Metastatic pulmonary calcification, commonly seen in patients on dialysis, is caused by deposition of calcium salts
A 64-year-old man with end-stage renal disease was evaluated in the pulmonary clinic for persistent abnormalities on axial computed tomography (CT) of the chest. He was a lifelong nonsmoker and had no history of exposure to occupational dust or fumes. His oxygen saturation was 100% on room air, and he denied any respiratory symptoms.
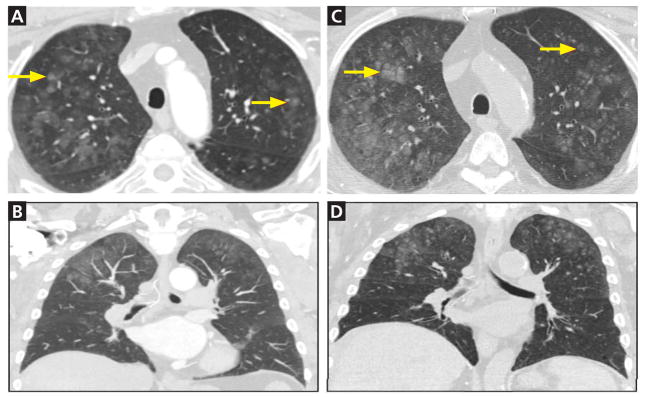
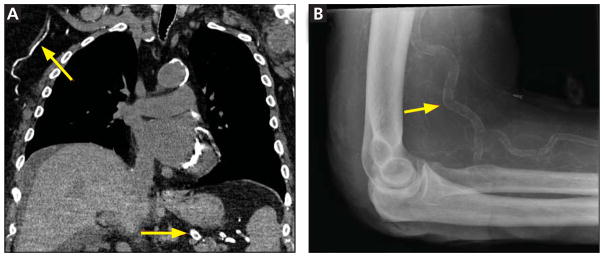
CT of the chest 1 year earlier had demonstrated bilateral ground-glass opacities predominantly in the upper lobes, findings confirmed by the results of CT done shortly before this clinic visit (Figure 1). CT and plain radiography also both showed extensive vascular calcification (Figure 2).
FIGURE 1.
Axial computed tomography of the chest 1 year before this clinic visit (A and B) and again shortly before this visit (C and D) showed ground-glass nodules (arrows) bilaterally and predominantly in the upper lobes.
FIGURE 2.
Computed tomography with coronal reconstruction showed densely calcified vessels (arrows), as did plain radiography of the elbow.
Results of pulmonary function testing were normal. The calcium-phosphorus product had been elevated for many years, and the most recent value was 67 mg2/dL2 (reference range < 55). The parathyroid hormone level was elevated at 200 pg/mL (15–65), and the 25-hydroxyvitamin D was low at 18 ng/mL (30–80), findings consistent with secondary hyperparathyroidism.
WHEN TO CONSIDER METASTATIC PULMONARY CALCIFICATION
The differential diagnosis for chronic upper-lobe-predominant ground-glass nodules is broad and includes atypical infections, recurrent alveolar hemorrhage, hypersensitivity pneumonitis, vasculitis, sarcoidosis, chronic eosinophilic pneumonia, occupational lung disease, and pulmonary alveolar microlithiasis. However, several aspects of our patient’s case suggested an often overlooked diagnosis, metastatic pulmonary calcification.
Metastatic pulmonary calcification is caused by deposition of calcium salts in lung tissue and is most commonly seen in patients on dialysis,1,2 and our patient had been dependent on dialysis for many years. The chronically elevated calcium-phosphorus product and secondary hyperparathyroidism often seen with end-stage renal disease may explain this association.
Our patient’s lack of symptoms is also an important diagnostic clue. Unlike many other causes of chronic upper-lobe-predominant ground-glass nodules, metastatic pulmonary calcification does not usually cause symptoms and is often identified only at autopsy.3 Results of pulmonary function testing are often normal.4
Metastatic pulmonary calcification can appear as diffusely calcified nodules or high-attenuation areas of consolidation on CT. However, as in our patient’s case, CT may demonstrate fluffy, centrilobular ground-glass nodules due to the microscopic size of the deposited calcium crystals.1 Identifying calcified vessels on imaging supports the diagnosis.4
In metastatic pulmonary calcification, the results of pulmonary function testing are often normal
Treatment of metastatic pulmonary calcification in a patient with end-stage renal disease is focused on correcting underlying metabolic abnormalities with phosphate binders, vitamin D supplementation, and dialysis.
Acknowledgments
The authors’ work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under K08 HL128867 (BDS), as well as by the Parker B. Francis Research Opportunity Award (BDS).
Contributor Information
JAMES M. WALTER, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL.
MARION STANLEY, Division of Hospital Medicine, Department of Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL.
BENJAMIN D. SINGER, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL.
References
- 1.Chan ED, Morales DV, Welsh CH, McDermott MT, Schwarz MI. Calcium deposition with or without bone formation in the lung. Am J Respir Crit Care Med. 2002;165:1654–1669. doi: 10.1164/rccm.2108054. [DOI] [PubMed] [Google Scholar]
- 2.Beyzaei A, Francis J, Knight H, Simon DB, Finkelstein FO. Metabolic lung disease: diffuse metastatic pulmonary calcifications with progression to calciphylaxis in end-stage renal disease. Adv Perit Dial. 2007;23:112–117. [PubMed] [Google Scholar]
- 3.Conger JD, Hammond WS, Alfrey AC, Contiguglia SR, Stanford RE, Huffer WE. Pulmonary calcification in chronic dialysis patients. Clinical and pathologic studies. Ann Intern Med. 1975;83:330–336. doi: 10.7326/0003-4819-83-3-330. [DOI] [PubMed] [Google Scholar]
- 4.Belem LC, Zanetti G, Souza AS, Jr, et al. Metastatic pulmonary calcification: state-of-the-art review focused on imaging findings. Respir Med. 2014;108:668–676. doi: 10.1016/j.rmed.2014.01.012. [DOI] [PubMed] [Google Scholar]