Abstract
A 3-D scaffold that simulates the microenvironment in vivo for regenerating cartilage is ideal. In this study, we combined silk fibroin and decellularized cartilage extracellular matrix by temperature gradient-guided thermal-induced phase separation to produce composite scaffolds (S/D). Resulting scaffolds had remarkable mechanical properties and biomimeticstructure, for a suitable substrate for attachment and proliferation of adipose-derived stem cells (ADSCs). Moreover, transforming growth factor β3 (TGF-β3) loaded on scaffolds showed a controlled release profile and enhanced the chondrogenic differentiation of ADSCs during the 28-day culture. The S/D scaffold itself can provide a sustained release system without the introduction of other controlled release media, which has potential for commercial and clinical applications. The results of toluidine blue, Safranin O, and immunohistochemical staining and analysis of collagen II expression showed maintenance of a chondrogenic phenotype in all scaffolds after 28-day culture. The most obvious phenomenon was with the addition of TGF-β3. S/D composite scaffolds with sequential delivery of TGF-β3 may mimic the regenerative microenvironment to enhance the chondrogenic differentiation of ADSCs in vitro.
Keywords: cartilage tissue engineering, composite scaffold, silk fibroin, decellularized cartilage extracellular matrix, adipose-derived stem cells, transforming growth factor β3 (TGF-β3)
Introduction
Articular cartilage tissue, which can be injured by trauma, infection, osteoarthritis and other diseases, provides near-frictionless motion between articulating surfaces and supplies support and protection for bones of synovial joints.1,2 Because of poor regenerative capacity of cartilage, the repair of defective cartilage remains a great challenge in clinical therapy. Tissue engineering represents a promising approach for repair of articular cartilage defects, because it could constitute complete recovery for the patient and meet the clinical need. Previous studies of cartilage tissue engineering have focused on scaffolds, seed cells, growth factors and other facets.3–5 However, the current regenerated cartilage in vitro is unsatisfactory for fabrication of ideal three dimensional (3-D) microenvironment because of non-homogeneous cartilage architecture, poor mechanical property and unfeasible controlled release system for growth factors.6
To overcome the problems of non-homogeneous architecture and poor mechanical properties of scaffolds, recent studies have found that oriented scaffolds, which can mimic the native cartilage structure, could better regulate the distribution, alignment, and migration of mesenchymal stem cells (MSCs) or chondrocytes compared with a non-oriented scaffold.5 However, the optimal scaffold matrix derived from both natural and synthetic materials is required for cartilage tissue engineering.3
Decellularized cartilage extracellular matrix (DC-ECM) prepared by removing chondrocytes from native cartilage tissue could preserve most of the main ECM constituents of native cartilage, including glycosaminoglycan (GAG) and collagen type II. The scaffolds derived from DC-ECM possess excellent biocompatibility and provide a natural microenvironment for supporting MSC attachment, proliferation and differentiation into chondrocytes.7 However, DC-ECM scaffolds cannot satisfy the clinical application because of poor biomechanical properties. To overcome this problem, bioactive composite scaffolds developed for cartilage regeneration have been considered an effective strategy.8,9 Silk fibroin (SF), a natural fibrous protein, has been used as a potential biomaterial for a number of biomedical and biotechnological applications because of its excellent biological compatibility, mechanical strength, and biodegradation.10,11 Therefore, a hybrid composite scaffold of SF and DC-ECM (S/D) might meet the needs of clinical application.
Adipose-derived stem cells (ADSCs), which can be harvested from autologous fat tissue with minimal injury, can be induced to differentiate into chondrocytes and osteoblasts under appropriate conditions.12,13 Thus, ADSCs as seeded cells are widely used for cartilage tissue engineering.14–16
Chondrocyte-related growth factors such as transforming growth factor β,17 bone morphogenetic proteins,18 and insulin-like growth factor19 play a critical role in developing an appropriate microenvironment in cartilage tissue engineering.20 However, the uncontrolled delivery of these factors may decrease their full reparative potential and have unwanted morphological effects.21,22 To regulate the release of factors, loading microparticle containing factors into the scaffolds23 and covalently binding the factors to the scaffolds have been used in recent research of chondrogenesis.24,25 However, the effect of microspheres themselves on cell differentiation and covalent binding on the activity of factors cannot be well controlled, so both methods do not mimic the natural presentation of the factors in vitro.26 In addition, the preparation of these controlled release systems is relatively complicated. Thus, there is an urgent need to develop simple and stable methods for the spatial and temporal control release of factors in 3-D scaffolds.
The aim of this study was to fabricate biomimetic S/D scaffolds with a controlled release system to mimic an ideal 3-D microenvironment of chondrogenesis in vitro. We first fabricated composite scaffolds with SF and DC-ECM, then evaluated the chondrogenic proliferation and differentiation of rabbit ADSCs on the scaffolds by the cell morphology, attachment, proliferation, and chondrogenic gene expression. The ECM production was analyzed by qualitative histology and immunohistochemistry and quantitative biochemical analysis. Finally, we utilized the release kinetics of factors to determine whether the S/D scaffold itself could be used as a delivery system to control the release of transforming growth factor-β3 (TGF-β3).
Materials and methods
Materials and reagents
Porcine articular cartilage ECM was obtained from Fresh porcine articular cartilage by decellularization with previously described methods.4 Bombyx mori silkworm silk was purchased from Yun Tun Silk Textile Co. (Tong Xiang, People’s Republic of China). SF solution was prepared as described.27 Other materials, including biochemical and chemical reagents, are listed in supporting information.
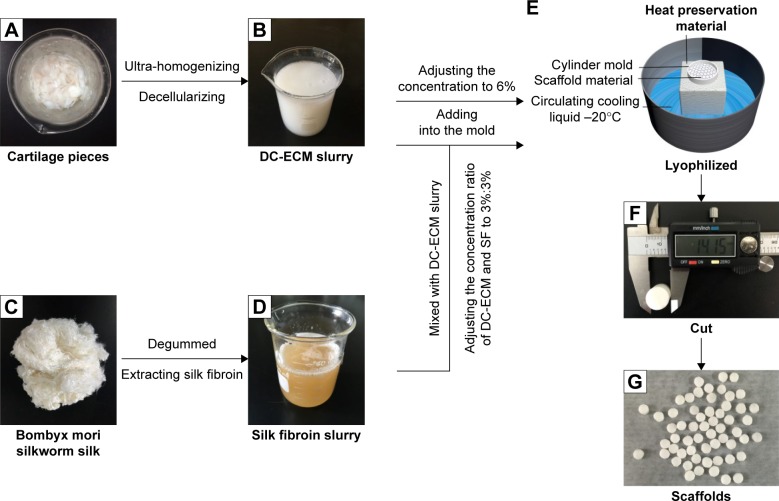
Preparation of scaffolds
DC-ECM scaffolds were prepared by using temperature gradient-guided thermal-induced phase separation (TIPS) followed by freeze-drying (Figure 1).3 Briefly, a plastic syringe with a flat bottom was surrounded by thermal insulation polystyrene material except for the top and bottom, and a mixed slurry with different composite of S/D at 3 wt% was loaded to form a mold-slurry device, which was placed onto the top of a cold liquid bath at −20°C to from a temperature gradient from the bottom to the top of the slurry. During the cold process, ice crystals in the slurry were formed and grew longitudinally from the bottom to the top. After 12 h, the frozen mold-slurry device was then quickly transferred into a lyophilizer and lyophilized for 24 h to obtain an oriented S/D composite scaffold. All scaffolds were cross-linked in an ethanol solution containing 50 mM 1-ethyl-3-3-dimethyl aminopropyl carbodiimide and 20 mM N-hydroxysuccinimide at 37°C for 24 h, then washed repeatedly with dH2O. To develop the TGF-β3 delivery system, TGF-β3 was coated onto scaffolds saturated with a buffer solution containing TGF-β3 (Peprotech, Rocky Hill, NJ, USA; 400 ng/mL) at 4°C for 24 h. The TGF-β3-loaded scaffolds were then lyophilized. All processes were carried out under sterile conditions.
Figure 1.
Schematic diagrams of the process of preparing the scaffolds.
Notes: (A) Cartilage pieces. (B) DC-ECM slurry. (C) Bombyx mori silkworm silk. (D) Silk fibroin. (E) Equipment for oriented structure. (F) Vernier caliper. (G) Lyophilized scaffolds.
Abbreviations: DC-ECM, decellularized cartilage extracellular matrix; SF, silk fibroin.
Isolation and culture of ADSCs
ADSCs were isolated from 4-month-old New Zealand rabbits as described.27 All experimental protocols were approved by the Animal Experimental Ethics Committee of Tianjin Hospital. All animals were handled in accordance with the animal care guidelines of Animal Experimental Ethics Committee of Tianjin Hospital. Briefly, adipose tissue derived from subcutaneous tissue of the necks of the rabbits was harvested and thoroughly washed 3 times with PBS solution containing 10% penicillin/streptomycin (both Gibco, Grand Island, NY, USA). Then visible blood vessels and connective tissue were removed. The cleaned adipose tissue was digested with 0.1% type I collagenase (Gibco) at 37°C for 1 h. To counteract the type I collagenase activity, 5 mL DMEM containing 10% fetal bovine serum (FBS) was added. The obtained tissue homogenate was centrifuged at 300 g, the supernate was removed along with the mature adipocytes, and the ADSCs were left as residue. The resulting ADSC pellet was resuspended in DMEM containing 20% FBS and 1% penicillin/streptomycin, then cultured in flasks in a 5% CO2 humidified incubator at 37°C. Non-adherent cells were removed by changing the medium, and adherent cells were expanded to passage 3.
Characterization of scaffolds
The morphology of scaffolds was characterized by scanning electron microscopy (SEM). Briefly, the scaffold specimens were cut into cross and longitudinal sections by using a scalpel blade. All sections were examined by SEM (Quanta 200, FEI; Hillsboro, OR, USA) after being coated with gold–palladium. Average pore size was determined by measuring >50 random pores with sizes >20 μm, selected from the SEM images by use of ImageJ (U.S. National Institutes of Health, Bethesda, MD, USA).
Cytotoxicity assay
The cytotoxicity of the scaffold resulting from the residual reagents and/or processing was determined by assessing cell proliferation with a cell counting kit-8 (CCK-8; Dojindo, Rockville, MD, USA). The leaching fluids of the scaffolds were obtained as described.27 ADSCs (3×103 in 200 μL suspension) were seeded into 96-well plates and incubated in leaching fluids for 1, 3, 5, and 7 days. As a control group, ADSCs of the same density were incubated in DMEM (Gibco) containing 10% FBS (Gibco) for 1, 3, 5, and 7 days. After incubation, cell samples (n=5) were obtained, rinsed in Hanks salt solution (Gibco), then incubated with 100 μL fresh DMEM containing 10% CCK-8 solution and 10% FBS at 37°C in a 5% CO2 humidified incubator at 37°C for 2 h. OD at 450 nm was measured by using a microplate reader (iMark, Bio-Rad, Tokyo, Japan).
Adhesion and viability of ADSCs within the scaffolds
To evaluate the adhesion of ADSCs on the DC-ECM and S/D scaffolds, scaffolds were first transferred to 12-well plates, then 50 μL of a suspension containing 5×105 ADSCs was seeded into each scaffold, and plates were incubated in a 5% CO2 humidified incubator at 37°C for 2 h, then 3 mL of medium was added to each well and plates were transferred back to the incubator for 7 days of culture. Medium was changed every 3 days. After 7 days of culturing, scaffolds with cells were fixed with 2.5% glutaraldehyde at 4°C for 12 h, then dehydrated through a graded ethanol series. The dried scaffolds were cut into cross sections of 1-mm thick and coated with gold. The adhesion of ADSCs on the scaffolds was observed by SEM.
The viability of the ADSCs within the scaffolds was assessed by use of a live/dead cell viability assay kit (Abcam, Cambridge, UK) as per the manufacturer’s instruction after 7 days of culture. After incubation with the live/dead staining solution for 30 min, live cells (green) and dead cells (red) were observed by confocal microscopy (Leica < Heidelberg, Germany).
Preparation of cell-scaffold constructs
Each scaffold was seeded with 5×105 ADSCs. As a control, cell-scaffolds not loaded with TGF-β3 were maintained in chemically defined chondrogenic medium (CDM) without TGF-β3 for 28 days. For the experimental group, non-TGF-β3-loaded constructs were maintained in CDM and TGF-β3-loaded constructs were maintained in CDM without TGF-β3 for 28 days. CDM consisted of DMEM supplemented with 10% FBS, penicillin (100 U/mL)/streptomycin (100 μg/mL), 100 μg/mL sodium pyruvate, 300 μg/mL L-glutamine, 40 μg/mL L-proline, 50 μg/mL L-ascorbic acid-2-phosphate, 1.5 mg/mL bovine serum albumin (BSA; Roche, San Francisco, CA, USA), 1× insulin-transferrin-selenium, 100 nM dexamethasone (all from Sigma, St Louis, MO, USA) and 10 ng/mL TGF-β3.
Biochemical analysis
Sulfated GAG and collagen are 2 key components of native cartilage.28,29 The constructs were biochemically analyzed for total GAG and collagen content on days 1, 14 and 28. Four samples (n=4) were analyzed for each time.
The content of GAG was estimated by using the dimethyl-methylene blue dye-binding assay kit (Biocolor, Carrickfergus, UK). Collagen content was determined by measuring hydroxyproline content after basic hydrolysis of the samples at 90°C for 20 min. Samples were assayed by using a chloramine-T assay assuming a hydroxyproline/collagen ratio of 1:7.69.
Histology and immunohistochemistry
After 14 and 28 days of culture, constructs were fixed in 4% paraformaldehyde (Solarbio, Beijing, People’s Republic of China) solution at 4°C for 12 h, washed in PBS, dehydrated through a graded ethanol series and wax-embedded, then sectioned in 10 μm thick slices and mounted on slides. Sections were deparaffinized, rehydrated and stained with hematoxylin and eosin (H&E; Sigma) to observe cells within the scaffolds,30 then stained with toluidine blue and safranin O to evaluate GAG. Collagen type II content was detected by immunohistochemistry. Deparaffinized and rehydrated sections were incubated for 10 min with a 3% peroxidase solution, blocked with 5% BSA (Roche) solution for 5 min, incubated with the mouse monoclonal anti-collagen II antibody (1:100; Abcam) at 4°C overnight, then washed and incubated with biotinylated secondary antibody for 20 min. The treated sections were incubated with streptavidin-biotin complex for 20 min at 37°C, followed by color development with diaminobenzidine tetrahydrochloride (Dako, Glostrup, Denmark), then observed by inverted light microscopy (Leica). Blank scaffolds were also analyzed as described previously.
TGF-β3 release from scaffolds
To evaluate the TGF-β3 release potency of the TGF-β3-loaded scaffolds, a TGF-β3 enzyme-linked immunosorbent assay (ELISA) assay kit (R&D Systems, Minneapolis, MN, USA) was used according to the manufacturer’s instructions. Briefly, 4 scaffold samples were placed in a 12-well plate supplemented with 3 mL sterile PBS per well and incubated in a 37°C, 5% CO2 incubator for 28 days. The PBS samples were collected for ELISA and exchanged with fresh PBS every day. Plates with 96 wells were coated with 360 μg/mL capture antibody (mouse anti-human TGF-β3) before assay. PBS samples and TGF-β3 standards were added and incubated for 2 h. After washing and drying, detection antibody (18 μg/mL of biotinylated goat anti-human TGF-β3) was added and incubated for 2 h. Plates were washed, dried, and incubated in horseradish peroxidase-conjugated streptavidin for 20 min in the dark. Substrate solution (1:1 mixture of H2O2 and tetramethylbenzidine) was added to each well for 20 min, avoiding direct light. Stop solution (2 N H2SO4) was added and the optical density was determined immediately with a microplate reader set to 450 nM.
Real-time reverse transcription polymerase chain reaction (RT-PCR) assay of chondrogenic-related gene expression
The expression of chondrogenic-related genes (superoxide dismutase 9 [SRY-Box 9], collagen type II, and aggrecan) was analyzed by RT-PCR. After 14, 21 and 28 days of culture, 4 cell-scaffold constructs at each time point were ground to a powder with use of a mortar filled with liquid nitrogen and a pestle, and the resulting powders were immersed in TRIzol reagent (Invitrogen, Camarillo, CA, USA). RNA was extracted by following the manufacturer’s protocol. The total RNA concentration was quantified by use of a NanoDrop1000 (Thermo Scientific, Chelmsford, MA, USA). Subsequently, 2 μg total RNA was reverse-transcribed by use of a First cDNA synthesis kit (Fermentas Life Sciences, York, UK). RT-PCR involved use of the SYBR green system (Fermentas Life Sciences) at 95°C for 10 min, followed by 40 cycles at 94°C for 30 s, 56°C for 60 s, and 72°C for 40 s. Expression was calculated by the 2−ΔΔCt method and normalized to that of glyceraldehyde- 3-phosphate dehydrogenase. Primer sequences are in Table 1. As controls, ADSCs were seeded into DC-ECM and S/D scaffolds, cultured in non-chondrogenic-induced medium for 1 day, for analysis of genes expression.
Table 1.
Reverse transcription polymerase chain reaction primer sequences
| Gene | Primer sequences
|
|
|---|---|---|
| Forward | Reverse | |
| GAPDH | GACTGATGTTGTTGACAGCCACTGC | TAGCCACTCCTTCTGTGACTCTAAC |
| Collagen II | CACCACGCTCTTCTGTCTACTGAAC | TGCCACAAGCAGGAATGAG |
| Aggrecan | CTGCCTCAGGGATCCGTAAAG | CCTCTGCCTCAGGAATGACAT |
| SOX-9 | CCTTGAGTCCTTGCGCGGCA | TTGGCCCTCCTCCTCCAGCC |
Abbreviation: GAPDH, glyceraldehyde 3-phosphate dehydrogenase.
Compression testing
Compressive elastic moduli of the blank scaffolds (n=4) and constructs (after 14 and 28 days of culture; n=4) were measured by using a micromaterial mechanical testing system (MTF-100, Tianjin, People’s Republic of China). Blank scaffolds were immersed in PBS for 12 h before testing. Blank scaffolds and constructs were fixed on the clamp of the testing system. A constant compression speed of 0.5 mm/min was used. Stress−strain curves were recorded by use of the computer software. Compressive elastic moduli were calculated from the slopes of the stress−strain curves.
Statistical analysis
SPSS v19.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Data are presented as mean ± SD and were compared by one-way analysis of variance and Newman–Keuls comparison test. P<0.05 was considered statistically significant.
Results
Characterization of the scaffolds
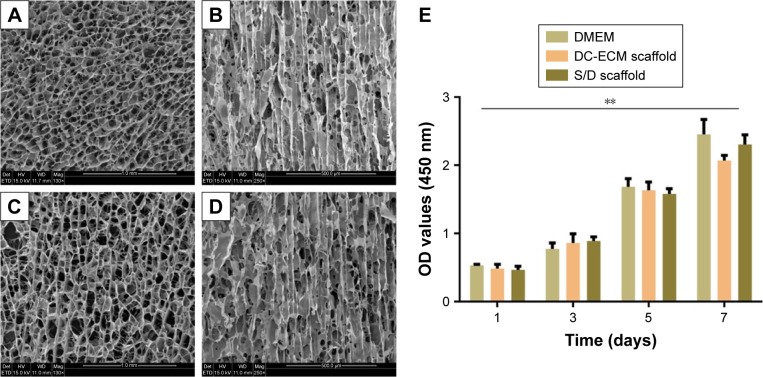
Cross sections of DC-ECM and S/D scaffolds were uniform microporous, and longitudinal sections showed oriented microtubular-like structures from the TIPS technique (Figure 2A–D). The mean pore diameter of DC-ECM and S/D scaffolds ranged from 100 to 200 μm and porosity from 100 to 300 μm. Cytotoxicity assay with a CCK-8 kit revealed no significant difference in absorbance between the leaching fluids of the scaffolds and DMEM (Figure 2E), which suggested no cytotoxic effect of the scaffolds on ADSCs.
Figure 2.
Representative SEM images of (A) cross sections and (B) longitudinal sections of S/D scaffold. SEM image of (C) cross sections and (D) longitudinal sections of DC-ECM scaffold. (E) Cytotoxicity assay of the scaffolds by CCK-8 kit to assess cell proliferation.
Notes: Data are mean ± SD, n=4. **P<0.01.
Abbreviations: DC-ECM, decellularized cartilage extracellular matrix; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; SEM, scanning electron microscope.
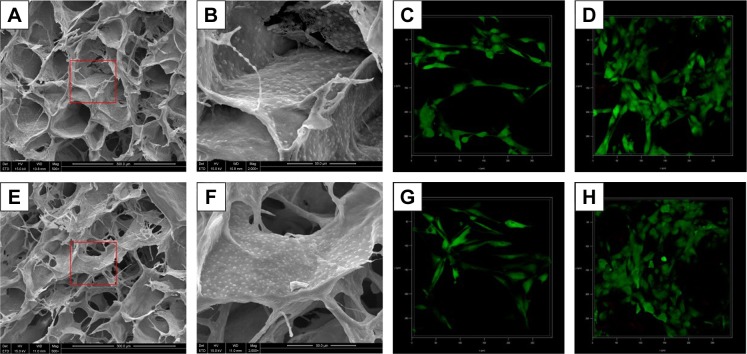
Adhesion and viability of ADSCs within the scaffolds
ADSCs could adhere and spread well on the walls of pores in both scaffolds (Figure 3A, B, E and F). Moreover, the adhered ADSCs could secrete ECM, which indicated that both scaffolds had good cytocompatibility with ADSCs and could support the attachment and growth of ADSCs. Live/dead staining after 3 and 7 days of culture revealed that ADSCs proliferated remarkably over time (Figure 3C, D, G and H). Most cells within both scaffolds were marked with green fluorescence (live cells), with almost no red fluorescence (dead cells). Therefore, ADSCs could survive within both scaffolds.
Figure 3.
Representative images of adhesion (A, B, E, F) and viability (C, D, G, H) of ADSCs within scaffolds.
Notes: SEM images of (A, B [enlarged inset of A]) S/D scaffolds and (E, F [enlarged inset of E]) of DC-ECM scaffolds seeded with ADSCs after 48 h of culture. Confocal microscopy images of live/dead staining of (C, D) S/D scaffolds and (G, H) DC-ECM scaffolds seeded with ADSCs after 3 and 7 days of culture, respectively.
Abbreviations: ADSCs, adipose-derived stem cells; DC-ECM, decellularized cartilage extracellular matrix; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3.
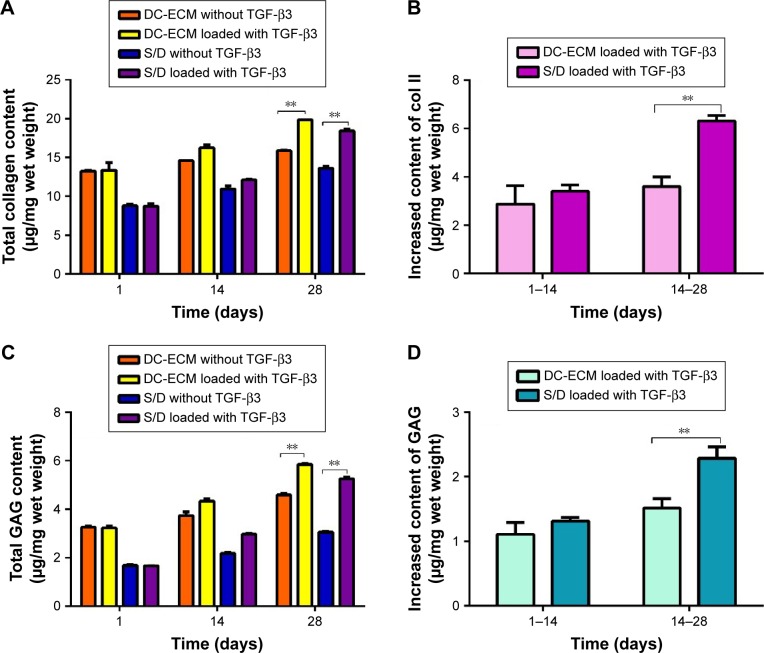
Biochemical analysis
Total collagen and GAG content of cell-scaffold constructs increased gradually with culture time, with much higher growth rates with than without TGF-β3 loading (Figure 4A and C). Exogenously supplying TGF-β3 could promote superior chondrogenesis. Furthermore, the increased total collagen and GAG content was higher in TGF-β3-loaded S/D than DC-ECM scaffolds after 28 days of culture (Figure 4B and D).
Figure 4.
Quantitative analysis of collagen and GAG content in cell-scaffold constructs.
Notes: Content of (A) total collagen and (B) collagen with TGF-β3 loading after 14 and 28 days of culture. Content of (C) total GAG and (D) GAG with TGF-β3 loading after 14 and 28-day culture. Data are mean ± SD, n=4. **P<0.01.
Abbreviations: GAG, glycosaminoglycan; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3.
Histology and immunohistochemistry
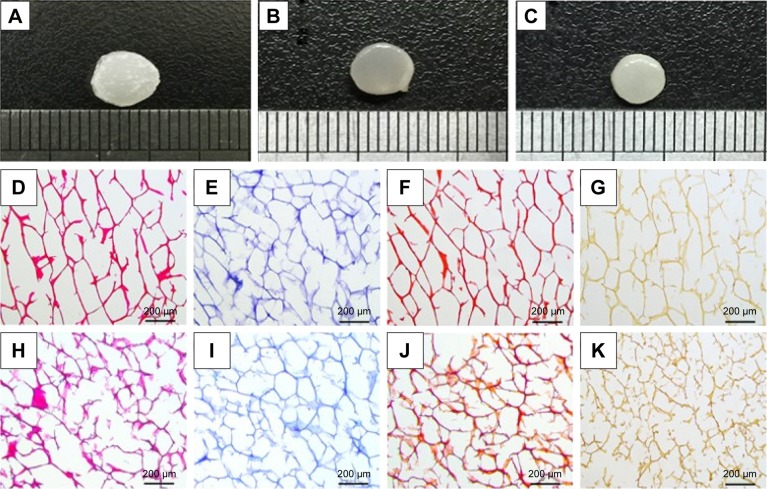
DC-ECM and S/D scaffolds loaded with TGF-β3 appeared similar to natural cartilage tissue after 28 days of culture (Figure 5A–C). However, scaffolds without TGF-β3 could not form natural cartilage-like constructs.
Figure 5.
Representative images of gross appearance of scaffolds after 28-day culture.
Notes: Histology and immunohistochemistry of blank scaffolds. (A) Scaffold without TGF-β3. (B) DC-ECM scaffold loaded with TGF-β3. (C) S/D scaffold loaded with TGF-β3. Histology and immunohistochemistry of (D–G) DC-ECM scaffold and (H–K) S/D scaffold. (D, H) H&E staining. (E, I) Toluidine blue staining. (F, J) Safranin O staining. (G, K) Immunohistology staining for collagen type II.
Abbreviations: DC-ECM, decellularized cartilage extracellular matrix; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3; H&E, hematoxylin-eosin.
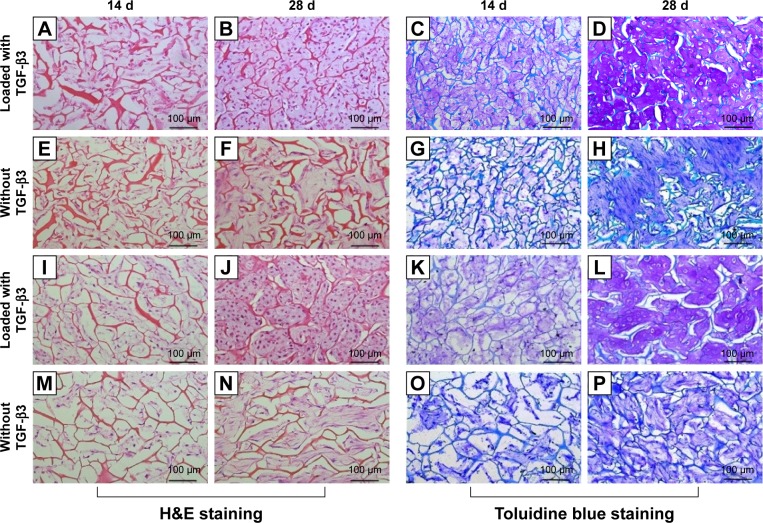
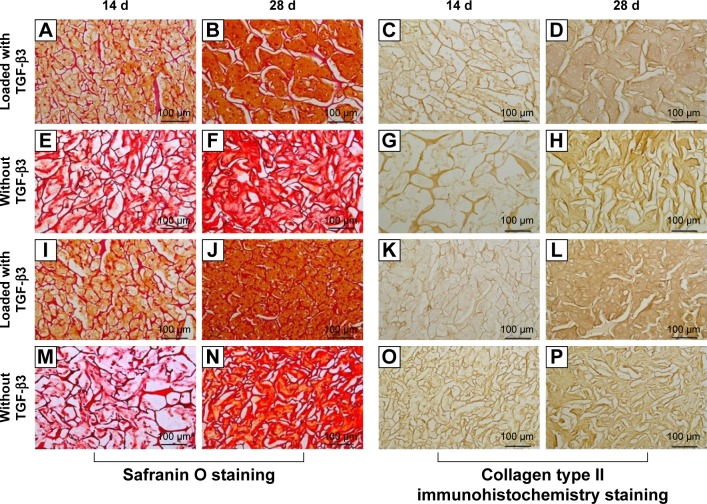
For blank scaffolds, H&E staining revealed no intact cell or nucleus within DC-ECM or S/D scaffolds (Figure 5D and H). Staining was positive for toluidine blue (Figure 5E and I), safranin O (Figure 5F and J), and immunohistology staining (Figure 5G and K) for both scaffolds, which revealed the presence of collagen type II and GAG components in both scaffolds. For cell-scaffold constructs, H&E staining revealed that ADSCs and its secretions adhere to scaffolds and uniformly distribute throughout the pores (Figure 6). In all groups, the density of cells and quantity of ECM increased with culture time, but more round chondrocyte-like cells and characteristic cartilage lacunas were observed and more ECM was secreted with TGF-β3 loading after 28 days of culture. Accordingly, toluidine blue staining (Figure 6), safranin O staining and immunochemistry staining (Figure 7) showed increased GAG and collagen type II content in the ECM with culture time, with greater staining with TGF-β3 loading after 28 days of culture. Thus, TGF-β3 could promote GAG and collagen type II secretion of the cells, with no difference between S/D and DC-ECM scaffolds.
Figure 6.
Representative images of H&E and Toluidine blue staining of cell-scaffold constructs after 14 and 28 days of culture.
Note: Tissue with or without TGF-β3 loading on (A–H) DC-ECM scaffolds and (I–P) S/D scaffolds.
Abbreviations: DC-ECM, decellularized cartilage extracellular matrix; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3; H&E, hematoxylin-eosin.
Figure 7.
Representative images of safranin O staining and collagen type II immunohistochemistry staining of cell-scaffold constructs after 14 and 28 days of culture.
Note: With or without TGF-β3 in (A–H) DC-ECM scaffolds and (I–P) S/D scaffolds.
Abbreviations: DC-ECM, decellularized cartilage extracellular matrix; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3.
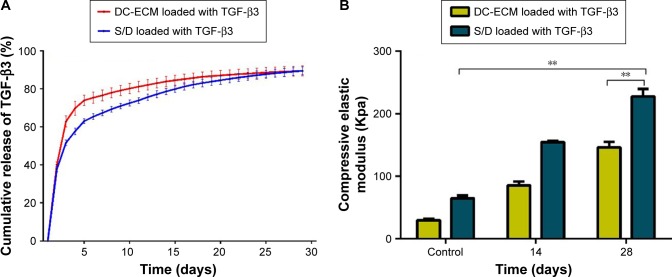
TGF-β3 release from the scaffolds
TGF-β3 was released abundantly from both DC-ECM and S/D scaffolds during the first 7 days (Figure 8A). Compared with the curve for DC-ECM scaffolds, that for S/D scaffolds was also stable and sustainable. Additionally, the release for both scaffolds increased up to 89% of the total amount after 28 days of culture.
Figure 8.
Release kinetics of TGF-β3 and compressive elastic modulus of scaffolds.
Notes: (A) Cumulative release values are presented as a percentage of the initial amount of TGF-β3 loaded onto scaffolds. (B) Compressive elastic modulus of DC-ECM and S/D scaffold loaded with TGF-β3 after 14 and 28 days of culture. Data are mean ± SD, n=4. **P<0.01.
Abbreviations: DC-ECM, decellularized cartilage extracellular matrix; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3.
Compressive elastic modulus
The compressive elastic modulus of S/D scaffold loaded with TGF-β3 significantly increased from 64.99±43.83 kPa for the control scaffold to 227.74±11.58 kPa after 28 days of culture (Figure 8B). The compressive elastic modulus of the DC-ECM scaffold loaded with TGF-β3 significantly increased from 29.8034±2.10 kPa for the control scaffold to 146.08±8.92 kPa after 28 days of culture (Figure 8B).
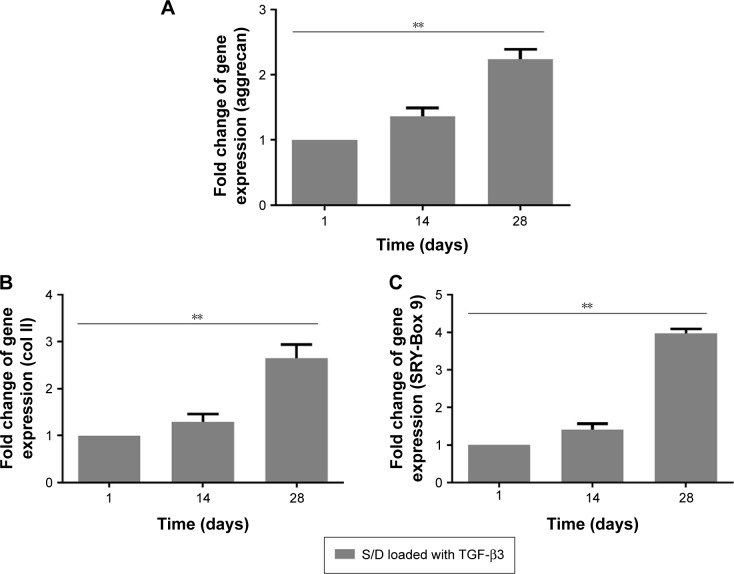
Expression of chondrogenic-related genes
The expression of chondrogenic-related genes (SRY-Box 9, collagen type II and aggrecan) significantly increased with increasing ADSC culture time of S/D scaffolds (Figure 9A–C). Compared with non-induced ADSCs, which were cultured for 1 day in non-chondrogenic-induced culture medium, with culture time, SRY-Box 9, collagen type II and aggrecan were all up-regulated at day 14 and the expression was significantly increased at day 28, which suggested that the chondrogenic-induced ADSCs could differentiate toward chondrocytes.
Figure 9.
(A–C) Expression profiles of chondrogenic-related genes: (A) aggrecan, (B) collagen type II, and (C) SRY-Box 9 with TGF-β3 loading after 14 and 28 days’ culture.
Notes: Data are mean ± SD, n=3. **P<0.01.
Abbreviations: SRY, sex-determining region Y; S/D, hybrid composite scaffold of silk fibroin and DC-ECM; TGF-β3, transforming growth factor β3.
Discussion
The microenvironment of chondrogenesis is a complex system composed of various components and plays an especially important role in cartilage tissue engineering.22,31,32 Although it contains many ingredients, proper seed cells, compatible 3-D scaffold and specific bioactive factors are the 3 most important components in the system.6,13,32,33 To mimic an ideal microenvironment in vitro, a comprehensive system, including these 3 sections is needed. In this study, we combined SF and DC-ECM by TIPS to produce composite scaffolds (S/D) that had remarkable mechanical properties and biomimetic structure, for a suitable substrate for attachment and proliferation of ADSCs. Moreover, TGF-β3 loaded on scaffolds showed a controlled release profile and enhanced the chondrogenic differentiation of ADSCs during the 28-day culture. Toluidine blue, safranin O, and histochemical staining and analysis of collagen II expression showed maintenance of a chondrogenic phenotype in all scaffolds after the 28-day culture. The most obvious phenomenon occurred with the addition of TGF-β3. S/D composite scaffolds with sequential delivery of TGF-β3 may mimic the regenerative microenvironment to enhance the chondrogenic differentiation of ADSCs in vitro.
Increasing studies have attached importance to developing 3-D porous scaffolds because they favor cell attachment, differentiation and proliferation in cartilage regeneration.30,34,35 However, these porous constructions of scaffolds cannot match the biological characteristics of cartilage. DC-ECM and other oriented scaffolds can facilitate the migration and expression of cells and strengthen the biomechanical properties of materials.5,36 We showed that the structure of scaffolds served as a guide for chondrogenic-induced ADSC adherence and alignment along the orientation of vertical microtubules, thus mimicking the physiological structure of native cartilage (Figure 3). The 3-D oriented architecture provides a 3-D natural support for cell induction and differentiation, as a basis to fabricate the ideal microenvironment of cartilage regeneration in vitro.
Many studies focused on the biochemical ingredients of scaffold to enhance their properties in cartilage repair and regeneration. To mimic natural cartilage components and clinical biological characteristics, DC-ECM combined with other materials has been investigated in vitro and in vivo.37–39 ECM and SF matrices provide suitable substrates for cell attachment and proliferation, and SF is a promising biomaterial for biological characteristics of cartilage because of its remarkable mechanical properties and ability to tailor its degradation.40 When we added stem cells and cytokines to scaffolds with a bionic cartilage structure, the S/D scaffold was more ideal than the DC-ECM scaffold in cartilage tissue engineering. Along with the accumulation of collagen type II and GAG content, the compressive elastic moduli of S/D scaffolds increased significantly in vitro. The differentiation and proliferation of ADSCs strengthened the compressive elastic moduli of scaffolds (Figure 8B). Our results agree with previous studies showing that accumulated GAG and collagen content can improve the biomechanical property of scaffolds3,41 and ADSCs seeded onto scaffolds can easily be differentiated into chondrocytes and induced to form new cartilage tissue with the addition of TGF-β3 (Figure 5).21,42 After 28 days of culture, the compressive module was higher for the S/D than DC-ECM scaffold. These properties were similar to native cartilage and could be applied in clinical treatment in vivo. Especially, suitable mechanical stimulation is critical for the biochemical and biomechanical development of chondrogenesis in vitro and in vivo43,44 that needs to be further studied. Because the DC-ECM scaffold preserves most of the structural and functional proteins of the ECM of cartilage, the presence of these constituents can affect the secretion of GAG and collagen.4 Many studies have shown that a DC-ECM scaffold can support chondrogenesis of stem cells under suitable conditions.3,4,45 In our study, although the GAG and collagen content of DC-ECM scaffolds had distinct advantages over those of S/D scaffolds in the initial stage of cultivation, both scaffolds finally had almost the same GAG and collagen content after 28 days of culture (Figure 4). The S/D scaffold could enhance the mechanical properties of the scaffold, which overcame the shortcomings of DC-ECM scaffolds, and also supported the chondrogenesis of ADSCs (Figures 6–9).
Finally, the prolonged exposure of MSCs to the inducer TGF-β is critical because this factor induces the various phases leading to chondrogenesis, from initiating the pre-cartilage condensation phase to the final differentiation process and DC-ECM production and deposition.46,47 However, because of the quite short half-life period of delivery, direct injection of TGF-β does not have clinical application. Previous studies certified that certain matrix components such as collagen and proteoglycans from ECM can act as growth factor reservoirs, to deliver TGF-β3 from such scaffolds in a controlled manner.48,49 Thus, via freeze-drying, the DC-ECM scaffold can build a natural affinity with TGF-β3 to produce an appropriate controlled system.21 However, mixing DC-ECM with other substances has not been reported as a sustained release system in cartilage tissue engineering. In our research, the release kinetics of TGF-β3 revealed stable and sustainable release of factors on both scaffolds (Figure 8A). Like the DC-ECM scaffold,21 the S/D scaffold can support the controlled release of TGF-β3 to improve chondrogenesis of stem cells. The addition of SF into the scaffold materials did not interfere with the controlled release system. Additionally, with the above characteristics of the S/D scaffold, it might be considered an “off-the-shelf ” construct, with TGF-β naturally adhering to S/D scaffolds, and stem cells and other cells from a stem cell bank seeded onto the scaffold or chemotactically recruited into the TGF-β-loaded construct50,51 before implantation for clinical surgery for articular cartilage repair and regeneration. Therefore, these results could be favorable for construction and development of an ideal microenvironment of chondrogenesis in vitro.
Conclusion
We successfully prepared oriented scaffolds by blending SF and DC-ECM. The blended S/D scaffolds supported the attachment, proliferation and differentiation of ADSCs with enhanced biomechanical characteristics of scaffolds after 4 weeks in a TGF-β3-based controlled release system. SF-DC-ECM blended scaffolds may be a suitable construct combining growth factors and seed cells to simulate the microenvironment of chondrogenesis in vitro.
Acknowledgments
This study was funded by the National Science Foundation of China (31470937, 31300798, 81572154), and the Research Foundation of the Tianjin Health Bureau (16KG114, 15KG125).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hunziker EB. Articular cartilage repair: are the intrinsic biological constraints undermining this process insuperable? Osteoarthritis Cartilage. 1999;7(1):15–28. doi: 10.1053/joca.1998.0159. [DOI] [PubMed] [Google Scholar]
- 2.Simon TM, Jackson DW. Articular cartilage: injury pathways and treatment options. Sports Med Arthrosc. 2006;14(3):146–154. doi: 10.1097/00132585-200609000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Jia S, Liu L, Pan W, et al. Oriented cartilage extracellular matrix-derived scaffold for cartilage tissue engineering. J Biosci Bioeng. 2012;113(5):647–653. doi: 10.1016/j.jbiosc.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 4.Yang Q, Peng J, Guo Q, et al. A cartilage ECM-derived 3-D porous acellular matrix scaffold for in vivo cartilage tissue engineering with PKH26-labeled chondrogenic bone marrow-derived mesenchymal stem cells. Biomaterials. 2008;29(15):2378–2387. doi: 10.1016/j.biomaterials.2008.01.037. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Y, Yang F, Liu K, et al. The impact of PLGA scaffold orientation on in vitro cartilage regeneration. Biomaterials. 2012;33(10):2926–2935. doi: 10.1016/j.biomaterials.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Temenoff JS, Mikos AG. Review: tissue engineering for regeneration of articular cartilage. Biomaterials. 2000;21(5):431–440. doi: 10.1016/s0142-9612(99)00213-6. [DOI] [PubMed] [Google Scholar]
- 7.Ravindran S, Kotecha M, Huang CC, et al. Biological and MRI characterization of biomimetic ECM scaffolds for cartilage tissue regeneration. Biomaterials. 2015;71:58–70. doi: 10.1016/j.biomaterials.2015.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karbasi S, Fekrat F, Semnani D, Razavi S, Zargar EN. Evaluation of structural and mechanical properties of electrospun nano-micro hybrid of poly hydroxybutyrate-chitosan/silk scaffold for cartilage tissue engineering. Adv Biomed Res. 2016;5:180. doi: 10.4103/2277-9175.194802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao J, Qu Y, Chu B, Zhang X, Qian Z. Biodegradable CSMA/PECA/Graphene Porous Hybrid Scaffold for Cartilage Tissue Engineering. Sci Rep. 2015;5:9879. doi: 10.1038/srep09879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hofmann S, Knecht S, Langer R, et al. Cartilage-like tissue engineering using silk scaffolds and mesenchymal stem cells. Tissue Eng. 2006;12(10):2729–2738. doi: 10.1089/ten.2006.12.2729. [DOI] [PubMed] [Google Scholar]
- 11.Rajkhowa R, Gil ES, Kluge J, et al. Reinforcing silk scaffolds with silk particles. Macromol Biosci. 2010;10(6):599–611. doi: 10.1002/mabi.200900358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Correa D, Lietman SA. Articular cartilage repair: Current needs, methods and research directions. Semin Cell Deve Biol. 2017;62:67–77. doi: 10.1016/j.semcdb.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Panadero JA, Lanceros-Mendez S, Ribelles JL. Differentiation of mesenchymal stem cells for cartilage tissue engineering: individual and synergetic effects of three-dimensional environment and mechanical loading. Acta Biomater. 2016;33:1–12. doi: 10.1016/j.actbio.2016.01.037. [DOI] [PubMed] [Google Scholar]
- 14.Correia C, Bhumiratana S, Yan LP, et al. Development of silk-based scaffolds for tissue engineering of bone from human adipose-derived stem cells. Acta Biomater. 2012;8(7):2483–2492. doi: 10.1016/j.actbio.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ude CC, Ng MH, Chen CH, et al. Improved functional assessment of osteoarthritic knee joint after chondrogenically induced cell treatment. Osteoarthritis Cartilage. 2015;23(8):1294–1306. doi: 10.1016/j.joca.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Zanetti AS, Sabliov C, Gimble JM, Hayes DJ. Human adipose-derived stem cells and three-dimensional scaffold constructs: a review of the biomaterials and models currently used for bone regeneration. J Biomed Mater Res B Appl Biomater. 2013;101(1):187–199. doi: 10.1002/jbm.b.32817. [DOI] [PubMed] [Google Scholar]
- 17.Fortier LA, Barker JU, Strauss EJ, McCarrel TM, Cole BJ. The role of growth factors in cartilage repair. Clin Orthop Relat Res. 2011;469(10):2706–2715. doi: 10.1007/s11999-011-1857-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puetzer JL, Petitte JN, Loboa EG. Comparative review of growth factors for induction of three-dimensional in vitro chondrogenesis in human mesenchymal stem cells isolated from bone marrow and adipose tissue. Tissue Eng Part B Rev. 2010;16(4):435–444. doi: 10.1089/ten.TEB.2009.0705. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt MB, Chen EH, Lynch SE. A review of the effects of insulin-like growth factor and platelet derived growth factor on in vivo cartilage healing and repair. Osteoarthritis Cartilage. 2006;14(5):403–412. doi: 10.1016/j.joca.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Cals FL, Hellingman CA, Koevoet W, Baatenburg de Jong RJ, van Osch GJ. Effects of transforming growth factor-beta subtypes on in vitro cartilage production and mineralization of human bone marrow stromal-derived mesenchymal stem cells. J Tissue Eng Regen Med. 2012;6(1):68–76. doi: 10.1002/term.399. [DOI] [PubMed] [Google Scholar]
- 21.Almeida HV, Liu Y, Cunniffe GM, et al. Controlled release of transforming growth factor-beta3 from cartilage-extra-cellular-matrix-derived scaffolds to promote chondrogenesis of human-joint-tissue-derived stem cells. Acta Biomater. 2014;10(10):4400–4409. doi: 10.1016/j.actbio.2014.05.030. [DOI] [PubMed] [Google Scholar]
- 22.Lam J, Lu S, Kasper FK, Mikos AG. Strategies for controlled delivery of biologics for cartilage repair. Adv Drug Deliv Rev. 2015;84:123–134. doi: 10.1016/j.addr.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bratt-Leal AM, Carpenedo RL, Ungrin MD, Zandstra PW, McDevitt TC. Incorporation of biomaterials in multicellular aggregates modulates pluripotent stem cell differentiation. Biomaterials. 2011;32(1):48–56. doi: 10.1016/j.biomaterials.2010.08.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merrett K, Griffith CM, Deslandes Y, Pleizier G, Dube MA, Sheardown H. Interactions of corneal cells with transforming growth factor beta 2-modified poly dimethyl siloxane surfaces. J Biomed Mater Res A. 2003;67(3):981–993. doi: 10.1002/jbm.a.10165. [DOI] [PubMed] [Google Scholar]
- 25.Ravindran S, Roam JL, Nguyen PK, Hering TM, Elbert DL, McAlinden A. Changes of chondrocyte expression profiles in human MSC aggregates in the presence of PEG microspheres and TGF-beta3. Biomaterials. 2011;32(33):8436–8445. doi: 10.1016/j.biomaterials.2011.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Re’em T, Kaminer-Israeli Y, Ruvinov E, Cohen S. Chondrogenesis of hMSC in affinity-bound TGF-beta scaffolds. Biomaterials. 2012;33(3):751–761. doi: 10.1016/j.biomaterials.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 27.Ding X, Zhu M, Xu B, et al. Integrated trilayered silk fibroin scaffold for osteochondral differentiation of adipose-derived stem cells. ACS Appl Mater Interfaces. 2014;6(19):16696–16705. doi: 10.1021/am5036708. [DOI] [PubMed] [Google Scholar]
- 28.Dai W, Kawazoe N, Lin X, Dong J, Chen G. The influence of structural design of PLGA/collagen hybrid scaffolds in cartilage tissue engineering. Biomaterials. 2010;31(8):2141–2152. doi: 10.1016/j.biomaterials.2009.11.070. [DOI] [PubMed] [Google Scholar]
- 29.Valonen PK, Moutos FT, Kusanagi A, et al. In vitro generation of mechanically functional cartilage grafts based on adult human stem cells and 3D-woven poly(epsilon-caprolactone) scaffolds. Biomaterials. 2010;31(8):2193–2200. doi: 10.1016/j.biomaterials.2009.11.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hwang Y, Sangaj N, Varghese S. Interconnected macroporous poly(ethylene glycol) cryogels as a cell scaffold for cartilage tissue engineering. Tissue Eng Part A. 2010;16(10):3033–3041. doi: 10.1089/ten.TEA.2010.0045. [DOI] [PubMed] [Google Scholar]
- 31.Goldberg A, Mitchell K, Soans J, Kim L, Zaidi R. The use of mesenchymal stem cells for cartilage repair and regeneration: a systematic review. J Orthop Surg Res. 2017;12(1):39. doi: 10.1186/s13018-017-0534-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liao J, Shi K, Ding Q, Qu Y, Luo F, Qian Z. Recent developments in scaffold-guided cartilage tissue regeneration. J Biomed Nanotechnol. 2014;10(10):3085–3104. doi: 10.1166/jbn.2014.1934. [DOI] [PubMed] [Google Scholar]
- 33.Makris EA, Gomoll AH, Malizos KN, Hu JC, Athanasiou KA. Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol. 2015;11(1):21–34. doi: 10.1038/nrrheum.2014.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang Y, Kim UJ, Blasioli DJ, Kim HJ, Kaplan DL. In vitro cartilage tissue engineering with 3D porous aqueous-derived silk scaffolds and mesenchymal stem cells. Biomaterials. 2005;26(34):7082–7094. doi: 10.1016/j.biomaterials.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 35.Wu X, Liu Y, Li X, et al. Preparation of aligned porous gelatin scaffolds by unidirectional freeze-drying method. Acta Biomater. 2010;6(3):1167–1177. doi: 10.1016/j.actbio.2009.08.041. [DOI] [PubMed] [Google Scholar]
- 36.Dai Y, Gao Z, Ma L, Wang D, Gao C. Cell-free HA-MA/PLGA scaffolds with radially oriented pores for in situ inductive regeneration of full thickness cartilage defects. Macromol Biosci. 2016;16(11):1632–1642. doi: 10.1002/mabi.201600218. [DOI] [PubMed] [Google Scholar]
- 37.Garrigues NW, Little D, Sanchez-Adams J, Ruch DS, Guilak F. Electrospun cartilage-derived matrix scaffolds for cartilage tissue engineering. J Biomed Mater Res A. 2014;102(11):3998–4008. doi: 10.1002/jbm.a.35068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moutos FT, Estes BT, Guilak F. Multifunctional hybrid three- dimensionally woven scaffolds for cartilage tissue engineering. Macromol Biosci. 2010;10(11):1355–1364. doi: 10.1002/mabi.201000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zheng X, Yang F, Wang S, et al. Fabrication and cell affinity of biomimetic structured PLGA/articular cartilage ECM composite scaffold. J Mater Sci Mater Med. 2011;22(3):693–704. doi: 10.1007/s10856-011-4248-0. [DOI] [PubMed] [Google Scholar]
- 40.Kasoju N, Bora U. Silk fibroin in tissue engineering. Adv Healthc Mater. 2012;1(4):393–412. doi: 10.1002/adhm.201200097. [DOI] [PubMed] [Google Scholar]
- 41.Kiyotake EA, Beck EC, Detamore MS. Cartilage extracellular matrix as a biomaterial for cartilage regeneration. Ann N Y Acad Sci. 2016;1383(1):139–159. doi: 10.1111/nyas.13278. [DOI] [PubMed] [Google Scholar]
- 42.Luo Z, Jiang L, Xu Y, et al. Mechano growth factor (MGF) and transforming growth factor (TGF)-β3 functionalized silk scaffolds enhance articular hyaline cartilage regeneration in rabbit model. Biomaterials. 2015;52:463–475. doi: 10.1016/j.biomaterials.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 43.Bueno EM, Bilgen B, Barabino GA. Hydrodynamic parameters modulate biochemical, histological, and mechanical properties of engineered cartilage. Tissue Eng Part A. 2009;15(4):773–785. doi: 10.1089/ten.tea.2008.0081. [DOI] [PubMed] [Google Scholar]
- 44.Guvendiren M, Burdick JA. Stiffening hydrogels to probe short- and long-term cellular responses to dynamic mechanics. Nat Commun. 2012;3:792. doi: 10.1038/ncomms1792. [DOI] [PubMed] [Google Scholar]
- 45.Cheng NC, Estes BT, Awad HA, Guilak F. Chondrogenic differentiation of adipose-derived adult stem cells by a porous scaffold derived from native articular cartilage extracellular matrix. Tissue Eng Part A. 2009;15(2):231–241. doi: 10.1089/ten.tea.2008.0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miura Y, Fitzsimmons JS, Commisso CN, Gallay SH, O’Driscoll SW. Enhancement of periosteal chondrogenesis in vitro. Dose-response for transforming growth factor-beta 1 (TGF-beta 1) Clin Orthop Relat Res. 1994;(301):271–280. [PubMed] [Google Scholar]
- 47.Tuli R, Tuli S, Nandi S, et al. Transforming growth factor-beta-mediated chondrogenesis of human mesenchymal progenitor cells involves N-cadherin and mitogen-activated protein kinase and Wnt signaling cross-talk. J Biol Chem. 2003;278(42):41227–41236. doi: 10.1074/jbc.M305312200. [DOI] [PubMed] [Google Scholar]
- 48.Holland TA, Mikos AG. Advances in drug delivery for articular cartilage. J Control Release. 2003;86(1):1–14. doi: 10.1016/s0168-3659(02)00373-5. [DOI] [PubMed] [Google Scholar]
- 49.Macri L, Silverstein D, Clark RA. Growth factor binding to the peri-cellular matrix and its importance in tissue engineering. Adv Drug Deliv Rev. 2007;59(13):1366–1381. doi: 10.1016/j.addr.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 50.Lee CH, Cook JL, Mendelson A, Moioli EK, Yao H, Mao JJ. Regeneration of the articular surface of the rabbit synovial joint by cell homing: a proof of concept study. Lancet. 2010;376(9739):440–448. doi: 10.1016/S0140-6736(10)60668-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mendelson A, Frank E, Allred C, et al. Chondrogenesis by chemotactic homing of synovium, bone marrow, and adipose stem cells in vitro. FASEB J. 2011;25(10):3496–3504. doi: 10.1096/fj.10-176305. [DOI] [PMC free article] [PubMed] [Google Scholar]