Abstract
Objective
Adaptive social functioning is severely impeded in depressive and anxiety disorders, even after remission. However, a comprehensive overview is still lacking.
Method
Using data from the Netherlands Study of Depression and Anxiety (NESDA), behavioural (network size, social activities, social support) and affective (loneliness, affiliation, perceived social disability) indicators of social functioning were analyzed in patients with anxiety (N = 540), depressive (N = 393), comorbid anxiety and depressive disorders (‘comorbid’, N = 748), remitted participants (N = 621), and healthy control subjects (N = 650).
Results
Analyses revealed an increasing trend of social dysfunction among patient groups, in patients with comorbid anxiety and depressive disorders, showing the most severe impairments, followed by depressed and anxious patients (P's < 0.001 for all social functioning indicators). Affective indicators showed the largest effect sizes (Cohen's d range from 0.13 to 1.76). We also found impairments in social functioning among remitted patients. Furthermore, perceived social disability among patients was predictive of still having a depressive and/or anxiety diagnosis 2 years later (P < 0.01).
Conclusions
Behavioural but especially affective indicators of social functioning are impaired in patients with anxiety or depressive disorders and most in patients with comorbid disorders. After remission of affective psychopathology, residual impairments tend to remain, while social dysfunction in patients seems predictive of future psychopathology.
Keywords: depression, anxiety, social functioning
Significant outcomes.
Social functioning is affected in patients with anxiety disorders, even more so in those with depressive disorders, and most prominently in patients with comorbid anxiety and depressive disorders.
Even after complete remission of affective psychopathology, residual impairments tend to remain.
Perceived social disability among patients is predictive of still having a depressive and/or anxiety diagnosis two years later.
Limitations.
Most of our analyses were cross‐sectional, thereby not allowing causal inferences.
More detailed aspects of social functioning, such as the exact composition of the social network, were not examined in our study.
Differences between our findings and previous findings might stem from the use of different measures of symptomatology and social functioning. Ideally, one would have used actual behavioural data, instead of retrospective self‐reports.
Introduction
Adequate social functioning is imperative for human wellbeing and survival 1, as is reflected by the severe health outcomes associated with social dysfunction, ranging from cardiovascular diseases to increased mortality rates 2, 3, 4. The influence of social functioning on premature mortality is believed to be higher than that of smoking, alcohol consumption, or obesity 3. Not only is social functioning essential for human wellbeing and survival, it is typically one of the main areas severely affected in common psychiatric disorders, such as depression and anxiety.
Social functioning can be studied in various manners, and little consensus exists on how to best describe it 5. In recent reviews 5, 6, 7, a multidimensional definition is proposed that includes both ‘behavioural’ and ‘affective’ indicators of social functioning. Behavioural indicators represent objective and quantitative measures of social function 5, including social network size, frequency of social activities, and frequency of perceived social support. Affective indicators, on the other hand, reflect more subjective and evaluative measures of interpersonal and socio‐emotional functioning 8 and include features such as loneliness, affiliation, and perceived social disability,
Overall, findings on social functioning in depression seem to suggest that affective indicators are more persistently affected compared to the behavioural indicators 6. Santini et al. 6 showed that perceived support (affective indicator) was more important for social functioning in depression than received support (behavioural indicator), and increased levels of perceived support played a protective role in depression onset. In addition, Cacioppo et al. 8 indicated that loneliness increases the risk for depression. Generally, when compared to healthy controls, patients with anxiety disorders have a lower quality of life especially in the areas of social interactions and subjective wellbeing 9. With regard to comparing social functioning between different anxiety disorders, findings are not unequivocal. McKnight et al. 10 showed that anxiety disorders such as agoraphobia and generalized anxiety disorder (GAD) have a stronger association with social isolation than social phobia (SP). This is in contrast to findings that GAD, SP, and panic disorder (PD) did not differ in the amount of social impairment 11 or to the finding that PD was most impaired in social functioning in comparison to other anxiety disorders 12.
In an estimated 50–70% of the patients, anxiety and depression tend to co‐occur (i.e., comorbidity) 13, 14, most likely as a result of common underlying pathophysiological processes 15. When these disorders co‐occur, the chronicity and functional impairments rise substantially 16, 17, 18. Yet, even though social dysfunction is among the most pervasive and debilitating symptoms of affective psychopathology and tends to persist long after remission, a thorough examination of social functioning in clinically anxious or depressed patients, as well in those presenting comorbidity and those in remission, is currently lacking 19, 20, 21, 22.
Aims of the study
Impairments of social functioning are typically examined separately for depressive and anxiety disorders, thereby not providing a comprehensive examination of differences and commonalities in social functioning in these disorders. We addressed this important issue, by comparing social functioning indices across five large groups of participants, including patients with either pure depression or anxiety disorders, as well as their combination (comorbid), along with remitted patients and healthy control participants. First, we examined to what extent various behavioural and affective indicators of social functioning are affected in patients with depression, anxiety, or comorbid disorders, as compared to healthy controls. Second, we examined to what extent these aspects of social functioning were still impaired in individuals remitted from these disorders. Third, we examined how clinical characteristics such as type of disorder (depression, panic, social phobia, or generalized anxiety disorder), severity, age of onset, and duration of disorder are associated with the level of social functioning. Fourth, we examined whether social dysfunction among patients is predictive of still having a clinical diagnosis of anxiety or depression after 2 years.
Material and methods
Study sample
Data for the current study were derived from the ongoing Netherlands Study of Depression and Anxiety (NESDA). NESDA is a longitudinal naturalistic cohort study, set up to provide more insight into the long‐term course and consequences of depression and anxiety disorders. Recruited between September 2004 and February 2007, a total of 2981 participants were enrolled from community care, primary care, and specialized mental health care from three regions in the Netherlands. The study includes individuals without lifetime psychiatric disorders (‘control subjects’) and participants with current or remitted depressive and anxiety disorders or comorbid anxiety and depressive disorders. Not speaking Dutch language and the presence of clinically overt primary psychiatric disorders (e.g. obsessive–compulsive, psychotic, bipolar, or severe addictive disorders) that might interfere with NESDA's main aim to examine etiology and course of common depressive and anxiety disorders were exclusion criteria.
The study was approved by the Ethics Review Board of the VU University Medical Centre Amsterdam and by the local review boards of all participating centers. All participants gave their verbal and written informed consent. A more detailed description of NESDA is described elsewhere 23. We excluded 29 participants for whom no information on social functioning was available. Thus, baseline data from 2952 participants were used for cross‐sectional analyses. Clinical follow‐up data after 2 years were available for 1409 of the 1681 (84%) patients with a current disorder at baseline.
Measurements
Depressive and anxiety disorders
The DSM‐IV Composite Interview Diagnostic Instrument (CIDI; WHO version 2.1) was used to diagnose major depressive disorder (MDD) and anxiety disorders [panic disorder (PD), social phobia (SP), generalized anxiety disorder (GAD), agoraphobia (AP)]. Based on the CIDI information, all 2952 respondents were categorized into one of five groups. The first group included healthy participants who have no current and past history of psychiatric disorders (‘control subjects’, N = 650). The second group included participants who have had a depressive or anxiety disorder during lifetime, but did not have this diagnosis in the last 6 months (‘remitted’, N = 621). The third and fourth group consisted of patients with diagnosis of either anxiety (‘pure anxiety’, N = 540) or depressive (‘pure depression’, N = 393) disorder in the last 6 months. The final group included participants with a comorbid anxiety and depressive disorder in the last 6 months (‘comorbid anxiety and depression’, N = 748).
Clinical characteristics
The earliest age of onset of disorders was determined using the CIDI. The Inventory of Depressive Symptoms‐Self‐Report (IDS) 24 was used to assess severity of depressive symptoms in the past week. The Beck Anxiety Index (BAI) 25 was used to assess severity of anxiety symptomatology. The Fear Questionnaire (FQ) measured severity of avoidance behaviour 26. The Life Chart method 27 provided more insight into the duration of symptoms in the past 4 years, estimated by dividing the duration of symptoms (number of affected months) by total number of follow‐up month. Course of disorder was additionally measured by the CIDI at the 2‐year follow‐up assessment. Current antidepressant use and psychotherapy (defined as having >1 contact with psychologist, social psychiatric nurse, or social worker in last 6 months) were determined by routine questioning.
Behavioural indicators of social functioning
We assessed network category, social activity status, and received social support as behavioural indicators of social functioning. Network category was operationalized as the number of adults with whom the participant has a regular and important contact. The answer is given on a six‐point scale; 1 (0 or 1 individuals in network), 2 (2–5 individuals), 3 (6–10 individuals), 4 (11–15 individuals), 5 (16–20 individuals), and 6 (>20 individuals in network). The social activity status is a self‐report regarding the frequency of visiting five different social activities (cultural events, trips to nature, visiting restaurants, social meetings, outdoor sport activities), ranging from almost never 1 to several times per week 6. A sum score was calculated adding up the frequency of conducting these five social activities, ranging from 5 to 30. The Close Persons Questionnaire (CPQ) measured the amount of received social support 28, 29. Participants answered ten questions about their partner and a maximum of two confidants. We calculated sum scores per partner or confidant, which were then recalculated into one mean social support score. For participants whom reported not to have a first (n = 662) or second (N = 543) confident, questions were scored as 0.
Affective indicators of social functioning
We assessed loneliness, affiliation, and perceived social disability as affective indicators of social functioning. The de Jong Gierveld loneliness scale 30 describes feelings of loneliness with 11 questions. Affiliation, in other words the perceived connection with others, was measured using the 6‐item self‐report ‘need for affiliation’ scale 31. Perceived social disability was measured using the 5‐item social interaction subscale from the World Health Organization Disability Assessment Schedule (WHO‐DAS), which includes questions about difficulties in making new or maintaining friendships 32.
Statistical analyses
Demographic and clinical characteristics were described and compared using chi‐square for dichotomous variables and analysis of variance (anova) for continuous variables. The independent Kruskal–Wallis test was used as nonparametric test when assumptions for parametric testing were not met. Spearman correlations described associations between social functioning indicators. Analyses of covariance (ancovas) adjusted for sex, age, years of education, and partner status (having a partner or not) probed for between‐groups differences in behavioural and affective indicators of social functioning. Effect sizes were estimated by calculating Cohen's d, comparing clinical groups to healthy controls. To examine the association of clinical characteristics (type of disease, severity, age of onset, duration) with behavioural and affective indicators of social functioning, multiple linear regression analyses in the subgroup of patients with a current disorder were conducted. Different disorders were coded using dummy variables in the linear regression model; this allowed us to eliminate the shared variance between disorder types.
Finally, within current patients of which we had longitudinal data (N = 1409), we conducted logistic regression analyses to examine whether social functioning indices at baseline were predictive of the presence of (still) having an affective disorder at two‐year follow‐up corrected for covariates (age, sex, educational level, partner status, and in a next model also severity of depression and anxiety). Statistical analyses were conducted using spss (IBM, version 22.0, IBM Corp., Armonk, NY, USA), and a two‐tailed significance level of P < 0.05 was considered statistically significant.
Results
The mean age of the study sample (N = 2952) was 41.9 years (SD = 13.1), and 66.4% were females (Table 1). Controls had a higher level of education and more often a partner than patients. As expected, groups differed significantly in all psychiatric characteristics, with the comorbid group showing the highest scores on all severity measures. Correlation analyses across all subjects revealed strong interrelations between social functioning indices (see Table S1). In brief, affective social functioning measures such as loneliness and perceived social disability were highly correlated with each other (r = 0.55), but correlations with affiliation were slightly lower (r = −0.32 for loneliness; r = −0.23 for perceived disability). Affective social functioning indices were significantly correlated with behavioural indices (network size, social activities, and social support) with correlations ranging between r = 0.13 (affiliation and network size) and r = −0.40 (loneliness and network size).
Table 1.
Baseline characteristics (N = 2952)
| Control subjects N = 650 | Remitted anxiety or depression N = 621 | Pure anxiety N = 540 | Pure depression N = 393 | Comorbid anxiety and depression N = 748 | P‐value | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age (years), mean (SD) | 41.2 (14.7) | 44.4 (12.9) | 41.8 (12.8) | 41.0 (12.2) | 41.3 (12.0) | <0.001 |
| Sex (% female) | 61.5% | 70.0% | 67.4% | 64.9% | 68.0% | <0.05 |
| Education (years), mean (SD) | 12.8 (3.2) | 12.5 (3.2) | 12.1 (3.2) | 12.2 (3.2) | 11.3 (3.3) | <0.001 |
| Partner status (% with partner) | 75.1% | 74.4% | 67.4% | 65.1% | 64.2% | <0.001 |
| Psychiatric characteristics | ||||||
| Depression severity, mean IDS score (SD) | 8.5 (7.5) | 14.1 (9.0) | 22.0 (9.7) | 27.8 (11.3) | 34.9 (12.2) | <0.001 |
| Anxiety severity, mean BAI score (SD) | 4.0 (4.9) | 7.1 (6.5) | 14.8 (9.4) | 12.2 (8.8) | 21.2 (11.2) | <0.001 |
| Severity of fear, mean FQ score | 0.8 (0.9) | 1.1 (0.9) | 2.1 (1.2) | 1.5 (1.2) | 2.6 (1.4) | <0.001 |
| Severity of worry, mean PSWQ score (SD) | 19.2 (9.9) | 24.5 (12.2) | 29.8 (14.3) | 29.6 (15.5) | 33.0 (17.8) | <0.001 |
| Symptom duration % of time with symptoms (months with) | NA | 21.7% | 44.8% | 33.3% | 51.8% | <0.001 |
| Age of onset (years), mean (SD) | NA | 26.1 (13.0) | 19.3 (12.6) | 25.5 (13.1) | 19.6 (12.1) | <0.001 |
| Antidepressant use (%) | ||||||
| SSRI | 0.6% | 10.1% | 19.1% | 23.7% | 32.1% | <0.001 |
| TCA | 0.2% | 1.6% | 3.7% | 2.8% | 4.8% | <0.001 |
| Other | 0.2% | 1.1% | 6.1% | 10.2% | 11.6% | <0.001 |
| Psychotherapy (%) | 3.8% | 6.6% | 17.8% | 29.5% | 32.4% | <0.001 |
Chi‐square values have been computed for categorical variables, anova for interval variables.
Independent‐samples Kruskal–Wallis test was used for nonparametric variables.
As shown in Table 2, between‐group differences emerged on all measures of social functioning (P's<0.001) adjusted for age, sex, education, and partner status (for network size F (4, 2938) = 50.978, P < 0.001; for loneliness F (4, 2611) = 173.252, P < 0.001 for perceived social disability F = (4, 2133) = 274.099, P < 0.001). Effect sizes for the significant effects ranged from small to large (Cohen's d 0.13–1.76). Overall, groups differed significantly (P < 0.001), with a trend visible for all behavioural and affective indicators, as depicted in Fig. 1 with unadjusted means. Controls had the highest levels of social functioning, and patients with comorbid disorders were the most impaired. Anxiety patients differed from healthy controls on all social functioning indices, with effect sizes larger for affective indicators. This pattern, but even less favorable, was also seen in depressed patients. Patients with comorbidity showed the most severe impairments on all indicators of social functioning and differed most significantly from healthy controls. Overall, affective indicators revealed larger effect sizes across disease status than behavioural indicators of social functioning.
Table 2.
Adjusted mean scores for social functioning indicators across psychopathology with effect sizes (Cohen's d)a
| Control subjects N = 650 | Remitted anxiety or depression N = 621 | Effect size | Pure anxiety N = 540 | Effect size | Pure depression N = 393 | Effect size | Comorbid anxiety and depression N = 748 | Effect Size | P‐value | Differencesc | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Social behavioural indicators | |||||||||||
| Network size, mean category (SD) | 3.2 (1.2) | 2.9 (1.1)b | 0.26 | 2.7 (1.1)b | 0.43 | 2.6 (1.0)b | 0.54 | 2.3 (1.0)b | 0.81 | <0.001 | 1 > 2 = 3 > 4 > 5 |
| Social activities, mean (SD) | 14.8 (4.0) | 14.2 (4.2) | 13.6 (4.2)b | 0.29 | 12.7 (4.4)b | 0.50 | 11.6 (4.2)b | 0.78 | <0.001 | 1 = 2 > 3 > 4 > 5 | |
| Social support, mean (SD) | 29.8 (11.4) | 28.6 (11.4)b | 0.11 | 27.9 (12.3)b | 0.16 | 27.4 (12.6)a | 0.20 | 25.3 (12.6)b | 0.38 | <0.001 | 1 > 2 = 3 = 4 > 5 |
| Social affective indicators | |||||||||||
| Loneliness, mean (SD) | 2.0 (2.6) | 3.3 (3.2)b | 0.45 | 4.9 (3.5)b | 0.94 | 5.5 (3.6)b | 1.11 | 6.7 (3.5)b | 1.52 | <0.001 | 1 > 2 > 3 > 4 > 5 |
| Affiliation, mean (SD) | 4.7 (1.6) | 4.7 (1.5) | 4.5 (1.6)b | 0.13 | 4.3 (1.6)b | 0.25 | 4.1 (1.7)b | 0.36 | <0.001 | 1 = 2 > 3 > 5; 3 = 4; 4 = 5 | |
| Perceived social disability, mean (SD) | 7.0 (2.8) | 8.4 (3.4)b | 0.45 | 10.5 (4.1)b | 1.00 | 11.4 (4.4)b | 1.19 | 13.7 (4.6)b | 1.76 | <0.001 | 1 > 2 > 3 > 4 > 5 |
Based on analyses Table 1: adjusted for age, sex, educational level, partner status.
As compared to control subjects.
Significant at P < 0.05 level as compared to control subjects.
Significant differences between control subjects (1), remitted anxiety or depression patients (2), pure anxiety patients (3), pure depression patients (4) and comorbid anxiety and depression patients (5).
Figure 1.
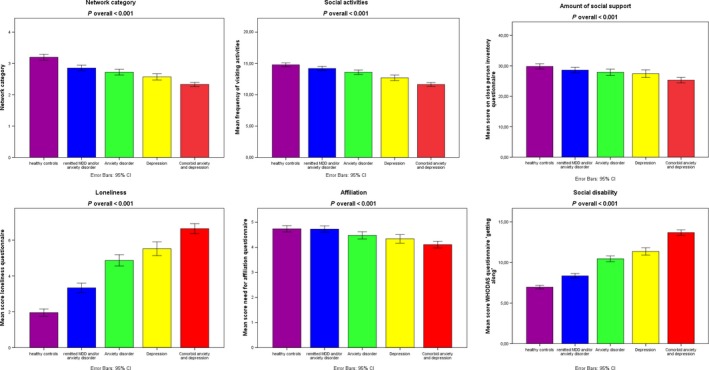
Means for social behavioural and social affective indicators across psychopathology, not adjusted for age, sex, education, and partner status. Error bars represent the standard error. Y‐axis depicts the different scores.
Next, regression analyses (Table 3) examined how dimensional and categorical measures of psychopathology relate to social functioning indicators within the subgroup of patients with current affective disorder (N = 1681), all adjusted for age, sex, education, and partner status. In the first model, comorbid anxiety and depression related to more severe impairments on all indicators of social functioning, when contrasted to pure anxiety (reference) (β = 0.343, P < 0.001 for perceived social disability). Pure depression similarly related to more severe impairments in social functioning when contrasted to pure anxiety (β = 0.081, P < 0.01 for perceived social disability), with exception of social support and affiliation. Subsequently, we explored whether different depressive or anxiety disorders similarly impact social functioning (Table 3). Overall, of the specific types of disorders, MDD and SP seemed to impact social functioning most (network size SP: β = −0.098, P < 0.001; MDD: β = −0.097, P < 0.001; loneliness SP: β = 0.100, P < 0.001; MDD: β = −0.136, P < 0.001; perceived social disability SP: β = 0.306, P < 0.001; MDD: β = 0.247, P < 0.001), followed by GAD, and dysthymia, with network size (GAD: β = −0.052, P < 0.05; dysthymia: β = −0.076, P < 0.01), loneliness (GAD: β = 0.072, P < 0.01; dysthymia: β = −0.119, P < 0.001), and perceived social disability (GAD: β = 0.077, P < 0.001; dysthymia: β = 0.133, P < 0.001). PD and AP were not associated with social functioning indicators in these analyses, in which shared variance between disorder types was eliminated.
Table 3.
Adjusteda associations of clinical characteristics and various social functioning indicatorsa within the group of current patients (N = 1681)
| Social behavioural indicators | Social affective indicators | |||||
|---|---|---|---|---|---|---|
| Network size | Social activities | Social support | Loneliness | Affiliation | Perceived social disability | |
| β | β | β | β | β | β | |
| Model 1 | ||||||
| Pure anxiety | Ref | Ref | Ref | Ref | Ref | Ref |
| Pure depression | −0.062* | −0.095*** | −0.012 | 0.072** | −0.038 | 0.081** |
| Comorbid | −0.174*** | −0.189*** | −0.084** | 0.227*** | −0.097*** | 0.343*** |
| Model 2 | ||||||
| Panic disorder | 0.020 | −0.020 | −0.015 | −0.032 | −0.020 | −0.007 |
| GAD | −0.052* | −0.033 | −0.034 | 0.072** | −0.003 | 0.077*** |
| Social phobia | −0.098*** | −0.062** | −0.048* | 0.100*** | −0.100*** | 0.306*** |
| Agoraphobia | 0.034 | −0.030 | −0.012 | 0.001 | −0.018 | 0.032 |
| MDD | −0.097*** | −0.128*** | −0.052* | 0.136*** | −0.088*** | 0.247*** |
| Dysthymia | −0.076** | −0.139*** | −0.067** | 0.119*** | −0.035 | 0.133*** |
| Model 3 | ||||||
| Severity of depression | −0.224*** | −0.255*** | −0.143*** | 0.374*** | −0.181*** | 0.599*** |
| Severity of anxiety | −0.090*** | −0.176*** | −0.054* | 0.207*** | −0.117*** | 0.382*** |
| Severity of fear | −0.124*** | −0.160*** | −0.061* | 0.231*** | −0.126*** | 0.438*** |
| Severity of worrying | −0.027 | −0.023 | 0.034 | 0.256*** | −0.079** | 0.131*** |
| Symptom duration | −0.091*** | −0.051* | −0.071*** | 0.135*** | −0.027 | 0.152*** |
| Age of onset | 0.100*** | 0.037 | 0.024 | −0.162*** | 0.058* | −0.236*** |
Corrected for sex, age, educational level and partner status.
*Significant at P < 0.05 level; **significant at P < 0.01; ***significant at P < 0.001
The third model assessed the association between dimensional measures of psychopathology and social functioning (Table 3). Overall, more severe depressive or anxiety symptomatology related to more impairment in social functioning. Depression severity was more strongly associated than anxiety severity with social functioning indicators. Severity of worrying was not significantly associated with social behavioural indicators, but highly associated with all affective indicators. Longer symptom duration was strongly associated with more unfavorable scoring on almost all social functioning indicators, except for social activities and affiliation. Lastly, a younger age of onset was associated with a smaller network size and all affective indicators (P's<0.01, except for affiliation P < 0.05). Loneliness and perceived social disability were negatively associated with all clinical characteristics.
Finally, we examined whether any of the social indicators was predictive for having a depressive or anxiety disorder 2 years later, using the clinical subsample of patients from the baseline with two‐year follow‐up data (N = 1409). Overall, 47% of the sample still had a diagnosis of anxiety or depressive disorder after 2 years. For low social activities (odds ratio 0.97 (0.94–1.00), P = 0.06, Table 4) and high loneliness (odds ratio 1.04 (1.00–1.08) P = 0.07, Table 4), non‐significant trends were visible when unadjusted for severity of depression and anxiety but adjusted for age, sex, years of education, and partner status. Higher perceived social disability predicted a higher risk of still having a disorder 2 years later, both adjusted for sex, age, education, partner status, and severity of anxiety and depression (odds ratio, respectively, 1.10 (1.07–1.14), P < 0.001, 1.05 (1.01–1.08), P < 0.01, Table 4).
Table 4.
Logistic regression analyses predicting still having a depression and/or anxiety disorders at 2 year follow up in persons with a current baseline disorder (N = 1409)
| Basic adjusteda Odds ratio (95% CI), P‐value | Adjusted for severity of depression and anxietyb Odds ratio (95% CI), P‐value | |
|---|---|---|
| Social behavioral indicators | ||
| Network size | 1.04 (0.91–1.19), 0.56 | 1.01 (0.88–1.15), 0.91 |
| Social activities | 0.97 (0.94–1.00), 0.06 | 0.98 (0.95–1.02), 0.28 |
| Social support | 1.00 (1.00–1.00), 0.86 | 1.00 (1.00–1.00), 0.76 |
| Social affective indicators | ||
| Loneliness | 1.04 (1.00–1.08), 0.07 | 1.01 (0.97–1.06), 0.51 |
| Affiliation | 0.97 (0.90–1.05), 0.50 | 0.99 (0.92–1.08), 0.85 |
| Perceived social disability | 1.10 (1.07–1.14), P < .001 | 1.05 (1.01–1.08), P < 0.01 |
Corrected for age, sex, years of education, partner status.
Corrected for age, sex, years of education, partner status, severity of depression (IDS), severity of anxiety (BAI).
Discussion
This comprehensive study of affective and behavioural indicators of social functioning found strong associations with depressive and anxiety disorders in a large naturalistic cohort. The findings indicate that social functioning is affected in patients with anxiety, even more so in those with depressive disorders, and most prominently in patients with comorbid anxiety and depression. Overall, affective aspects of social functioning seemed more hampered than behavioural ones. Interestingly, even after complete remission of affective psychopathology, residual impairments in social functioning exist, while social dysfunction in patients was predictive of future psychopathology. To our knowledge, no previous study has examined social functioning within a large sample comprising anxious, depressed, comorbid, remitted patients, and healthy controls.
Our study clearly indicates both affective and behavioural aspects of social functioning are affected in patients with depressive and/or anxiety disorders, with affective aspects being most severely impaired. These findings are in line with two prior studies that combined both behavioural and affective indicators of social functioning in relation to physical and psychological wellbeing 6, 33. Rico‐Uribe et al. 33 showed that loneliness was the strongest contributor to diminished physical health in comparison with network size, frequency of contact, and quality of social network. Santini et al. 6 described in a review that perceived support is more important in depressive disorders than received support. Our findings of impairments of behavioural aspects are in agreement with the findings of a prior study showing that the absence of close friends and relatives is associated with increased risk of clinical anxiety and depression 34.
We found that remitted patients differed significantly from healthy controls in network size, social support, loneliness, and perceived social disability. This is in line with earlier findings 35, 36, 37 showing that social functioning remains impaired in remitted depressed participants. Stout et al. 22 also described that social functioning levels remain impaired for up to 18 months following remission from panic disorder. This impaired social functioning following remission can be the result of residual cognitive of affective symptoms or ‘social scarring’. However, such impaired social functioning can also be reflective of a vulnerability toward development of affective disorders, as was recently described by Schopman et al. 38 for anxiety disorders and by Ormel et al. 39 and Papmeyer et al. 40 for depression. Longitudinal studies have tried to disentangle these different causal routes and have found evidence for both routes 22, 38, 39, 40.
Although impairment of social functioning seemed generally more prominent in depressive disorders than in anxiety disorders, the largest effect sizes were found in patients with comorbid anxiety and depression. These results support previous data comparing psychosocial functioning in pure anxiety or depressive disorders 17, 41 and their comorbidity 42. With regard to specific anxiety disorders, we found that GAD and especially SP are more strongly associated with social dysfunction or higher impairment compared to PD and AP, which is in agreement with findings of several other studies 9, 34, 43. Some authors suggest that GAD resembles MDD when it comes to social impairment 43, while others opine that SP perturbs social functioning more strongly than many other psychiatric disorders 44. In our study, we found no differences in social functioning between SP, MDD, and dysthymia, although overall the effect sizes in MDD were larger than those of anxiety disorders. Remarkably, McKnight et al. 10 described in their review a significantly lower correlation between social functioning impairment and SP, compared to the other anxiety disorders. This contrasts the findings reported here, as well as those documented previously 5, 9, 20, 44, which indicate that SP involves more severe impairments on all social functioning indicators, as compared to other anxiety disorders.
The current study also found that high perceived social disability was predictive of clinical anxiety or depression 2 years later. Evidence suggests that residual psychosocial impairment increases the recurrence of depressive and anxious symptomatology 41, 45, and the affective components are suggested to drive this effect. Several studies have for instance shown that loneliness is predictive of both depressive symptomatology within geriatric populations 8, 46, 47 and social phobia 48. Yet, in our analyses, loneliness was not predictive of future psychopathology, with perceived social disability emerging as the sole significant predictor of anxiety and/or depressive disorders 2 years after the initial screening. Despite this apparent discrepancy, our results do further implicate impaired affective social functioning as a strong predictor of future psychopathology. Of note, this analysis implicates that disability contributes to subsequent psychopathology course. This possible preexistent vulnerability for psychopathology has been described by others 38, 39, 40. Although this was not addressed in our study, it is likely that there is also a reversed link, that is, a longitudinal impact of psychopathology on subsequent social functioning.
As described, impaired social functioning is highly associated with anxious and depressive symptomatology, although the underlying pathophysiological mechanisms remain largely elusive 49, 50. One possible explanation is that social interactions might be appreciated as less rewarding in anxious or depressed patients, due to impaired signaling of brain's reward system, in which the amygdala is crucially implicated 51. This inability to gain reward from social interactions may lead to anhedonia symptoms 49. Future studies focusing specifically on the ‘social brain’, including the social reward system, could greatly advance our understanding of the underlying pathomechanisms of impaired social functioning.
This study is unique in its large size and its comparison of different patient groups and characteristics in relationship to social functioning. Some limitations, however, need to be discussed as well. First, most of our analyses were cross‐sectional, thereby not allowing causal inferences. Also, more detailed aspects of social functioning, such as the exact composition of the social network, were not examined in our study. Differences between our findings and previous findings might stem from the use of different measures of symptomatology and social functioning. In addition, cognitive biases associated with depression or anxiety may have influenced the patient's response and thus their reported social function. Ideally, we would have used actual behavioural data, instead of retrospective self‐reports. An interesting new development is the use of tools like ecological momentary assessment, which allows obtaining real‐time information about social activities of patients and their affective state.
In summary, this study reveals that social functioning is affected in patients with anxiety, even more so in those with depressive disorders, and most prominently in patients with comorbid disorders. Interestingly, even after complete remission of affective psychopathology, residual impairments of social functioning exist, which might indicate possible ‘social scarring’ or preexisting vulnerability factors, with perceived social disability in patients additionally predicting future psychopathology. As social impairments are one of the earliest presenting symptoms in a wide variety of psychopathologies, future studies should aim to disentangle common and specific (biological) characteristics of social functioning using a transdiagnostic approach.
Declaration of interest
We declare that we have no conflicts of interest.
Supporting information
Table S1. Correlations of indicators for all groups.
Acknowledgements
The infrastructure for the NESDA study (www.nesda.nl) has been funded through the Geestkracht Programme of the Netherlands Organisation for Health Research and Development (Zon‐Mw, grant number 10‐000‐1002) and participating universities (VU University Medical Center, Leiden University Medical Center, University Medical Center Groningen). Analyses were supported by the EU‐PRISM Project (www.prism-project.eu), which received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No 115916. This Joint Undertaking receives support from the European Union's Horizon 2020 research and innovation programme and EFPIA.
Saris IMJ, Aghajani M, van der Werff SJA, van der Wee NJA, Penninx BWJH. Social functioning in patients with depressive and anxiety disorders.
Reference
- 1. Eisenberger NI, Cole SW. Social neuroscience and health: neurophysiological mechanisms linking social ties with physical health. Nat Neurosci 2012;15:669–674. [DOI] [PubMed] [Google Scholar]
- 2. Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical Import and Interventions. Perspect Psychol Sci 2015;10:238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Holt‐Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta‐analytic review. PLoS Med 2010;7:e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patterson A, Veenstra G. Loneliness and risk of mortality: a longitudinal investigation in Alameda County, CA. Soc Sci Med 2010;71:181–186. [DOI] [PubMed] [Google Scholar]
- 5. Teo AR, Lerrigo R, Rogers MAM. The role of social isolation in social anxiety disorder: a systematic review and meta‐analysis. J Anxiety Disord 2013;27:353–364. [DOI] [PubMed] [Google Scholar]
- 6. Santini ZI, Koyanagi A, Tyrovolas S, Mason C, Haro JM. The association between social relationships and depression: a systematic review. J Affect Disord 2015;175:53–65. [DOI] [PubMed] [Google Scholar]
- 7. Dickens A, Richards S, Greaves C, Campbell J. Interventions targeting social isolation in older people: a systematic review. BMC Public Health 2011;11:647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross‐sectional and longitudinal analyses. Psychol Aging 2006;21:140–151. [DOI] [PubMed] [Google Scholar]
- 9. Cramer V, Torgersen S, Kringlen E. Quality of life and anxiety disorders: a population study. J Nerv Ment Dis 2005;193:196–202. [DOI] [PubMed] [Google Scholar]
- 10. McKnight PE, Monfort SS, Kashdan TB, Blalock DV, Calton JM. Anxiety symptoms and functional impairment: a systematic review of the correlation between the two measures. Clin Psychol Rev 2016;45:115–130. [DOI] [PubMed] [Google Scholar]
- 11. Barrera TL, Norton PJ. Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. J Anxiety Disord 2009;23:1086–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Markowitz J, Weissman M, Ouellette R, Lish J, Klerman G. Quality of life in panic disorder. Arch Gen Psychiatry 1989;46:984–992. [DOI] [PubMed] [Google Scholar]
- 13. de Graaf R, Bijl R, Spijker J, Beekman A, Vollebergh W. Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders‐findings from the Netherlands mental health survey and incidence study. Soc Psychiatry 2003;38:1–11. [DOI] [PubMed] [Google Scholar]
- 14. Lamers F, van Oppen P, Comijs HC et al. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: the Netherlands Study of Depression and Anxiety (NESDA). J Clin Psychiatry 2011;72:341–348. [DOI] [PubMed] [Google Scholar]
- 15. Lonescu D, Niciu M, Mathews D, Richards E, Zarate CJ. Neurobiology of anxious depression: a review. Depress Anxiety 2013;30:374–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Penninx BWJH, Nolen WA, Lamers F et al. Two‐year course of depressive and anxiety disorders: results from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2011;133:76–85. [DOI] [PubMed] [Google Scholar]
- 17. Hecht H, Von Zerssen D, Krieg C, Possl J, Wittchen H‐U. Anxiety and depression: comorbidity, psychopathology, and social functioning. Compr Psychiatry 1989;30:420–433. [DOI] [PubMed] [Google Scholar]
- 18. Norton PJ, Chase TE. Is gin‐tonic more like gin or more like tonic. Psychiatry Res 2015;225:179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kamenov K, Cabello M, Caballero FF et al. Factors related to social support in neurological and mental disorders. PLoS ONE 2016;11:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: a meta‐analytic review. Clin Psychol Rev 2007;27:572–581. [DOI] [PubMed] [Google Scholar]
- 21. Kennedy N, Foy K, Sherazi R, McDonough M, McKeon P. Long‐term social functioning after depression treated by psychiatrists: a review. Bipolar Disord 2007;9:25–37. [DOI] [PubMed] [Google Scholar]
- 22. Stout RL, Dolan R, Dyck I, Eisen J, Keller MB. Course of social functioning after remission from panic disorder. Compr Psychiatry 2001;42:441–447. [DOI] [PubMed] [Google Scholar]
- 23. Penninx BWJH, Beekman ATF, Smit JH et al. The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int J Methods Psychiatr Res 2008;17:121–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med 1996;26:477–486. [DOI] [PubMed] [Google Scholar]
- 25. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893–897. [DOI] [PubMed] [Google Scholar]
- 26. Marks IM, Mathews AM. Brief standard self‐rating for phobic patients. Behav Res Ther 1979;17:263–267. [DOI] [PubMed] [Google Scholar]
- 27. Lyketsos CG, Nestadt G, Cwi J, Heithoff K, Eaton WW. The life chart interview: a standardized method to describe the course of psychopathology. Int J Methods Psychiatr Res 1994;4:143–155. [Google Scholar]
- 28. Fuhrer R, Stansfeld SA. How gender affects patterns of social relations and their impact on health: a comparison of one or multiple sources of support from “close persons”. Soc Sci Med 2002;54:811–825. [DOI] [PubMed] [Google Scholar]
- 29. Stansfeld S, Marmot M. Deriving a survey measure of social support: the reliability and validity of the Close Persons Questionnaire. Soc Sci Med 1992;35:1027–1035. [DOI] [PubMed] [Google Scholar]
- 30. de Jong‐Gierveld J, Kamphuis F. The development of a Rasch‐type loneliness scale. Appl Psychol Meas 1985;9:289–299. [Google Scholar]
- 31. van Tilburg TG. Verkregen en gewenste ondersteuning in het licht van eenzaamheidservaringen [Obtained and desired social support in association with loneliness]. Dissertatie, Vrije Universiteit Amsterdam, 1988; 58‐60‐121.
- 32. Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the world health organization disability assessment schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol 2003;56:507–514. [DOI] [PubMed] [Google Scholar]
- 33. Rico‐Uribe LA, Caballero FF, Olaya B et al. Loneliness, social networks, and health: a cross‐sectional study in three countries. PLoS ONE 2016;11:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chou K, Liang K, Sareen J. The association between social isolation and DSM‐IV mood, anxiety, and substance use disorders: wave 2 of the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 2011;72:1468–1476. [DOI] [PubMed] [Google Scholar]
- 35. Ormel J, Von Korff M, Van Den Brink W, Katon W, Brilman E, Oldehinkel T. Depression, anxiety, and social disability show synchrony of change in primar. Am J Public Health 1993;83:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL. The enduring psychosocial consequences of mania and depression. Am J Psychiatry 1993;150:720–727. [DOI] [PubMed] [Google Scholar]
- 37. Furukawa TA, Azuma H, Takeuchi H, Kitamura T, Takahashi K. 10‐year course of social adjustment in major depression. Int J Soc Psychiatry 2010;57:501–508. [DOI] [PubMed] [Google Scholar]
- 38. Schopman SME, ten Have M, van Dorsselaer S, de Graaf R, Batelaan NM. Limited functioning after remission of an anxiety disorder: trait‐ and/or scar effect? Results of a longitudinal general population study. J Clin Psychiatry 2017. (in print). [DOI] [PubMed] [Google Scholar]
- 39. Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode. Arch Gen Psychiatry 2004;61:990. [DOI] [PubMed] [Google Scholar]
- 40. Papmeyer M, Sussmann JE, Hall J et al. Neurocognition in individuals at high familial risk of mood disorders with or without subsequent onset of depression. Psychol Med 2015;45:3317–3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rodriguez BF, Bruce SE, Pagano ME, Keller MB. Relationships among psychosocial functioning, diagnostic comorbidity, and the recurrence of generalized anxiety disorder, panic disorder, and major depression. J Anxiety Disord 2005;19:752–766. [DOI] [PubMed] [Google Scholar]
- 42. Norberg MM, Diefenbach GJ, Tolin DF. Quality of life and anxiety and depressive disorder comorbidity. J Anxiety Disord 2008;22:1516–1522. [DOI] [PubMed] [Google Scholar]
- 43. Kessler RC, Ph D, Dupont RL, Berglund P, Wittchen H, Ph D. Impairment in pure and Comorbid Generalized Anxiety Disorder and major Depression at 12 months in Two National Surveys. Am J Psychiatry 1999;156:1915–1923. [DOI] [PubMed] [Google Scholar]
- 44. Torgrud LJ, Walker JR, Murray L, Cox BJ, Kjernisted KD. Deficits in perceived social support associated with generalized social phobia. Cogn Behav Ther 2004;33:87–96. [DOI] [PubMed] [Google Scholar]
- 45. Solomon DA, Leon AC, Endicott J et al. Psychosocial impairment and recurrence of major depression. Compr Psychiatry 2004;45:423–430. [DOI] [PubMed] [Google Scholar]
- 46. Hagerty BM, Reg WA. The effects of sense of belonging, social support, conflict, and loneliness on depression. Nurs Res 1999;48:215–219. [DOI] [PubMed] [Google Scholar]
- 47. Heikkinen R, Kauppinen M. Depressive symptoms in late life: a 10‐year. Arch Gerontol Geriatr 2004;38:239–250. [DOI] [PubMed] [Google Scholar]
- 48. Lim MH, Rodebaugh TL, Zyphur MJ, Gleeson JFM. Loneliness over time: the crucial role of social anxiety. J Abnorm Psychol 2016;125:620–630. [DOI] [PubMed] [Google Scholar]
- 49. Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev 2016;69:313–332. [DOI] [PubMed] [Google Scholar]
- 50. Iorfino F, Hickie IB, Lee RSC, Lagopoulos J, Hermens DF. The underlying neurobiology of key functional domains in young people with mood and anxiety disorders: a systematic review. BMC Psychiatry 2016;16:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Germine LT, Garrido L, Bruce L, Hooker C. Social anhedonia is associated with neural abnormalities during face emotion processing. NeuroImage 2011;58:935–945. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Correlations of indicators for all groups.


