Summary
This is the first systematic review of reviews to assess the effect of obesity and weight loss on health‐related quality of life (HRQoL). We identified 12 meta‐analyses/systematic reviews published between January 2001 and July 2016. They addressed the following themes: (i) the relationship between weight/body mass index and HRQoL (baseline/pre‐intervention; n = 2). (ii) HRQoL after weight loss (varied interventions and/or study design; n = 2). (iii) HRQoL after weight loss (randomized controlled trials only; n = 2). (iv) HRQoL after bariatric surgery (n = 6). We found that in all populations, obesity was associated with significantly lower generic and obesity‐specific HRQoL. The relationship between weight loss and improved HRQoL was consistently demonstrated after bariatric surgery, perhaps due to a greater than average weight loss compared with other treatments. Improved HRQoL was evident after non‐surgical weight loss, but was not consistently demonstrated, even in randomized controlled trials. This inconsistency may be attributed to variation in quality of reporting, assessment measures, study populations and weight‐loss interventions. We recommend longer‐term studies, using both generic and obesity‐specific measures, which go beyond HRQoL in isolation to exploring mediators of HRQoL changes and interactions with other variables, such as comorbidities, fitness level and body image.
Keywords: Obesity, quality of life, weight loss, weight management
Introduction
People with obesity have an increased risk of a multitude of diseases and early mortality 1, 2, 3, 4, 5. Beyond health risks, obesity has also been shown to negatively impact quality of life (QoL) 6, defined as an individual's own assessment of well‐being, often with reference to physical and mental health status, social relationships and environmental and economic factors 7, 8, 9. When the focus in clinical and health research is on the quantification of QoL related to health status, it is referred to as health‐related QoL (HRQoL) 7, 8, 10. This term is most commonly understood to refer to a multidimensional measurement of the individual's perception of the impact of illness and its treatment 10, 11. HRQoL captures, at a minimum, physical, psychological and social functioning 10. The various measures for assessing different aspects of an individual's HRQoL can be grouped into two categories: generic measures and disease‐specific measures 7, 12. Generic measures assess broad aspects of HRQoL, while disease‐specific measures are designed to assess HRQoL in relation to a specific medical condition or clinical population.
Because studies on obesity and/or weight loss increasingly include measures of HRQoL, a large number of review articles have been written on this topic. We considered that a systematic review of review articles, comprising a comprehensive examination of the current state of the field, is needed to evaluate the impact of obesity and weight loss on HRQoL. According to Smith et al., one goal of a systematic review of reviews is to identify and appraise all published reviews within an area of interest in order to summarize and compare conclusions, as well as discuss the strength of these conclusions 13. The aim of this review is to synthesize the information found in obesity and/or weight‐loss reviews that assess HRQoL and to evaluate the impact of obesity and weight reduction on HRQoL.
Methods
We conducted a systematic review of reviews in accordance with the Preferred Reporting Items for Systematic Review and Meta‐Analysis (PRISMA) guidelines (http://www.prisma‐statement.org/). The PubMed and Embase databases were used to identify review articles that have evaluated the evidence of the impact of obesity and weight management on HRQoL (Fig. 1). The search terms applied to the PubMed and Embase databases are detailed in Fig. 2. A search string was defined and limits were applied (Fig. 2). The search was restricted to January 2001 to July 2016. The selection of review articles to include was performed by three independent reviewers (RK; JRA; AXON) and articles were excluded if they met specific predefined exclusion criteria (Fig. 2).
Figure 1.
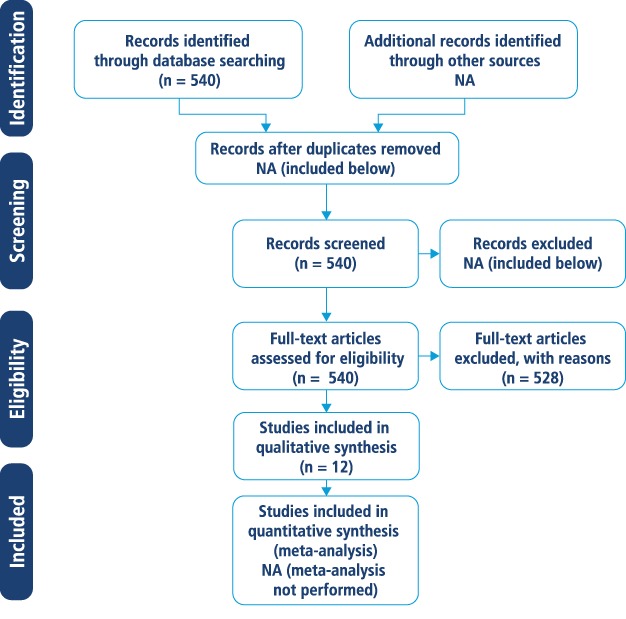
Preferred Reporting Items for Systematic Review and Meta‐Analysis (PRISMA) flow chart. NA, not applicable. [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.
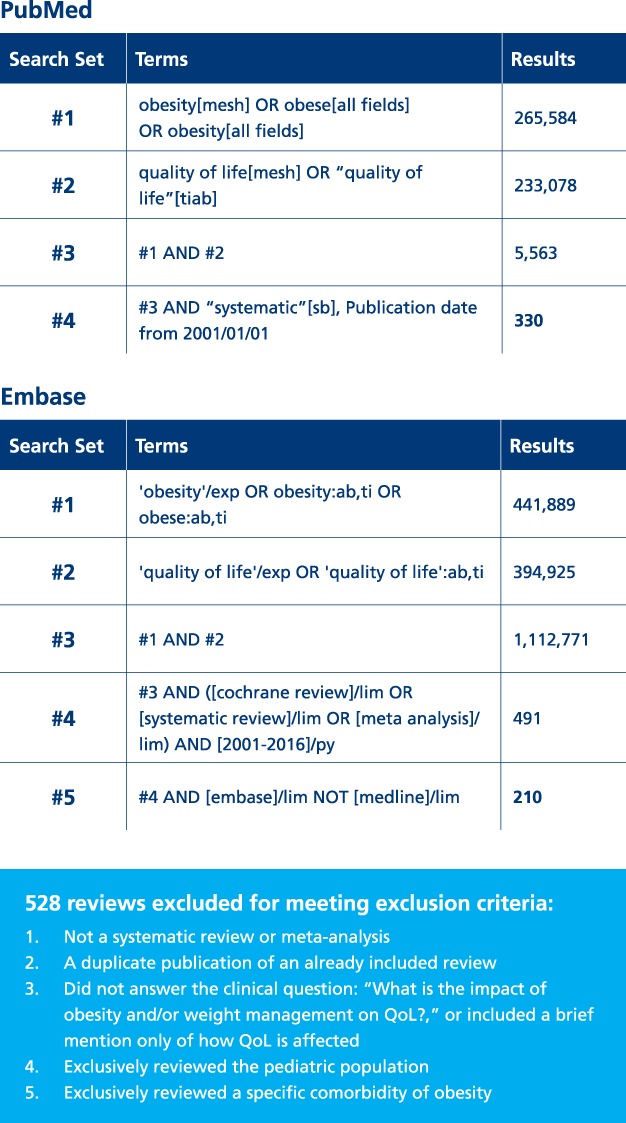
Identification and selection of published review articles on obesity and/or weight management and quality of life from January 2001 to July 2016. QoL, quality of life. [Colour figure can be viewed at wileyonlinelibrary.com]
Results
A total of 540 review articles were retrieved from PubMed and Embase, of which 12 were selected for inclusion in this systematic review of reviews. Table 1 provides a detailed overview of the 12 review articles selected for inclusion; 5 were systematic reviews 16, 17, 21, 22, 29, 4 were meta‐analyses 14, 15, 18, 19 and 3 were both a systematic review and a meta‐analysis 12, 20, 33. In the 12 reviews, a total of 240 individual studies were reviewed; 64 studies were included in two or more of the 12 reviews, while 176 studies were included in only one of the 12 reviews (Table S1, Supporting Information).
Table 1.
Review articles focusing on obesity or weight management and HRQoL
| No. | Author, date | Type/goal of review | Studies | Key findings | Strengths | Limitations |
|---|---|---|---|---|---|---|
| Category 1: Relationship between weight/BMI and HRQoL (baseline/pre‐intervention) | ||||||
| 1 | van Nunen et al., 2007 14 |
|
|
|
|
|
| 2 | Ul‐Haq et al., 2013 15 |
|
|
|
|
|
| Category 2: HRQoL after weight loss (varied interventions and/or varied study design) | ||||||
| 3 | Carson et al., 2014 16 |
|
|
|
|
|
| 4 | Kroes et al., 2016 17 |
|
|
|
|
|
| Category 3: HRQoL after weight loss (RCTs only) | ||||||
| 5 | Maciejewski et al., 2005 18 |
|
|
|
|
|
| 6 | Warkentin et al., 2013 12 |
|
|
|
|
|
| Category 4: HRQoL after bariatric surgery | ||||||
| 7 | Magallares and Schomerus, 2015 19 |
|
|
|
|
|
| 8 | Lindekilde et al., 2015 20 |
|
|
|
|
|
| 9 | Andersen et al., 2015 21 |
|
|
|
|
|
| 10 | Jumbe, 2015 22 |
|
|
|
|
|
| 11 | Hachem et al., 2016 29 |
|
|
|
|
|
| 12 | Driscoll et al., 2016 33 |
|
|
|
|
|
HRQoL‐HSP is sometimes referred to as ‘Lewin‐TAG’.
15D, 15‐dimensional measure; EQ‐5D, EuroQuol‐5D measure; GHQ, General Health Questionnaire; GHRI, General Health Rating Index; GIQLI, Gastrointestinal Quality of Life measure; GWB, General Well‐Being measure; HRQoL, health‐related quality of life; HRQoL‐HSP, Health‐related quality of life‐Health State Preference Assessment; IWQOL, Impact of Weight on Quality of Life; IWQOL‐Lite, Impact of Weight on Quality of Life‐Lite; M–A QoLQII, Moorehead–Ardelt Quality of Life Questionnaire II; NHP, Nottingham Health Profile; OAS, Obesity Adjustment Survey; OP, Obesity‐related Problems scale; ORWELL, Obesity‐Related Well‐Being questionnaire; OWLQOL, Obesity and Weight Loss Quality of Life; QOLOD, Quality of Life, Obesity and Dietetics Rating Scale; QWB, Quality of Well‐Being scale; RCT, randomized controlled trial; SF‐36, Medical Outcomes Study Short‐Form‐36; SIP, Sickness Impact Profile; VAS, Visual Analogue Scale; WRSM, Weight‐Related Symptoms Measure.
Some of the review articles provided a definition of QoL and/or HRQoL 12, 16, 20, 21, 29. Definitions were similar and confirmed HRQoL as a multidimensional concept of the individual's perceptions of the impact of their disease on an individual level. All reviews aimed to analyse HRQoL in relation to weight, and could be logically organized into four categories (Table 1). Following a brief discussion of the assessment methods used in all included reviews, the reviews are described by category, below.
Assessment of health‐related quality of life
Among the 12 review articles examined, a total of 23 different measures of HRQoL were identified (Table S2) and could be categorized as follows: 11 generic, 10 obesity‐specific, 1 combined generic/obesity‐specific and 1 gastrointestinal‐specific. We did not report results of measures of depression, anxiety, stress or emotions 12, 18, 22, nor did we include any non‐obesity‐specific disease measures (e.g. Minnesota Living with Heart Failure Questionnaire, Pelvic Floor Impact Questionnaire), as these measures are not true assessments of HRQoL 34. We have also not reported results obtained from the Bariatric Analysis and Reporting Outcome System (BAROS) 35, as it can only be applied to post‐surgical (not pre‐ vs. post‐surgical) outcomes for bariatric surgery patients.
A total of 10 of the 12 review articles included studies that used both generic and obesity‐specific measures of HRQoL 12, 14, 16, 17, 18, 20, 21, 22, 29, 33, whereas 2 of the review articles included only generic measures 15, 19. The most commonly used measures were the generic Medical Outcomes Study Short‐Form‐36 (SF‐36) 36 and the obesity‐specific Impact of Weight on Quality of Life‐Lite (IWQOL‐Lite) questionnaires 37. A total of 5 of 12 the reviews specified that they included both generic and obesity‐specific measures in order to provide a more complete understanding of the patient populations 12, 17, 18, 20, 29.
Category 1: Relationship between weight/body mass index and health‐related quality of life (baseline/pre‐intervention)
A total of 2 of 12 reviews examined the association between weight/body mass index (BMI) and HRQoL without, or prior to, any intervention 14, 15. van Nunen et al. performed a meta‐analysis of cross‐sectional differences among five subgroups, including: non‐patient subgroups (general population, general population with obesity and non‐treatment‐seeking people with obesity) and patient subgroups (non‐surgical weight‐loss patients and bariatric surgery patients) 14 (Table 1). For both SF‐36 and IWQOL‐Lite, the greatest reduction in HRQoL was observed in the surgical patients. SF‐36 results varied widely by subscale, with only a consistent reduction in the physical functioning HRQoL subscale for patient vs. non‐patient groups.
However, reduced HRQoL was found on all IWQOL‐Lite subscales for patient (compared with non‐patient) groups. After adjustment for BMI, reduced HRQoL on most SF‐36 subscales remained for surgical patients, whereas for IWQOL‐Lite differences between general, non‐treatment, conservative treatment and surgical treatment subgroups disappeared, suggesting that when using the IWQOL‐Lite questionnaire in cross‐sectional analyses, body weight is the main determinant of HRQoL.
Ul‐Haq et al. evaluated HRQoL across studies that used SF‐36 and cross‐sectional data from six countries (Table 1) 15. In this well‐designed meta‐analysis, the authors analysed pooled estimates (totalling 43 086 participants) of the weighted mean difference in the Physical Component Summary (PCS) score and the Mental Component Summary (MCS) score with reference to normal weight, determined the degree of heterogeneity, assessed publication bias and applied a statistical method to reduce the risk of Type I errors. Compared with normal‐weight adults, those with higher BMI (≥25 kg m−2) had significantly reduced PCS scores and a dose relationship was evident across all BMI categories. In contrast, compared with the normal‐weight adults, MCS scores were significantly reduced only in those with Class III obesity (BMI ≥ 40 kg m−2), but not Class I (BMI 30–34.9 kg m−2) or Class II (BMI 35–39.9 kg m−2) obesity 15.
Category 2: Health‐related quality of life after weight loss (varied interventions and/or study design)
Carson et al. 16 assessed changes in HRQoL after dietary interventions in 21 randomized controlled trials (RCTs) and 3 non‐RCTs (Table 1) 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61. Twenty‐two studies reported improvements in HRQoL over time; 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 52, 53, 54, 56, 57, 58, 59, 60, 61 however, 3 of these 22 studies used only non‐obesity‐specific disease measures to assess HRQoL 38, 44, 54. Mean weight loss ranged from 2 to 10 kg for the groups receiving active treatment (i.e. calorie restriction, healthy diet or commercial programme).
Four studies demonstrated that changes in HRQoL were independent of weight loss; 39, 40, 41, 42 11 studies indicated that changes in HRQoL were probably a result of weight loss 38, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52 (three of these included only a non‐obesity‐specific measure of disease impairment); 38, 44, 51 and in the remaining nine studies, the role of weight loss in HRQoL changes was unclear 53, 54, 55, 56, 57, 58, 59, 60, 61.
Kroes et al. assessed the impact of weight/BMI change on HRQoL (SF‐36, IWQOL‐Lite, or both) in 8 RCTs and 12 non‐RCTs following a number of different interventions, including lifestyle approaches (exercise, dietary weight loss or counselling), pharmaceutical intervention and bariatric surgery 17. For the seven studies that reported the association of weight loss and HRQoL, one study of lifestyle change resulted in a median weight loss of 0.36 kg; for the one pharmaceutical intervention, mean weight loss was 2.7%; for the studies of bariatric surgery with ≥1‐year follow‐up, percent weight reduction was 20–38.8% and percent excess weight loss was 56.4–62.7%. Regardless of intervention, improvements in the physical aspects of the SF‐36 were reported more frequently than improvements in mental/psychosocial aspects, whereas improvements in all or most of the obesity‐specific IWQOL‐Lite subscales were demonstrated. However, a significant degree of heterogeneity in the included studies precluded drawing conclusions about the specific association between weight/BMI change and HRQoL.
Category 3: Health‐related quality of life after weight‐loss (randomized controlled trials only)
Two reviews described HRQoL outcomes after RCTs of weight‐loss interventions, one published in 2005 18 and the other in 2013 12 (Table 1). The earlier review included 34 studies, while the later one included 53 studies (with 14 overlapping studies; see Table S1). As well as an increase in the number of studies, the quality of reporting of HRQoL results improved over time, allowing more sophisticated analyses in the more recent review.
One similarity between these two reviews is that weight‐loss interventions were quite diverse. Although both reviews included meta‐analyses, the 2005 review 18 − due to poor quality of reporting and insufficient data on measures of HRQoL − used a meta‐analysis only on the effect of weight‐loss treatment on depressive symptoms, whereas in the 2013 review 12 meta‐analyses were used to examine the relationship between changes in weight and HRQoL.
In the studies reported in the 2005 review 18, 9 of 34 RCTs demonstrated improvements in generic HRQoL in one or more domains, although the domains varied by study. Six of the 11 that used obesity‐specific measures showed positive treatment effects. Weight loss was not reported in this review. In the studies reported in 2013 by Warkentin et al. 12, 14 of 36 studies reporting generic measures of HRQoL found significant improvements, whereas 4 of 15 studies reporting obesity‐specific measures found significant improvements. Weight loss varied from ≤5 to ≥10% (specific weight loss values were not reported). Conclusions from both of these reviews of RCTs were similar. Maciejewski et al. 18 concluded: ‘HRQoL outcomes, including depression, were not consistently improved in RCTs of weight loss.’ Warkentin et al. 12 concluded: ‘Certainly, compelling and definitive RCT‐level data to support the notion that HRQoL is consistently and robustly improved following weight loss is not available.’
Category 4: Health‐related quality of life after bariatric surgery
Six reviews examined HRQoL after bariatric surgery (Table 1) 19, 20, 21, 22, 29, 33. Inclusion/exclusion criteria differed between the reviews, resulting in eight overlapping studies between Lindekilde et al. 20 and Magallares and Schomerus 19, six between Lindekilde et al. 20 and Andersen et al. 21, four between Lindekilde et al. 20 and Hachem et al. 29, and three between Lindekilde et al. 20 and Jumbe et al. (Table S1) 22. The remaining review combinations had two or fewer overlapping studies. Each of these reviews of bariatric surgery outcomes has its own strengths and limitations (Table 1).
The six reviews reported and/or analysed HRQoL data using different methods, making a comparison of the results challenging. Only the reviews by Andersen et al. 21, Lindekilde et al. 20, and Magallares and Schomerus 19 reported results in terms of standardized effect sizes (i.e. the magnitude of the pre‐ to post‐surgery changes were reported in a standardized fashion). Reporting standardized effect sizes allows direct comparisons across studies. Nevertheless, the specific methods used to calculate effect sizes varied across reviews, making comparisons less meaningful.
Additional inconsistencies in HRQoL reporting were observed across studies. In Andersen et al. 21, primary outcomes (defined as summary scores of generic or obesity‐specific measures or a measure of overall health status or overall well‐being) and secondary outcomes (defined as domain scores, such as social interaction, physical appearance and self‐regard) were reported separately to minimize multiple comparisons. In the review by Lindekilde et al. 20, all of the HRQoL scales and subscales were categorized into five domains: ‘physical’, ‘mental’, ‘social’, ‘functional’ and ‘total’, together with ‘overall HRQoL’ and ‘HRQoL for all measures’. However, no information was provided on how the various subscales of each assessment measure were assigned to these domains, nor was the distinction between total HRQoL and overall HRQoL described, making their analyses difficult to replicate and results difficult to interpret. Finally, reporting of study results was inconsistent in the reviews by Hachem et al. 29 and Jumbe et al. 22, with some reporting overall scores, some reporting composite scores and some reporting subscale scores, also making results difficult to interpret.
Weight loss was reported differently across bariatric surgery reviews, as well as inconsistently within any single review. Study duration ranged from 5 to 72 months. For reviews reporting change in BMI from baseline to end of study 20, 21, 22, 33, BMI change ranged from 4.6 to 30.6 kg m−2. For reviews reporting mean weight loss in kg 22, weight reduction was 13.5−45.1 kg. Two reviews 19, 29 did not report any end‐of‐trial values for change in BMI or weight.
Medical Outcomes Study Short‐Form‐36 (SF‐36) results of bariatric surgery studies
All bariatric surgery reviews included SF‐36 results. Magallares and Schomerus 19 found a large variation in the degree of improvement in both PCS and MCS at ≤1‐year post‐surgery. Although effect sizes associated with these changes were much greater for the physical component than the mental component, both effects were very large.
Although Lindekilde et al. 20 did not report results separately for PCS and MCS, they examined differences between ‘physical and mental domains on the SF‐36’ adjusted for baseline scores, reporting that these differences were significantly greater for the physical than for the mental domains. In addition to the SF‐36 analysis, these authors computed physical and mental scores from the various measures administered. The effect size for physical HRQoL was significantly greater than that for mental HRQoL and this difference remained significant, even after adjusting for other factors (baseline BMI, age, type of measure, type of surgery, months to follow‐up, year of publication and country in which the study was carried out).
The review by Jumbe et al. 22 revealed significantly better SF‐36 outcomes in three out of three studies for people who had undergone bariatric surgery compared with those receiving non‐surgical interventions. One out of the three RCTs reported significantly better outcomes across all SF‐36 subscales. Five out of seven studies in which SF‐36 outcomes after bariatric surgery were compared with those obtained in non‐treated control groups showed greater improvements in the surgery group compared with the controls, although there was some overlap among the patient populations included in these studies (see Table 1).
Four of the six studies reporting SF‐36 results in the review by Hachem et al. 29 reported a significant improvement in the physical aspects of HRQoL and three of the studies reported a significant improvement in the mental aspects of HRQoL after bariatric surgery, whereas there were no significant changes in these domains in the non‐surgical comparator groups in two of the studies.
Two of the reviews included herein comprised only long‐term studies (≥5‐year duration) 21, 33. In the review by Andersen et al. 21, two of the three studies using the SF‐36 showed significant improvements in both PCS and MCS at 5–6 years; 25, 62 the remaining study showed significant improvements only in PCS 63. Peak improvements in PCS occurred at 1–2 years across all three studies. MCS scores showed a less consistent pattern. While the systematic review conducted by Driscoll et al. 33 showed some inconsistencies in SF‐36 results, meta‐analysis results revealed significant improvements in both physical and mental health domains of the SF‐36 after 5 years, favouring surgical over control groups. Improvements were greater in the physical compared with the mental domains.
In general, results of SF‐36 scores following bariatric surgery showed improvements in HRQoL relative to non‐surgical groups. Moreover, although these changes were seen in both mental and physical domains, improvements in physical domains of HRQoL seem to be greater.
Obesity‐specific health‐related quality of life results of bariatric surgery studies
Five of the six reviews included obesity‐specific HRQoL results 20, 21, 22, 29, 33. In the three studies 25, 30, 64 reviewed by Andersen et al. 21 that used an obesity‐specific measure of HRQoL, significant and very large effects were reported at 5–10 years. In addition, effect sizes were generally larger for obesity‐specific than for generic measures. Similarly, effect sizes were greater for obesity‐specific than for generic measures of HRQoL in the Lindekilde et al. 20 review.
Two studies included in the review by Hachem et al. reported between‐group differences on obesity‐specific measures of HRQoL 26, 65. Specifically, in the study by Adams et al. 26, significant improvements were found on the IWQOL‐Lite questionnaire in the post‐gastric bypass surgery vs. two comparator groups (people with obesity seeking bariatric surgery who did not have surgery and people with obesity who were not seeking surgery).
In the Brunault et al. 65 study, both laparoscopic adjustable gastric banding (LAGB) and laparoscopic sleeve gastrectomy (LSG) resulted in improved physical, psychosocial, sexual and diet experience domains on the QoL, Obesity and Dietetics Rating Scale vs. pre‐operative assessments. In addition, the ‘comfort with food scale’ showed greater improvement in the LSG group compared with the LAGB group at 6, but not at 12, months.
In the review by Driscoll et al. 33, three studies 30, 66, 67 included the Obesity‐related Problems scale (OP scale) and one study 25 included the IWQOL‐Lite. An observational, cross‐sectional study by Raoof et al. 66 indicated that OP scores for patients who had undergone gastric bypass surgery an average of 11.5 ± 2.7 years earlier showed improved HRQoL vs. scores obtained by a matched group awaiting bariatric surgery; however, OP scores for the post‐surgical group also revealed that HRQoL remained impaired when compared with the general population. In the study by Karlsson et al. 30, the OP scale improved significantly for bariatric surgery patients at 10 years vs. pre‐surgery and these improvements were greater than those seen in patients treated with non‐surgical interventions. In the study by Aftab et al 67,. OP scores obtained in post‐bariatric surgery patients at 5 years were superior to those obtained in patients pre‐surgery. Kolotkin et al. 25 found that patients who had undergone gastric bypass surgery 6 years previously had significantly greater improvements from baseline in all five IWQOL‐Lite domains compared with people with obesity who sought but did not receive gastric bypass, and also compared with people with severe obesity in the general population.
In summary, using obesity‐specific HRQoL measures, positive effects on HRQoL were seen following bariatric surgery, and these changes tended to be greater than those seen with SF‐36.
Discussion
This is the first systematic review of reviews to synthesize published information on the impact of obesity and weight loss on HRQoL. By including only meta‐analyses and systematic reviews, and excluding narrative reviews, bias was minimized. Moreover, by reviewing multiple reviews, we were able to integrate information from a large number of studies: only 64 (27%) of the 240 studies were included in more than one review, and this small degree of overlap limited the risk of duplication of conclusions, while ensuring the reviews were not overly selective. This systematic review of reviews illustrates the significant and negative impact that overweight/obesity has on HRQoL, regardless of study population 14, 15.
In reviews examining the relationship between HRQoL and obesity in various populations without or prior to intervention, increased obesity was associated with decreased HRQoL, particularly in those with Class III obesity (BMI ≥ 40 kg m−2) 15 and those seeking bariatric surgery 14, suggesting that low HRQoL may provide motivation in these patients to undergo an invasive intervention. Furthermore, the physical aspects of HRQoL seem to be more closely associated with degree of obesity than the mental aspects of HRQoL; in population data from six countries the relationship between BMI and SF‐36 PCS was dose‐dependent, with poorer physical HRQoL occurring in those with higher BMIs, whereas MCS scores were reduced only in those with Class III obesity.
Reviews limited to RCTs 12, 18 represent the most robust dataset available, and although one might expect consistent associations between weight loss and improved HRQoL, these studies are not conclusive, despite inclusion of both generic and obesity‐specific data. In the two reviews limited to RCTs, one reported significant improvements in one or more domains of generic HRQoL in 9 out of 34 included RCTs 18, whereas the other review reported improvements in 14 out of 36 included studies evaluating HRQoL using a generic measure 12. Obesity‐specific HRQoL results were also inconsistent, with one review reporting improved obesity‐specific HRQoL in 6 out of 11 included studies 18 and the other reporting improved obesity‐specific HRQoL in 4 out of 15 included studies 12.
The lack of consistently demonstrated associations between weight loss and improved HRQoL in RCTs may be due to the following factors: diverse HRQoL measures have been used; weight‐loss interventions have been heterogeneous, with some more successful at inducing weight loss than others; studies may have been underpowered to detect differences in HRQoL outcomes; and there has been poor reporting of HRQoL outcomes (since weight loss, rather than HRQoL, is usually the primary outcome). To bring more clarity to these results, authors of two of the systematic reviews recommend that future research focus on prospective, long‐term studies, especially RCTs or large, well‐designed, observational studies with high retention rates, comparator groups and carefully chosen generic and obesity‐specific HRQoL measures 12, 21.
Results from reviews that include studies of mixed design (RCTs and non‐RCTs) and/or mixed interventions are even more difficult to interpret 16, 17, especially when treatments are diverse (e.g. bariatric surgery, pharmaceutical interventions and lifestyle treatments) and result in vastly divergent weight loss outcomes 17. Overall, more randomized, controlled, high‐quality studies are needed to better understand the relationship between the various possible weight‐loss interventions and changes in HRQoL.
When reviews were limited to those undergoing bariatric surgery, there was less variation in results, with post‐bariatric surgery patients demonstrating improvements in both physical and mental aspects of generic HRQoL. It is likely that the greater weight reductions seen with bariatric surgery, compared with dietary, medical and lifestyle treatments, contribute to the consistency of improvements in HRQoL. In addition, baseline HRQoL scores are more impaired for people undergoing bariatric surgery than for patients receiving non‐surgical treatments 14 allowing the possibility of greater improvement. Improvements in physical aspects were greater and reported more consistently than improvements in mental aspects of HRQoL when assessed with the SF‐36. Comparison of post‐surgical effect sizes indicated consistently larger effects with obesity‐specific measures compared with generic measures, suggesting that obesity‐specific measures may be more sensitive to change.
That such effects were generally more marked when obesity‐specific measures were utilized is consistent with recommendations made in several reviews that both types of measures be incorporated into future studies 12, 17, 20, 21, 29.
In the reviews comparing HRQoL outcomes in patients who have undergone weight‐loss surgery with non‐surgical comparator groups, improvements in HRQoL were generally greater in the surgical groups, despite some inconsistency of findings. Taken as a whole, these findings suggest the value of assessing HRQoL in patients with clinically severe obesity so that they may receive the HRQoL benefits from bariatric surgery.
It is encouraging that weight loss is often associated with improvements in HRQoL in people with obesity. Nevertheless, some reviews demonstrated significant variability in HRQoL after weight‐loss intervention. Articles included in this systematic review of reviews cited several potential limitations, including insufficient data due to patient dropout and lack of follow‐up, and a shortage of studies reporting on obesity‐specific HRQoL. For example, in the review by Warkentin et al. 12, only 25% of studies using SF‐36 could be included in the quantitative data pooling due to poor reporting quality. This low quality of reporting and lack of data may be because HRQoL is usually a secondary outcome in studies. Another limitation in the included reviews of weight‐loss studies is that length of follow‐up varied considerably, some with durations as short as 6 weeks, making it difficult to draw meaningful conclusions about longer‐term outcomes. The majority of studies had a short‐term (<24 months) or medium‐term (24–60 months) follow‐up period and only two reviews (both evaluating the effects of bariatric surgery on HRQoL) focused exclusively on studies with long‐term follow‐up periods (≥5 years) 21, 33.
The assessment of the quality of studies included in a review is also an important indicator of the strength of the conclusions of the authors; yet, only approximately 40% of systematic reviews evaluate the quality of included studies 68.
Notably, in this systematic review of reviews, a higher number (9 of the 12 review articles [75%]) concerned themselves with study quality, either by including a direct assessment of study quality 12, 16, 17, 18, 22, 33 or by using ‘acceptable quality’ (variably defined) as selection criteria for study inclusion 20, 21.
We also noted differences across the 12 reviews with respect to HRQoL measures, country and language of the studies, reporting of results, method for determining effect sizes, length of follow‐up, type of weight‐loss intervention and population being studied. We made every effort to describe similarities and differences among reviews and to report the number of reviews that made particular conclusions. We believe our review represents a true synthesis of current and diverse reviews in this field and, as such, has broad applicability.
We make no attempt to draw conclusions about the HRQoL of specific patient populations/subgroups (e.g. different ethnicities/cultures, age or comorbidities). Studies not discussed in this review have shown that these variables may be helpful in predicting the impact that weight and/or weight loss have on HRQoL 69, 70, 71, 72. For example, increasing age in people with overweight or obesity is associated with increased impairment in some domains of HRQoL, such as physical function, sexual life and work, but not others 72. Some studies conclude that women with overweight or obesity report more impairment than men in some HRQoL domains 71, 72. Furthermore, HRQoL in people with obesity varies depending on presence of comorbidities 69, 70. Two reviews 15, 17 recommend that future studies assess the impact of comorbidities on HRQoL.
Four reviews 12, 16, 17, 18 recommended exploring mediators of changes in HRQoL to understand if the driver of HRQoL improvements is weight loss itself, the weight‐loss intervention or changes in other variables. A recent study 73 used multiple mediation analysis to explore causal mechanisms underlying the relationship between weight loss and improved HRQoL in two weight‐loss trials investigating phentermine/topiramate. Results indicated that improved HRQoL was primarily mediated by weight loss, but decreased depressive symptoms also accounted for improvements in HRQoL.
Similarly, a mediation analysis of three RCTs with liraglutide 3.0 mg showed that improvements in IWQOL‐Lite total and physical function scores in patients with type 2 diabetes were primarily driven by weight loss 74. Several other recommendations for future research were provided in the included reviews (see Fig. 3 for summary).
Figure 3.
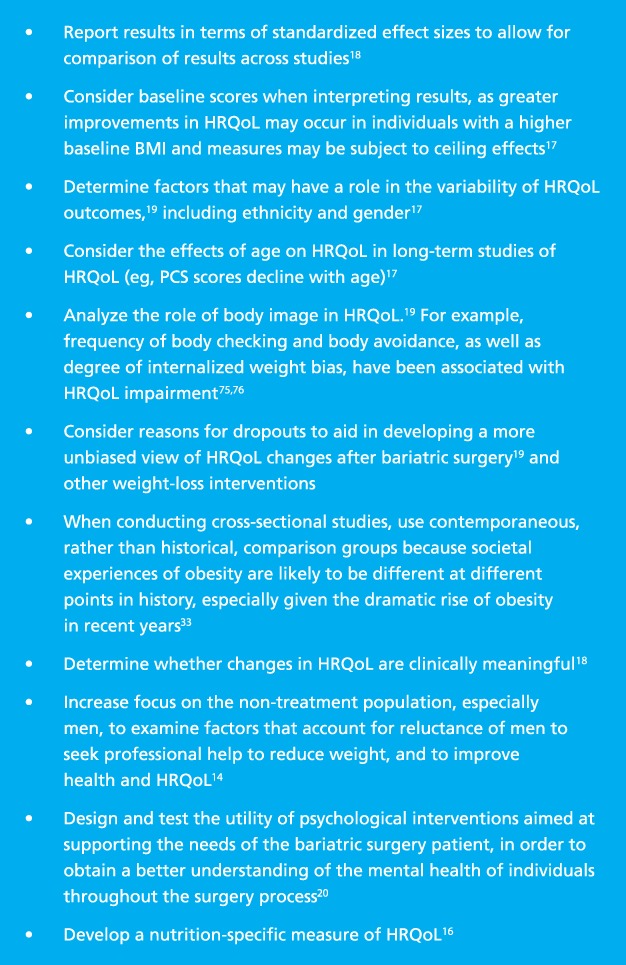
Summary of recommendations for future studies. BMI, body mass index; HRQoL, health‐related quality of life; PCS, Physical Component Summary. [Colour figure can be viewed at wileyonlinelibrary.com]
After conducting this systematic review of reviews, we believe the next wave of research studies should focus on the interactions between HRQoL and other variables, such as gender, fitness level, comorbidities or body image. For example, do the associations between HRQoL and obesity and/or weight loss consistently vary by other variables and how do these variables interact with each other? Is there a gradient in HRQoL by weight‐loss treatment, such that treatments inducing greater weight loss are or are not associated with greater HRQoL improvements? How much weight loss is needed for improvement in HRQoL and what is the impact of weight regain on HRQoL? Is improvement in HRQoL after weight‐loss treatment dependent primarily on amount of weight loss, or do other factors have a role? Can we predict which individuals will experience improved HRQoL after weight loss?
Inclusion of HRQoL assessments, especially obesity‐specific assessments, in regular patient evaluations could guide the development of broad healthcare policies that recognize the bio‐psychosocial impact of the growing obesity epidemic. HRQoL assessments can help patients and providers differentiate between treatments that have similar weight‐loss patterns but different side‐effect profiles or different impacts on HRQoL. It is desirable to reach a consensus for the best way to evaluate the impact of obesity and/or weight loss on HRQoL in future studies to facilitate comparison of results across studies 77.
In summary, this is the first systematic review of reviews to synthesize research on the impact of obesity and weight loss on HRQoL. We found that obesity was associated with significantly lower HRQoL in all populations. We also established an important relationship between weight loss and improved HRQoL, which is demonstrated most consistently following bariatric surgery, but less consistently following non‐surgical weight‐loss interventions.
In order to build upon these findings, we recommend longer‐term studies that use both generic and obesity‐specific measures and that evaluate the impact of other factors (e.g. comorbidities, fitness level, body image) on HRQoL after various weight‐loss interventions. These findings, plus those of future studies and review articles, will help us better understand the complex and multifaceted nature of obesity and its impact on the daily lives of our patients.
Conflict of Interest Statement
RLK receives royalties from Duke University as IWQOL‐Lite developer; support as a consultant to Eisai, Janssen and Novo Nordisk; and grant support from University of Utah (Grant DK055006; the National Institutes of Health/The National Institute of Diabetes and Digestive and Kidney Diseases). JRA has no conflicts to declare.
Author contributions
Both RLK and JRA were responsible for the content and organization of the manuscript, as well as the search parameters of this systematic review of reviews. RLK did the majority of the writing of the manuscript, with JRA contributing significantly to the discussion and recommendations. Both authors take full responsibility for the content of this manuscript.
Supporting information
Table S1. Overlap of studies included in the reviews.
Table S2. Health‐related quality‐of‐life measures.
Acknowledgements
The authors are grateful to Dr Matthew Maciejewski for his consultation, to Megan von Isenburg for her guidance with the search string and AXON Communications for writing and editorial assistance in the development of this manuscript. Medical writing assistance was funded by Novo Nordisk. Novo Nordisk was also provided with the opportunity to perform a medical accuracy review.
References
- 1. Adams KF, Schatzkin A, Harris TB et al Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006; 355: 763–778. [DOI] [PubMed] [Google Scholar]
- 2. Kurth T, Gaziano JM, Berger K et al Body mass index and the risk of stroke in men. Arch Intern Med 2002; 162: 2557–2562. [DOI] [PubMed] [Google Scholar]
- 3. Zammit C, Liddicoat H, Moonsie I, Makker H. Obesity and respiratory diseases. Int J Gen Med 2010; 3: 335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention . Overweight & Obesity; 2016 [WWW document]. URL https://www.cdc.gov/obesity/ (accessed 27 January 2017).
- 5. Young T, Shahar E, Nieto FJ et al Predictors of sleep‐disordered breathing in community‐dwelling adults: the Sleep Heart Health Study. Arch Intern Med 2002; 162: 893–900. [DOI] [PubMed] [Google Scholar]
- 6. Kolotkin RL, Haaz S, Fontaine KR. Assessment of health‐related quality of life in obesity and eating disorders In: Allison D, Baskin M. (eds). Handbook of Assessment Methods for Eating Behaviors and Weight Related Problems. Sage Publications, Inc.: Thousand Oaks, CA, 2009. [Google Scholar]
- 7. Fontaine KR, Barofsky I. Obesity and health‐related quality of life. Obes Rev 2001; 2: 173–182. [DOI] [PubMed] [Google Scholar]
- 8. WHOQOL Group. Development of the World Health Organization WHOQOL‐BREF quality of life assessment. The Whoqol Group. Psychol Med 1998; 28: 551–558. [DOI] [PubMed] [Google Scholar]
- 9. Sullivan MB, Sullivan LG, Kral JG. Quality of life assessment in obesity: physical, psychological, and social function. Gastroenterol Clin North Am 1987; 16: 433–442. [PubMed] [Google Scholar]
- 10. Andersen JR, Karlsen T‐I, Kolotkin RL. Obesity and its impact upon quality of life In: Mullin G, Cheskin L, Matarese L. (eds). Integrative Weight Management: A Guide for Clinicians. Springer: New York, 2014, pp. 225–234. [Google Scholar]
- 11. Moons P, Budts W, De Geest S. Critique on the conceptualisation of quality of life: a review and evaluation of different conceptual approaches. Int J Nurs Stud 2006; 43: 891–901. [DOI] [PubMed] [Google Scholar]
- 12. Warkentin LM, Das D, Majumdar SR, Johnson JA, Padwal RS. The effect of weight loss on health‐related quality of life: systematic review and meta‐analysis of randomized trials. Obes Rev 2013; 15: 169–182. [DOI] [PubMed] [Google Scholar]
- 13. Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 2011; 11: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Nunen AM, Wouters EJ, Vingerhoets AJ, Hox JJ, Geenen R. The health‐related quality of life of obese persons seeking or not seeking surgical or non‐surgical treatment: a meta‐analysis. Obes Surg 2007; 17: 1357–1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ul‐Haq Z, Mackay DF, Fenwick E, Pell JP. Meta‐analysis of the association between body mass index and health‐related quality of life among adults, assessed by the SF‐36. Obesity (Silver Spring) 2013; 21: E322–E327. [DOI] [PubMed] [Google Scholar]
- 16. Carson TL, Hidalgo B, Ard JD, Affuso O. Dietary interventions and quality of life: a systematic review of the literature. J Nutr Educ Behav 2014; 46: 90–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kroes M, Osei‐Assibey G, Baker‐Searle R, Huang J. Impact of weight change on quality of life in adults with overweight/obesity in the United States: a systematic review. Curr Med Res Opin 2016; 32: 485–508. [DOI] [PubMed] [Google Scholar]
- 18. Maciejewski ML, Patrick DL, Williamson DF. A structured review of randomized controlled trials of weight loss showed little improvement in health‐related quality of life. J Clin Epidemiol 2005; 58: 568–578. [DOI] [PubMed] [Google Scholar]
- 19. Magallares A, Schomerus G. Mental and physical health‐related quality of life in obese patients before and after bariatric surgery: a meta‐analysis. Psychol Health Med 2015; 20: 165–176. [DOI] [PubMed] [Google Scholar]
- 20. Lindekilde N, Gladstone BP, Lubeck M et al The impact of bariatric surgery on quality of life: a systematic review and meta‐analysis. Obes Rev 2015; 16: 639–651. [DOI] [PubMed] [Google Scholar]
- 21. Andersen JR, Aasprang A, Karlsen TI et al. Health‐related quality of life after bariatric surgery: a systematic review of prospective long‐term studies. Surg Obes Relat Dis 2015; 11: 466–473. [DOI] [PubMed] [Google Scholar]
- 22. Jumbe S, Bartlett C, Jumbe SL, Meyrick J. The effectiveness of bariatric surgery on long term psychosocial quality of life – A systematic review. Obes Res Clin Pract 2015; 10: 225–242. [DOI] [PubMed] [Google Scholar]
- 23. Ding SA, Simonson DC, Wewalka M et al Adjustable gastric band surgery or medical management in patients with type 2 diabetes: a randomized clinical trial. J Clin Endocrinol Metab 2015; 100: 2546–2556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Halperin F, Ding S, Simonson DC et al Roux‐en‐Y gastric bypass surgery or lifestyle with intensive medical management in patients with type 2 diabetes: feasibility and 1‐year results of a randomized clinical trial. JAMA Surg 2014; 149: 716–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kolotkin RL, Davidson LE, Crosby RD, Hunt SC, Adams TD. Six‐year changes in health‐related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis 2012; 8: 625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Adams TD, Pendleton RC, Strong MB et al Health outcomes of gastric bypass patients compared to nonsurgical, nonintervened severely obese. Obesity (Silver Spring) 2010; 18: 121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Adams TD, Davidson LE, Litwin SE et al Health benefits of gastric bypass surgery after 6 years. JAMA 2012; 308: 1122–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Adams TD. Two‐year changes in health‐related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis 2009; 5: 250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg 2016; 26: 395–409. [DOI] [PubMed] [Google Scholar]
- 30. Karlsson J, Taft C, Ryden A, Sjostrom L, Sullivan M. Ten‐year trends in health‐related quality of life after surgical and conventional treatment for severe obesity: the SOS Intervention Study. Int J Obes (Lond) 2007; 31: 1248–1261. [DOI] [PubMed] [Google Scholar]
- 31. Canetti L, Elizur Y, Karni Y, Berry EM. Health‐related quality of life changes and weight reduction after bariatric surgery vs. a weight‐loss program. Isr J Psychiatry Relat Sci 2013; 50: 194–200. [PubMed] [Google Scholar]
- 32. Canetti L, Berry EM, Elizur Y. Psychosocial predictors of weight loss and psychological adjustment following bariatric surgery and a weight‐loss program: the mediating role of emotional eating. Int J Eat Disord 2009; 42: 109–117. [DOI] [PubMed] [Google Scholar]
- 33. Driscoll S, Gregory DM, Fardy JM, Twells LK. Long‐term health‐related quality of life in bariatric surgery patients: a systematic review and meta‐analysis. Obesity (Silver Spring) 2016; 24: 60–70. [DOI] [PubMed] [Google Scholar]
- 34. Ahmed S, Berzon RA, Revicki DA et al, on behalf of the International Society for Quality of Life Research . The use of patient‐reported outcomes (PRO) within comparative effectiveness research: implications for clinical practice and health care policy. Med Care 2012; 50: 1060–1070. [DOI] [PubMed] [Google Scholar]
- 35. Oria HE, Moorehead MK. Updated bariatric analysis and reporting outcome system (BAROS). Surg Obes Relat Dis 2009; 5: 60–66. [DOI] [PubMed] [Google Scholar]
- 36. Ware JE Jr. SF‐36 health survey update. Spine (Phila PA 1976) 2000; 25: 3130–3139. [DOI] [PubMed] [Google Scholar]
- 37. Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res 2001; 9: 102–111. [DOI] [PubMed] [Google Scholar]
- 38. Evangelista LS, Heber D, Li Z et al. Reduced body weight and adiposity with a high‐protein diet improves functional status, lipid profiles, glycemic control, and quality of life in patients with heart failure: a feasibility study. J Cardiovasc Nurs 2009; 24: 207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Blissmer B, Riebe D, Dye G et al. Health‐related quality of life following a clinical weight loss intervention among overweight and obese adults: intervention and 24 month follow‐up effects. Health Qual Life Outcomes 2006; 4: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Davis NJ, Tomuta N, Isasi CR, Leung V, Wylie‐Rosett J. Diabetes‐specific quality of life after a low‐carbohydrate and low‐fat dietary intervention. Diabetes Educ 2012; 38: 250–255. [DOI] [PubMed] [Google Scholar]
- 41. Rejeski WJ, Focht BC, Messier SP et al. Obese, older adults with knee osteoarthritis: weight loss, exercise, and quality of life. Health Psychol 2002; 21: 419–426. [DOI] [PubMed] [Google Scholar]
- 42. Yancy WS Jr, Almirall D, Maciejewski ML et al. Effects of two weight‐loss diets on health‐related quality of life. Qual Life Res 2009; 18: 281–289. [DOI] [PubMed] [Google Scholar]
- 43. Ackermann RT, Edelstein SL, Narayan KM et al Changes in health state utilities with changes in body mass in the Diabetes Prevention Program. Obesity (Silver Spring) 2009; 17: 2176–2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Darga LL, Magnan M, Mood D et al. Quality of life as a predictor of weight loss in obese, early‐stage breast cancer survivors. Oncol Nurs Forum 2007; 34: 86–92. [DOI] [PubMed] [Google Scholar]
- 45. Fontaine KR, Barofsky I, Andersen RE et al Impact of weight loss on health‐related quality of life. Qual Life Res 1999; 8: 275–277. [DOI] [PubMed] [Google Scholar]
- 46. Heshka S, Anderson JW, Atkinson RL et al Weight loss with self‐help compared with a structured commercial program: a randomized trial. JAMA 2003; 289: 1792–1798. [DOI] [PubMed] [Google Scholar]
- 47. Imayama I, Alfano CM, Kong A et al Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: a randomized controlled trial. Int J Behav Nutr Phys Act 2011; 8: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pope L, Harvey‐Berino J, Savage P et al. The impact of high‐calorie‐expenditure exercise on quality of life in older adults with coronary heart disease. J Aging Phys Act 2011; 19: 99–116. [DOI] [PubMed] [Google Scholar]
- 49. Rippe JM, Price JM, Hess SA et al Improved psychological well‐being, quality of life, and health practices in moderately overweight women participating in a 12‐week structured weight loss program. Obes Res 1998; 6: 208–218. [DOI] [PubMed] [Google Scholar]
- 50. Ross KM, Milsom VA, Rickel KA et al The contributions of weight loss and increased physical fitness to improvements in health‐related quality of life. Eat Behav 2009; 10: 84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. von Gruenigen VE, Gibbons HE, Kavanagh MB et al. A randomized trial of a lifestyle intervention in obese endometrial cancer survivors: quality of life outcomes and mediators of behavior change. Health Qual Life Outcomes 2009; 7: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Williamson DA, Rejeski J, Lang W et al Impact of a weight management program on health‐related quality of life in overweight adults with type 2 diabetes. Arch Intern Med 2009; 169: 163–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Barham K, West S, Trief P et al. Diabetes prevention and control in the workplace: a pilot project for county employees. J Public Health Manag Pract 2011; 17: 233–241. [DOI] [PubMed] [Google Scholar]
- 54. Ladson G, Dodson WC, Sweet SD et al The effects of metformin with lifestyle therapy in polycystic ovary syndrome: a randomized double‐blind study. Fertil Steril 2011; 95: 1059–1066.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kennedy BM, Paeratakul S, Champagne CM et al A pilot church‐based weight loss program for African‐American adults using church members as health educators: a comparison of individual and group intervention. Ethn Dis 2005; 15: 373–378. [PubMed] [Google Scholar]
- 56. Malone M, Alger‐Mayer SA, Anderson DA. The lifestyle challenge program: a multidisciplinary approach to weight management. Ann Pharmacother 2005; 39: 2015–2020. [DOI] [PubMed] [Google Scholar]
- 57. Melanson KJ, Dell'Olio J, Carpenter MR, Angelopoulos TJ. Changes in multiple health outcomes at 12 and 24 weeks resulting from 12 weeks of exercise counseling with or without dietary counseling in obese adults. Nutrition 2004; 20: 849–856. [DOI] [PubMed] [Google Scholar]
- 58. Villareal DT, Banks M, Sinacore DR, Siener C, Klein S. Effect of weight loss and exercise on frailty in obese older adults. Arch Intern Med 2006; 166: 860–866. [DOI] [PubMed] [Google Scholar]
- 59. Villareal DT, Chode S, Parimi N et al Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med 2011; 364: 1218–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wolf AM, Conaway MR, Crowther JQ et al Translating lifestyle intervention to practice in obese patients with type 2 diabetes: Improving Control with Activity and Nutrition (ICAN) study. Diabetes Care 2004; 27: 1570–1576. [DOI] [PubMed] [Google Scholar]
- 61. Womble LG, Wadden TA, McGuckin BG et al. A randomized controlled trial of a commercial internet weight loss program. Obes Res 2004; 12: 1011–1018. [DOI] [PubMed] [Google Scholar]
- 62. Aasprang A, Andersen JR, Vage V, Kolotkin RL, Natvig GK. Five‐year changes in health‐related quality of life after biliopancreatic diversion with duodenal switch. Obes Surg 2013; 23: 1662–1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Zijlstra H, Larsen JK, Wouters EJM, van Ramshorst B, Geenen R. The long‐term course of quality of life and the prediction of weight outcome after laparoscopic adjustable gastric banding: a prospective study. Bariatric Surg Practi Patient Care 2013; 8: 18–22. [Google Scholar]
- 64. Mathus‐Vliegen EM, de Wit LT. Health‐related quality of life after gastric banding. Br J Surg 2007; 94: 457–465. [DOI] [PubMed] [Google Scholar]
- 65. Brunault P, Jacobi D, Léger J et al Observations regarding ‘Quality of Life’ and ‘Comfort with Food’ after bariatric surgery: comparison between laparoscopic adjustable gastric banding and sleeve gastrectomy. Obes Surg 2011; 21: 1225–1231. [DOI] [PubMed] [Google Scholar]
- 66. Raoof M, Neaslund I, Rask E et al Health‐related quality‐of‐life (HRQoL) on average of 12 years after gastric bypass surgery. Obes Surg 2015; 25: 1119–1127. [DOI] [PubMed] [Google Scholar]
- 67. Aftab H, Risstad H, Sovik TT et al Five‐year outcome after gastric bypass for morbid obesity in a Norwegian cohort. Surg Obes Relat Dis 2014; 10: 71–78. [DOI] [PubMed] [Google Scholar]
- 68. Terwee CB, Prinsen CA, Ricci Garotti MG et al. The quality of systematic reviews of health‐related outcome measurement instruments. Qual Life Res 2016; 25: 767–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Doll HA, Petersen SE, Stewart‐Brown SL. Obesity and physical and emotional well‐being: associations between body mass index, chronic illness, and the physical and mental components of the SF‐36 questionnaire. Obes Res 2000; 8: 160–170. [DOI] [PubMed] [Google Scholar]
- 70. Ul‐Haq Z, Mackay DF, Fenwick E, Pell JP. Impact of metabolic comorbidity on the association between body mass index and health‐related quality of life: a Scotland‐wide cross‐sectional study of 5,608 participants. BMC Public Health 2012; 12: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kolotkin RL, Crosby RD, Gress RE et al. Health and health‐related quality of life: differences between men and women who seek gastric bypass surgery. Surg Obes Relat Dis 2008; 4: 651–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Zabelina DL, Erickson AL, Kolotkin RL, Crosby RD. The effect of age on weight‐related quality of life in overweight and obese individuals. Obesity (Silver Spring) 2009; 17: 1410–1413. [DOI] [PubMed] [Google Scholar]
- 73. Kolotkin RL, Gadde KM, Peterson CA, Crosby RD. Health‐related quality of life in two randomized controlled trials of phentermine/topiramate for obesity: what mediates improvement? Qual Life Res 2016; 25: 1237–1244. [DOI] [PubMed] [Google Scholar]
- 74. Bays H, Pi‐Sunyer X, Hemmingsson JU et al Liraglutide 3.0 mg for weight management: weight‐loss dependent and independent effects. Curr Med Res Opin 2017; 33: 225–229. [DOI] [PubMed] [Google Scholar]
- 75. Latner JD, Mond JM, Vallance JK, Gleaves DH, Buckett G. Body checking and avoidance in women: associations with mental and physical health‐related quality of life. Eat Behav 2012; 13: 386–389. [DOI] [PubMed] [Google Scholar]
- 76. Latner JD, Barile JP, Durso LE, O'Brien KS. Weight and health‐related quality of life: the moderating role of weight discrimination and internalized weight bias. Eat Behav 2014; 15: 586–590. [DOI] [PubMed] [Google Scholar]
- 77. Levine MN, Ganz PA. Beyond the development of quality‐of‐life instruments: where do we go from here? J Clin Oncol 2002; 20: 2215–2216. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Overlap of studies included in the reviews.
Table S2. Health‐related quality‐of‐life measures.


