Abstract
OBJECTIVE
To assess the contraception and fertility counseling provided to women with solid organ transplants.
METHODS
A telephone survey of 309 women aged 19–49 years who had received a solid organ transplant at the University of Nebraska Medical Center was performed. Of the 309 eligible women, 183 responded. Patients were asked 19 questions regarding pretransplant and posttransplant fertility awareness and contraception counseling. Data were summarized using descriptive statistics.
RESULTS
Patients had undergone a variety of solid organ transplantations: 40% kidney (n=73); 32% liver (n=59); 6% pancreas (n=11); 5% heart (n=9); 3% intestine (n=5); and 14% multiple organs (n=26). Before their transplantations, 79 women (44%) reported they were not aware that a woman could become pregnant after transplantation. Only 66 women aged 13 and older at the time of transplantation reported that a health care provider discussed contraception before transplantation. Approximately half of women surveyed were using a method of contraception. Oral contraceptive pills were the most commonly recommended method. Twenty-two of the 31 pregnancies after organ transplantation were planned, which is higher than that of the general population.
CONCLUSION
Few women with transplants are educated regarding the effect of organ transplantation on fertility and are not routinely counseled about contraception or the potential for posttransplant pregnancy. Health care providers should incorporate contraceptive and fertility counseling as part of routine care for women with solid organ transplants.
From January 2000 to October 2012, there have been 139,247 women who have undergone solid organ transplantation in the United States, according to the Organ Procurement and Transplantation Network.1 Of these women, 60,154 (43%) were between the ages of 18 and 49 years. The most commonly transplanted organs in women of reproductive age are kidneys (61%) and livers (13%).1 Organ transplantation has significantly improved the quality of life for women and is usually associated with a return of fertility.2,3 There is a consensus among both transplant providers and gynecologists that women should wait at least 12–24 months after their transplantation before trying to become pregnant, which allows for stabilization of the allograft function, lower maintenance doses of immuno-suppressive agents, decreased risk of rejection, and optimization of other medical conditions.2–5 Unfortunately, the literature regarding contraception use in female transplant recipients is scant and little is known about whether these women receive counseling about their fertility after transplantation. The rate of unplanned pregnancy in women with transplants has been reported as high as 93%.6 Pregnancy poses several risks to women posttransplantation, specific to the organ transplanted. According to the National Transplantation Pregnancy Registry, pregnant women with a kidney transplant are at increased risk for intrauterine growth restriction, preterm labor, preterm premature rupture of membranes, and preeclampsia.7 Pregnant women with a liver transplant are at increased risk for preeclampsia, hypertension, and graft rejection.7 With the return of fertility after transplantation and the recommendation to postpone pregnancy, sexually active women who have received an organ transplant are in need of effective contraception. We surveyed women with solid organ transplants to assess patient awareness regarding posttransplantation fertility and to determine what contraceptive methods, if any, were recommended to them after transplantation.
MATERIALS AND METHODS
We conducted a telephone survey with the assistance of the Department of Health Services Research and Administration with the College of Public Health. The Institutional Review Board at the Nebraska Medical Center approved this study. Women aged 19–49 years at the time of the study who had ever undergone solid organ transplantation (including kidney, liver, pancreas, intestine, heart, or any combination) at the University of Nebraska Medical Center were eligible to participate. We chose this age group as a convenient sample because the Organ Procurement and Transplantation Network maintains data by the age groups of 18–34 years and 35–49 years, and the age of consent in the state of Nebraska is 19 years. We identified patients using the Organ Transplant Tracking Record database maintained at this institution. Women were excluded if they were currently hospitalized or deceased.
All individuals conducting the telephone survey completed a training session before the initiation of the survey to become familiar with the study. Prospective patients received a mailed notification letter 1–2 weeks before being contacted for the telephone survey. Patients were contacted by telephone a maximum of two times to participate in the survey. Interviewers obtained informed consent before administering the questionnaire. Surveys were voluntary and conducted in English and Spanish. The survey consisted of 19 multiple choice questions and inquired about many aspects of reproductive health, including the woman’s pretransplant awareness of her potential posttransplant fertility, her awareness of the need for posttransplant contraception, current method of contraception, current sexual activity, and outcomes of any posttransplant pregnancies. Data summarization was performed using SAS 9.3. Summarizations included descriptive reports of simple frequencies and percentages.
RESULTS
For this study, 309 women met inclusion criteria and 183 women responded to the survey. Patients interviewed had undergone a variety of solid organ transplantations (Table 1). The most common procedure was kidney transplantation. Our study population had more women with small bowel transplants compared with the national data, because our institution has an active small bowel transplantation program. For women who had undergone more than one transplantation surgery, the most recent procedure was recorded. The average age at transplantation was 29 years (range 5 months–49 years) and the average time from transplantation to participation in this survey was 10 years (range 1 month–26 years).
Table 1.
Organs Transplanted in Survey Population Compared With National Data From the Organ Procurement and Transplantation Database*
| Organ Transplanted | Nebraska Medical Center† | Organ Procurement and Transplantation Network† |
|---|---|---|
| Bowel | 5 (3) | 325 (less than 1) |
| Heart | 9 (5) | 2,574 (5) |
| Kidney | 73 (40) | 363,573 (69) |
| Kidney and pancreas | 19 (10) | 3,537 (7) |
| Liver | 59 (32) | 7,885 (15) |
| Liver and bowel | 1 (1) | 15‡ |
| Liver, bowel and pancreas | 3 (2) | 112‡ |
| Liver and kidney | 3 (2) | 1,265‡ |
| Pancreas | 11 (6) | 2,061 (4) |
Data are frequency (%).
Data from January 2000 to November 2012. Data not included for transplantations not performed in the survey population (lung, heart and lung, and others). Data from United States Department of Health and Human Services Organ Procurement and Transplantation Network. Available at: http://optn.transplant.hrsa.gov/data. Retrieved November 29, 2012.
Percentages do not add up to 100% because of rounding.
Data not available by age. Numbers reflect all women older than age 18 years with listed organs transplanted; therefore, percentages were not calculated.
Before transplantation, 79 women (44%) reported they were not aware that a woman could become pregnant after transplantation. Women with kidney transplants most often reported awareness of posttransplant pregnancy (63/103 women [61%]), whereas women with liver transplants least often reported awareness (34/69 women [49%]). Younger women (age 19–29 years) reported awareness of posttransplant pregnancy (20/45 [44%]) less frequently when compared with women older than age 30 years (82/136 women [60%]).
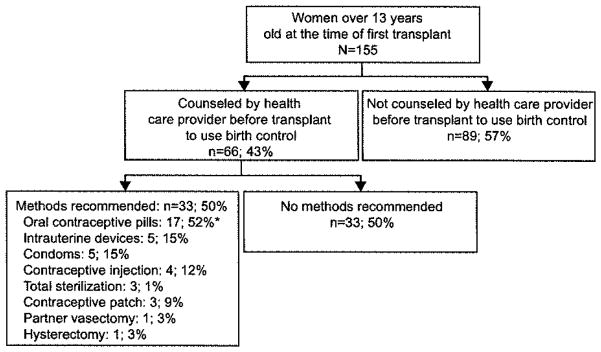
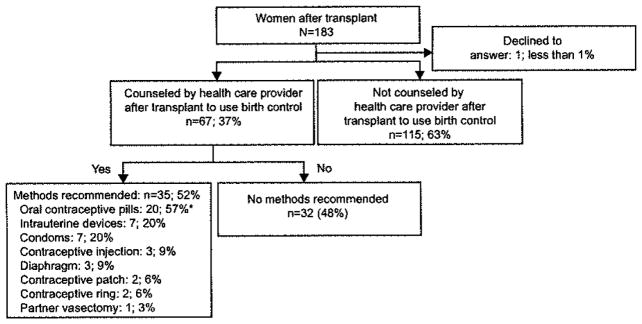
There were 155 women older than 13 years of age at the time of receiving their first transplant, 66 of whom reported that a health care provider discussed contraception before organ transplantation. Of these women, half (36) reported that a specific method was recommended, with oral contraceptive pills as the most common (Fig. 1). Women who were children at the time of transplantation were excluded from the pretransplantation analysis; however, these patients should be counseled regarding contraception as adolescents. After organ transplantation, 67 women (37%) reported that a health care provider discussed contraception and approximately half had a method recommended by their provider (Fig. 2). The data presented in Figures 1 and 2 were analyzed with Fisher exact tests to compare the proportions who were recommended each contraception method before and after transplantation. There were no significant differences found between the method of contraception that was discussed before and after transplantation.
Fig. 1.
Contraceptive counseling before organ transplantation. *Sum of percentages is more than 100% because participants were allowed to choose more than one response.
Fig. 2.
Contraceptive counseling after organ transplantation. *Sum of percentages is more than 100% because participants were allowed to choose more than one response.
Sixty-six women reported that a health care provider discussed the potential for pregnancy after organ transplantation. This varied depending on the organ transplanted; women with kidney transplants (as single organ transplanted or as part of multiple organs transplanted) were most often counseled (n=43 [42%]), followed by those with liver transplants (as single organ transplanted or as part of multiple organs transplanted; n=21 [30%]), and women with heart transplants were the least often counseled (n=2 [22%]). For women who did discuss posttransplant pregnancy, they most commonly talked with their transplant health care provider (n=45 [67%]), primary care provider (n= 11 [16%]), or gynecologist (n=8 [12%]).
One hundred nineteen women (65%) reported sexual activity at least once per month after organ transplantation compared with 110 women (60%) reporting sexual activity at least once per month before organ transplantation. Approximately half of women surveyed (88/183; Table 2) were using a method of contraception at the time of the survey and their methods are displayed in Table 3. Female sterilization was the most commonly used method, followed by oral contraceptive pills. Contraceptive use was most common in women aged 19–29 years (28/45 [62%]).
Table 2.
Contraceptive Use by Women With Solid Organ Transplants (n=183)
| Women With Transplants at the Nebraska Medical Center | % of Women Aged 15–44 y Using Specified Contraception During Month of Interview: Data From the National Survey of Family Growth23 | |
|---|---|---|
| Not currently using any contraception | 95 (52) [45–59] | 38 |
| Currently using any method of contraception | 88 (48) [41–55] | 62 |
Data are n (%) [95% confidence interval] unless otherwise specified.
Table 3.
Methods of Contraception Used by Women Who Received Solid Organ Transplants (n=88)
| Method of Contraception | Women With Transplants at the Nebraska Medical Center*† | % of Women Using Specified Contraception During Month of Interview: Data From the National Survey of Family Growth23‡ |
|---|---|---|
| Female sterilization | 27 (31) [22–41] | 27 |
| Oral contraceptive pills | 25 (28) [20–39] | 28 |
| Condoms | 12 (14) [8–22] | 16 |
| Intrauterine device | 12 (14) [8–22] | 6 |
| Partner vasectomy | 6 (7) [3–14] | 10 |
| Other hormonal methods§ | 7 (8) [4–16] | 7 |
| Other methods¶ | 1 (1) [0–6] | 6 |
| Not sure | 2 (2) [1–8] | — |
Data are n (%) [95% confidence interval] unless otherwise specified.
Number does not add to the total because women may have reported using more than one method.
Percentages do not add up to 100% because of rounding.
Percentages do not add up to 100% because women may have reported using more than one method during the month of the interview.
Includes 3-month contraceptive injection, contraceptive patch, contraceptive ring, and contraceptive implant.
Includes calendar rhythm, natural family planning, cervical mucus test, and temperature rhythm.
There were 20 women who became pregnant after organ transplantation: 12 women experienced 1 pregnancy; 5 women experienced 2 pregnancies; and 3 women experienced 3 pregnancies. The outcomes of these 31 pregnancies and any complications are displayed in Table 4. The median time from first transplant to the first pregnancy was 8 years (range 1–23 years). Four women had undergone more than one transplantation surgery. The organs transplanted in the women who became pregnant were as follows: 12 liver, small bowel, or both, seven kidney, pancreas, or both, and one heart Women with unplanned pregnancies were counseled regarding pregnancy (2/8 [25%]) less often than women with planned pregnancies (7/12 [58%]). Women who were counseled regarding pregnancy after transplant had more planned pregnancies than those who were not counseled (7/9 [78%] compared with 5/11 [45%]).
Table 4.
Pregnancy Outcomes and Complications After Organ Transplantation at the Nebraska Medical Center
| Pregnancies After Solid Organ Transplantation*
|
||||
|---|---|---|---|---|
| First Pregnancy | Second Pregnancy | Third Pregnancy | All Pregnancies | |
| Planned pregnancy | 12 (60) | 7 (88) | 3 (100) | 22 (71) |
| All pregnancies | 20 | 8 | 3 | 3 |
| Outcome | ||||
| Full-term delivery | 7 (36) | 3 (38) | 1 (33) | 11 (35) |
| Preterm delivery | 4 (21) | 2 (25) | 1 (33) | 7 (23) |
| Spontaneous abortion | 7 (36) | 3 (38) | 1 (33) | 11 (35) |
| Elective abortion | 1 (5) | 0 | 0 | 1 (3) |
| Complications of delivered pregnancies | ||||
| Delivered pregnancies | 11 | 5 | 2 | 18 |
| Preterm labor | 4 (36) | 3 (60) | 1 (5) | 7 (39) |
| Preterm premature rupture of membranes | 1 (9) | 0 | 0 | 1 (6) |
| Intrauterine growth restriction | 0 | 0 | 0 | 0 |
| Preeclampsia | 6 (55) | 2 (40) | 0 | 6 (44) |
| Gestational diabetes | 3 (27) | 0 | 0 | 3 (17) |
| Hypertension | 7 (64) | 3 (60) | 0 | 10 (56) |
| Transplant rejection | 2 (18) | 1† (20) | 0 | 3 (17) |
Data are n (%) or n.
Percentages may not add to 100 because of rounding.
Patient was unsure if she experienced a transplant rejection during her pregnancy.
DISCUSSION
Both the transplant and gynecologic literature support the return of fertility and need for contraception Posttransplant;3–5,8,9 however, our study indicates that women themselves do not understand these issues well. Fertility returns quickly after transplantation, with ovulation occurring in women within a few months after transplantation.10,11 Most women of reproductive age continue to be sexually active. The combination of newly restored fertility and sexual activity begs the following question: are providers discussing fertility and contraception with the transplant population? Reproductive counseling is recommended as part of transplant care, beginning at the pretransplantation evaluation.12,13 Despite these recommendations, women with transplants are poorly informed of their posttransplantation fertility and need for contraception.
Women with transplants are in frequent contact with members of the transplant team and, subsequently, much of their contraception and fertility counseling comes from these providers. Women also receive counseling from primary care providers, family members, and gynecologists. The quality and consistency of this information likely varies widely, giving women mixed messages regarding how a transplant will affect their reproductive health. As experts in family planning, gynecologists should be included in the pretransplantation evaluation as part of a multidisciplinary team approach to ensure appropriate contraception and pregnancy counseling.
Oral contraceptive pills were the most commonly recommended contraceptive method for women with transplants. Although this method is safe in this population,14,15 it has a higher rate of failure when compared with long-acting reversible contraception methods.16 The findings of the Contraceptive CHOICE project recently established that long-acting reversible contraception, including intrauterine devices and contraceptive implants, provides the most effective contraception and decreases the rate of unplanned pregnancies.17 Long-acting reversible contraception is an ideal method of contraception for women with transplants because they are highly effective, require a single office visit for initiation, and do not require daily adherence.16 Intrauterine devices previously have been recommended against in women with transplants, based on a small cases series in 1981.18 In 2010, the Division of Reproductive Health at the Centers for Disease Control and Prevention published a systemic review of contraceptive use among solid organ transplant recipients14 as part of the creation of the United States Medical Eligibility Criteria for Contraceptive Use that states that based on the available data, the benefits generally outweigh the risks for most contraceptive methods (including intrauterine devices) in an uncomplicated solid organ transplantation patient.19
The rate of planned pregnancies in our population (71%) was higher than that of the general population (51%)20 and was much higher than previously reported for women with kidney transplants (7%).6 The rate of planned pregnancies is high despite the low rates of contraception counseling. This may indicate that women with transplants are more motivated to plan pregnancies than the general population, perhaps because of their own health concerns. The difference in the rate of unplanned pregnancies found in our study may be attributable to cultural attitudes toward contraception and perception of pregnancy in women with complex medical conditions. Only one woman reported having an elective abortion, which is much lower than expected based on the rate of unplanned pregnancies and the rate of termination in the United States.20 It has been established that abortions are systematically underreported;21,22 therefore, it is likely that the true number of abortions in our study population is higher than stated. Underreporting of abortions (and unplanned pregnancies) also would increase the number of unplanned pregnancies seen in this patient population.
The strengths of this study include a high response rate, likely attributable to a motivated patient population, and a unique perspective of posttransplant fertility and contraception knowledge from the woman who underwent the transplantation. Our population included a variety of organs transplanted, including small bowel and heart, both of which have limited data regarding reproductive health after transplantation. Limitations of the study include recall bias and the small sample size of the number of pregnancies after organ transplantation, which prevented us from drawing statistically significant conclusions regarding the effect of contraception and fertility counseling on the rate of planned pregnancies. Additionally, these results may not be generalizable to other programs providing transplant services because our data are from a single institution.
Women with transplants are in need of education regarding the potential for pregnancy and need for contraception after organ transplantation. Our study indicates that more than half of women with transplants did not recall receiving counseling about the potential for posttransplant pregnancy or the need for contraception. Long-acting reversible contraception should be recommended as first-line methods for women who desire reversible contraception, and gynecologists should be involved in the contraceptive counseling of women with transplants. A multicenter study of women with solid organ transplants would provide more insight regarding the contraceptive counseling and fertility awareness in this growing population.
Acknowledgments
Funded by the American College of Obstetricians and Gynecologists/Bayer Healthcare Contraceptive Counseling Award and supported by the Olson Center for Women’s Health and VA Medical Center.
This work was supported in part by Health Resources and Services Administration contract 234-2005-37011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
The authors thank Dr. Alan Langnas at the Nebraska Medical Center, Section of Transplant Surgery, for his assistance with project development and participant recruitment.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
LEVEL OF EVIDENCE: II
References
- 1.Organ Procurement and Transplantation Network. Organ Procurement and Transplantation Network, HRSA, DHHS. 9 A.D Available at: http://optn.transplant.hrsa.gov/latestData/rptData.asp. Retrieved November 29, 2012.
- 2.Surti B, Tan J, Saab S. Pregnancy and liver transplantation. Liver Int. 2008;28:1200–6. doi: 10.1111/j.1478-3231.2008.01871.x. [DOI] [PubMed] [Google Scholar]
- 3.Watnick S, Rueda J. Reproduction and contraception after kidney transplantation. Curr Opin Obstet Gynecol. 2008;20:308–12. doi: 10.1097/GCO.0b013e3282f8b009. [DOI] [PubMed] [Google Scholar]
- 4.Mastrobattista JM, Katz AR. Pregnancy after organ transplant. Obstet Gynecol Clin North Am. 2004;31:415–28. doi: 10.1016/j.ogc.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Krajewski CM, Geetha D, Gomez-Lobo V. Contraceptive options for women with a history of solid organ transplantation. Transplantation. 2013;95:1183–6. doi: 10.1097/TP.0b013e31827c64de. [DOI] [PubMed] [Google Scholar]
- 6.Guazzelli CA, Torloni MR, Sanches TF, Barbieri M, Pestana JO. Contraceptive counseling and use among 197 female kidney transplant recipients. Transplantation. 2008;86:669–72. doi: 10.1097/TP.0b013e3181817e7d. [DOI] [PubMed] [Google Scholar]
- 7.Coscia LA, Constantinescu S, Moritz MJ, Frank A, Ramirez CB, Maley WL. Report from the National Transplantation Pregnancy Registry (NTPR): outcomes of pregnancy after transplantation. Clin Transpl. 2009:103–22. [PubMed] [Google Scholar]
- 8.Parhar KS, Gibson PS, Coffin CS. Pregnancy following liver transplantation: review of outcomes and recommendations for management. Can J Gastroenterol. 2012;26:621–6. doi: 10.1155/2012/137129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watnick S. Pregnancy and contraceptive counseling of women with chronic kidney disease and kidney transplants. Adv Chronic Kidney Dis. 2007;14:126–31. doi: 10.1053/j.ackd.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Abramovici H, Brandes JM, Better OS, Peretz A, Paldi E. Menstrual cycle and reproductive potential after kidney transplantation: report of 2 patients. Obstet Gynecol. 1971;37:121–53. [PubMed] [Google Scholar]
- 11.Jabiry-Zieniewicz Z, Kaminski P, Bobrowska K, Pietrzak B, Wielgos M, Smoter P, et al. Menstrual function in female liver transplant recipients of reproductive age. Transplant Proc. 2009;41:1735–9. doi: 10.1016/j.transproceed.2009.03.073. [DOI] [PubMed] [Google Scholar]
- 12.Josephson MA, McKay DB. Pregnancy and Kidney transplantation. Semin Nephrol. 2011;31:100–10. doi: 10.1016/j.semnephrol.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Bunnapradist S, Danovitch GM. Evaluation of adult kidney transplant candidates. Am J Kidney Dis. 2007;50:890–8. doi: 10.1053/j.ajkd.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 14.Paulen ME, Folger SG, Curtis KM, Jamieson DJ. Contraceptive use among solid organ transplant patients: a systematic review. Contraception. 2010;82:102–12. doi: 10.1016/j.contraception.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Curtis KM, Jamieson DJ, Peterson HB, Marchbanks PA. Adaptation of the World Health Organization’s medical eligibility criteria for contraceptive use for use in the United States. Contraception. 2010;82:3–9. doi: 10.1016/j.contraception.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Long-acting reversible contraception: implants and intrauterine devices. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 121. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2011;118:184–96. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 17.Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 18.Zerner J, Doil KL, Drewry J, Leeber DA. Intrauterine contraceptive device failures in renal transplant patients. J Reprod Med. 1981;26:99–102. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) U S. medical eligibility criteria for contraceptive use, 2010. MMWR Recomm Rep. 2010;59(RR-4):1–86. [PubMed] [Google Scholar]
- 20.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones RK, Kost K. Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth. Stud Fam Plann. 2007;38:187–97. doi: 10.1111/j.1728-4465.2007.00130.x. [DOI] [PubMed] [Google Scholar]
- 22.Fu H, Darroch JE, Henshaw SK, et al. Measuring the extent of abortion underreporting in the 1995 National Survey of Family Growth. Fam Plann Perspect. 1998;30:128–33. [PubMed] [Google Scholar]
- 23.Jones J, Mosher W, Daniels K. National Health Statistics Reports. 60. Hyatts ville (MD): National Center for Health Statistics; 2012. Current Contraceptive Use in the United States, 2006–2010, and Changes in Patterns of Use Since 1995. [PubMed] [Google Scholar]