Abstract
Background
Disease risk calculators are increasingly web‐based, but previous studies have shown that risk information often poses problems for lay users.
Objective
To examine how lay people understand the result derived from an online cardiometabolic risk calculator.
Design
A qualitative study was performed, using the risk calculator in the Dutch National Prevention Program for cardiometabolic diseases. The study consisted of three parts: (i) attention: completion of the risk calculator while an eye tracker registered eye movements; (ii) recall: completion of a recall task; and (iii) interpretation: participation in a semi‐structured interview.
Setting and participants
We recruited people from the target population through an advertisement in a local newspaper; 16 people participated in the study, which took place in our university laboratory.
Results
Eye‐tracking data showed that participants looked most extensively at numerical risk information. Percentages were recalled well, whereas natural frequencies and verbal labels were remembered less well. Five qualitative themes were derived from the interview data: (i) numerical information does not really sink in; (ii) the verbal categorical label made no real impact on people; (iii) people relied heavily on existing knowledge and beliefs; (iv) people zoomed in on risk factors, especially family history of diseases; and (v) people often compared their situation to that of their peers.
Discussion and conclusion
Although people paid attention to and recalled the risk information to a certain extent, they seemed to have difficulty in properly using this information for interpreting their risk.
Keywords: informed decision making, lay perspective, patient education, prevention, risk communication
1. INTRODUCTION
Informing people about their personal risk plays a key role in the prevention of lifestyle‐related diseases, such as cardiovascular diseases (CVD), diabetes and chronic kidney disease (CKD).1, 2, 3, 4 For example, clinical guidelines in different countries stipulate that general practitioners practise cardiovascular risk assessment and communication.5, 6 Online personalized risk calculators are increasingly being used in this context, often as a first step in prevention programmes.7, 8 These risk calculators provide people with personalized information such as the risk factors (eg age, smoking, BMI) that modify their susceptibility, with numerical information about their likelihood of developing the illness within a particular time frame and with advice on how to reduce their risk. People are expected to use this information and obtain insight into their risk, thereby enabling them to make informed health‐related decisions, which would ultimately improve population health.9, 10
Precisely how an individual's personalized risk resulting from an online risk calculator should be communicated has become a crucial question.8, 11, 12 Although some risk formats (eg natural frequencies and some graphical formats in addition to numerical information) in general seem to evoke better risk understanding than other formats (eg percentages only),13, 14, 15 it remains unclear how the provided risk information supports an individual's understanding of their risk. Previous user tests have shown that risks presented as percentages in risk calculators often have unclear or ambiguous meaning for end‐users, even when accompanied by graphical information.8, 16, 17 Other more general problems revealed by such user tests are that the risk message does not necessarily match the individual's existing beliefs and expectations about risk factors, and that, perhaps partly as a result of this, many end‐users with relatively high risks tend to undervalue or normalize their risk.17, 18 Such problems are particularly urgent as many people, not only those with lower educational levels, have poor health literacy and numeracy skills,19, 20 thereby placing them at a higher risk of misinterpreting information and making non‐informed decisions.15 It is therefore important to investigate how end‐users of risk calculators make sense of their risk result and to improve risk communication accordingly.
To date, little qualitative work has been performed to investigate how people exactly understand risk information in risk calculators.4, 8, 17 Most of this research has employed think‐aloud protocols and/or user evaluations, but it can be questioned whether these methods fully capture how people understand risk information. User evaluations typically investigate the user‐friendliness of information from the perspective of end‐users themselves, which does not give a more “objective” assessment of how people understand information.14 Think‐aloud protocols provide insight into the thought processes of people who use information21, 22; although this can be useful in assessing how people understand the provided information, the method does not necessarily capture how people subsequently utilize this information to interpret and make sense of their risk. We therefore adopted a novel qualitative approach that followed different essential phases in the process of understanding risk information provided in a risk calculator. The aim of this study was to examine how lay people understand the result from the above‐mentioned online cardiometabolic risk calculator using eye tracking, a recall task and qualitative post‐test interview questions. We assumed that in order to understand their personal disease risk in a risk calculator, people have to (i) pay attention to essential information; (ii) be able to recall this essential information; and (iii) use this essential information in their risk interpretations. Previous qualitative studies did not adopt such a qualitative approach that specifically focused on these phases in the process of individual comprehension and interpretation, but rather focused on general reactions to provided information.
2. METHODS
2.1. Study design
Our case study involved the online risk calculator that is part of the Dutch National Prevention Program for CVD, type 2 diabetes and CKD. This risk calculator, which is the first step in the prevention programme, can be used by general practitioners to identify high‐risk individuals. General practitioners can invite patients between 45 and 65 years of age to fill out the risk calculator at home for a first risk estimation based on sex, age, smoking status, BMI, waist circumference and family history of type 2 diabetes and CVD.23 Only individuals whose test results reveal an elevated risk are advised to see their general practitioner for further screening. Figure 1 shows the risk communication in the risk calculator. The study was exempted from review by a medical research ethics committee in accordance with local regulatory guidelines and standards for human subjects’ protection in the Netherlands (Medical Research Involving Human Subjects Act (WMO), 2005).
Figure 1.
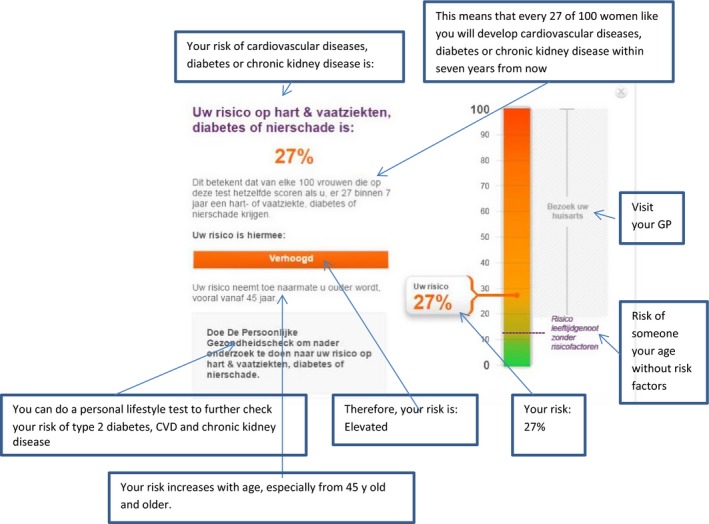
The risk communication in the risk calculator [Colour figure can be viewed at wileyonlinelibrary.com]
We performed a qualitative study consisting of three parts, corresponding to the assumed essential phases in the process of understanding risk information.
Attention: participants completed a risk calculator while an eye tracker (TOBII) registered their eye movements; the interviewer did not intervene in this phase.
Recall: participants were provided with a recall task after they had completed the risk calculator, assessing their recall of different parts of the risk information.
Interpretation: Semi‐structured questions were posed during a 30‐minute interview, focusing on participants’ subsequent risk interpretations.
We assumed that in order to understand their risk, people should, at a minimum: (i) pay attention to some of the numerical information to get an idea of the size of their risk24 and also of the verbal categorical label, bar graph or comparative risk information (the risk of someone of the same age without risk factors) that form part of the risk communication to provide intuitive or “gist” meaning of the number25; (ii) recall the size of their risk (ie in numbers) and some of the information aimed to provide intuitive meaning, for example the verbal label; and (iii) use this information as well as information about qualitative dimensions of risk (ie their personal risk factors, the controllability of their risk26, 27) to interpret and make sense of their risk result.
2.2. Recruitment and sample characteristics
We recruited people from the target population of the prevention programme (people aged between 45 and 60 years without a medical history of type 2 diabetes, CVD and CKD) through an advertisement placed in a free distributed local newspaper. This advertisement mentioned that the study would focus on people's opinions about health websites. A total of 21 people responded and were provided with further details. These 21 people were initially all willing to participate; 16 of them actually participated. The participants’ characteristics are presented in Table 1.
Table 1.
Participants’ characteristics
| Variable | N (%) |
|---|---|
| Age | |
| 45‐50 years | 6 (37%) |
| 51‐55 years | 6 (37%) |
| 56‐60 years | 1 (6%) |
| 60‐65 years | 3 (20%) |
| Gender | |
| Male | 3 (19%) |
| Female | 13 (81%) |
| Educational level | |
| Low (no or primary education) | 1 (6%) |
| Medium (secondary education) | 7 (44%) |
| High (tertiary education) | 8 (50%) |
| Subjective numeracya | M=3.5 (2.1‐5.1) |
| Subjective health literacyb | |
| Inadequate | 10 (63%) |
| Adequate | 6 (37%) |
| Result risk calculator | |
| No elevated risk | 4 (25%) |
| Slightly elevated risk | 10 (63%) |
| Elevated risk | 2 (13%) |
Based on the eight subjective numeracy items developed by Fagerlin et al.28 All questions use 6‐point Likert‐type scales with endpoints as marked (1‐6). A higher score indicates a higher subjective rating of numeracy abilities and preferences.
Based on the three subjective health literacy screening items developed by Chew et al.29: (i) “How often do you have someone help you read hospital materials?” (ii) “How confident are you filling out medical forms by yourself?” and (iii) “How often do you have problems learning about your medical condition because of difficulty understanding written information?”. Inadequate health literacy if answers other than “never” on items 1 or 3 and/or answers other than “extremely” or “quite a bit” on item 2.
2.3. Procedure
Participants were interviewed at the VU University. To make sure the participants would feel comfortable, the interviews were conducted in an attractive laboratory setting that was especially designed to facilitate laboratory research in a realistic environment. The interviewer (NB) informed participants about the online risk calculator and the aim of the interview and then instructed them about the use of the eye tracker and asked permission to audiotape the interviews. After providing written consent, the interviewer started the online risk calculator on the computer screen. Participants completed the risk calculator while an eye tracker registered their eye movements and fixations (part 1); in this phase, the interviewer sat a few metres behind the participant and did not intervene; she viewed the eye movements on a second screen. After completing the risk calculator, the interviewer provided the participant with a recall task (part 2, Section 2.4). Next, the interviewer conducted the semi‐structured interview using an interview guide (part 3, see Section 2.4). Finally, participants’ socio‐demographic characteristics (sex, age, educational level, language spoken at home), subjective numeracy28 and subjective health literacy29 were assessed in a short survey. Participants were thanked for their participation and were given a small financial reward (€20).
2.4. Materials
The online risk calculator communicates people's personalized risk in different formats on a single web page (Figure 1): a percentage (eg your risk is 14%), a natural frequency (eg 14 of 100 men/women like you will develop the diseases within 7 years from now), a bar graph, a categorical verbal label (eg your risk is “slightly elevated”) and comparative risk information (eg the risk of someone your age without risk factors is 10%). Information about the risk factors contributing to people's personal risk was provided on another web page. In part 2, we used a recall task that assessed participants’ recall of the personalized risk information as provided in Figure 1. A blank hard copy page of this web page was provided to participants (Figure 2) and they were asked to fill out their test results, that is the percentage, the natural frequency, the categorical verbal label and the statement on the right side of the bar graph.
Figure 2.
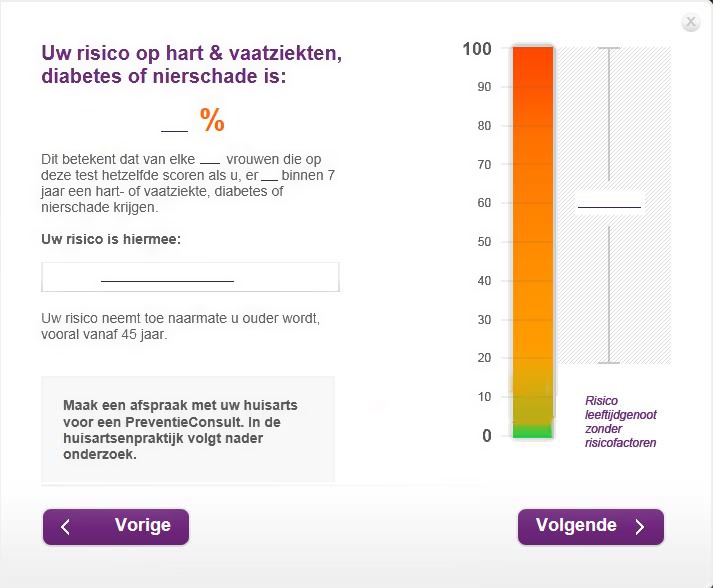
Blank hard copy page of the risk result as used in the recall task [Colour figure can be viewed at wileyonlinelibrary.com]
Part 3 used an interview guide specifically designed to let participants elaborate on their risk interpretations and to make sense of their test result. We first asked questions about how people perceived their risk after receiving their test result. Examples included: “How do you interpret your risk of getting type 2 diabetes, CVD and CKD?” “How likely do you think you are to develop one of these diseases and why?” In the second part, we again provided people with their personalized risk on the computer screen and compared it to people's answers to the recall task. We asked participants explicitly about perceived difficulties in completing the recall task and then together reviewed the different parts of the risk communication. Examples of interview questions were as follows: “What were your thoughts on seeing your risk percentage?” “How do you feel about having a risk that is elevated/slightly elevated/not elevated?”
2.5. Data analysis
All interviews were audio‐recorded and transcribed verbatim. We analysed the eye‐tracking data by searching for patterns in the individual absolute gaze duration heat maps (showing the observed and unobserved areas30) and individual gaze plots (showing gaze motions as a sequence of saccades and fixations31) of the web page showing people's risk result. While these analyses are well suited to shedding some light on the attention paid by people to the information, one should remain careful in interpreting the data, because heat maps and gaze plots cannot fully stand on their own.32 In making inferences about the eye‐tracking patterns in relation to risk understanding, we compared the eye‐tracking data to the recall data and the qualitative themes.
Analysis of the interview data in MAXQDA followed the phases of thematic analysis as described by Braun and Clarke.33 Initially, three researchers (NB, OD and MH) read all transcriptions. Observations made by the interviewer (NB) during the interview about how respondents interpreted and used the risk information were discussed. Subsequently, all interviews were coded by two researchers independently (11 were performed by NB and OD, and five were performed by NB and MH). First, the interviews of two different participants were each coded openly by NB and OD (ie we assigned preliminary codes to text fragments). This open coding meant that we had no pre‐existing coding or classification scheme. After discussing these codes, the three researchers further coded the remaining interviews while being able to access the codes of the first two interviews in an Excel sheet. When differences between the codes of the different researchers occurred, these were discussed in consensus meetings in which the two researchers participated; sometimes, the code of one of the researchers was adopted, and sometimes, a new code was created. In all cases, we were able to reach consensus. Next, the data were axially coded (integrating codes in broader related concepts), which resulted in a hierarchical list of codes. Based on this, initial themes were defined by two researchers (NB and OD). These themes were discussed with the other members of the research team (MH and DT) and the eye‐tracking and recall data were used to further refine the themes where necessary.
3. RESULTS
We will first describe the attention paid by people to the information, followed by their recall of that information. Next, people's risk interpretations are described by means of five qualitative themes.
3.1. Attention for information
We used the eye‐tracking data of 11 participants; of the remaining five participants, the data were of insufficient quality due to failed calibration. Note that this only concerned the eye‐tracking data; the recall and interview data were complete and fully analysed for 16 participants. Supplementary file 1 provides one example of a heat map and one example of a gaze plot, both of which were quite representative for our participants. Supplementary file 2 provides three individual gaze plots of three different participants. Both the heat maps and the gaze plots revealed that, overall, participants most extensively looked at the numerical risk information (percentage and frequency) and also, to some extent, at the verbal label. Participants particularly looked at the natural frequency in detail: many participants read this information 2‐3 times, as the gaze plots showed, which may suggest that this was hard to understand. They paid less attention to the bar graph, which is an important result because the bar graph was explicitly meant as a graphical aid to provide intuitive meaning to the information. Participants did look at the comparative risk information, which was another attempt to provide such intuitive meaning (bottom of bar graph), although not very extensively. Notably, participants rarely exactly read out their own risk from the bar; although most participants did look at the percentage displayed next to the bar, they did not place it on a scale from 0% to 100% (see the examples in supplementary file 2).
3.2. Information recall
Table 2 presents the information recall of all participants. Percentages were overall remembered well, whereas natural frequencies and verbal labels were remembered less well. Only one person adequately recalled the statement at the bar graph (“visit your GP”).
Table 2.
Recall of different parts of the risk information
| Participant | Percentage | Natural frequency | Verbal categorical level | Statement at the bar graph (visit your GP) |
|---|---|---|---|---|
| 1 (A001) | + | − Filled in nothing | − Filled in nothing | − Filled in nothing |
| 2 (A003) | + | ± Only filled in numerator and not the denominator | − Filled in “light risk” instead of “slightly elevated risk” | − Filled in nothing |
| 3 (A004) | + | − Filled in nothing | − Filled in nothing | − Filled in nothing |
| 4 (A005) | + | − Filled in 100 (numerator) and 100 (denominator) | + | − Filled in nothing |
| 5 (A007) | + | + | + | − Filled in nothing |
| 6 (A008) | − Filled in nothing | + | + | − Filled in her weight instead of the statement |
| 7 (A009) | + | − Filled in 5 out of 7 | − Filled in the percentage again | − Filled in nothing |
| 8 (A010) | + | + | − Filled in “small risk” instead of “slightly elevated risk” | − Filled in nothing |
| 9 (A011) | + | − Filled in nothing | − Filled in “marginal risk” instead of “not elevated” | − Filled in nothing |
| 10 (A012) | − Filled in 60% instead of 23% | − Filled in nothing | − Filled in nothing | − Filled in nothing |
| 11 (A013) | + | − Filled in nothing | − Filled in “small risk” instead of “slightly elevated risk” | − Filled in nothing |
| 12 (A015) | + | + | + | − Filled in nothing |
| 13 (A017) | + | − Filled in nothing | − Filled in nothing | − Filled in nothing |
| 14 (A018) | + | + | − Filled in nothing | − Filled in nothing |
| 15 (A019) | + | − Filled in nothing | − Filled in “light risk” instead of “slightly elevated risk” | − Filled in nothing |
| 16 (A020) | + | + | + | + |
+, correctly recalled; −, incorrectly recalled or not recalled.
3.3. Risk interpretation
We identified five qualitative themes related to how people interpreted and made sense of their personalized disease risk information. The next section describes these themes and their corresponding subthemes, illustrated by respondents’ quotes in Table 3.
Table 3.
Qualitative themes relating to people's risk interpretations, illustrated by key quotes from participants
| Qualitative theme | Participant's quote | Participant's characteristics |
|---|---|---|
| Theme 1: numerical information does not really sink in | ||
| Subtheme 1a: struggling to comprehend and recall numerical information |
|
Woman, 64 years of age, medium educational level, inadequate subjective health literacy, risk of 23% (elevated) |
|
Woman, 45 years of age, medium educational level, adequate subjective health literacy, risk of 5% (slightly elevated) | |
| Subtheme 1b: risk undervaluation |
|
Woman, 58 years of age, low educational level, inadequate subjective health literacy, risk of 12% (slightly elevated) |
|
Woman, 52 years of age, high educational level, adequate subjective health literacy, risk of 7% (slightly elevated) | |
| Theme 2: the verbal categorical label made no real impact on people |
|
Woman, 53 years of age, high educational level, adequate subjective health literacy, risk of 13% (slightly elevated) |
| Theme 3: people relied heavily on knowledge and beliefs about risk factors | ||
| Subtheme 3a: reliance on knowledge and beliefs about risk factors |
|
Man, 49 years of age, medium educational level, inadequate subjective health literacy, risk of 6% (not elevated) |
|
Woman, 58 years of age, low educational level, inadequate subjective health literacy, risk of 12% (slightly elevated) | |
| Subtheme 3b: Reliance on knowledge and beliefs about (lack of) complaints |
|
Woman, 58 years of age, low educational level, inadequate subjective health literacy, risk of 12% (slightly elevated) |
| Subtheme 3c: Reliance on knowledge and beliefs about the diseases |
|
Woman, 54 years of age, medium educational level, inadequate subjective health literacy, risk of 7% (slightly elevated) |
|
Woman, 45 years of age, medium educational level, adequate subjective health literacy, risk of 5% (slightly elevated). | |
|
Woman, 61 years of age, medium educational level, inadequate subjective health literacy, risk of 23% (elevated) | |
| Theme 4: people zoomed in on risk factors, especially family history of diseases | ||
| Subtheme 4a: focus on a diverse range of risk factors, including factors that were not part of the risk calculator |
|
Woman, 64 years of age, medium educational level, inadequate subjective health literacy, risk of 23% (elevated) |
|
Woman, 45 years of age, medium educational level, adequate subjective health literacy, risk of 5% (slightly elevated) | |
|
Woman, 53 years of age, high educational level, adequate subjective health literacy, risk of 13% (slightly elevated) | |
|
Woman, 61 years of age, medium educational level, inadequate subjective health literacy, risk of 23% (elevated) | |
| Subtheme 4b: family history of diseases was a salient risk factor |
|
Man, 49 years of age, medium educational level, adequate subjective health literacy, risk of 6% (not elevated) |
|
Woman, 50 years of age, high educational level, inadequate subjective health literacy, risk of 6% (slightly elevated) | |
| Subtheme 4c: interest in more information about risk factors |
|
Woman, 52 years of age, high educational level, adequate subjective health literacy, risk of 7% (slightly elevated) |
| Theme 5: people often compared their situation to that of their peers |
|
Man, 49 years of age, medium educational level, adequate subjective health literacy, risk of 6% (not elevated) |
|
Woman, 58 years of age, low educational level, inadequate subjective health literacy, risk of 12% (slightly elevated) | |
|
Woman, 55 years of age, medium educational level, inadequate subjective health literacy, risk of 6% (not elevated) | |
3.3.1. Theme 1: numerical information does not really sink in
We found that many participants struggled to adequately comprehend and recall the numbers provided, including the probability information (subtheme 1a). Furthermore, even if people did focus to some extent on the numerical information, for example as a result of probing questions, many participants tended to undervalue these numbers and seemed to interpret the risk as less severe than medical experts (subtheme 1b), indicating that the numerical information did not fully sink in. Theme 1 was related to themes 3 and 4 in the sense that people did not rely heavily on the numerical information in making sense of their risk, but rather on other aspects such as information about risk factors (Theme 4) as well as on existing knowledge and beliefs about a number of topics (Theme 3). Eye‐tracking data and recall data showed that participants did look at and remember numerical information, which suggests that participants did process this information to some extent.
Subtheme 1a: struggling to comprehend and recall numerical information
Many people struggled with comprehending and recalling the provided numerical information correctly. This became clear from post‐test interview questions about how people interpreted the numerical information, but also from people's responses to the recall task. Some participants tried to unite the percentage and the frequency of the probability information, which often proved hard for them. In addition, probability information was also confused with other numerical information, such as the time frame of the risk (7 years) and people's BMI. It was noticeable, in this respect, that participants did adequately recall the risk percentage.
Subtheme 1b: risk undervaluation
It also became clear that participants perceived relatively high risks (eg ranging from 12% to 23%) as rather low, and saw no reason for worry. This seemed to occur partly because of difficulties in interpreting numerical information (subtheme 1a), but also because people used their own risk factors in risk interpretations more than the size of the risk (subtheme 3a).
People also spontaneously talked about reasons why they felt that their risk was actually different from what was communicated in the test, causing them to downplay the size of their risk. For example, some participants believed that because they felt healthy, the risk that was communicated to them was an overestimation of their actual risk. Another reason why risk undervaluation might have occurred can be ascribed to the way the risk was presented; for example, the bar graph ascended all the way up to 100%. Although a bar graph that goes up to 100% is of course an adequate way to present percentages, risks of 15% or 20%, which would be considered severe risks by experts, can seem minor because they are in the lower part of the bar.
3.3.2. Theme 2: the verbal categorical label made no real impact on people
Like the numerical risk information, the verbal categorical risk label (either “elevated,” “slightly elevated” or “not elevated”) made no real impact on participants. From an expert/epidemiological perspective, these labels are important information because they form the basis for deciding who needs further screening and who does not. However, our participants did not seem to regard this label as an essential element of their test result and recall data showed that many did not recall the label. Several participants with a “slightly elevated risk” who did not recall their verbal label correctly thought their label was “minor” or “small”. This might be related to the fact that people tended to undervalue their risk (subtheme 1b).
3.3.3. Theme 3: people relied heavily on existing knowledge and beliefs
We found that participants primarily relied on their existing knowledge and beliefs to interpret their risk, rather than on the actual risk information provided (see themes 1 and 2). Many participants used their knowledge about risk factors to make sense of their own risk (subtheme 3a). Many participants also used their perceived physical complaints (or lack thereof) to judge their susceptibility, rather than the size of the risk as communicated in the risk calculator (subtheme 3b). Related to subthemes 3a and 3b, a third subtheme was that people's perceived susceptibility also depended on beliefs about, or “images” of, the diseases (subtheme 3c).
Subtheme 3a: reliance on knowledge and beliefs about risk factors
All participants more or less knew which risk factors from the risk calculator would apply to them personally and would thus contribute to their risk. Many participants, both with relatively low and with relatively high risks, relied heavily on such own knowledge and beliefs about risk factors, rather than on the numerical risk information provided.
Subtheme 3b: reliance on knowledge and beliefs about complaints (or lack thereof)
Many participants also used their perceived complaints (or lack thereof) to judge their susceptibility. It seemed that many participants believed that as long as they felt healthy and were free from medical/physical complaints, their risk would be rather low. The risk information did not affect these beliefs and perceptions.
Subtheme 3c: reliance on knowledge and beliefs about the diseases
Participants’ perceived susceptibility also partly depended on existing beliefs about the diseases in the risk calculator, which were, in turn, related to how familiar these were to people. In general, participants thought that cardiometabolic diseases were not very severe, for example in comparison with cancer. Several participants also indicated, without being prompted, that they had no clear picture of cardiometabolic diseases, especially of type 2 diabetes and CKD.
3.3.4. Theme 4: people zoomed in on risk factors, especially family history of diseases
Apart from using existing knowledge and beliefs about risk factors in interpreting their personal risk as provided in the risk calculator (subtheme 3a), participants in general made numerous spontaneous causal attributions to a diverse range of risk factors, included or not included in the risk calculator (subtheme 4a). Particularly, family history seemed to be salient in participants’ risk perceptions and interpretations (subtheme 4b). Another indication that people focused on risk factors was that they wanted to have more detailed information about risk factors (subtheme 4c).
Subtheme 4a: focus on a diverse range of risk factors, including factors that were not part of the risk calculator
Unsolicited, participants made causal attributions with respect to ageing, overweight/obesity, smoking and family history of type 2 diabetes and CVD (all part of the risk calculator), but also with respect to an unhealthy diet, lack of physical activity (not explicitly in the test but underlying factors of overweight/obesity) as well as to alcohol use and stress (not part of the risk calculator). Participants’ perceived susceptibility also largely depended on the presence or absence of such risk factors, including those not included in the test (eg blood pressure, stress).
Subtheme 4b: family history of diseases was a salient risk factor
In particular, family history appeared to be prominent in participants’ risk perceptions and interpretations. Both the presence and absence of a family history of cardiometabolic diseases were used in risk interpretation. Actual examples in the family led to a clearer picture of the diseases, compared with people who had no examples in the family. These examples were often not the direct relatives referred to in the test, but having such examples nevertheless contributed to perceptions of susceptibility.
Subtheme 4c: interest in more information about risk factors
People wanted to have more detailed information about risk factors, both those included in the risk calculator, especially lifestyle factors, and those not included.
3.3.5. Theme 5: people often compared their situation to that of their peers
Participants spontaneously compared their risk to that of peers, to make sense of their own risk result. They had stereotypical beliefs about “which people have an elevated risk” and they compared their own risk to these stereotypes to judge the severity of their own risk. This tendency seemed to be related to a risk undervaluation (subtheme 1b), although not all participants who compared their risk to the risk of (hypothetical) other people undervalued their own risk. While participants were curious to know the risk of others, our eye‐tracking data showed that they hardly looked at the comparative risk information available in the bar graph (supplementary file 2).
4. DISCUSSION
This study aimed to examine how lay people understand and make sense of the result from a disease risk calculator. We combined eye tracking with a recall task and qualitative post‐test interview questions in a qualitative study using a Dutch cardiometabolic risk calculator. Our findings showed that when making sense of their risk, people did not make extensive use of the risk information provided. Neither the numerical risk information nor the categorical verbal labels seemed to make a real impact on people's risk perceptions and interpretations, although they did look at and recall this information to a certain extent. Instead, people primarily relied on existing knowledge and beliefs, for example about the presence or absence of risk factors or about the severity of diseases.
The finding that participants relied so heavily on existing knowledge and beliefs and that, as a result, their perceptions and interpretations seemed hardly affected by the information provided was significant. Although research about this topic is scarce (see review of Sheridan2), previous studies have shown that giving people information about their cardiovascular disease risk can alter their risk perceptions. One explanation for our finding that the risk information hardly affected people's perceptions might be that the risk communication from our case example was suboptimal, and did not effectively guide end‐users to essential information about the size and severity of their risk. We did find that people attended to and recalled aspects of the provided risk information, most notably the risk percentage, but this did not always occur without any difficulties. Although we do not know for sure why so few participants filled in the natural frequency in our recall task (eg it might be that they believed that they did not have to fill in this frequency because it is essentially the same information as the percentage), it was noticeable that this natural frequency was badly recalled and discussed by participants. Overall, indeed, people had difficulties with interpreting and providing meaning to the numerical information, a result which has previously been found in the general field of risk communication34 as well as in studies that specifically focused on online disease risk calculators.4, 17 It was noticeable that people made limited use of the verbal categorical label and the graphical bar chart, which are formats explicitly intended to provide intuitive meaning to the numbers. In addition, the comparative risk information was often neglected, while it obviously has the potential to provide meaning to people's personalized risk.35 Graphical risk formats do have the potential to attract end‐users’ attention35 and to support their understanding.14, 36 We can only speculate about the reasons why our participants discounted this information. It might be that people themselves did not experience any problems in comprehending the percentage, and therefore found it unnecessary to also view the bar graph that again emphasized the percentage. The neglect of the verbal categorical label could indicate that the label itself had insufficient meaning or that the display of the label was suboptimal (use of colour, font, shading, etc.). Another explanation may be that the other cues on the page distracted from the verbal message. More in general, the total amount of information on the page may have been too much for people, leading them to neglect some parts of it. It is interesting to note that most experiments testing the effects of visual formats typically use hypothetical scenarios, while in our study people were confronted with their own actual risk. This may make a difference regarding how people use particular pieces of information.
Participants’ reliance on existing knowledge and beliefs might also reflect a more inherent tendency in people that is not particularly related to how information is communicated. It is known that existing knowledge and beliefs in general are very influential in shaping people's perceptions of and reactions to health and illness.37 Particularly when new information does not fit existing knowledge and beliefs, as was the case for many of our participants, it is likely that new information does not have much value for people38 and that people become sceptical about it.39 Several previous studies testing different risk formats have also shown that both risk perceptions and subsequent decisions of people are more influenced by their perceptions of individual risk factors, the experience of symptoms, as well as by negative emotions than by the size of their risk.4, 18, 40, 41 Our findings indeed suggest that people have salient knowledge and beliefs about particular risk factors and health symptoms in general. New information about the size of cardiometabolic risk is probably interpreted in the light of already existing beliefs or “mental models”.
One particularly salient aspect of people's existing beliefs that might be interesting in the light of better risk communication was having a family history of diseases. Although the risk calculator provided reliable information by using single enquiries for family history, our participants were rather sceptical about this “small set” of questions. Furthermore, participants talked a lot about family history in their answers to interview questions about their risk interpretations, which indicated that family history largely influenced their perceived susceptibility. A similar finding has been previously reported in the context of a breast cancer risk calculator.18 A more detailed family history assessment might lead to better use of the risk information, because it directly increases the perceived relevance of information and, by doing so, probably also increases people's motivation to process the information.42 A previous study also revealed that a detailed familial risk questionnaire contributed to users’ risk acceptance and motivation to adapt healthier lifestyles among people with a positive family history.43 An important caveat is that putting more emphasis on family history of diseases in risk communication may have reverse effects for people without a family history of diseases who do have other risk factors. Previous studies have demonstrated that the absence of diseases in the family can lead to low perceptions of risk.44, 45
4.1. Strengths and limitations
Our study might be limited by the fact that participants were all people who were interested in health websites, as we recruited them through an advertisement that mentioned health websites. A further limitation was that the eye‐tracking data of several participants (N=5) were of insufficient quality due to failed calibration. We should thus be cautious in drawing firm conclusions about people's attention for risk information. Another limitation is that we did not ask participants about their knowledge or basic perceptions of risk before they completed the risk calculator. Had we done so, we might have gained more insight into how pre‐existing beliefs influenced people's risk interpretations. An important strength of this study is that we used a novel approach to test how people interpret and make sense of their disease risk, that is a combination of eye tracking with a recall task and qualitative post‐test interview questions. This approach provided us with valuable insights into how people used the risk information from the risk calculator and how they interpreted their risk of cardiometabolic diseases.
5. CONCLUSION
Although people pay attention to and recall risk information in an online risk calculator to a certain extent, they do not seem to optimally use it in their risk interpretations. Risk communication in an online disease risk calculator could be improved by building on people's existing knowledge and beliefs (eg about risk factors such as family history of diseases), by providing clear, more elaborate information about the diseases and using alternative graphical formats of numerical risk.
Supporting information
ACKNOWLEDGEMENTS
All participants are thanked for their participation.
Damman OC, Bogaerts NMM, van den Haak MJ, Timmermans DRM. How lay people understand and make sense of personalized disease risk information. Health Expect. 2017;20:973‐983. https://doi.org/10.1111/hex.12538
Funding information
This study was funded by The Netherlands Organisation for Scientific Research (NWO) within the programme “Comprehensible Language and Effective Communication.” The Dutch Diabetes Research Foundation, the Dutch Heart Foundation and the Dutch Kidney Foundation also contributed financially to the project. The Intertain Lab of the VU University in Amsterdam, the Netherlands, allowed us to use their laboratory setting and Tobii eye tracker free of charge.
REFERENCES
- 1. Koelewijn‐van Loon MS, Van der Weijden T, Van Steenkiste B, et al. Involving patients in cardiovascular risk management with nurse‐led clinics: a cluster randomized controlled trial. Can Med Assoc J. 2009;181:E267–E274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sheridan SL, Viera AJ, Krantz MJ, et al. The effect of giving global coronary risk information to adults: a systematic review. Arch Intern Med. 2010;170:230–239. [DOI] [PubMed] [Google Scholar]
- 3. Soureti A, Hurling R, Murray P, van Mechelen W, Cobain M. Evaluation of a cardiovascular disease risk assessment tool for the promotion of healthier lifestyles. Eur J Cardiovasc Prev Rehabil. 2010;17:519–523. [DOI] [PubMed] [Google Scholar]
- 4. Nolan T, Dack C, Pal K, et al. Patient reactions to a web‐based cardiovascular risk calculator in type 2 diabetes: a qualitative study in primary care. Br J Gen Pract. 2015;65:e152–e160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Greenland JS, Alpert GA, Beller EJ, et al. ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guideline. Circulation. 2010;122:e584–e636. [DOI] [PubMed] [Google Scholar]
- 6. Nielen MMJ, Assendelft WJJ, Drenthen AJM, Van den Hombergh P, Van Dis I, Schellevis FG. Primary prevention of cardiometabolic diseases in general practice: a Dutch survey of attitudes and working methods of general practitioners. Eur J Gen Pract. 2010;16:139–142. [DOI] [PubMed] [Google Scholar]
- 7. Laan EK, Kraaijenhagen RA, Peek N, et al. Effectiveness of a web‐based health risk assessment with individually‐tailored feedback on lifestyle behaviour: study protocol. BMC Public Health. 2012;19:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bonner C, Jansen J, Newell B, et al. I don't believe it, but i'd better do something about it: patient experiences of online heart age risk calculators. J Med Internet Res. 2014;16:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Waters EA, Sullivan HW, Nelson W, Hesse BW. What is my cancer risk? How internet‐based cancer risk assessment tools communicate individualized risk estimates to the public: content analysis. J Med Internet Res. 2009;11:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Holmberg C, Harttig U, Schulze MB, Boeing H. The potential of the Internet for health communication: the use of an interactive on‐line tool for diabetes risk prediction. Patient Educ Couns. 2011;83:106–112P. [DOI] [PubMed] [Google Scholar]
- 11. Witteman HO, Zikmund‐Fisher BJ, Waters EA, Gavaruzzi T, Fagerlin A . Risk estimates from an online risk calculator are more believable and recalled better when expressed as integers. J Med Internet Res. 2011;13:e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zikmund‐Fisher BJ, Dickson M, Witteman HO. Cool but counterproductive: interactive, Web‐based risk communications can backfire. J Med Internet Res. 2011;13:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Waldron CA, van der Weijden T, Ludt S, Gallacher J, Elwyn G. What are effective strategies to communicate cardiovascular risk information to patients? A systematic review. Patient Educ Couns. 2011;82:169–181. [DOI] [PubMed] [Google Scholar]
- 14. Trevena LJ, Zikmund‐Fisher BJ, Edwards A, et al. Presenting quantitative information about decision outcomes: a risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak. 2013;13(Suppl 2):S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oudhoff JP, Timmermans DR. The effect of different graphical and numerical likelihood formats on perception of likelihood and choice. Med Decis Making. 2015;35:487–500. [DOI] [PubMed] [Google Scholar]
- 16. Farrimond H, Saukko PM, Qureshi N, Evans PH. Making sense of being at ‘high risk’ of coronary heart disease within primary prevention. Psychol Health. 2010;25:289–304. [DOI] [PubMed] [Google Scholar]
- 17. Damman OC, Bogaerts NMM, Van Dongen D, Timmermans DRM. Barriers in using cardiometabolic risk information among consumers with low health literacy. Br J Health Psychol. 2016;21:135–156. [DOI] [PubMed] [Google Scholar]
- 18. Scherer LD, Ubel PA, McClure J, et al. Belief in numbers: when and why women disbelieve tailored breast cancer risk statistics. Patient Educ Couns. 2013;92:253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: theory and practice. Ann Behav Med. 2008;35:261–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Van der Heide I, Rademakers J, Schipper M, Droomers M, Sørensen K, Uiters E. Health literacy of Dutch adults: a cross sectional survey. BMC Public Health. 2013;13:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ericsson KA, Simon HA. Protocol Analysis: Verbal Reports as Data. Cambridge, MA: MIT Press; 1993. [Google Scholar]
- 22. Van den Haak MJ, De Jong MDT, Schellens PJ. Retrospective versus concurrent think‐aloud protocols: testing the usability of an online library catalogue. Behav Inform Technol. 2003;22:339–351. [Google Scholar]
- 23. Dekker JM, Alssema M, Janssen PGH, Van der Paardt M, Festen CSS, Van Oosterhout MJW. NHG‐standard prevention consultation cardiometabolic risk from the Dutch College of General Practitioners [in Dutch]. Huisarts en Wetenschap. 2011;54:138–155. [Google Scholar]
- 24. Weinstein ND. What does it mean to understand a risk? Evaluating risk comprehension J Natl Cancer Inst Monogr. 1999;25:15–20. [DOI] [PubMed] [Google Scholar]
- 25. Zikmund‐Fisher BJ. The right tool is what they need, not what we have: a taxonomy of appropriate levels of precision in patient risk communication. Med Care Res Rev. 2013;70(1 Suppl):37S–49S. [DOI] [PubMed] [Google Scholar]
- 26. Cameron L. Conceptualizing and assessing risk perceptions: a self‐regulatory perspective Paper Presented at the Conceptualizing and Measuring Risk Perceptions Workshop. Washington, DC: Division of Cancer Control and Population Sciences, National Cancer Institute; 2003. [Google Scholar]
- 27. Damman OC, Timmermans DR. Educating health consumers about cardiometabolic health risk: what can we learn from lay mental models of risk? Patient Educ Couns. 2012;89:300–308. [DOI] [PubMed] [Google Scholar]
- 28. Fagerlin A, Zikmund‐Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale (SNS). Med Decis Making. 2007;27:672–680. [DOI] [PubMed] [Google Scholar]
- 29. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 30. Špakov O, Miniotas D. Visualization of eye gaze data using heat maps. Electron Electr Eng. 2007;2:55–58. [Google Scholar]
- 31. Asan O, Yang Y. Using eye trackers for usability evaluation of health information technology: a systematic literature review. JMIR Hum Factors. 2015;2:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bojko A. Informative or misleading? Heatmaps deconstructed In: Jacko J.A. (eds) Human‐Computer Interaction. New Trends. HCI 2009. Lecture Notes in Computer Science, vol 5610. Springer, Berlin, Heidelberg. [Google Scholar]
- 33. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 34. Reyna V, Brainerd CJ. The importance of mathematics in health and human judgment: numeracy, risk communication, and medical decision making. Learn Individ Differ. 2007;17:147–159. [Google Scholar]
- 35. Waters EA, McQueen A, Cameron LD. Perceived risk and health risk communication In: Hamilton H. & Chou S. (Eds). The Handbook of Language and Health Communication, Routledge Press, 2013. [Google Scholar]
- 36. Smerecnik CM, Mesters I, Kessels LT, Ruiter RA, De Vries NK, De Vries H. Understanding the positive effects of graphical risk information on comprehension: measuring attention directed to written, tabular, and graphical risk information. Risk Anal. 2010;30:1387–1398. [DOI] [PubMed] [Google Scholar]
- 37. Leventhal H, Nerenz D. The assessment of illness cognition In: Karoly P, ed. Measurement Strategies in Health Psychology. New York, NY: Wiley; 1985:517–555. [Google Scholar]
- 38. Morgan MG, Fischhoff B, Bostrom A, Atman CJ. Risk Communication. A Mental Models Approach. New York, NY: Cambridge University Press; 2002. [Google Scholar]
- 39. Ditto PH, Lopez DF. Motivated skepticism: use of differential decision criteria for preferred and nonpreferred conclusions. J Pers Soc Psychol. 1992;63:568. [Google Scholar]
- 40. Bonner C, Jansen J, McKinn S, et al. How do general practitioners and patients make decisions about cardiovascular disease risk? Health Psychol. 2015;34:253–261. [DOI] [PubMed] [Google Scholar]
- 41. Holmberg C. Decision making in the context of breast cancer chemoprevention: patient perceptions and the meaning of risk. Am Soc Clin Oncol Educ Book. 2015;35:e59–e64. [DOI] [PubMed] [Google Scholar]
- 42. Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. Adv Exp Soc Psychol. 1986;19:123–205. [Google Scholar]
- 43. Wijdenes M, Henneman L, Dondorp WJ, Cornel MC, Timmermans DR. Users evaluate a detailed familial risk questionnaire as valuable and no more time consuming than a simple enquiry in a web‐based diabetes risk assessment tool. Public Health 2016;130:87–90. [DOI] [PubMed] [Google Scholar]
- 44. Pijl M, Henneman L, Claassen L, Detmar SB, Nijpels G, Timmermans DR. Family history of diabetes: exploring perceptions of people at risk in the Netherlands. Prev Chronic Dis. 2009;6:A54. [PMC free article] [PubMed] [Google Scholar]
- 45. Walter FM, Emery J, Sanderson S, Sutton S. Determinants of familial risk perception of common diseases. Eur J Hum Genet. 2006;14:s408. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


