Abstract
Cognitive-Behavioral Group Therapy (CBGT) and Mindfulness-Based Stress Reduction (MBSR) are efficacious in treating social anxiety disorder (SAD). It is not yet clear, however, whether they share similar trajectories of change and underlying mechanisms in the context of SAD. This randomized controlled study of 108 unmedicated adults with generalized SAD investigated the impact of CBGT vs. MBSR on trajectories of social anxiety, cognitive reappraisal, and mindfulness during 12 weeks of treatment. CBGT and MBSR produced similar trajectories showing decreases in social anxiety and increases in reappraisal (changing the way of thinking) and mindfulness (mindful attitude). Compared to MBSR, CBGT produced greater increases in disputing anxious thoughts/feelings and reappraisal success. Compared to CBGT, MBSR produced greater acceptance of anxiety and acceptance success. Granger Causality analyses revealed that increases in weekly reappraisal and reappraisal success predicted subsequent decreases in weekly social anxiety during CBGT (but not MBSR), and that increases in weekly mindful attitude and disputing anxious thoughts/feelings predicted subsequent decreases in weekly social anxiety during MBSR (but not CBGT). This examination of temporal dynamics identified shared and distinct changes during CBGT and MBSR that both support and challenge current conceptualizations of these clinical interventions.
Keywords: social anxiety, cognitive-behavioral therapy, MBSR, mindfulness, cognitive reappraisal, randomized controlled trial, mechanisms
Social anxiety disorder (SAD) is a very common and psychologically debilitating psychiatric disorder with a lifetime prevalence rate of 12.1% (Kessler et al., 2005). Early onset of SAD frequently precedes the subsequent onset of other anxiety disorders, alcohol/substance use, and major depression (Otto et al., 2001). SAD is characterized by chronically distressing levels of social fear, humiliation, embarrassment, and social isolation (Heimberg et al., 2014; Stein & Stein, 2008). It is associated with significant functional impairment in social, educational, and occupational functioning (Acarturk, de Graaf, van Straten, ten Have, & Cuijpers, 2008; Alonso et al., 2004; Stein & Kean, 2000), poorer quality of life (Alonso et al., 2004), greater frequency of suicide attempts, and high rates of alcohol and nicotine dependence (Wittchen, Stein, & Kessler, 1999). Because it is often unrecognized and untreated (Blanco et al., 2011), SAD is associated with a significant societal burden (Acarturk et al., 2009; Patel, Knapp, Henderson, & Baldwin, 2002).
Cognitive-Behavioral Therapy for SAD
Cognitive-behavioral therapy (CBT) is considered the most efficacious and effective psychosocial intervention for SAD (Gordon et al., 2014). CBT for SAD trains patients to implement cognitive restructuring of maladaptive beliefs and interpretations in the context of within-session and in vivo exposures to feared situations. Several cognitive processes have been identified as potential mechanisms of CBT-related reductions in social anxiety symptoms in adults with SAD. These include CBT-related changes in probability bias for negative social events (Hoffart, Borge, Sexton, & Clark, 2009; McManus, Clark, & Hackmann, 2000; Smits, Rosenfield, McDonald, & Telch, 2006), self-focus, perceived acceptance by others, safety behaviors (Hoffart et al., 2009), anticipated aversive social outcomes (Hofmann, 2004), interpersonal judgments, and degree of interpersonal feedback on self-evaluations (Taylor & Alden, 2008).
One important question is whether cognitive and behavioral changes during CBT predict subsequent clinical outcomes. Formal mediation analyses of the impact of CBT for SAD on social anxiety symptom severity have provided support for several potential mediators of CBT for SAD clinical outcomes. These include decreases in maladaptive interpersonal beliefs (Boden et al., 2012), negative cognitions (Niles et al., 2014), subtle avoidance behaviors (Goldin et al., 2016), cognitive distortions (Goldin et al., 2016), and perceived social costs (Hofmann, 2004), as well as increases in positive self-views (Goldin et al., 2013a), cognitive reappraisal frequency (Goldin et al., 2016; Kocovski et al., 2015), cognitive reappraisal self-efficacy (Goldin et al., 2012b), and threat reappraisal (Smits, Rosenfield, & Powers, 2012). Thus, there is evidence that changes in specific cognitive and behavioral variables mediate the impact of CBT for SAD on social anxiety symptoms.
However, to better understand the temporal dynamics of possible mechanisms of therapeutic change, a more refined measurement strategy is needed. Fewer studies have examined weekly changes in cognitive, behavioral, and symptom measures. A recent study of trauma-focused CBT for posttraumatic stress disorder found a unidirectional relationship of weekly decreases in dysfunctional trauma related appraisals predicting subsequent reduction in weekly PTSD symptoms (Kleim et al., 2013). A study of CBT for panic disorder found that antecedent changes in anxiety sensitivity and self-efficacy temporally preceded changes in panic symptoms (Gallagher et al., 2013). More specifically for SAD, CBT has been found to produce weekly decreases in the probability of a negative social outcome that predicted subsequent fear reduction (Smits et al., 2006) and weekly increases in reappraisal success that predicted subsequent decreases in weekly social anxiety during individual CBT (Goldin et al., 2014). Thus, there is growing evidence that during CBT earlier changes in cognitive processes may impact subsequent decreases in social anxiety symptoms.
Mindfulness-Based Stress Reduction
Despite the effectiveness of CBT, only about 40% of SAD patients achieve remission from SAD (Leichsenring et al., 2014). Furthermore, many patients do not have access to quality CBT or are hesitant to enter psychotherapy (Wolitzky-Taylor et al., 2015). Thus, there is growing interest in examining non-traditional psychosocial interventions that can be offered as alternatives to CBT for SAD. One promising such alternative is Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990).
MBSR is a psychosocial intervention that consists of a combination of formal sitting, body scan, walking meditation, mindful movement (e.g., hatha yoga and qi-gong) and brief informal mindfulness practices. Like other mindfulness-based interventions (e.g., mindfulness-based cognitive therapy [Teasdale, Segal, & Williams, 1995]; acceptance and commitment therapy [Hayes, Strosahl, & Wilson, 2011]; and mindfulness and acceptance-based group therapy [Kocovski, Fleming, Hawley, Huta, & Antony, 2013]), MBSR is focused on developing mindfulness and acceptance via a variety of meditation practices (Kabat-Zinn, 1990). Because MBSR does not include training in cognitive restructuring or structured exposure to feared situations, there is very little overlap with the techniques of CBT for SAD. A potential common result of MBSR and CBT, however, is the cultivation of a metacognitive perspective, namely, awareness and understanding of one's own thought processes (Mennin, Ellard, Fresco, & Gross, 2013). MBSR is thought to enhance present-moment awareness of thoughts, emotions, and sensations via focused attention and open monitoring, and to engender the attitudes of acceptance, non-judging, and curiosity about ongoing experience.
A recent meta-analysis of mindfulness-based interventions (Hofmann, Sawyer, Witt, & Oh, 2010) showed that they reliably reduced anxiety symptoms across a variety of psychiatric and medical populations (Hedges's g = 0.63), and more so in patients with anxiety and mood disorders (g = 0.97). More specifically, in patients with SAD, MBSR has been shown to increase mindfulness skills, attention regulation, self-esteem, functioning and quality of life, as well as decrease negative self-views, trait anxiety, negative emotional reactivity, and depression (Goldin & Gross, 2010; Goldin, Ramel, & Gross, 2009; Goldin, Ziv, Jazaieri, & Gross, 2012a; Goldin, Ziv, Jazaieri, Hahn, & Gross, 2013b; Jazaieri, Goldin, Werner, Ziv, & Gross, 2012; Koszycki, Benger, Shlik, & Bradwejn, 2007).
However, a recent review (Norton, Abbott, Norberg, & Hunt, 2015) concluded that, although mindfulness and acceptance-based treatments may reduce social anxiety symptoms in adults with SAD, methodological weaknesses (e.g., small sample sizes, lack of an active treatment comparisons or control groups) limit the confidence that should be placed in the results reported for MBSR in patients with SAD. Thus, the authors called for greater methodologically rigor and a more refined examination of the processes that mediate the observed reductions in SAD symptoms during mindfulness-based interventions versus CBT. A recent randomized controlled trial of cognitive-behavioral group therapy (CBGT) versus MBSR in patients with SAD found similar improvements in social anxiety symptoms (Goldin et al., 2016). Thus, there is initial evidence that MBSR may be as effective as CBT. However, it is still not clear whether CBT and MBSR produce similar changes across therapeutic processes during treatment.
To understand mechanisms underlying the efficacy of MBSR, it is important to examine trajectories of change that occur during training and that predict outcome. To date, the single study that examined trajectories of change in MBSR found that significant increases in mindfulness skills during the first three weeks predicted decreases in perceived stress after completion of MBSR in a mixed sample of 87 adults with elevated stress related to chronic illness, chronic pain, and other life circumstances (Baer, Carmody, & Hunsinger, 2012). The trajectories of multiple indicators of mindfulness and other potential processes of change such as cognitive reappraisal have not been investigated during MBSR for any anxiety disorder. Furthermore, weekly trajectories of mindfulness and cognitive reappraisal and their relationship to clinical symptoms have not been examined during MBSR and have not been compared to CBT for SAD.
Present Study
The goals of the present study were to examine trajectories of change in weekly social anxiety, cognitive reappraisal (disputation of anxious thoughts, cognitive reappraisal, and cognitive reappraisal success), and mindfulness (mindful attitude, acceptance of anxious thoughts and feelings, and acceptance success) during 12 weeks of cognitive-behavioral group therapy (CBGT) vs. MBSR, and to test whether prior changes in weekly cognitive reappraisal and mindfulness predicted subsequent changes in weekly social anxiety.
Specifically, we tested three inter-related hypotheses. Hypothesis 1 (social anxiety trajectory): We expected that CBGT and MBSR would produce similar significant decreases in the trajectory of weekly social anxiety intensity. Hypothesis 2 (cognitive reappraisal and mindfulness trajectories): We expected that, compared to MBSR, CBGT would produce greater increases in cognitive reappraisal, and that, compared to CBGT, MBSR would produce greater increases in mindfulness. Hypothesis 3 (lead-lag analysis of time series data using Granger Causality tests on trajectories): Granger Causality (Granger, 1969) is a statistical test for determining whether values in time series A at time × predict subsequent values in another time series B at time x+1, after controlling for the autocorrelation of × and x+1 in time series B. By implementing the Granger Causality analysis in both directions (A predicting subsequent B, B predicting subsequent A), the test can determine whether the predictive relationship of time series A and B is unidirectional or bidirectional. We expected that prior week increases in cognitive reappraisal would predict subsequent week decreases in social anxiety during CBGT, and that prior week increases in mindfulness would predict subsequent week decreases in social anxiety during MBSR, whereas we expected that prior week decreases in social anxiety would not predict subsequent week increases in either cognitive reappraisal or mindfulness.
METHOD
Participants
Patients met DSM-IV-TR (American Psychiatric Association, 2000) criteria for a principal diagnosis of generalized SAD based on the Anxiety Disorders Interview Schedule for the DSM-IV-Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994). Patients met criteria for the generalized subtype of SAD if they endorsed greater than moderate social fear in 5 or more distinct social situations assessed by the ADIS-IV-L. Furthermore, patients had to achieve a score greater than 60 on the Liebowitz Social Anxiety Scale – Self-Report (LSAS-SR), the cut-off score for the generalized subtype of SAD as determined by receiver operator characteristics analysis of the LSAS-SR (Rytwinski et al., 2009). Patients were excluded for pharmacotherapy or psychotherapy during the past year, participation in CBT for any anxiety disorder during the last two years, any previous MBSR course, previous participation in long-term meditation retreats, history of regular mediation practice of 10 minutes or more 3 or more times per week, history of neurological disorders, cardiovascular disorders, thought disorders, or bipolar disorder, as well as current substance and alcohol abuse/dependence.
As reported in Goldin and colleagues (2016), from 2012 to 2014, 724 potential participants completed an online screener, of whom 307 were screened by telephone (see the flowchart for Consolidated Standards of Reporting Trials, Supplemental Figure 1). The 173 patients who were potentially eligible were administered the ADIS-IV-L in person to determine whether they met diagnostic inclusion/exclusion criteria. After 65 patients were excluded because they did not meet diagnostic criteria or failed to complete baseline assessments, the remaining 108 patients were randomly assigned in cohorts of 6 patients to CBGT (n = 36), MBSR (n = 36), or waitlist (WL) control group (n = 36). After completing the waitlist period, WL participants were randomized to CBGT or MBSR. Data from immediate and delayed (i.e., after completing the WL) treatment arms were combined after we determined that there were no between group differences in each dependent variable, as explained in more detail below.
Procedure
Potential patients were recruited through clinician referrals and web-based community listings for a study delivered in a university setting. After passing a telephone screening, a face-to-face diagnostic interview was used to determine current and past Axis I psychiatric disorders and current clinician-rated severity. After completing all baseline assessments, each set of 6 consecutive patients was assigned to one of the three groups (CBGT, MBSR, or WL). The sequence of groups was determined by a random number generator constrained to 6 instances for each of the three types of group so that at the end of the study we had 18 groups of 6 patients, with 6 groups each for CBGT, MBSR or WL. Participants in CBGT and MBSR completed a weekly assessment at baseline and during the 12 weeks of treatment. Patients received treatment at no cost and were not paid to participate. All patients provided informed consent in accordance with the Institutional Review Board at Stanford University.
Diagnostic Assessment
Diagnostic interviews were conducted at baseline using the ADIS-IV-L (Di Nardo et al., 1994). The ADIS-IV has demonstrated excellent inter-rater reliability (Brown, Di Nardo, Lehman, & Campbell, 2001). Each diagnostician was trained to criterion with an expert clinical diagnostic interviewer in our laboratory prior to conducting diagnostic interviews. To assess the inter-rater reliability of the ADIS-IV-L, we had PhD clinical psychologists and doctoral students review 20% of the interviews. There was 100% agreement with the original principal diagnosis of SAD (κ = 1.0).
Measures
To investigate weekly changes, we used Qualtrics software to administer a set of questions once a week on the day prior to each group session. The weekly questions assessed indicators of social anxiety, cognitive reappraisal, and mindfulness during CBGT and MBSR. We asked patients to rate how often they engaged with each construct from 0 to 100% of the time during social situations during the past week. For social anxiety, we asked “During the past week, how intense has your social anxiety been?” For reappraisal, we asked “how often were you disputing or challenging your anxious thoughts and feelings?” (disputing), “how often did you try to change the way you were thinking about the situation you were in?” (reappraisal), and “how successful was this strategy at decreasing your anxiety?” (perceived reappraisal success).
For mindfulness, we asked “How often were you adopting a mindful, open, curious, and willing attitude about your anxious thoughts and feelings?” (mindful attitude), “How often did you just accept your anxiety and not change it in any way?” (acceptance of anxiety), and with respect to acceptance “How able were you at doing this? (perceived acceptance success). Patients completed the weekly assessment online at baseline, during treatment, at post-treatment completion and every 3 months during 1-year follow-up.
Cognitive-Behavioral Group Therapy
CBGT was delivered by CBT-trained PhD-level clinical psychologists using the protocol developed by Heimberg’s group (Heimberg & Becker, 2002). Groups of six patients met for 12 sessions of 2.5 hours each (total time = 30 hours). To support understanding, we gave patients a CBT workbook (Hope, Heimberg, & Turk, 2010) to supplement relevant portions of the protocol. The treatment comprised four major components: (1) psychoeducation and orientation to CBGT; (2) cognitive restructuring skills training exercises and practice; (3) graduated exposure to feared social situations, within session and as homework; and (4) relapse prevention and termination. Further details are available elsewhere (Heimberg & Becker, 2002).
Mindfulness-Based Stress Reduction
MBSR was delivered by two instructors, separately, one PhD clinical psychologist and one MS in Education). Both were trained on the standard MBSR curriculum outline compiled at the University of Massachusetts Center for Mindfulness by Jon Kabat-Zinn and had experience leading multiple MBSR courses. The standard protocol was modified so that the one-day meditation retreat was converted to 4 additional weekly group sessions between the standard class 6 and 7 so that there were 12 weekly 2.5 hour sessions (total time = 30 hours). This was done to match exactly the CBGT protocol in dose, duration, and number of group members. To support the practice, each participant was given A Mindfulness-Based Stress Reduction Workbook (Stahl & Goldstein, 2010), which includes descriptions of mindfulness exercises together with pre-recorded audio files to support ongoing practice.
Adherence and Treatment Completer Status
Ph.D.-level trained clinical psychologists were trained and supervised by Dr. Heimberg in the delivery of CBGT. The MBSR instructors were supervised by the first author (PG) to deliver MBSR to adults with SAD. To assure treatment adherence, a trained rater was present in every CBGT and MBSR session to conduct real-time rating of adherence using adherence scales developed for CBT (Cognitive-Behavioral Therapy for Social Anxiety Disorder: Therapist Adherence Scale; Hope et al., unpublished, as modified by Bjornsson for group treatment) and for MBSR (Mindfulness Based Stress Reduction for Social Anxiety Disorder: Instructor Adherence Scale; Goldin & Jazaieri, unpublished) treatment of SAD. Adherence ratings indicated that both CBGT therapists and MBSR instructors were “in protocol” (rating > 4 of 5 for each session) with no between-group differences, t(11) = 0.83, p = .43, in adherence for CBGT (Mean ± SD: 4.92 ± 0.27) versus MBSR (4.81 ± 0.17). Based on a criterion of 9 of 12 sessions attended for treatment completer status, 33 (92%) of patients completed CBGT and 33 (92%) completed MBSR. Mean number of sessions attended for CBGT (Mean ± SD = 10.47 ± 1.56) and MBSR (10.37 ± 2.09) was not significantly different, t(71) = 0.22, p = .82. The mean number of within-session exposures per patient in CBGT was 4.5 (SD = 0.84).
Statistical Analyses
Weekly change intent-to-treat analyses included all patients except two who did not provide weekly data. Thus, the final sample was 106 patients. Because we did not collect weekly assessments from patients in the WL group, we focused our analyses on the direct comparison of change during CBGT versus MBSR. We first tested using between-group t-tests whether there were significant differences in the pre-to-post-treatment changes in each dependent variable among patients randomized to immediate CBGT/MBSR versus delayed (i.e., CBGT/MBSR post-WL) treatment. Because there were no significant differences, we combined data from the immediate and delayed treatment groups to increase statistical power to detect changes during CBGT (n = 54) versus MBSR (n = 52).
To account for missing data in analyses of weekly measures, multilevel modeling (MLM) was used to analyze change over time in the 106 patients included in the analyses. To examine whether missing data could be predicted, we conducted logistic regression analyses with clinical (e.g., treatment condition, baseline social anxiety and depression severity) and demographic (e.g., gender, age, education) variables as predictors of the likelihood of having a missing data pattern (0 = not missing, 1 = missing) at p < .05. Older age was associated with greater likelihood of missing data for the last three sessions, b = 0.06, Wald’s Z = 4.62, p = .031, Odds Ratio = 1.06. Therefore, we included age as a covariate in all multilevel modeling analyses. No other variables predicted missingness.
For Hypothesis 1 (social anxiety trajectory) and Hypothesis 2 (reappraisal and mindfulness trajectories), we implemented MLM in SPSS 22 to test for significant changes in the weekly items from the first session to post-treatment and whether the rates of change differed by treatment condition. MLM is an extension of the general linear model and facilitates analysis of hierarchically structured data (e.g., weekly ratings nested within participant within treatment groups) by directly modeling the clustering as level-specific orthogonal components (e.g., between- and within-persons). This approach allows for lower-level parameters (e.g., intercept and slope coefficients) to vary across higher-level units (e.g., individuals), yields unbiased standard errors (avoiding Type I errors) and estimates of variance explained (R2), and allows for testing of complex hypotheses (Hox, 2002; Snijders & Bosker, 1999).
Multilevel models were implemented to model weekly session change over time in individual patients as a function of treatment group. Group was set by coding MBSR as 0 and CBGT as 1. We modeled time at Level 1 and individual patients at Level 2. The Level 1 predictor was session and the Level 2 predictor was group. To test whether change in each weekly item differed by group, we included the session by group interaction. We modeled session as a continuous variable. Visual inspection of the shape of change in several weekly items revealed differing shapes across groups (e.g., no change in one group versus strong linear/modest quadratic change in the other group). We included only a linear effect of session to address the primary question of interest, that is, whether the treatment groups differed in rates of change over treatment. Random effects of the intercept and slope terms were included. We used an unstructured covariance structure.
For Hypothesis 3 (Granger Causality of trajectories), we used SPSS to implement a Granger causality test (Granger, 1969) to determine whether weekly ratings of reappraisal and mindfulness variables at time t-1 predicted weekly ratings of social anxiety at time t during CBGT and MBSR, separately. We also tested the inverse relationships, namely, whether social anxiety at time t-1 predicted reappraisal and mindfulness variables at time t, to determine the specificity of prediction. This analysis entailed modeling and removing the autoregression of the dependent variable and then examining the effect of the independent variable at t-1 on the dependent variable at time t.
RESULTS
Preliminary Analyses
CBGT, MBSR, and WL groups did not differ significantly (all ps > .05) on gender, age, education, ethnicity, marital status, income, current or past Axis I comorbidity, past psychotherapy or pharmacotherapy, age at symptoms onset, or years since symptom onset (Table 1).
Table 1.
Demographics and Clinical Characteristic of Randomized Participants (N = 108)
| Characteristic | CBGT (n= 36) |
MBSR (n= 36) |
WL (n= 36) |
|---|---|---|---|
| Males, No. (%) | 16 (44.4) | 16 (44.4) | 16 (44.4) |
| Age, mean (SD), years | 34.1 (8.0) | 29.9 (7.6) | 34.1 (7.8) |
| Education, mean (SD), years | 17.4 (3.3) | 16.2 (1.7) | 16.5 (2.9) |
| Ethnicity, No. (%) | |||
| Caucasian | 18 (50.0) | 14 (38.9) | 15 (41.7) |
| Asian | 15 (41.7) | 13 (36.1) | 14 (38.9) |
| Latino | 2 (5.5) | 7 (19.4) | 1 (2.8) |
| African American | 0 | 1 (2.8) | 0 |
| American Indian / Alaskan Native | 0 | 0 | 1 (2.8) |
| More than One Race | 1 (2.8) | 1 (2.8) | 5 (13.9) |
| Yearly income, No. (%) | |||
| <10k | 3 (8.3) | 3 (8.3) | 1 (2.8) |
| 10–25k | 3 (8.3) | 2 (5.6) | 4 (11.1) |
| 25–50k | 5 (13.9) | 5 (13.9) | 5 (13.9) |
| 50–75k | 6 (16.7) | 5 (13.9) | 3 (8.3) |
| 75–100k | 4 (11.1) | 3 (8.3) | 4 (11.1) |
| >100k | 9 (25.0) | 9 (25.0) | 10 (27.8) |
| Not reported | 6 (16.7) | 9 (25.0) | 9 (25.0) |
| Marital status, No. (%) | |||
| Single, never married | 20 (55.6) | 23 (63.9) | 18 (50.0) |
| Married | 12 (33.3) | 8 (23.8) | 16 (44.4) |
| Divorced, separated, widowed | 1 (2.8) | 0 | 0 |
| Living with partner | 3 (8.3) | 5 (13.9) | 1 (2.8) |
| Not reported | 0 | 0 | 1 (2.8) |
| Current Axis I Comorbidity, No. (%) | |||
| Generalized anxiety disorder | 13 (36.1) | 10 (27.8) | 8 (22.2) |
| Specific phobia | 4 (11.1) | 10 (27.8) | 5 (13.9) |
| Panic disorder | 8 (22.2) | 4 (11.1) | 2 (5.6) |
| Major depressive disorder | 1 (2.8) | 2 (5.6) | 1 (2.8) |
| Dysthymic disorder | 2 (5.6) | 2 (5.6) | 3 (8.3) |
| Obsessive compulsive disorder | 0 | 1 (2.8) | 0 |
| Past Axis I Comorbidity, No. (%) | |||
| Generalized anxiety disorder | 1 (2.8) | 0 | 1 (2.8) |
| Panic disorder | 3 (8.3) | 3 (8.3) | 1 (2.8) |
| Major depressive disorder | 13 (36.1) | 17 (47.2) | 12 (33.3) |
| Dysthymic disorder | 1 (2.8) | 1 (2.8) | 2 (5.6) |
| Obsessive compulsive disorder | 1 (2.8) | 1 (2.8) | 1 (2.8) |
| Post-traumatic stress disorder | 0 | 0 | 0 |
| Substance abuse disorder | 3 (8.3) | 3 (8.3) | 2 (5.6) |
| Eating disorder | 2 (5.6) | 1 (2.8) | 2 (5.6) |
| Past non-CBT Psychotherapy, No. (%) | 20 (55.6) | 18 (50.0) | 23 (63.9) |
| Past Pharmacotherapy, No. (%) | 15 (41.7) | 15 (41.7) | 13 (36.1) |
| Age at symptom onset, mean (SD), years | 9.0 ± 5.1 | 9.4 ± 5.1 | 8.3 ± 5.0 |
| Years since symptom onset, mean (SD), years | 25.1 ± 1.3 | 20.5 ± 9.1 | 25.8 ± 8.3 |
Note: All comparisons (between-group t-test or χ2 tests) are non-significant, p > .05. CBGT = cognitive behavioral group therapy, MBSR = mindfulness-based stress reduction, WL = waitlist group, SD = standard deviation, No. = number, k = thousand dollars. Previously published in Goldin et al., 2016; published with permission from American Psychological Association.
We computed Pearson-product correlations for the three indicators of reappraisal (disputing, reappraisal, perceived reappraisal success) and three indicators of mindfulness (mindful attitude, acceptance, acceptance success) at baseline. As shown in Table 2, we found that all three CBT related variables were significantly inter-correlated, as were the two MBSR related variables. One unexpected finding was the significant correlation of mindful attitude and reappraisal success.
Table 2.
Inter-correlation of three indicators of cognitive reappraisal and three indicators of mindfulness skills in 108 adults with social anxiety disorder at baseline
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1 Disputing | x | ||||
| 2 Reappraisal | .36**** | x | |||
| 3 Reappraisal Success | .28*** | .31**** | x | ||
| 4 Mindful Attitude | .50**** | .31**** | .33**** | x | |
| 5 Acceptance | .01 | −.14 | .07 | .10 | x |
| 6 Acceptance Success | −.02 | −.06 | .16 | .12 | .64**** |
p<.05,
p<.01,
p<.005,
p<.001
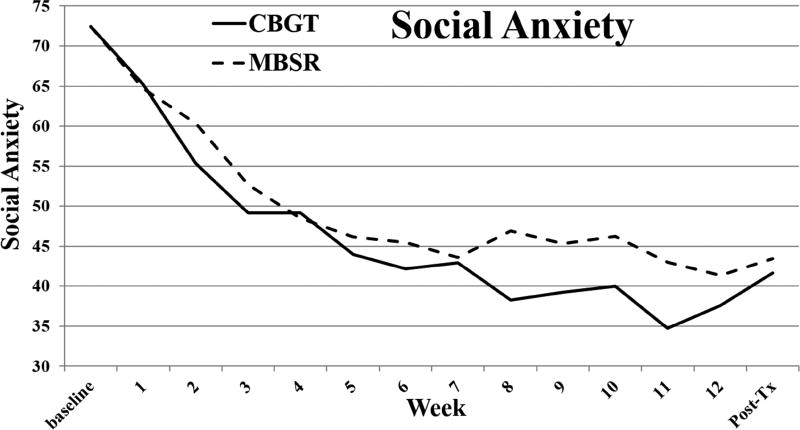
Hypothesis 1: Treatment Effects on Weekly Social Anxiety Intensity
As shown in Table 3, MLM revealed significant linear decreases from baseline to post-treatment in social anxiety for CBGT (43% decrease) and MBSR (40% decrease). However, there was no weekly session by group interaction for social anxiety (Figure 1). Our test of a model that included linear and quadratic components of the trajectory of social anxiety changes during treatment showed a similar amount of the variance explained for MBSR (93%) and CBGT (96%). Furthermore, the correlation of the MBSR and CBGT trajectories was r = 0.97. Additionally, a 2 group × 14 time point repeated-measures GLM with polynomial contrasts found no evidence of a group by time interaction for linear (F = 1.07, p = .30), quadratic (F = 0.03, p = .85) or cubic (F = 0.41, p = .52) trends in the trajectories. These results indicate that CBGT and MBSR resulted in similar trajectories of decreasing social anxiety during treatment.
Table 3.
Weekly Trajectory of Social Anxiety during CBGT and MBSR
| Social Anxiety | ||
|---|---|---|
| b | t | |
| Intercept | 65.64 | 10.99*** |
| Age | −0.20 | −1.12 |
| Session | −1.46 | −6.52*** |
| Group | −0.89 | −0.27 |
| Session × Group | −0.50 | −1.57 |
| Residuals | Wald Z | |
| Level 1 | 131.30 | 21.76*** |
| Intercept | 224.06 | 5.89*** |
| Session | 1.61 | 4.42*** |
| Intercept / Session Covariance | −7.97 | −2.66** |
| Model Fit | ||
| −2LL | 9308.44 | |
| AIC | 9326.44 | |
| BIC | 9371.91 | |
Note: Group refers to CBGT (cognitive behavioral group therapy) vs. MBSR (mindfulness-based stress reduction). −2LL = −2 × log-likelihood, AIC = Akaike’s Information Criterion, BIC = Bayesian’s Information Criterion
p < .01,
p < .005,
p < .001
Figure 1. Social anxiety weekly during CBGT and MBSR.
Multilevel modeling revealed significant linear decreases in social anxiety during CBGT (cognitive behavioral group therapy), b = −1.83, 95% CI [−2.28, −1.39], t = −8.18, p < .001, and MBSR (mindfulness-based stress reduction), b = −1.42, 95% CI [−1.87, −0.99], t = −6.40, p < .001. The group × session interaction was not significant, b = −0.40, 95% CI = −1.03 to 0.23, t = −1.27, p = .201.
Hypothesis 2: Treatment Effects on Weekly Reappraisal and Mindfulness
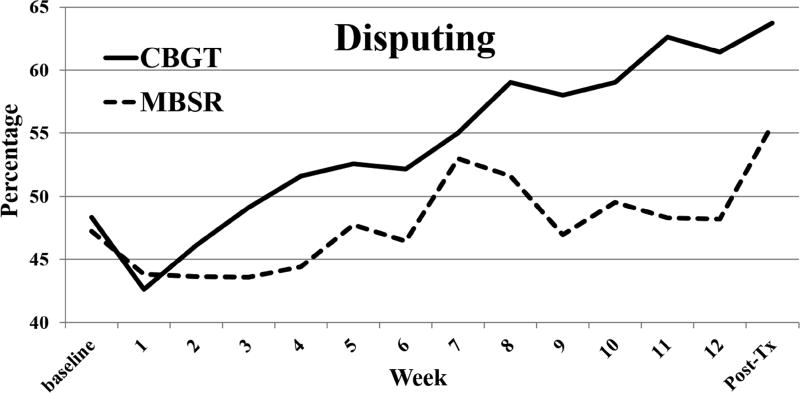
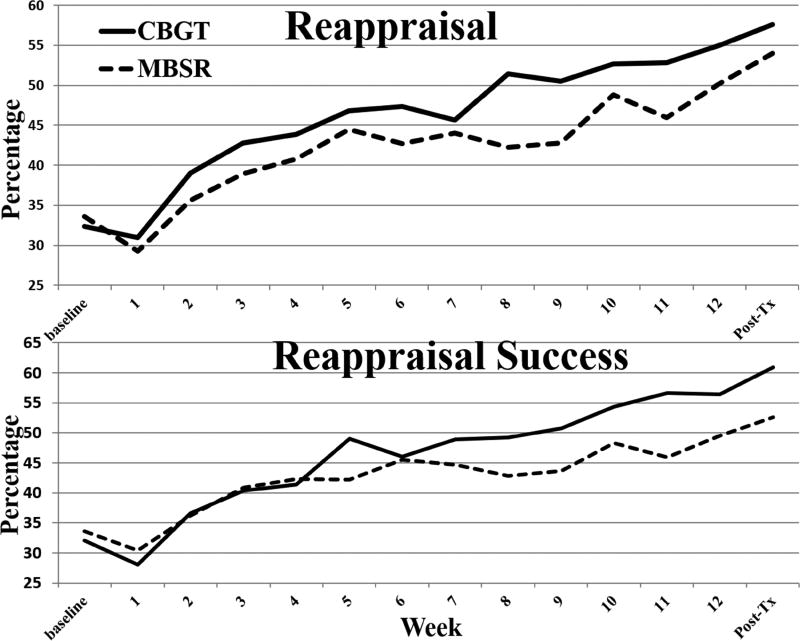
Reappraisal
As shown in Table 4, MLM analysis revealed that weekly disputing (i.e., challenging anxious thought and feelings) increased significantly during CBGT (32% increase from baseline to post-treatment) and MBSR (18% increase) (Figure 2). The session by group interaction was significant, indicating greater increases during CBGT vs. MBSR. Weekly reappraisal (i.e., changing the way you were thinking) increased significantly during CBGT (78% increase) and MBSR (61% increase), but the session by group interaction was not significant. Weekly reappraisal success increased during CBGT (90% increase) and MBSR (56% increase), with a significant session by group interaction, indicating greater increases during CBGT vs. MBSR (Figure 3). In summary, all three indicators of reappraisal improved significantly during both CBGT and MBSR, but CBGT resulted in greater improvement than MBSR for disputing and reappraisal success.
Table 4.
Multilevel Modeling Results for Cognitive Reappraisal Indicators
| Disputing | Reappraisal | Perceived Reappraisal Success |
||||
|---|---|---|---|---|---|---|
|
| ||||||
| b | t | b | t | b | T | |
| Intercept | 35.79 | 6.37*** | 26.6 | 4.50*** | 26.69 | 4.87*** |
| Age | 0.20 | 1.23 | 0.17 | 1.00 | 0.22 | 1.40 |
| Session | 0.76 | 3.10** | 1.50 | 5.69*** | 1.31 | 5.87*** |
| Group | 1.43 | 0.44 | 3.46 | 1.02 | −1.86 | −0.63 |
| Session × Group | 0.84 | 2.44* | 0.15 | 0.40 | 0.91 | 2.89** |
| Residuals | Wald Z | Wald Z | ||||
| Level 1 | 166.68 | 21.81*** | 224.79 | 21.83*** | 181.47 | 21.80*** |
| Intercept | 207.71 | 5.51*** | 210.91 | 5.08*** | 157.95 | 4.99*** |
| Session | 1.87 | 4.40*** | 1.99 | 4.03*** | 1.29 | 3.63*** |
| Int/Session Covariance | −9.95 | −3.00** | −9.34 | −2.47* | −4.31 | −1.61 |
| Model Fit | ||||||
| −2LL | 9538.10 | 9840.87 | 9590.02 | |||
| AIC | 9556.10 | 9858.87 | 9608.02 | |||
| BIC | 9601.56 | 9904.33 | 9653.47 | |||
Note: Group refers to CBGT (cognitive behavioral group therapy) vs. MBSR (mindfulness-based stress reduction). −2LL = −2 × log-likelihood, AIC = Akaike’s Information Criterion, BIC = Bayesian’s Information Criterion
p < .01,
p < .005,
p < .001
Figure 2. Disputing during CBGT and MBSR.
Weekly disputing or challenging anxious thought and feelings increased significantly during CBGT (cognitive behavioral group therapy), b = 1.60, 95% CI [1.11, 2.08], t = 6.57, p < .001, and MBSR (mindfulness-based stress reduction), b = 0.76, 95% CI [0.27, 1.24], t = 3.10, p = .003. The session by group interaction was significant, indicating greater increases during CBGT vs. MBSR, b = 0.84, 95% CI [0.16, 1.52], t = 2.44, p = .016.
Figure 3. Reappraisal and perceived reappraisal success during CBGT and MBSR.
Weekly reappraisal increased significantly during CBGT (cognitive behavioral group therapy), b = 1.65, 95% CI [1.13, 2.17], t = 6.27, p < .001, and MBSR (mindfulness-based stress reduction), b = 1.50, 95% CI [0.98, 2.02], t = 5.69, p < .001. The session by group interaction was not significant, b = 0.15, 95% CI [−0.59, 0.89], t = 0.40, p = .69. Weekly perceived reappraisal success increased significantly during CBGT, b = 2.22, 95% CI [1.78, 2.67], t = 9.98, p < .001, and MBSR, b = 1.31, 95% CI [0.87, 1.75], t = 5.87, p < .001, with a significant session by group interaction indicating greater increases during CBGT (vs. MBSR), b = 0.91, 95% CI [0.29, 1.54], t = 2.89, p = .005.
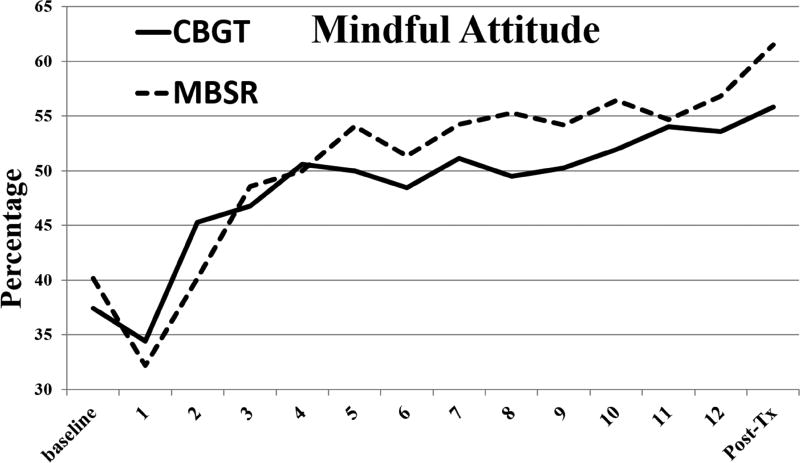
Mindfulness
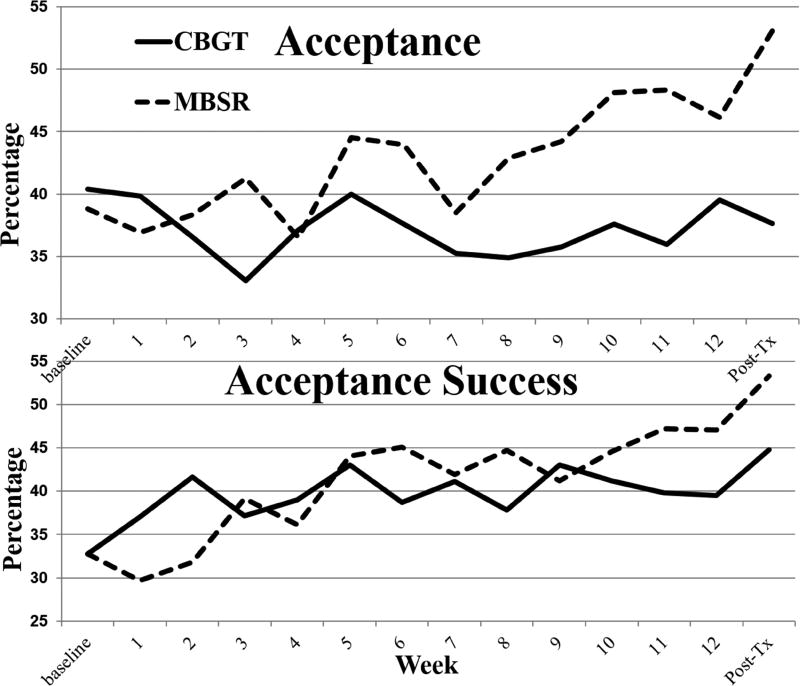
As shown in Table 5, MLM showed that weekly mindful attitude increased during both CBGT (49% increase from baseline to post-treatment) and MBSR (53% increase) (Figure 4), with no interaction of session by group. Acceptance of anxiety increased during MBSR (37% increase), but not during CBT (7% decrease) (Figure 5), with a significant interaction of group by session indicating greater increases in acceptance during MBSR. Acceptance success increased during MBSR (63% increase), but not during CBGT (37% increase). The session by group interaction was significant, indicating greater increases during MBSR. In summary, while both CBGT and MBSR produced increases in weekly mindful attitude, only MBSR produced increases in acceptance and acceptance success.
Table 5.
Multilevel Modeling Results for Mindfulness Indicators
| Mindful Attitude |
Acceptance of Anxiety |
Perceived Acceptance Success |
||||
|---|---|---|---|---|---|---|
| b | t | b | t | b | t | |
| Intercept | 24.89 | 3.82*** | 29.84 | 4.07*** | 30.07 | 3.99*** |
| Age | 0.42 | 2.22* | 0.22 | 1.06 | 0.08 | 0.36 |
| Session | 1.76 | 7.13*** | 1.16 | 3.75*** | 1.60 | 5.19*** |
| Group | 2.76 | 0.81 | 0.26 | 0.06 | 6.05 | 1.45 |
| Session × Group | −0.51 | −1.46 | −1.23 | −2.84** | −1.44 | −3.32** |
| Residuals | Wald Z | Wald Z | Wald Z | |||
| Level 1 | 168.04 | 21.79*** | 207.23 | 21.78*** | 209.80 | 21.76*** |
| Intercept | 241.00 | 5.72*** | 387.96 | 5.97*** | 375.33 | 5.91*** |
| Session | 1.91 | 4.38*** | 3.36 | 4.96*** | 3.33 | 4.89*** |
| Int/Session Covariance | −6.77 | −2.03* | −19.74 | −3.58*** | −16.59 | −3.11** |
| Model Fit | ||||||
| −2LL | 9581.81 | 9838.83 | 9857.54 | |||
| AIC | 9599.81 | 9856.83 | 9875.54 | |||
| BIC | 9645.28 | 9902.29 | 9921.00 | |||
Note: Group refers to CBGT (cognitive behavioral group therapy) vs. MBSR (mindfulness-based stress reduction). −2LL = −2 × log-likelihood, AIC = Akaike’s Information Criterion, BIC = Bayesian’s Information Criterion
p < .01,
p < .005,
p < .001
Figure 4. Mindful attitude during CBGT and MBSR.
Weekly mindful attitude increased during both CBGT (cognitive behavioral group therapy), b = 1.25, 95% CI [0.76, 1.74], t = 5.09, p < .001, and MBSR (mindfulness-based stress reduction), b = 1.76, 95% CI [1.27, 2.25], t = 7.13, p < .001, with no interaction of session by group, b = −0.51, 95% CI [−1.20, 0.18], t = −1.46, p = .15.
Figure 5. Acceptance and perceived acceptance success during CBGT and MBSR.
Acceptance of anxiety increased during MBSR (mindfulness-based stress reduction), b = 1.16, 95% CI [0.55, 1.77], t = 3.75, p < .001, but not in CBGT (cognitive behavioral group therapy), b = −0.08, 95% CI [−0.69, 0.53], t = −0.25, p = .80, with a significant interaction of group by session indicating greater increases in acceptance during MBSR, b = −1.23, 95% CI[−2.10, −0.37], t = −2.84, p = .006. Perceived acceptance success did not change during CBGT, b = 0.16, 95% CI [−0.45, 0.76], t = 0.51, p = .61, but did increase during MBSR, b = 1.60, 95% CI [0.99, 2.21], t = 5.19, p < .001. The session by group interaction was significant, indicating greater increases during MBSR, b = −1.44, 95% CI [−2.31, −0.58], t = −3.32, p = .001.
Hypothesis 3: Weekly Reappraisal and Mindfulness Predicting Social Anxiety Reduction
Reappraisal
Using Granger Causality lead-lag analysis of time series data and a criterion p-value of .05, as shown in Table 6, during CBGT increases in weekly reappraisal predicted subsequent decreases in weekly social anxiety. The inverse relationship, namely, weekly social anxiety predicting subsequent weekly reappraisal, was not significant, F(2,11) = 0.63, p > .05, ΔR2 = .01, indicating a unidirectional relationship. During MBSR, increases in weekly reappraisal did not predict subsequent decreases in weekly social anxiety, F(2,11) = 1.86, p > .05, ΔR2 = .01. The inverse relationship was also not significant, F(2,11) = 0.93, p > .05, ΔR2 = .01
Table 6.
Granger Causality Time Series Analysis of Weekly Cognitive Reappraisal and Mindfulness Predicting Subsequent Weekly Social Anxiety Intensity During CBGT and MBSR
| Predictor | F, ΔR2 | b, SE of b, 95% CI | β, t |
|---|---|---|---|
| CBT-related Processes | |||
| Reappraisal | |||
| CBGT | 4.95*, .03 | −.70, .33,[−1.44, .04] | −.46, 2.12 |
| MBSR | 1.86, .01 | −.32, .25, [−.87, .23] | −.21, 1.30 |
| Perceived Reappraisal Success | |||
| CBGT | 4.52*, .03 | −.50, .25, [−1.-5, .05] | −.42, 2.03 |
| MBSR | 1.54, .01 | −.37, .31, [−1.05, .32] | −.22, 1.19 |
| Disputing | |||
| CBGT | 3.76, .03 | −.64, .34, [−1.40, .13] | −.38, 1.85 |
| MBSR | 8.13*, .03 | −.57, .21, [−1.03, −.10] | −.23, 2.72* |
| MBSR-related Processes | |||
| Mindful Attitude | |||
| CBGT | 2.47, .02 | −.59, .40, [−1.47, .29] | −.29, 1.50 |
| MBSR | 4.89*, .02 | −.57, .27, [−1.16, .03] | −.46, 2.11 |
| Acceptance | |||
| CBGT | 1.16, .01 | −.53, .52, [−1.70, .63] | −.10, 1.03 |
| MBSR | 1.51, 009 | −.23, .20, [−.66, .21] | −.12, 1.17 |
| Perceived Acceptance Success | |||
| CBGT | 1.14, .010 | −.47, .46, [−1.49, .55] | −.10, 1.10 |
| MBSR | 2.77, .014 | −.36, .23, [−.86, .14] | −.25, 1.59 |
Note: F-value tests the additional variance explained (ΔR2) when adding the predictor variable after controlling for the one-lag autoregression model AR(1) and has degrees of freedom (2,11). b = unstandardized beta, β = standardized beta, SE = standard error, CI = confidence interval.
p < .05,
p < .01,
p < .001
During CBGT, increases in weekly reappraisal success predicted subsequent decreases in weekly social anxiety. The inverse relationship was not significant, F(2,11) = 0.58, p > .05, ΔR2 = .01. During MBSR, weekly reappraisal success did not predict subsequent decreases in weekly social anxiety, and inverse relationship was also not significant, F(2,11) = 2.96, p > .05, ΔR2 = .01.
During CBGT, increases in weekly disputing did not predict subsequent decreases in weekly social anxiety. The inverse relationship was also not significant, F(2,11) = 1.22, p > .05, ΔR2 = .02. During MBSR, increases in weekly disputing predicted subsequent decreases in weekly social anxiety, and the inverse relationship was not significant, F(2,11) = 0.12, p > .05, ΔR2 = .01.
In summary, the Granger Causality analysis showed that 2 of 3 cognitive reappraisal indicators during CBGT and one cognitive reappraisal indicator during MBSR predicted subsequent social anxiety reduction during treatment.
Mindfulness
During CBGT, weekly changes in mindful attitude did not predict subsequent decreases in weekly social anxiety. However, the inverse relationship was significant, F(2,11) = 7.17, p < .05, ΔR2 = .13, unstandardized b = −.56, SE of b = .22, 95% CI [−1.06, −.07], standardized β = −.78, t(11) = 2.55, p = .029. During MBSR, weekly changes in mindful attitude predicted subsequent decreases in weekly social anxiety. The inverse relationship was also significant, F(2,11) = 4.41, p < .05, ΔR2 = .09, unstandardized b = −1.01, SE of b = .51, 95% CI [−2.15, .11], standardized β = −.93, t(11) = 2.00, p = .07, suggesting a bi-directional relationship.
Weekly changes in acceptance did not predict subsequent decreases in weekly social anxiety during CBGT, F(2,11) = 1.16, p > .05, ΔR2 = .01, and the inverse relationship was not significant during CBGT, F(2,11) = 1.86, p > .05, ΔR2 = .03. During MBSR, weekly changes in acceptance did not predict subsequent decreases in social anxiety, F(2,11) = 1.51, p > .05, ΔR2 = .01, and the inverse relationship was not significant, F(2,11) = 3.34, p > .05, ΔR2 = .15
Weekly changes in acceptance success did not predict subsequent decreases in weekly social anxiety during CBGT, F(2,11) = 1.16, p > .05, ΔR2 = .01, and the inverse relationship was not significant, F(2,11) = 0.34, p > .75, ΔR2 = .01. During MBSR, acceptance success did not predict subsequent decreases in weekly social anxiety, F(2,11) = 2.77, p > .05, ΔR2 = .01. However, the inverse relationship was significant, F(2,11) = 5.40, p > .05, ΔR2 = .12.
In summary, the Granger Causality analysis showed that none of the mindfulness indicators during CBGT and only one mindfulness indicator during MBSR predicted subsequent social anxiety reduction during treatment.
DISCUSSION
The goal of this study was to investigate the effects of CBGT vs. MBSR on the weekly trajectories of social anxiety, cognitive reappraisal, and mindfulness over 12 weeks in adults with generalized SAD. CBGT and MBSR produced similar trajectories of decreasing social anxiety. There were greater increases for CBGT (vs. MBSR) in the trajectories of 2 of 3 indicators of reappraisal (disputing and reappraisal success), and greater increases for MBSR (vs. CBGT) in the trajectories of 2 of 3 indicators of mindfulness (acceptance and acceptance success). Granger Causality lead-lag time series analysis demonstrated that different indicators of weekly cognitive reappraisal predicted subsequent decreases in weekly social anxiety during CBGT (reappraisal, and reappraisal success) and MBSR (disputing). One indicator of weekly mindfulness (mindful attitude) predicted subsequent decreases in weekly social anxiety during MBSR (but not CBGT).
Trajectory of Social Anxiety during CBGT and MBSR
In support of Hypothesis 1, CBGT and MBSR resulted in similar trajectories of decreasing social anxiety during 12 weeks of treatment. No prior studies have examined the weekly trajectories of social anxiety in CBT and MBSR. The single study that directly compared CBGT (n = 27) to MBSR (n = 26) in patients with SAD (Koszycki et al., 2007) found comparable pre-to-post-treatment improvement in mood, functioning, and quality of life, and, importantly, greater improvement for CBGT vs. MBSR in social anxiety, response rates and remission rates. Another study that compared CBGT with a mindfulness and acceptance-based group therapy found similar pre-to-post-treatment improvement on social anxiety (Kocovski et al., 2013). Thus, the available data are mixed with regard to whether CBGT and MBSR produce similar reductions of social anxiety symptoms. This study extends the two prior studies by demonstrating that the temporal patterns of change in social anxiety measured weekly during treatment is similar for CBGT and MBSR.
The Role of Cognitive Reappraisal in CBGT and MBSR
To investigate underlying psychological processes that might explain how CBGT and MBSR work, we examined the weekly trajectories of multiple indicators of cognitive reappraisal and mindfulness. We found partial support for Hypothesis 2 in the analyses of cognitive reappraisal-related variables. Compared to MBSR, CBGT led to greater increases in the weekly trajectories of disputing and reappraisal success. These findings align with the CBT emphasis on training cognitive restructuring of maladaptive thoughts and interpretations that trigger anxiety. Furthermore, repeated within-session and in vivo exposures to feared situations during CBT provide the opportunity to experience reappraisal success and self-efficacy. CBT-related increases in cognitive reappraisal processes have been observed in prior studies of patients with SAD (Goldin et al., 2014; Goldin et al., 2012b). The similar increases in response to “how often did you try to change the way you were thinking about the situation you were in?” (i.e., reappraisal) may be related to enhancement of perspective taking, awareness of patterns of thoughts and emotions, and reduction in maladaptive cognitive elaborations and interpretations during both CBGT and MBSR. Observing one’s own mental habits from multiple perspectives and learning how to modulate the relationships between thought, emotion and behavior may be common processes in both CBT and MBSR.
Interestingly, both CBGT and MBSR yielded significant increases in all three indicators of cognitive reappraisal. This is not surprising for CBT given its explicit focus on training reappraisal in the context of fear exposure. This might, however, be an unexpected result for MBSR, at least at first glance. However, Garland and colleagues (Garland, Farb, Goldin, & Fredrickson, 2015) recently introduced a mindfulness-to-meaning theory (MMT) that suggests mindfulness meditation practice will facilitate reappraisal of adversity and savoring of positive experience by enhancing interoceptive attention and cognitive flexibility. MMT predicts that mindfulness meditation training should increase the ability to implement a variety of emotion regulation strategies, including reappraisal, attention deployment, and acceptance. Two studies have found increases in the ability to implement attention deployment emotion regulation strategies following MBSR for SAD, specifically, for participant-generated negative self-beliefs embedded in autobiographical social anxiety related situations (Goldin & Gross, 2010; Goldin, Ziv, Jazaieri, Hahn, & Gross, 2013a). Thus, our findings confirm the expected impact of CBGT on cognitive reappraisal and suggest that MBSR also may increase cognitive reappraisal ability and implementation. These findings support the view that there may be some shared mechanisms of change for CBT and MBSR.
The Role of Mindfulness in CBGT and MBSR
For mindfulness related variables, our Hypothesis 2 was partially supported. Both CBGT and MBSR produced similar weekly increases in mindful attitude, which was characterized as an open, curious and willing attitude toward one’s own anxiety-related thoughts and feelings. This is a surprising result for CBGT, but expected for MBSR. One explanation is that during CBGT reappraisal skills increase, anxiety decreases, and these changes may disinhibit latent mindfulness skills and attitudes that had been chronically suppressed in patients with SAD. A similar perspective may explain why MBSR, a program of training that does not explicitly train cognitive reappraisal, indirectly scaffolds emotion regulation abilities that may be suppressed by chronic anxiety and low self-efficacy in SAD patients. It is important to note that traditional Buddhist models characterize mindfulness meditation training as a set of tools for enhancing mental qualities, skills and attitudes that already exist in human beings but require enhancement and refinement (Thera, 1998). Thus, the observation of increases in reappraisal processes during MBSR and increases in mindfulness skills during CBT may help explain why recent randomized controlled comparisons of CBT to other mindfulness and acceptance based interventions, such as Acceptance and Commitment Therapy (Craske et al., 2014) and Mindfulness and Acceptance-based Group Therapy (Kocovski et al., 2013) have produced similar results (i.e., social anxiety symptom reduction) in patients with SAD.
However, under the rubric of mindfulness, there are a variety of practices that likely impact different types of mindfulness skills and attitudes. When we examined the more specific constructs of acceptance of anxiety (an emotion regulation strategy) and acceptance success (a meta-cognitive perspective), we found significant group effects, which were demonstrated in weekly increases during MBSR and no change during CBGT. However, the percentage increase in acceptance during MBSR and CBGT was much lower than for any of the other mindfulness variables. This may be due to acceptance of emotion being difficult to do and being unfamiliar in patients with SAD. In the case of CBGT, there is no training in acceptance of emotion. In contrast, MBSR explicitly trains decentering via merely observing mental phenomenon while reducing reactivity, elaboration and identification with those phenomenon.
More broadly, acceptance of experience may be viewed as an emotion regulation strategy that may incorporate aspects of cognitive reappraisal, at least initially, and then may differ more when the individual begins to implement acceptance more spontaneously rather than volitionally. Furthermore, as mentioned earlier, some models (i.e., MMT) predict that mindfulness meditation training should increase the ability to implement cognitive reappraisal. This suggests a synergistic relationship between mindfulness skills (e.g., acceptance) and cognitive reappraisal. However, the specifics of this relationship, for example, the degree of trait overlap, temporal precedence during training, and differential prediction of training outcome, and clinical status, remains to be investigated.
In CBT, cognitive reappraisal refers to volitional attempts to change emotional experience by means of active reinterpretation of maladaptive thoughts. In contrast, in the context of MBSR, acceptance involves allowing emotional experience to arise, change and dissipate naturally with no volitional effort to change emotion. The importance of acceptance as an emotion regulation strategy has been established in prior research. A cross-sectional study in a community sample demonstrated that acceptance of emotion is implemented to a greater extent across different situations than any other emotion regulation strategy, including cognitive reappraisal, and negatively predicted psychopathology (Aldao & Nolen-Hoeksema, 2012). Our study shows the effects of MBSR on the weekly trajectory of acceptance frequency and perceived successful implementation during MBSR. Thus, acceptance of anxiety appears to be a distinctive feature of MBSR for SAD that differentiates it from CBT for SAD.
The Clinical Impact of Changes in Reappraisal and Mindfulness
We examined whether changes in the trajectories of reappraisal and mindfulness predicted subsequent changes in social anxiety using Granger Causality lead-lag analyses. We found partial support for Hypothesis 3, with prior increases in 2 of 3 weekly reappraisal indicators (reappraisal, reappraisal success) predicting subsequent decreases in social anxiety during CBGT (but not during MBSR), and increases in 1 of 3 weekly mindfulness indicators (mindful attitude) predicting subsequent decreases in social anxiety during MBSR (but not during CBGT). The reappraisal prediction of social anxiety was unidirectional, suggesting that prior reductions in social anxiety did not predict subsequent increases in any of the three indicators of reappraisal. These predictive relationships identify distinctive potential mechanisms of social anxiety reduction that are consistent with models of CBT that pinpoint increases in cognitive reappraisal and with models of MBSR that highlight increases in mindful orientation toward experience, specifically, a mindful, open, curious, and willing attitude. These results support the view that prior cognitive (and perhaps meta-cognitive) changes may be related to subsequent improvement in clinical outcomes.
However, a surprising apparent inconsistency that contradicts current conceptualization of MBSR is that increases in weekly disputing or challenging your anxious thoughts and feelings predicted subsequent decreases in weekly social anxiety during MBSR, but not during CBGT. Disputing or challenging anxious thoughts was practiced in the context of exposures which did not start until week 3 during CBGT. However, weekly social anxiety began to decrease before exposure sessions started. This may partially explain why weekly disputing did not predict subsequent social anxiety during CBGT. In contrast, during MBSR, patients begin learning and implementing mindfulness practices from the very first session. Although smaller than CBGT, there was a significant increase in disputing during MBSR. Thus, the impact of weekly mindfulness training and the concomitant increase in acceptance and reappraisal during MBSR may enhance the capacity to dispute anxious thoughts and feelings. These findings both support and contradict our current conceptualization of how we expect MBSR to work. Perhaps a necessary extension of mechanisms of change during MBSR training is that, as a mindful attitude towards mental experience and physical sensations in general and anxiety more specifically increases, it may facilitate many different forms of emotion regulation such as cognitive reappraisal (i.e., re-interpreting the meaning of thoughts and interpretation), disputing anxiety inducing thoughts (i.e., challenging and debating maladaptive beliefs), and so forth. Such an interpretation is in alignment with mindfulness-to-meaning theory (Garland et al., 2015), which proposes increases in emotion regulation as an important sequela of mindfulness training. If enhancement of emotion regulation ability is a reliable result of MBSR, then this may help explain the similar decrease and maintenance of social anxiety immediately and 1-year post-CBT and post-MBSR in this sample of patients with SAD (Goldin et al., 2016).
We also found that prior decreases in social anxiety predicted subsequent increases in mindful attitude during both CBGT and MBSR, and subsequent increases in acceptance success during MBSR only. This suggests the hypothesis that social anxiety inhibits the experience of a mindful, open, curious, and willing attitude toward mental phenomena, and meta-cognitive awareness of the ability to implement acceptance. Implementation of mindfulness skills may be less effortful than cognitive reappraisal, and thus the access to cognitive resources and executive functioning afforded by even small reductions in social anxiety impact mindfulness skills more easily relative to cognitive reappraisal strategies.
Limitations and Directions for Future Research
Findings from this study elucidate the trajectories of change in cognitive reappraisal and mindfulness and their predictive relationship to social anxiety reduction during CBGT and MBSR. However, the results are limited by the specific set of indicators that were used to measure weekly changes during treatment. More specifically, this study found evidence that prior changes in cognitive process (reappraisal, reappraisal success, mindful attitude) predicted subsequent reduction in social anxiety symptoms. However, we did not include weekly behavioral measures that might also change and predict clinical improvement. This is important because it is still not clear how weekly changes in cognitive relative to behavioral measures may independently or interactively predict clinical outcome.
Also, we do not know to what extent reflecting on and responding to the weekly questions influenced what participants chose to do in anxiety producing situations during CBGT and MBSR. It is possible that this set of weekly questions might have re-directed the patient’s attention to their experience and possibly modified subsequent behavior independently from the skills taught in CBGT and MBSR.
Future studies could examine a wider range of emotion regulation strategies (such as situation modification, expressive suppression, different types of attention deployment and cognitive change) and different features of mindfulness (such as decentering, self-identification, non-elaboration). Furthermore, differences in the meaning of what is being assessed by some of the weekly questions, for example, “try to change the way you were thinking” (cognitive change strategy of reappraisal) versus “adopting a mindful, open, curious, and willing attitude” (observing/noticing/accepting/allowing strategy) are subtle, and there is no guarantee that the participants in our study after 12 weeks of MBSR or CBGT did not cultivate and implement an alternative strategy. This non-differentiation of the meaning of weekly questions may have interfered with accurate responses.
Although this study focused on a single psychiatric group (patients with unmedicated generalized SAD), future studies would benefit from examining patients with different mood and anxiety disorders to determine whether the trajectories observed in this study generalize across psychiatric categories treated with CBT and MBSR. Another potential design choice that might be helpful would be to assess patients during the waitlist period at the same frequency as the treated groups in order to look at natural variability in the trajectories of anxiety, reappraisal and mindfulness. Although our study used weekly self-reported measures of change, future studies should consider (a) greater temporal resolution via daily measurements and (b) supplementing self-report with daily or weekly neural measures of emotion regulation and mindfulness skills collected with smartphone or mobile wireless EEG tools. Whereas our study examined the impact of CBT and MBSR on weekly reduction of social anxiety symptoms, future studies could add a focus on the trajectory of well-being in patients with anxiety disorders.
Supplementary Material
Highlights.
CBGT and MBSR produced similar decreases in social anxiety
CBGT (vs. MBSR): greater disputing anxiety and reappraisal success
CBGT: weekly reappraisal and reappraisal success predict social anxiety
MBSR (vs. CBGT): greater acceptance of anxiety and acceptance success
MBSR: weekly mindful attitude and disputing anxiety predict social anxiety
Acknowledgments
This research was supported by an NIMH Grant R01 MH076074, awarded to James Gross, Ph.D. Richard Heimberg, Ph.D. is the author of the commercially available CBT protocol which was utilized in this study. Philippe Goldin, Ph.D., who is independent of any commercial funder, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
ClinicalTrials.gov identifier: NCT02036658
PRG was involved with every aspect of this study and drafted the paper. HJ participated in the study design, data collection, and data management. AM participated in data collection, data management, and data analyses. RH participated in study design and paper revisions. JJG was involved in study design and paper revisions.
None of the authors of this manuscript have any biomedical financial interests or potential conflicts of interest.
Portions of this paper were presented at ABCT 2016.
References
- Acarturk C, de Graaf R, van Straten A, ten Have M, Cuijpers P. Social phobia and number of social fears, and their association with comorbidity, health-related quality of life and help seeking. Social Psychiatry and Psychiatric Epidemiology. 2008;43:273–279. doi: 10.1007/s00127-008-0309-1. [DOI] [PubMed] [Google Scholar]
- Acarturk C, Smit F, de Graaf R, van Straten A, ten Have M, Cuijpers P. Economic costs of social phobia: A population-based study. Journal of Affective Disorders. 2009;115:421–429. doi: 10.1016/j.jad.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. The influence of context on the implementation of adaptive emotion regulation strategies. Behaviour Research and Therapy. 2012;50:493–501. doi: 10.1016/j.brat.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, Vollebergh WA. Disability and quality of life impact of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica Supplement. 2004;s420:38–46. doi: 10.1111/j.1600-0047.2004.00329.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. [Google Scholar]
- Baer RA, Carmody J, Hunsinger M. Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2012;68:755–765. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Schneier FR, Okuda M, Liu SM, Heimberg RG. Predictors of persistence of social anxiety disorder: a national study. Journal of Psychiatric Research. 2011;45:1557–1563. doi: 10.1016/j.jpsychires.2011.08.004. doi:S0022-3956(11)00175-0/10.1016/j.jpsychires.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Boden MT, John OP, Goldin PR, Werner K, Heimberg RG, Gross JJ. The role of maladaptive beliefs in cognitive behavioral therapy: Evidence from social anxiety disorder. Behaviour Research & Therapy. 2012;50:287–291. doi: 10.1016/j.brat.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037/0021-843X.110.1.49. [DOI] [PubMed] [Google Scholar]
- Craske MG, Niles AN, Burklund LJ, Wolitzky-Taylor KB, Vilardaga JCP, Arch JJ, Lieberman MD. Randomized controlled trial of cognitive behavioral therapy and acceptance and commitment therapy for social phobia: Outcomes and moderators. Journal of Consulting and Clinical Psychology. 2014;82:1034–1048. doi: 10.1037/a0037212. doi:10.1037.a0037212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L) New York, NY: Oxford University Press; 1994. [Google Scholar]
- Gallagher MW, Payne LA, White KS, Shear KM, Woods SW, Gorman JM, Barlow DH. Mechanisms of change in cognitive behavioral therapy for panic disorder: The unique effects of self-efficacy and anxiety sensitivity. Behaviour Research and Therapy. 2013;51:767–777. doi: 10.1016/j.brat.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin P, Fredrickson BL. Mindfulness broadens awareness and builds eudaimonic meaning: A process model of mindful positive emotion regulation. Psychological Inquiry. 2015;26:293–314. doi: 10.1080/1047840x.2015.1064294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ziv M, Jazaieri H, Gross JJ. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: Effects on the self-referential brain network in social anxiety disorder. Frontiers in Human Neuroscience. 2012a;6:295. doi: 10.3389/fnhum.2012.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Jazaieri H, Ziv M, Kraemer H, Heimberg RG, Gross JJ. Changes in positive self-views mediate the effect of cognitive-behavioral therapy for social anxiety. Clinical Psychological Science. 2013a;1:301–310. doi: 10.1177/2167702613476867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ziv M, Jazaieri H, Hahn K, Gross JJ. MBSR vs aerobic exercise in social anxiety: fMRI of emotion regulation of negative self-beliefs. Social Cognitive Affective Neuroscience. 2013b;8:65–72. doi: 10.1093/scan/nss054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10:83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Lee I, Ziv M, Jazaieri H, Heimberg RG, Gross JJ. Trajectories of change in emotion regulation and social anxiety during cognitive-behavioral therapy for social anxiety disorder. Behaviour Research and Therapy. 2014;56:7–15. doi: 10.1016/j.brat.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2016;84:427–37. doi: 10.1037/ccp0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ramel W, Gross JJ. Mindfulness meditation training and self-referential processing in social anxiety disorder: Behavioral and neural effects. Journal of Cognitive Psychotherapy. 2009;23:242–257. doi: 10.1891/0889-8391.23.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ziv M, Jazaieri H, Werner K, Kraemer H, Heimberg RG, Gross JJ. Cognitive reappraisal self-efficacy mediates the effects of individual cognitive-behavioral therapy for social anxiety disorder. Journal of Consulting and Clinical Psychology. 2012b;80:1034–1040. doi: 10.1037/a0028555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon D, Wong J, Heimberg RG. The Wiley-Blackwell handbook of social anxiety disorder. New York: Wiley-Blackwell; 2014. Cognitive-behavioral therapy for social anxiety disorder: The state of the science. [Google Scholar]
- Granger C. Investigating Causal Relations by Econometric Models and Cross-spectral Methods. Econometrica. 1969;37(3):424–438. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 2011. [Google Scholar]
- Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York: Guilford Press; 2002. [Google Scholar]
- Heimberg RG, Hofmann SG, Liebowitz MR, Schneier FR, Smits JAJ, Stein MB, Craske MG. Social anxiety disorder in DSM-5. Depression and Anxiety. 2014;31:472–479. doi: 10.1002/da.22231. [DOI] [PubMed] [Google Scholar]
- Hoffart A, Borge FM, Sexton H, Clark DM. Change processes in residential cognitive and interpersonal psychotherapy for social phobia: A process-outcome study. Behavior Therapy. 2009;40:10–22. doi: 10.1016/j.beth.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive mediation of treatment change in social phobia. Journal of Consulting and Clinical Psychology. 2004;72:392–399. doi: 10.1037/0022-006X.72.3.392. doi.org/10.1037/0022-006X.72.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope D, Heimberg R, Turk C. Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach. 2. New York, NY: Oxford University Press; 2010. [Google Scholar]
- Hox JJ. Multilevel analysis: Techniques and applications. Majwah, New Jersey: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- Jazaieri H, Goldin PR, Werner K, Ziv M, Gross JJ. A randomized trial of mbsr versus aerobic exercise for social anxiety disorder. Journal of Clinical Psychology. 2012;68:715–731. doi: 10.1002/jclp.21863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living : using the wisdom of your body and mind to face stress, pain, and illness. New York, N.Y: Dell Publishing; 1990. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kleim B, Grey N, Wild J, Nussbeck FW, Stott R, Hackmann A, Ehlers A. Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81:383–393. doi: 10.1037/a0031290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocovski NL, Fleming JE, Hawley LL, Huta V, Antony MM. Mindfulness and acceptance-based group therapy versus traditional cognitive behavioral group therapy for social anxiety disorder: A randomized controlled trial. Behaviour Research and Therapy. 2013;51:889–898. doi: 10.1016/j.brat.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Kocovski NL, Fleming JE, Hawley LL, Ho MHR, Antony MM. Mindfulness and acceptance-based group therapy and traditional cognitive behavioral group therapy for social anxiety disorder: Mechanisms of change. Behaviour Research and Therapy. 2015;70:11–22. doi: 10.1016/j.brat.2015.04.005. http://dx.doi.org/10.1016/j.brat.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy. 2007;45:2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Salzer S, Beutel ME, Herpertz S, Hiller W, Hoyer J. Long-term outcome of psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder. American Journal of Psychiatry. 2014;171:1074–1082. doi: 10.1176/appi.ajp.2014.13111514. [DOI] [PubMed] [Google Scholar]
- McManus F, Clark DM, Hackmann A. Specificity of cognitive biases in social phobia and their role in recovery. Behavioural and Cognitive Psychotherapy. 2000;28:201–209. doi: 10.1017/S1352465800003015. [DOI] [Google Scholar]
- Mennin DS, Ellard KK, Fresco DM, Gross JJ. United we stand: emphasizing commonalities across cognitive-behavioral therapies. Behaviour Therapy. 2013;44:234–248. doi: 10.1016/j.beth.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles AN, Burklund LJ, Arch JJ, Lieberman MD, Saxbe D, Craske MG. Cognitive mediators of treatment for social anxiety disorder: comparing acceptance and commitment therapy and cognitive-behavioral therapy. Behaviour Therapy. 2014;45:664–677. doi: 10.1016/j.beth.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton AR, Abbott MJ, Norberg MM, Hunt C. A systematic review of mindfulness and acceptance-based treatments for social anxiety disorder. Journal of Clinical Psychology. 2015;71:283–301. doi: 10.1002/jclp.22144. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Maki KM, Gould RA, Worthington JJ, 3rd, Smoller JW, Rosenbaum JF. Childhood history of anxiety disorders among adults with social phobia: Rates, correlates, and comparisons with patients with panic disorder. Depression and Anxiety. 2001;14:209–213. doi: 10.1002/da.1068. [DOI] [PubMed] [Google Scholar]
- Patel A, Knapp M, Henderson J, Baldwin D. The economic consequences of social phobia. Journal of Affective Disorders. 2002;68:221. doi: 10.1016/S0165-0327(00)00323-2. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowitz MR, Cissell S, Hofmann SG. Screening for social anxiety disorder with the self-report version of the liebowitz social anxiety scale. Depression and Anxiety. 2009;26:34. doi: 10.1002/da.20503. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Rosenfield D, McDonald R, Telch MJ. Cognitive mechanisms of social anxiety reduction: An examination of specificity and temporality. Journal of Consulting and Clinical Psychology. 2006;74:1203–1212. doi: 10.1037/0022-006X.74.6.1203. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Rosenfield D, Powers MB. Threat reappraisal as a mediator of symptom change in cognitive-behavioral treatment of anxiety disorders: a systematic review. Journal of Consulting and Clinical Psychology. 2012;80:624–635. doi: 10.1037/a0028957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders TA, Bosker RJ. Introduction to multilevel analysis. Sage Publications; 1999. [Google Scholar]
- Stahl B, Goldstein E. A mindfulness-based stress reduction workbook. Oakland, CA: New Harbinger; 2010. [Google Scholar]
- Stein MB, Kean YM. Disability and quality of life in social phobia: Epidemiologic findings. American Journal of Psychiatry. 2000;157:1606–1613. doi: 10.1176/appi.ajp.157.10.1606. [DOI] [PubMed] [Google Scholar]
- Stein MB, Stein DJ. Social anxiety disorder. Lancet. 2008;371:1115–1125. doi: 10.1016/S0140-6736(08)60488-2. [DOI] [PubMed] [Google Scholar]
- Taylor CT, Alden LE. Self-related and interpersonal judgment biases in social anxiety disorder: changes during treatment and relationship to outcome. International Journal of Cognitive Therapy. 2008;1:125–137. doi: 10.1521/ijct.2008.1.2.125. [DOI] [Google Scholar]
- Teasdale JD, Segal Z, Williams JMG. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy. 1995;33:25–39. doi: 10.1016/0005-7967(94)E0011-7. [DOI] [PubMed] [Google Scholar]
- Thera S. The way of mindfulness: the satipatthana sutta and its commentary. Kandy: Buddhist Publication Society; 1998. [Google Scholar]
- Wittchen HU, Stein MB, Kessler RC. Social fears and social phobia in a community sample of adolescents and young adults: prevalence, risk factors and co-morbidity. Psychological Medicine. 1999;29:309–323. doi: 10.1017/s0033291798008174. [DOI] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, Zimmermann M, Arch JJ, De Guzman E, Lagomasino I. Has evidence -based psychosocial treatment for anxiety disorders permeated usual care in community mental health settings? Behaviour Research and Therapy. 2015;72:9–17. doi: 10.1016/j.brat.2015.06.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.