Abstract
Background
Little is known about expenditure items of multiple sclerosis (MS) patients over recent years in France.
Objective
To describe healthcare expenditure among MS patients and identify the main expenditure drivers.
Methods
All healthcare expenditure reimbursed by French National Health Insurance to MS patients in 2013 was described on the basis of nationwide health administrative databases (SNIIRAM/PMSI). Expenditure was described globally and according to age and sex.
Results
The average expenditure among the 90,288 MS patients included was €11,900 per patient. Pharmacy and hospitalisation accounted for 47% and 23% of healthcare expenditure, respectively (38% and 22% of MS patients were treated with disease-modifying therapies and hospitalised overnight or longer, respectively). Average expenditure did not differ according to age. However, pharmacy expenditure decreased with age (from 71% between the ages of 20 and 29 years to 18% between the ages of 70 and 79 years), whereas hospitalisation expenditure increased with age (from 15% to 35%). Paramedical fees accounted for 2% of expenditure between the ages of 20 and 29 years and 24% between the ages of 70 and 79 years.
Conclusion
Overall, pharmacy expenditure was the main expenditure item, which decreased with increasing age, while hospitalisation and paramedical expenditure increased with increasing age.
Keywords: Multiple sclerosis, healthcare expenditure, SNIIRAM, PMSI, health administrative database
Introduction
Multiple sclerosis (MS) is an inflammatory, demyelinating, neurodegenerative disorder of the central nervous system of unknown aetiology. It is the leading cause of non-traumatic neurological disability in young adults in the USA and Europe.1 Clinically, it is characterised by various combinations or isolated symptoms such as fatigue, sensory disorders, acute and subacute motor dysfunction of the limbs, partial or complete visual loss. The most prevalent form of MS is relapsing–remitting MS, which is often transformed into secondary progressive MS, but the disease may be a progressive accumulation of disability from onset (primary progressive MS).2,3 A recent study based on French health administrative databases estimated that about 100,000 persons have MS in France,4 corresponding to a national prevalence of MS in France of 150 per 100,000 inhabitants.
Although MS is a severe disease leading to high healthcare resource use as well as short and long-term disability, the economic burden of the disease and the main cost drivers in France over the last decade have been poorly documented. Progress has been made in the management of MS patients with the arrival of new disease-modifying therapies (DMTs) such as natalizumab and fingolimod, authorised throughout the European Union in 2006 and 2011, respectively. In the current context of escalating healthcare expenditure and growing constraints on healthcare budgets,5,6 there is a need for accurate information concerning the expenditure related to chronic diseases such as MS.7,8
The aim of this study was to describe healthcare expenditure reimbursed by French National Health Insurance to MS patients in 2013 and identify the main expenditure drivers.
Materials and methods
A prevalence-based cost study9 was performed using 2013 French health administrative databases.
The French healthcare system
The French healthcare system is based on a mix of public and private practice, with universal coverage by a public health insurance system called social security, complemented by mutual funds or private insurance companies.10,11 This universal system covers most medical expenses to varying degrees.
French National Health Insurance comprises several insurance schemes. Individuals and their families are covered by a scheme based on their employment status and remain covered by this scheme after retirement. The general scheme covers 87% of the population living in France, and insures private and public employees, including civil servants and students, and the unemployed. There are no major differences between these schemes in terms of coverage.
The majority of medical costs are reimbursed by French National Health Insurance,12 usually about 70% of doctors’ fees, 80% of hospital fees and 65% of prescribed medications considered to be useful and 100% of very expensive drugs administered during a hospital stay, such as natalizumab.11,13 Certain serious, costly or long-term illnesses, called long-term diseases (LTDs), such as MS, are eligible for 100% reimbursement of healthcare expenditure by French National Health Insurance. The remaining medical fees constitute out-of-pocket expenses for the patient, who usually subscribe to mutual funds or private health insurance or are eligible for state-funded free complementary healthcare (Couverture médicale universelle complémentaire, CMUc).11
Data sources
This study was based on French National Health Insurance data (Système National d’Information Interrégimes de l’Assurance Maladie, SNIIRAM) linked to the national hospital discharge database (Programme de Médicalisation des Systèmes d’Information, PMSI) by means of a unique anonymous identifier allocated to each individual.10,14–16
The SNIIRAM contains comprehensive individualised and anonymous data on all healthcare expenditures reimbursed by the French National Health Insurance. It also contains the patient’s LTD status, coded according to the International Statistical Classification of Diseases and Related Health Problems – 10th Revision (ICD-10).
The PMSI describes hospital stays in conventional medical units (short-stay wards), rehabilitation units, homecare units and psychiatric institutions in France. These databases comprise a medical part, indicating the primary and secondary diagnoses according to ICD-10. The PMSI database also contains information on expensive drugs administered in hospital and charged in addition to the stay, such as natalizumab, which can only be administered in the context of a specific one-day hospitalisation.
Study population
This study was based on the prevalent population of MS patients on 31 December 2012, as defined by Foulon et al. in a recent study based on French health administrative databases (SNIIRAM/PMSI).4 Briefly, four criteria were used to identify a prevalent MS case: reimbursement of DMTs, LTD status for MS or disability pension for MS in 2011 or 2012, and any hospitalisation with a diagnosis of MS between 2008 and 2012. Persons who died before 31 December 2012 were excluded.
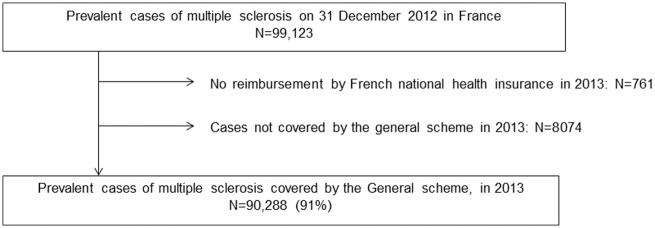
The few subjects ((N=761 (0.8%), Figure 1) who did not receive any reimbursements for healthcare in 2013 were excluded, as they may correspond to people no longer living in France and no longer covered by French National Health Insurance. Furthermore, this study was limited to MS patients covered by the general scheme in 2013 (91% of MS patients, Figure 1), as aggregate expenditure by type of healthcare resource use at the patient level is not available for the other schemes.16
Figure 1.
Patient selection flow chart.
Healthcare utilisation and related expenditures
All healthcare expenditures reimbursed by French National Health Insurance in 2013 to patients with MS were included in the analyses. Healthcare expenditure comprised direct medical costs and certain direct non-medical costs, such as medical devices and transportation services, as defined by Trisolini et al.,9 reimbursed by French National Health Insurance. Expenditure items were classified according to the following subgroups: pharmacy, hospitalisations in public and private institutions, medical fees (physician visits and imaging, including hospital outpatient consultations), paramedical fees (such as nurses and physiotherapists), medical devices (wheelchair, internal prosthesis,…), laboratory tests, transportation and the use of any other resources. Pharmacy included all reimbursed drugs dispensed in pharmacies, as well as expensive drugs administered in hospital.
Sickness benefits
Sick pay and disability pensions paid by French National Health Insurance to general scheme beneficiaries were also described, after excluding students and civil servants for which sickness benefits are not reported, and people older than 59 years, as retired persons are not eligible for these benefits.
Ethical approval
Data access was approved by the French data protection agency (Commission Nationale de l’Informatique et des Libertés).
Results
Study population
A total of 90,288 general scheme beneficiaries in 2013 were included (Figure 1); 65,575 (73%) of these patients were women (Table 1). This population had a mean age of 50 years and LTD status was reported for 75,055 (83%) of them.
Table 1.
Characteristics of multiple sclerosis patients included in the present study (N = 90,288).
| N (%) or mean; standard deviation | |
|---|---|
| Women | 65,575 (73%) |
| Age (years) | 50; 14 |
| Less than 20 | 557 (1%) |
| 20–29 | 5948 (7%) |
| 30–39 | 15,454 (17%) |
| 40–49 | 22,924 (25%) |
| 50–59 | 22,617 (25%) |
| 60–69 | 15,246 (17%) |
| 70–79 | 5596 (6%) |
| More than 80 | 1946 (2%) |
| Long-term disease status for MS | 75,055 (83%) |
| Duration of long-term disease status (years) | 12; 8 |
MS: multiple sclerosis.
Healthcare utilisation and related expenditure
The mean healthcare expenditure per MS patient reimbursed by French National Health Insurance was €11,900 in 2013, for a total healthcare expenditure of €1074 million (Table 2).
Table 2.
Healthcare expenditure of multiple sclerosis patients reimbursed by French national health insurance in 2013 (general scheme).
| MS patients N = 90,288 (%) | Costs reimbursed by French national health insurance in € million (%) | Average annual reimbursement per MS patient concerned by the item in € | Average annual reimbursement per MS patient in € (%) | |
|---|---|---|---|---|
| Medical fees | 89,578 (99%) | 69.0 (6%) | 770 | 764 (6%) |
| Paramedical fees | 63,951 (71%) | 117.4 (11%) | 1836 | 1301 (11%) |
| Laboratory tests | 72,658 (81%) | 10.7 (1%) | 147 | 119 (1%) |
| Transport | 35,160 (39%) | 52.0 (5%) | 1480 | 576 (5%) |
| Other non-hospital expenses | 1689 (2%) | 1.0 (0%) | 580 | 11 (<1%) |
| Medical devices | 62,837 (70%) | 73.4 (7%) | 1168 | 813 (7%) |
| Pharmacy | 87,460 (97%) | 509.2 (47%) | 5822 | 5640 (47%) |
| Disease-modifying therapies | 33,995 (38%) | 409.5 (38%) | 12,046 | 4535 (38%) |
| Glatiramer acetate | 8158 (9%) | 65.5 (6%) | 8032 | 726 (6%) |
| Interferon beta | 19,107 (21%) | 175.0 (16%) | 9159 | 1938 (16%) |
| Fingolimod | 4562 (5%) | 81.0 (8%) | 17,745 | 897 (8%) |
| Natalizumab | 4620 (5%) | 88.0 (8%) | 19,052 | 975 (8%) |
| Hospitalisation | 40,547 (45%) | 241.7 (22%) | 5960 | 2676 (22%) |
| Short-stay units | 37,190 (41%) | 150.8 (14%) | 4055 | 1670 (14%) |
| Rehabilitation units | 8960 (10%) | 76.5 (7%) | 8538 | 847 (7%) |
| Psychiatry | 886 (1%) | 13.9 (1%) | 15,687 | 154 (1%) |
| Total healthcare expenditure | 1074.4 | 11,900 (100%) |
MS: multiple sclerosis.
Pharmacy expenditure represented the leading expenditure item with a mean of €5640, and concerned 97% of MS patients. More specifically, about one-third of MS patients were treated with DMTs, which accounted for 38% of all healthcare expenditure. The direct expenditure of drugs was more than twofold higher for fingolimod (€17,745) and natalizumab (€19,052) than for glatiramer acetate (€8032) and interferon beta (€9159) (Table 2). Symptomatic treatments dispensed in pharmacies accounted for 9% of total expenditure. Most patients received analgesics (81%), 33% received antidepressants and 38% received anxiolytics (Supplementary Table 1).
Hospitalisation was also a substantial expenditure driver, representing 22% of all healthcare expenditure (Table 2). Forty-five per cent of MS patients were hospitalised, including 41% in short-stay units (22% were hospitalised for one night or more) (Supplementary Table 2). Of note, the mean expenditure related to one-day hospitalisations for natalizumab administrations in 2013 was €3950 per treated patient.
Medical fees and paramedical visits accounted for 17% of healthcare expenditure (Table 2). Ninety-two per cent of patients visited their general practitioner in 2013, with a median of six visits (Supplementary Table 3). Fifty-two per cent of all patients and 49% of patients who were never hospitalised in 2013 consulted a private or outpatient neurologist, with a median of two visits. Nurses and physiotherapists were the main paramedical professionals consulted, by 58% and 46% of patients, respectively (Supplementary Table 3). Regarding medical devices, 14% of patients were reimbursed for assisted living devices including crutches and walkers, and 11% were reimbursed for wheelchairs (repairs, rental or purchase).
Analysis of the distribution of healthcare expenditures per patient in 2013 showed that total expenditure was less than €576 for 10% of patients, less than €8933 for 50% of patients, and exceeded €28,418 for 10% of patients (Figure 2). Overall, about 10% of patients accounted for 36% of all expenditure and 20% of patients accounted for 56% of all expenditure.
Figure 2.
Decile of expenditure per multiple sclerosis patient in 2013.
Distribution of healthcare expenditure by gender and age
Mean healthcare expenditure reimbursed by French National Health Insurance in 2013 was close for men (€12,651) and for women (€11,617), with a similar distribution of expenditure items by subgroups (Figure 3).
Figure 3.
Distribution of healthcare expenditure by age and gender.
More than two-thirds of healthcare expenditures concerned persons aged 40–69 years. Mean healthcare expenditure per person with MS remained constant according to age, but with a different distribution of expenditure items (Figure 2). Pharmacy expenditure represented a large share of total expenditure for young MS patients (71% between 20 and 29 years) and decreased with age (18% of expenditure between the ages of 70 and 79 years and 12% after the age of 80 years). Conversely, the share of hospitalisation expenditure increased from 15% between the ages of 20 and 29 years to 35% between the age of 70 and 79 years. Similarly, paramedical fees, including nursing and physiotherapy fees, increased from 2% between the ages of 20 and 29 years to 24% between the ages of 70 and 79 years, respectively.
Sickness benefits
Thirty per cent of patients under the age of 60 years received a disability pension in 2013, corresponding to a mean sum of €9720 paid by French National Health Insurance, and 21% presented with at least one period of sick pay (median number of 29 days of sick leave) (Supplementary Table 4).
Discussion
Main results
This study provides the most comprehensive update on healthcare expenditure reimbursed by French National Health Insurance of MS patients in France since the introduction in Europe of the expensive new DMTs such as fingolimod or natalizumab. This study adds population-based estimates to the data derived from questionnaire-based studies commonly conducted in this field of research. The mean healthcare expenditure, for French National Health Insurance was €11,900 per MS patient in 2013. Although MS patients required a substantial amount of healthcare services, DMTs were the main expenditure driver. Pharmacy expenditure decreased with age, while hospitalisation and paramedical expenditures increased with age.
National healthcare expenditure for all prevalent MS patients identified in France based on health insurance data4 would be €1.2 billion in 2013, by assuming that healthcare expenditure per MS patients was similar among the 90,288 MS patients covered by the general scheme and included in the present study, and the 8074 MS patients covered by other schemes.
Strengths and limitations
The main strength of this study concerns the comprehensive data collection, as this study was based on two comprehensive databases providing prospectively and independently collected complementary data.10,14–16 The SNIIRAM captures all outpatient healthcare reimbursements, whereas PMSI covers all hospital stays in France, in both public and private institutions. In the present study, healthcare expenditures concerned people covered by the general scheme and 91% of the French prevalent population with MS on 31 December 2012 was included; 0.8% (which is negligible) was excluded because they had not received any reimbursements for healthcare in 2013, and 8% because they were covered by a scheme other than the general scheme. The inclusion of these people would probably not have modified the results, as there is no evidence that healthcare is substantially different between schemes.
These health administrative databases contain reliable reimbursement data, as they were constructed for that purpose.10,14,16 Consequently, this analysis was conducted from the French National Health Insurance perspective and we did not report all costs to MS patients. This study assessed direct medical costs, as defined by Trisolini et al.,9 and certain direct non-medical costs such as mobility devices and transportation services. However, we did not compute other direct non-medical costs such as informal care, or home or automobile modifications, for example, and indirect costs, characterised by loss of employment and early mortality, which represent a real burden in MS.7,9,17–19 The algorithm developed by Foulon et al.4 and used in this study to identify MS cases cannot be formally validated, and some MS patients may not have been identified. However, unidentified patients would probably correspond to patients with early disease, in whom the diagnosis remained uncertain, or who did not take any specific MS treatment.
Finally, the severity of disability, measured clinically by the Expanded Disability Status Scale (EDSS) and the precise notion of MS relapses were also not available. Several studies have shown that costs increase with increasing disease severity as measured by the EDSS score,8,17,19–23 or during relapses.21
Comparison with previous French data
Two previous studies have evaluated the cost burden of MS in France based on French health administrative databases.24–26 In contrast with the present study, these studies were based on data from 199425 and 2004,24,26 before the availability of the new expensive DMTs, natalizumab and fingolimod. Using the French consumer price index to take inflation into account and to convert 1994 and 2004 euros into 2013 euros (1.345 to convert 1994 euros to 2013 euros and 1.152 to convert 2004 euros to 2013 euros, www.insee.fr), the healthcare expenditure per patient increased from €7700 per patient in 1994 to €11,626 in 2004 and €12,658 in 2013 among MS patients with LTD status covered by the general scheme (which constituted the study population of the two previous studies, Supplementary Table 5). Healthcare expenditure items shifted from non-medication expenditure towards medications mainly between 1994 and 2004, with a slowdown over the following decade. Indeed, pharmacy expenditure accounted for 13%, 43% and 47% of total expenditure in 1994, 2004 and 2013, respectively. Conversely, hospitalisation expenditure decreased from €3357 in 1994 to €3114 in 2013, accounting for 43% and 25% of total expenditure, respectively (Supplementary Table 5). Interestingly, mean reimbursement per MS patient increased only slightly between 2004 and 2013 in France. A slight modification of the distribution of expenditure items was observed: pharmacy expenditure increased slightly, probably as a result of the introduction of the new DMTs, natalizumab and fingolimod, whereas hospitalisation expenditure decreased slightly.
In a cross-sectional study based on standard questionnaires including 1344 French MS patients, Kobelt et al. estimated the total cost of MS in 2007, considering all direct and indirect costs.27 They reported a mean cost of €44,384, comprising direct costs of €23,654 and indirect costs of €20,730. The direct cost was €16,855 from a public payer perspective, higher than that reported in the present study and by Vallier et al.24,26 However, inpatient care in rehabilitation centres accounted for €4779 per MS patient (corresponding to €5244 after converting to 2013 euros), compared to €847 in the present study, suggesting that the population included in the survey by Kobelt et al. was not entirely comparable to the MS patients identified according to claims diagnoses based on French health administrative data. In another survey including patients from 16 European countries, including 491 from France,19 direct costs in Europe remained higher than in the present study but the public payer perspective was not available. Furthermore, a higher proportion of MS patients in France were treated by DMTs than in the present study (78%, including 51% treated by new DMTs).
Comparison with other previous studies
In a recent systematic review comprising between-country comparisons, Ernstsson et al. observed that the total cost per patient and per year varied considerably between studies, mainly due to differences in terms of the costs included in the analysis and the way in which disease severity was taken into account.8 They also observed that drugs were the main cost drivers for MS patients with low disease severity, whereas the main cost components for groups with more advanced MS were production losses and informal care. Similarly, in the recent cross-sectional study conducted in 16 European countries, Kobelt et al. reported that DMT costs decreased with increasing EDSS, whereas other direct healthcare costs, informal care service, and productivity losses increased with increasing EDSS.19 In the present study, we computed healthcare expenditure by age. Interestingly, medication was the main direct healthcare expenditure item among younger patients, while paramedical care and hospitalisation were the main drivers of direct healthcare expenditure among older patients.
Conclusion
In conclusion, although MS patients required a substantial amount of healthcare, DMTs were the main expenditure driver in 2013 in France. Pharmacy expenditure decreased with increasing age, while hospitalisation and paramedical expenditure increased with age.
Supplementary Material
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the French National Health Insurance Fund (CNAMTS).
Supplementary material
Supplementary material is available for this article online.
References
- 1.Dutta R, Trapp BD. Pathogenesis of axonal and neuronal damage in multiple sclerosis. Neurology 2007; 68: S22-31–54. [DOI] [PubMed] [Google Scholar]
- 2.Hauser SL, Oksenberg JR. The neurobiology of multiple sclerosis: genes, inflammation, and neurodegeneration. Neuron 2006; 52: 61–76. [DOI] [PubMed] [Google Scholar]
- 3.Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology 2014; 83: 278–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foulon S, Maura G, Dalichampt M, et al. Prevalence and mortality of patients with multiple sclerosis in France in 2012: a study based on French health insurance data. J Neurol 2017; 264: 1185–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Comptes nationaux de la Santé 2013 - Édition 2014. Direction de la recherche, des études, de l’évaluation et des statistiques. http://drees.social-sante.gouv.fr/IMG/pdf/comptes_sante_2013_edition_2014.pdf (accessed 30 May 2017).
- 6.Nay O, Béjean S, Benamouzig D, et al. Achieving universal health coverage in France: policy reforms and the challenge of inequalities. Lancet 2016; 387: 2236–2249. [DOI] [PubMed] [Google Scholar]
- 7.Adelman G, Rane SG, Villa KF. The cost burden of multiple sclerosis in the United States: a systematic review of the literature. J Med Econ 2013; 16: 639–647. [DOI] [PubMed] [Google Scholar]
- 8.Ernstsson O, Gyllensten H, Alexanderson K, et al. Cost of illness of multiple sclerosis – a systematic review. PLOS ONE 2016; 11: e0159129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trisolini M, Honeycutt A, Wiener J, et al. Global Economic Impact of Multiple Sclerosis. RTI International for Multiple Sclerosis International Federation, May 2010.
- 10.Bezin J, Duong M, Lassalle R, et al. The national healthcare system claims databases in France, SNIIRAM and EGB: powerful tools for pharmacoepidemiology. Pharmacoepidemiol Drug Saf. Epub ahead of print 24 May 2017. DOI: 10.1002/pds.4233. [DOI] [PubMed]
- 11.Chevreul K, Berg Brigham K, Durand-Zaleski I, et al. France: Health System Review. European Observatory on Health Systems and Policies. Health Systems in Transition 2015; 17: 1–218. [PubMed] [Google Scholar]
- 12.Global Burden of Disease Health Financing Collaborator Network. Evolution and patterns of global health financing 1995–2014: development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. Lancet 2017; 389: 1981–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tableau récapitulatif des taux de remboursement. https://www.ameli.fr/assure/remboursements/rembourse/tableau-recapitulatif-taux-remboursement/tableau-recapitulatif-taux-remboursement (accessed 6 June 2017).
- 14.Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique 2010; 58: 286–290. [DOI] [PubMed] [Google Scholar]
- 15.Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Intern 2015; 36: 411–417. [DOI] [PubMed] [Google Scholar]
- 16.Tuppin P, Rudant J, Constantinou P, et al. Value of a national administrative database to guide public decisions: from the Système National d’Information Interrégimes de l’Assurance Maladie (SNIIRAM) to the Système National des Données de Santé (SNDS) in France. Rev Epidemiol Sante Publique. Epub ahead of print 26 July 2017. DOI: 10.1016/j.respe.2017.05.00. [DOI] [PubMed]
- 17.McCrone P, Heslin M, Knapp M, et al. Multiple sclerosis in the UK: service use, costs, quality of life and disability. Pharmacoeconomics 2008; 26: 847–860. [DOI] [PubMed] [Google Scholar]
- 18.Gyllensten H, Wiberg M, Alexanderson K, et al. Costs of illness of multiple sclerosis in Sweden: a population-based register study of people of working age. Eur J Health Econ. Epub ahead of print 9 May 2017. DOI: 10.1007/s10198-017-0894-6. [DOI] [PMC free article] [PubMed]
- 19.Kobelt G, Thompson A, Berg J, et al. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler 2017; 1352458517694432. [DOI] [PMC free article] [PubMed]
- 20.Kobelt G, Berg J, Lindgren P, et al. Costs and quality of life of patients with multiple sclerosis in Europe. J Neurol Neurosurg Psychiatry 2006; 77: 918–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naci H, Fleurence R, Birt J, et al. Economic burden of multiple sclerosis: a systematic review of the literature. Pharmacoeconomics 2010; 28: 363–379. [DOI] [PubMed] [Google Scholar]
- 22.Karampampa K, Gustavsson A, Miltenburger C, et al. Treatment experience, burden and unmet needs (TRIBUNE) in MS study: results from five European countries. Mult Scler 2012; 18: 7–15. [DOI] [PubMed] [Google Scholar]
- 23.Karampampa K, Gustavsson A, Miltenburger C, et al. Treatment experience, burden, and unmet needs (TRIBUNE) in multiple sclerosis: the costs and utilities of MS patients in Canada. J Popul Ther Clin Pharmacol 2012; 19: e11–e25. [PubMed] [Google Scholar]
- 24.Vallier N, Weill A, Salanave B, et al. [Cost of thirty long-term diseases for beneficiaries of the French general health insurance scheme in 2004]. Pratique et organisation des Soins 2006; 37: 267–283. [Google Scholar]
- 25.Fender P, Paita M, Salanave B, et al. [National Health Insurance expenditures in 1994 for thirty long-term illness]. Sante Publique 2000; 12: 5–19. [PubMed] [Google Scholar]
- 26.Fromont A, Lehanneur M-N, Rollot F, et al. [Cost of multiple sclerosis in France]. Rev Neurol (Paris) 2014; 170: 432–439. [DOI] [PubMed] [Google Scholar]
- 27.Kobelt G, Texier-Richard B, Lindgren P. The long-term cost of multiple sclerosis in France and potential changes with disease-modifying interventions. Mult Scler 2009; 15: 741–751. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.