Abstract
Background:
Improvements in pain, function, and patient satisfaction are used to evaluate the outcomes of hip arthroscopic surgery.
Purpose:
To identify correlations between the visual analog scale (VAS) score for pain and patient satisfaction with 4 commonly used patient-reported outcome (PRO) scores to determine to what extent changes in these 2 parameters are reflected in each of the PRO scores.
Study Design:
Cohort study (diagnosis); Level of evidence, 3.
Methods:
Patients undergoing hip arthroscopic surgery between February 2008 and February 2013 were assessed prospectively before surgery, at 3 months, and annually thereafter with the modified Harris Hip Score (mHHS), Nonarthritic Hip Score (NAHS), Hip Outcome Score–sports-specific subscale (HOS-SSS), and Hip Outcome Score–activities of daily living (HOS-ADL). Patients were also assessed using a 10-point VAS for pain and queried for satisfaction at the same time points (“0” indicated no pain, and “10” indicated complete satisfaction with surgery). The VAS score and patient satisfaction were correlated with changes in the 4 PRO scores.
Results:
During the study period, 1417 patients underwent hip arthroscopic surgery, of whom 1137 patients had 2-year postoperative PRO scores after primary surgery. There was a significant improvement in all PRO scores at 2-year follow-up. The mean improvements in mHHS, NAHS, HOS-ADL, and HOS-SSS scores were 16.7, 21.6, 19.7, and 22.7 points, respectively. The mean improvement in the VAS score was 2.9 points. Mean patient satisfaction at 2-year follow-up was 7.74 (of 10). There was a statistically significant correlation between the VAS and patient satisfaction scores and changes in each of the 4 PRO scores. The strength of the correlation was moderate.
Conclusion:
This study demonstrated a moderate correlation between the VAS and patient satisfaction outcomes and changes in 4 commonly used PRO scores in hip arthroscopic surgery (mHHS, HOS-ADL, HOS-SSS, and NAHS). In addition to several PRO instruments, a VAS for pain and patient satisfaction may add to the overall assessment of the efficacy of hip arthroscopic surgery.
Keywords: hip arthroscopic surgery, patient-reported outcomes, patient satisfaction, visual analog scale for pain
The efficacy of arthroscopic hip interventions has largely been determined by outcome-based research.6,18,20 Outcomes assess improvements in pain and function and patient satisfaction with the procedure.1,13,19,20 Clinimetric analysis has suggested that no single patient-reported outcome (PRO) measure is adequate to assess the efficacy of hip arthroscopic surgery.8,10,13,17 Hence, applying several outcome tools is more effective than a single PRO for measuring pain, function, and satisfaction.8,10,13,17 However, the practical limitations of using multiple outcome tools include time restraints and questionnaire fatigue, leading to inaccurate responses.
Currently, there are several PRO questionnaires in use for patients with hip disorders.9,20 The most commonly used questionnaires are the Hip Outcome Score (HOS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the Nonarthritic Hip Score (NAHS), the modified Harris Hip Score (mHHS), and the Merle d’Aubigne hip score.1 Each of these hip outcome tools has its limitations. The HOS is a functional score that did not include patients in its development, the WOMAC was developed for an elderly population with arthritis, and the NAHS uses 10 questions from the WOMAC and is potentially undermined by ceiling effects.2,13,20 The mHHS is probably the most commonly used outcome measure worldwide because it can be used for both arthroscopic and arthroplasty procedures of the hip.3,4,9,15
With respect to assessments for pain, the HOS–activities of daily living (ADL) and HOS–sports-specific subscale (SSS) do not contain specific pain profile questions.11,14,16,19 The NAHS assesses pain on a scale from 0 to 4 (0 being extreme pain) with 5 specific activities.14 The mHHS has 1 question on pain.1 The visual analog scale (VAS) is a patient-reported pain scale from 0 to 10 (with 0 being no pain and 10 being the worst pain imaginable) that is increasingly being used to assess outcomes after arthroscopic hip interventions.11 A limitation of the VAS for pain is that it is an instantaneous measure and does not take into account the temporal arrangement of pain.11
Recently, questionnaires specific to PROs after hip arthroscopic surgery have been developed to address these limitations. These include the International Hip Outcome Tool 33 (iHOT-33). The iHOT-33 was developed in 2012 and measures 4 domains: (1) symptoms and functional limitations, (2) sports and recreational physical activities, (3) job-related concerns, and (4) social, emotional, and lifestyle concerns.16 It has been shown to be reliable; shows face, content, and construct validity; is highly responsive to clinical change; and has been suggested to be a primary outcome measure for prospective patient evaluations and randomized clinical trials.17 However, as it is a recently developed tool, it has not been as widely used as the other questionnaires, which are more prevalent in studies with longer term follow-up.7
The most commonly used questionnaires do not specifically assess patient satisfaction. Instead, patient satisfaction is often separately measured with either a binary response of “yes” or “no” to the question “were you satisfied with the surgery?” or a scale from 0 to 10 (where 0 is not satisfied and 10 is completely satisfied).4 Furthermore, patient satisfaction may be related to factors beyond the scope of the surgical procedure. Aprato et al1 analyzed the correlation between patient satisfaction and the mHHS score and concluded that the mHHS does have limitations as an outcome measure in the prediction of patient satisfaction.
To date, there have been no studies that have correlated the VAS or patient satisfaction outcomes to other commonly used PRO scores in hip arthroscopic surgery. The purpose of this article was to identify possible correlations between the VAS score and patient satisfaction with PRO scores (mHHS, NAHS, HOS-SSS, HOS-ADL) in hip arthroscopic surgery to determine to what extent changes in these 2 parameters are reflected in each of the PRO scores.
Methods
Patient Selection and Outcome Measures Collected
All patients who underwent hip arthroscopic surgery performed by the senior author (B.G.B.) between the period of February 2008 and February 2013 were included in this study. Patients were excluded if they had undergone revision surgery; had arthritis rated greater than Tönnis grade 1 on radiographs; or had previous hip conditions such as inflammatory arthritis, avascular necrosis, slipped femoral capital epiphysis, or fractures. Patient age at surgery, side of surgery, sex, and body mass index were prospectively recorded in a customized database. Patients were assessed prospectively before surgery, at 3 months postoperatively, and annually thereafter with the mHHS, NAHS, HOS-SSS, HOS-ADL, and VAS. Patients were also instructed to rate their satisfaction with surgery out of 10, with 10 being completely satisfied and 0 being not satisfied with surgery, at each of the above follow-up time points. Approval for the study was obtained from our institutional review board.
Surgical Procedure
All hip arthroscopic procedures were performed in the supine position using a traction table and a well-padded perineal post under general anesthesia. Intraoperative procedures performed in the central, peripheral, and peritrochanteric compartments were recorded. As a general treatment algorithm, pincer impingement was treated with acetabuloplasty, and cam impingement was treated with femoroplasty. Labral lesions were debrided, repaired, or reconstructed with an autograft or allograft depending on the size and available labral tissue for repair. Iliopsoas release was performed in patients with symptomatic internal snapping or a positive iliopsoas impingement sign on the labrum. The capsule was repaired routinely except in patients in whom a release was considered to be therapeutic, such as patients with stiff hips or thickened capsules. Peritrochanteric procedures included trochanteric bursectomy, gluteus medius and minimus repairs, and iliotibial band fractional lengthening. Postoperative rehabilitation was tailored to the specific intraoperative procedure performed.
Statistical Analysis
Statistical analysis was performed using Excel 2007 (Microsoft). Normal data distribution was checked by the test for equality of variance. Correlations were analyzed with the Pearson test of linear correlation when data were numerical and with the Pearson chi-square test when data were categorical. Correlation strength was defined according to Dancey and Reidy5 as weak (0.1-0.3), moderate (0.4-0.6), or strong (0.7-0.9). Differences between preoperative and postoperative PRO scores were analyzed with the paired-samples t test. P values <.05 were considered statistically significant.
Results
Demographics and Intraoperative Procedures Performed
During the study period, 1417 patients underwent hip arthroscopic surgery, of whom 1137 (80.2%) had 2-year PRO scores recorded. Table 1 shows demographic characteristics of the study population, including the mean age, number of male patients, and mean body mass index. Moreover, 6.3% of patients required revision arthroscopic surgery, and 3.0% of the patients required conversion to arthroplasty within 2 years of their index arthroscopic surgery. Table 2 shows the type and number of soft tissue and bony procedures performed in the population.
TABLE 1.
Demographics of Study Population (N = 1137)
| Characteristic | n (%) or mean (range) |
|---|---|
| Male sex | 297 (26.1) |
| Left side | 495 (43.5) |
| Age at surgery, y | 36.7 (13.1-76.3) |
| Body mass index, kg/cm2 | 25.1 (13.5-48.7) |
| Follow-up time, mo | 28.4 (23.5-69.0) |
| Revision arthroscopic surgery | 72 (6.3) |
| Conversion to total hip arthroplasty/Birmingham hip resurfacing | 34 (3.0) |
TABLE 2.
Procedures Performed in Study Population
| Procedure | n (%) |
|---|---|
| Labral treatment | |
| Repair | 670 (58.93) |
| Debridement | 382 (33.60) |
| Reconstruction | 20 (1.76) |
| Other | 14 (1.23) |
| None | 5 (0.44) |
| Capsular treatment | |
| Repair | 206 (18.12) |
| Release | 248 (21.81) |
| Partial capsulotomy | 18 (1.58) |
| None | 3 (0.26) |
| Acetabuloplasty | 789 (69.39) |
| Acetabular microfracture | 110 (9.67) |
| Acetabular chondroplasty | 207 (18.20) |
| Acetabular subchondral cyst removal | 34 (2.99) |
| Femoral osteoplasty | 818 (71.94) |
| Femoral head microfracture | 14 (1.23) |
| Femoral head chondroplasty | 76 (6.68) |
| Femoral subchondral cyst removal | 34 (2.99) |
| Notchplasty | 60 (5.28) |
| Subspine decompression | 16 (1.41) |
| Ligamentum teres treatment | 433 (38.08) |
| Iliopsoas release | 368 (32.37) |
| Iliopsoas bursectomy | 12 (1.06) |
| Iliotibial band release | 11 (0.97) |
| Trochanteric bursectomy | 136 (11.96) |
| Gluteus medius/minimus repair | 49 (4.31) |
| Gluteus maximus transfer | 0 (0.00) |
| Piriformis release | 10 (0.88) |
| Sciatic neurolysis | 9 (0.79) |
| Removal of loose body | 158 (13.90) |
| Removal of heterotopic ossification | 1 (0.09) |
PROs, VAS, and Patient Satisfaction at 2-Year Follow-up
Table 3 shows the mean change in PRO and VAS scores and patient satisfaction from baseline to 2 years for the study population. Patients who underwent revision arthroscopic surgery or arthroplasty before 2-year follow-up were excluded from the analysis of PROs, VAS, and patient satisfaction. There was a significant improvement in all mean PRO scores at 2-year follow-up. There was also a significant improvement in the mean VAS score from 5.74 to 2.75 points for the same time period. Mean patient satisfaction was 7.74.
TABLE 3.
PRO and VAS Scores and Patient Satisfaction at Baseline and 2-Year Follow-upa
| Score | Preoperative | Postoperative | Change | P Value |
|---|---|---|---|---|
| mHHS | 62.1 ± 15.5 | 78.9 ± 17.4 | 16.7 ± 19.6 | <.05 |
| NAHS | 58.8 ± 18.0 | 80.5 ± 18.1 | 21.6 ± 19.8 | <.05 |
| HOS-ADL | 63.1 ± 19.7 | 83.4 ± 18.4 | 19.7 ± 19.6 | <.05 |
| HOS-SSS | 41.3 ± 24.2 | 64.4 ± 30.4 | 22.7 ± 33.0 | <.05 |
| VAS | 5.7 ± 2.3 | 2.8 ± 2.5 | –2.9 ± 3.0 | <.05 |
| Patient satisfaction | 7.7 ± 2.4 |
aHOS-ADL, Hip Outcome Score–activities of daily living; HOS-SSS, Hip Outcome Score–sports-specific subscale; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score; VAS, visual analog scale.
Correlation Between PROs, VAS, and Patient Satisfaction
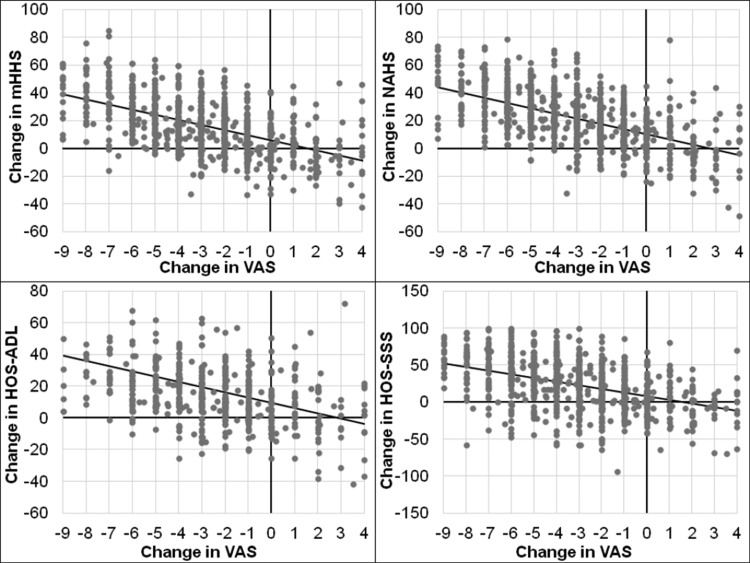
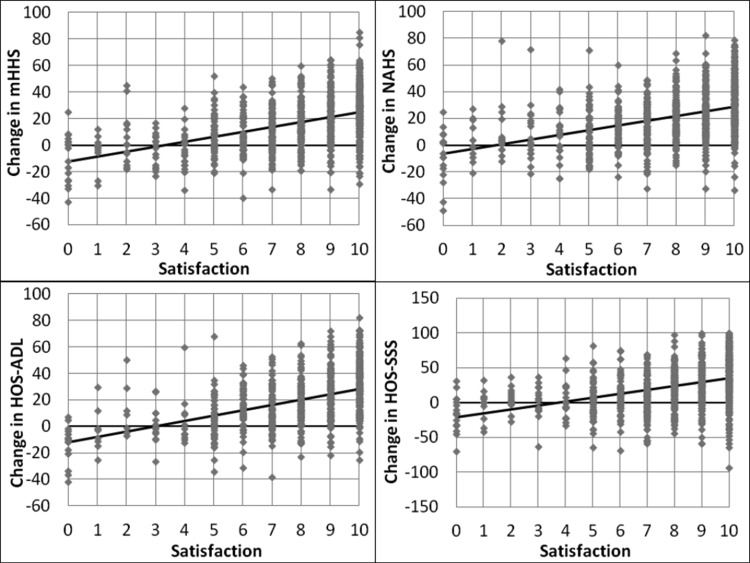
Table 4 and Figure 1 show the correlations between changes in mean PRO scores with the mean VAS score at 2-year follow-up. The mean VAS score was significantly correlated with changes in each of the mean PRO scores (P < .05). The strongest correlation was for the mHHS, followed by the NAHS, HOS-ADL, and HOS-SSS. The strength of the correlations, as defined by Dancey and Reidy,5 was moderate for all the PROs and VAS. However, there was no significant difference in the strength of the correlation between each of the PROs and the VAS. Table 4 and Figure 2 show the correlations between changes in mean PRO scores with mean patient satisfaction at 2-year follow-up. The strongest correlation was for the mHHS, followed by the NAHS, HOS-ADL, and HOS-SSS. The strength of the correlations, as defined by Dancey and Reidy,5 was moderate for all the PROs and patient satisfaction. However, there was no significant difference in the strength of the correlation between each of the PROs and patient satisfaction. There was a moderate correlation between improvements in the VAS score and patient satisfaction (Table 4).
TABLE 4.
Pearson Correlation Coefficients for VAS Score and Patient Satisfaction and Changes in PRO Scoresa
| Score | ΔmHHS | ΔNAHS | ΔHOS-ADL | ΔHOS-SSS | ΔVAS |
|---|---|---|---|---|---|
| VAS | 0.57844 | 0.57245 | 0.49265 | 0.46032 | N/A |
| Patient satisfaction | 0.482217 | 0.458132 | 0.453796 | 0.419955 | 0.45907 |
aHOS-ADL, Hip Outcome Score–activities of daily living; HOS-SSS, Hip Outcome Score–sports-specific subscale; mHHS, modified Harris Hip Score; N/A, not applicable; NAHS, Nonarthritic Hip Score; PRO, patient-reported outcome; VAS, visual analog scale.
Figure 1.
Correlation between improvements in visual analog scale (VAS) and patient-reported outcome (PRO) scores. There was only a moderate correlation between changes in VAS and PRO scores, with the strongest correlation being with the modified Harris Hip Score (mHHS). HOS-ADL, Hip Outcome Score–activities of daily living; HOS-SSS, Hip Outcome Score–sports-specific subscale; NAHS, Nonarthritic Hip Score.
Figure 2.
Correlation between improvements in patient satisfaction and patient-reported outcome (PRO) scores. There was only a moderate correlation between patient satisfaction and changes in PRO scores, with the strongest correlation being with the modified Harris Hip Score (mHHS). HOS-ADL, Hip Outcome Score–activities of daily living; HOS-SSS, Hip Outcome Score–sports-specific subscale; NAHS, Nonarthritic Hip Score.
Discussion
The present study demonstrated a statistically significant correlation between the VAS and patient satisfaction scores and changes in 4 commonly used PRO scores in hip arthroscopic surgery. However, the strength of the correlation was only moderate, with the strongest correlation being for the mHHS. This may be because 25% of the mHHS questionnaire consists of pain-related items. The results of this study suggest that no single PRO of the 4 analyzed in the study sufficiently assesses pain, function, and patient satisfaction after hip arthroscopic surgery and that scales of pain and patient satisfaction are helpful in addition to PROs to assess the efficacy of the procedure.
Several other studies have similarly concluded that multiple PROs are required to assess the efficacy of hip arthroscopic surgery. Lodhia et al13 conducted a systematic review of the content and clinimetric evidence of published PROs used to assess femoroacetabular impingement and labral abnormalities. They identified 6 related PRO instruments, of which only the HOS, NAHS, and WOMAC had clinimetric evidence. The HOS had the greatest amount of clinimetric evidence and was the most proven instrument for use in patients with femoroacetabular impingement and labral abnormalities. This is despite the fact that the HOS does not have any specific questions relating to pain.
Several studies have looked at the clinical utility of more recently developed questionnaires specific to the young adult hip population. Kemp et al10 have suggested that the iHOT-33 and the Hip Disability and Osteoarthritis Outcome Score (HOOS) demonstrated greater psychometric properties than the mHHS and HOS. Ramisetty et al17 reported that the iHOT-33 scored better than the other PROs and gave it the highest recommendation for the assessment of hip preservation procedures. However, these tools have been more recently developed, and several long-term studies still report using the mHHS, HOS, and NAHS.7 The current study suggests that improvements in these PRO scores in isolation only moderately correlate with improvements in pain and patient satisfaction. Further research is required as to whether the more newly developed PROs will ultimately lead to a single measure that best assesses the efficacy of hip procedures.
Aprato et al1 evaluated the correlation between patient satisfaction and the mHHS score after hip arthroscopic surgery. They found that patient satisfaction was correlated with both pain- and function-specific questions of the mHHS. However, the strength of these correlations was limited because both groups of questions could be influenced by patient expectations and desired activity levels.
Kersten et al11,12 evaluated whether the VAS was linear and responsive to change in 221 patients with hip or knee pain waiting for joint replacement. They found that the VAS was a valid tool for measuring pain at a single point in time but that it did not behave linearly; in addition, responsiveness varied along the trait of pain. They concluded that minimum clinically important differences using raw data, or changes in scores in general, were invalid, as these would either underestimate or overestimate the true change.
Our findings are in concordance with the above-mentioned studies. Specifically, there was no ideal PRO instrument to determine the effectiveness of outcomes after hip arthroscopic surgery. Further, correlating the VAS score with changes in other PRO scores was difficult because of heterogeneity in patient expectations of outcomes. Further clinimetric analyses of many of the PROs, including newer ones such as the iHOT-33, are still required to assess their utility in the population undergoing hip arthroscopic surgery.
The strengths of this study include the large patient numbers and the use of 4 PROs, the VAS, and patient satisfaction. There are also limitations of this study. Most notably, the VAS and patient satisfaction were instantaneous measures of outcomes that may not be reflective of outcomes over a prolonged time period. Moreover, these measures are influenced by variations in patient expectations and experiences. Also, the VAS questionnaire can be administered at different time points in relation to the other PROs, and this may have an impact on responses. A possible method to address this for future research may include the assessment of total analgesic use as a surrogate marker of pain. Finally, newer PROs, although currently being implemented, were not assessed because there were not sufficient 2-year outcome data for statistical analysis. Hopefully, this can be addressed in the future.
Conclusion
This study demonstrated a moderate correlation between the VAS and patient satisfaction outcomes and changes in 4 commonly used PRO scores in hip arthroscopic surgery (mHHS, HOS-ADL, HOS-SSS, and NAHS). The equivalence of changes in these PRO scores with the VAS and patient satisfaction suggests that in addition to several PRO instruments, a VAS for pain and patient satisfaction may add to the overall assessment of the efficacy of hip arthroscopic surgery.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.G.D. is a consultant for Arthrex, Pacira, Stryker, Amplitude, and Medacta; receives institutional research support from Arthrex, Breg, ATI, Pacira, Stryker, Medacta, and Adventist Hinsdale Hospital; and receives royalties from Orthomerica and DJO Global.
Ethical approval for this study was obtained from the Advocate Health Care Institutional Review Board (ID: 5276).
References
- 1. Aprato A, Jayasekera N, Villar RN. Does the modified Harris Hip Score reflect patient satisfaction after hip arthroscopy? Am J Sports Med. 2012;40(11):2557–2560. [DOI] [PubMed] [Google Scholar]
- 2. Baldwin KD, Harrison RA, Namdari S, Nelson CL, Hosalkar HS. Outcomes of hip arthroscopy for treatment of femoroacetabular impingement: a systematic review. Curr Orthop Pract. 2009;20(6):669–673. [Google Scholar]
- 3. Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90(12):1570–1575. [DOI] [PubMed] [Google Scholar]
- 4. Ben Tov T, Amar E, Shapira A, Steinberg E, Atoun E, Rath E. Clinical and functional outcome after acetabular labral repair in patients aged older than 50 years. Arthroscopy. 2014;30(3):305–310. [DOI] [PubMed] [Google Scholar]
- 5. Dancey CP, Reidy J. Statistics Without Maths for Psychology: Using SPSS for Windows. Harlow, UK: Prentice Hall; 2004. [Google Scholar]
- 6. Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31(4):643–650. [DOI] [PubMed] [Google Scholar]
- 7. Harris-Hayes M, McDonough CM, Leunig M, Lee CB, Callaghan JJ, Roos EM. Clinical outcomes assessment in clinical trials to assess treatment of femoroacetabular impingement: use of patient-reported outcome measures. J Am Acad Orthop Surg. 2013;21 Suppl 1: S39–S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hinman RS, Dobson F, Takla A, O’Donnell J, Bennell KL. Which is the most useful patient-reported outcome in femoroacetabular impingement? Test-retest reliability of six questionnaires. Br J Sports Med. 2014;48(6):458–463. [DOI] [PubMed] [Google Scholar]
- 9. Kemp JL, Collins NJ, Makdissi M, Schache AG, Machotka Z, Crossley K. Hip arthroscopy for intra-articular pathology: a systematic review of outcomes with and without femoral osteoplasty. Br J Sports Med. 2012;46(9):632–643. [DOI] [PubMed] [Google Scholar]
- 10. Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013;41(9):2065–2073. [DOI] [PubMed] [Google Scholar]
- 11. Kersten P, White PJ, Tennant A. Is the pain visual analogue scale linear and responsive to change? An exploration using Rasch analysis. PLoS ONE. 2014;9(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kersten P, White PJ, Tennant A. The visual analogue WOMAC 3.0 scale: internal validity and responsiveness of the VAS version. BMC Musculoskelet Disord. 2010;11:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lodhia P, Slobogean GP, Noonan VK, Gilbart MK. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthroscopy. 2011;27(2):279–286. [DOI] [PubMed] [Google Scholar]
- 14. Mohtadi NGH, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28(5):595–605, quiz 606-610.e1. [DOI] [PubMed] [Google Scholar]
- 15. Philippon MJ, Schroder E Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59–65. [DOI] [PubMed] [Google Scholar]
- 16. Potter BK, Freedman BA, Andersen RC, Bojescul JA, Kuklo TR, Murphy KP. Correlation of Short Form-36 and disability status with outcomes of arthroscopic acetabular labral debridement. Am J Sports Med. 2005;33(6):864–870. [DOI] [PubMed] [Google Scholar]
- 17. Ramisetty N, Kwon Y, Mohtadi N. Patient-reported outcome measures for hip preservation surgery: a systematic review of the literature. J Hip Preserv Surg. 2015;2(1):15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Srinivasan SC, Hosny HA, Williams MR. Combined hip arthroscopy and limited open osteochondroplasty for anterior femoroacetabular impingement: early patient reported outcomes. Hip Int. 2013;23(2):218–224. [DOI] [PubMed] [Google Scholar]
- 19. Thorborg K, Roos EM, Bartels EM, Petersen J, Hölmich P. Validity, reliability and responsiveness of patient-reported outcome questionnaires when assessing hip and groin disability: a systematic review. Br J Sports Med. 2010;44(16):1186–1196. [DOI] [PubMed] [Google Scholar]
- 20. Tijssen M, van Cingel R, van Melick N, de Visser E. Patient-reported outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskelet Disord. 2011;12:117. [DOI] [PMC free article] [PubMed] [Google Scholar]