Abstract
Objective
The objectives of this study were to: (a) describe teen feedback on an asthma question prompt list/video intervention designed to motivate teens to be more engaged during visits and (b) examine teen demographics associated with teen acceptance of the intervention.
Methods
Two hundred and fifty-nine teens ages 11 to 17 with persistent asthma were enrolled into a randomized, controlled trial and assigned to either a standard care or an intervention group where they watched an educational video with their parents and received a prompt list to complete before visits. Teens were interviewed after visits.
Results
Of the 185 teens randomized to the intervention group: 93% said teens should complete the prompt lists before visits; 95% recommended teens should watch the video before visits; teens with moderate/severe persistent asthma were significantly more likely to find the prompt list useful; non-White teens were significantly more likely to find the prompt list and video more useful.
Conclusions
Teens exposed to the question prompt list/video had very positive feedback about the intervention.
Practice Implications
Providers/practices should consider having teens complete question prompt lists during pre-visit wait time for use during visits and watch the video with their parents before visits.
Keywords: Asthma, children, question prompt list, educational video
1. Introduction
Prior research has found that children and adolescents with asthma are not actively involved during their medical visits [1-3]. Active involvement is important, especially for adolescents who have chronic diseases such as asthma, because interactive discussions with providers can help adolescents learn how to self-manage their treatment regimens [4]. The Centers for Disease Control emphasizes that adolescents with asthma should be empowered to manage their asthma [5]. The clinical practice guidelines of the National Asthma Education and Prevention Program encourage providers to determine treatment goals jointly with the patient and family [4, 6] and the Institute of Medicine has emphasized that shared decision-making should occur during visits [7].
In our prior work that examined provider-patient communication during pediatric asthma visits, we found that only 13% of teens asked questions about asthma management and that the majority of questions that teens asked were about asthma medications [2]. We also found that 78% of teens expressed one or more asthma medication problems yet only 11% asked a question about their medications during their medical visits [8-12].
Other research has shown that children and adolescents are not actively involved during their medical visits [13, 14]. Traditionally, the adolescent's contribution during medical visits has been limited to approximately 10% of the visit and the communication is dominated by the physician and parent [15, 16]. Parents often restrict the adolescent's participation and want to dominate the medical visit [15]. Actively involving adolescents during medical visits can improve their medication knowledge and their overall physical functioning [17, 18]. One promising mechanism to increase active adolescent participation is through the use of “question prompt lists”. A “question prompt list” is a list of common questions a patient might want to ask their doctor about their condition and its treatment. Cancer researchers have found that giving cancer patients “question prompt lists” before their visits increased the number of questions that cancer patients asked their doctors, improved patient recall of information, and prompted doctors to give patients more information [19-22]. Moreover, cancer specialists believed that implementation of the prompt lists into routine practice was feasible and did not strain resources [23].
Although question prompt lists have not been used specifically to encourage teens with asthma to actively participate in office visits, other interventions have sought to increase teen participation during visits more generally[24,25]. For example, AskMe3 is a program that was developed by the Partnership for Clear Health Communication that encourages patients to ask questions by placing posters and brochures in clinic areas that encourage patients to ask three key questions: (a) What is my main problem?, (b) What do I need to do (about the problem)?, and (c) Why is this important for me to do? [24]. The American Academy of Pediatrics' Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents has a one- page pre-visit sheet that encourage adolescents to write down what they want to discuss during their visits and then they can check off topics they most want to cover during their visits (e.g. stress, healthy eating, staying active, alcohol) [25]. These two programs take a general approach to encouraging patients to ask questions during visits [24, 25].
In our formative work, we developed our adolescent “asthma question prompt list” intervention with the input of adolescents. In addition to the question prompt list, we also developed a short educational video (less than 11 minutes) that stresses the importance of teen involvement during asthma visits that teens and parents watch together in the waiting room before visits [26]. Our intervention was developed using Social Cognitive Theory (SCT) with a focus on increasing teen self-efficacy so that they could “have the deliberative ability to make choices and action plans, [plus] the ability to give shape to appropriate courses of action and to motivate and regulate their execution” [27]. Application of SCT in pediatric asthma populations has shown that technical advice from providers is one external factor that can improve adolescents' self-management self-efficacy [28]. Our hypothesis was that watching the video and completing the asthma question prompt list would increase teen confidence in asking questions during visits. We also hypothesized that having parents watch the video with teens before visits might encourage parents to let their adolescents lead more of the discussion of their asthma with their providers. Prior work in the provider-communication area found that patient involvement during visits can improve satisfaction, adherence to recommendations, and patient health outcomes [2, 4, 7, 15, 29-32].
As part of an ongoing randomized, controlled trial of the intervention with 259 teens with persistent asthma, we interviewed teens for their feedback on an asthma question prompt list/video intervention designed to motivate teens to be more engaged during visits and examined what teen demographics were associated with teen acceptance of the intervention.
2. Methods
2.1 Procedure
2.1.1 Initial Development of the Teen Asthma Question Prompt List
Initially, we developed our asthma “question prompt list” using the actual questions asked by children/teens ages 8 through 16 during 296 pediatric asthma visits that were audio-tape recorded between 2006 and 2009 at five rural clinics [2]. In 2012, we showed two versions of the “question prompt list” to 20 children/teens with asthma between the ages of 8 and 16 to ask them how the lists could be improved. The teens were paid $10 for their time. Seventy percent of the children/teens were female (N=15); 65% were White (N=13), 20% African American (N=4), 10% Hispanic (N=2), and 5% Native American (N=1).
The first version was a list of 22 questions and we asked the children which questions they would eliminate. They were asked to cross out the ones that they would eliminate. Next, a formatted question prompt list was presented to the teens for feedback on presentation, readability, and ease of use. We asked them how they liked the formatting of the prompt list and what they thought about the directions at the top of the questions prompt list.
When asked how the prompt lists could be improved, several children/teens told us to shorten the directions at the top to make them easier to understand. One teen suggested just saying “Read these questions and put check marks by the ones you want to ask the doctor” so we made that change. We then discarded five out of twenty-two questions because 35% or more of the children/teens suggested cutting them. The resulting question prompt list had fifteen questions about asthma medications, two questions about triggers, and an area where the teen could write in questions.
2.1.2 Focus Groups with Teens, Parent, and Providers about Video Development and the Question Prompt List
We conducted focus groups with teens, parents, and providers on how to refine the question prompt list and to develop an educational video that would help improve teen self-efficacy in being actively involved during medical visits [27]. Our published article on the development of the video explains the methods used for the focus groups, who participated in the focus groups, and the video focus group results [26]. The video used teen newscasters and emphasized six major themes and the importance of teens talking about these areas with providers: asthma triggers, how to get mom off your back, staying active with asthma, tracking asthma symptoms, how to talk to your doctor, and having confidence with asthma [26].
Based on the focus group findings, the questions “What is a diskus?” and “What is a turbuhaler?” were removed. All parties told us that diskuses and turbuhalers were not used much anymore because the medications in them were now available in other forms. The question “Should I bring the medicine to school?” was also removed because most teens did already bring their rescue inhalers to school. Three questions about triggers were added, “Can you tell me what asthma triggers are?”, “What can I do if someone is smoking around me?”, and “When should I stay indoors?”. Three questions about asthma were added, “What causes my asthma?”, “How can I make my asthma better?”, and “How severe is my asthma?” Five other questions on the prompt list were reworded for clarity. The resulting question prompt list had 21 questions (eight about triggers or asthma in general and thirteen about asthma medications) and an area where the teen could write in questions that they had. Figure 1 contains the resulting asthma question prompt list that was used in the randomized controlled trial.
Figure 1.
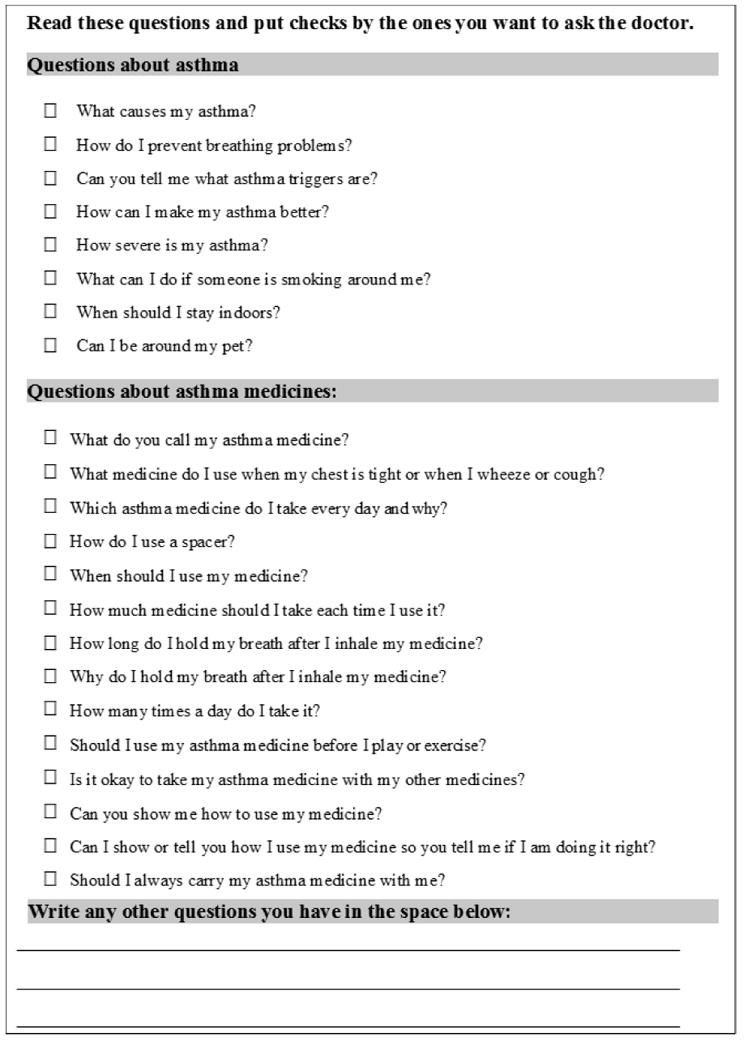
The Asthma Question Prompt List
2.1.3 Randomized Controlled Trial of the Asthma Question Prompt List/Video Intervention
Forty-six providers across four pediatric practices (one academic and three private) in North Carolina agreed to participate in the study. Clinic staff referred potentially eligible patients who were interested in learning more about the study to a research assistant. The research assistant explained the study, obtained parent consent and teen assent, and administered an eligibility screener [1, 11]. Children were eligible if they were: ages 11 to 17 years; spoke and read English or Spanish; had persistent asthma; were present for an acute or follow-up asthma visit or a well-child visit; and had previously visited the clinic at least once for asthma. Using information from the eligibility screener that parents completed with the research assistant, persistent asthma was defined as experiencing asthma-related daytime symptoms more than twice a week, asthma-related nighttime symptoms more than twice a month, or receiving one or more long-term controller therapies for asthma [1, 4, 6, 11]. Eligible teens were randomized to the intervention or control group. Teens in the intervention group watched the video with their parents on an iPad. Depending on the clinic, they either watched it in a private area before the visit or they watched it with earphones in the waiting area. The teens then received a one-page asthma question prompt list to complete before their visits and their visits were audio-tape recorded. Teens in the intervention group were interviewed after their medical visits by a research assistant and asked for their feedback on the question prompt list and video. Teens received $25 for their time.
2.2 Measurement in the Randomized Controlled Trial
2.2.1 Teen Demographics
Teen age and years the teen has been living with asthma were measured as continuous variables. Teen gender was measured as a dichotomous variable. Teen race was coded into five categories: Non-Hispanic White, African American, Native American/American Indian, Hispanic, or Other. Asthma severity was classified as mild persistent versus moderate/severe persistent according to the National Heart Lung and Blood Institute's guidelines [4, 6].
2.2.2 Teen Feedback on the Intervention
Teens were asked by the research assistant in English or Spanish if they would recommend that other teens with asthma fill out the prompt lists before their visits (yes/no) and if they would recommend that other teens with asthma watch the videos before their visits (yes/no). Teens were asked how useful the prompt list was and how useful the video was to encourage them to talk more with their provider about their asthma during the visit (not at all useful, a little useful, fairly useful, and very useful). Teens were also asked in what ways the question prompt list was helpful during their medical visits: it helped me think of questions I want to ask my provider, it helped me feel more confident to ask my provider questions, it helped me to remember to ask questions, and it didn't help me. Teens were asked in what ways the video was helpful during their medical visits: it helped me feel more knowledgeable about my asthma, it made me feel more confident to talk to my provider, and it didn't help me.
2.3 Data Analysis
First, we present descriptive statistics. For the bivariate analyses, teen race was recoded into a dichotomous variable (i.e. White versus non-White) based on analysis of variance post hoc testing. Next, we examined the bivariate relationships between the sociodemographic variables and (a) whether teens recommended that other teens use the video and question prompt lists before visits and (b) how useful the teens thought the question prompt list and video were, using Pearson correlation coefficients, chi-square statistics, or t-tests.
3. Results
3.1 Randomized, Controlled Trial Results
Two hundred and fifty-nine teens were enrolled in the randomized, controlled trial from June 2015 to November 2016. One hundred and eighty five were randomized to the intervention group. Table 1 presents the demographic characteristics of the teens in the intervention group. Close to fifty-nine percent were male. Thirty-eight percent of the teens were African American, 32% non-Hispanic White, 13% Native American, 14% Hispanic, and 2% other.
Table 1. Demographics of Teens in the Intervention Group (N=185).
| Percent (N) | |
|---|---|
| Child Gender | |
| Female | 41.1 (76) |
| Male | 58.9 (109) |
| Child Race | |
| Non-Hispanic White | 32.4 (60) |
| African American | 38.4 (71) |
| Native American/American Indian | 13.0 (24) |
| Hispanic | 14.1 (26) |
| Other | 2.2 (4) |
| Asthma Severity | |
| Mild Persistent | 49.2 (91) |
| Moderate or Severe Persistent | 50.8 (94) |
| Mean (Standard Deviation), Range | |
| Child Age | 13.15 (1.89), 11-17 years old |
| Years living with asthma | 9.14 (4.29), 0-17 years |
Table 2 presents teen feedback on the educational video. Almost 95% of teens recommended that other teens should watch the educational video before their pediatric visits. Over sixty-seven percent of the teens stated the video helped them feel more knowledgeable about their asthma and 39.5% said it made them feel more confident to talk to their provider.
Table 2. Teen Feedback on the Educational Video and Question Prompt List (N=185).
| Percent (N) | |
|---|---|
| Teen recommends that other teens should watch the video before asthma visits? | |
| Yes | 94.6 (175) |
| No | 5.4 (10) |
| In what ways did the video help you talk more with your provider about your asthma?* | |
| It helped me feel more knowledgeable about my asthma | 67.6 (125) |
| It made me feel more confident to talk to my provider | 39.5 (73) |
| It didn't help me | 4.9 (9) |
| Teen recommends that other teens should complete the question prompt list before asthma visits? | |
| Yes | 93.0 (172) |
| No | 7.0 (13) |
| In what ways did the question prompt list help you talk more with your provider about your asthma?* | |
| It helped me think of questions for the provider | 36.2 (67) |
| It helped me feel more confident to ask questions | 49.2 (91) |
| It helped me remember to ask questions | 29.7 (55) |
| It didn't help me | 8.6 (16) |
Teens checked all that applied
Females were significantly more likely to recommend that other teens watch the video before their visits than males (Pearson chi-square=4.2, p=0.04). Almost 99% of females thought other teens should watch the video before visits compared to 92% of males. Age, race, years living with asthma, and severity of asthma were not significantly associated with recommending that other teens watch the video before visits.
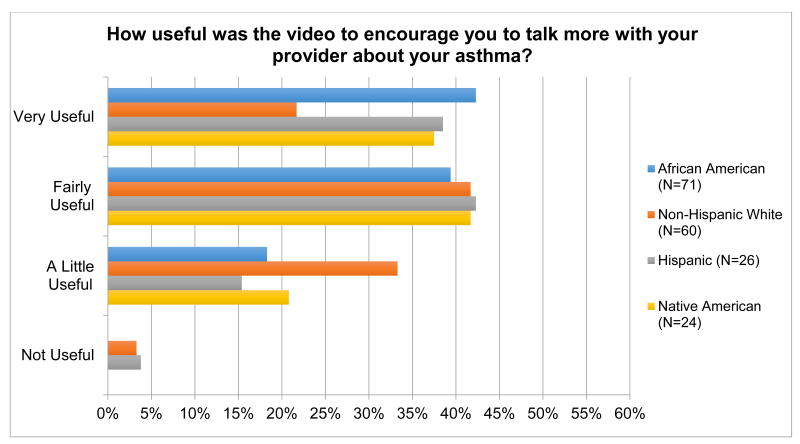
Figure 2 presents how useful teens thought the video was in encouraging them to talk with their provider about their asthma by teen race/ethnicity. Non-White teens were significantly more likely to believe that the educational video was more useful than White teens (t-test=3.0, p=0.003, mean score= 3.2 versus 2.8). Age, gender, years living with asthma, and asthma severity were not significantly associated with how teens viewed the video's usefulness.
Figure 2.
Rating “Usefulness of the Educational Video” by Race/Ethnicity (%)
Table 2 also presents teen feedback on the question prompt list. Ninety-three percent of teens said that other teens should complete the question prompt lists before their visits. Forty-nine percent of teens said it helped them feel more confident to ask their provider questions, 36% stated it helped them think of questions to ask, and 30% said it helped them to remember to ask questions. Females were more likely than males to think that other teens should complete the question prompt lists before visits but it almost reached statistical significance (Pearson chi-square=3.81, p=0.05). Age, race, years living with asthma, and severity of asthma were not significantly associated with recommending that other teens complete the prompt lists before visits.
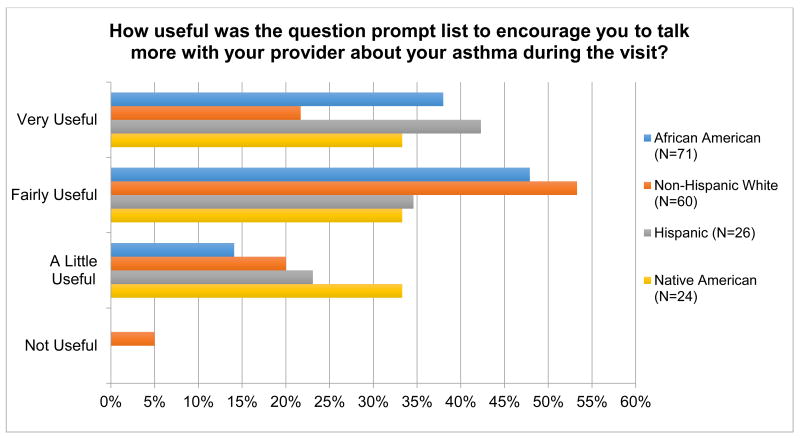
Figure 3 presents teen race/ethnicity as it relates to how useful teens thought the question prompt list was in encouraging them to talk with their provider about their asthma. Very few teens felt as though the question prompt list was not useful at all. Non-White teens were significantly more likely to believe the question prompt list was more useful than White teens (t-test=2.2, p=0.03, mean=3.2 versus mean=2.9). Patients with moderate/severe persistent asthma were significantly more likely to rate the prompt list as more useful than teens with mild persistent asthma (t-test=2.29, p=0.02, mean=3.2 versus mean=3.0).
Figure 3.
Rating “Usefulness of the Question Prompt List” by Race/Ethnicity (%)
4. Discussion and Conclusion
4.1 Discussion
The majority of teens in the randomized, controlled trial who were in the intervention group believed that other teens with asthma should use the question prompt list and watch the educational video before visits. Teens might have viewed the intervention in such a positive light because they helped develop it and their input was considered most important when finalizing the question prompt list and educational video content. Also, the intervention was guided using Social Cognitive Theory as a theoretical framework and our primary goal was to increase teen self-efficacy or confidence in being involved during pediatric asthma visits [25]. Therefore, by focusing on increasing teen confidence to be engaged during visits this approach might have contributed to why teens rated the intervention as being useful [28].
Teens not only felt as though the educational video made them feel more confident to talk with their provider, but over two-thirds of the teens stated that the video helped them feel more knowledgeable about their asthma. The video was approximately 11 minutes long and it emphasized six major themes and the importance of teens talking about these areas with providers: asthma triggers, how to get mom off your back, staying active with asthma, tracking asthma symptoms, how to talk to your doctor, and having confidence with asthma [26]. Pediatric practices should consider having teens with asthma watch the video with their parents while they are in the waiting area prior to seeing their providers. Once our randomized, controlled trial is over, the videos will be placed on a YouTube channel so that practices and families can access them from anywhere where there is Internet available.
Our finding that the majority of teens rated the asthma question prompt list as useful is similar to the results of a study which implemented AskMe3 [33]. The researchers found that 93% of patients found the three questions in the AskMe3 brochure helpful and 91% stated they knew more about their medical condition after the visit [33]. In another study where posters and brochures about AskMe3 were made available in clinics, 42% of patients reported hearing about AskMe3 compared to none before, and half of those who had heard about it, asked questions during their visits [34]. Additionally, patients reported thatAskMe3 helped them remember to ask questions and to think about what questions to ask which is similar to the results of our study [34].
Pediatric practices should also consider having all teens with persistent asthma complete the question prompt list while waiting to see their providers so that they can refer to it during their visits. The asthma question prompt list will also be made available on a website for families or practices to access from anywhere where there is Internet access. Non-White teens and teens with moderate/severe asthma were significantly more likely to find the question prompt lists useful so practices may want to especially encourage these individuals to use them.
The results cannot be generalized beyond the four practices in North Carolina from which the teens were recruited. Future research should be conducted in other parts of the United States. Another limitation is that we just enrolled only 11 to 17 year-olds and those being seen in pediatric practices. Future research should examine whether younger children and those children who see physicians in other settings (family medicine, community health centers) react as favorably to the intervention.
4.2 Conclusion
Teens exposed to the videos and asthma question prompt list gave positive feedback about both parts of the intervention. Non-White teens were significantly more likely than White teens to find the video and question prompt list more useful.
4.3 Practice Implications
Practices should consider having teens complete question prompt lists during pre-visit wait time. Clinics caring for teens with asthma should consider having teens with asthma watch the educational video with their parents in the waiting area before visits. The reason teens and parents should watch the video together is that the video emphasizes the importance of teen involvement during visits so that teens can learn how to take more responsibility for their asthma.
Highlights.
93% of teens recommended the asthma question prompt list for other teens.
Almost 95% of teens recommended the educational video for other teens.
African American teens found the question prompt list and video more useful than non-African American teens.
Providers/practices should consider having teens complete asthma question prompt lists during pre-visit wait time and watch the educational video with their parents before visits.
Acknowledgments
Informed consent and patient details: The authors confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Financial Support: This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Program Award (1402-09777). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Dr. Sleath is additionally supported by the University of North Carolina (UNC) Clinical and Translational Science Award (CTSA), National Institutes of Health, through Grant Award Number UL1TR001111-03 NIH. Drs. Sleath and Reuland are also supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 1UL1TR001111. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest and Disclosure Statement: The authors have no conflict of interest.
Author Contributions: Betsy Sleath, Scott A. Davis, Claire Hayes Watson, and Gail Tudor contributed to drafting the article. Betsy Sleath, Delesha M. Carpenter, Charles Lee, Nacire Garcia, Ceila E. Loughlin, Dana Etheridge, Laura Rivera-Duchesne, Karolyne Batey, Cristina Duchesne, and Gail Tudor contributed to conception and design of study. Betsy Sleath, Delesha M. Carpenter, Nacire Garcia, Daniel S. Reuland, and Gail Tudor contributed to acquisition of data. Betsy Sleath, Delesha M. Carpenter, Scott A. Davis, Claire Hayes Watson, and Gail Tudor contributed to analysis and interpretation of data. All authors gave final approval of the submitted version of the article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sleath B, Carpenter DM, Slota C, Williams D, Tudor G, Yeatts K, Davis S, Ayala GX. Communication during pediatric asthma visits and self-reported asthma medication adherence. Pediatrics. 2012;(130):627–33. doi: 10.1542/peds.2012-0913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sleath BL, Carpenter DM, Sayner R, Ayala GX, Williams D, Davis S, Tudor G, Yeatts K. Child and caregiver involvement and shared decision-making during asthma pediatric visits. J Asthma. 2011;(48):1022–31. doi: 10.3109/02770903.2011.626482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wassmer E, Minnaar G, Abdel Aal N, Atkinson M, Gupta E, Yuen S, Rylance G. How do paediatricians communicate with children and parents? Acta Paediatr. 2004;(93):1501–6. doi: 10.1080/08035250410015079. [DOI] [PubMed] [Google Scholar]
- 4.National Heart Lung and Blood Institute. National Heart Lung and Blood Institute Publication Number 08-5846. [Accessed April 8, 2017];Guidelines for the Diagnosis and Management of Asthma. 2007 Expert panel report 3. http://www.nhlbi.nih.gov/files/docs/guidelines/asthsumm.pdf.
- 5.Centers for Disease Control and Prevention. Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001--2009. MMWR Morb Mortal Wkly Rep. 2011;(60):547–52. [PubMed] [Google Scholar]
- 6.National Heart Lung and Blood Institute. National Heart Lung and Blood Institute Publication Number 97-4051. [Accessed April 8, 2017];Guidelines for the Diagnosis and Management of Asthma. 1997 Apr; Expert panel report 2. http://www.nhlbi.nih.gov/files/docs/guidelines/asthgdln_archive.pdf. [PubMed]
- 7.Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system of the 21st century. Washington, DC: National Academy Press; 2001. [Accessed April 8, 2017]. http://iom.nationalacademies.org/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx. [Google Scholar]
- 8.Sleath B, Carpenter DM, Beard A, Gillette C, Williams D, Tudor G, Ayala GX. Child and caregiver reported problems in using asthma medications and question-asking during paediatric asthma visits. Int J Pharm Pract. 2014;(22):69–75. doi: 10.1111/ijpp.12043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sleath B, Carpenter DM, Ayala GX, Williams D, Davis S, Tudor G, Yeatts K, Gillette C. Communication during pediatric asthma visits and child asthma medication device technique 1 month later. J Asthma. 2012;(49):918–25. doi: 10.3109/02770903.2012.719250. [DOI] [PubMed] [Google Scholar]
- 10.Sleath B, Carpenter DM, Ayala GX, Williams D, Davis S, Tudor G, Yeatts K, Gillette C. Provider Discussion, Education, and Question-Asking about Control Medications during Pediatric Asthma Visits. Int J Pediatr. 2011;(2011):212160. doi: 10.1155/2011/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sleath B, Ayala GX, Gillette C, Williams D, Davis S, Tudor G, Yeatts K, Washington D. Provider demonstration and assessment of child device technique during pediatric asthma visits. Pediatrics. 2011;(127):642–8. doi: 10.1542/peds.2010-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sleath B, Ayala GX, Davis S, Williams D, Tudor G, Yeatts K, Washington D, Gillette C. Child- and caregiver-reported problems and concerns in using asthma medications. J Asthma. 2010;(47):633–8. doi: 10.3109/02770901003692785. [DOI] [PubMed] [Google Scholar]
- 13.Cox ED, Smith MA, Brown RL, Fitzpatrick MA. Effect of gender and visit length on participation in pediatric visits. Patient Educ Couns. 2007;(65):320–8. doi: 10.1016/j.pec.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 14.Butz AM, Walker JM, Pulsifer M, Winkelstein M. Shared decision making in school age children with asthma. Pediatr Nurs. 2007;(33):111–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Tates K, Meeuwesen L. Doctor-parent-child communication. A (re)view of the literature. Soc Sci Med. 2001;(52):839–51. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- 16.Wissow LS, Roter D, Bauman LJ, Crain E, Kercsmar C, Weiss K, Mitchell H, Mohr B. Patient-provider communication during the emergency department care of children with asthma. 36. The National Cooperative Inner-City Asthma Study, National Institute of Allergy and Infectious Diseases; NIH, Bethesda, MD, Med Care: 1998. pp. 1439–50. [DOI] [PubMed] [Google Scholar]
- 17.Levinson W. Doctor-patient communication and medical malpractice: implications for pediatricians. Pediatr Ann. 1997;(26):186–93. doi: 10.3928/0090-4481-19970301-10. [DOI] [PubMed] [Google Scholar]
- 18.O'Neill KA. Kids speak: effective communication with the school-aged/adolescent patient. Pediatr Emerg Care. 2002;(18):137–40. doi: 10.1097/00006565-200204000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Dimoska A, Tattersall MH, Butow PN, Shepherd H, Kinnersley P. Can a “prompt list” empower cancer patients to ask relevant questions? Cancer. 2008;(113):225–37. doi: 10.1002/cncr.23543. [DOI] [PubMed] [Google Scholar]
- 20.Smets EM, van Heijl M, van Wijngaarden AK, Henselmans I, van Berge Henegouwen MI. Addressing patients' information needs: a first evaluation of a question prompt sheet in the pretreatment consultation for patients with esophageal cancer. Dis Esophagus. 2012;(25):512–9. doi: 10.1111/j.1442-2050.2011.01274.x. [DOI] [PubMed] [Google Scholar]
- 21.Brown RF, Butow PN, Dunn SM, Tattersall MH. Promoting patient participation and shortening cancer consultations: a randomised trial. Br J Cancer. 2001;(85):1273–9. doi: 10.1054/bjoc.2001.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langbecker D, Janda M, Yates P. Development and piloting of a brain tumour-specific question prompt list. Eur J Cancer Care (Engl) 2012;(21):517–26. doi: 10.1111/j.1365-2354.2012.01328.x. [DOI] [PubMed] [Google Scholar]
- 23.Dimoska A, Butow PN, Lynch J, Hovey E, Agar M, Beale P, Tattersall MH. Implementing patient question-prompt lists into routine cancer care. Patient Educ Couns. 2012;(86):252–8. doi: 10.1016/j.pec.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 24.Graham S, Brookey J. Do patients understand? Perm J. 2008;(12):67–9. doi: 10.7812/tpp/07-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hagan JF, Shaw JS, Duncan P. Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd. Elk Grove Village, IL: American Academy of Pediatrics; 2007. [Google Scholar]
- 26.Sleath B, Carpenter DM, Lee C, Loughlin CE, Etheridge D, Rivera-Duchesne L, Reuland DS, Batey K, Duchesne CI, Garcia N, Tudor G. The development of an educational video to motivate teens with asthma to be more involved during medical visits and to improve medication adherence. J Asthma. 2016;(53):714–9. doi: 10.3109/02770903.2015.1135945. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;(52):1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 28.Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav. 2001;(28):769–82. doi: 10.1177/109019810102800608. [DOI] [PubMed] [Google Scholar]
- 29.Harrington J, Noble LM, Newman SP. Improving patients' communication with doctors: a systematic review of intervention studies. Patient Educ Couns. 2004;(52):7–16. doi: 10.1016/s0738-3991(03)00017-x. [DOI] [PubMed] [Google Scholar]
- 30.Roter D. The medical visit context of treatment decision-making and the therapeutic relationship. Health Expect. 2000;(3):17–25. doi: 10.1046/j.1369-6513.2000.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Med Care. 1988;(26):657–75. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Roter D, Lipkin M, Jr, Korsgaard A. Sex differences in patients' and physicians' communication during primary care medical visits. Med Care. 1991;(29):1083–93. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Michalopoulou G, Falzarano P, Arfken C, Rosenberg D. Implementing Ask Me 3 to improve African American patient satisfaction and perceptions of physician cultural competency. J Cult Divers. 2010;(17):62–7. [PubMed] [Google Scholar]
- 34.Mika VS, Wood PR, Weiss BD, Trevino L. Ask Me 3: improving communication in a Hispanic pediatric outpatient practice. Am J Health Behav. 2007;(31 Suppl 1):S115–21. doi: 10.5555/ajhb.2007.31.supp.S115. [DOI] [PubMed] [Google Scholar]