Abstract
Objectives
Rising demand for emergency and urgent care services is well documented, as are the consequences, for example, emergency department (ED) crowding, increased costs, pressure on services, and waiting times. Multiple factors have been suggested to explain why demand is increasing, including an aging population, rising number of people with multiple chronic conditions, and behavioral changes relating to how people choose to access health services. The aim of this systematic mapping review was to bring together published research from urgent and emergency care settings to identify drivers that underpin patient decisions to access urgent and emergency care.
Methods
Systematic searches were conducted across Medline (via Ovid SP), EMBASE (via Ovid), The Cochrane Library (via Wiley Online Library), Web of Science (via the Web of Knowledge), and the Cumulative Index to Nursing and Allied Health Literature (CINAHL; via EBSCOhost). Peer‐reviewed studies written in English that reported reasons for accessing or choosing emergency or urgent care services and were published between 1995 and 2016 were included. Data were extracted and reasons for choosing emergency and urgent care were identified and mapped. Thematic analysis was used to identify themes and findings were reported qualitatively using framework‐based narrative synthesis.
Results
Thirty‐eight studies were identified that met the inclusion criteria. Most studies were set in the United Kingdom (39.4%) or the United States (34.2%) and reported results relating to ED (68.4%). Thirty‐nine percent of studies utilized qualitative or mixed research designs. Our thematic analysis identified six broad themes that summarized reasons why patients chose to access ED or urgent care. These were access to and confidence in primary care; perceived urgency, anxiety, and the value of reassurance from emergency‐based services; views of family, friends, or healthcare professionals; convenience (location, not having to make appointment, and opening hours); individual patient factors (e.g., cost); and perceived need for emergency medical services or hospital care, treatment, or investigations.
Conclusions
We identified six distinct reasons explaining why patients choose to access emergency and urgent care services: limited access to or confidence in primary care; patient perceived urgency; convenience; views of family, friends, or other health professionals; and a belief that their condition required the resources and facilities offered by a particular healthcare provider. There is a need to examine demand from a whole system perspective to gain better understanding of demand for different parts of the emergency and urgent care system and the characteristics of patients within each sector.
The trend of increasing annual demand for emergency and urgent care is consistent across both developed countries and different providers of emergency and urgent care. Studies from the United States, Canada, the United Kingdom, and Australia report that demand for emergency department (ED) care is increasing by as much as 3% to 6% each year.1, 2, 3, 4, 5 In the United States, ED attendance increased from 34.1% to 40.5% per 100 persons between 1996 and 20066 and in England demand has doubled from an estimated 6.8 million ED attenders in 1966 and 19677 to 13.6 million in 2006 and 2007, with a further increase to 14.3 million in 2012 and 2013.7 Demand for urgent care center services in the United Kingdom has also grown, with attendances increasing by 46% between 2006 and 2013.7 In addition, demand for prehospital emergency services has risen dramatically over the past 20 years, rising in England by 125%, from around 4 million calls in 1994 and 1995 to 9 million ambulance calls in 2014 and 20158 and in the U.S. emergency medical services (EMS) transports have risen from 16,000,000 in 2006 to 28,004,624 in 2009.9, 10
The impact of increased demand for emergency and urgent care is well known and includes issues such as ED crowding, increased costs, longer waiting times, and overstretched services. ED crowding has been a recognized problem in the United States since the mid‐1980s,3, 11 occurs in most developed countries,12, 13, 14, 15 and is described as a “worldwide public health problem.”16 Increased demand for services also results in increased service provision costs. For example, in the United Kingdom demand for ambulance services rises annually by 6.5% and increases costs annually by £60 million ($85 million).17
Published literature suggests that some of the increase in demand is attributable to people with primary care problems who use emergency and urgent care services to access care,18 and some studies suggest that large proportions of patients (10%–60%) can be managed using lower‐acuity‐care services.19 However, this is not the only reason and factors contributing to increased demand for emergency and urgent care are often complex and multifactorial. Several studies report that increased demand for emergency and urgent care services is due to a proportionate rise of older people in the population who may have different and more complex care needs.20, 21 Other studies have reported that patients bypass their primary care physician (PCP; also known as a general practitioner [GP]) and instead go directly to urgent or emergency care,22 particularly for out‐of‐hours care and in urban centers.23 Factors such as perceived superior treatment at hospitals,18 lack of access to other care,24 a belief that the problem was serious enough to warrant emergency treatment,24 and lack of awareness of other services19 have all been reported as potential reasons why people choose emergency and urgent care and thus may all impact on why demand for these services is continually increasing. The aim of this study was to systematically review the related literature and, using narrative synthesis, to identify the factors behind patient decisions to access urgent and emergency care, including why patients access emergency and urgent care and how and why they choose which service to access.
Methods
Study Design
This review was one of five linked reviews undertaken by our Evidence Synthesis Center to examine the effectiveness of different models of delivering urgent care.25 The Evidence Synthesis Center provides rapid evidence synthesis about relevant health issues and evidence gaps to the U.K. National Institute for Health Research (NIHR). This information is used to inform calls for new research. A timeline of 6 months was given by NIHR for the Evidence Synthesis Center to complete five separate but interlinked reviews around emergency and urgent care, and this paper presents one of the reviews. The review reported here explores patient's reasons for choosing emergency and urgent care.
We were required to provide answers to the research commissioner (NIHR) within a time scale that was prohibitive to a full systematic review. The short time frame and vast scope of the review subject area lends itself to rapid review methods, to efficiently identify and synthesize the most relevant evidence within the study time frame. A rapid review is defined as “a type of knowledge synthesis in which components of the systematic review process are simplified or omitted to produce information in a short period of time,”26 for example, by limiting inclusion by date or language and reporting results narratively.27 Rapid reviews have been described as a “streamlined alternative to standard systematic reviews”28 and a key use of this type of review is to provide summary evidence in an environment where health service delivery decisions need to be made quickly and not within the time frames of traditional reviews. They also provide a format that makes evidence accessible for decision makers and are a valuable way of supporting evidenced‐based decision making.28
The type of review undertaken here can also be described as a mapping review. Mapping reviews are typically used to map, summarize, and categorize broad research bases, particularly with the intention of identifying evidence gaps and are defined as “a systematic search of a broad field to identify gaps in knowledge and/or future research needs.”29 Mapping reviews are frequently used within policy development and health services research.30 The review reported here used a systematic search strategy. However, other stages of the review are typologically different from a traditional systematic review method. For example, we did not attempt to intensively identify all applicable evidence, but instead utilized structured searches to identify key evidence. Findings were reported qualitatively using a framework‐based narrative synthesis.31
Literature Search and Selection
Database Searches
Search terms were developed based on discussions with the research team, which included an information specialist (AC). Where possible, we identified similar reviews and expanded preexisting search strategies to meet the broad remit of this search. We combined relevant terms relating to the following: population; users of the range of services within the emergency and urgent care system (ambulance services, ED, other urgent care facilities, telephone access services, primary care‐based urgent care services); outcomes; service effects—ED attendances, emergency admissions, ambulance calls, dispatches or transports, demand, appropriateness of level of care, cost consequences; and patient outcomes—patient experience and satisfaction, decision making, adverse events, and cost impact.
An information specialist (AC) conducted targeted database searches using the following databases: Medline (via Ovid SP), EMBASE (via Ovid), The Cochrane Library (via Wiley Online Library), Web of Science (via the Web of Knowledge), and the Cumulative Index to Nursing and Allied Health Literature (CINAHL; via EBSCOhost). Searches were initially limited to January 1, 1995, to December 2014 and were updated to April 2016 to ensure that current findings are included in the analysis and that results are relevant to current services. We used a combination of free‐text and medical subject headings (MeSH) search terms, as well as appropriate subheadings. Keywords related to emergency and urgent care services; health service demand; factors, for example, crowding or aging; and rising demand and were combined using BOOLEAN logic. Search results were limited to English‐language papers published from 1995. A detailed description of the search strategy is provided in Data Supplement S1 (available as supporting information in the online version of this paper, which is available at https://doi.org/onlinelibrary.wiley.com/doi/10.1111/acem.13220/full). Search results were downloaded into EndNote version X7.2.1 (Thomson Reuters).Other key evidence was identified through the following supplementary searching methods: examining reference lists of relevant systematic reviews; using our own extensive archives of previous related research, including a number of related evidence reviews; an evidence review produced by NHS England as part of its review of urgent and emergency care;32 and consultation with internally based topic experts and some external topic experts.33
Inclusion Criteria
To manage the review process, we used the following broad inclusion criteria: empirical data; quantitative, qualitative, and mixed‐method studies; emergency or urgent care service users; written in English; report relevant outcomes (patient experiences and perspectives); peer‐review publications; and published between 1995 and 2016. We did not include studies that presented evidence relating to clinical interventions for specific conditions or specific condition–related studies, as these did not fit with the whole‐service, whole‐population perspective of this review. However, where evidence was presented for broad population groups, for example, children or the elderly, these were included.
Study Selection
References were managed using Endnote version. After removal of duplicates, 1,724 remaining references were screened for relevance, using the title and abstract; 1,647 irrelevant papers were excluded at this stage and the most common reason for exclusion was lack of empirical evidence or publication type (editorial, letter, conference abstract, etc.). Where it was unclear if studies were relevant, the full‐text paper was obtained.
Seventy‐seven full‐text papers were reviewed for inclusion by one researcher (JT) and the results were discussed and confirmed with two other researchers (JC, DB); 38 papers were excluded at this stage. The most frequent reason for exclusion was not an empirical study (n = 14). Where additional input was required specific papers were discussed with the wider review team as part of regular project meetings.
Data Extraction
Results from 38 included studies were extracted directly into summary tables study by one reviewer (DB) and verified by a second reviewer (JC). Regular project meetings were held during this review stage and any differences in extracted data were reviewed and discussed to ensure consensus on extracted data items. Data were extracted using standardized predefined headings and included main purpose and objectives, key findings, and conclusions.
Data Analysis
A thematic mapping analysis was undertaken for all included papers, including those reporting survey and quantitative data.31 The thematic approach used in rapid reviews attempts to characterize the body of literature qualitatively rather than to quantify numbers of studies. This reduces the need to identify a comprehensive sample (as in a systematic review) as opposed to a representative sample which indicates the major trends without having to find all instances. Patient‐derived reasons for choosing emergency or urgent care service were identified and extracted from each included research paper and mapped against emerging themes by two reviewers (JT and JC). A qualitative‐based thematic analysis process was used to identify and code emerging themes, using methods similar to those used in qualitative framework analysis.34 Themes were reviewed and discussed with the study team and further refined and developed, until a final agreed coding framework was applied to the review findings, resulting in the identification of six themes that encompassed reported reasons for choosing emergency or urgent care services. We have narratively synthesized and reported data by theme. The narrative synthesis summarizes the findings from multiple studies using mainly words or text information.
Quality Assessment
Rapid reviews tend to be descriptive rather than analytical. For example, they prioritize the research questions that have been addressed rather than the results. This is one reason why approaches to quality assessment are less thorough. For example, study types are described rather than appraised. However, to ensure the conclusions of this research are based on robust evidence, we assessed the quality of studies using commonly used quality assessment tools. Fifteen qualitative interview or focus group studies were assessed using the Critical Appraisal Skills Programme Qualitative Checklist.35 This tool was chosen as it incorporates both broad and study‐specific quality issues and is a widely recognized quality assessment tool. Twenty‐three cross‐sectional studies were assessed using the National Institutes Health (NIH) Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies.36 We defined cross‐sectional studies as structured interviews, structured telephone interviews or surveys, or postal surveys that used statistical analysis methods. As no cohort studies were included in this review, we adapted the NIH tool to remove questions that primarily referred to quality issues in cohort studies.
Results
Search Results
We identified 38 individual studies relevant to this review. Search results are reported using Preferred Reporting Items for Systematic reviews and Meta‐analysis (PRISMA)37 in Figure 1. The main study characteristics are reported in Table 1. Complete summary tables of all included papers are available as Data Supplement S2 (available as supporting information in the online version of this paper, which is available at https://doi.org/onlinelibrary.wiley.com/doi/10.1111/acem.13220/full). Included studies were primarily concerned with patients presenting with urgent rather than emergency conditions.
Figure 1.
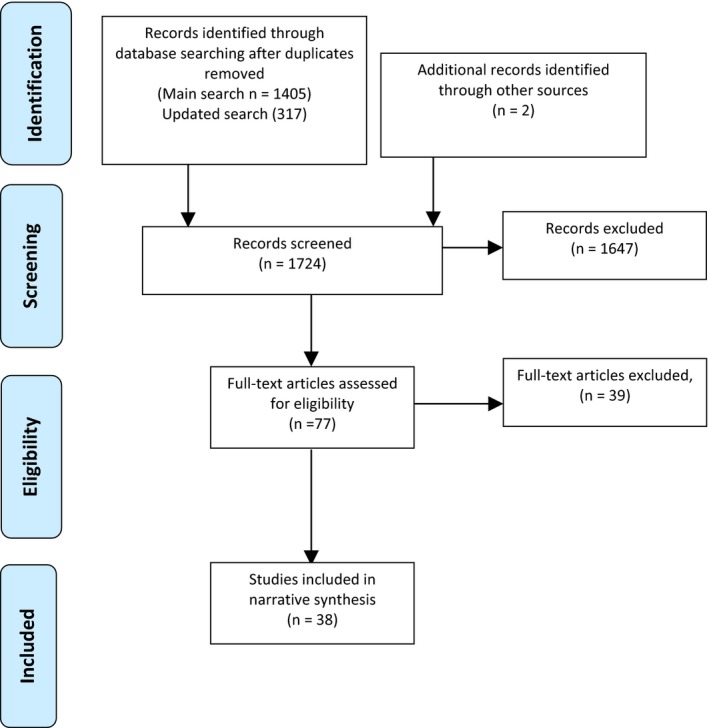
PRISMA 2009 flow diagram.
Table 1.
Characteristics of Included Studies
| Characteristics | Number of included studies, n (%) |
|---|---|
| Total | 38 (100) |
| Country | |
|
United States United Kingdom Other Europe Other |
13 (34.2) 15 (39.4) 4 (10.5) 6 (15.8) |
| Study design | |
|
Multiple qualitative (e.g., focus group and interviews) Mixed method (e.g., interviews and survey Focus group Patient interviews Cross‐sectional studies (e.g., survey or structured interviews) Secondary data analysis |
3 (7.9) 3 (7.9) 2 (5.3) 7 (18.4) 21 (46.2) 2 (5.3) |
| Setting | |
|
ED ED and urgent care centre or out of hours Ambulance Out‐of‐hours urgent Urgent care center Primary care/community based Hospital/ED |
26 (68.4) 3 (7.9) 2 (5.3) 2 (5.3) 1 (2.6) 3 (7.9) 1 (2.6) |
| Key themes | |
| Access to and confidence in primary care | 26/38 (68.4) |
| Perceived urgency and anxiety and the value of reassurance from emergency‐based services | 24/38 (63.1) |
| Views of family, friends, or healthcare professionals | 11/38 (28.9) |
| Convenience in terms of location, not having to make appointments, and opening hours | 15/38 (39.4) |
| Individual patient factors | 8/38 (21.5) |
| Perceived need for EMS or hospital care, treatment, or investigations | 13/38 (34.2) |
Study Quality and Relevance
All included studies were published in peer‐reviewed journals. Given that the main purpose of most studies was to identify patient‐derived factors or reasons for emergency and urgent care service use, the use of qualitative and cross‐sectional study designs was appropriate. The majority of studies were undertaken in the United States, United Kingdom, Australia, and Canada (n = 32/38; 84.2%), giving the data and results greater congruency due to the similarity of health systems. Most (n = 21; 52.6%) studies reported data relating to a single site or health facility. However, where data were reported within national surveys the results were consistent with those from single site studies.24 Quality assessment (see Data Supplement S3, available as supporting information in the online version of this paper, which is available at https://doi.org/onlinelibrary.wiley.com/doi/10.1111/acem.13220/full) identified that overall, the quality of included studies is high, but identified limitations with some study methodologies. Only 13 of the 23 cross‐sectional studies reported a sample size justification or power description or provided variance and effect estimates. It was not possible to calculate the response rate for one study, due to insufficient detail given.18 However, for the 22 studies that did provide this information, the mean response rate was 77% and the range was 45% to 99%. Only one study had a response rate lower than 50%.38 The 15 qualitative studies had fewer quality issues and overall the quality of included studies was high. Three studies did not provide sufficient information about ethical or research approvals and two studies lacked information about the considerations of the relationship between the research and the patient. Some studies used multiple methods incorporating a range of qualitative methods across whole populations, while others employed simpler designs with less comprehensive samples, for example, multisite studies using focus groups and interviews39 and multisite surveys24 compared to single‐site qualitative studies.18
Summary of Findings
A summary of the main characteristics of all included studies is given in Table 1.
Narrative Synthesis
We identified frequently occurring themes regarding patients’ decisions on where to access care and, in particular, why patients chose to access emergency or urgent care for nonurgent health problems. We identified six themes that accounted for the majority of the factors related to ED attendance and urgent care usage. Descriptions of each theme are outlined in Table 2.
Table 2.
Theme Descriptions
| Confidence in primary care and access to care appointments | Factors identified included lack of awareness of options (particularly OOH services), dissatisfaction with GPs, limited opening hours, anticipated waiting times for appointments, previous experience using OOH services, and perceived barriers. This theme encompasses service defined barriers to care, whereas the convenience theme is about patient defined barriers to care. |
| Perceived urgency, anxiety, and the value of reassurance from emergency‐based services | Self‐perceived urgency and reassurance from increased confidence in emergency and urgent healthcare providers. This theme is based on patient‐based anxieties rather than a desire for specific medical investigations. |
| Views of family, friends or healthcare professionals | Being advised to attend the ED by family, friends, or healthcare professionals. |
| Convenience | In terms of location, not having to make an appointment and opening hours was a factor. Older people were more likely to contact a GP first, whereas younger patients contacted urgent care centers, the ED, or OOH services, as they found this more convenient. This theme is about patient‐specific issues around access to care facilities and how these are viewed by population subgroups. |
| Individual patient factors | In some health systems, costs and transport options affected decision‐making. |
| Perceived need for EMS or hospital care, treatment, or investigations | A belief that their condition needed the resources offered by a hospital, including hospital doctors (rather than GPs), diagnostics (particularly radiography), and treatment. |
GP = general practitioner; OOH = out of hospital.
Confidence in Primary Care and Access to Appointments
Access to and confidence in primary care was a key factor identified by 26 studies and nearly all reported access related issues. In most studies patients had access to primary healthcare and chose instead to seek more urgent or emergency care, often without contacting a PCP first. There were multiple reasons why people felt accessing primary healthcare services was difficult. Anticipated waiting times for appointments and PCPs (including GPs) being busy were key factors,40, 41, 42 with one study reporting that 44% of patients found their GP “inaccessible to their needs.” This was also linked to patient perceptions around accessibility and availability of appointments at times of day that were convenient to patients,43 limited PCP opening hours,44 with a small proportion of patients reporting that they were unable to obtain a PCP appointment.38 Lack of primary health service available after hours was raised by one study.18 Another factor was lack of awareness of other services, with one study reporting that seven of 30 patients who attended ED had no knowledge of alternative primary care options.38 GP dissatisfaction influenced 10% of patients in their decision to attend an urgent care center39 and in some cases high rates of PCP dissatisfaction was reported.45 One study reported that patients felt that out‐of‐hours care was impersonal.46
There was evidence that different population groups had different views and used services differently and for different reasons. For example, older people were distrustful of telephone services and preferred to see a familiar PCP than to contact an out‐of‐hours service.47 Conversely, the study by Benger et al.48 identified younger people tended to choose emergency and urgent care over general practice. Young females were identified in a Brazilian study as being more likely to use ED inappropriately, due to lack of access to primary care services.49 Migrant populations often had no PCP and often sought ED care for nonurgent health problems due to difficulties accessing primary healthcare.50
Perceived Urgency Anxiety and the Value of Reassurance From Emergency‐based Services
Twenty‐four studies reported results categorized within this theme, with 14 of 24 studies reporting data from ED‐based studies. A key finding here was that patient anxiety was strongly related to healthcare‐seeking behavior51, 52 and this linked closely with the reassurance that patients obtain from emergency services53 and their trust of ED services.54 In some cases anxiety was due to worries about the legitimacy of need,39 with patients not wishing to use services inappropriately. There was a strong sense that patients viewed their conditions to be serious.40, 42, 43, 48, 55, 56, 57 This was juxtaposed with evidence that patients were not always capable of assessing which health problems required emergency care and were sometimes unsure of the legitimacy of their health needs.39, 58
While self‐perceived urgency is a strong theme within included studies, one study38 reported that 52% of ED attending patients described their condition as nonurgent, and 48% urgent, with no patients describing their problem as very urgent. Patients may also gain reassurance from having greater confidence in ED and hospital services, with 39% of patients stating that they had more confidence in their ED than in their PCP service22 and 24% believing that hospital treatment is superior.18
Perceived Need for EMS or Hospital Care, Treatment, or Investigations
Thirteen studies reported evidence categorized within this theme, with most reporting that patients believe that emergency or urgent care was required for their health problem. This often stems from a belief that their condition needs the resources offered by a hospital, including hospital doctors (rather than PCPs or GPs) and diagnostics particularly x‐rays and treatment.38, 43, 46, 59 Some patients felt that they were too sick to be seen within a primary care setting, with the study by Lobachova and colleagues57 reporting that 80% of patient felt that they were too ill to be seen and treated in primary care. Others felt that their condition was too difficult or complex for PCPs to control or could only be effectively dealt with by the ED.19, 55, 56 The study by Redstone et al.55 reported that 24% of patients who presented to ED with problems that were subsequently triaged as nonurgent attended the ED because they felt that they needed to be admitted to hospital.
Being Advised to Attend ED by Family Friends or Healthcare Professionals
The views of family, friends, and healthcare professionals were important contributory factors in patient decision making to utilize ED services in 11 of the included studies. Six studies reported that patients attended ED due to recommendations or referrals from other health professionals19, 38, 42, 54, 57, 60 and five studies identified that patients attended due to the views of family and friends,38, 40, 42, 57, 61 with some studies describing both family and friends and healthcare professionals advice as an explanatory factor. One study found that 52% of patients attended the ED due to advice from a healthcare professional or friends and family.38 A study by Hodgins and Wuest40 identified views of family and friends as one of the highest ranking explanatory factors behind ED attendance and Lobachova et al.57 found that while 35% of patients attended the ED due to being referred by other health professionals, 48% came due to advice from friends or family. The study by Penson et al.19 described the most common reason for attendance being advice from others, but this was more usually advice from health professionals rather than family or friends. One study identified that females were more likely to attend ED due to the recommendations of others than males61 and that the source of the advice was more likely to be family and friends.
Convenience in Terms of Location, Not Having to Make Appointment, and Opening Hours
The perceived convenience of emergency and urgent care services was a identified in 15 studies as a key driver in patient decision making, and this is also linked to negative views around inconvenient access to primary care. Access to primary care is often viewed as limited, due to more structured opening hours and perceptions around difficulty obtaining appointments, and there is a view that the ED is more convenient due to factors such as 24‐hour availability and not having to make an appointment.38, 43, 49, 55, 62 In one study, 60% of patients viewed the ED as more convenient than their PCP55 and several other studies reported that people chose to visit the ED for low‐urgency problems due to ED being closer or faster,63 the accessibility of the ED,43, 54 the convenience of the ED location,42 or service.40 Conversely, one study reported that patients attended the ED with primary care problems even though few people believed that they would be seen more quickly or that it was more convenient.19
Individual Patient Factors (e.g., Costs and Transport)
This theme also relates to the convenience and primary care access themes. In some health systems, costs and transport options affected decision making and these were identified as explanatory factors for choosing emergency and urgent care services in eight studies. Four studies (three from the United States and one from Australia) identified costs as an issue,57, 58, 60, 63 and in some cases reported that services users take into account the costs of using primary or EMS care when making decisions on which service to access.60 One study identified that 15% of urgent care center service users chose to access that particular service due to nonmandatory payment. Wilkin and colleagues58 reported that healthcare costs may prevent people from changing their current health‐seeking behavior.
Transportation issues, for example, not having a car, prompted some service users to choose the ED, ambulance, or urgent care services rather than primary care and this was identified by three studies.58, 60, 64 One study reported that 34% of patients chose to use the ambulance service instead of primary care due to not having a car.64 However, for some population groups there were barriers to using out‐of‐hours and ED services and this affected their choice of service. For example, older people faced specific barriers to using ED and urgent care services. In particular, traveling at night and using the telephone were factors that dissuaded older people from using out‐of‐hours services; instead they preferred to wait for an appointment with a familiar PCP. Campbell et al.41 found that out‐of‐hours decisions were often influenced by personal opinions around out‐of‐hours services and that trends differed between rural and urban areas, with people in rural areas often delaying contact until their own doctor was available, whereas people in urban areas were more likely to use out‐of‐hours emergency and urgent care services.
Discussion
We have identified six key themes that describe why patients choose to access emergency and urgent care instead of primary care for low‐urgency health problems. The themes are broad categories; each contain multiple and specific patient‐derived explanatory factors and are applicable to emergency and urgent care health systems in most developed countries.
The factors identified in the themes are supported by other research. For example, a qualitative interview study to identify which aspects of the emergency ambulance service care are valued by service users found that service users had high levels of anxiety and valued the reassurance that was provided by the ambulance service.65 This directly supports the theme identified from this research around “perceived urgency, anxiety and the value of reassurance from emergency based services.”
Perceptions of urgency may differ between patients and healthcare professionals. The study by Coleman et al.59 identified a discrepancy between patients’ perceptions of the seriousness of their health problem and related expectations of care and the views of healthcare professionals. This may lead to patients accessing care or treatment that is unnecessary due to a belief that the problem was serious and supports the theme “Perceived need for EMS or hospital care, treatment, or investigations.” However, identifying whether patients are choosing care inappropriately is difficult and sometimes controversial; many cases are retrospectively determined as nonurgent and there is often disagreement among health professionals about appropriateness.66 Even if there are more appropriate ways for patients to receive care this does not mean that it is inappropriate for patients to attend ED. Some studies have shown that some patients face anxiety about whether they are choosing the right level of care and do not wish to be categorized as time wasters.67 In particular, older people are sometimes reluctant to access emergency care perceive without first seeking the views of other people and this can be a barrier to seeking timely emergency and urgent care.48 In contrast, young adults are more likely to go to the ED or seek urgent care than contact their PCP and have lower satisfaction with primary care services.
Most studies reported that patients’ perceptions of access to and confidence in primary care was a key factor in low‐urgency ED attendances. Patient satisfaction with care is predictive of future healthcare choices68 and when patients experience difficulties obtaining appointments or are unsatisfied with the care they receive from their PCP, this may impact on future health‐seeking behavior and choices. Past research shows that patients with an urgent healthcare problem are unwilling to wait more than 1 day for an appointment with their own physician.69 Demand for unplanned services is rising and this has been shown to rise further when access to PCP care is reduced.70 A systematic review of primary care factors that impact on unscheduled secondary care use showed that better primary care access led to reduced unscheduled care,71 with increased access to primary care leading to a reduction in ED attendances. Many people also value the convenience of ED, not having to make an appointment, and access to specialist care if needed. Important drivers for ED use were identified using factor analysis by Ragin and colleagues72 and five factors were identified as having good reliability. These included convenience, belief that the problem was serious/medical necessity, preference for hospital facilities, and individual patient factors related to cost of care and insurance. Capp and colleagues73 examined in detail the impact of health insurance on ED usage and identified that lack of access to alternative care was a key driver for low‐acuity ED attendance. While Kangovi and colleagues74 also identified patients of low socioeconomic status prefer hospital care over primary care because they view it as more convenient and accessible whilst also providing higher quality care for less cost. A study about ED closures by Hsia et al.75 found that ED closures disproportionately affected vulnerable communities, for example, those without medical insurance, minority groups, or comorbidities. It may be that convenience and accessibility issues are more important to subgroups who already experience difficulties accessing care.
Multiple sources have identified the views and advice of others as a key driver in ED utilization. However, young people are reported as more likely to directly seek urgent care or attend ED76 and a criticism of some telephone‐based urgent care services is that advice can lead to a rise in ED attendances.77
As well as patient‐based factors, demand is likely to be influenced by a range of other characteristics and factors. These include aging populations with chronic conditions and complex health needs, socioeconomic factors often related to deprivation and lack of social support, and policy decisions around health planning and service provision, for example, access to primary care and geographical differences in provision. Future research to identify independent risk factors associated with accessing emergency and urgent care, as part of a population‐based whole‐system study, are required to identify and describe the sources and impact of demand on the emergency and urgent care system as a whole and to identify what demand is for different parts of the system and how these interact.
Limitations
This was a rapid review; therefore, some aspects of systematic review methodology have been omitted or simplified to produce a review in a short time frame.26 By limiting the evidence to 1995 to 2016, we have ensured that the evidence assessed has context and relevance to current policy and practice. In balancing the large scope of this review against the time and resource constraints, we aimed to provide a broad overview of existing evidence and utilized rapid review methods to structure the review process. For example, data extraction was focused toward the most pertinent evidence and information, rather than an exhaustive critique of all available information, and we used a framework‐based synthesis, which is an efficient method for synthesizing evidence to inform policy within short time scales.31
As part of the review search strategy, we excluded non–English‐language studies, gray literature, abstracts, and conference items. We excluded non–English‐language studies as papers not published in English are less likely be congruent to English and U.K. healthcare systems. As befits a systematic review of patient‐reported reasons for accessing emergency and urgent care, most of the evidence was from qualitative or survey‐based research. Each of these methods has its limitations and we undertook a quality assessment to ensure that the studies included in this review met accepted quality thresholds. For example, the mean survey response rate for included studies reporting survey data was >74%. This review examined empirical evidence that may help explain why demand for emergency and urgent care services is changing. Evidence was not assessed to identify or make recommendations regarding future services or optimum service configuration.
Research and Policy
Currently, most developed countries are exploring ways to reverse what is often termed as a “crisis in emergency medicine.”78 In particular, healthcare policy makers are examining methods to reduce ED crowding and medically unnecessary use of emergency and urgent services, while at the same time promoting methods to ensure that patients receive care from the most appropriate service. For example, in the United Kingdom, the NHS Five Year Forward View presents the case for redesigning current urgent and emergency care services.79 By understanding what drives patients with low‐urgency health problems to access emergency and urgent healthcare, this research will help policy makers to plan future ways of managing demand so that service provision works for patients, is sustainable, and helps people with urgent care needs access the right care first time.32
Conclusions
We identified six distinct reasons explaining why patients choose to access emergency and urgent care services, for mainly low‐urgency health problems. Limited access to or confidence in primary care; patient perceived urgency; convenience; views of family, friends, or other health professionals; and a belief that their condition required the resources and facilities offered by a particular healthcare provider were all key factors that influence patients when they make decisions about whether to access emergency and urgent care and the type of emergency and urgent care they choose. By understanding why more people are choosing to access these services we are better able to direct and provide patients with the right care at the right time. However, there is a need to examine demand from a whole‐system perspective and, in doing so, gain better understanding of demand for different parts of the emergency and urgent care system and the characteristics of patients within each sector.
Supporting information
Data Supplement S1. Search strategy.
Data Supplement S2. Summary tables of all included papers.
Data Supplement S3. Quality assessment of included studies.
Academic Emergency Medicine 2017;24:1137–1149.
An earlier version of this review formed part of a report to Health Services and Delivery Research (HS&DR). Turner J, Coster J, Chambers D, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3(43).
The study was funded as an independent research project by The National Institute for Health Research HS&DR Program grant number 13/05/12. The funders contributed to the development of the research questions to be addressed. The funders had no role in conducting the study, writing the paper or the decision to submit the paper for publication. The views expressed are those of the authors and do not necessarily reflect those of the NIHR Health Services and Delivery Research program or the Department of Health. The research was funded by the Health Services and Delivery Research (HS&DR) programme, which awarded ScHARR a HS&DR Evidence Synthesis Centre contract; ScHARR, the University of Sheffield; and salary support for staff at the University of Sheffield to undertake the research.
The authors have no potential conflicts to disclose.
[This article was modified on 25 August 2017 after initial publication to correct the copyright line.]
References
- 1. Lowthian JA, Curtis AJ, Jolley DJ, Stoelwinder JU, McNeil JJ, Cameron PA. Demand at the emergency department front door: 10‐year trends in presentations. Med J Aust 2012;196:128–32 [DOI] [PubMed] [Google Scholar]
- 2. Department of Health . Accident and Emergency Attendances (data for 1987–88 to 2009–10). Available at: http://webarchive.nationalarchives.gov.uk/20130107105354/ http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_077485Accessed May 2017.
- 3. Drummond AJ. No room at the inn: overcrowding in Ontario's emergency departments CJEM 2002;4:91–7. [DOI] [PubMed] [Google Scholar]
- 4. Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 Emergency Department Summary. Hyattsville, MD: National Center for Health Statistics, 2008. [PubMed] [Google Scholar]
- 5. Australian Institute of Health and Welfare . Australian Hospital Statistics 2009–10: Emergency Department Care and Elective Surgery Waiting Times. Canberra: AHIW, 2010. [Google Scholar]
- 6. Schappert SM, Rechtsteiner EA. Ambulatory Medical Care Utilization Estimates for 2006. National Health Statistics Reports, Number 8, 2008. [PubMed]
- 7. Nicholl J, Mason S. Return of the “corridors of shame”? BMJ 2013;346:F4343. [DOI] [PubMed] [Google Scholar]
- 8. Health and Social Care Information Centre (HSCIC) .Ambulance Services, England 2014‐15. 2015 . Available at: http://content.digital.nhs.uk/catalogue/PUB17722/ambu-serv-eng-2014-2015-rep.pdf Accessed Feb 8, 2016.
- 9. Emergency Medical Services at the Crossroads . Future of Emergency Care Series. Washington, DC: Institute of Medicine, 2001. [Google Scholar]
- 10. McCallion T. NASEMSO Survey Provides Snapshot of EMS Industry. 2011. Available at: http://www.jems.com/articles/2011/11/nasemso-survey-provides-snapshot-ems-ind.html Accessed Feb 8, 2016. [DOI] [PubMed]
- 11. Gallagher EJ, Lynn SG. The etiology of medical gridlock: causes of emergency department overcrowding in New York City. J Emerg Med 1990;8:785–90. [DOI] [PubMed] [Google Scholar]
- 12. He J, Hou XY, Toloo S, Patrick JR, Fitz Gerald G. Demand for hospital emergency departments: a conceptual understanding. World. J Emerg Med 2011;2:253–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Boyle P, Pineeault R, Roberge D. Assessing Quebecs's multicomponent program to reduce emergency room overcrowding. Can Public Policy 1992;18:189–202. [Google Scholar]
- 14. Derlet R, Richardson J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med 2001;8:151–5. [DOI] [PubMed] [Google Scholar]
- 15. Richardson LD, Asplin BR, Lowe RA. Emergency department overcrowding as a health policy issues: past development, future directions. Ann Emerg Med 2002;40:388–93. [DOI] [PubMed] [Google Scholar]
- 16. Di Somma S, Paladino L, Vaughan L, Lalle I, Magrini L, Magnanti M. Overcrowding in emergency department: an international issue. Intern Emerg Med 2015;10:171–5. [DOI] [PubMed] [Google Scholar]
- 17. Department of Health . Tackling Demand Together: A Toolkit for Improving Urgent and Emergency Care Pathways by Understanding Increases in 999 Demand. 2009. Available at: http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_106924.pdf Accessed Oct 2016.
- 18. Becker J, Dell A, Jenkins L, Sayed R. Reasons why patients with primary health care problems access a secondary hospital emergency centre. S Afr Med J 2012;102:800–1. [DOI] [PubMed] [Google Scholar]
- 19. Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department? Emerg Med J 2012;29:487–91. [DOI] [PubMed] [Google Scholar]
- 20. Lowthian JA, Jolley DJ, Curtis AJ, Currell A, Cameron PA, Stoelwinder JU. The challenges of population ageing: accelerating demand for emergency ambulance services by older patients, 1995‐2015. Med J Aust 2011;194:574–8. [DOI] [PubMed] [Google Scholar]
- 21. Leonard C, Bein KJ, Latt M, Muscatello D, Veillard AS, Dinh MM. Demand for emergency department services in the elderly: an 11 year analysis of the Greater Sydney Area. Emerg Med Australas 2014;26:356–60. [DOI] [PubMed] [Google Scholar]
- 22. Müller U, Winterhalder R, Businger A, Zimmermann H, Exadaktylos AK. Why do walk‐in patients prefer a busy urban emergency department during office hours? A pilot survey of 200 consecutive patients from Switzerland. Swiss Med Wkly 2012;142:w13565. [DOI] [PubMed] [Google Scholar]
- 23. Huber CA, Roseman T, Zoller M, Eichler K, Senn O. Out‐of‐hours demand in primary care: frequency, mode of contact and reasons for the encounter in Switzerland. J Eval Clin Pract 2011;17:174–9. [DOI] [PubMed] [Google Scholar]
- 24. Gindi RM, Black LI, Cohen RA. Reasons for emergency room use among U.S. adults aged 18‐64: national interview survey, 2013 and 2014. Natl Health Stat Rep 2016;(90):1–16. [PubMed] [Google Scholar]
- 25. Turner J, Coster J, Chambers D, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015. Nov. [PubMed] [Google Scholar]
- 26. Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst Rev 2012;1:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tricco AC, Antony J, Zarin W, et al. A scoping review of rapid review methods. BMC Med 2015;13:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Peterson K, Floyd N, Ferguson L, Christensen V, Helfand M. User survey finds rapid evidence reviews increase uptake of evidence by Veterans Health Administration leadership to inform fast‐paced health‐system decision‐making. Syst Rev 2016;5:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miake‐Lye IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev 2016;5:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Clapton J, Rutter D, Shariff N. SCIE Research Resource 03: SCIE Systematic Mapping Guidance (Draft) 2009. Available at: http://www.scie.org.uk/publications/researchresources/rr03.asp Accessed Feb 2017.
- 31. Dixon‐Woods M. Using framework‐based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. NHS England . High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England—Urgent and Emergency Care Review End of Phase 1 Report 2013. http://www.nhs.uk/NHSEngland/keoghreview/Documents/UECR.Ph1Report.FV.pdf (accessed 27 June 2016).
- 33. Booker M, Heawood A, Purdy S. Why do patients with ‘primary care sensitive’ problems access ambulance services? BMJ Open 2015;5:e007726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Richie J, Spencer L. Qualitative DATA ANALYSIS for applied policy research In: Bryman A, Burgess B, eds. Analysing Qualitative Data. London: Routledge, 1994. p. 173–94. [Google Scholar]
- 35. Critical Appraisals Skills Programme (CASP). Available at: http://www.casp-uk.net/checklists Accessed Mar 9, 2017.
- 36. National Institute Health . Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies. Available at: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort Accessed Mar 9, 2017.
- 37. Moher D, Liberati A, Tetzlaff J, Altman DG; The Prisma Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nelson J. Why patients visit emergency units rather than use primary care services. Emerg Nurse 2011;19:32–6. [DOI] [PubMed] [Google Scholar]
- 39. Worth A, Boyd K, Kendall M, et al. Out‐of‐hours palliative care: a qualitative study of cancer patients, carers and professionals. Br J Gen Pract 2006;56:6–13. [PMC free article] [PubMed] [Google Scholar]
- 40. Hodgins MJ, Wuest J. Uncovering factors affecting use of the emergency department for less urgent health problems in urban and rural areas. Can J Nurs Res 2007;39:78–102. [PubMed] [Google Scholar]
- 41. Campbell NC, Iversen L, Farmer J, Guest C, MacDonald J. A qualitative study in rural and urban areas on whether–and how–to consult during routine and out of hours. BMC Fam Pract 2006;7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Oetjen RM, Oetjen DM, Rotarius T, Liberman A. Emergency department utilization by insured users: a study of motivating factors. Health Care Manag 2010;29:199–212. [DOI] [PubMed] [Google Scholar]
- 43. Fieldston ES, Alpern ER, Nadel FM, Shea JA, Alessandrini EA. A qualitative assessment of reasons for nonurgent visits to the emergency department: parent and health professional opinions. Pediatr Emerg Care 2012;28:220–5. [DOI] [PubMed] [Google Scholar]
- 44. Gomide MF, Pinto IC, de Figueiredo LA. Accessibility and demand at an emergency care unit: the user's perspective. Acta Paul Enferm 2012;25:19–25. [Google Scholar]
- 45. Amiel C, Williams B, Ramzan F, et al. Reasons for attending an urban urgent care centre with minor illness: a questionnaire study. Emerg Med J 2014;31:E71–5. [DOI] [PubMed] [Google Scholar]
- 46. van Moll Charante EP, van Steenwijk‐Opdam PC, Bindels PJ. Out‐of‐hours demand for GP care and emergency services: patients’ choices and referrals by general practitioners and ambulance services. BMC Fam Pract 2007;8;46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Foster J, Dale J, Jessopp L. Qualitative study of older people's views of out‐of‐hours services. Br J Gen Pract 2001;51:719–23. [PMC free article] [PubMed] [Google Scholar]
- 48. Benger JR, Jones V. Why are we here? A study of patient actions prior to emergency hospital admission. Emerg Med J 2008;25:424–7. [DOI] [PubMed] [Google Scholar]
- 49. Carret ML, Fassa A, Kawachi I. Demand for emergency health service: factors associated with inappropriate use. BMC Health Serv Res 2007;7:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Norredam M, Mygind A, Nielsen AS, Bagger J, Krasnik A. Motivation and relevance of emergency room visits among immigrants and patients of Danish origin. Eur J Public Health 2007;17:497–502. [DOI] [PubMed] [Google Scholar]
- 51. Adamson J, Ben‐Shlomo Y, Chaturvedi N, Donovan J. Exploring the impact of patient views on ‘appropriate’ use of services and help seeking: a mixed method study. Br J Gen Pract 2009;59:e226–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision‐making process. Emerg Med J;31:448–52. [DOI] [PubMed] [Google Scholar]
- 53. Agarwal S, Banerjee J, Baker R, et al. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2012;29:e3. [DOI] [PubMed] [Google Scholar]
- 54. Afilalo J, Marinovich A, Afilalo M, et al. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med 2004;11:1302–10. [DOI] [PubMed] [Google Scholar]
- 55. Redstone P, Vancura JL, Barry D, Kutner JS. Nonurgent use of the emergency department. J Ambul Care Manage 2008;31:370–6. [DOI] [PubMed] [Google Scholar]
- 56. Masso M, Bezzina A, Siminski P, Middleton R, Eagar K. Why patients attend emergency departments for conditions potentially appropriate for primary care: reasons given by patients and clinicians differ. Emerg Med Australas 2007;2007:333–40. [DOI] [PubMed] [Google Scholar]
- 57. Lobachova L, Brown DF, Sinclair J, Chang YC, Thielker KZ, Nagurney JT. Patient and provider perceptions of why patients seek care in emergency departments. J Emerg Med 2014;46:104–12. [DOI] [PubMed] [Google Scholar]
- 58. Wilkin HA, Cohen EL, Tannebaum MA. How low‐income residents decide between emergency and primary health care for non‐urgent treatment. Howard J Commun 2012;23:157–74. [Google Scholar]
- 59. Coleman P, Irons R, Nicholl J. Will alternative immediate care services reduce demands for non‐urgent treatment at accident and emergency? Emerg Med J 2001;18:482–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shaw EK, Howard J, Clark EC, Etz RS, Arya R, Tallia AF. Decision‐making processes of patients who use the emergency department for primary care needs. J Health Care Poor Undeserved 2013;24:1288–305. [DOI] [PubMed] [Google Scholar]
- 61. McGuigan T, Watson P. Non‐urgent attendance at emergency departments. Emerg Nurse 2010;18:34–8. [DOI] [PubMed] [Google Scholar]
- 62. Scott DR, Batal HA, Majeres S, Adams JC, Dale R, Mehler PS. Access and care issues in urban urgent care clinic patients. BMC Health Serv Res 2009;9:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Gill JM, Riley AW. Nonurgent use of hospital emergency departments: urgency from the patient's perspective. J Fam Pract 1996;42:491–6. [PubMed] [Google Scholar]
- 64. Toloo G, FitzGerald GJ, Aitken PJ, et al. Ambulance use is associated with higher self‐rated illness seriousness: user attitudes and perceptions. Acad Emerg Med 2013;20:576–83. [DOI] [PubMed] [Google Scholar]
- 65. Togher F, O'Cathain A, Phung VH, Turner J, Siriwardena N. Reassurance as a key outcome valued by emergency ambulance service users: a qualitative interview study. Health Expect 2014;18:2951–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Richardson S, Ardagh M, Hider P. New Zealand health professionals do not agree about what defines appropriate attendance at an emergency department. N Z Med J 2006;119:U1933. [PubMed] [Google Scholar]
- 67. Goode J, Greatbatch D, O'Cathain A, Luff D, Hanlon G, Strangleman T. Risk and the responsible health consumer: the problematics of entitlement among callers to NHS Direct. Crit Soc Policy 2004;24:210–32. [Google Scholar]
- 68. Ware JE Jr, Davies AR. Behavioral consequences of consumer dissatisfaction with medical care. Eval Prog Plan 1983;6:291–7. [DOI] [PubMed] [Google Scholar]
- 69. Love MM, Mainous AG III. Commitment to a regular physician: how long will patients wait to see their own physician for acute illness? J Fam Pract 1999;48:202–7. [PubMed] [Google Scholar]
- 70. Cecil E, Bottle A, Cowling TE, Majeed A, Wolfe I, Saxena S. Primary care access, emergency department visits, and unplanned short hospitalizations in the UK. Pediatrics 2016;137:e20151492. [DOI] [PubMed] [Google Scholar]
- 71. Huntley A, Lasserson D, Wye L, et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open 2014;4:e004746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ragin DF, Hwang U, Cydulka RK, et al. Reasons for using the emergency department: results of the EMPATH Study. Acad Emerg Med 2005;12:1158–66. [DOI] [PubMed] [Google Scholar]
- 73. Capp R, Rooks SP, Wiler JL, Zane RD, Ginde AA. National study of health insurance type and reasons for emergency department use. J Gen Intern Med 2014;29:621–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood) 2013;32:1196–203. [DOI] [PubMed] [Google Scholar]
- 75. Hsia RY, Kellerman AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA 2011;305:1978–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Citizens Advice . Younger Adults More Likely to Turn to Walk‐in Centres and A&E. 2014. Available at: https://www.citizensadvice.org.uk/about-us/how-citizens-advice-works/media/press-releases/younger-adults-more-likely-to-turn-to-walk-in-centres-and-a-amp-e/ Accessed Oct 21, 2016.
- 77. Turner J, O'Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3:e003451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. O'Shea J. The Crisis in America's Emergency Rooms and What Can Be Done. Health Care Reform. Washington, DC: The Heritage Foundation, 2008. [Google Scholar]
- 79. Five Year Forward View. NHS England . 2014. Available at: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf Accessed Mar 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Search strategy.
Data Supplement S2. Summary tables of all included papers.
Data Supplement S3. Quality assessment of included studies.


