ABSTRACT
Exposure to soil or water contaminated with the urine of Leptospira-infected animals is the most common way in which humans contract leptospirosis. Entire populations can be at high risk of leptospirosis while working in inundated fields, when engaging in aquatic sports, or after periods of heavy rainfall. The risk of infection after contact with these environmental sources depends on the ability of Leptospira bacteria to survive, persist, and infect new hosts. Multiple variables such as soil and water pH, temperature, and even environmental microbial communities are likely to shape the environmental conditions needed by the pathogen to persist. Here we review what is known about the environmental phase of the infectious Leptospira transmission cycle and identify knowledge gaps that will serve as a guide for future research.
KEYWORDS: Leptospira, leptospirosis, environment, water, soil, transmission, survival
INTRODUCTION
Leptospirosis is a zoonotic disease caused by spirochete bacteria in the genus Leptospira. It produces different symptoms and signs, such as headaches, fever, jaundice, kidney and liver failure, and even death (1, 2), in 1.03 million annual cases around the world. Leptospira bacteria are shed in bodily fluids (urine, placenta, and vaginal fluids), and infection occurs when the pathogen penetrates the skin through small abrasions or mucosal membranes (e.g., the eyes and mouth) (1, 3). Veterinarians, farmers, and other individuals who work with animals and their products are at high risk of contracting the disease because of the likelihood of exposure to contaminated fluids (1). Other occupations (e.g., plumbing, sewer work, and garbage collection) also involve indirect contact with infected animal products such as urine. Likewise, agricultural workers may be exposed to contaminated soil or water. Importantly, when the pathogen is shed into the environment, nonoccupational exposure in urban and rural settings is also possible and can place entire populations at risk for leptospirosis (2). Because of the complex and diverse interactions between animals (including humans) and their living environment, the risk of infection by exposure to contaminated environmental sources is not well understood and is thus challenging to control. Our aims here are to provide a broad overview of environmental survival, persistence, and transmission of infectious Leptospira bacteria and to identify knowledge gaps to guide future research.
EXPOSURE TO SOIL OR WATER IS A COMMON RISK FACTOR FOR HUMAN LEPTOSPIROSIS
The literature is replete with examples of human leptospirosis cases without clear evidence of direct contact with animals that are thus likely due to contact with contaminated soil or water. Such examples are common among farmers working in inundated fields or among fishermen, with mean odds ratios (ORs) of >2 (1, 4). Risk factors include exposure to stagnant or moving water or mud (1, 5–7). Manual laborers such as trash collectors, miners, or cane cutters are particularly prone to skin cuts and abrasions that may put them at additional risk for contracting leptospirosis. Recreational exposure has also been widely associated with this disease, with mean ORs similar to those related to occupational activities, particularly after swimming and practicing aquatic sports in rivers and other water sources. Outbreaks have been linked to kayaking, surfing, canoeing, rafting, triathlons, and military training exercises, among others with documented exposure to water (2). In addition to occupational and recreational activities, weather conditions have also been associated with Leptospira infection. Increased leptospirosis rates are usually reported during and after extreme weather events or heavy rainfall, especially in tropical countries. Moreover, the risk of infection due to exposure to floodwater, mud, or wet soil associated with these events varies from region to region and in some cases shows seasonal variation (7–11).
While the association of leptospirosis with rain and extreme weather events is well established, we can only speculate about how these conditions might favor the persistence and dispersal of Leptospira bacteria in the environment in a manner that leads to increased human infections. Site-specific features may further impact the survival and dispersal of this pathogen. In urban settings, large quantities of floodwater frequently overwhelm sewage systems, increasing the risk of infection through direct contact with contaminated water or by facilitating dispersal to soils that may be primed by rainfall to become increasingly suitable for pathogen survival and persistence. An additional consequence of flooding is that rats and domestic animals may be forced to seek refuge in the same noninundated places as humans, increasing the likelihood that noninfected animals (and humans) will be exposed to and have contact with infected animals (12). In rural settings, an increased quantity and diversity of peridomestic animals, which may be particularly important sources of Leptospira bacteria (13), may increase transmission in this manner. Moreover, under flood conditions where dry habitat is scarce, sylvatic animals may increasingly encroach on the peridomestic environment, further complicating the environmental cycling of infectious Leptospira bacteria.
RESERVOIRS AND THE ENVIRONMENTAL LOAD OF INFECTIOUS LEPTOSPIRA
The risk of human infection posed by different animal species is likely to be greatly influenced by the amount of Leptospira bacteria shed into the environment and the likelihood of human contact with the resulting contaminated soil. A wide diversity of peridomestic animals (rats, horses, cows, dogs, and pigs) and feral animals (bats, coyotes, sea lions, and even frogs) can carry Leptospira bacteria in their kidneys and therefore presumably excrete the pathogen into the environment. The amount of pathogen that these animals shed is likely to be very important for the establishment of environmental sources and the risk of infection upon exposure to those sources. Rats shed about 5.7 × 106 Leptospira bacteria/ml of urine; and cows, deer, dogs, mice, and humans have been reported to shed an average of 3.7 × 104, 1.7 × 105, 1.4 × 102, 3.1 × 103, and 7.9 × 102 Leptospira bacteria/ml of urine, respectively. Information on the quantities of Leptospira bacteria shed by other animals is completely lacking (14). Host weight might also affect the amount of pathogen excreted, as has been reported for naturally infected young black rats, where higher weight was significantly associated with renal Leptospira loads (15). Multiple variables such as the volume of urine shed by each host, prevalence among hosts, and local host densities will define the pathogen load excreted into an environment (13, 14, 16, 17). In urban areas where small animals (rats and dogs) predominate, a high risk of human infection may depend on a high animal densities and a high prevalence of disease among these animals. Conversely, in places where large mammals (e.g., cows) are the main reservoirs, the sheer volume of urine excreted into the environment by very few animals may convey vast amounts of Leptospira bacteria and result in a high risk of human infection (13, 14). Also, Leptospira bacteria shed by domestic and peridomestic animals may present a greater infection risk to humans than those presumably shed by wild animals in areas not frequently visited by humans. The roles of different animals in transmission among animals and environmental maintenance of Leptospira bacteria have not been investigated.
INOCULUM REQUIRED FOR INFECTION
Leptospira infection typically occurs when bacterial spirochetes penetrate the body through mucosal membranes or skin cuts (1, 2), enter the bloodstream of the host, and disseminate to cause systemic infection (3, 18). Unfortunately, our knowledge of the quantity of Leptospira bacteria required to cause infections in a natural environment is based on laboratory studies using hamster (19, 20), guinea pig (21, 22), and monkey (23) models. Animals inoculated with large doses of Leptospira bacteria through the conjunctival (105 to 108 bacteria) (22, 24, 25), subcutaneous (2 × 106 bacteria) (26), and epicutaneous (5 × 108 bacteria) (27) routes have been used to establish infections. However, these studies were not intended to provide infectious dose estimates and it is likely that infectious doses are considerably smaller because such extremely large doses are very unlikely to occur in nature. The greatest reported load of Leptospira bacteria in an environmental sample was 104 Leptospira bacteria/ml (28, 29). Even direct sampling of urine from animals is likely to results in an amount of Leptospira bacteria that is less than what is typically used to induce laboratory infections; median amounts of Leptospira bacteria per milliliter of urine from infected animals range from 102 (dogs) to 106 (rats) (14). Swallowing water is thought to be an important route of entry (2); however, we were not able to find any published study that used the oral or intranasal inoculation route to establish infection. The relationship between the infectious dose and route of infection with different strains is a basic but critical knowledge gap that is crucial for accurately defining the risk of infection in animals (and humans) after contact with contaminated environmental sources.
CURRENT KNOWLEDGE OF PERSISTENCE OF INFECTIOUS LEPTOSPIRA IN THE ENVIRONMENT
The survival and longevity of a pathogen once it is shed into the environment will have a direct bearing on the infection risk. Although few rigorous studies have considered the environmental phase of infectious Leptospira bacteria, relevant observations about their presence and survival have been compiled since the beginning of the 20th century (30) and suggest that environmental survival and persistence are highly dependent on environmental conditions. Such conditions include the medium type, as well as the location and seasonal variation. Also, even though the survival and persistence rates of these bacteria may differ among species and strains, comparative experiments have not been performed. There is therefore a great need for research to address how multiple biotic and abiotic variables interact together and with different pathogen strains to influence environmental survival and the ability to infect another host.
Presence of infectious Leptospira in the natural environment.
In the last decades, the presence of infectious Leptospira bacteria in different natural environments has been evaluated by culturing the pathogen or by detecting its DNA. Most of these reports are observational but have shaped our understanding of environmental conditions and media likely to harbor these pathogens. Leptospira bacteria have been found in water and soil samples from rural and urban settings (31–33), in the jungle (34), after periods of heavy rainfall (35), and even during the summer (36). In summary, Leptospira bacteria have been found in a wide variety of environments, but unfortunately, only a few systematic studies provide detail information on the positivity (prevalence) and sources of the samples analyzed (Table 1) (17, 28, 29, 32, 33, 37–52). Results from individual studies suggest that the likelihood of finding infectious Leptospira bacteria in the environment is site dependent, differing among regions, medium sources, and seasons. For example, analysis of water samples collected in South Andaman Island showed higher positivity in urban sewage water and household drainage water than in ponds or civic toilet drainage. In the same study, higher positivity was found in rural paddy field water than in streams, ponds, and other water sources (39). Likewise, samples collected in streams in the Peruvian Amazon Basin show higher positivity than well water samples and there were higher pathogen concentrations in samples collected in urban settings than in those from rural ones (28). An important variable that might impact the likelihood of contact with Leptospira bacteria in the environment is animal urine dilution. We expect large amounts of pathogens washed into small water bodies such as stagnant water or ponds formed after periods of heavy rainfall because of the relatively low dilution of urine (53, 54), in contrast with big water bodies such as rivers or floodwater, where we expect highly diluted urine and lower pathogen concentrations. We can speculate that Leptospira aggregation behavior (55) might counteract the dilution factor in big water bodies, maintaining concentrations sufficient for infection. Such aggregation might partially explain why many studies do not detect infectious Leptospira bacteria in large bodies of water in regions where leptospirosis is endemic or when investigating outbreaks (56, 57). Detection of infectious Leptospira bacteria in the environment is also subject to seasonal variation (17). This might explain why the pathogen is not always found in environmental samples collected from localities where leptospirosis is endemic, such as Kelantan, Malaysia (Table 1) (38). These and other studies that have found infectious Leptospira bacteria (or their DNA) in the environment provide valuable epidemiological information about the general site characteristics that influence pathogen presence. Specific abiotic and biotic microsite conditions may also impact the presence of Leptospira bacteria in soil and water.
TABLE 1.
Studies with detailed data on the positivity of infectious Leptospira bacteria in environmental samples
| Sample type and origin | Reference(s) | % (no.) of samples positive |
Source(s) of positive samplesa | Leptospira species | Detection/identification method(s) | |
|---|---|---|---|---|---|---|
| Rural | Urban | |||||
| Water | ||||||
| South Asia | 39 | 9 (133) | 12.4 (113) | Urban household drainage and sewage, rural paddy fields and water from stream and vegetable fields | Pathogenic and intermediate | Culture and PCR/PCR and sequencing |
| 40 | 22.1 (86) | 26.8 (56) | Urban sewers; rural sewers, rainwater, and paddy fields | Pathogenic | PCR | |
| Southeast Asia | 38 | 0 (36) | 0 (36) | Culture/PCR and sequencing | ||
| 31 | 6.4 (110) | Urban floodwater | Pathogenic and intermediate | Culture and PCR/PCR and sequencing | ||
| 41 | 0 (18) | 8.3 (12) | Urban floodwater | Pathogenic | PCR | |
| 42 | 2.5 (121) | Urban street drain water and lake water | Pathogenic and intermediate | Culture/PCR and sequencing | ||
| 43 | 5.5 (18) | 0 (39) | Rural water | Intermediate | Culture/PCR and sequencing | |
| 85 | 21.4 (14) | Rural underground water | L. interrogans, L. weilii | PCR/sequencing | ||
| 37 | 1.9 (324) | Urban stagnant water | L. borgpetersenii, L. interrogans, L. wolffii, L. inadai | Culture/PCR and sequencing | ||
| High-income Asia Pacific | 43 | 6.3 (16) | Urban water from a university campus | L. alstonii | Culture/PCR and sequencing | |
| Caribbean | 44 | 18.2 (44) | Rural puddles, mountain springs, and water dams | Pathogenic | PCR | |
| Central Latin America | 33 | 3.7 (54) | Rural water from farms | Pathogenic | Culture/PCR | |
| 45 | 3.7 (54) | Rural farm wastewater | L. interrogans | Culture/PCR | ||
| Andean Latin America | 28 | 25.4 (236) | 47.4 (192) | Urban gutters, river shore, puddles, and underground water; rural stream and well water | Pathogenic and intermediate | Culture and PCR/PCR |
| Southern Latin America | 32 | 13.5 (570) | Rural wells, barrels, old tires, ponds, rivers, canals, and springs | Pathogenic | PCR | |
| 17 | 19.6 (576) | 16.7 (240) | Urban puddle, human drinking water, flowing source, container; rural animal drinking water, puddle, flowing source, container | L. interrogans, L. kirschneri, L. weilii, pathogenic | PCR/PCR and sequencing | |
| Tropical Latin America | 46 | 1 (100) | Urban community water supply | Pathogenic | PCR | |
| Western Europe | 29 | 6.4 (47) | Urban ponds | Pathogenic | PCR | |
| 47 | 50 (4) | Urban water from toilet | L. interrogans | PCR/PCR and sequencing | ||
| 48 | 3.9 (151) | Urban river, canal water | Pathogenic | PCR | ||
| Central Europe | 49 | 1.9 (104) | Rural wells | Pathogenic | PCR | |
| High-income North America | 50 | 100 (22) | Rural and urban stream water | Pathogenic | PCR/sequencing | |
| 51 | 50 (2) | Rural stagnant pool | Pathogenic | Culture/serotyping | ||
| Soil | ||||||
| Southeast Asia | 38 | 0 (36) | 2.8 (36) | Urban market soil samples | L. alstonii | Culture/PCR |
| 42 | 0 (30) | |||||
| 43 | 0 (3) | |||||
| 43 | 47.8 (23) | Urban inundated soil | Pathogenic, L. kmetyi | Culture/PCR | ||
| 37 | 11.6 (292) | Urban soil | L. noguchii, L. borgpetersenii, L. weilii, L. wolffii | Culture/PCR and sequencing | ||
| High-income Asia Pacific | 43 | 25 (12) | Urban soil | L alstonii | Culture/PCR and sequencing | |
| Western Europe | 47 | 100 (2) | Urban soil from inside and outside a pond | L. interrogans | PCR/PCR and sequencing | |
| Central Europe | 49 | 0 (108) | ||||
| Eastern Europe | 52 | 0.8 (630) | Urban soil near a lake | Pathogenic | Culture/serotyping | |
Rural areas include rural villages and farms.
Abiotic conditions impacting pathogen survival in the environment.
High morbidity in tropical climate regions, especially during periods of heavy rain, and the sporadic nature of cases that typify temperate regions (58) are consistent with the ability of Leptospira bacteria to better survive and persist under specific environmental conditions. Survival and persistence of infectious Leptospira bacteria in the environment may rely on the interaction of multiple factors, including abiotic soil and water conditions. These pathogenic spirochetes can live in soil with a moisture content of >20% (43, 59), water and soil with pHs around 5.5 and 7.6 (43, 59–62), and temperatures ranging from 4 to 40°C (36, 60, 63, 64). Likewise, it has been reported that pathogenic Leptospira bacteria can metabolize urea (65) and that they are able to survive for 6 to 18 h in pure (pH 7 to 8) cattle urine, although longer survival times have been observed when urine is diluted (62, 66). Also, the ability of infectious Leptospira bacteria to survive in the environment might be assisted by their ability to resist changes in osmolality (67). Moreover, there is no evidence to suggest that infectious Leptospira bacteria lose their infectivity when they are in the environment and have been shown to remain infectious for at least 43 days in wet soil (61) and 20 months in freshwater (60).
Motility and dispersal of infectious Leptospira bacteria may also be critical for environmental survival by enabling escape from inhospitable microenvironments and tropism toward more favorable conditions. Leptospira bacteria have been shown to move on viscous matrices (around 15 μm/s) and liquid surfaces (5 μm/s) (67). In aqueous environments, chemotaxis toward hemoglobin might lead the pathogen to reach an entrance into the animal body (68). Motility might also facilitate the avoidance of some harmful environmental conditions such as prolonged exposure to sunlight (62, 69, 70).
Additional variables, related to animal reservoirs, might also be important for defining the environmental persistence of Leptospira bacteria in the environment. For instance, the longitudinal survival rate after shedding in urine might depend on urine pH, which is influenced by specific local features such as animal nutrition (71, 72). Abiotic conditions under which infectious Leptospira bacteria survive and persist in the environment have been established mainly from experiments performed under controlled laboratory conditions, and multiple combinations of abiotic conditions have not been tested. Furthermore, these experiments were all qualitative, providing information about the length of survival but not the dynamics of survival over time. There is an unmet need to better comprehend how infectious Leptospira bacteria respond to exposure to a wide diversity of natural soil and water conditions. This information is clearly important for determining the risk of infection from environmental sources.
Relevance of environmental bacteria.
The composition of microbial communities is also likely to influence the survival and persistence of infectious Leptospira bacteria. While it is probable that some microbial taxa are antagonistic to infectious Leptospira survival in the environment, others might be beneficial. For example, recent research has found that infectious Leptospira bacteria coaggregate with environmental bacteria isolated from freshwater and can live within environmental bacterial biofilms from paddy field water, sewers, and stagnant rainwater (40, 73). While microbial communities may play a very important role in the survival and persistence of infectious Leptospira bacteria in the environment, our knowledge and understanding of this are very limited. More research is needed to further identify, qualify, and quantify the roles of these bacteria in influencing survival, persistence, and ultimately the risk of human/animal infections.
Genetic factors linked to environmental persistence.
Environmental persistence of pathogenic Leptospira bacteria varies among species (74), but little is known about the genetic mechanisms that drive this difference. From laboratory experiments and whole-genome sequence data, we know that not all Leptospira species have the same ability to survive and reproduce outside a host. For example, after 48 h of incubation in water, Leptospira borgpetersenii serovar Hardjo showed a limited capacity to survive compared to that of Leptospira interrogans (74); however, further details about this observation have not been published. In fact, L. interrogans has been shown to survive and retain virulence in water for up to 344 days (60). The ability of L. interrogans to survive in the environment is consistent with the finding that its genome contains multiple genes (80 in serovar Copenhageni) that code for signal transduction proteins (75) and a higher number of two-component response regulators than L. borgpetersenii (74). Recent research using transposon mutagenesis has provided evidence that the expression of ebpA, a gene that encodes an enhancer binding protein that interacts with σ54 to activate the transcription of specific genes, is essential for the survival of L. interrogans in freshwater (76). Also, from whole-genome microarray assays, we know that this species has genes that are differentially regulated when it is exposed to environmental temperatures and different osmolality conditions (77, 78). All of these genetic characteristics might play an important role in facilitating the transition of this pathogen between mammalian hosts and soil and water. Additionally, overexpression of the GroEL protein, encoded by groEl, has been shown in L. interrogans and Leptospira fainei biofilms, suggesting that these protein might have an important role in the persistence of the pathogen in the environment after it is shed in animal urine (79–81).
The scarcity of whole-genome sequences has limited our knowledge of genetic variation within and between Leptospira species. Indeed, half of the whole-genome sequences of the genus in public databases belong to L. interrogans. Fortunately, this situation is changing and between 2014 and 2017, the number of whole-genome sequences increased by about 40%. A major hurdle has been the difficulty in detecting and culturing Leptospira bacteria; however, recent successful experiences in isolating infectious Leptospira bacteria from the environment (38, 82) and new or optimized assays that allow to amplify their DNA and RNA directly from environmental samples with high sensitivity and specificity (17, 39, 40, 83, 84) will help to overcome these limitations. Additionally, genotyping methods have evolved such that now we can better assess the diversity of Leptospira bacteria in a given area or among animal species. For example, older studies have suggested a strong correlation between host species and pathogen type; however, recent work has shown a surprisingly high degree of pathogen diversity in a single reservoir species (13). Furthermore, the use of modern sequencing technologies together with new bioinformatics tools will facilitate the study of the pathogen obtained directly from soil or water, under different conditions, without the need for culturing.
LINKING LEPTOSPIRA INFECTION TO SPECIFIC ENVIRONMENTAL SOURCES
Despite our knowledge of potential environmental sources and host reservoirs, as well as risk factors for human infection, strong molecular evidence linking individual human cases to specific environmental sources is completely lacking. Evidence that highlights the importance of contact with soil and water as a risk factor for leptospirosis is largely limited to traditional epidemiological surveys that assess exposure to environmental factors. Importantly, molecular evidence that ties a leptospirosis case to a source by establishing contact and a matching genotype has not been found. In many instances, case investigations failed to even detect the pathogen at environmental sites suspected to be the source of outbreaks (56, 57). Nevertheless, there are few examples where the same genotype or serotype was found in water or animal sources from the same community or neighboring sites as a clinical case (13, 17, 28). In one of those studies, clinical samples from the Peruvian Amazon basin were collected from a local hospital while environmental sampling was mainly performed in public areas. Even though a genotype match (at the species level) between an environmental and a clinical sample was found, there was no evidence that patients were in contact with these public areas (28). In another study, clinical samples from the Ecuadorian coast were collected from local health centers while animal samples were extracted from local slaughterhouses. Results were similar to those of the previously cited study; genotype matches were found, but there was no evidence that the clinical cases had direct or indirect contact with the infected animals (13). Another study performed in southern Chile compared clinical samples to those collected from the peridomestic environment of clinical patients but found no genotype matches (17). Unfortunately, to date, there are no studies reporting the detection of infectious Leptospira bacteria from a source where a leptospirosis patient was known (or even likely) to be exposed. This lack of strong evidence that ties individual clinical cases to an environmental source presents a major knowledge gap in our attempts to better understand and identify how humans are infected with Leptospira bacteria.
CONCLUSION
Leptospira infection most commonly occurs upon exposure to infected animals and contaminated environments; however, filling the critical gaps in our knowledge of the transmission cycle would greatly benefit our efforts to understand the epidemiology of this disease (Fig. 1). To reduce the morbidity rate, we need to better understand how environmental conditions impact Leptospira survival in natural surroundings. What are the characteristics that make some environments more suitable for pathogen persistence? How do different Leptospira species respond to different environmental conditions? What, if any, is the role of environmental bacteria in Leptospira persistence? Can we identify genetic mechanisms that facilitate or restrict survival under certain conditions? Can such genetic characteristics be used as markers for predicting the length of time for which circulating genotypes pose a significant risk of infection? To ascertain the risk of infection, it is extremely important to know the amount of pathogen needed to cause infection in animals and humans. Information about the infectious dose, joined with quantification of the pathogen and knowledge of survival under different environmental conditions, will allow us to make longitudinal predictions of the infection risk posed by exposure to a certain environmental source (Fig. 1).
FIG 1.
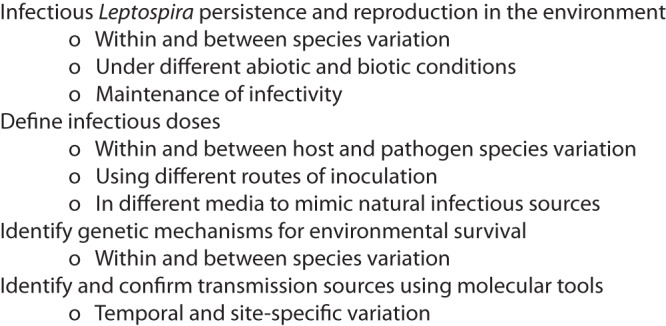
Important aspects to consider for future research.
Leptospirosis has been associated with a wide variety of environmental factors by traditional epidemiological studies. However, routes of exposure to the pathogen are complex and critical differences between sites might exist. Emerging molecular techniques offer the opportunity to better comprehend the relative importance of different potential sources by genotyping the pathogen and matching clinical cases with environmental sources. Although we have much to learn about the relative relevance of each environmental source to human infection, accurate identification of the likelihood of the many different possible sources of infection is critical for understanding the variables associated with environmental exposure.
Understanding temporal and site-specific differences in environmental survival and reproduction of infectious Leptospira bacteria, as well as the likelihood of transmission to humans, will be critical for the development of realistic and effective public health preventive plans. The many possible sources of variation present challenges and opportunities for researchers to incorporate diversity into their laboratory and animal models. Field work in different settings and over longer periods of time will also help identify the relative importance of variables and the extent to which results and conclusions are generalizable across time and space.
ACKNOWLEDGMENTS
This work was funded by National Institute of Allergy and Infectious Disease, National Institutes of Health, grant R15AI101913; a SENESCYT scholarship from the Ecuadorian Government; Universidad San Francisco de Quito Ecuador; and the Cowden Endowment, Northern Arizona University.
REFERENCES
- 1.Levett PN. 2001. Leptospirosis. Clin Microbiol Rev 14:296–326. doi: 10.1128/CMR.14.2.296-326.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haake DA, Levett PN. 2015. Leptospirosis in humans. Curr Top Microbiol Immunol 387:65–97. doi: 10.1007/978-3-662-45059-8_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ko AI, Goarant C, Picardeau M. 2009. Leptospira: the dawn of the molecular genetics era for an emerging zoonotic pathogen. Nat Rev Microbiol 7:736–747. doi: 10.1038/nrmicro2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mwachui MA, Crump L, Hartskeerl R, Zinsstag J, Hattendorf J. 2015. Environmental and behavioural determinants of leptospirosis transmission: a systematic review. PLoS Negl Trop Dis 9:e0003843. doi: 10.1371/journal.pntd.0003843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parveen SM, Suganyaa B, Sathya MS, Margreat AA, Sivasankari K, Shanmughapriya S, Hoffman NE, Natarajaseenivasan K. 2016. Leptospirosis seroprevalence among blue metal mine workers of Tamil Nadu, India. Am J Trop Med Hyg 95:38–42. doi: 10.4269/ajtmh.16-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray KO, Fischer RS, Chavarria D, Duttmann C, Garcia MN, Gorchakov R, Hotez PJ, Jiron W, Leibler JH, Lopez JE, Mandayam S, Marin A, Sheleby J. 2015. Mesoamerican nephropathy: a neglected tropical disease with an infectious etiology? Microbes Infect 17:671–675. doi: 10.1016/j.micinf.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Hagan JE, Moraga P, Costa F, Capian N, Ribeiro GS, Wunder EA Jr, Felzemburgh RD, Reis RB, Nery N, Santana FS, Fraga D, Dos Santos BL, Santos AC, Queiroz A, Tassinari W, Carvalho MS, Reis MG, Diggle PJ, Ko AI. 2016. Spatiotemporal determinants of urban leptospirosis transmission: four-year prospective cohort study of slum residents in Brazil. PLoS Negl Trop Dis 10:e0004275. doi: 10.1371/journal.pntd.0004275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karande S, Bhatt M, Kelkar A, Kulkarni M, De A, Varaiya A. 2003. An observational study to detect leptospirosis in Mumbai, India, 2000. Arch Dis Child 88:1070–1075. doi: 10.1136/adc.88.12.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goarant C, Laumond-Barny S, Perez J, Vernel-Pauillac F, Chanteau S, Guigon A. 2009. Outbreak of leptospirosis in New Caledonia: diagnosis issues and burden of disease. Trop Med Int Health 14:926–929. doi: 10.1111/j.1365-3156.2009.02310.x. [DOI] [PubMed] [Google Scholar]
- 10.Pappachan MJ, Sheela M, Aravindan KP. 2004. Relation of rainfall pattern and epidemic leptospirosis in the Indian state of Kerala. J Epidemiol Community Health 58:1054. doi: 10.1136/jech.2003.018556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barcellos C, Sabroza PC. 2001. The place behind the case: leptospirosis risks and associated environmental conditions in a flood-related outbreak in Rio de Janeiro. Cad Saude Publica 17(Suppl):59–67. doi: 10.1590/S0102-311X2001000700014. [DOI] [PubMed] [Google Scholar]
- 12.Gubler DJ, Reiter P, Ebi KL, Yap W, Nasci R, Patz JA. 2001. Climate variability and change in the United States: potential impacts on vector- and rodent-borne diseases. Environ Health Perspect 109(Suppl 2):S223–S233. doi: 10.2307/3435012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barragan V, Chiriboga J, Miller E, Olivas S, Birdsell D, Hepp C, Hornstra H, Schupp JM, Morales M, Gonzalez M, Reyes S, de la Cruz C, Keim P, Hartskeerl R, Trueba G, Pearson T. 2016. High leptospira diversity in animals and humans complicates the search for common reservoirs of human disease in rural Ecuador. PLoS Negl Trop Dis 10:e0004990. doi: 10.1371/journal.pntd.0004990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barragan V, Nieto N, Keim P, Pearson T. 2017. Meta-analysis to estimate the load of Leptospira excreted in urine: beyond rats as important sources of transmission in low-income rural communities. BMC Res Notes 10:71. doi: 10.1186/s13104-017-2384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desvars A, Michault A, Chiroleu F. 2013. Influence of risk factors on renal leptospiral load in naturally infected wild black rats. Acta Trop 125:258–261. doi: 10.1016/j.actatropica.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Litvin V, Karaseva EV, Karulin BE. 1979. Leptospira distribution in the soil of a natural focus of the infection (an attempt at the radioisotopic labelling of infected voles). Zh Mikrobiol Epidemiol Immunobiol 6:74–79. (In Russian.) [PubMed] [Google Scholar]
- 17.Mason MR, Encina C, Sreevatsan S, Muñoz-Zanzi C. 2016. Distribution and diversity of pathogenic Leptospira species in peri-domestic surface waters from south central Chile. PLoS Negl Trop Dis 10:e0004895. doi: 10.1371/journal.pntd.0004895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barocchi MA, Ko AI, Reis MG, McDonald KL, Riley LW. 2002. Rapid translocation of polarized MDCK cell monolayers by Leptospira interrogans, an invasive but nonintracellular pathogen. Infect Immun 70:6926–6932. doi: 10.1128/IAI.70.12.6926-6932.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haake DA. 2006. Hamster model of leptospirosis. Curr Protoc Microbiol Chapter 12:Unit 12E.12. doi: 10.1002/9780471729259.mc12e02s02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silva EF, Santos CS, Athanazio DA, Seyffert N, Seixas FK, Cerqueira GM, Fagundes MQ, Brod CS, Reis MG, Dellagostin OA, Ko AI. 2008. Characterization of virulence of Leptospira isolates in a hamster model. Vaccine 26:3892–3896. doi: 10.1016/j.vaccine.2008.04.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nally JE, Chantranuwat C, Wu XY, Fishbein MC, Pereira MM, Da Silva JJ, Blanco DR, Lovett MA. 2004. Alveolar septal deposition of immunoglobulin and complement parallels pulmonary hemorrhage in a guinea pig model of severe pulmonary leptospirosis. Am J Pathol 164:1115–1127. doi: 10.1016/S0002-9440(10)63198-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lourdault K, Aviat F, Picardeau M. 2009. Use of quantitative real-time PCR for studying the dissemination of Leptospira interrogans in the guinea pig infection model of leptospirosis. J Med Microbiol 58:648–655. doi: 10.1099/jmm.0.008169-0. [DOI] [PubMed] [Google Scholar]
- 23.Pereira MM, Da Silva JJ, Pinto MA, Da Silva MF, Machado MP, Lenzi HL, Marchevsky RS. 2005. Experimental leptospirosis in marmoset monkeys (Callithrix jacchus): a new model for studies of severe pulmonary leptospirosis. Am J Trop Med Hyg 72:13–20. [PubMed] [Google Scholar]
- 24.Wunder EA Jr, Figueira CP, Santos GR, Lourdault K, Matthias MA, Vinetz JM, Ramos E, Haake DA, Picardeau M, Dos Reis MG, Ko AI. 2016. Real-time PCR reveals rapid dissemination of Leptospira interrogans after intraperitoneal and conjunctival inoculation of hamsters. Infect Immun 84:2105–2115. doi: 10.1128/IAI.00094-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zilber AL, Belli P, Grezel D, Artois M, Kodjo A, Djelouadji Z. 2016. Comparison of mucosal, subcutaneous and intraperitoneal routes of rat Leptospira infection. PLoS Negl Trop Dis 10:e0004569. doi: 10.1371/journal.pntd.0004569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coutinho ML, Matsunaga J, Wang LC, de la Pena Moctezuma A, Lewis MS, Babbitt JT, Aleixo JA, Haake DA. 2014. Kinetics of Leptospira interrogans infection in hamsters after intradermal and subcutaneous challenge. PLoS Negl Trop Dis 8:e3307. doi: 10.1371/journal.pntd.0003307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Lou XL, Yang HL, Guo XK, Zhang XY, He P, Jiang XC. 2012. Establishment of a leptospirosis model in guinea pigs using an epicutaneous inoculations route. BMC Infect Dis 12:20. doi: 10.1186/1471-2334-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ganoza CA, Matthias MA, Collins-Richards D, Brouwer KC, Cunningham CB, Segura ER, Gilman RH, Gotuzzo E, Vinetz JM. 2006. Determining risk for severe leptospirosis by molecular analysis of environmental surface waters for pathogenic Leptospira. PLoS Med 3:e308. doi: 10.1371/journal.pmed.0030308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vein J, Perrin A, Berny PJ, Benoit E, Leblond A, Kodjo A. 2012. Adaptation of a real-time PCR method for the detection and quantification of pathogenic leptospires in environmental water. Can J Microbiol 58:828–835. doi: 10.1139/w2012-060. [DOI] [PubMed] [Google Scholar]
- 30.Noguchi H. 1918. The survival of Leptospira (Spirochaeta) icterohaemorrhagiae in nature; observations concerning microchemical reactions and intermediary hosts. J Exp Med 27:609–625. doi: 10.1084/jem.27.5.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thaipadungpanit J, Wuthiekanun V, Chantratita N, Yimsamran S, Amornchai P, Boonsilp S, Maneeboonyang W, Tharnpoophasiam P, Saiprom N, Mahakunkijcharoen Y, Day NP, Singhasivanon P, Peacock SJ, Limmathurotsakul D. 2013. Leptospira species in floodwater during the 2011 floods in the Bangkok metropolitan region, Thailand. Am J Trop Med Hyg 89:794–796. doi: 10.4269/ajtmh.13-0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muñoz-Zanzi C, Mason MR, Encina C, Astroza A, Romero A. 2014. Leptospira contamination in household and environmental water in rural communities in southern Chile. Int J Environ Res Public Health 11:6666–6680. doi: 10.3390/ijerph110706666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Romero-Vivas CM, Thiry D, Rodriguez V, Calderón A, Arrieta G, Mattar S, Cuello M, Levett PN, Falconar AK. 2013. Molecular serovar characterization of Leptospira isolates from animals and water in Colombia. Biomedica 33(Suppl 1):S179–S184. [PubMed] [Google Scholar]
- 34.Alexander AD, Evans LB, Baker MF, Baker HJ, Ellison D, Marriapan M. 1975. Pathogenic leptospiras isolated from Malaysian surface waters. Appl Microbiol 29:30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ridzlan FR, Bahaman AR, Khairani-Bejo S, Mutalib AR. 2010. Detection of pathogenic Leptospira from selected environment in Kelantan and Terengganu, Malaysia. Trop Biomed 27:632–638. [PubMed] [Google Scholar]
- 36.Ryu E, Liu CK. 1966. The viability of leptospires in the summer paddy water. Jpn J Microbiol 10:51–57. doi: 10.1111/j.1348-0421.1966.tb00291.x. [DOI] [PubMed] [Google Scholar]
- 37.Pui CF, Bilung LM, Apun K, Su'ut L. 2017. Diversity of Leptospira spp. in rats and environment from urban areas of Sarawak, Malaysia. J Trop Med 2017:3760674. doi: 10.1155/2017/3760674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Azali MA, Yean Yean C, Harun A, Aminuddin Baki NN, Ismail N. 2016. Molecular characterization of Leptospira spp. in environmental samples from north-eastern Malaysia revealed a pathogenic strain, Leptospira alstonii. J Trop Med 2016:2060241. doi: 10.1155/2016/2060241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lall C, Kumar KV, Raj RV, Vedhagiri K, Vijayachari P. 2016. Prevalence and diversity of leptospires in different ecological niches of urban and rural areas of South Andaman Island. Microbes Environ 31:79–82. doi: 10.1264/jsme2.ME15149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vinod Kumar K, Lall C, Vimal Raj R, Vedhagiri K, Vijayachari P. 2016. Molecular detection of pathogenic leptospiral protein encoding gene (lipL32) in environmental aquatic biofilms. Lett Appl Microbiol 62:311–315. doi: 10.1111/lam.12533. [DOI] [PubMed] [Google Scholar]
- 41.Chaturongkasumrit Y, Techaruvichit P, Takahashi H, Kimura B, Keeratipibul S. 2013. Microbiological evaluation of water during the 2011 flood crisis in Thailand. Sci Total Environ 463-464:959–967. doi: 10.1016/j.scitotenv.2013.06.071. [DOI] [PubMed] [Google Scholar]
- 42.Benacer D, Woh PY, Mohd Zain SN, Amran F, Thong KL. 2013. Pathogenic and saprophytic Leptospira species in water and soils from selected urban sites in peninsular Malaysia. Microbes Environ 28:135–140. doi: 10.1264/jsme2.ME12154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saito M, Villanueva SY, Chakraborty A, Miyahara S, Segawa T, Asoh T, Ozuru R, Gloriani NG, Yanagihara Y, Yoshida S. 2013. Comparative analysis of Leptospira strains isolated from environmental soil and water in the Philippines and Japan. Appl Environ Microbiol 79:601–609. doi: 10.1128/AEM.02728-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rawlins J, Portanova A, Zuckerman I, Loftis A, Ceccato P, Willingham AL, Verma A. 2014. Molecular detection of leptospiral DNA in environmental water on St. Kitts. Int J Environ Res Public Health 11:7953–7960. doi: 10.3390/ijerph110807953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calderón A, Rodriguez V, Mattar S, Arrieta G. 2014. Leptospirosis in pigs, dogs, rodents, humans, and water in an area of the Colombian tropics. Trop Anim Health Prod 46:427–432. doi: 10.1007/s11250-013-0508-y. [DOI] [PubMed] [Google Scholar]
- 46.Vital-Brazil JM, Balassiano IT, de Oliveira FS, Costa ADD, Hillen L, Pereira MM. 2010. Multiplex PCR-based detection of Leptospira in environmental water samples obtained from a slum settlement. Mem Inst Oswaldo Cruz 105:353–355. doi: 10.1590/S0074-02762010000300020. [DOI] [PubMed] [Google Scholar]
- 47.Luchini D, Meacci F, Oggioni MR, Morabito G, D'Amato V, Gabbrielli M, Pozzi G. 2008. Molecular detection of Leptospira interrogans in human tissues and environmental samples in a lethal case of leptospirosis. Int J Legal Med 122:229–233. doi: 10.1007/s00414-007-0212-4. [DOI] [PubMed] [Google Scholar]
- 48.Aviat F, Blanchard B, Michel V, Blanchet B, Branger C, Hars J, Mansotte F, Brasme L, De Champs C, Bolut P, Mondot P, Faliu J, Rochereau S, Kodjo A, Andre-Fontaine G. 2009. Leptospira exposure in the human environment in France: a survey in feral rodents and in fresh water. Comp Immunol Microbiol Infect Dis 32:463–476. doi: 10.1016/j.cimid.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 49.Wójcik-Fatla A, Zajac V, Wasinski B, Sroka J, Cisak E, Sawczyn A, Dutkiewicz J. 2014. Occurrence of Leptospira DNA in water and soil samples collected in eastern Poland. Ann Agric Environ Med 21:730–732. doi: 10.5604/12321966.1129924. [DOI] [PubMed] [Google Scholar]
- 50.Viau EJ, Boehm AB. 2011. Quantitative PCR-based detection of pathogenic Leptospira in Hawai'ian coastal streams. J Water Health 9:637–646. doi: 10.2166/wh.2011.064. [DOI] [PubMed] [Google Scholar]
- 51.Diesch SL, McCulloch WF. 1966. Isolation of pathogenic leptospires from waters used for recreation. Public Health Rep 81:299–304. doi: 10.2307/4592702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Karaseva EV, Chernukha Yu G, Sakhartseva TF. 1977. Results of the investigation of soil for contamination with pathogenic leptospires. Folia Parasitol (Praha) 24:301–304. [PubMed] [Google Scholar]
- 53.Crawford RP, Heinemann JM, McCulloch WF, Diesch SL. 1971. Human infections associated with waterborne leptospires, and survival studies on serotype pomona. J Am Vet Med Assoc 159:1477–1484. [PubMed] [Google Scholar]
- 54.Corwin A, Ryan A, Bloys W, Thomas R, Deniega B, Watts D. 1990. A waterborne outbreak of leptospirosis among United States military personnel in Okinawa, Japan. Int J Epidemiol 19:743–748. doi: 10.1093/ije/19.3.743. [DOI] [PubMed] [Google Scholar]
- 55.Trueba G, Zapata S, Madrid K, Cullen P, Haake D. 2004. Cell aggregation: a mechanism of pathogenic Leptospira to survive in fresh water. Int Microbiol 7:35–40. [PubMed] [Google Scholar]
- 56.Katz AR, Manea SJ, Sasaki DM. 1991. Leptospirosis on Kauai—investigation of a common source waterborne outbreak. Am J Public Health 81:1310–1312. doi: 10.2105/AJPH.81.10.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stern EJ, Galloway R, Shadomy SV, Wannemuehler K, Atrubin D, Blackmore C, Wofford T, Wilkins PP, Ari MD, Harris L, Clark TA. 2010. Outbreak of leptospirosis among adventure race participants in Florida, 2005. Clin Infect Dis 50:843–849. doi: 10.1086/650578. [DOI] [PubMed] [Google Scholar]
- 58.Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, Stein C, Abela-Ridder B, Ko AI. 2015. Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis 9:e0003898. doi: 10.1371/journal.pntd.0003898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hellstrom JS, Marshall RB. 1978. Survival of Leptospira interrogans serovar Pomona in an acidic soil under simulated New Zealand field conditions. Res Vet Sci 25:29–33. [PubMed] [Google Scholar]
- 60.Andre-Fontaine G, Aviat F, Thorin C. 2015. Waterborne leptospirosis: survival and preservation of the virulence of pathogenic Leptospira spp. in fresh water. Curr Microbiol 71:136–142. doi: 10.1007/s00284-015-0836-4. [DOI] [PubMed] [Google Scholar]
- 61.Smith DJ, Self HR. 1955. Observations on the survival of Leptospira australis A in soil and water. J Hyg (Lond) 53:436–444. doi: 10.1017/S0022172400000942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khairani-Bejo S, Bahaman AR, Zamri-Saad M, Mutalib AR. 2004. The survival of Leptospira interrogans serovar Hardjo in the Malaysian environment. J Anim Vet Adv 3:123–129. [Google Scholar]
- 63.Parker J, Walker M. 2011. Survival of a pathogenic Leptospira serovar in response to combined in vitro pH and temperature stresses. Vet Microbiol 152:146–150. doi: 10.1016/j.vetmic.2011.04.028. [DOI] [PubMed] [Google Scholar]
- 64.Chang SL, Buckingham M, Taylor MP. 1948. Studies on Leptospira icterohaemorrhagiae; survival in water and sewage; destruction in water by halogen compounds, synthetic detergents, and heat. J Infect Dis 82:256–266. doi: 10.1093/infdis/82.3.256. [DOI] [PubMed] [Google Scholar]
- 65.Kadis S, Pugh WL. 1974. Urea utilization by Leptospira. Infect Immun 10:793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Leonard F, Quinn PJ, Ellis WA. 1992. Possible effect of pH on the survival of leptospires in cattle urine. Vet Rec 131:53–54. doi: 10.1136/vr.131.3.53. [DOI] [PubMed] [Google Scholar]
- 67.Takabe K, Nakamura S, Ashihara M, Kudo S. 2013. Effect of osmolarity and viscosity on the motility of pathogenic and saprophytic Leptospira. Microbiol Immunol 57:236–239. doi: 10.1111/1348-0421.12018. [DOI] [PubMed] [Google Scholar]
- 68.Yuri K, Takamoto Y, Okada M, Hiramune T, Kikuchi N, Yanagawa R. 1993. Chemotaxis of leptospires to hemoglobin in relation to virulence. Infect Immun 61:2270–2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stamm LV, Charon NW. 1988. Sensitivity of pathogenic and free-living Leptospira spp. to UV radiation and mitomycin C. Appl Environ Microbiol 54:728–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chadsuthi S, Wong-ekkabut J, Triampo W, Doungchawee G, Triampo D. 2010. Comparison of the effects of UV-A radiation on Leptospira interrogan [sic] serovar Bataviae, Canicola and Pomona. Afr J Biotechnol 9:3196–3206. [Google Scholar]
- 71.Welch AA, Mulligan A, Bingham SA, Khaw KT. 2008. Urine pH is an indicator of dietary acid-base load, fruit and vegetables and meat intakes: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk population study. Br J Nutr 99:1335–1343. doi: 10.1017/S0007114507862350. [DOI] [PubMed] [Google Scholar]
- 72.Andersen-Ranberg EU, Pipper C, Jensen PM. 2016. Global patterns of Leptospira prevalence in vertebrate reservoir hosts. J Wildl Dis 52:468–477. doi: 10.7589/2014-10-245. [DOI] [PubMed] [Google Scholar]
- 73.Kumar KV, Lall C, Raj RV, Vedhagiri K, Vijayachari P. 2015. Coexistence and survival of pathogenic leptospires by formation of biofilm with Azospirillum. FEMS Microbiol Ecol 91:fiv051. doi: 10.1093/femsec/fiv051. [DOI] [PubMed] [Google Scholar]
- 74.Bulach DM, Zuerner RL, Wilson P, Seemann T, McGrath A, Cullen PA, Davis J, Johnson M, Kuczek E, Alt DP, Peterson-Burch B, Coppel RL, Rood JI, Davies JK, Adler B. 2006. Genome reduction in Leptospira borgpetersenii reflects limited transmission potential. Proc Natl Acad Sci U S A 103:14560–14565. doi: 10.1073/pnas.0603979103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nascimento AL, Verjovski-Almeida S, Van Sluys MA, Monteiro-Vitorello CB, Camargo LE, Digiampietri LA, Harstkeerl RA, Ho PL, Marques MV, Oliveira MC, Setubal JC, Haake DA, Martins EA. 2004. Genome features of Leptospira interrogans serovar Copenhageni. Braz J Med Biol Res 37:459–477. doi: 10.1590/S0100-879X2004000400003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hu WL, Pappas CJ, Zhang JJ, Yang YY, Yan J, Picardeau M, Yang XF. 2017. The EbpA-RpoN regulatory pathway of the pathogen Leptospira interrogans is essential for survival in the environment. Appl Environ Microbiol 83:e02377-16. doi: 10.1128/AEM.02377-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lo M, Bulach DM, Powell DR, Haake DA, Matsunaga J, Paustian ML, Zuerner RL, Adler B. 2006. Effects of temperature on gene expression patterns in Leptospira interrogans serovar Lai as assessed by whole-genome microarrays. Infect Immun 74:5848–5859. doi: 10.1128/IAI.00755-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Matsunaga J, Lo M, Bulach DM, Zuerner RL, Adler B, Haake DA. 2007. Response of Leptospira interrogans to physiologic osmolarity: relevance in signaling the environment-to-host transition. Infect Immun 75:2864–2874. doi: 10.1128/IAI.01619-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Barragan VA, Mejia ME, Travez A, Zapata S, Hartskeerl RA, Haake DA, Trueba GA. 2011. Interactions of leptospira with environmental bacteria from surface water. Curr Microbiol 62:1802–1806. doi: 10.1007/s00284-011-9931-3. [DOI] [PubMed] [Google Scholar]
- 80.Vinod Kumar K, Lall C, Vimal Raj R, Vedhagiri K, Kartick C, Surya P, Natarajaseenivasan K, Vijayachari P. 2017. Overexpression of heat shock GroEL stress protein in leptospiral biofilm. Microb Pathog 102:8–11. doi: 10.1016/j.micpath.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 81.Ristow P, Bourhy P, Kerneis S, Schmitt C, Prevost MC, Lilenbaum W, Picardeau M. 2008. Biofilm formation by saprophytic and pathogenic leptospires. Microbiology 154:1309–1317. doi: 10.1099/mic.0.2007/014746-0. [DOI] [PubMed] [Google Scholar]
- 82.Chakraborty A, Miyahara S, Villanueva SY, Saito M, Gloriani NG, Yoshida S. 2011. A novel combination of selective agents for isolation of Leptospira species. Microbiol Immunol 55:494–501. doi: 10.1111/j.1348-0421.2011.00347.x. [DOI] [PubMed] [Google Scholar]
- 83.Riediger IN, Hoffmaster AR, Casanovas-Massana A, Biondo AW, Ko AI, Stoddard RA. 2016. An optimized method for quantification of pathogenic Leptospira in environmental water samples. PLoS One 11:e0160523. doi: 10.1371/journal.pone.0160523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen HW, Weissenberger G, Ching WM. 2016. Development of lyophilized loop-mediated isothermal amplification reagents for the detection of Leptospira. Mil Med 181:227–231. doi: 10.7205/MILMED-D-15-00149. [DOI] [PubMed] [Google Scholar]
- 85.Kurilung A, Chanchaithong P, Lugsomya K, Niyomtham W, Wuthiekanun V, Prapasarakul N. 2017. Molecular detection and isolation of pathogenic Leptospira from asymptomatic humans, domestic animals and water sources in Nan Province, a rural area of Thailand. Res Vet Sci 115:146–154. doi: 10.1016/j.rvsc.2017.03.017. [DOI] [PubMed] [Google Scholar]


