Abstract
We examined the effect of Ca2+ on skeletal muscle glucose transport and fatty acid oxidation using L6 cell cultures. Ca2+ stimulation of glucose transport is controversial. We found that caffeine (a Ca2+ secretagogue) stimulation of glucose transport was only evident in a two-part incubation protocol (“post-incubation”). Caffeine was present in the first incubation, the media removed, and labeled glucose added for the second. Caffeine elicited a rise in Ca2+ in the first incubation that was dissipated by the second. This post-incubation procedure was insensitive to glucose concentrations in the first incubation. With a single, direct incubation system (all components present together) caffeine caused a slight inhibition of glucose transport. This was likely due to caffeine induced inhibition of phosphatidylinositol 3-kinase (PI3K), since nanomolar concentrations of wortmannin, a selective PI3K inhibitor, also inhibited glucose transport, and previous investigators have also found this action.
We did find a Ca2+ stimulation (using either caffeine or ionomycin) of fatty acid oxidation. This was observed in the absence (but not the presence) of added glucose. We conclude that Ca2+ stimulates fatty acid oxidation at a mitochondrial site, secondary to malonyl CoA inhibition (represented by the presence of glucose in our experiments). In summary, the experiments resolve a controversy on Ca2+ stimulation of glucose transport by skeletal muscle, introduce an important experimental consideration for the measurement of glucose transport, and uncover a new site of action for Ca2+ stimulation of fatty acid oxidation.
Abbreviations: CaMKK, Calmodulin kinase; PI3K, Phosphatidylinositol 3-kinase; KHB, Krebs Henseleit bicarbonate; CAT I, Carnitine acyl transferase
Keywords: Glucose transport, Fatty acid oxidation, AMP kinase, Skeletal muscle, L6 cells
Highlights
-
•
Calcium stimulates muscle palmitate oxidation but not glucose transport.
-
•
Previous studies indicating calcium stimulation of glucose transport required to separate incubation (“post-incubation”).
-
•
Glucose transport in the post-incubation protocols are independent of glucose as a substrate and show stimulation by caffeine independent of calcium concentration.
-
•
Calcium stimulation of palmitate oxidation is suppressed by glucose.
-
•
Glucose uncompetitively suppresses fatty acid oxidation.
1. Introduction
Muscle contraction is attended by two established signals: AMP Kinase (AMPK) and Ca2+. AMPK is known to activate two pathways in energy metabolism: glucose transport and fatty acid oxidation [1], [2], [3], [4], [5]. The metabolic actions of Ca2+ are controversial.
It has been proposed that Ca2+ stimulates glucose transport by skeletal muscle, but the findings are controversial [6], [7], [8]. It has been suggested that the ability of Ca2+ to activate a calmodulin-dependent kinase kinase (CaMKK) which in turn activates AMPK may lead to an increased glucose transport [7]. However, in the same review, the authors cautioned that this relies on relatively nonselective inhibitors, such as KN62 which also blocks insulin-stimulated glucose transport [7]. Ca2+ can increase the translocation of GLUT4 both in L6 cells [9] and cardiomyocytes [10]. Surprisingly, the latter study found that Ca2+ elevation had no effect on the pathway of glucose transport itself in cardiomyocytes [10].
There are fewer studies on Ca2+ activation of fatty acid oxidation. Abbott et al. [11] proposed that the Ca2+ activation of the Calmodulin dependent Kinase (CaMKK) activates AMPK, which in turn leads to an increased fatty acid oxidation [12]. However, the experiments of Abbott et al. [11] were indirect, based on inhibition of fatty acid oxidation by the CaMKK inhibitor STO-609. A side effect of STO-609 is direct inhibition of AMPK [13], complicating the interpretation of the results. No evidence exists to show that Ca2+ can stimulate fatty acid oxidation in an intact cell system. Watt et al. [14] performed experiments with cyclopiazolic acid, which inhibits reuptake of cytosolic Ca2+ into the sarcoplasmic reticulum. They found that incubation with cyclopiazolic acid increased uptake and esterification of added palmitate, but did not change the rate of fatty acid oxidation. In cardiomyocytes, elevation of Ca2+ did not stimulate palmitate uptake, although fatty acid oxidation itself was not measured in that study [10].
In the present study, we investigated glucose transport and fatty acid oxidation by isolated L6 skeletal muscle cells. We were able to replicate both sides of the controversy for glucose transport. Neither caffeine nor ionomycin stimulated glucose transport in direct assays, but did in a post-incubation procedure. We showed that the post-incubation procedure does not faithfully report the glucose transport as a function of added glucose itself, while direct incubation did so. We also provide the first evidence of a Ca2+ stimulation of fatty acid oxidation that is secondary to the mitochondrial import step.
2. Methods
2.1. Materials
L6 cells were generously provided by Dr. K.M. Ojama (North Shore University Hospital, Manhasset, New York). Dulbecco's Modified Eagles’ Medium, Fetal Bovine Serum, Hank's Balanced Salt Solution, trypsin, α-Minimum Essential Medium (α-MEM) and Horse Serum (HS) were from Life Technologies, Inc. Palmitic acid was from Nuchek Prep, Inc. 2-Deoxy-d-[2,6-3H]glucose and [U-14C]palmitate were from Amersham Pharmacia Biotech. Scintillation vials were obtained from Wheaton and Scintisafe cocktail was from Fischer Chemical. Tissue culture flasks and multi well plates were obtained from Corning. BAPTA-AM was purchased from Molecular Probes. Indo-1AM was obtained from Life Technologies, Eugene, OR. All other compounds were from Sigma-Aldrich.
2.2. Cell culture
L6 rat skeletal muscle cells were cultured in growth medium composed of the proliferation medium DMEM supplemented with 10% FBS. Cells were converted to myotubes by switching to a low serum medium (2% horse serum) for 1 day, and then 1% horse serum for 7 days prior to use for experiments. Details of cell preparation are provided in a prior publication [15]. All experiments were carried out using fully differentiated L6 myotubes.
2.3. Glucose transport assay
Glucose transport was determined as the rate of 2-deoxy-d-[2,6-3H]glucose uptake, using modification of a previous method [16]. The cells were first incubated for 15 min with Krebs–Henseleit bicarbonate buffer (KHB), glucose, and other agents as indicated. At this point, the labeled deoxyglucose (0.6 μCi) was added to each well and the incubation continued for 45 min. The media was aspirated, and the wells were washed three times with ice-cold KHB to remove exogenous label. The cells were lysed by the addition of 0.1% Triton-X100 (1 ml). Samples of each well were mixed with aqueous scintillation fluid and measured by liquid scintillation counting.
2.4. Glucose transport assay – post-incubation method
This procedure was modified from that of Klip et al. [17]. α-MEM containing 1% (v/v) HS was aspirated and the cells were washed with HBSS. 2 ml of fresh serum-free α-MEM was added and the cells were pre-incubated in an atmosphere of 5% CO2 at 37 °C for 2 h. At the end of the 2 h pre-incubation period, the medium was aspirated and 1 ml of Krebs–Henseleit bicarbonate buffer (pH 7.4) containing 1% albumin was added. Subsequently, the indicated concentrations of glucose, palmitate and 2 mM carnitine were added (along with test compounds) and cells were incubated in an atmosphere of 5% CO2 at 37 °C for 1 h (first incubation). The media was then aspirated and the cells were rinsed three times with HEPES buffer (20 mM HEPES, 118 mM NaCl, 1.2 mM MgSO4, 1 mM CaCl2, pH 7.4), after which cells were incubated in HEPES buffer containing 0.1 mM glucose and 0.6 µCi of 2-deoxy-d-[2,6-3H]glucose in a CO2-free incubator for 15 min at 37 °C. Subsequently, the media was aspirated and the cells were washed three times with cold HEPES buffer. The cells were lysed with a 0.1% Triton-X100 solution, analyzed by scintillation counting.
2.5. Palmitate oxidation assay
Palmitate oxidation was measured as the rate of 14CO2 production from 14C-labeled palmitic acid, based on an established procedure [18] with the following modifications. The KHB for these incubations was supplemented with fatty-acid poor albumin, dialyzed against the same buffer (three changes). The final albumin concentration was 1%. After an initial 10 min incubation, all samples received 2 mM carnitine and [1-14C]palmitic acid (1 µCi/mole), and other additions as noted, and incubations continued to the end of 3 h. Aliquots of 0.8 ml were taken from each well to an Eppendorf tube. Each tube had a circular piece of filter paper (produced by a paper punch) attached to the inside of the lid, to which 15 µl of 2 M NaOH was added. 200 µL of 3 M perchloric acid was carefully added to the side of the tube, and the lid was quickly closed. The tubes were incubated overnight to allow the [14C]CO2 to be absorbed into the wick. The caps were removed with scissors and placed in 10 ml of liquid scintillation fluid for counting.
2.6. Total protein
Protein was determined using the bicinchoninic acid protein assay [19]. Bovine serum albumin was used as the standard.
2.7. Cytosolic Ca2+ measurement
Free cytosolic Ca2+ was measured using the ester Indo-AM, by procedures used previously in our lab [20]. Cells were incubated with 4 µM of Indo-AM dye in HBSS Hank's Balanced Salt Solution) for 1 h. Probenecid and pluronic acid were added at final concentrations of 0.03% and 2.7 mM respectively. Cells were washed twice after incubation with the dye and then incubated in HBSS for another hour to allow de-esterification. Subsequently, ACLAR sheets were placed in a quartz cuvette containing 1 ml of Ca2+ buffer at an inclination of approximately 45°. Ca2+ measurements were performed with an Hitachi F-2500 spectrofluorimeter at excitation wavelengths of 405 and 485 nm and the emission wavelength of 510 nm. In the post-incubation Ca2+ assay, cells were moved to new media by removing the strip containing the cells from one cuvette to another; the interval between media was less than 15 s. Following intracellular Ca2+ measurements, the ACLAR strip was subjected to treatment with 0.1% Triton X100 and 20 mM of EGTA in order to calculate maximum and minimum background calcium. Maximum calcium fluorescence (Fmax) was measured after Triton X100 treatment, and minimum calcium fluorescence (Fmin) after EGTA addition. Standard radiometric analysis using the Grynkewicz equation [21] was conducted as in our prior studies [22].
2.8. Statistical analysis
Statistical evaluation was performed using independent t-test and Analysis of Variance with the use of Tukey's test for post-hoc comparisons. Data represents the average of 3 or more experiments. Data are expressed as means±S.E.M. The level of significance was set at p<0.05.
3. Results
3.1. Effect of caffeine on glucose transport
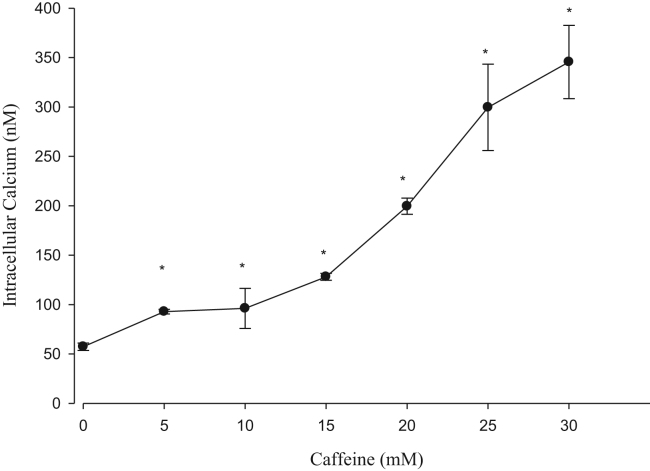
To assess a possible role for Ca2+ in glucose transport, we incubated cells with caffeine, which is known to release Ca2+ from muscle sarcoplasmic reticulum [23]. We have previously used caffeine for this purpose in L6 and other cell types [24], [25]. For confirmation, we conducted a caffeine titration (Fig. 1) which showed the expected caffeine-induced elevation of cytosolic Ca2+ in L6 cells.
Fig. 1.
Caffeine increases cytosolic Ca2+. Cells were incubated with various concentrations of caffeine and cytosolic Ca2+ measured by Indo fluorescence. n=4.
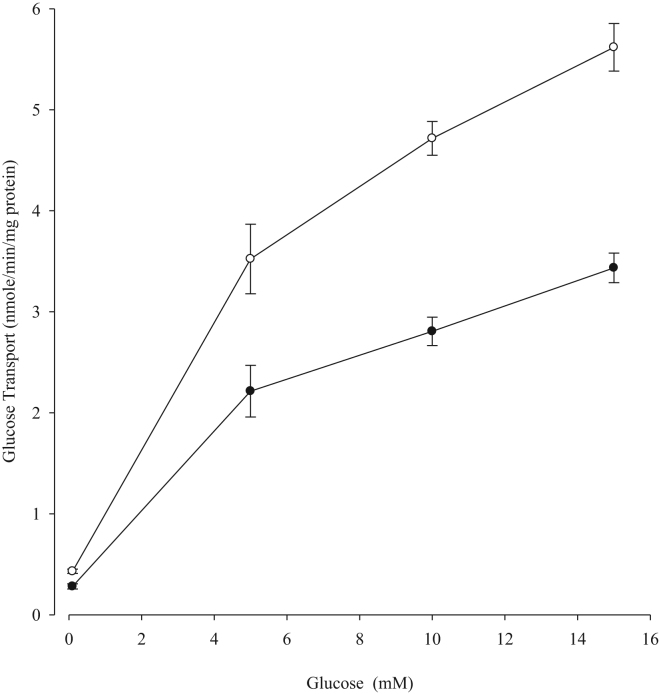
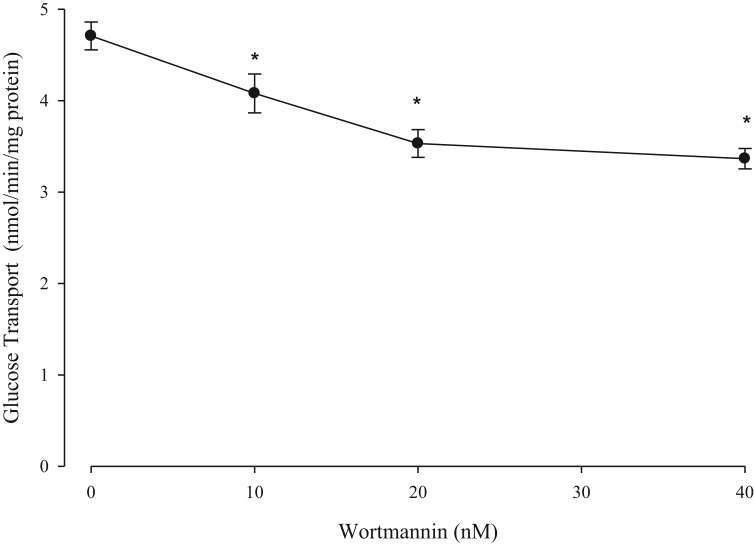
However, when L6 cells were treated with 10 mM caffeine (Fig. 2), glucose transport was partially inhibited over a wide range of glucose concentrations. While inhibition of glucose transport by caffeine is surprising, it is known that caffeine has other actions on cells, including an inhibition of phosphatidylinositol 3-kinase [26], which could explain this result. For confirmation, we examined the effect of wortmannin (a selective inhibitor of the PI3K [27]) on glucose transport. We found an inhibition similar to caffeine, occurring over a range of concentrations for which wortmannin is known to be selective for the PI3K (Fig. 3).
Fig. 2.
Caffeine inhibition of glucose transport. Glucose transport was measured over a range of glucose concentrations, in the absence (○) or presence (•) of 10 mM caffeine. *p<0.05 vs. corresponding glucose concentration with no caffeine present. n=3.
Fig. 3.
Wortmannin inhibition of glucose transport. Glucose transport was inhibited by nanomolar concentrations of wortmannin, the inhibitor of PI3 kinase. *p<0.05 vs. no wortmannin present. n=3.
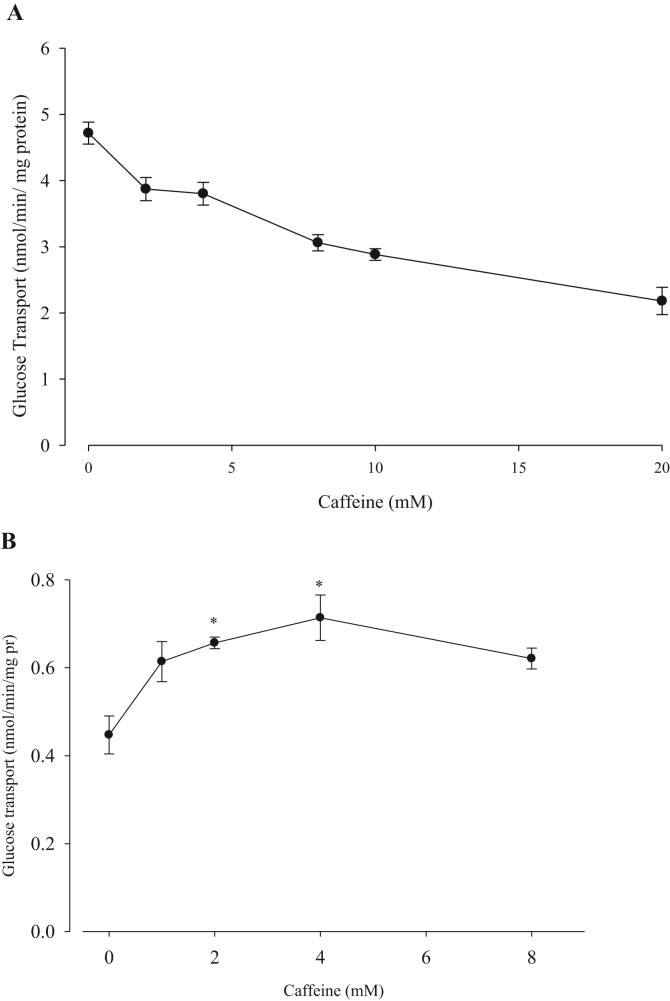
Some investigators have reported caffeine stimulation of glucose transport in muscle [6], [28], [29], [30]. All of those investigators used an indirect incubation method (“post-incubation”) for glucose transport. Specifically, a first incubation was performed with caffeine, after which the medium was replaced with a caffeine-free solution containing only HEPES buffer, and labeled glucose. We compared both methods over a range of concentrations of caffeine as shown in Fig. 4. While caffeine had a slightly inhibitory effect on glucose transport in our direct assay (Fig. 4A), using the two-step post-incubation method, caffeine showed a stimulation of glucose transport (Fig. 4B).
Fig. 4.
Caffeine titration of glucose transport. The effects of caffeine on glucose transport were measured over a wide range of caffeine concentrations by (A) direct glucose transport assay, and (B) post-incubation method. *p<0.05 vs. no caffeine present. n=3.
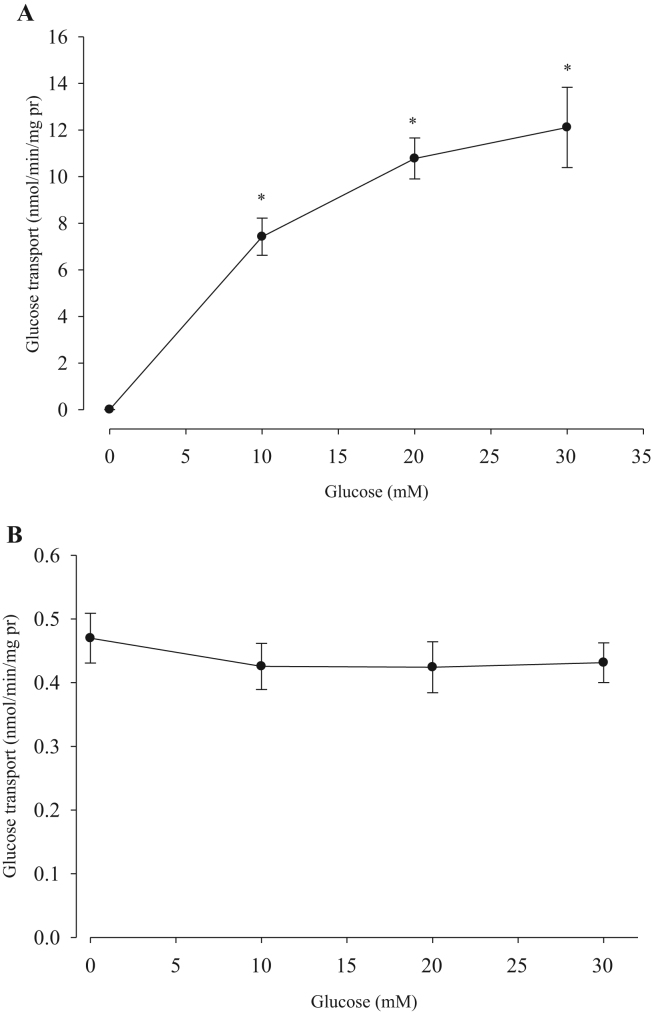
Because of the striking difference in transport rates between the two methods, we examined the fundamental dependence of glucose on this process for both. In the direct assay (Fig. 5A) the expected dependence on glucose was observed, along with the range of response to glucose in the millimolar range. However, in the post-incubation procedure, (Fig. 5B), the rates of glucose transport were very low and insensitive to glucose concentration in the initial incubation medium. The cells in in the post-incubation procedure are responding to the very low glucose concentration present in the second incubation.
Fig. 5.
Glucose dependence of Glucose transport. Glucose transport was measured over a range of medium glucose concentrations by (A) direct glucose transport assay, and (B) post-incubation method. For (B), the glucose concentrations were those present in the first incubation. *p<0.05 vs. no glucose present. n=3.
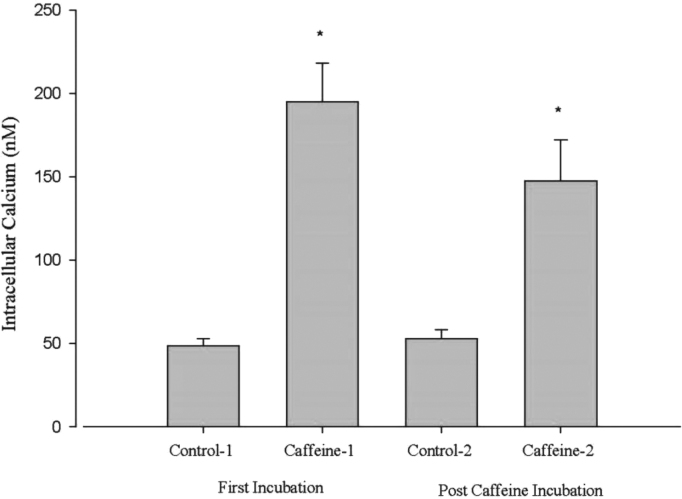
Measurement of cytosolic Ca2+ concentrations were conducted to further probe the role of this ion and its response to caffeine (Fig. 6). In this experiment, the presence of caffeine was compared to control in the first incubation. It is apparent that caffeine elicited a rise in cytosolic Ca2+. Next, the media of the caffeine-containing incubation was removed and replaced with fresh media for a “post-caffeine” incubation. It is apparent that Ca2+ was no longer elevated under these conditions (the Control-2 data of Fig. 6). Nonetheless, these cells could still respond to a subsequent addition of caffeine with an increase in Ca2+ (Caffeine-2 in Fig. 6). Thus, it is apparent that when caffeine-containing solutions are removed, the elevation of Ca2+ is lost.
Fig. 6.
Effect of caffeine on cytosolic calcium in post-incubation conditions. Cells were placed in the first incubation after which 10 mM Ca2+ was added. The cells, adhering to a plastic strip, were removed from their cuvette and placed in fresh media in a new cuvette, and the measurement and addition of caffeine repeated, for the second incubation. This is indicated by the second pair of bars labeled “Post Caffeine Incubation”. n=3.
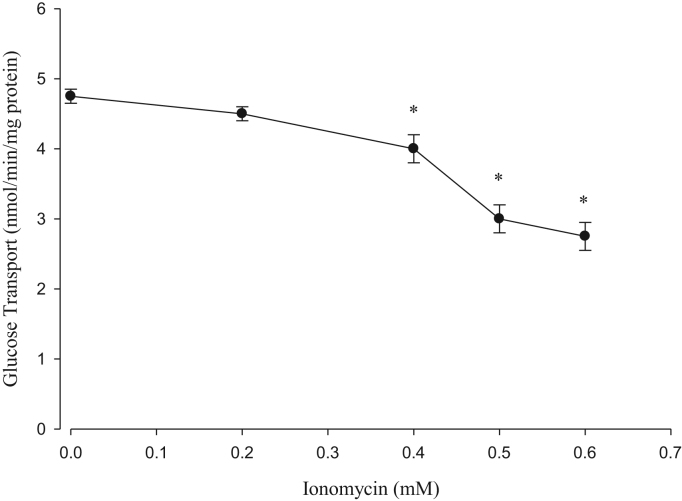
3.2. Effect of ionomycin on glucose transport
As an alternative method to increase intracellular [Ca2+], we used ionomycin, a selective Ca2+ ionophore which has also been proposed to stimulate muscle glucose transport [31]. Ionomycin produced quantitatively similar increases in cytosolic Ca2+ as maximal caffeine (data not shown). A titration curve showed no stimulation of glucose transport in the presence of ionomycin (Fig. 7), with a slight inhibition evident at higher concentrations.
Fig. 7.
Ionomycin effect on glucose transport. Glucose transport was measured in response to various concentrations of ionomycin, the calcium ionophore. *p<0.05 vs. no ionomycin present. n=3.
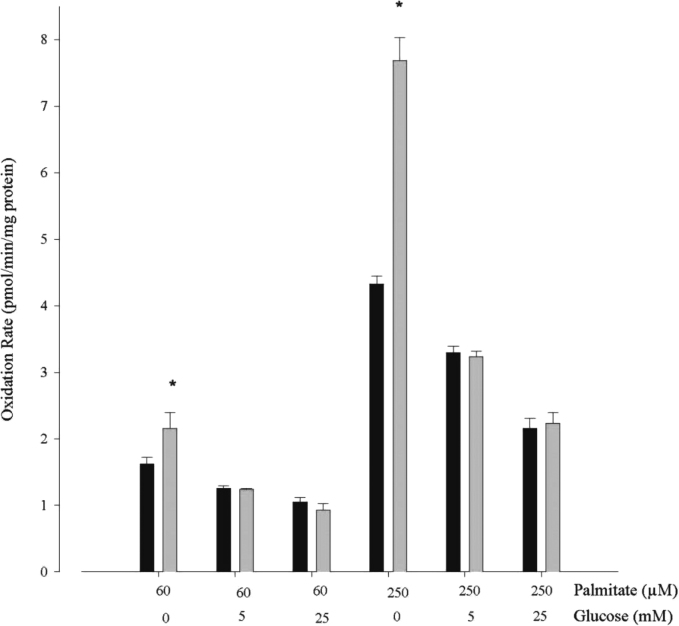
3.3. Effect of caffeine and ionomycin on fatty acid oxidation
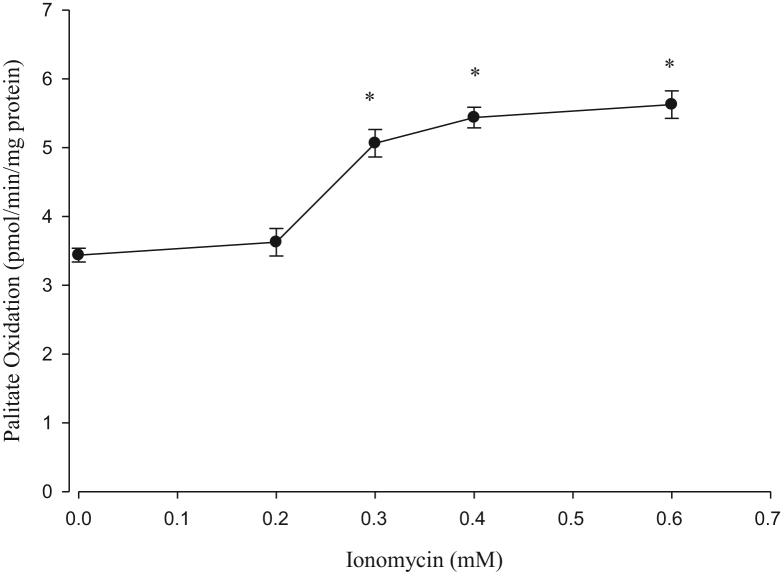
We examined the same Ca2+ releasing agents that we used for glucose transport for their influence on palmitate oxidation. Fig. 8 shows that caffeine stimulated fatty acid oxidation at low or high levels of palmitate, but only when glucose was omitted from the incubation medium. We also examined the effect of ionomycin on fatty acid oxidation. As shown in Fig. 9, ionomycin stimulated palmitate oxidation in a dose dependent manner, in experiments in which glucose was omitted from the incubation medium. As a control, incubation of cells with the acetoxy ester of the cytosolic chelator BAPTA (40 μM) prevented ionomycin induced stimulation of palmitate oxidation (data not shown). Thus, both caffeine and ionomycin caused stimulation of fatty acid oxidation, implying a Ca2+ stimulation of this pathway in the absence of glucose in muscle cell cultures.
Fig. 8.
Effects of caffeine and glucose on palmitate oxidation. Cells were incubated in the absence (black bars) or presence (gray bars) of 20 mM caffeine. Both palmitate and glucose concentrations were varied. With no added glucose, caffeine stimulated palmitate oxidation at 60 µM or 250 µM palmitate concentrations. *p<0.05 vs. corresponding control at a given palmitate concentration with no caffeine present. n=3.
Fig. 9.
Ionomycin stimulation of palmitate oxidation. Palmitate oxidation was measured in response to various concentrations of ionomycin. *p<0.05 vs. no ionomycin present. n=3.
3.4. Effects of glucose on fatty acid oxidation
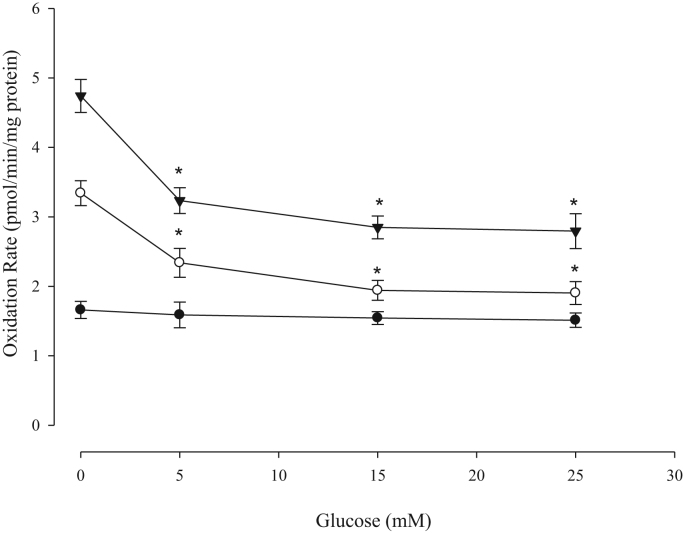
As the effect of Ca2+ on fatty acid oxidation required the absence of glucose, we sought to confirm glucose suppression of fatty acid oxidation [32] using the L6 cells. We varied both glucose and palmitate concentrations in the experiments shown in Fig. 10. The suppression by glucose was more pronounced at higher fatty acid concentrations, suggesting an uncompetitive type of inhibition of the process.
Fig. 10.
Effect of glucose on palmitate oxidation. Palmitate oxidation was measured at various concentrations of palmitate: 60 µM (•), 120 µM (○), and 250 µM (▼). *p<0.05 vs. no glucose present. n=3.
4. Discussion
Fig. 11 shows the pathways and control points discussed in the present study. Our most significant findings are the resolution of controversial findings implicating Ca2+ in the stimulation of glucose transport, and a new site for Ca2+ stimulation of fatty acid oxidation. In our study of the literature on glucose transport, we also found that various laboratories use one of two distinct methods for its measurement which can account for the fact that Ca2+ is reported to stimulate glucose transport by some laboratories, but not by others.
Fig. 11.
Glucose, fatty acids and calcium in skeletal muscle. The transport of glucose is shown to be affected by insulin, wortmannin, and caffeine, through the kinase akt (also known as protein kinase B). The latter is stimulated by phosphorylation through the activation of PI3K, stimulated by insulin, but inhibited by wortmannin and caffeine. Caffeine also stimulates Ca2+ release from the sarcoplasmic reticulum. An elevation of Ca2+ is also elicited by the selective ionophore ionomycin.Ca2+ has known stimulation points at glycogen phosphorylase, CaMKK, and α-Ketoglutarate dehydrogenase (αKGDH) which in turn activates the Krebs Cycle. The activation of AMPK by AMP and LKB1 is shared by CaMKK, although as indicated by the question mark, as the metabolic effects that would be exerted through AMPK on both glucose transport and fatty acid oxidation were not apparent in the present study. The connection between glucose and fatty acid metabolism is at malonyl-CoA, which inhibits the formation of the fatty acid-carnitine ester needed for transport and subsequent oxidation in the mitochondrion. The figure indicates inhibitory points as lines terminating in a perpendicular line; dotted arrows with plus signs indicate allosteric activation. Double lined arrows indicate transformations other than metabolic conversion, such as binding to elicit Ca2+ release or covalent activation through phosphorylation. Single arrows indicate metabolic transformation. The bidirectional arrows indicate near equilibrium reactions at lactate dehydrogenase and glucose phosphate isomerase. Also shown is the step catalyzing decarboxylation of the malonyl CoA back to acetyl CoA; this is the malonyl CoA carboxylase, abbreviated as MCD. Exogenous substrates (glucose and palmitate) are indicated in boxes.
Holloszy and coworkers were the first to show that caffeine stimulates glucose transport [2], [6], [28], [29], [30]. Kappel et al. [33] reported that the polyphenol rutin stimulates glucose transport by skeletal muscle and increases the import of cellular Ca2+. Yang et al. [34] showed that endothelin could stimulate glucose transport and Ca2+ levels in L6 cells. Ma et al. [35] showed that genipin, a natural product from Gardenia jasmonica, stimulates glucose transport in C2C12 cells in a Ca2+-dependent manner.
What all of the studies showing a Ca2+ stimulation of glucose transport have in common is an indirect “post-incubation” method. In this procedure, agents under investigation are added to cells during the first incubation, such as caffeine. Next, the cells are washed and the second incubation is conducted to measure glucose transport in a simple buffered saline medium. Yet, the elevation of Ca2+ is transient, and does not survive the second incubation as we demonstrate in this study. As pointed out by Jessen et al. [7], this makes it unlikely that Ca2+ has a direct action on glucose transport, as the contractile signal is very brief. We were able to reproduce the stimulation by caffeine (Fig. 3B) in the post-incubation protocol. That the Ca2+ signal is transient was confirmed by direct measurement of Ca2+ after a change of medium following caffeine administration: the Ca2+ returned to baseline, and the cells were capable of a further Ca2+ release upon a second exposure to caffeine (Fig. 6). As shown in Fig. 5, glucose transport in the post-incubation procedure is independent of the concentration of glucose in the first incubation. For this reason, the method is not an appropriate measure of this process and this technique should be avoided in future evaluation of agents affecting glucose transport. In its place a direct incubation should be used.
Caffeine inhibited glucose transport in our standard assay, an action replicated by nanomolar levels of wortmannin. This suggests the inhibition of glucose transport was likely the result of an inhibition of phosphatidyl inositol 3-kinase (PI3K). It is also indicated by studies of Riley et al. [36] in which PI3K was genetically ablated, and caffeine inhibition relieved [37]. Since PI3K is a part of the insulin pathway but not believed to be part of the contraction induced pathway [38], [39], [40], [41] this inhibition should not be evident. However, all of the studies separating insulin from contraction used a post-incubation procedure, as glucose transport could not be measured during the contraction phase. Even including compounds in the second incubation does not provide a valid measurement because the event itself occurs in the prior incubation, and because the rate of transport is severely limited by the low (and different) glucose concentration present in the second incubation. It must be admitted that the amount of wortmannin inhibition we have observed is modest, so that it is likely that the PI3K contribution to basal glucose transport is modest.
We also examined the effect of the Ca2+ ionophore ionomycin on the glucose transport. Ionomycin did not show a stimulation of glucose transport over a variety of concentrations. By contrast, ionomycin stimulated fatty acid oxidation over the same titration range (Fig. 9). This suggests that ionomycin can functionally increase Ca2+ in cells. The slight inhibition of glucose transport observed may be due to the broad nature of the ionophore, enabling Ca2+ release to all cellular spaces. Thus, even with this distinct Ca2+ secretagogue, we found no evidence for a direct action of Ca2+ on glucose transport.
A possible explanation for the observation of an apparent Ca2+ stimulation of glucose transport in the post-incubation method is Ca2+ activation of glycogen phosphorylase in the first incubation that enhances glucose transport in the second. Shulman and colleagues [42], [43] investigated the relationship between glycogen content, glycogen synthesis, and glucose transport in muscle in vivo. They found that lowered glycogen content corresponds to an enhanced glucose transport. Several studies have shown an inverse relationship between glycogen accumulation and glucose transport in muscle [44], [45], [46], [47]. It is well established that glycogen phosphorylase is simulated by Ca2+ in muscle [48]. Jessen and Goodyear [7] raised the possibility that a brief change in Ca2+ could lead to a more stable one if Ca2+ activated CaMKK and subsequently AMPK. While this could be used to explain the post-incubation data, an increased glucose transport should also have been apparent in the direct assay.
A common measurement in the study of glucose transport in muscle is GLUT4 translocation between a plasma membrane location and an intracellular vesicle. It is well known that insulin stimulates this translocation, and it has been suggested that Ca2+ is a requirement for this action [49]. More recently, it has been observed that GLUT4 protein translocation is increased in the presence of ionomycin in L6 cells [9]. However, translocation of GLUT4 is not the equivalent of glucose transport. In the present study, we have shown the process of glucose transport itself was not stimulated by either ionomycin or caffeine, despite their ability to raise cytosolic Ca2+. In accordance with this, a recent study of cardiomyocytes, another striated muscle cell model that employs GLUT4, also showed that calcium stimulates GLUT4 translocation [10], but glucose transport was unaffected under the same conditions. These investigators used a direct method for glucose transport. They speculated that an increase in the GLUT4 translocation without an increase in the pathway for transport may mean that calcium, while not stimulating the glucose transport step, plays a permissive role in the stimulation by other agents such as AMPK and insulin. It is possibly that this may also be the case for skeletal muscle.
Both caffeine and ionomycin can increase cytosolic Ca2+ as well as mitochondrial Ca2+. The caffeine induced rise in mitochondria is likely due to a primary increase in the cytosol, followed by transport of Ca2+ into the mitochondria [50]. We found that these agents stimulated fatty acid oxidation (Fig. 6, Fig. 7) so long as glucose was omitted from the incubation medium. Physiologically, cells do not experience a lack of glucose in the extracellular space. The exaggerated effect in the cell experiments may reflect a situation that does occur when malonyl CoA inhibition of the transport process for fatty acid oxidation [32] is removed. Malonyl CoA regulates the transport step of fatty acid oxidation, and is derived from glucose. Experimentally, omitting glucose from the incubation medium of the cells removes that inhibitor. Under these conditions, Ca2+ stimulates fatty acid oxidation, implicating sites of action distal to transport – that is, mitochondrial enzymes, such as 2-ketoglutarate dehydrogenase, a well-established site of Ca2+ stimulation in the mitochondria [51]. Rather than a depletion of extracellular glucose, situations in which malonyl CoA production is depressed, such as an increase in the AMPK activity, may then uncover a further site of Ca2+ regulation within the mitochondria.
We examined the kinetics of glucose suppression of fatty acid oxidation (Fig. 10). Glucose produces malonyl CoA that inhibits carnitine acyl transferase I (CAT I), the enzyme responsible for formation of the carnitine ester prior to import into the mitochondria [52], [53], [54]. Thus, the result can be interpreted as malonyl CoA inhibition of CAT I in intact cells. A similar approach, using intact cells to evaluate specific enzyme inhibition sites was earlier used by Rognstad [55] and us [56]. The inhibition pattern of Fig. 10 suggests malonyl CoA is a mostly uncompetitive inhibitor, with greater effects at high substrate concentrations (see [57]). While data on muscle CPT I is currently uncertain [58] studies of the liver CPT I in isolated mitochondria indicate a noncompetitive inhibition by malonyl CoA [59]. It is also possible that the inhibition might vary between mixed and competitive inhibition in vitro, the result of CAT I phosphorylation [60].
The relationship between the two muscle contraction signals AMPK and Ca2+ was explored by several investigators. As discussed above in reference to glucose transport, a brief rise in Ca2+ could activate CaMKK and then AMPK. It cannot explain the action of fatty acid oxidation either, since AMPK action requires lowering of malonyl CoA, and the latter accumulation depends on glucose. As we demonstrate, Ca2+ stimulation of fatty acid oxidation occurs in the absence of glucose. The findings of Abbott [11] that STO-609 (a CaMKK blocker) inhibits fatty acid oxidation could be considered evidence in favor of a role for CaMKK. However, our findings are at odds with this interpretation. In the data of Fig. 8, we varied both the concentration of palmitate and the concentration of glucose to determine the effects of caffeine addition on fatty acid oxidation. Glucose suppressed fatty acid oxidation at both 5 and 25 mM, and the latter suppression was clearly greater when a saturating (250 μM) concentration of palmitate was present. The inability of caffeine to stimulate fatty acid oxidation in the presence of glucose suggests that Ca2+ does not act through the CaMKK and subsequent AMPK activation, since that would require glucose to form malonyl CoA that would be lowered by AMPK. The inhibitory effects of STO-609, which implicates CaMKK, are complicated by the known direct inhibition of AMPK by STO-609 [13]. It may also be the case that assay conditions strongly influence the results, as indicated in the present report. As shown by Watt et al. [61] direct elevation of cytosolic Ca2+ using cyclopiazonic acid did not stimulate fatty acid oxidation in soleus muscle. It should also be noted that the same investigators who found no effect of Ca2+ on glucose transport in cardiomyocytes also found no effect on the transport of fatty acids, although the oxidation of fatty acids was not determined in that study [10].
Use of agents that indirectly raise cytosolic Ca2+ clearly also introduce their own complications, as is evident from the use of caffeine and ionomycin. However, the conclusions against a role of Ca2+ for fatty acid oxidation based on a lack of effect with cyclopiazonic acid [62] must be tempered by the fact that this compound has very modest effects on Ca2+ when directly measured, and effects on lipid synthesis may relate to changes in ATP utilization upon inhibition of CaATPase [63]. Thus, each means of manipulating Ca2+ concentration in the cytosol may produce a unique side effect.
We conclude that regulation of long chain fatty acids thus involves at least two key intracellular sites: the transport limitation by malonyl CoA, contributed by the prevailing glucose level and the activity of its formation enzyme acetyl CoA carboxylase (inhibited by AMPK), and the subsequent mitochondrial oxidation that is stimulated by Ca2+.
Footnotes
Transparency document associated with this article can be found in the online version at doi:10.1016/j.bbrep.2016.01.007.
Contributor Information
Darrick Balu, Email: dbalu@mclean.harvard.edu.
Jiangyong Ouyang, Email: oyjiangyong@gmail.com.
Rahulkumar A. Parakhia, Email: rahulparakhia@yahoo.co.in.
Saumitra Pitake, Email: saumitra_14@yahoo.com.
Raymond S. Ochs, Email: ochsr@stjohns.edu.
Appendix A. Transparency document
Transparency document
References
- 1.Smith A.C., Bruce C.R., Dyck D.J. AMP kinase activation with AICAR further increases fatty acid oxidation and blunts triacylglycerol hydrolysis in contracting rat soleus muscle. J. Physiol. Lond. 2005;565:547–553. doi: 10.1113/jphysiol.2004.081687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wright D.C., Hucker K.A., Holloszy J.O., Han D.H. Ca2+ and AMPK both mediate stimulation of glucose transport by muscle contractions. Diabetes. 2004;53:330–335. doi: 10.2337/diabetes.53.2.330. [DOI] [PubMed] [Google Scholar]
- 3.Minokoshi Y., Kahn B.B. Role of AMP-activated protein kinase in leptin-induced fatty acid oxidation in muscle. Biochem. Soc. Trans. 2003;31:196–201. doi: 10.1042/bst0310196. [DOI] [PubMed] [Google Scholar]
- 4.Ouyang J., Parakhia R.A., Ochs R.S. Metformin activates AMP kinase through inhibition of AMP deaminase. J. Biol. Chem. 2011;286:1–11. doi: 10.1074/jbc.M110.121806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steinberg G.R. Role of the AMP-activated protein kinase in regulating fatty acid metabolism during exercise. Report. Appl. Physiol., Nutr., Metab. 2009;34:315. doi: 10.1139/H09-009. (318) [DOI] [PubMed] [Google Scholar]
- 6.Henriksen E.J., Rodnick K.J., Holloszy J.O. Activation of glucose transport in skeletal muscle by phospholipase C and phorbol ester. Evaluation of the regulatory roles of protein kinase C and calcium. J. Biol. Chem. 1989;264:21536–21543. [PubMed] [Google Scholar]
- 7.Jessen N., Goodyear L.J. Contraction signaling to glucose transport in skeletal muscle. J. Appl. Physiol. 2005;99:330–337. doi: 10.1152/japplphysiol.00175.2005. [DOI] [PubMed] [Google Scholar]
- 8.Park S., Scheffler T.L., Gunawan A.M., Shi H., Zeng C., Hannon K.M., Grant A.L., Gerrard D.E. Chronic elevated calcium blocks AMPK-induced GLUT-4 expression in skeletal muscle. Am. J. Physiol. Cell Physiol. 2009;296:C106–C115. doi: 10.1152/ajpcell.00114.2008. [DOI] [PubMed] [Google Scholar]
- 9.Li Q., Zhu X., Ishikura S., Zhang D., Gao J., Sun Y., Contreras-Ferrat A., Foley K.P., Lavandero S., Yao Z., Bilan P.J., Klip A., Niu W. Ca(2)(+) signals promote GLUT4 exocytosis and reduce its endocytosis in muscle cells. Am. J. Physiol. Endocrinol. Metab. 2014;307:E209–E224. doi: 10.1152/ajpendo.00045.2014. [DOI] [PubMed] [Google Scholar]
- 10.Angin Y., Schwenk R.W., Nergiz-Unal R., Hoebers N., Heemskerk J.W., Kuijpers M.J., Coumans W.A., van Zandvoort M.A., Bonen A., Neumann D., Glatz J.F., Luiken J.J. Calcium signaling recruits substrate transporters GLUT4 and CD36 to the sarcolemma without increasing cardiac substrate uptake. Am. J. Physiol. Endocrinol. Metab. 2014;307:E225–E236. doi: 10.1152/ajpendo.00655.2013. [DOI] [PubMed] [Google Scholar]
- 11.Abbott M.J., Edelman A.M., Turcotte L.P. CaMKK is an upstream signal of AMP-activated protein kinase in regulation of substrate metabolism in contracting skeletal muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009;297:R1724–R1732. doi: 10.1152/ajpregu.00179.2009. [DOI] [PubMed] [Google Scholar]
- 12.Osler M.E., Zierath J.R. Adenosine 5′-monophosphate-activated protein kinase regulation of fatty acid oxidation in skeletal muscle. Endocrinology. 2008;149:935–941. doi: 10.1210/en.2007-1441. [DOI] [PubMed] [Google Scholar]
- 13.Hurley R.L., Anderson K.A., Franzone J.M., Kemp B.E., Means A.R., Witters L.A. The Ca2+/calmodulin-dependent protein kinase kinases are AMP-activated protein kinase kinases. J. Biol. Chem. 2005;280:29060–29066. doi: 10.1074/jbc.M503824200. [DOI] [PubMed] [Google Scholar]
- 14.Keun H.C., Athersuch T.J. Application of metabonomics in drug development. Pharmacogenomics. 2007;8:731–741. doi: 10.2217/14622416.8.7.731. [DOI] [PubMed] [Google Scholar]
- 15.Wingertzahn M.A., Ochs R.S. Changes in ryanodine receptor-mediated calcium release during skeletal muscle differentiation. Proc. Soc. Exp. Biol. Med. 1999;221:234–241. doi: 10.1046/j.1525-1373.1999.d01-81.x. [DOI] [PubMed] [Google Scholar]
- 16.Hardy R.W., Ladenson J.H., Hendrickson F.J., Holloszy J.O. Palmitate stimulates glucose transport in rat adipocytes by a mechanism involving translocation of the insulin sensitive glucose transporter. Biochem. Biophys. Res. Commun. 1991;177:343–349. doi: 10.1016/0006-291x(91)91989-p. [DOI] [PubMed] [Google Scholar]
- 17.Klip A., Li G., Logan W.J. Induction of sugar uptake response to insulin by serum depletion in fusing L6 myoblasts. AJP – Regul., Integr. Comp. Physiol. 1984;247:E291–E296. doi: 10.1152/ajpendo.1984.247.3.E291. [DOI] [PubMed] [Google Scholar]
- 18.Saddik M., Lopaschuk G.D. Myocardial triglyceride turnover and contribution to energy substrate utilization in isolated working rat hearts. J. Biol. Chem. 1991;266:8162–8170. [PubMed] [Google Scholar]
- 19.Smith P.K., Krohn R.I., Hermanson G.T., Mallia A.K., Gartner F.H., Provenzano M.D., Fujimoto E.K., Gopeke N.M., Olson B.J., Klenk D.C. Measurement of protein using bicinchoninic acid. Anal. Biochem. 1985;150:76–85. doi: 10.1016/0003-2697(85)90442-7. [DOI] [PubMed] [Google Scholar]
- 20.Narayanan B., Islam M.N., Bartelt D., Ochs R.S. A direct mass-action mechanism explains capacitative calcium entry in jurkat and skeletal L6 muscle cells. J. Biol. Chem. 2003 doi: 10.1074/jbc.M306538200. [DOI] [PubMed] [Google Scholar]
- 21.Grynkiewicz G., Poenie M., Tsien R.Y. A new generation of Ca2+ indicators with greatly improved fluorescence properties. J. Biol. Chem. 1985;260:3440–3450. [PubMed] [Google Scholar]
- 22.Narayanan B., Islam M.N., Bartlelt D., Ochs R.S. A direct mass-action mechanism explains capacitative calcium entry in jurkat and skeletal L6 muscle cells. J. Biol. Chem. 2003 doi: 10.1074/jbc.M306538200. [DOI] [PubMed] [Google Scholar]
- 23.Stephenson D.G. Caffeine – a valuable tool in excitation–contraction coupling research. J. Physiol. 2008;586:695–696. doi: 10.1113/jphysiol.2007.148270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam M.N., Narayanan B., Ochs R.S. A mechanism for both capacitative Ca2+ entry and excitation–contraction coupled Ca2+ release by the sarcoplasmic reticulum of skeletal muscle cells. Exp. Biol. Med. (Maywood) 2002;227(6):425–431. doi: 10.1177/153537020222700608. [DOI] [PubMed] [Google Scholar]
- 25.Wingertzahn M.A., Ochs R.S. Changes in ryanodine receptor-mediated calcium release during skeletal muscle differentiation. II Resolution of caffeine-ryanodine paradox. Exp. Biol. Med. 2001;226(2):119–126. doi: 10.1177/153537020122600209. [DOI] [PubMed] [Google Scholar]
- 26.Foukas L.C., Daniele N., Ktori C., Anderson K.E., Jensen J., Shepherd P.R. Direct effects of caffeine and theophylline on p110 delta and other phosphoinositide 3-kinases. Differential effects on lipid kinase and protein kinase activities. J. Biol. Chem. 2002;277:37124–37130. doi: 10.1074/jbc.M202101200. [DOI] [PubMed] [Google Scholar]
- 27.Vanhaesebroeck B., Leevers S.J., Ahmadi K., Timms J., Katso R., Driscoll P.C., Woscholski R., Parker P.J., Waterfield M.D. Synthesis and function of 3-phosphorylated inositol lipids. Annu. Rev. Biochem. 2001;70:535–602. doi: 10.1146/annurev.biochem.70.1.535. [DOI] [PubMed] [Google Scholar]
- 28.Holloszy J.O., Narahara H.T. Enhanced permeability to sugar associated with muscle contraction. Studies of the role of Ca2+ J. Gen. Physiol. 1967;50:551–562. doi: 10.1085/jgp.50.3.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wright D.C., Geiger P.C., Holloszy J.O., Han D.H. Contraction- and hypoxia-stimulated glucose transport is mediated by a Ca2+-dependent mechanism in slow-twitch rat soleus muscle. AJP – Endocrinol. Metab. 2005;288:E1062–E1066. doi: 10.1152/ajpendo.00561.2004. [DOI] [PubMed] [Google Scholar]
- 30.Youn J.H., Gulve E.A., Holloszy J.O. Calcium stimulates glucose transport in skeletal muscle by a pathway independent of contraction. Am. J. Physiol. 1991;260:C555–C561. doi: 10.1152/ajpcell.1991.260.3.C555. [DOI] [PubMed] [Google Scholar]
- 31.Lee A.D., Gulve E.A., Chen M., Schluter J., Holloszy J.O. Effects of Ca2+ ionophore ionomycin on insulin-stimulated and basal glucose transport in muscle. Am. J. Physiol. 1995 doi: 10.1152/ajpregu.1995.268.4.R997. (R997-1002) [DOI] [PubMed] [Google Scholar]
- 32.Saha A.K., Vavvas D., Kurowski T.G., Apazidis A., Witters L.A., Shafrir E., Ruderman N.B. Malonyl-CoA regulation in skeletal muscle: its link to cell citrate and the glucose-fatty acid cycle. AJP – Regul. Integr. Comp. Physiol. 1997;272:E641–E648. doi: 10.1152/ajpendo.1997.272.4.E641. [DOI] [PubMed] [Google Scholar]
- 33.Kappel V.D., Zanatta L., Postal B.G., Silva F.R.M.B. Rutin potentiates calcium uptake via voltage-dependent calcium channel associated with stimulation of glucose uptake in skeletal muscle. Arch. Biochem. Biophys. 2013;532:55–60. doi: 10.1016/j.abb.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 34.Yang X.Y., Fekete Z., Gardner J., Benevenia J., Aviv A. Endothelin mobilizes calcium and enhances glucose uptake in cultured human skeletal myoblasts and L6 myotubes. Hypertension. 1994;23:1075–1081. doi: 10.1161/01.hyp.23.6.1075. [DOI] [PubMed] [Google Scholar]
- 35.Ma C.J., Nie A.F., Zhang Z.J., Zhang Z.G., Du L., Li X.Y., Ning G. Genipin stimulates glucose transport in C2C12 myotubes via an IRS-1 and calcium-dependent mechanism. J. Endocrinol. 2013;216:353–362. doi: 10.1530/JOE-11-0473. [DOI] [PubMed] [Google Scholar]
- 36.Riley J.K., Carayannopoulos M.O., Wyman A.H., Chi M., Moley K.H. Phosphatidylinositol 3-kinase activity is critical for glucose metabolism and embryo survival in murine blastocysts. J. Biol. Chem. 2006;281:6010–6019. doi: 10.1074/jbc.M506982200. [DOI] [PubMed] [Google Scholar]
- 37.Harmon A.W., Patel Y.M. Naringenin inhibits phosphoinositide 3-kinase activity and glucose uptake in 3T3-L1 adipocytes. Biochem. Biophys. Res. Commun. 2003;305:229–234. doi: 10.1016/s0006-291x(03)00720-4. [DOI] [PubMed] [Google Scholar]
- 38.Lund S., Holman G.D., Schmitz O., Pedersen O. Contraction stimulates translocation of glucose transporter GLUT4 in skeletal muscle through a mechanism distinct from that of insulin. Proc. Natl. Acad. Sci. 1995;92:5817–5821. doi: 10.1073/pnas.92.13.5817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yeh J.I., Gulve E.A., Rameh L., Birnbaum M.J. The effects of wortmannin on rat skeletal muscle. Dissociation of signaling pathways for insulin- and contraction-activated hexose transport. J. Biol. Chem. 1995;270:2107–2111. doi: 10.1074/jbc.270.5.2107. [DOI] [PubMed] [Google Scholar]
- 40.Lee A.D., Hansen P.A., Holloszy J.O. Wortmannin inhibits insulin-stimulated but not contraction-stimulated glucose transport activity in skeletal muscle. FEBS Lett. 1995;361:51–54. doi: 10.1016/0014-5793(95)00147-2. [DOI] [PubMed] [Google Scholar]
- 41.Hayashi T., Hirshman M.F., Kurth E.J., Winder W.W., Goodyear L.J. Evidence for 5′ AMP-activated protein kinase mediation of the effect of muscle contraction on glucose transport [in process citation] Diabetes. 1998;47:1369–1373. doi: 10.2337/diab.47.8.1369. [DOI] [PubMed] [Google Scholar]
- 42.Jue T., Rothman D.L., Shulman G.I., Tavitian B.A., DeFronzo R.A., Shulman R.G. Direct observation of glycogen synthesis in human muscle with 13C NMR. Proc. Natl. Acad. Sci. 1989;86:4489–4491. doi: 10.1073/pnas.86.12.4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Price T.B., Laurent D., Petersen K.F., Rothman D.L., Shulman G.I. Glycogen loading alters muscle glycogen resynthesis after exercise. J. Appl. Physiol. 2000;88:698–704. doi: 10.1152/jappl.2000.88.2.698. [DOI] [PubMed] [Google Scholar]
- 44.Fisher J.S., Nolte L.A., Kawanaka K., Han D.H., Jones T.E., Holloszy J.O. Glucose transport rate and glycogen synthase activity both limit skeletal muscle glycogen accumulation. Am. J. Physiol. Endocrinol. Metab. 2002;282:E1214–E1221. doi: 10.1152/ajpendo.00254.2001. [DOI] [PubMed] [Google Scholar]
- 45.Iozzo P., Pratipanawatr T., Pijl H., Vogt C., Kumar V., Pipek R., Matsuda M., Mandarino L.J., Cusi K.J., DeFronzo R.A. Physiological hyperinsulinemia impairs insulin-stimulated glycogen synthase activity and glycogen synthesis. Am. J. Physiol. Endocrinol. Metab. 2001;280:E712–E719. doi: 10.1152/ajpendo.2001.280.5.E712. [DOI] [PubMed] [Google Scholar]
- 46.Laurent D., Hundal R.S., Dresner A., Price T.B., Vogel S.M., Petersen K.F., Shulman G.I. Mechanism of muscle glycogen autoregulation in humans. Am. J. Physiol. Endocrinol. Metab. 2000;278:E663–E668. doi: 10.1152/ajpendo.2000.278.4.E663. [DOI] [PubMed] [Google Scholar]
- 47.Derave W., Lund S., Holman G.D., Wojtaszewski J., Pedersen O., Richter E.A. Contraction-stimulated muscle glucose transport and GLUT-4 surface content are dependent on glycogen content. Am. J. Physiol. Endocrinol. Metab. 1999;277:E1103–E1110. doi: 10.1152/ajpendo.1999.277.6.E1103. [DOI] [PubMed] [Google Scholar]
- 48.Meinke M.H., Edstrom R.D. Muscle glycogenolysis. Regulation of the cyclic interconversion of phosphorylase a and phosphorylase B. J. Biol. Chem. 1991;266:2259–2266. [PubMed] [Google Scholar]
- 49.Li Y., Wang P., Xu J., Gorelick F., Yamazaki H., Andrews N., Desir G.V. Regulation of insulin secretion and GLUT4 trafficking by the calcium sensor synaptotagmin VII. Biochem. Biophys. Res. Commun. 2007;362:658–664. doi: 10.1016/j.bbrc.2007.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hansford R.G. Relation between mitochondrial calcium transport and control of energy metabolism. Rev. Physiol. Biochem. Pharmacol. 1985;102:1–72. doi: 10.1007/BFb0034084. [DOI] [PubMed] [Google Scholar]
- 51.Ochs R.S. Glutamine metabolism of isolated rat hepatocytes. Evidence for catecholamine activation of alpha-ketoglutarate dehydrogenase. J. Biol. Chem. 1984;259:13004–13010. [PubMed] [Google Scholar]
- 52.McGarry J.D., Foster D.W. In support of the roles of malonyl-CoA and carnitine acyltransferase I in the regulation of hepatic fatty acid oxidation and ketogenesis. J. Biol. Chem. 1979;254:8163–8168. [PubMed] [Google Scholar]
- 53.Mills S.E., Foster D.W., McGarry J.D. Interaction of malonyl-CoA and related compounds with mitochondria from different rat tissues. Relationship between ligand binding and inhibition of carnitine palmitoyltransferase I. Biochem. J. 1983;214:83–91. doi: 10.1042/bj2140083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saha A.K., Kurowski T.G., Colca J.R., Ruderman N.B. A malonyl CoA fuel-sensing mechanism in muscle-effects of insulin, glucose and denervation. Am. J. Physiol. Endocrinol. Metab. 1995:E282–E289. doi: 10.1152/ajpendo.1995.269.2.E283. [DOI] [PubMed] [Google Scholar]
- 55.Rognstad R. Rate-limiting steps in metabolic pathways. J. Biol. Chem. 1979;254:1875–1878. [PubMed] [Google Scholar]
- 56.Ochs R.S., Lardy H.A. Catecholamine stimulation of hepatic gluconeogenesis at the site between pyruvate and phosphoenolpyruvate. J. Biol. Chem. 1983;258:9956–9962. [PubMed] [Google Scholar]
- 57.Ochs R.S. Understanding enzyme Inhibition. J. Chem. Educ. 2000;77:1453–1456. [Google Scholar]
- 58.Alam N., Saggerson E.D. Malonyl-CoA and the regulation of fatty acid oxidation in soleus muscle. Biochem. J. 1998;334:233–241. doi: 10.1042/bj3340233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fraser F., Padovese R., Zammit V.A. Distinct kinetics of carnitine palmitoyltransferase I in contact sites and outer membranes of rat liver mitochondria. J. Biol. Chem. 2001;276:20182–20185. doi: 10.1074/jbc.M101078200. [DOI] [PubMed] [Google Scholar]
- 60.Kerner J., Distler A.M., Minkler P., Parland W., Peterman S.M., Hoppel C.L. Phosphorylation of rat liver mitochondrial carnitine palmitoyltransferase-I: effect on the kinetic properties of the enzyme. J. Biol. Chem. 2004;279:41104–41113. doi: 10.1074/jbc.M406570200. [DOI] [PubMed] [Google Scholar]
- 61.Watt M.J., Steinberg G.R., Heigenhauser G.J.F., Spriet L.L., Dyck D.J. Hormone-sensitive lipase activity and triacylglycerol hydrolysis are decreased in rat soleus muscle by cyclopiazonic acid. Am. J. Physiol. – Endocrinol. Metab. 2003;285:E412–E419. doi: 10.1152/ajpendo.00023.2003. [DOI] [PubMed] [Google Scholar]
- 62.Watt M.J., Steinberg G.R., Chen Z.P., Kemp B.E., Febbraio M.A. Fatty acids stimulate AMP-activated protein kinase and enhance fatty acid oxidation in L6 myotubes. J. Physiol. Lond. 2006;574:139–147. doi: 10.1113/jphysiol.2006.107318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jensen T.E., Sylow L., Rose A.J., Madsen A.B., Angin Y., Maarbjerg S.J., Richter E.A. Contraction-stimulated glucose transport in muscle is controlled by AMPK and mechanical stress but not sarcoplasmatic reticulum Ca(2+) release. Mol. Metab. 2014;3:742–753. doi: 10.1016/j.molmet.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document