Abstract
Outdoor time is considered to reduce the risk of developing myopia. The purpose is to evaluate the evidence for association between time outdoors and (1) risk of onset of myopia (incident/prevalent myopia); (2) risk of a myopic shift in refractive error and c) risk of progression in myopes only. A systematic review followed by a meta‐analysis and a dose–response analysis of relevant evidence from literature was conducted. PubMed, EMBASE and the Cochrane Library were searched for relevant papers. Of the 51 articles with relevant data, 25 were included in the meta‐analysis and dose–response analysis. Twenty‐three of the 25 articles involved children. Risk ratio (RR) for binary variables and weighted mean difference (WMD) for continuous variables were conducted. Mantel–Haenszel random‐effects model was used to pool the data for meta‐analysis. Statistical heterogeneity was assessed using the I 2 test with I 2 ≥ 50% considered to indicate high heterogeneity. Additionally, subgroup analyses (based on participant's age, prevalence of myopia and study type) and sensitivity analyses were conducted. A significant protective effect of outdoor time was found for incident myopia (clinical trials: risk ratio (RR) = 0.536, 95% confidence interval (CI) = 0.338 to 0.850; longitudinal cohort studies: RR = 0.574, 95% CI = 0.395 to 0.834) and prevalent myopia (cross‐sectional studies: OR = 0.964, 95% CI = 0.945 to 0.982). With dose–response analysis, an inverse nonlinear relationship was found with increased time outdoors reducing the risk of incident myopia. Also, pooled results from clinical trials indicated that when outdoor time was used as an intervention, there was a reduced myopic shift of −0.30 D (in both myopes and nonmyopes) compared with the control group (WMD = −0.30, 95% CI = −0.18 to −0.41) after 3 years of follow‐up. However, when only myopes were considered, dose–response analysis did not find a relationship between time outdoors and myopic progression (R 2 = 0.00064). Increased time outdoors is effective in preventing the onset of myopia as well as in slowing the myopic shift in refractive error. But paradoxically, outdoor time was not effective in slowing progression in eyes that were already myopic. Further studies evaluating effect of outdoor in various doses and objective measurements of time outdoors may help improve our understanding of the role played by outdoors in onset and management of myopia.
Keywords: dose–response analysis, meta‐analysis, myopia, outdoor time
Introduction
It was said that by the year 2050, nearly half of the world's population will have myopia (short‐sightedness) and nearly one‐tenth of the world's population will have high myopia (myopia worse than −5.00D; Holden et al. 2016). Myopia is already a major public health concern in many countries in East and South‐East Asia (Morgan et al. 2012), where the prevalence of myopia has rapidly increased over the past few decades (Morgan & Rose 2005) with nearly 80–90% of high school graduates having myopia and 10–20% having sight‐threatening high myopia (Lin et al. 2004). Elsewhere in the world, as in North America, Europe and the Middle East, myopia is also on the rise, albeit slower compared with the prevalence in Asia (Bar Dayan et al. 2005; Vitale et al. 2009). Although easily correctable with spectacles, contact lenses or refractive surgery, uncorrected refractive errors of which myopia is the most common still remain a major cause of visual impairment due to the lack of screening and availability and affordability of refractive correction (Resnikoff et al. 2008; Pascolini & Mariotti 2011). In addition, progressive myopia is associated with increased risks of retinal detachment, cataracts, glaucoma and even blindness (Marcus et al. 2011; Flitcroft 2012).
A number of interventions including special multifocal‐like soft contact lenses, progressive addition or executive bifocal spectacle lenses, overnight orthokeratology and atropine have been shown to slow progression of myopia (Hasebe et al. 2008; Sankaridurg et al. 2011; Berntsen et al. 2012; Chia et al. 2012, 2016; Cho & Cheung 2012; Chen et al. 2013; Walline et al. 2013; Huang et al. 2016) and are increasingly considered as part of the tool kit that the practitioner has to manage myopia. In contrast, with respect to preventing the onset of myopia, to date, outdoor time has been the only factor that was found to be protective. However, its role in controlling progression in already myopic eyes is not conclusive. Also, while various theories such as increased light exposure, release of dopamine from retina, increased depth of field have been suggested to explain the protective effect of outdoor time, the mechanism remains to be elucidated (French et al. 2013a). It remains that if indeed the protective effect of outdoor time is validated in independent studies, it paves the way for tackling the rising burden of myopia in an economical and effective manner. In this respect, a comprehensive analysis of the existing literature on outdoor time and myopia onset provides an avenue to determine the efficacy of outdoor time against onset and progression of myopia. Indeed, Sherwin et al. (2012c) performed and published a meta‐analysis of seven cross‐sectional studies (published up until September 2011) on the association between time outdoors and myopia and reported that a one‐hour increase in the time spent outdoors each day would reduce the risk of prevalent myopia by 13.3%. However, using cross‐sectional data, an association between outdoor time and myopia can be determined and it does not establish if such an association led to or was a result of myopia. In addition, there have been a number of longitudinal cohort studies and clinical trials that were conducted recently to determine whether outdoor time is protective for myopia (Guggenheim et al. 2012; French et al. 2013; Wu et al. 2013; He et al. 2015; Jin et al. 2015).
We therefore performed a systematic review followed by a meta‐analysis and a dose–response analysis that considers and includes data from more recently published clinical trials since the review of Sherwin et al. (2012) to evaluate the effect of outdoor time on the risk of incident/prevalent myopia, the risk of a myopic shift in refractive error and the risk of progression in myopic eyes.
Subjects and Methods
Search strategy
A search of PubMed, EMBASE and the Cochrane Library was undertaken for articles published up to 30 December 2015 including the search terms: ‘outdoor*’, ‘outside’ in combination with ‘myopia’, ‘nearsightedness’, ‘shortsightedness’, ‘near‐sight’, ‘near‐sighted’, ‘near‐sightedness’, ‘short‐sight’, ‘short‐sighted’, ‘short‐sightedness’ and ‘refractive error’. Each primary article obtained from the search was studied to determine its potential inclusion in the review with no restriction placed on the language of the article.
Study selection
Two reviewers (S.Y.X. and X.G.H.) independently assessed the studies for possible eligibility, and studies were included if they (1) were human studies that investigated the relationship between outdoor time and myopia; (2) investigated effect of outdoor time in relation to the prevalence and incidence of myopia and/or myopic shift or progression; (3) reported an effect estimate with a 95% CI or standard error (SE) or provision of sufficient data to calculate these values; and (4) reported specific increased amounts of time spent on outdoor activities (or the ability to calculate this parameter from the data provided) and the incidence of myopia and/or myopia progression; these studies were included in dose–response analysis. The exclusion criteria were as follows: (1) duplicates; (2) nonhuman studies/experiments; (3) topics investigating other aspects of outdoor exposure (e.g. light exposure); (4) articles reporting study design; and (5) review, comments, letter or conference abstract. For studies that assessed a single population, the most relevant study was included.
Data extraction
Data were extracted by two reviewers (S.Y.X. and J.J.Z.) independently for authors, year of publication, location, sample size, subject age, follow‐up duration, method of assessment of outdoor activities, adjusted covariates in multivariable analysis, outcomes and their 95% CIs or standard deviations, and information needed to evaluate study quality. The studies considered fell into three categories: clinical trials, cohort studies and cross‐sectional studies.
Quality assessment
The methodological qualities of the included studies were assessed independently by both reviewers using an adapted Downs and Black checklist (Downs & Black 1998). The original tool consists of 27 items rated as no/unable to determine = 0 and yes = 1, of which 25 items were applicable for clinical trials evaluating healthcare interventions, 15 for longitudinal cohort studies, and 12 for cross‐sectional studies. Item 14 of the checklist pertains to participant blinding that is not suitable for an intervention such as increased time outdoors and was excluded. Because few studies calculated the sample size or reported post hoc statistical power, question 27 was also excluded. For longitudinal cohort studies, items related to the intervention and control groups (4, 5, 8, 13–15, 19, 21–24) were further omitted, and an additional three items (9, 17, 26) regarding follow‐up were not applied for assessment of the cross‐sectional studies. As varying number of items were used to assess each study, a percentage value (Items determined/Total items × 100) was assigned for each study. A study score of ≥66.8% was deemed high quality, 33.4–66.7% deemed to be medium and ≤33.3% considered to be poor. Any discrepancies in data extraction and scoring between the two reviewers were resolved by discussion, using the original article as the reference.
Statistical analysis
Analyses were performed to determine the association between outdoor time and (1) risk of incident/ prevalent myopia from pooled estimates and dose–response analysis; (2) risk of a myopic shift in refractive error (both myopes and nonmyopes) from pooled estimates; and (3) risk of progression of myopia (in myopic eyes) from dose–response analysis.
Statistical analyses were performed with stata version 12.0 software (STATA Corporation, College Station, TX, USA). Dichotomous outcome data were analysed using the pooled RR/odds ratio (OR) with 95% CI and continuous outcomes analysed using the WMD and 95% CI. The Mantel–Haenszel random‐effects model was used to pool the data for meta‐analysis and estimate the overall effect with its 95% CI. Due to the varying length of follow‐up across the clinical trials, the incidence of myopia and myopic shift in refractive error were estimated at 3 years. Data of studies with one‐year follow‐up were multiplied by a factor of 2.3, assuming that the progression reduces with age (Donovan et al. 2012; Wu et al. 2013; Jin et al. 2015). For the cross‐sectional studies, if the exposure variable was defined as hours per day, results were standardized to hours per week by dividing the log(OR) and SE by 7 (Sherwin et al. 2012). Standard error (SE) was estimated by dividing the width of the CI by 2 × 1.96 (Chinn 2000).
A dose–response analysis based on method proposed by Greenland & Longnecker (1992) and Orsini et al. (2006) was performed. Firstly, the amount of increase in the time outdoors was calculated. For clinical trials conducted by He et al. (2015) and Jin et al. (2015), the additional time outdoors in the intervention group was considered the increase in time between the intervention and control groups, whereas in that by Wu et al. (2013) the exposure was assumed from the time children were not allowed to stay in their classrooms. For those cohort studies where outdoor time was measured as a categorical variable, the increase in time outdoors between groups was estimated by subtracting the dose of high category with the low. Specifically, the mid‐point of the upper and lower boundaries was considered the dose for each category; if the highest category was open‐ended, the mid‐point of the category was set at 1.5 times the lower boundary, whereas if the lower boundary for the lowest category was not provided, the assigned median value was half of that of the upper boundary. In longitudinal cohort studies, the RR was calculated from the OR with correction for the incidence of myopia in the sample studied, as previously described (Zhang & Yu 1998). A scatter diagram was generated using Microsoft Excel, and trends if any between increased time outdoors and the corresponding effect size was studied.
Statistical heterogeneity was assessed using the I 2 test, with I 2 ≥ 50% considered to indicate high heterogeneity. For estimates with high heterogeneity, ±2xTau, which is the standard deviation across studies, is reported to present the approximate 95% range of the underlying effects. Sensitivity analysis was also performed by sequentially removing individual studies to determine whether it resulted in a substantial change in the magnitude or direction of the pooled estimates and heterogeneity.
Subgroup analyses were performed to assess reliability and were based on participant's age groups, prevalence of myopia (<20%, 20–80% and >80%) and study type. Statistical significance was maintained at p < 0.05.
Results
Search results
A total of 604 articles were identified from searching the databases. After removing duplicates, the title and abstracts of 330 records were screened and a further 252 articles excluded at this stage. The full text of the remaining 78 articles was reviewed, articles that did not meet the study criteria were excluded, and a total of 51 articles published between 2002 and 2015 were included. (Peckham et al. 1977; Parssinen & Lyyra 1993; Saw et al. 2000; Tan et al. 2000; Saw et al. 2001; Mutti et al. 2002; Saw et al. 2002, 2006; Jones et al. 2007; Onal et al. 2007; Ip et al. 2008; Rose et al. 2008a,b; Dirani et al. 2009; Lu et al. 2009; Deng et al. 2010; Low et al. 2010; Ming‐Ming et al. 2010; Wu et al. 2010; Zhang et al. 2010; Jones‐Jordan et al. 2011; Yi & Li 2011; Guggenheim et al. 2012; Jones‐Jordan et al. 2012; Sherwin et al. 2012; Cheng et al. 2013; French et al. 2013; Guo et al. 2013a,b; Wu et al. 2013; Xie et al. 2013; Han et al. 2014; Lin et al. 2014; Parssinen et al. 2014; Read et al. 2014; Scheiman et al. 2014; Zhou et al. 2014; Chua et al. 2015; Guo et al. 2015; He et al. 2015; Jin et al. 2015; Lee et al. 2015; Li et al. 2015; Oner et al. 2015; Pan et al. 2015; Ramessur et al. 2015; Saxena et al. 2015; Wen et al. 2015; Wu et al. 2015; Zadnik et al. 2015; Zhou et al. 2015) Of these, 25 studies were finally considered for the analysis. Figure 1 presents a flow diagram of the procedure that resulted in the final list of articles considered for the analyses.
Figure 1.
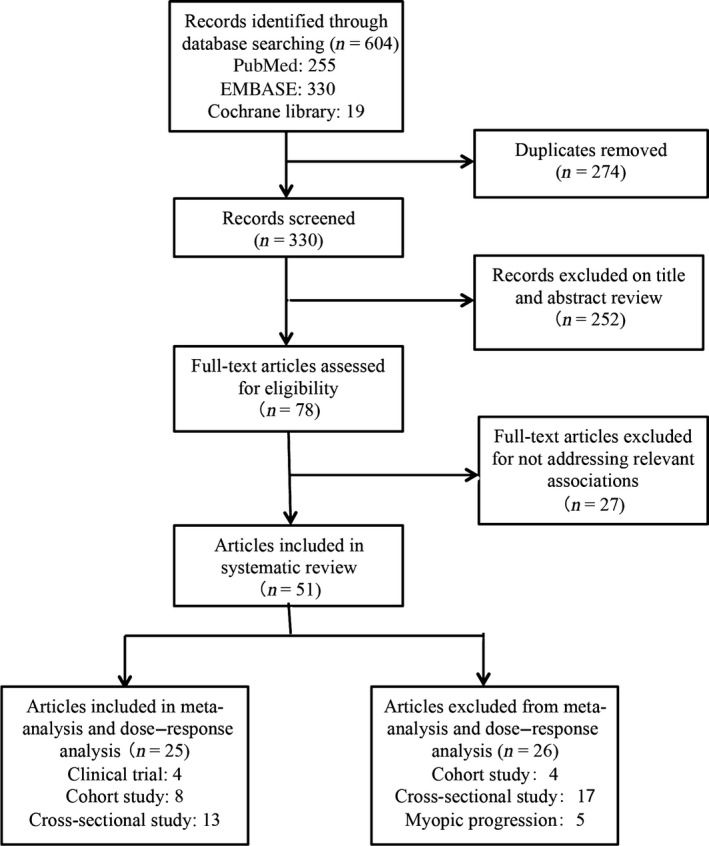
Flow diagram of the literature search and study selection.
Characteristics and quality of the articles included
Table 1 details the relevant features of the 25 articles. Briefly, the articles included four clinical trials (2945 participants), eight cohort studies (8363 participants) and 13 cross‐sectional studies (23 112 participants).
Table 1.
Characteristics of studies included in meta‐analysis and dose–response analysis
| Study (first author, year) | Participants [region] | Outcomes | Total score (percentage) | Quality |
|---|---|---|---|---|
| Myopia Incidence – Clinical Trial | ||||
| He et al. (2015) | 1903 schoolchildren; mean age: 6.61 years in the intervention group and 6.57 years in the control group; follow‐up for 3 years. [Guangzhou, China] | An additional 40‐min class of outdoor activities was added to each school day in the intervention group. Cumulative incidence of myopia: intervention group: 30.4%, control group: 39.5%; cumulative myopia progression: intervention group: −1.42 (−1.58 to −1.27) D, control group: −1.59 (−1.76 to −1.43) D. | 23 (92%) | High |
| Jin et al. (2015) | 391 schoolchildren; mean age: 10.77 years in the intervention group and 10.42 years in the control group; follow‐up for 1 year. [Shenyang, China] | An additional 40‐min class of outdoor activities was added to each school day in the intervention group. Incidence of myopia: intervention group: 3.7%, control group: 8.5%; myopia progression: intervention group: −0.10 ± 0.65 D, control group: −0.27 ± 0.52D. | 19 (76%) | High |
| Wu et al. (2013) | 571 schoolchildren; mean age: 8.89 years in the intervention group and 9.02 years in the control group; follow‐up for 1 year. [Taiwan] | Children were encouraged to go outside for outdoor activities during recess. Incidence of myopia: intervention group: 8.41%, control group: 17.65%; myopia progression: intervention group: −0.25 ± 0.68 D, control group: −0.38 ± 0.69D. | 15 (60%) | Medium |
| Yi & Li (2011) | 80 schoolchildren; mean age: 8.8 years in the intervention group and 8.9 years in the control group; follow‐up for 1 years. [Changsha, China] | Did near‐ and middle‐vision activities <30 hr/week and more outdoor activities than 14–15 hr/week. Annual myopia progression: intervention group: −0.38 ± 0.15D, control group: −0.52 ± 0.19D. | 15 (60%) | Medium |
| Myopia Incidence – Cohort Study | ||||
| French et al. (2013) | 863 schoolchildren in younger cohort; mean age: 6 years; follow‐up for an average of 6.1 years. | In both younger and older cohorts, there was a significant trend towards greater incident myopia in children who spent less time outdoors (younger cohort: low versus high: OR = 2.84, moderate versus high: OR = 1.14; older cohort: low versus high: OR = 2.15, moderate versus high: OR = 2.00) after adjusting for age, gender and parental myopia. | 11 (73.3%) | High |
| 1196 schoolchildren in older cohort; mean age: 12 years; follow‐up for an average of 4.6 years. [Sydney, Australia] | ||||
| Guggenheim et al. (2012) | 2005 schoolchildren; mean age: 11 years; follow‐up for an average of 4 years. [UK] | Time spent outdoors in age 8–9 years was predictive for incident myopia in age 11 years (OR = 0.65, 95% CI = 0.45 to 0.96). Adjusted for parental myopia, time reading, gender, physical activity/sedentary behaviour and constant. | 11 (73.3%) | High |
| Saw et al. (2006) | 994 schoolchildren; age: 7–9 years; follow‐up for an average of 3 years. [Singapore] | Outdoor activity was not associated with incident myopia (RR = 1.01, 95% CI = 0.98 to 1.04) in multivariate analyses. | 12 (80%) | High |
| Myopia Prevalence – Cross‐sectional Study | ||||
| Chua et al. (2015) | 572 children; age: 3 years. [Singapore] | Outdoor activity at 24 months was not associated with myopia in 3 years old (OR = 0.84, 95% CI = 0.61 to 1.17). | 11 (91.7%) | High |
| Zhou et al. (2015) | 1902 schoolchildren; mean age: 9.8 years. [Guangzhou, China] | More time outdoors was associated with less myopia (OR = 0.97, 95% CI = 0.95 to 0.99) in multilevel mixed‐effects logistic regression models of potential predictors of age, gender, total CSHQ score, night‐time sleep time and total time spent in near work. | 11 (91.7%) | High |
| Lee et al. (2015) | 5048 male military conscripts; age: 18–24 years. [Taiwan] | Engaging in fewer outdoor activities was significantly related to prevalence of myopia (OR = 0.94, 95% CI = 0.90 to 0.98) after adjusting for age, parental myopia, education level, reading distance, time spent reading, using computer, watching television and urbanization level. | 10 (83.3%) | High |
| Pan et al. (2015) | 4413 residents; age: 50 years or older. [Yunnan, China] | Less time spent outdoors per day in childhood was significantly associated with the presence of myopia (OR = 0.92, 95% CI = 0.84 to 0.98). | 12 (100%) | High |
| Guo et al. (2015) | 1565 schoolchildren; mean age: 11.9 years. [Inner Mongolia, China] | Presence of myopia was significantly associated with less hours spent outdoors after school (OR = 0.80, 95% CI = 0.64 to 0.99). | 9 (75%) | High |
| Zhou et al. (2014) | 823 schoolchildren; mean age: 9.21 years. [Lanzhou, China] | Outdoor activities was inversely associated with prevalence of myopia, although not statistically significant (OR = 0.937, 95% CI = 0.775 to 1.896) | 9 (75%) | High |
| Guo et al. (2013) | 681 primary students in rural and urban regions; mean age: 7.7 years. [Beijing, China] | Presence of myopia was associated with less time spent outdoors (OR = 0.32, 95% CI = 0.21 to 0.48) after adjusting for age and maternal myopia. | 10 (83.3%) | High |
| Low et al. (2010) | 3009 preschool children; age: 6–72 months. [Singapore] | Outdoor activity was not associated with preschool myopia (OR = 0.95, 95% CI = 0.85 to 1.07). Adjusted for familial clusters, age, gender, height, parental myopia and time spent reading words or pictures alone. | 10 (83.3%) | High |
| Deng et al. (2010) | 147 schoolchildren; age: 6–18 years. 89 | There was a statistically significant association between myopia and outdoor activities during the school year (OR = 0.915, 95% CI: 0.843 to 0.994) and the summer (OR = 1.00, 95% CI, 0.969 to 1.033), adjusting for age and number of myopic parents. | 8 (66.7%) | Medium |
| Dirani et al. (2009) | 1249 schoolchildren; mean age: 13.7 years. [Singapore] | Children who spent more time outdoors were 0.90 (95% CI = 0.84 to 0.96) times likely to have myopia, after adjusting for age, gender, ethnicity, school, books read per week, height and parental myopia, father's education level and IQ level. | 9 (75%) | High |
| Lu et al. (2009) | 998 schoolchildren; mean age: 14.6 years. [Xichang, China] | In logistic regression models of factors potentially predictive of myopia, outdoor activity was not significantly associated with myopia (OR = 1.14, 95% CI = 0.69 to 1.89). | 11 (91.7%) | High |
| Ip et al. (2008) | 2339 schoolchildren; mean age: 12 years. [Sydney, Australia] | Outdoor activity was significantly associated with myopia (OR = 0.97, 95% CI = 0.94 to 0.995). | 12 (100%) | High |
| Mutti et al. (2002) | 366 schoolchildren; mean age: 13.7 years. 89 | Myopes tended to spend less time engaged in sports activities (OR = 0.936, 95% CI = 0.892 to 0.983). Adjusted for parental myopia, dioptre‐hours per week, ITBS reading local and ITBS total language local. | 9 (75%) | High |
| Myopia Progression – Cohort Study | ||||
| Oner et al. (2015) | 50 myopic children; age: 9–14 years; follow‐up for 33.3 ± 10.3 (ranging from 17 to 55) months. [Turkey] | Outdoor activities had no correlation with annual myopia progression rate (r = −0.041, p = 0.766). | 10 (66.7%) | Medium |
| Li et al. (2015) | 2267 grade 7 students; age: 10 to 15 years; follow‐up for two years. [Anyang, China] | Outdoor activity was measured as a categorical variable and was not associated with change in SER (high versus low: β = 0.029 D/y, 95% CI = −0.015 to 0.072, p = 0.196). | 14 (93.3%) | High |
| Jones‐Jordan et al. (2012) | 835 myopic children who participated in CLEERE study; ages: ranging from 6 to 14 years; 1‐year progression interval. [USA] | An additional 10 hr of weekly outdoor activity was associated with 0.01 D progression per year (95% CI = −0.03 to 0.06), which was not statistically significant. | 12 (80%) | High |
| Jones et al. (2007) | 514 schoolchildren; mean age: 8.63 years; follow‐up for an average of 5 years. [USA] | The nonmyopic child participated in an average of 11.65 ± 6.97 hr/week of sports and outdoor activity, whereas the future myopic child participated in an average of 7.98 ± 6.54 hr/week (OR = 0.91, 95% CI = 0.87 to 0.95) after adjusting for parental myopia. | 13 (86.7%) | High |
| Saw et al. (2000) | 153 children; age: 6 to 12 years; mean follow‐up for 28 months. [Singapore] | No statistically significant associations between SER change and outdoor activities (hr/week) were observed (β: 0.013; 95% CI = −0.013 to 0.04; p: 0.33). | 10 (66.7%) | Medium |
OR = odds ratio, CI = confidence interval, RR = relative risk.
With respect to geographical location of the studies considered in the articles, 17 studies were conducted in East Asia (China, Taiwan and Singapore) with the remainder of the studies from Australia (one cohort study and one cross‐sectional; Ip et al. 2008; French et al. 2013), UK (one cohort; Guggenheim et al. 2012), USA (two cohort and two cross‐sectional studies; Mutti et al. 2002; Jones et al. 2007; Deng et al. 2010; Jones‐Jordan et al. 2012) and Turkey (one cohort; Oner et al. 2015). Participants in these studies were mostly schoolchildren aged 6–18 years with a small number of studies considering other ages (children aged 6–72 months (Low et al. 2010), children aged 3 years (Chua et al. 2015), adults aged 18–24 years (Lee et al. 2015) and adults aged 50 years or older (Pan et al. 2015).
The quality assessment scores for the articles ranged from 60% (Yi & Li 2011; Wu et al. 2013) to 100% (Ip et al. 2008; Pan et al. 2015; mean = 79.99%) with the most prominent deficiency being the lack of representativeness of the recruited participants. Selection of participants based on a random cluster sampling strategy was adopted in eight studies, of which four studies used stratified sampling (Low et al. 2010; French et al. 2013; He et al. 2015; Zhou et al. 2015), two studies used simple sampling (Lu et al. 2009; Pan et al. 2015) and a single study from Ejina, where only three schools were available, recruited an unselected sample of consecutive participants (Guo et al. 2015). Randomization was either not adopted or not mentioned in the remaining 18 studies.
Ten studies compared the characteristics of participants with those of nonparticipants(Mutti et al. 2002; Ip et al. 2008; Dirani et al. 2009; Lu et al. 2009; Low et al. 2010; Chua et al. 2015; He et al. 2015; Jin et al. 2015; Lee et al. 2015; Pan et al. 2015). However, no significant difference was reported in only four studies (Ip et al. 2008; He et al. 2015; Jin et al. 2015; Pan et al. 2015).
Any adverse effects related to the intervention such as the development of skin and ocular cancers or growths were not reported in any of the four clinical trials, and additionally, the examiners were not masked (Yi & Li 2011; Wu et al. 2013; He et al. 2015; Jin et al. 2015).
Other reasons for loss of scores included lack of adjustments for confounding factors (Yi & Li 2011; Jin et al. 2015), lack of information regarding participants lost to follow‐up (Yi & Li 2011; Guggenheim et al. 2012; French et al. 2013; Wu et al. 2013) and the absence of actual probability values (Deng et al. 2010).
Association between Outdoor time and risk of Incident/Prevalent Myopia
Pooled estimates
Figure 2 details the results of pooled main random‐effects meta‐analysis.
Figure 2.
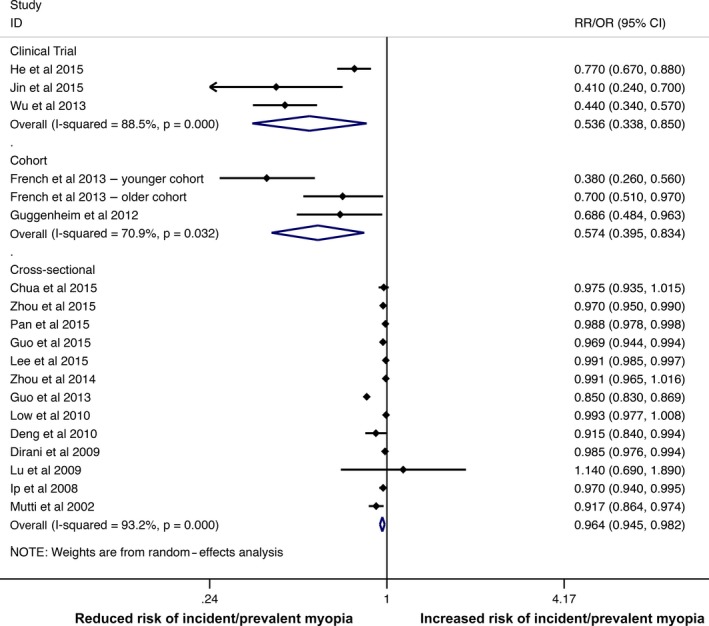
Forest plot corresponding to main random‐effects meta‐analysis performed to quantify the relationship between the time spent on outdoor activities and the incidence or prevalence of myopia. All statistical tests were two‐sided. CI = confidence interval. [Colour figure can be viewed at wileyonlinelibrary.com].
Data from the three clinical trials shows significant protective effect of increasing outdoor time for risk of incident myopia during school recess (RR = 0.536, 95% CI = 0.338 to 0.850, I 2 = 87.7%, p value for heterogeneity <0.001, ±2xTau = ±0.743). Similarly, pooled data from cohort studies comparing high versus low levels of outdoor time found that high level of outdoor time was significantly associated with a reduced risk of incident myopia (RR = 0.574, 95% CI = 0.395 to 0.834, I 2 = 70.9%, p value for heterogeneity = 0.032, ±2xTau = ±0.555).
The OR estimates from the cross‐sectional studies were pooled after their conversion into a standardized effect estimate, yielding a final OR of 0.964 (95% CI = 0.945 to 0.982, I 2 =93.2%, p value for heterogeneity <0.001, ±2xTau = ±0.063) for myopia per additional hour of time spent outdoors per week.
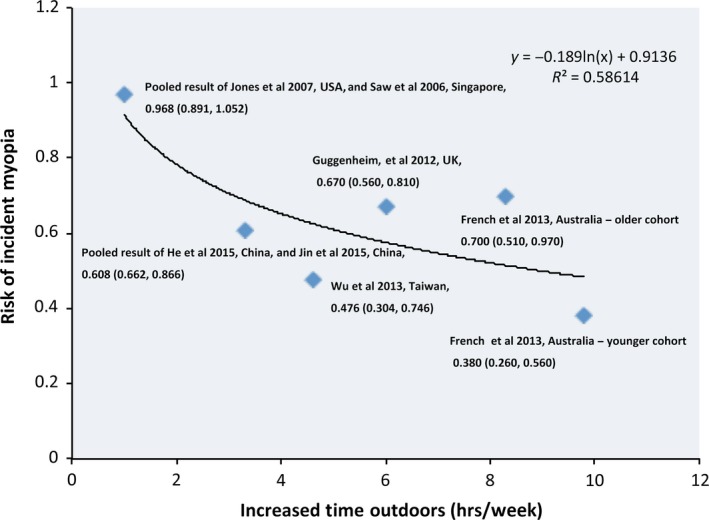
Dose–response relationship
Five studies from America, Singapore, UK, China and Taiwan (six cohorts) were included in the dose–response analysis, of which only the study in Australia by French et al. (2013) investigated varying doses of outdoor time. In this study, odds ratios for incident myopia were significantly higher for the lowest tertile (≤13 hr/week in younger cohort and ≤13 hr/week in older cohort) of time outdoors compared with the highest (>22.5 hr/week in younger and older cohorts). Results of the included five studies showed curve linearity (Fig. 3) and an inverse relation with increased time outdoors associated with lowered risk of incident myopia (R 2 = 0.586). Using the equation provided in Fig. 3, an increase of 8.9 hr of time outdoors per week compared with the control or baseline, or an increase of 76 min/day, was needed to obtain a 50% reduction in incident myopia, while an increase of 1 hr/day or 7 hr/week will result in a 45% reduction in incident myopia compared with controls.
Figure 3.
Dose–response analysis of the time spent outdoors and the risk of myopia (y: risk ratio; and x: increased time spent outdoors). [Colour figure can be viewed at wileyonlinelibrary.com].
Sensitivity analysis
For clinical trial, when the RCT by He et al. (2015) was excluded, the pooled RR of the two CCTs was relatively lower with reduced heterogeneity (RR = 0.435, 95% CI = 0.344 to 0.550, I 2 = 0%, p value for heterogeneity = 0.829), while the exclusion of Jin et al. (2015)) and Wu et al. (2013)), respectively, resulted in higher RR with still high heterogeneity (Table 2). For cohort study, the exclusion of younger cohort in study by French et al. (2013) resulted in higher RR with reduced heterogeneity (RR = 0.693, 95% CI = 0.548 to 0.877, I 2 = 0%, p value for heterogeneity = 0.933), while the exclusion of older cohort in study by French et al. (2013) and study by Guggenheim et al. (2012), respectively, resulted in relatively lower RR with increased heterogeneity (Table 2). For cross‐sectional study, overall risk estimates were not substantially modified by any single study, with a range of 0.960 (95% CI: 0.939 to 0.982; Pan et al. 2015) to 0.984 (95% CI: 0.979 to 0.991; Guo et al. 2013a). However, following exclusion of the study by Guo et al. (2013a), heterogeneity decreased significantly (93.2% to 39.8% in I 2; Table 2).
Table 2.
Sensitivity analysis of the meta‐analysis results of cross‐sectional study
| Study excluded | Random‐effects models | Heterogeneity | ||
|---|---|---|---|---|
| OR | 95% CI | I 2 (%) | p Value | |
| Clinical trial | ||||
| None | 0.536 | 0.338 to 0.850 | 88.5 | <0.001 |
| He et al. (2015) | 0.435 | 0.344 to 0.550 | 0.00 | 0.829 |
| Jin et al. (2015) | 0.589 | 0.340 to 1.018 | 92.9 | <0.001 |
| Wu et al. (2015) | 0.594 | 0.323 to 1.091 | 80.0 | 0.025 |
| Cohort Study | ||||
| None | 0.574 | 0.395 to 0.834 | 70.9 | 0.032 |
| French et al. (2013) – younger cohort | 0.693 | 0.548 to 0.877 | 0.00 | 0.933 |
| French et al. (2013) – older cohort | 0.514 | 0.288 to 0.917 | 80.2 | 0.025 |
| Guggenheim et al. (2012) – | 0.521 | 0.286 to 0.947 | 82.5 | 0.017 |
| Cross‐sectional Study | ||||
| None | 0.964 | 0.945 to 0.982 | 93.2 | <0.001 |
| Chua et al. (2015) | 0.963 | 0.944 to 0.982 | 93.7 | <0.001 |
| Zhou et al. (2015) | 0.963 | 0.943 to 0.983 | 93.7 | <0.001 |
| Pan et al. (2015) | 0.960 | 0.939 to 0.982 | 93.7 | <0.001 |
| Guo et al. (2015) | 0.963 | 0.944 to 0.983 | 93.7 | <0.001 |
| Lee et al. (2015) | 0.960 | 0.937 to 0.983 | 93.2 | <0.001 |
| Zhou et al. (2014) | 0.961 | 0.942 to 0.981 | 93.7 | <0.001 |
| Guo et al. (2013) | 0.984 | 0.979 to 0.991 | 39.8 | 0.075 |
| Low et al. (2010) | 0.960 | 0.940 to 0.981 | 93.7 | <0.001 |
| Deng et al. (2010) | 0.965 | 0.947 to 0.984 | 93.7 | <0.001 |
| Dirani et al. (2009) | 0.961 | 0.938 to 0.983 | 93.7 | <0.001 |
| Lu et al. (2009) | 0.963 | 0.945 to 0.982 | 93.7 | <0.001 |
| Ip et al. (2008) | 0.963 | 0.944 to 0.983 | 93.7 | <0.001 |
| Mutti et al. (2002) | 0.966 | 0.948 to 0.985 | 93.6 | <0.001 |
Subgroup analysis
Figure 4 details the results of the subgroup analysis.
Figure 4.
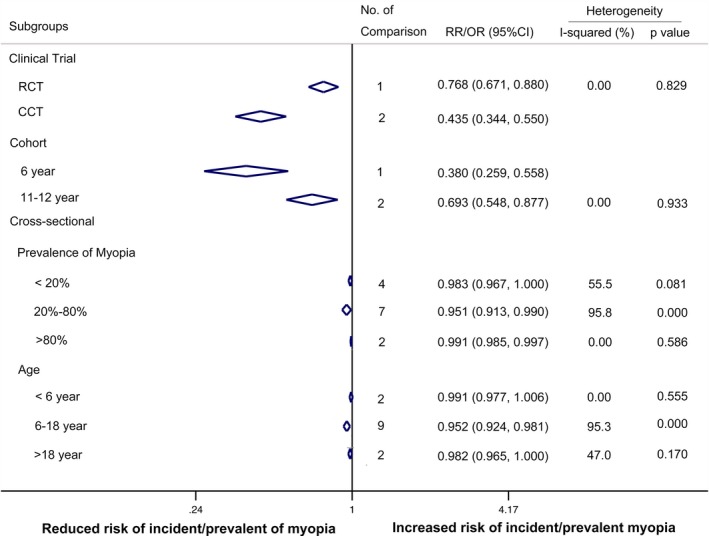
Subgroup analysis of the trials included to assess the relationship between outdoor activities and the myopia incidence or prevalence, CI = confidence interval, RR = relative risk, OR = odds ratio, RCT = randomized clinical trial, and CCT = controlled clinical trial. [Colour figure can be viewed at wileyonlinelibrary.com].
When the trial type (RCT versus CCT) was considered, the pooled RR of the two CCTs indicated a stronger protective effect with narrower 95% CI (CCTs: RR = 0.435, 95% CI = 0.344 to 0.550). The effect of age was carried out in both cohort and cross‐sectional studies. In the cohort studies, the younger age group of 6‐year‐olds had a stronger protective effect (RR: 0.380, 95% CI: 0.259 to 0.558) compared with older kids aged 11–12 years. Both groups had protective effects. However in the cross‐sectional studies, the protective effect of outdoor time was not significantly different between the three age groups (<6, 6–18 and >18 years). It was also observed from cross‐sectional studies that the protective effect of outdoor time was not significantly different between the three groups of myopia prevalence (<20%, 20–80% and >80%).
Association between Outdoor time and risk of myopic shift in refractive error
Pooled estimates
Data from three clinical trials were pooled to estimate the relationship between the time outdoors and risk of a myopic shift in refractive error in both myopes and nonmyopes (Fig. 5; Wu et al. 2013; He et al. 2015; Jin et al. 2015). Increased time outdoors was associated with a reduction in myopic shift by −0.30 D in the intervention group compared with the control group (WMD = −0.30D, 95% CI = −0.18 to −0.41D, I 2 = 58.6%, p value for heterogeneity = 0.089, ±2xTau = ±0.155). The pooled estimate from the CCT and RCT studies showed that the CCT studies showed a greater reduction in myopic shift compared with the RCT studies (CCTs: WMD = −0.34D, 95% CI = −0.26 to −0.43 versus RCT: WMD = −0.17D, 95% CI = −0.01 to −0.33).
Figure 5.
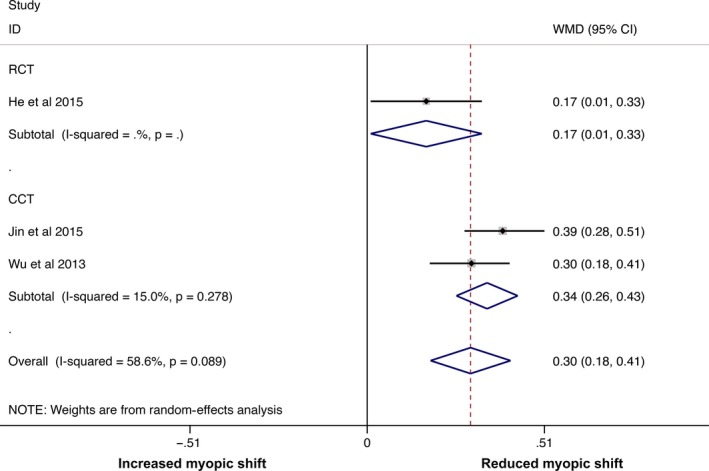
Forest plot corresponding to main random‐effects meta‐analysis performed to quantify the mean difference in myopic shift in refraction in the whole sample between the intervention group, with increased time spent outdoors, and the control group. All statistical tests were two‐sided. CI = confidence interval, and WMD = weighted mean difference. [Colour figure can be viewed at wileyonlinelibrary.com].
Dose–response analysis
Six studies reporting on time outdoors and the associated progression in myopes were included in evaluation of the dose–response relationship and found the absence of a dose–response relationship between an increased time spent outdoors and myopic progression (R 2 = 0.00064; Fig. 6). Only one of the six studies showed a significant protective effect of outdoor time on myopic progression (mean difference between control and test: −0.14, 95% CI: −0.22 to −0.06; Yi & Li 2011). Another study also showed a protective effect (mean difference: −0.12, 95% CI: −0.31 to 0.06); however, it did not reach statistical significance (Wu et al. 2013). The other four cohort studies reported a treatment effect ranging from −0.003 D (Li et al. 2015) to 0.013 D (Saw et al. 2000) that were not statistically significant.
Figure 6.
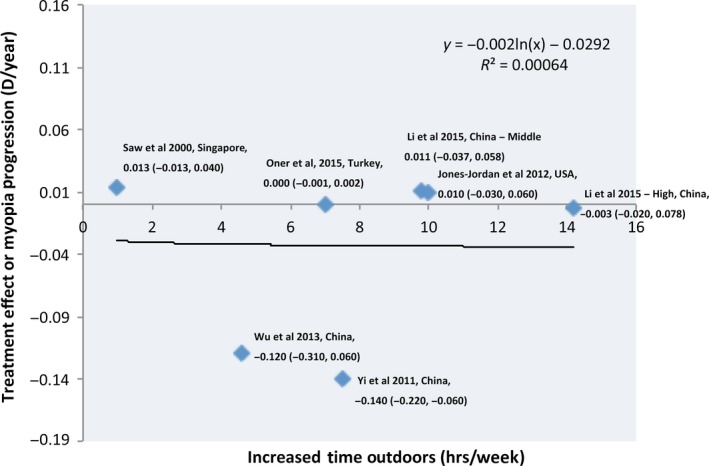
Dose–response analysis of the time spent outdoors and myopic progression rate (y: treatment effect or annual myopic progression, and x: increased time spent outdoors). [Colour figure can be viewed at wileyonlinelibrary.com].
Estimates of association in studies excluded from meta‐analysis and dose–response analysis
Table 3 presents the details of the articles excluded from the analyses.
Table 3.
Studies excluded from meta‐analysis and dose–response analysis
| Study (first author, year) | Participants [region] | Outcomes | Reasons for exclusion | Total score (percentage) | Quality |
|---|---|---|---|---|---|
| Myopia Incidence – Cohort Study | |||||
| Zadnik et al. (2015) | 4512 schoolchildren enrolled in CLEERE study; age: 6 through 13 years. [USA] | Time outdoors was not associated with risk of myopia onset in multivariate models (data not shown). | Data from multivariate model were not available | 9 (60%) | Medium |
| Jones‐Jordan et al. (2011) | 731 incident myopes and 587 emmetropes in the CLEERE study. [USA] | Hours per week spent in outdoor/sports activities were significantly less for children who became myopic 3 years before onset through 4 years after onset by 1.1–1.8 hr/week. | No multivariate OR or RR was presented. | 9 (60%) | Medium |
| Onal et al. (2007) | 207 Turkish medical students; mean age: 21.11 ± 1.58 years (range: 18 to 26 years); follow‐up for 1 year. [Turkey] | Nonmyopes reported a significantly higher prevalence of outdoor activity before and at age seven (68.4%) than did myopes (48.6%; p < 0.009). Outdoor activity during early childhood was found to be protective for myopia on multivariate analysis (OR = 0.44, 95% CI = 0.23 to 0.82). | Activity was measured as mostly indoor activities or mostly outdoor activities, but not a continuous variable. | 11 (73.3%) | High |
| Peckham et al. (1977) | 383 children aged 7–11 years from a birth cohort. [UK] | Children with myopia participated in outdoor sports as often as those without. | No multivariable OR was available. | 4 (26.7%) | Low |
| Myopia Prevalence – Cross‐sectional Study | |||||
| Saxena et al. (2015) | 9884 schoolchildren; mean age: 11.6 years. [Delhi, India] | An inverse association with outdoor activities/playing was observed with children playing >14 hr in a week (OR = 0.2, 95% CI = 0.14 to 0.26). | Exposure (outdoor activity) was measured as a categorical variable. | 10 (83.3%) | High |
| Ramessur et al. (2015) | 64 monozygotic (MZ) twin pairs discordant for refractive error; mean age: 56 (range 30 to 79 years)14 | The twins who spent more time outdoors (mean score for children aged <16 years, 0.09; 95% CI = 0.03 to 0.15; mean score for children aged 16–25 years, 0.28; 95% CI = 0.15 to 0.41) or performed more outdoors sports (mean score for children aged <16 years, 0.13; 95% CI = 0.04 to 0.21; mean score for children aged 16 – 25 years, 0.23, 95% CI = 0.10 to 0.36) were less likely to be myopic than their twin. | Difference in time spent outdoors between twins was analysed in relation to spherical equivalent discordancy. | 8 (66.7%) | Medium |
| Wen et al. (2015) | 1218 schoolchildren; grade 1 through grade 6 [Sanya, China] | Nonmyopes spent more time outdoors than myopes (7.25 ± 5.35 versus 11.86 ± 6.65 hr/week), although the association was not statistically significant in multivariable regression analysis (<10 hr/week: β = 0.297, SE = 0.125, p = 0.035; >10.0 hr/week: β = 0.365, SE = 0.198, p = 0.073). | No multivariate OR or RR was presented. | 3 (25%) | Low |
| Han et al. (2014) | 2209 schoolchildren; age: 11–15 years. [Qinghai, China] | Outdoor activities per week were associated with myopia (<7 hr/week versus ≥7 hr/week: OR = 1.977, SE = 0.439). | Exposure (outdoor activity) was measured as a categorical variable. | 7 (58.3%) | Medium |
| Lin et al. (2014) | 370 children from primary (age: 6 to 12 years) and secondary (age: 13 to 17 years) [Beijing, China] | A significant association between outdoor activity time and the children's spherical equivalent was found in the primary school students (β = 0.27, p = 0.03) but not in the secondary school students (β = 0.04, p = 0.70). | The association between outdoor activity time and the spherical equivalent but not the prevalence of myopia was estimated. | 10 (83.3%) | High |
| Read et al. (2014) | 102 children (41 myopes and 61 emmetropes) age: 10 to 15 years. [Australia] | The amount of daily time spent in outdoor bright light conditions (>1000 lux) was significantly greater in emmetropes (127 ± 51 min) compared with myopes (91 ± 44 min, p < 0.001) | No multivariate OR or RR was presented. | 7 (58.3%) | Medium |
| Cheng et al. (2013) | 1894 children of grade 1 through grade 6. [Taiwan] | No difference in the time spent outdoors was noted between myopes and nonmyopes. Based on linear regression analysis, weekly daily outdoor activities with sunlight exposure can only predict 0.2% of its extent of association with the refractive error. | The association between outdoor activity time and the spherical equivalent but not the prevalence of myopia was estimated. | 9 (75%) | High |
| Xie et al. (2013) | 929 freshmen who have normal vision when they graduated from primary school. [China] | The prevalence of myopia among students engaging mostly in outdoor activities after class was significantly lower than those engaging mostly in homework (OR = 0.547, SE = −0.140). | The prevalence of myopia was compared between three different kinds of activities including doing homework, playing outdoors and watching TV after class. | 8 (66.7%) | Medium |
| Sherwin et al. (2012) | 636 permanent residents aged ≥15 years from Norfolk Island. [Australia] | UVAF was independently associated with myopia: OR for total UVAF (per 10 mm2) was 0.81, 95% CI = 0.69 to 0.94, p = 0.007. Time spent outdoors was not significantly associated with myopia in the same multivariable model. | The area of UVAF was measured to estimate time spent outdoors. And the amount of time spent outdoors was not measured as hours, but estimated as the proportion of the day. | 10 (83.3%) | High |
| Wu et al. (2010) | 145 schoolchildren; age: 6–12 years. [Taiwan] | Outdoor activity was significantly associated with decreased risk of myopia (adjusted OR = 0.3, 95% CI = 0.1 to 0.9). | Exposure (outdoor activity) was measured as a categorical variable. | 9 (75%) | High |
| Zhang et al. (2010) | 2480 participants with refractive and questionnaire data were included in the final analysis, with a mean age of 13.8 ± 1.1 years. [China] | In multivariable model, outdoor activities were not associated with SER (β = −0.004, 95% CI = −0.019 to 0.011, p = 0.61). | The association between outdoor activity time and the spherical equivalent but not the prevalence of myopia was estimated. | 10 (83.3%) | High |
| Ma et al. (2010)61 | 1363 students; age: 13–18 years. [Zhejiang, China] | Outdoor activity during weekdays was associated with an increased odd of emmetropia relative to myopia (OR 1.145; 95% CI 1.047 to 1.252, p = 0.003). | Data from multivariate model were not available | 8 (66.7%) | Medium |
| Rose et al. (2008a) | 1765 year 1 schoolchildren and 2367 year 7 schoolchildren participated in the Sydney Myopia Study; mean age: 6.7 years for year 1 participants and 12.7 years for year 7 participants. [Sydney, China] | After adjustment for gender, ethnicity, parental myopia, near work, maternal and parental education and maternal employment, a greater number of hours spent outdoors was associated with a more hyperopic mean SER in both year 1 (p < 0.009) and year 7 (p < 0.0003) students. | The association between outdoor activity time and the spherical equivalent but not the prevalence of myopia was estimated. | 10 (83.3%) | High |
| Rose et al. (2008b) | Two cross‐sectional samples of age‐ and ethnicity‐matched primary school children participated: 124 from the Sydney Myopia Study and 628 from the Singapore Cohort Study on the Risk Factors for Myopia. [Sydney and Singapore] | Children in Sydney spent more time on outdoor activities (13.75 versus 3.05 hr/week; p < 0.001), which was the most significant factor associated with the differences in the prevalence of myopia between the two sites. | No multivariate OR or RR was presented. | 10 (83.3%) | High |
| Saw et al. (2002) | 957 Chinese schoolchildren aged 7 to 9 years in Singapore and Xiamen, China. [Singapore and Xiamen, China] | Myopic children spent less time on outdoor activities (p = 0.03). No association between outdoor activity and myopia or high myopia, after adjustment (estimate of association not available) was seen. | No multivariate OR or RR estimating the association between outdoor activity and myopia was presented. | 7 (58.3%) | Medium |
| Saw et al. (2001) | Children aged 8–9 years attending second grade from one school in Xiamen city (n = 119) and one school in the Xiamen countryside (n = 91) were recruited. [Xiamen, China] | Myopes spent less time outdoors than nonmyopes (8.9 hr/week for myopia versus 9.8 hr/week for nonmyopia), although not statistically significant (p = 0.12). | Did not provide a measure of association for outdoor activity as a risk factor for myopia that adjusted for potential confounders. | 6 (50%) | Medium |
| Tan et al. (2000) | 414 kindergarten children aged 4 to 6 years. [Singapore] | Children with <7 hr of outdoor activity per week had a higher prevalence of myopia, although this was not statistically significant (RR = 0.81; 95% CI = 0.50 to 1.32). | Univariable analysis was available, but without multivariable analysis. | 7 (58.3%) | Medium |
| Myopia Shift – Cohort Study | |||||
| Wu et al. (2015) | 5052 schoolchildren; age: 6 through 12 years; follow‐up for one year. [Beijing, China] | Significant myopic shift (the change in SER ≤ −0.50D) was independently associated with longer time outdoors for leisure (OR = 0.87, 95% CI = 0.78 to 0.97, p < 0.013) | Myopic shift in refraction in the whole sample but not in the baseline myopes was analysed. | 13 (86.7%) | High |
| Scheiman et al. (2014) | 469 myopic children with SER between −1.25 and −4.50 D; age: 6–11 years; follow‐up for 6–11 years. [USA] | The Gompertz function was used to define the myopia stabilization of each individual. No association between baseline outdoor activities and stabilization by age 15 was observed whether outdoor activity was considered as a categorical or a continuous variable (as a categorical variable: OR = 0.93, 95% CI = 0.53 to 1.65; as a continuous variable: OR = 1.02, 95% CI = 0.99 to 1.06). | Myopia for each child was categorized as stable/not stable by the age of 15 years. Changes in refraction were not analysed in relation to time spent in outdoor activities. | 11 (73.3%) | High |
| Parssinen et al. (2014) | 240 myopic children; mean age at baseline was 10.9, ranging from 8.7 to 12.8 years; follow‐up for 23 years. [Finland] | Myopia increased faster among those who spent 0.5–3 hr on outdoor activities than those who spent >3 hr (p = 0.012). | Trend was demonstrated in a figure. No absolute value of mean differences was presented. | 11 (73.3%) | High |
| Guo et al. (2013) | 681 schoolchildren; the mean age of the children was 7.7 ± 1.6 (ranging 5–13) years; follow‐up for one year. [Beijing, China] | An increase in the SER was significantly associated with less time spent outdoors for leisure (p = 0.006; β = −0.10). | Myopic shift in refraction in the whole sample but not in the baseline myopes was analysed. | 10 (66.7%) | Medium |
| Parssinen & Lyyra (1993) | 240 myopic children; age: 10.9 years; follow‐up for three years. [Finland] | The amount of time spent outdoors was significantly connected with myopic progression in boys (β = 0.23; SE = 0.09; p < 0.01), but not in girls. | The correlation was analysed for boys and girls separately. | 8 (53.3%) | Medium |
CLEERE = Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study, UVAF = ultraviolet autofluorescence, SER = spherical equivalent refraction.
Incidence/prevalence of Myopia
Twenty‐one studies (four prospective cohort studies (Peckham et al. 1977; Onal et al. 2007; Jones‐Jordan et al. 2011; Zadnik et al. 2015) and 17 cross‐sectional studies (Tan et al. 2000; Saw et al. 2001, 2002; Rose et al. 2008a,b; Ming‐Ming et al. 2010; Wu et al. 2010; Zhang et al. 2010; Sherwin et al. 2012; Cheng et al. 2013; Xie et al. 2013; Han et al. 2014; Lin et al. 2014; Read et al. 2014; Ramessur et al. 2015; Saxena et al. 2015; Wen et al. 2015)) were excluded from meta‐analysis for analysis of incident/prevalent myopia. The quality scores of these studies ranged from 25% (Wen et al. 2015) to 86.7% (Jones et al. 2007; mean = 63.93%).
The reasons for exclusion were as follows: nonavailability of multivariate OR or RR (10 studies; Peckham et al. 1977; Tan et al. 2000; Saw et al. 2001, 2002; Rose et al. 2008; Ming‐Ming et al. 2010; Jones‐Jordan et al. 2011; Read et al. 2014; Wen et al. 2015; Zadnik et al. 2015); exposure measured as a categorical variable (six studies; Onal et al. 2007; Wu et al. 2010; Sherwin et al. 2012; Xie et al. 2013; Han et al. 2014; Saxena et al. 2015); and estimation of spherical equivalent rather than prevalence of myopia (five studies; Rose et al. 2008; Zhang et al. 2010; Cheng et al. 2013; Lin et al. 2014; Ramessur et al. 2015).
The participants of two cohort studies by Jones‐Jordan et al. (2011) and Zadnik et al. (2015) were schoolchildren enrolled in the CLEERE. The remaining two cohort studies by Onal et al. and Peckham et al. had small sample sizes (<500 participants). Zadnik et al. (2015) did not found an association between time outdoors and risk of myopia onset in multivariate models (data not shown), while the other three studies observed a protective association (Peckham et al. 1977; Onal et al. 2007; Jones‐Jordan et al. 2011).
A total of 11 of the 17 cross‐sectional studies were carried out in East Asia(Tan et al. 2000; Saw et al. 2001, 2002; Ming‐Ming et al. 2010; Wu et al. 2010; Zhang et al. 2010; Cheng et al. 2013; Xie et al. 2013; Han et al. 2014; Lin et al. 2014; Wen et al. 2015), and two additional studies included participants from East Asia (Rose et al. 2008a,b). Thirteen studies (Tan et al. 2000; Rose et al. 2008a,b; Ming‐Ming et al. 2010; Wu et al. 2010; Sherwin et al. 2012; Xie et al. 2013; Han et al. 2014; Lin et al. 2014; Read et al. 2014; Ramessur et al. 2015; Saxena et al. 2015; Wen et al. 2015) suggested that outdoor activities have a protective effect against myopia, of which two (Tan et al. 2000; Wen et al. 2015) studies did not demonstrate a statistically significant association and four studies (Saw et al. 2001, 2002; Zhang et al. 2010; Cheng et al. 2013) did not observe any relationship between outdoor activities and myopia.
Myopic Shift in refractive error
A total of five cohort studies (Parssinen & Lyyra 1993; Guo et al. 2013; Parssinen et al. 2014; Scheiman et al. 2014; Wu et al. 2015) that investigated the association between outdoor time and a myopic shift in refractive error were excluded. Two of these studies investigated myopic shift in refraction in the overall sample (Guo et al. 2013; Wu et al. 2015). Increased time outdoors was reported to be significantly associated with less myopic shift in these two studies. The remaining three studies investigated myopic shift in refraction in baseline myopes (Parssinen & Lyyra 1993; Parssinen et al. 2014; Scheiman et al. 2014), which was deemed as myopic progression. No association between time outdoors and myopic progression was observed in study by Scheiman et al. (2014). The two studies carried out by Pärssinen et al. shared the same baseline participants, with an additional 20‐year follow‐up period in the most recent study (Parssinen & Lyyra 1993; Parssinen et al. 2014). Although a slower rate of myopic progression was observed among the participants who spent increased time outdoors, a protective effect of outdoor time for myopic progression could not be determined because significant correlations were also observed between the amounts of outdoor, reading and TV times during childhood and adulthood.
Discussion
The pooled results of this systematic review and meta‐analysis demonstrate a protective effect of outdoor time for the onset of myopia but not for myopic progression. The results include an additional six studies conducted since the analysis of Sherwin et al. (2012) but are in agreement with the previous analysis and show that outdoor time is protective for incident myopia (Sherwin et al. 2012). However, the dose–response analysis indicated that while an increase in the time spent outdoors could result in greater protection against myopia onset, it did not result in slowing the progression of myopia in eyes that were already myopic.
Our dose–response analysis indicated a curve linearity between increased time outdoors and the risk of myopia onset with a relatively good fit (R 2 = 0.586). Based on this association, an increase of approximately 76 min/day compared with control/baseline time spent outdoors is needed to obtain a 50% reduction in incident myopia. However, it should be noted that our analysis only considered studies wherein the increase in time outdoors ranged from 1 to 9.8 hr/week (Saw et al. 2006; French et al. 2013), and thus, protective effect of time outdoors if any beyond this upper limit remains to be determined. Also the threshold with respect to duration of time outdoors required to prevent myopia onset is unknown and requires further investigation (Jones et al. 2007; Rose et al. 2008a; French et al. 2013; Lin et al. 2014). Interestingly, even in those studies that failed to demonstrate a protective effect, children with myopia, on an average, spent less time outdoors compared with those without myopia. Lu et al. 2009 (Lu et al. 2009) reported an average of 6.0 versus 6.2 hr/week spent on outdoor activities in those with and without myopia, and Zhang et al. (2010) reported an average of 5.6 versus 5.7 hr in those with and without myopia, respectively.
High heterogeneity was observed among the studies, especially among the cross‐sectional studies. Sensitivity analyses suggested some possible sources of this heterogeneity. After excluding the RCT (He et al. 2015), the combined results of the two CCTs indicated a much stronger protective effect of outdoor time with lower heterogeneity (I 2 = 0%, p = 0.767). In the two CCTs, the intervention and control groups were from two nearby schools; thus, potential contamination may have occurred in relation to whether the children in the intervention group had asked their friends in the control group to go outside to play together during recess (Wu et al. 2013; Jin et al. 2015). In addition, the two CCTs had less hyperopic refraction at baseline. When the younger cohort was omitted, the pooled results for the remaining two older cohorts suggested a less protective effect against myopia when the children who spent an increased amount of time outdoors were compared to those who spent a decreased amount of time outdoors with lower heterogeneity (I 2 = 0%, p = 0.933). Following exclusion of the study conducted by Guo et al. (2013), the heterogeneity reduced significantly, with a reduction in the I 2 value from 93.2% to 39.8%. In the study by Guo et al., noncycloplegic autorefraction was adopted and noncycloplegic assessment of refractive status has been shown to result in an overestimation of the prevalence of myopia and misclassification of children with low hyperopia as myopia; thus, the protective effect of outdoor activities was likely overestimated (Hu et al. 2015; Morgan et al. 2015).
Subgroup analysis of the cross‐sectional studies did not find significant difference in protective effect of outdoor time for the onset of myopia between different age groups and different prevalence of myopia. However, it should be noted that the number of comparisons is fewer for ages <6 and >18 years and for prevalence <20% and >80%; thus, this finding needs to be confirmed in other studies. On the other hand, subgroup analysis of cohort studies indicated a stronger protective effect of outdoor activities in children aged 6 years compared with kids aged 11 to 12 years. It is well known that the various ocular components undergo growth and maturation in younger children, and thus, the ocular growth patterns may be more sensitive to environmental influences including outdoor time during this period.
Our analysis also investigated a myopic shift in refraction of the entire population (i.e. considering both myopes and nonmyopes), and the pooled results from the clinical trials considered in the meta‐analysis demonstrated that outdoor time was protective against a myopic shift in refractive error. From the trials that were considered for the meta‐analysis, He et al. (2015) did not investigate the preventive effect of outdoor activities on baseline myopes because the prevalence of myopia was too low at baseline. Wu et al. (2013) have shown that participation in outdoor activities during recess has a significant effect on myopic shift in nonmyopic children but not in myopic children.
Given the above, it appears that outdoor time had a greater effect on nonmyopic than on myopic eyes. Indeed, when our analysis considered studies that included only myopic children, no significant association between outdoor time and a myopic shift in myopia was seen (Parssinen & Lyyra 1993; Saw et al. 2000; Jones‐Jordan et al. 2012; Parssinen et al. 2014; Scheiman et al. 2014; Li et al. 2015; Oner et al. 2015), with the exception of one clinical trial (Yi & Li 2011). In this clinical trial, the children in the intervention group were instructed to participate in less near‐ and middle‐vision activities and more outdoor activities; thus, it may be that the significant difference in myopic progression might be due to a combined effect of outdoor and near‐vision activities rather than an effect of outdoor activities alone. These findings form the basis of an important public health message, as increasing the time spent outdoors was found to be limited to preventing myopia onset and myopic shift among the children who were not yet myopic.
Questionnaires were frequently used for evaluation of the time spent outdoors, but they represent a potential source of error due to inaccurate reporting or recall bias of participants. Although questionnaires such as the multi‐item questionnaire developed for the Sydney Myopia Study are reproducible and sufficiently robust to detect the effects of time spent outdoors on the development of myopia (Rose et al. 2008; French et al. 2013), they need to be validated against more objective measures, such as data obtained using wearable detectors, including HOBO light metres (Dharani et al. 2012), actigraphy devices (Read et al. 2014, 2015) and systems based on GPS (Tandon et al. 2013). Biomarkers such as vitamin D (Guggenheim et al. 2014; Tideman et al. 2016) and conjunctival UVAF (Sherwin et al. 2012; Sherwin et al. 2012) have also been investigated as objective measures of sunlight exposure, although the relationship between sun exposure and UVAF is currently unclear.
Our review has several limitations. First, the heterogeneity was high among the studies, especially the cross‐sectional studies. This high heterogeneity is possibly reflective of the differences in the study designs, age and ethnicities of the study populations. However, despite the high heterogeneity, a protective effect of outdoor time for myopia onset was established in the majority of studies. Secondly, dose–response analysis of myopia onset in our review only suggested the existence of an inverse nonlinear relationship with increased time outdoors and myopia onset; however, the threshold or the amount of time outdoors required to reduce the incidence of myopia remains to be determined. Finally, conversion of the original effect estimates based on hours of exposure per day to estimates based on hours of exposure per week might have potentially resulted in a bias as the time spent outdoors could have varied between weekdays versus weekends, and such information was available from a limited number of studies (Dirani et al. 2009; Deng et al. 2010; Low et al. 2010; Guggenheim et al. 2012; Guo et al. 2013; Zhou et al. 2015).
In conclusion, this meta‐analysis demonstrates a protective effect of improved outdoor time for onset but not progression of myopia. These findings indicate that (1) further research is required to confirm and determine the reasons for outdoor time not being effective for myopic progression; and (2) there is a need to determine the optimal duration and strategy to implement outdoor time as an intervention to control or delay the onset of myopia.
This work was supported by three‐year action programme of Shanghai Municipality for strengthening the construction of the public health system (2015–2017) (Grant no. GWIV‐13.2), National Natural Science Foundation of China for Young Staff (Grant no. 81402695), Key Discipline of Public Health – Eye health in Shanghai (Grant No. 15GWZK0601), Overseas High‐end Research Team – Eye health in Shanghai and Brien Holden Vision Institute, Sydney, Australia.
References
- Bar Dayan Y, Levin A, Morad Y et al. (2005): The changing prevalence of myopia in young adults: a 13‐year series of population‐based prevalence surveys. Invest Ophthalmol Vis Sci 46: 2760–2765. [DOI] [PubMed] [Google Scholar]
- Berntsen DA, Sinnott LT, Mutti DO & Zadnik K (2012): A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci 53: 640–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Cheung SW & Cho P (2013): Myopia control using toric orthokeratology (TO‐SEE study). Invest Ophthalmol Vis Sci 54: 6510–6517. [DOI] [PubMed] [Google Scholar]
- Cheng CY, Huang W, Su KC, Peng ML, Sun HY & Cheng HM (2013): Myopization factors affecting urban elementary school students in Taiwan. Optom Vis Sci 90: 400–406. [DOI] [PubMed] [Google Scholar]
- Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A & Tan D (2012): Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology 119: 347–354. [DOI] [PubMed] [Google Scholar]
- Chia A, Lu QS & Tan D (2016): Five‐year clinical trial on atropine for the treatment of myopia 2: myopia control with Atropine 0.01% Eyedrops. Ophthalmology 123: 391–399. [DOI] [PubMed] [Google Scholar]
- Chinn S (2000): A simple method for converting an odds ratio to effect size for use in meta‐analysis. Stat Med 19: 3127–3131. [DOI] [PubMed] [Google Scholar]
- Cho P & Cheung SW (2012): Retardation of myopia in Orthokeratology (ROMIO) study: a 2‐year randomized clinical trial. Invest Ophthalmol Vis Sci 53: 7077–7085. [DOI] [PubMed] [Google Scholar]
- Chua SY, Ikram MK, Tan CS et al. (2015): Relative contribution of risk factors for early‐onset myopia in young Asian children. Invest Ophthalmol Vis Sci 56: 8101–8107. [DOI] [PubMed] [Google Scholar]
- Deng L, Gwiazda J & Thorn F (2010): Children's refractions and visual activities in the school year and summer. Optom Vis Sci 87: 406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharani R, Lee CF, Theng ZX et al. (2012): Comparison of measurements of time outdoors and light levels as risk factors for myopia in young Singapore children. Eye (Lond) 26: 911–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirani M, Tong L, Gazzard G et al. (2009): Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol 93: 997–1000. [DOI] [PubMed] [Google Scholar]
- Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL 3rd & Holden BA (2012): Myopia progression rates in urban children wearing single‐vision spectacles. Optom Vis Sci 89: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs SH & Black N (1998): The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health 52: 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flitcroft DI (2012): The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 31: 622–660. [DOI] [PubMed] [Google Scholar]
- French AN, Ashby RS, Morgan IG & Rose KA (2013a): Time outdoors and the prevention of myopia. Exp Eye Res 114: 58–68. [DOI] [PubMed] [Google Scholar]
- French AN, Morgan IG, Mitchell P & Rose KA (2013b): Patterns of myopigenic activities with age, gender and ethnicity in Sydney schoolchildren. Ophthalmic Physiol Opt 33: 318–328. [DOI] [PubMed] [Google Scholar]
- French AN, Morgan IG, Mitchell P & Rose KA (2013c): Risk factors for incident myopia in Australian schoolchildren: The Sydney Adolescent Vascular and Eye Study. Ophthalmology 120: 2100–2108. [DOI] [PubMed] [Google Scholar]
- Greenland S & Longnecker MP (1992): Methods for trend estimation from summarized dose‐response data, with applications to meta‐analysis. Am J Epidemiol 135: 1301–1309. [DOI] [PubMed] [Google Scholar]
- Guggenheim JA, Northstone K, McMahon G, Ness AR, Deere K, Mattocks C, Pourcain BS & Williams C (2012): Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci 53: 2856–2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guggenheim JA, Williams C, Northstone K, Howe LD, Tilling K, St Pourcain B, McMahon G & Lawlor DA (2014): Does vitamin D mediate the protective effects of time outdoors on myopia? Findings from a prospective birth cohort. Invest Ophthalmol Vis Sci 55: 8550–8558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, Meng M & Jonas JB (2013a): Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 120: 277–283. [DOI] [PubMed] [Google Scholar]
- Guo Y, Liu LJ, Xu L, Tang P, Lv YY, Feng Y, Meng M & Jonas JB (2013b): Myopic shift and outdoor activity among primary school children: one‐year follow‐up study in Beijing. PLoS ONE 8: e75260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo K, Yang DY, Wang Y et al. (2015): Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert children eye study. Invest Ophthalmol Vis Sci 56: 1769–1774. [DOI] [PubMed] [Google Scholar]
- Han X, Miao HL & Huang D (2014): Investigation of junior school student myopia in high‐altitude Tibetan areas in Qinghai Province. Int Eye Sci 14: 913–915. [Google Scholar]
- Hasebe S, Ohtsuki H, Nonaka T, Nakatsuka C, Miyata M, Hamasaki I & Kimura S (2008): Effect of progressive addition lenses on myopia progression in Japanese children: a prospective, randomized, double‐masked, crossover trial. Invest Ophthalmol Vis Sci 49: 2781–2789. [DOI] [PubMed] [Google Scholar]
- He M, Xiang F, Zeng Y et al. (2015): Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA 314: 1142–1148. [DOI] [PubMed] [Google Scholar]
- Holden BA, Fricke TR, Wilson DA et al. (2016): Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123: 1036–1042. [DOI] [PubMed] [Google Scholar]
- Hu YY, Wu JF, Lu TL, Wu H, Sun W, Wang XR, Bi HS & Jonas JB (2015): Effect of cycloplegia on the refractive status of children: the Shandong children eye study. PLoS ONE 10: e0117482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Wen D, Wang Q et al. (2016): Efficacy comparison of 16 interventions for myopia control in children: a network meta‐analysis. Ophthalmology 123: 697–708. [DOI] [PubMed] [Google Scholar]
- Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ & Mitchell P (2008): Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci 49: 2903–2910. [DOI] [PubMed] [Google Scholar]
- Jin JX, Hua WJ, Jiang X et al. (2015): Effect of outdoor activity on myopia onset and progression in school‐aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol 15: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML & Zadnik K (2007): Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci 48: 3524–3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones‐Jordan LA, Mitchell GL, Cotter SA et al. (2011): Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci 52: 1841–1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones‐Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, Twelker JD & Zadnik K (2012): Time outdoors, visual activity, and myopia progression in juvenile‐onset myopes. Invest Ophthalmol Vis Sci 53: 7169–7175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YY, Lo CT, Sheu SJ & Yin LT (2015): Risk factors for and progression of myopia in young Taiwanese men. Ophthalmic Epidemiol 22: 66–73. [DOI] [PubMed] [Google Scholar]
- Li SM, Li H, Li SY et al. (2015): Time outdoors and myopia progression over 2 years in chinese children: the Anyang childhood eye study. Invest Ophthalmol Vis Sci 56: 4734–4740. [DOI] [PubMed] [Google Scholar]
- Lin LL, Shih YF, Hsiao CK & Chen CJ (2004): Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore 33: 27–33. [PubMed] [Google Scholar]
- Lin Z, Vasudevan B, Jhanji V et al. (2014): Near work, outdoor activity, and their association with refractive error. Optom Vis Sci 91: 376–382. [DOI] [PubMed] [Google Scholar]
- Low W, Dirani M, Gazzard G et al. (2010): Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol 94: 1012–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu B, Congdon N, Liu X et al. (2009): Associations between near work, outdoor activity, and myopia among adolescent students in rural China: the Xichang Pediatric Refractive Error Study report no. 2. Arch Ophthalmol 127: 769–775. [DOI] [PubMed] [Google Scholar]
- Ma MM, Zhang ZW, Song JG, Wang XC, Zhang YM & Bi‐Lian KE (2010): An epidemiological survey of refractive error and associated factors among middle school students in Deqing County of Zhejiang Province, China. Fudan Univ J Med Sci 37: 680–684. [Google Scholar]
- Marcus MW, de Vries MM, Junoy Montolio FG & Jansonius NM (2011): Myopia as a risk factor for open‐angle glaucoma: a systematic review and meta‐analysis. Ophthalmology 118: 1989–1994. e1982. [DOI] [PubMed] [Google Scholar]
- Morgan I & Rose K (2005): How genetic is school myopia? Prog Retin Eye Res 24: 1–38. [DOI] [PubMed] [Google Scholar]
- Morgan IG, Ohno‐Matsui K & Saw SM (2012): Myopia. Lancet 379: 1739–1748. [DOI] [PubMed] [Google Scholar]
- Morgan IG, Iribarren R, Fotouhi A & Grzybowski A (2015): Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol 93: 581–585. [DOI] [PubMed] [Google Scholar]
- Mutti DO, Mitchell GL, Moeschberger ML, Jones LA & Zadnik K (2002): Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci 43: 3633–3640. [PubMed] [Google Scholar]
- Onal S, Toker E, Akingol Z, Arslan G, Ertan S, Turan C & Kaplan O (2007): Refractive errors of medical students in Turkey: one year follow‐up of refraction and biometry. Optom Vis Sci 84: 175–180. [DOI] [PubMed] [Google Scholar]
- Oner V, Bulut A, Oruc Y & Ozgur G (2015): Influence of indoor and outdoor activities on progression of myopia during puberty. Int Ophthalmol 36: 121–125. [DOI] [PubMed] [Google Scholar]
- Orsini N, Bellocco R & Greenland S (2006): Generalized least squares for trend estimation of summarized dose–response data. STATA J 6: 40–57. [Google Scholar]
- Pan CW, Chen Q, Sheng X et al. (2015): Ethnic variations in myopia and ocular biometry among adults in a rural community in China: the yunnan minority eye studies. Invest Ophthalmol Vis Sci 56: 3235–3241. [DOI] [PubMed] [Google Scholar]
- Parssinen O & Lyyra AL (1993): Myopia and myopic progression among schoolchildren: a three‐year follow‐up study. Invest Ophthalmol Vis Sci 34: 2794–2802. [PubMed] [Google Scholar]
- Parssinen O, Kauppinen M & Viljanen A (2014): The progression of myopia from its onset at age 8‐12 to adulthood and the influence of heredity and external factors on myopic progression. A 23‐year follow‐up study. Acta Ophthalmol 92: 730–739. [DOI] [PubMed] [Google Scholar]
- Pascolini D & Mariotti SP (2011): Global estimates of visual impairment: 2010. Br J Ophthalmol 96: 614–618. [DOI] [PubMed] [Google Scholar]
- Peckham CS, Gardiner PA & Goldstein H (1977): Acquired myopia in 11‐year‐old children. Br Med J 1: 542–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramessur R, Williams KM & Hammond CJ (2015): Risk factors for myopia in a discordant monozygotic twin study. Ophthalmic Physiol Opt 35: 643–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read SA, Collins MJ & Vincent SJ (2014): Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci 91: 330–341. [DOI] [PubMed] [Google Scholar]
- Read SA, Collins MJ & Vincent SJ (2015): Light exposure and eye growth in childhood. Invest Ophthalmol Vis Sci 56: 6779–6787. [DOI] [PubMed] [Google Scholar]
- Resnikoff S, Pascolini D, Mariotti SP & Pokharel GP (2008): Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ 86: 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W & Mitchell P (2008a): Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115: 1279–1285. [DOI] [PubMed] [Google Scholar]
- Rose KA, Morgan IG, Smith W, Burlutsky G, Mitchell P & Saw SM (2008b): Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol 126: 527–530. [DOI] [PubMed] [Google Scholar]
- Sankaridurg P, Holden B, Smith E 3rd et al. (2011): Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one‐year results. Invest Ophthalmol Vis Sci 52: 9362–9367. [DOI] [PubMed] [Google Scholar]
- Saw SM, Nieto FJ, Katz J, Schein OD, Levy B & Chew SJ (2000): Factors related to the progression of myopia in Singaporean children. Optom Vis Sci 77: 549–554. [DOI] [PubMed] [Google Scholar]
- Saw SM, Hong RZ, Zhang MZ, Fu ZF, Ye M, Tan D & Chew SJ (2001): Near‐work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus 38: 149–155. [DOI] [PubMed] [Google Scholar]
- Saw SM, Zhang MZ, Hong RZ, Fu ZF, Pang MH & Tan DT (2002): Near‐work activity, night‐lights, and myopia in the Singapore‐China study. Arch Ophthalmol 120: 620–627. [DOI] [PubMed] [Google Scholar]
- Saw SM, Shankar A, Tan SB, Taylor H, Tan DT, Stone RA & Wong TY (2006): A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci 47: 1839–1844. [DOI] [PubMed] [Google Scholar]
- Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Menon V & Mani K (2015): Prevalence of myopia and its risk factors in urban school children in Delhi: the North India Myopia Study (NIM Study). PLoS ONE 10: e0117349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheiman M, Zhang Q, Gwiazda J, Hyman L, Harb E, Weissberg E, Weise KK & Dias L (2014): Visual activity and its association with myopia stabilisation. Ophthalmic Physiol Opt 34: 353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwin JC, Hewitt AW, Coroneo MT, Kearns LS, Griffiths LR & Mackey DA (2012a): The association between time spent outdoors and myopia using a novel biomarker of outdoor light exposure. Invest Ophthalmol Vis Sci 53: 4363–4370. [DOI] [PubMed] [Google Scholar]
- Sherwin JC, McKnight CM, Hewitt AW, Griffiths LR, Coroneo MT & Mackey DA (2012b): Reliability and validity of conjunctival ultraviolet autofluorescence measurement. Br J Ophthalmol 96: 801–805. [DOI] [PubMed] [Google Scholar]
- Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, MacKey DA & Foster PJ (2012c): The association between time spent outdoors and myopia in children and adolescents: A systematic review and meta‐analysis. Ophthalmology 119: 2141–2151. [DOI] [PubMed] [Google Scholar]
- Tan GJ, Ng YP, Lim YC, Ong PY, Snodgrass A & Saw SM (2000): Cross‐sectional study of near‐work and myopia in kindergarten children in Singapore. Ann Acad Med Singapore 29: 740–744. [PubMed] [Google Scholar]
- Tandon PS, Saelens BE, Zhou C, Kerr J & Christakis DA (2013): Indoor versus outdoor time in preschoolers at child care. Am J Prev Med 44: 85–88. [DOI] [PubMed] [Google Scholar]
- Tideman JW, Polling JR, Voortman T et al. (2016): Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur J Epidemiol 31: 491–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale S, Sperduto RD & Ferris FL 3rd (2009): Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol 127: 1632–1639. [DOI] [PubMed] [Google Scholar]
- Walline JJ, Greiner KL, McVey ME & Jones‐Jordan LA (2013): Multifocal contact lens myopia control. Optom Vis Sci 90: 1207–1214. [DOI] [PubMed] [Google Scholar]
- Wen XF, Zhang J & Zhao Y (2015): Analysis of poor vision conditions and risk factors of myopia in primary school He'xi district of Sanya. Int Eye Sci 15: 684–686. [Google Scholar]
- Wu PC, Tsai CL, Hu CH & Yang YH (2010): Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol 17: 338–342. [DOI] [PubMed] [Google Scholar]
- Wu PC, Tsai CL, Wu HL, Yang YH & Kuo HK (2013): Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 120: 1080–1085. [DOI] [PubMed] [Google Scholar]
- Wu LJ, Wang YX, You QS et al. (2015): Risk factors of myopic shift among primary school children in Beijing, China: a prospective study. Int J Med Sci 12: 633–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie HL, Xie ZK, Zhou F & Hu L (2013): [Myopia prevalence and influencing factor analysis of primary and middle school students in our country]. Zhonghua yi xue za zhi 93: 999–1002. [PubMed] [Google Scholar]
- Yi JH & Li RR (2011): [Influence of near‐work and outdoor activities on myopia progression in school children]. Zhongguo Dang Dai Er Ke Za Zhi 13: 32–35. [PubMed] [Google Scholar]
- Zadnik K, Sinnott LT, Cotter SA et al. (2015): Prediction of juvenile‐onset myopia. JAMA Ophthalmol 133: 683–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J & Yu KF (1998): What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280: 1690–1691. [DOI] [PubMed] [Google Scholar]
- Zhang M, Li L, Chen L et al. (2010): Population density and refractive error among Chinese children. Invest Ophthalmol Vis Sci 51: 4969–4976. [DOI] [PubMed] [Google Scholar]
- Zhou R, Zhang WF, Yang Y, Li YT, Zhang J & Wang WP (2014): Analysis of myopia prevalence and influencing factors among primary school students in the urban area of Lanzhou city. Int Eye Sci 14: 903–907. [Google Scholar]
- Zhou Z, Morgan IG, Chen Q, Jin L, He M & Congdon N (2015): Disordered sleep and myopia risk among Chinese children. PLoS ONE 10: e0121796. [DOI] [PMC free article] [PubMed] [Google Scholar]


