good test-retest reproducibility of the Visual Analogue Scale (VAS), the 6MWT, and the OOAKHQOL instrument.
PAR, POP and intensity of pain after the 6MWT were evaluated using a VAS. This instrument consists of a continuous horizontal line with endpoints labeled with verbal descriptors for defining the limits of the painfulness experience, from “no pain” to “the worst pain experienced,” respectively11). Participants were asked to mark with an X the point that represented the intensity of the pain they had on the day of the test.
POP was evaluated after palpation in the medial region (insertion of the pes anserinus/goose’s foot tendon), lateral region (femoral condyle, over the insertion of the fascia lata), antero-inferior region (tibial tuberosity, over the insertion of the quadriceps tendon), and posterior region (popliteal fossa) of the knee. Intensity of pain after the 6MWT was assessed immediately after the 6MWT had been performed.
Knee flexion-extension ROM was evaluated with a universal plastic 0–180° goniometer with two 30-cm long arms (Int Standar Goniometer. SEC, Company Orthopaedic Ltd.), in accordance with the recommendations of Norkin and White12). This measurement was made twice and the greater value was recorded as the joint ROM and was measured at intervals of 1 or 5 degrees.
Quadricep and ischiotibial muscle strength was measured in pounds (lb) using a manual dynamometer (Microfet 2 model, Hoggan Health Industries Inc.), following the manufacturer’s instructions and the recommendations of Kendall and Kendall13). Three measurements were taken at 1-minute intervals, and their average was recorded as the muscle strength.
Function was assessed using the 6MWT following the protocol proposed by the American Thoracic Society14) This test has been used to measure functional state in the elderly15). The test was conducted in a 30-meter-long flat and straight indoor hallway which was marked with tape at the start and finish lines and every three meters to facilitate the measure of the distance covered by the individual. The time was controlled using a digital chronometer, and at the end of the test the number of meters walked was recorded.
The information was recorded by a physical therapist with six years of clinical experience who is a candidate for a Master’s degree in Physiotherapy.
Quality of life was evaluated by applying the OOAKHQOL, an instrument specifically used for hip and knee OA. This is comprised of 43 items, 40 of which evaluate five attributes: physical activity, mental health, pain, social support, and social activities −and three of which evaluate independent attributes. The scoring of the instrument gives five results, one for each attribute on a scale from 0 (the worst quality of life) to 100 (the best quality of life)10).
The intermediate (T1) evaluation was performed on the sixth day of treatment, before application of TUS, and included PAR, POP, intensity of pain after the 6MWT, and function. The final evaluation (T2) was performed on the day after the 10th session of treatment and included all variables of the study, as previously described.
The procedures for evaluation of the variables in every participant were carried out at the same time of day, to avoid variations due to circadian rhythm. All of the measurements were made by a physical therapist with 10 years of experience in the musculoskeletal area who is a candidate for a Master’s degree in Physiotherapy
The body region to be treated was marked out with a 4-cm wide × 8-cm long template, twice as large as the head of the TUS equipment. The center of the template was placed over the inter-articular line, between the distal end of the femur and the proximal end of the tibia. This template was used during the intervention sessions for all participants.
The therapeutic ultrasound equipment (Sonicator® 730 model, Mettler Electronics,) was calibrated in accordance with IEC (International Electrotechnical Commission) Standard 6116, before using it in the study. The following were the parameters used for treatment: pulsed ultrasound with a duty cycle=20%, ERA=10 cm2, BNR=6:1, SATP intensity=2.2 W/cm2, frequency=1 MHz, time=4 minutes and SATA=0.44 W/cm2. The target body area was twice the ERA of the ultrasound equipment head, and was marked out on the medial and lateral compartments of the knee. In accordance with those parameters, energy of 1,056 J was applied to the medial and lateral compartments of the knee, in each session.
The treatment consisted of 10 sessions—one session a day, five days a week, for two weeks. During the application of therapeutic ultrasound, participants were in a supine position. A 10 cm3 topical gel without any active pharmacological component was used as a coupling medium. Therapeutic ultrasound was applied with longitudinal movements at the speed set by a metronome operating at 40 bits per minute.
The distributions of outcome variables were evaluated in rating scales using the Shapiro-Wilk test. TUS induced changes in intensity of pain and function were compared between the baseline and the 5th and 10th sessions (T0, T1 and T2) by repeated measures ANOVA. Outcome variables between the starting and the finishing phases were compared using the Student’s paired t test, except for intensity of pain after the 6MWT, joint mobility at extension and function, which were evaluated with the Wilcoxon rank test because of their non-parametric distribution.
Bland-Altman agreement limits and their respective confidence intervals (CI) were calculated for every variable of interest to establish the cut-off points for significance of changes attributable to the intervention and not to variance of measurements. The higher value of the upper CI for the Bland-Altman agreement limit was chosen as cut-off point for those variables expected to decrease after treatment, such as PAR, POP and intensity of pain after the 6MWT. The lower value of the lower CI for the Bland-Altman agreement limit was chosen as cut-off point for those variables expected to increase after treatment, such as joint mobility, muscle strength, function and quality of life (Table 1).
Table 1. Cut-off points of outcome variables of the study.
| Variable | Cut-off point | |
|---|---|---|
| VAS (mm) | Rest | 26.7 |
| Palpation | 38.4 | |
| End of functional activities | 17.0 | |
| ROM (°) | Flexion | 30.5 |
| Extension | 7.6 | |
| Muscle strength (lb) | Quadriceps | 5.2 |
| Ischiotibials | 6.2 | |
| 6WMT (m) | 16.1 | |
| OOAKHQOL (0–100) | Physical activity | 21.7 |
| Pain | 27.2 | |
| Mental health status | 28.4 | |
| Social support | 44.7 | |
| Social activities | 73.5 | |
VAS: Visual Analogue Scale; ROM: Range of Motion; 6WMT: Six-Minute Walk Test; OOAKHQOL: Osteoathritis Knee Hip Quality of Life; mm: millimeter; ° degrees Celsius; lb: pound; m: meter
The database was prepared in duplicate using Microsoft Excel (2013). The validation of the database and analysis of information were carried out with Stata 12 software (StataCorp. 2011. Stata: Release 12. Statistical Software. The College Station, TX: StataCorp LP) at a significance level of α=0.05.
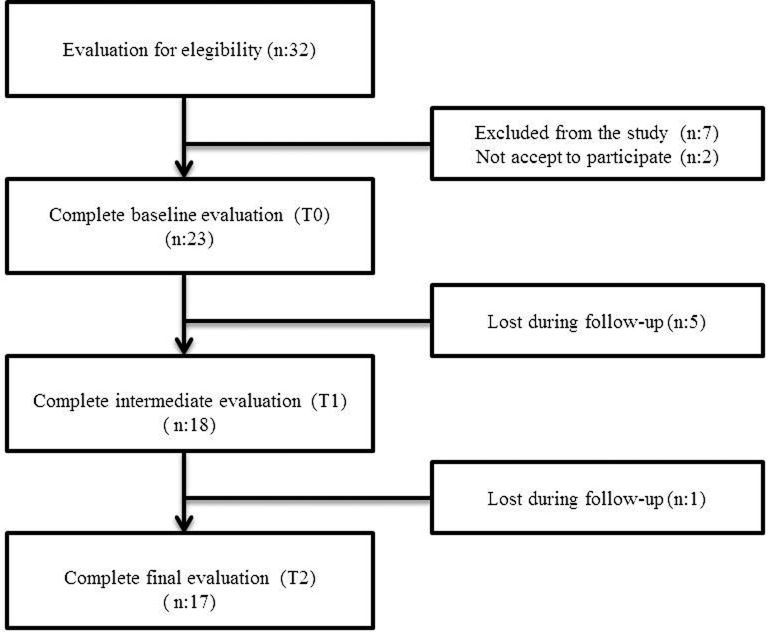
The present study included 17 participants, (Fig. 1), 70.5% females; mean age: 61.4 ± 6 years. Four individuals had unilateral knee OA, and thirteen had bilateral knee OA. Only the most compromised knee was included in the analysis of individuals with bilateral knee OA
Fig. 1.
Flow chart of participants through the phases of the study
RESULTS
The main characteristics of participants at the onset of the study are shown in Table 2.
Table 2. Features of participants at baseline.
| Feature | Total (%) n=17(100) | |
|---|---|---|
| Sociodemographic | Gender | |
| Male | 5 (29.4) | |
| Female | 12 (70.5) | |
| Average age | 61.4 ± 6* | |
| Socioeconomic status | Low 2–3 | 9 (47) |
| Medium/High 4–5 | 8 (52.9) | |
| Schooling | Primary | 6 (35.2) |
| Secondary | 4 (23.5) | |
| Technical/ University | 7 (41.1) | |
| Anthropometric | BMI | |
| Not overweight (BMI 25) | 2 (11.7) | |
| Overweight (BM >25 and ˂30) | 6 (35.2) | |
| Obesity (BM >30) | 9 (52.9) | |
| Dominant extremity | Right | 14 (82.3) |
| Left | 3 (17.6) | |
| Involvement | Unilateral | 4 (23.5) |
| Bilateral | 13 (76.4) | |
| Ingestion of analgesics | Yes | 11 (64.8) |
| No | 6 (35.2) | |
| Type of analgesics | NSAIDs | 5 (29.4) |
| Non-NSAIDs | 2 (11.7) | |
| Opioids | 0 | |
| Other | 4 (23.5) | |
| None | 6 (35.2) | |
| Level of physical activity (%) | Low | 6 (35.2) |
| Moderate | 6 (35.2) | |
| Vigorous | 5 (29.4) | |
| Severity of OA | Grade ll | 11 (64.7) |
| Grade lll | 6 (35.3) | |
| Patellofemoral OA | Present | 16 (94.1) |
| Absent | 1 (5.8) | |
*Median ± standard deviation (SD), BMI: body mass index; n: sample size
A significant decrease in PAR and POP, as well as improvement in function, were found at the three moments evaluated (p<0.03) (Table 3). Moreover, there was a significant decrease in intensity of pain after the 6MWT (p<0.01) and a notable increase in function when baseline and final evaluations were compared (p<0.01) (Table 4).
Table 3. Intensity of pain and function at three moments of evaluation (n=17).
| Variable | T0 | T1 | T2 | p** | |
|---|---|---|---|---|---|
| Intensity (mm) | Rest | 35.2 ± 25.5 | 16.8 ± 15.8 | 11.8 ± 9.7 | 0.03 |
| Palpation | 42.1 ± 28.7 | 18.5 ± 14.1 | 15.5 ± 12.3 | 0.004 | |
| End of functional activities | 43.6 ± 24.8 | 25.1 ± 15.9 | 22.5 ± 22.8 | 0.07 | |
| Function (m) | 436 ± 111.2 | 451 ± 77 | 490 ± 72.3 | 0.0001 | |
Median ± SD, mm: millimeters, ** Greinhouse
Table 4. Differences between outcome variables at baseline (T0) and the end (T2) of treatment (n=17).
| Variable | T0 | T2 | p | |
|---|---|---|---|---|
| Intensity of pain (mm) | Rest | 35.2 ± 25.5 | 11.8 ± 9.7 | 0.0006‡ |
| Palpation | 42.1 ± 28.7 | 15.5 ± 12.3 | 0.0005‡ | |
| After the 6MWT | 45 (25–67)* | 12 (10–34) | 0.006‡ | |
| Function (m) | 449.3 (422.5–465.3)* | 484.6 (473.1–512.3) | 0.008‡ | |
| Joint mobility (°) | Flexion | 132 ± 5.0 | 132 ± 6.1 | 0.6 |
| Extension | 130 (120–135) | 130 (125–135) | 0.1 | |
| Muscle strength (lb) | Quadriceps | 33 ± 10.2 | 38.3 ± 7.5 | 0.04‡ |
| Ischiotibials | 24 ± 5.3 | 25.5 ± 4.1 | 0.1 | |
| Quality of life | Physical activity | 47.4 ± 17.2 | 67.4 ± 19.0 | 0.0001 |
| Pain | 40.7 ± 24.4 | 67.4 ± 23.8 | 0.0001 | |
| Mental health status | 52.6 ± 21.3 | 71.3 ± 17.1 | 0.0001 | |
| Social support | 67.3 ± 19.7 | 67.3 ± 24.2 | 0.9 | |
Median ± SD; * Median (ranges 25–75%), mm: millimeters: m: meters, (°): grades, ‡Significant differences in accordance with cut-off points
No changes in joint mobility or quality of life of the participants were observed (p>0.05). Quadriceps muscle strength increased significantly based on the established cut-off points (Table 4).
DISCUSSION
This study was proposed with the hypothesis that relief of pain might increase knee ROM and the strength of the quadriceps and ischiotibial muscles, and hence give rise to a positive change in the function and quality of life of the participants. For this reason, the aim of the research was to evaluate the effect of therapeutic pulsed ultrasound on PAR, POP and intensity of pain after the 6MWT.
Five sessions of TUS, applied in accordance with the parameters described above, significantly decreased the intensity of pain, although there was no change in function. These results suggest that function may be influenced by other variables, such as muscle strength and joint mobility16), which were not evaluated at T1. Moreover, age-related comorbidities could bias the observed results.
The findings related to relief of pain were higher than those reported by Cakir et al.17) and Tascioglu et al18). They applied ten sessions of therapeutic pulsed ultrasound and found a clinical and statistically significant decrease in PAR and at movements of 28.8 mm and 24.3 mm, respectively. However, these authors evaluated the intensity of pain in accordance with a self-reporting form based on symptoms during the week previous to the evaluation. This might have biased the classification because previous experiences of pain may be associated with their emotional and cognitive aspects, thereby influencing the results19).
In contrast to the studies mentioned above, the present study evaluated pain immediately after finishing a functional activity, specifically the 6MWT. This is an appropriate evaluation taking into account that pain in people with knee OA could be exacerbated during weight-bearing activities such as walking20). This is a variable that should be considered when assessing the post-treatment outcomes in this population.
The post-treatment reduction of intensity of pain after the 6MWT, observed in this study, is likely related to a therapeutic effect of ultrasound on patellofemoral OA, given that the joint is quite near the lateral and medial sides of knee where ultrasound was applied20). Additional support for this hypothesis arises from the observation that patellofemoral OA was present in 94.1% of participants, and it is well known that it is a main source of pain in these persons20).
The decrease in POP could be influenced by the effect of TUS on soft tissues in the treated region. The knee zone targeted for treatment was comprised of the interarticular line, the tibiofemoral joint, and tissues such as the goose’s foot tendon, the iliotibial band and the collateral ligaments, all of which are tissues that tend to be inflamed and painful in people with knee OA. Because of their high collagen content, those tissues have a high ultrasound energy absorption coefficient21, 22).
The mechanisms by which TUS could be effective for decreasing pain in patients with knee OA are not well defined, but could be related to a decrease in function of the sodium/potassium pump in the pain conduction fibers23), an increase in membrane permeability which favors a higher vascularization of tissues that are being repaired24), and a decrease in nitric oxide synthase, which promotes inflammation and chronicity of pain25). However, these mechanisms were not evaluated in the present study. The assessment of these physiological mechanisms in vitro, and in vivo in animal models, is necessary.
With respect to joint mobility, flexion-extension of knee was in the range of 0–135° in the baseline of the study. This range is considered normal for the study population26), and was unlikely to improve.
Assessment of muscle strength showed significant differences in quadriceps strength at the end of the intervention. This result could be attributable to a reverse effect of TUS over the inhibited muscle. Published studies show that during chronic pathological joint processes, such as OA, the excitability of spinal and supraspinal reflex pathways is impaired, causing limitation in the activation of alpha motoneurons (α-MN) of the joint-related muscles; this, in turn, produces a continuous reflex inhibition of the muscle, known as arthrogenic muscle inhibition (AMI)27).
Hence, the application of TUS and the associated tissue micro-massage it produces28) potentially adjust the afferents of Pacinian mechanoreceptors and of free nervous terminations, reversing the inhibition of pathway Ib, facilitating the activation of α-MN and the recruitment of muscle fibers, thereby increasing muscle strength27). However, the reviewed literature does not contain any studies about the effects of TUS on AMI, and the variables assessed in the present study do not corroborate that hypothesis. Future studies could verify the effect of ultrasound on the activation of the quadriceps muscle through analysis of the H-Reflex and the central activation ratio.
Additionally, the firm contact between the skin and the device head, and its movement over the therapy-targeted zone might activate length-change-sensitive receptors located in the muscle. This in turn would increase the afferents of the Ia pathway, favoring the gamma-alpha stimulation which improves complete muscle activation27). Future random clinical trials could include a placebo group to verify the proposed mechanism.
The effect of TUS on quadriceps muscle strength has only been studied by Huang et al9). They analyzed this effect after application of a pulsed ultrasound protocol and found a significant increase in muscle strength. However, in that study, participants were subjected to a quadriceps muscle strengthening program together with the ultrasound intervention, so those results are not comparable to the ones observed in the present work.
The increased muscle strength after treatment, observed in this work, has clinical relevance, taking into account that a decrease in quadriceps muscle strength is considered to be a predictive factor of the progression of OA29), a risk factor for knee arthroplasty and a predictive factor of function after knee arthroplasty. The present results showed that participants had an average 0.25 kgf/kg gain in their quadriceps muscle strength at the end of the ultrasound intervention. This might denote a functional improvement and a lower risk of the need for a walking orthosis30). In the present study, the results of quadriceps muscle strength correspond to the functional improvement of the participants (Table 3).
No change was recorded in the quality of life at the end of therapeutic ultrasound intervention. This might be explained by the multidimensional nature of this variable and the difficulty of assessing the perception a person has of how each one of those dimensions impacts his/her life. For this reason, it is difficult to track the changes of those dimensions in response to ultrasound treatment, especially when only 10 sessions were applied to treat a disease that is chronic. It is likely that studies with a greater number of treatment sessions will produce significant changes in the quality of life of people with knee OA.
The results of this study indicate that therapeutic ultrasound applied in accordance with the parameters used, could be recommended during the treatment of individuals with knee OA, because it significantly decreased the PAR, POP and intensity of pain after the 6MWT, after the 5th session, and this reduction was maintained until the end of the intervention. Moreover, ten sessions of treatment notably increased quadriceps muscle strength, what could contribute to an increase in the function of the participants.
REFERENCES
- 1.Zhang W, Moskowitz RW, Nuki G, et al. : OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage, 2008, 16: 137–162. [DOI] [PubMed] [Google Scholar]
- 2.Holt HL, Katz JN, Reichmann WM, et al. : Forecasting the burden of advanced knee osteoarthritis over a 10-year period in a cohort of 60–64 year-old US adults. Osteoarthritis Cartilage, 2011, 19: 44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peñaloza RE, Salamanca N, Rodríguez JM, et al. : Estimación de la carga de enfermedad para Colombia, 2010, 1st ed. Bogotá: Editorial Pontificia Universidad Javeriana, 2014. [Google Scholar]
- 4.Arden N, Nevitt MC: Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol, 2006, 20: 3–25. [DOI] [PubMed] [Google Scholar]
- 5.Loyola-Sánchez A, Richardson J, MacIntyre NJ: Efficacy of ultrasound therapy for the management of knee osteoarthritis: a systematic review with meta-analysis. Osteoarthritis Cartilage, 2010, 18: 1117–1126. [DOI] [PubMed] [Google Scholar]
- 6.Jamtvedt G, Dahm KT, Christie A, et al. : Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews. Phys Ther, 2008, 88: 123–136. [DOI] [PubMed] [Google Scholar]
- 7.Ozgönenel L, Aytekin E, Durmuşoglu G: A double-blind trial of clinical effects of therapeutic ultrasound in knee osteoarthritis. Ultrasound Med Biol, 2009, 35: 44–49. [DOI] [PubMed] [Google Scholar]
- 8.Ulus Y, Tander B, Akyol Y, et al. : Therapeutic ultrasound versus sham ultrasound for the management of patients with knee osteoarthritis: a randomized double-blind controlled clinical study. Int J Rheum Dis, 2012, 15: 197–206. [DOI] [PubMed] [Google Scholar]
- 9.Huang MH, Yang RC, Lee CL, et al. : Preliminary results of integrated therapy for patients with knee osteoarthritis. Arthritis Rheum, 2005, 53: 812–820. [DOI] [PubMed] [Google Scholar]
- 10.Rat AC, Coste J, Pouchot J, et al. : OAKHQOL: a new instrument to measure quality of life in knee and hip osteoarthritis. J Clin Epidemiol, 2005, 58: 47–55. [DOI] [PubMed] [Google Scholar]
- 11.Gagliese L: Assesment of Pain in Elderly People. In: Turk D, Melzack R. Handbook of pain assessment, 2nd ed. New York, London: The Guilford Press, 2001, pp119–123. [Google Scholar]
- 12.Norkin C, White C: Measurement of joint motion: a guide to goniometry, 3rd ed. Philadelphia: F.A. Davis Company, 1995, p 237. [Google Scholar]
- 13.Kendall F, Kendall E, Geise P: Músculos, pruebas, funciones y dolor postural, 4th ed. Santiago de Chile: Mediterráneo, 2001, p 237. [Google Scholar]
- 14.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories: ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med, 2002, 166: 111–117. [DOI] [PubMed] [Google Scholar]
- 15.Bohannon RW, Bubela D, Magasi S, et al. : Comparison of walking performance over the first 2 minutes and the full 6 minutes of the Six-Minute Walk Test. BMC Res Notes, 2014, 7: 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rutherford D, Moreside J, Wong I: Knee joint motion and muscle activation patterns are altered during gait in individuals with moderate hip osteoarthritis compared to asymptomatic cohort. Clin Biomech (Bristol, Avon), 2015, 30: 578–584. [DOI] [PubMed] [Google Scholar]
- 17.Cakir S, Hepguler S, Ozturk C, et al. : Efficacy of therapeutic ultrasound for the management of knee osteoarthritis: a randomized, controlled, and double-blind study. Am J Phys Med Rehabil, 2014, 93: 405–412. [DOI] [PubMed] [Google Scholar]
- 18.Tascioglu F, Kuzgun S, Armagan O, et al. : Short-term effectiveness of ultrasound therapy in knee osteoarthritis. J Int Med Res, 2010, 38: 1233–1242. [DOI] [PubMed] [Google Scholar]
- 19.Sandkühler J, Lee J: How to erase memory traces of pain and fear. Trends Neurosci, 2013, 36: 343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arokoski J: Pain in hip and knee osteoarthritis. Pain Manag, 2014, 4: 177–180. [DOI] [PubMed] [Google Scholar]
- 21.Antich TJ, Randall CC, Westbrook RA, et al. : Physical therapy treatment of knee extensor mechanism disorders: comparison of four treatment modalities. J Orthop Sports Phys Ther, 1986, 8: 255–259. [DOI] [PubMed] [Google Scholar]
- 22.Rodríguez-Grande EI, Ramírez-Ramírez LC: Uso del ultrasonido terapéutico pulsado en el tratamiento de personas con osteoartritis de rodilla. Rev Univ Ind Santander Salud, 2015, 47: 337–348. [Google Scholar]
- 23.Binder A, Hodge G, Greenwood AM, et al. : Is therapeutic ultrasound effective in treating soft tissue lesions? Br Med J (Clin Res Ed), 1985, 290: 512–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rawool NM, Goldberg BB, Forsberg F, et al. : Power Doppler assessment of vascular changes during fracture treatment with low-intensity ultrasound. J Ultrasound Med, 2003, 22: 145–153. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh YL: Effects of ultrasound and diclofenac phonophoresis on inflammatory pain relief: suppression of inducible nitric oxide synthase in arthritic rats. Phys Ther, 2006, 86: 39–49. [DOI] [PubMed] [Google Scholar]
- 26.Walker JM, Sue D, Miles-Elkousy N, et al. : Active mobility of the extremities in older subjects. Phys Ther, 1984, 64: 919–923. [DOI] [PubMed] [Google Scholar]
- 27.Rice DA, McNair PJ: Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum, 2010, 40: 250–266. [DOI] [PubMed] [Google Scholar]
- 28.Baker KG, Robertson VJ, Duck FA: A review of therapeutic ultrasound: biophysical effects. Phys Ther, 2001, 81: 1351–1358. [PubMed] [Google Scholar]
- 29.Segal NA, Findlay C, Wang K, et al. : The longitudinal relationship between thigh muscle mass and the development of knee osteoarthritis. Osteoarthritis Cartilage, 2012, 20: 1534–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katoh M, Kaneko Y: An investigation into reliability of knee extension muscle strength measurements, and into the relationship between muscle strength and means of independent mobility in the ward: examinations of patients who underwent femoral neck fracture surgery. J Phys Ther Sci, 2014, 26: 15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]