Abstract
Objective
To examine the extent to which a WIC intervention improved BMI z-scores and obesity-related behaviors among children age 2–4 years.
Methods
In two Massachusetts communities, we implemented practice-changes in WIC as part of the MA-CORD initiative to prevent obesity among low-income children. One WIC program was the comparison. We assessed changes in BMI z-scores pre- and post-intervention and prevalence of obesity-related behaviors of WIC participants. We used linear mixed models to examine BMI z-score change and logistic regression models to examine changes in obesity-related behaviors in each intervention site versus comparison over two years.
Results
WIC-enrolled children in both intervention sites (v. Comparison) had improved sugar-sweetened beverage consumption and sleep duration. Compared to the comparison WIC program (n=626), we did not observe differences in BMI z-score among children in Intervention site #1 (n= 198) or #2 (n=637). In sensitivity analyses excluding Asian children, we observed a small decline in BMI z-score (−0.08 units/year [95% CI: −0.14 to −0.02], p=0.01) in Intervention Site #2 v. comparison.
Conclusions
Among children enrolled in WIC, the MA-CORD intervention was associated with reduced prevalence of obesity risk factors in both intervention communities and a small improvement in BMI z-scores in one of two intervention communities in non-Asian children.
Keywords: obesity, prevention, community health, public health services
Introduction
Obesity prevalence remains historically high among all age groups, and is a major driver of chronic disease, reduced quality of life, and health care costs.1, 2 The only age group of children in the United States (U.S.)with recent improvement in national obesity prevalence estimates are children age 2–5 years, underscoring the promise of early childhood as a critical period for childhood obesity prevention.1 Yet, racial/ethnic disparities in childhood obesity persist. Hispanic and black children between age 2–5 years have two- to three-fold higher obesity prevalence compared to white counterparts.1 The origins of obesity are complex with interlinking, multi-factorial influences ranging across environmental, social-contextual, family, and biologic levels. Thus, solutions to reduce childhood obesity must seek to build multi-sector linkages to support change at the individual, system, and community levels.3
The Special Supplemental Nutrition Program for Women, Infants and Children (WIC) provides nutrition assessment, counseling, and food benefits to families with income ≤ 185% of the U.S. Poverty Income guidelines who have a child under age 5 years, and to pregnant and post-partum women. Given the focus of the WIC program in early life, WIC is well-positioned to serve as the platform for early childhood obesity prevention in high-risk groups such as racial/ethnic minority and low-income populations.4–8 Prior childhood obesity prevention interventions within WIC demonstrated improvement in WIC provider self-efficacy in obesity-related counseling and WIC participant obesity-related behaviors, but did not evaluate the impact on child weight outcomes. 5, 8–10 A qualitative study of Kentucky WIC providers identified time as a barrier to counseling, and stated a need for more collaboration with primary health care providers and community agencies.11 Thus, incorporating WIC into larger-scale efforts that include primary care and community sectors could have lasting impacts on reducing childhood obesity. However, few community-wide childhood obesity prevention intervention studies include WIC in their efforts.
The Centers for Disease Control and Prevention (CDC)-funded Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project tests an integrated approach to childhood obesity prevention and treatment among children in low-income communities. In each of two MA-CORD communities, childhood obesity prevention interventions were implemented in the local WIC programs. This article reports the two-year outcomes of the WIC intervention delivered as part of MA-CORD among enrolled children age 2–4 years. We used a quasi-experimental, pre-post design to compare outcomes for WIC-enrolled children in each MA-CORD intervention community to those in a comparison community. We hypothesized that children receiving WIC support in the two intervention communities, compared to those receiving WIC support in a demographically-matched Massachusetts community, would have slower rates of increase in age- and sex-specific BMI z-score over a 2-year period. We also hypothesized that compared to WIC-enrolled children in a comparison community, WIC-enrolled children in the MA-CORD intervention communities would have greater improvements in obesity-related target behaviors.
METHODS
Study overview
We conducted a quasi-experimental trial in two WIC programs – one in each of two Massachusetts communities selected to participate as intervention sites for MA-CORD based on size, per capita income, and prevalence of childhood overweight and obesity. MA-CORD built upon a state public health department community level obesity prevention initiative, Mass in Motion, to extend the initiative to childhood obesity-focused intervention components in multiple sectors. The two Intervention sites and the Comparison site were selected from established Mass in Motion communities. The MA-CORD conceptual framework, intervention design and evaluation methods have been described in detail.12, 13 Briefly, MA-CORD spanned several sectors including community health centers; WIC; public elementary and middle schools; after-school settings, and the broader community. In each of these sectors in both communities, we implemented evidence-based programs to promote childhood obesity prevention. We provide a summary of the WIC intervention components that were part of MA-CORD and their effectiveness. The intervention start date in WIC was September 1, 2012. Children over age 2 years and under age 5 years were included in the evaluation. The primary outcome was rate of change in child age- and sex-specific BMI z-score over a two-year intervention period assessed using electronic WIC records from the two intervention and one comparison site.
Eligibility and Recruitment
The MA-CORD WIC study protocol was approved by the human subjects committees of the Massachusetts Department of Public Health. Children enrolled in WIC routinely attend nutrition assessment and counseling visits where anthropometric measurements (height and weight) are performed at least every 6 months. Each child with a qualifying WIC visit at any of the two intervention or comparison communities between October 1, 2010 and June 1, 2015 was eligible for inclusion for the primary outcome of child BMI z-score over time. A longitudinal de-identified dataset including child height and weight was extracted from the WIC electronic record. Children were considered eligible for inclusion if they had at least one visit during the pre-intervention period; had at least one visit 6 months after the intervention start date; were between age 2–4 years at the time of the visit; and lived in a MA-CORD or comparison community at the time of the visit. To assess child behaviors, we surveyed parents of children between age 2–4 years at baseline (September 17, 2012-February 28, 2013) and post-intervention (January 2, 2015 – May 1, 2015) and entered responses into the WIC electronic record. We extracted a de-identified dataset including behavioral survey responses during the baseline and 2-year time period from the WIC electronic record. A waiver of informed consent was obtained and the institutional review board at Massachusetts Department of Public Health (MDPH) approved all protocols.
WIC Intervention
WIC providers provided usual care for participants in all three sites (2 intervention and 1 comparison site). In usual care, nutritionists and nutrition assistants provide nutrition assessment and counseling to WIC participants during in-person visits at least three, but typically four, times yearly. Child weight and height are measured as part of the nutrition assessment. In Massachusetts, electronic WIC records calculate child BMI and flag abnormal values. Nutrition education is offered each time benefits are issued.
Within the MA-CORD Intervention WIC sites, evidence-informed practice changes formed the basis of WIC intervention components and have been described previously.12, 14, 15 Briefly, MA-CORD WIC intervention components included 1) training of WIC providers in best practices and consistent delivery of MA-CORD target behavior counseling and health messaging across sectors; 2) development of MA-CORD WIC provider resource and training materials; 3) incorporation of MA-CORD patient and family educational materials into WIC participant counseling; and 4) linkage of WIC providers to local MA-CORD clinical and community obesity prevention initiatives and enhanced healthy weight clinic referrals. WIC Provider trainings were implemented in two phases. In the first phase, MA-CORD staff and MA WIC staff collaborated on the development of full-day childhood obesity prevention trainings for WIC providers in WIC Intervention sites. The curriculum included a primer on best practices in childhood obesity prevention, rationale for selection of target behaviors, a refresher on participant-centered interviewing techniques, and an overview of practical approaches to counseling on obesity risk factors. Small-group sessions for skills practice used case-based scenarios and participant-centered techniques, and a review of existing WIC education materials that aligned with MA-CORD messaging. In the second-phase, WIC providers joined with local initiatives to strengthen cross-sector collaboration. WIC providers participated in a learning collaborative with members from health care, child care, school/after-school, and community sectors. Based on WIC staff feedback, we implemented a half-day train-the-trainer program for WIC providers to enhance confidence and practices on the topics of child screen time and sleep routines, and developed new educational materials on these topics.
The target behaviors of MA-CORD in the WIC sector were elimination of sugar-sweetened beverage intake and limitation of 100% juice intake; replacement of non-nutritious foods with fruit and vegetables; limitation of screen time to no more than 2 hours daily and elimination of televisions from bedrooms; at least 1 hour of moderate to vigorous physical activity daily; and an average of 11 hours of sleep for children between age 2–4 years.
Outcome Measurements
In routine practice standardized across the three WIC sites, trained WIC staff measured children’s weight using calibrated scales and children’s height using a stadiometer16 and entered the data into an electronic record. We extracted longitudinal BMI data of children from the electronic WIC records and calculated age- and sex-specific BMI z-scores at each visit.17
For behavioral outcome measures, WIC providers at all three sites interviewed two cross-sectional samples of parents at routine WIC visits before the intervention began and after it concluded. Parents responded to questionnaires in English, Spanish, or Portuguese at routine WIC visits for children ages 2–4 years. Trained WIC providers documented parent responses in the WIC electronic record at the time of the WIC visit. Detailed descriptions of the rationale and sources for cross-sector MA-CORD behavior questionnaires were previously described.13 Fruit, vegetable, and beverage intake were measured using five questions. 18, 19 Child physical activity was reported as days per week that children were physically active for a total of at least 60 minutes.20 Daily minutes of screen time watching screens and presence of TV in bedroom were assessed in two questions.21 Average sleep time over 24-hour periods for week and weekend days was measured in two questions.22 We obtained child age, gender, race/ethnicity, and city of residence from the electronic WIC record.
Statistical Analysis
Analysis was performed December 2015 through July 2016. For the main outcome of BMI z-score, we assessed longitudinal change in individual-level BMI z-scores in each MA-CORD intervention community compared to change in the comparison community, using multilevel, mixed effects linear regression. Models were adjusted for child age, gender, and race/ethnicity. By analyzing repeated BMI z-score measures at the individual-level in this manner, observations within person over time and within community were taken into account. To be considered in the analysis, each child had to have at least one measurement before (i.e., “baseline”) and at least one measurement six months after (i.e., “follow-up”) the intervention began.
To examine community-level pre-post differences in behavior, we compared two cross-sectional samples, drawn from all three sites before and after the intervention. Reported behaviors were coded dichotomously and reflected meeting vs. not meeting recommendations for that behavior (e.g., reporting physical activity at least 1 hour per day/7 days per week). To assess differences in behavior before and after the intervention, we used multi-level multivariable logistic regression models. Regression models were adjusted for random effect of community, and for fixed effects of child age, gender, and race/ethnicity. An interaction term was computed for each MA-CORD community to assess time by community (i.e, intervention compared to control community) effects for each behavior. SAS version 9.4 (Cary, NC) was used for all analyses.
RESULTS
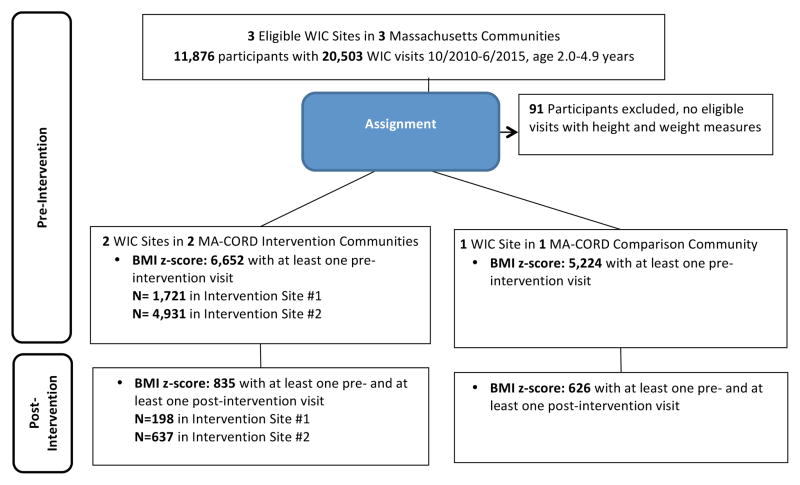
Across the two intervention and one comparison sites, 11,876 children age 2–4 years had an eligible visit between October 1, 2010 and June 1, 2015 (Figure 1). Of these, 1,474 children had at least 1 visit prior to the start of the intervention and 1 visit post intervention. After exclusion for implausible height or weight and missing covariate data, 1,461 children met eligibility criteria of at least one baseline and one follow-up visit, forming the study sample for the longitudinal cohort. Table 1 shows sample characteristics of the longitudinal cohort. For race/ethnicity at the pre-intervention period, we found a higher prevalence of WIC-enrolled children of Asian descent in the comparison community (20.6%) than in Intervention site #1 (2.6%) and Intervention site #2 (0.8%). For the longitudinal cohort with BMI data, WIC-enrolled children in the MA-CORD intervention communities also had a higher prevalence of overweight and obesity during the pre-intervention period.
Figure 1.
Participant Flow Diagram for the MA-CORD WIC Intervention
Abbreviations: MA-CORD, Massachusetts Childhood Obesity Research Demonstration Study; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children
Table 1.
Baseline Characteristics of the Longitudinal Cohort of Children in MA-CORD WIC Sites, by Intervention Assignment. Data from 1,461 Massachusetts Children age 2–4 years.
| Baseline Participant Characteristics | Intervention Site #1 N=198 |
Intervention Site #2 N=637 |
Comparison Site N=626 |
p-value |
|---|---|---|---|---|
| Mean (SD) or N (%) | ||||
| Age, mean (SD), months | 28.60 (3.82) | 27.89 (4.52)* | 28.79 (4.66)* | <0.001 |
| Boy, n (%) | 89 (45.0) | 334 (52.4) | 324 (51.8 ) | 0.17 |
| Race/ethnicity, n (%) | <0.001 | |||
| White, non-Hispanic | 86 (43.4) | 402 (63.1) | 217 (34.7) | |
| Hispanic/Latino | 83 (41.9) | 133 (20.9) | 182 (29.1) | |
| Black, non-Hispanic | 15 (7.6) | 89 (14.0) | 72 (11.5) | |
| Other, non-Hispanic (including Asian) | 14 (7.1) | 13 (2.0) | 155 (24.8) | |
| BMI z-score, last pre-intervention visit, mean (SD) | 0.48 (1.15)ǂ | 0.52 (1.21)* | 0.07 (1.30)*,ǂ | <0.001 |
| BMI Percentile, n (%) | 0.01 | |||
| <5th %ile | 4 (3.1) | 18 (4.2) | 30 (7.4) | |
| 5th to <85th %ile | 85 (66.4) | 273 (64.2) | 292 (71.6) | |
| ≥85th %ile to <95th %ile | 21 (16.4) | 67 (15.8) | 42 (10.3) | |
| ≥95th %ile | 18 (14.1) | 67 (15.8) | 44 (10.8) |
Abbreviations: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; MA-CORD, Massachusetts Childhood Obesity Research Demonstration Study BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Statistically significant difference between means, using Scheffe pairwise comparison (α < 0.05)
Statistically significant difference between means, using Scheffe pairwise comparison (α < 0.05)
For the behavioral survey outcomes, we excluded 65 participants in the pre-intervention sample and 74 participants in the post-intervention sample due to missing data. The final number considered for analysis was 633 in the pre-intervention sample and 732 in the post-intervention sample. Table 2 shows characteristics of the sample of children with behavioral survey data.
Table 2.
Characteristics of Children with Repeated Cross-sectional Behavioral Survey Responses. Data from 1,365 WIC-enrolled Massachusetts Children Age 2–5 Years in MA-CORD Intervention and Comparison Sites.
| Intervention Site #1 |
Intervention Site #2 |
Comparison Site |
p-value | |
|---|---|---|---|---|
| Child Characteristics, Baseline and Year 2 Samples | N=352 | N=395 | N=618 | |
| Age, mean (SD), months | 39.97 (10.20) | 38.33 (9.77) | 38.88 (9.86) | 0.07 |
| Boy, n(%) | 181 (51.4) | 200 (50.6) | 316 (51.1) | 0.98 |
| Race/ethnicity, n (%) | <0.001 | |||
| White, non-Hispanic | 188 (53.4) | 262 (66.3) | 262 (42.4) | |
| Hispanic/Latino | 109 (31.0) | 69 (17.5) | 128 (20.7) | |
| Black, non-Hispanic | 31 (8.8) | 40 (10.1) | 77 (12.5) | |
| Asian | 9 (2.6) | 3 (0.8) | 127 (20.6) | |
| Other race, non-Hispanic | 15 (4.3) | 21 (5.3) | 24 (3.9) | |
| BMI category at Year 2, n (%) | 0.01 | |||
| <5th %ile | 2 (1.2) | 2 (0.9) | 22 (6.6) | |
| 5th to <85th %ile | 124 (73.8) | 161 (70.6) | 230 (68.4) | |
| ≥85th %ile to <95th %ile | 24 (14.3) | 35 (15.3) | 43 (12.8) | |
| ≥95th %ile | 18 (10.7) | 30 (13.2) | 41 (12.2) |
Abbreviations: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; MA-CORD, Massachusetts Childhood Obesity Research Demonstration Study BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
BMI Outcomes
Table 3 shows changes in BMI z-score from the pre-intervention and post-intervention time periods by site. In multivariate linear mixed models, both MA-CORD Intervention site #1 and MA-CORD Intervention site #2 had small decreases in BMI z-score (−0.02 units/year [95% CI: −0.11 to −0.07], p-value=0.61; and −0.05 [−0.11 to −0.07, p-value=0.09], respectively) compared to the comparison site after implementation of the intervention, but these findings were not statistically significant.
Table 3.
Changes in Body Mass Index Z-Score from Pre-Intervention to Post-Intervention Implementation among WIC-enrolled Children, by Intervention Assignment.
| Main Outcome | Unadjusted change in BMI z-score/year after intervention start* | Adjusted change in BMI z-score/year after intervention start** | ||
|---|---|---|---|---|
| BMI z-score (units) | β Value (95% CI) | P value | β Value (95% CI) | P value |
| All Participants (N=1,461) | ||||
| Intervention Site #1 | −0.02 (−0.12 to 0.07) | 0.63 | −0.02 (−0.11 to 0.07) | 0.61 |
| Intervention Site #2 | −0.05 (−0.11 to 0.01) | 0.08 | −0.05 (−0.11 to 0.01) | 0.09 |
| Comparison Site | 0.0 (Reference) | 0.0 (Reference) | ||
| Excluding children with Asian/other race (N=1,262 participants) | ||||
| Intervention Site #1 | −0.03 (−0.12 to 0.07) | 0.59 | −0.03(−0.12 to 0.07) | 0.58 |
| Intervention Site #2 | −0.08 (−0.15 to −0.02) | 0.01 | −0.08 (−0.14 to −0.02) | 0.01 |
| Comparison Site | 0.0 (Reference) | 0.0 (Reference) | ||
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; MA-CORD, Massachusetts Childhood Obesity Research Demonstration Study.
Indicates the multilevel linear regression mixed-effects model analysis with all models corrected for clustering by community and correlation within individual.
Additionally adjusted for child age, sex, and race/ethnicity
Type 3 P value evaluates equality of effects according to community as obtained from time*arm interaction term.
We found a higher proportion of children in the comparison site were of Asian descent than in each MA-CORD intervention site Since national prevalence data shows that Asian children have lower prevalence of overweight and obesity,1 the imbalance in children of Asian ancestry between communities could bias our results. Thus, we performed sensitivity analyses excluding children with Asian race. (Table 3) In unadjusted multi-level regression models, we found that WIC-enrolled children in the Intervention site #2 site had a decrease in BMI z-score (−0.08 units/year [95% CI: −0.15 to −0.02], p-value=0.01) compared to the comparison site, and that these findings persisted in fully-adjusted models (−0.08 [−0.14 to −0.02], p-value=0.01). In sensitivity analyses, Intervention site #1 had no statistically significant difference in BMI z-score change over time compared to the comparison.
Change in Behavior Outcomes
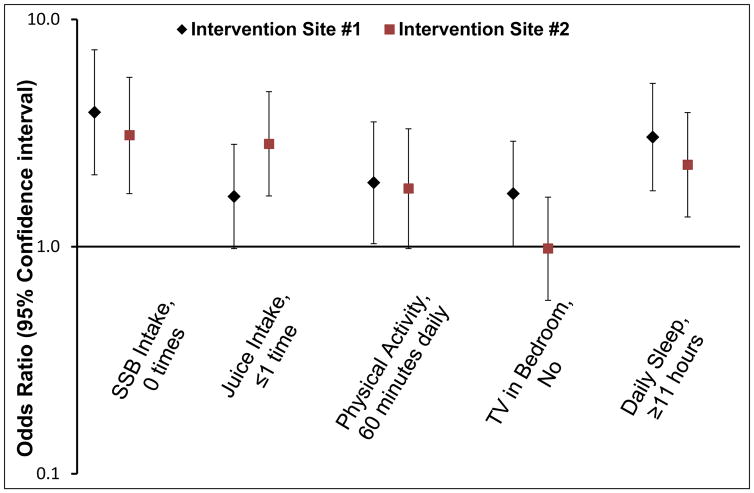
Table 4 shows prevalence of obesity-related behaviors among WIC-enrolled children by MA-CORD site. Figure 2 shows that in adjusted models, both Intervention site #1 (adjusted odds ratio [AOR] 3.90 [95% CI: 2.07,7.35], p <0.001) and Intervention site #2 (3.09 [1.71, 5.56]), p<0.001]) had greater odds of eliminating SSB consumption over time compared to the reference (Figure 2). For limiting juice intake to once daily, only Intervention site #2 (AOR 2.83 [95% CI: 1.67–4.81], p < 0.001) improved rates more than the Comparison site. In Intervention site #1, rates improved for meeting goals for physical activity (AOR 1.91 [95% CI: 1.03–3.54], p=0.04) and TV in the bedroom (AOR 1.71 [95% CI: 1.00–2.91], p=0.05) compared to the Comparison site. Participants in Intervention Site #1 (3.03 [1.76–5.23], p<0.001) and Intervention site #2 (AOR 2.29 [95% CI: 1.35–3.89], p<0.01) had greater likelihood for sufficient sleep (i.e, at least 11 hours nightly on average) compared to those in the comparison site. There were no statistically significant differences between either MA-CORD intervention site and the comparison community for meeting fruit and vegetable intake or screen time target behavior goals over time (adjusted model data not shown).
Table 4.
Pre-intervention, 2-year Post-intervention, and Changes in Meeting Behavioral Goals among 1,365 Children Age 2–4 Years Enrolled in WIC, by Intervention Assignment.
| Percent (n) | |||
|---|---|---|---|
| Fruit and vegetable, 5+ times yesterday | Baseline | Year 2 | Change in Prevalence |
| Intervention Site #1 | 25.0% (46) | 29.8% (50) | 4.8 |
| Intervention Site #2 | 16.8% (28) | 23.2% (53) | 6.4 |
| Comparison Site | 29.1% (82) | 31.8% (107) | 2.7 |
| SSB intake (soda and fruit punch), 0 times yesterday | |||
| Intervention Site #1 | 72.3% (133) | 82.7% (139) | 10.4 |
| Intervention Site #2 | 69.5% (116) | 78.1% (178) | 8.6 |
| Comparison Site | 79.1% (223) | 64.0% (215) | −15.1 |
| 100% Juice intake, ≤1 times yesterday | |||
| Intervention Site #1 | 45.1% (83) | 48.8% (82) | 3.7 |
| Intervention Site #2 | 31.7% (53) | 48.2% (110) | 16.5 |
| Comparison Site | 53.5% (151) | 45.2% (152) | −8.3 |
| Physical Activity – 7 days per week, 60 min | |||
| Intervention Site #1 | 63.0% (116) | 77.4% (130) | 14.4 |
| Intervention Site #2 | 67.1% (112) | 79.8% (182) | 12.7 |
| Comparison Site | 79.4% (224) | 80.1% (269) | 0.7 |
| Screen time, < 2 hours daily | |||
| Intervention Site #1 | 67.9% (125) | 74.4% (125) | 6.5 |
| Intervention Site #2 | 70.7% (118) | 86.0% (196) | 15.3 |
| Comparison Site | 73.8% (208) | 81.8% (275) | 8.0 |
| TV in bedroom, No | |||
| Intervention Site #1 | 50.5% (93) | 58.3% (98) | 7.8 |
| Intervention Site #2 | 55.0% (155) | 50.0% (168) | −5.0 |
| Comparison Site | 47.3% (79) | 43.4% (99) | −3.9 |
| Sleep, at least 11 hours, weighted daily average | |||
| Intervention Site #1 | 41.8% (77) | 51.8% (87) | 10.0 |
| Intervention Site #2 | 41.3% (69) | 46.9% (107) | 5.6 |
| Comparison Site | 53.2% (150) | 38.4% (129) | −14.8 |
Abbreviations: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; MA-CORD, Massachusetts Childhood Obesity Research Demonstration Study; SSB, sugar-sweetened beverage; TV, television.
Figure 2.
Adjusted Odds of Increase in Prevalence of Meeting Behavioral Goals among Children Age 2–4 Years Enrolled in WIC by MA-CORD Intervention Site, Compared to Control Site.a,b
Abbreviations: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; MA-CORD, Massachusetts Childhood Obesity Research Demonstration Study; SSB, sugar-sweetened beverage; TV, television.
aIncludes 1,365 WIC-enrolled children age 2–4 years in 2 intervention and 1 comparison WIC sites. Intervention components are described in the Methods section.
bLogistic regression models adjusted for town. Adjusted for child age, gender, and race/ethnicity
DISCUSSION
In this multi-sector, multi-level intervention to reduce childhood obesity in low-income communities, we found small BMI z-score declines among non-Asian children. When all children were included in the BMI z-score analyses, the difference in BMI z-scores were not statistically significant. However, differences in race/ethnicity and prevalence of overweight/obesity existed between communities at baseline. In the comparison community, more children were of Asian ancestry and fewer children had overweight or obesity. After excluding Asian children, the difference in BMI z-score for WIC-enrolled children in Intervention site #2 was statistically significant.
We also found improvements in prevalence of obesity-related behaviors in MA-CORD WIC Intervention sites in comparison to the usual care site. Children in WIC Intervention site #1 showed improvements in elimination of SSB intake, daily physical activity, avoiding TVs in bedrooms, and sleep sufficiency. Children in WIC Intervention site #2 had improvements in SSB intake, juice intake, and sleep. These results suggest that the MA-CORD intervention components positively influenced population-level behavior change among low-income children.
MA-CORD is one of the few studies that has implemented and evaluated community-wide efforts to reduce childhood obesity in low-income settings in the US, and is unique in its inclusion of WIC as an intervention and evaluation sector. In Shape Up Somerville, a multi-level community-based intervention in Massachusetts, school-aged children (mean baseline age 7.61 years) in an intervention community had a −0.06 decrease in BMI z-score compared to control sites.23 Shape Up Somerville had school-, home-, and community-based intervention components, with BMI outcomes measured in school settings. Given the similar magnitude of decrease in BMI z-score, our results extend this prior research to younger children and support the importance of including WIC in multi-sector interventions.
In addition to the similarities in magnitude of BMI z-score findings between Shape Up Somerville and MA-CORD, the impact of MA-CORD WIC Intervention components on child BMI z-score and behaviors is supported by the inclusion of a Comparison site that was part of the Mass in Motion initiative. The Mass in Motion initiative is a state public health initiative that seeks to curb obesity in Massachusetts communities, but did not previously include intervention components tailored to early childhood. By including WIC in MA-CORD Intervention communities and creating age-appropriate and linguistically-tailored intervention tools, the MA-CORD WIC Intervention expanded existing Mass in Motion efforts to children age 2–4 years. As none of the three sites were restricted from participating in other educational campaigns and the comparison site was a Mass in Motion site, our results show the effect of including targeted efforts to prevent obesity among young children, an age group that shows promise for responding to obesity prevention efforts in national data. 1, 24
Children with a healthy weight at age five years are likely to maintain a healthy weight throughout childhood, and modifiable early childhood obesity risk factors, including SSB consumption, excessive juice intake, lack of physical activity, and insufficient sleep, contribute to development of an unhealthy weight.25 Efforts to reduce early childhood obesity risk factors must incorporate settings that will reach children early in life in order to successfully reduce subsequent childhood obesity. An estimated 8 million women, infants, and children participated in WIC during fiscal year 2015, demonstrating an important potential reach for childhood obesity prevention initiatives.26 Given the high prevalence of childhood overweight and obesity in MA-CORD intervention communities, our findings suggest that a multi-level, multi-sector intervention improved target intervention behaviors in WIC-enrolled children who are at disproportionate risk for obesity. These results support the inclusion of WIC in multi-sector interventions to promote a healthy weight for low-income children under age five years, thus reducing disparities in childhood obesity.
The MA-CORD study has several unique features that will inform future efforts to reverse the high prevalence of childhood obesity. First, we worked with key WIC stakeholders at local and state levels to enhance linkage with existing clinical and community resources. Second, the Massachusetts Department of Public Health (MDPH) led the MA-CORD intervention implementation and evaluation. The bulk of the intervention components in WIC focused on systems-level changes by enhancing WIC providers’ ability to address obesity-related behaviors in children through one day of training, a train-the-trainer program, and consistent multi-sector linkages that can be replicated in other settings. By working with MDPH, WIC, and several other existing infrastructures, we strengthened the ability to scale-up the MA-CORD model to disseminate evidence-based interventions. Finally, although this paper reports outcomes in WIC-enrolled children, child BMI and target behaviors were measured in primary care and school settings, and findings will be reported elsewhere. Thus, MA-CORD truly represents a multisector approach to implementation and evaluation of childhood obesity prevention interventions in low-income communities.
Because the goal of this research was to evaluate the implementation of best practices for childhood obesity prevention across multiple sectors and levels in communities, randomization of intervention components was not feasible. Some imbalance between community demographics may have limited our ability to detect differences between groups as the comparison community had more underweight and Asian children than MA-CORD sites. Also, we are unable to quantify the effect of sector-specific doses of MA-CORD intervention components on BMI or to account for other initiatives to promote healthy behaviors that took place in MA-CORD or comparison communities during the intervention period. Additionally, because behavior data was obtained from serial, cross-sectional data, we were unable to attribute specific behaviors with changes in BMI z-score. Also, because behaviors were parent-reported, social desirability on the part of parents or WIC providers could have influenced behavior results. To reduce the possibility of reporting bias, we used previously validated questions. Additionally, WIC providers performed BMI and behavior assessments in either an intervention or a usual care site, not in both, thus reducing the risk for bias related to selective reporting. Overall, this research demonstrates the real-world effective of implementing interventions shown to be efficacious in BMI reduction.
In conclusion, the MA-CORD intervention was associated with improvements in BMI z-scores over 2 years in WIC-enrolled children in one of two intervention communities, and improvements in prevalence of intervention target behaviors in both intervention sites. Our findings demonstrate that WIC-enrolled children ages 2–4 years living in low-income communities with high prevalence of childhood obesity improved obesity risk factors in the context of a community-wide intervention.
STUDY IMPORTANCE QUESTIONS.
What is already known about this subject?
Children in low-income communities have increased risk for obesity.
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides nutrition education and counseling to low-income families.
Few multi-sector interventions to reduce childhood obesity have incorporated WIC.
What does this study add?
In the context of a quasi-experimental trial, a systems-level WIC intervention delivered at two WIC sites as part of the MA-CORD initiative resulted in reduction of obesity risk factors among WIC-enrolled children age 2-4 years versus a comparison site.
In sensitivity analyses, the intervention resulted in a small decline in BMI z-score for one of two intervention sites versus a comparison site.
Acknowledgments
Funding: This study was supported by the Centers for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion (Award no.: U18DP003370). Dr. Taveras is supported by grant K24 DK10589 from the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Woo Baidal is supported by the National Center for Advancing Translational Sciences KL2 TR001874. This work is solely the responsibility of the authors and does not represent the official views of the CDC, NIH, or any of the other funders.
We thank the families, institutions, faculty, research staff, and students that participated in the MA-CORD study.
Footnotes
Clinical Trial Registration: NCT02110615
Disclosure: No conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. Jama. 2016;315:2292–9. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. Jama. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foltz JL, May AL, Belay B, et al. Population-level intervention strategies and examples for obesity prevention in children. Annu Rev Nutr. 2012;32:391–415. doi: 10.1146/annurev-nutr-071811-150646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andreyeva T, Luedicke J, Henderson KE, et al. Grocery Store Beverage Choices by Participants in Federal Food Assistance and Nutrition Programs. Am J Prev Med. 2012;43:411–418. doi: 10.1016/j.amepre.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Sekhobo JP, Egglefield K, Edmunds LS, et al. Evidence of the adoption and implementation of a statewide childhood obesity prevention initiative in the New York State WIC Program: the NY Fit WIC process evaluation. Health Educ Res. 2012;27:281–91. doi: 10.1093/her/cyr100. [DOI] [PubMed] [Google Scholar]
- 6.Black MM, Quigg AM, Cook J, et al. WIC participation and attenuation of stress-related child health risks of household food insecurity and caregiver depressive symptoms. Arch Pediatr Adolesc Med. 2012;166:444–51. doi: 10.1001/archpediatrics.2012.1. [DOI] [PubMed] [Google Scholar]
- 7.Barkin SL, Gesell SB, Po’e EK, et al. Culturally Tailored, Family-Centered, Behavioral Obesity Intervention for Latino-American Preschool-aged Children. Pediatrics. 2012 doi: 10.1542/peds.2011-3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bocca G, Corpeleijn E, Stolk RP, et al. Results of a multidisciplinary treatment program in 3-year-old to 5-year-old overweight or obese children: a randomized controlled clinical trial. Arch Pediatr Adolesc Med. 2012;166:1109–15. doi: 10.1001/archpediatrics.2012.1638. [DOI] [PubMed] [Google Scholar]
- 9.Crawford PB, Gosliner W, Strode P, et al. Walking the talk: Fit WIC wellness programs improve self-efficacy in pediatric obesity prevention counseling. Am J Public Health. 2004;94:1480–5. doi: 10.2105/ajph.94.9.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davison KK, Edmunds LS, Wyker BA, et al. Feasibility of increasing childhood outdoor play and decreasing television viewing through a family-based intervention in WIC, New York State, 2007–2008. Prev Chronic Dis. 2011;8:A54. [PMC free article] [PubMed] [Google Scholar]
- 11.Chamberlin LA, Sherman SN, Jain A, et al. The challenge of preventing and treating obesity in low-income, preschool children: perceptions of WIC health care professionals. Arch Pediatr Adolesc Med. 2002;156:662–8. doi: 10.1001/archpedi.156.7.662. [DOI] [PubMed] [Google Scholar]
- 12.Taveras EM, Blaine RE, Davison KK, et al. Design of the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) study. Child Obes. 2015;11:11–22. doi: 10.1089/chi.2014.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davison KK, Falbe J, Taveras EM, et al. Evaluation overview for the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) project. Child Obes. 2015;11:23–36. doi: 10.1089/chi.2014.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165:714–22. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haines J, McDonald J, O’Brien A, et al. Healthy Habits, Happy Homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr. 2013;167:1072–9. doi: 10.1001/jamapediatrics.2013.2356. [DOI] [PubMed] [Google Scholar]
- 16.Crespi CM, Alfonso VH, Whaley SE, et al. Validity of child anthropometric measurements in the Special Supplemental Nutrition Program for Women, Infants, and Children. Pediatr Res. 2012;71:286–92. doi: 10.1038/pr.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuczmarski RJ, Ogden CL, Guo SS, et al. CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2000;2002:1–190. [PubMed] [Google Scholar]
- 18.Hoelscher DM, Day RS, Kelder SH, et al. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. J Am Diet Assoc. 2003;103:186–94. doi: 10.1053/jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- 19.Thiagarajah K, Fly AD, Hoelscher DM, et al. Validating the food behavior questions from the elementary school SPAN questionnaire. J Nutr Educ Behav. 2008;40:305–10. doi: 10.1016/j.jneb.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 20.Helmerhorst HJ, Brage S, Warren J, et al. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int J Behav Nutr Phys Act. 2012;9:103. doi: 10.1186/1479-5868-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmitz KH, Harnack L, Fulton JE, et al. Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. J Sch Health. 2004;74:370–7. doi: 10.1111/j.1746-1561.2004.tb06632.x. [DOI] [PubMed] [Google Scholar]
- 22.Chervin RD, Hedger K, Dillon JE, et al. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1:21–32. doi: 10.1016/s1389-9457(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 23.Economos CD, Hyatt RR, Must A, et al. Shape Up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev Med. 2013;57:322–7. doi: 10.1016/j.ypmed.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Pan L, Freedman DS, Sharma AJ, et al. Trends in Obesity Among Participants Aged 2–4 Years in the Special Supplemental Nutrition Program for Women, Infants, and Children - United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;65:1256–1260. doi: 10.15585/mmwr.mm6545a2. [DOI] [PubMed] [Google Scholar]
- 25.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370:403–11. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.United States Department of Agriculture. WIC Program. http://www.fns.usda.gov/pd/wic-program.