Abstract
Objective:
To assess the prevalence of injury of the talonavicular ligament (TNL) in ankle sprains, its anatomy and the stability of the talonavicular joint (TNJ) before and after dividing the TNL in a cadaver.
Methods:
During a prospective study of 100 patients to assess the outcome of ankle injuries, we noted high incidence of TNL injuries; we will discuss here the TNL findings. Each patient had undergone ultrasound and cone beam CT examination of the ankle. Six TNLs were dissected off fresh-frozen cadaveric feet for histological analysis. In further six cadaveric feet, the stability of the TNJ was assessed by mechanical stress before and after division of the TNL; movement at the joint was assessed by measuring the distance between the talus and navicular bone [talonavicular distance (TD)] using ultrasound. The TD was measured on ten randomly selected ultrasound images by three independent observers and repeated twice by a single observer to determine the inter- and intraobserver reliability.
Results:
21% of the patients had an injury to the TNL. Histological examination demonstrated a dense connective tissue composed of bundles of collagen in parallel arrangement along the ligament length. The interobserver and intraobserver reliability of the TD showed almost perfect agreement. Displacement at the TNJ after stress with the TNL intact measured 0.18 ± 0.08 cm and 0.29 ± 0.07 cm (p < 0.005) when divided.
Conclusion:
The TNL is surprisingly commonly injured in ankle sprains. Its anatomy and histology suggest a role in tensile force transmission during the windlass mechanism in gait.
Advances in knowledge:
Injury to the TNL is common and has not been described. Its anatomy suggests resistance to tensile forces and its injury allows excessive movement at the TNJ.
INTRODUCTION
Acute ankle injuries account for approximately 10% of all emergency department attendances.1 Several publications cover the incidence of ligament injuries, especially the lateral ligamentous complex and deltoid ligament (DL). In one study, there were anterior talofibular ligament (ATFL) injuries in 75% of patients after acute inversion ankle sprain with a combined ATFL and calcaneofibular ligament (CFL) in 41%.2 In another study, the prevalence of DL injury in patients with chronic lateral ankle instability was 36%.3 There are no studies to our knowledge investigating injury of the talonavicular ligament (TNL) in patients presenting with an ankle sprain.
The talonavicular joint (TNJ) is part of the transverse tarsal joint in the foot, which includes the calcaneocuboid joint. These joints act synchronously with the subtalar and ankle joints when walking.4 Stability of the TNJ is conferred by both static and dynamic stabilizers, including the spring ligament (SL) and tibialis posterior on the plantar aspect, but dorsally, the anatomy and structure of the TNL is poorly defined.5 The TNJ is at the apex of the longitudinal arch, which is elevated when the toes are extended and the plantar fascia is tightened during the push-off phase of walking (windlass mechanism) (Figure 1).4 We hypothesize that the TNL has a role in resisting those tensile forces dorsally and therefore becomes susceptible to frequent injury. Histological analysis and structural composition of foot and ankle ligaments have previously been used to predict function.6 In addition, TNL injury may result in TNJ instability, which may predispose to talonavicular arthritis and neighbouring joint disease. History of an ankle sprain has been associated with radiological evidence of TNJ arthritis.7
Figure 1.
The windlass mechanism and changes in foot shape. Simple illustration of the windlass mechanism and tracing from radiographs of a living foot, standing. Dotted line: toe-flexed low-arch position. Continuous line: toe-extended high-arch position. Acknowledgments to Wiley Editors for the use of the tracings taken from Hicks4 with permission from Wiley.
The aims of our study were: first, to study the importance of the TNL by reviewing the prevalence of TNL injuries in ankle sprains and its association with injury to other foot and ankle ligaments; second, to describe the anatomy and structure of the TNL and, third, to assess the stability of the TNJ following TNL injury.
METHODS AND MATERIALS
Patient study
The study was approved and monitored by the local research and ethics committee. In the period between February 2013 and November 2014 (21 months), 100 patients who arrived at the emergency department with ankle sprain were enrolled. To be included in the study, the patients had to be over 18 years of age, not pregnant and meet the Ottawa rules for ankle radiographic examination following a simple ankle sprain.8 They were discharged from the emergency department after their ankle sprain, with radiographic examination negative for fracture and managed with conservative treatment (Protection, Rest, Ice, Compression and Elevation). These patients were asked if they would like to be included in the study and undergo an ultrasound examination and extremity cone beam CT examination within 5 days of their presentation at the emergency department. All patients signed a consent form. This study includes an analysis of occult fractures and outcome assessments for up to 1 year after the injury. This material has been submitted for publication elsewhere.
During the ultrasound examination, the following ligaments were reviewed: ATFL, anterior tibiofibular ligament, CFL, DL, plantar calcaneonavicular or SL, calcaneocuboid ligament and TNL. The ligaments were examined statically and dynamically, and neovascularity was assessed using Doppler ultrasound examination. Joint effusions were recorded.
The sonograms were performed by two experienced consultant musculoskeletal radiologists with a General Electric Logiq™ E9 ultrasound machine using a 5- to 15-MHz linear array probe and an 8- to 18-MHz hockey stick probe. Static and dynamic study of the ligaments was performed. Colour Doppler examination of the ligaments was used to differentiate acute injuries from old. Oedema or fluid adjacent to the ligament was also considered as a sign of acute injury. In the absence of any sign of oedema or vascularity, ligamentous injuries were regarded as old.
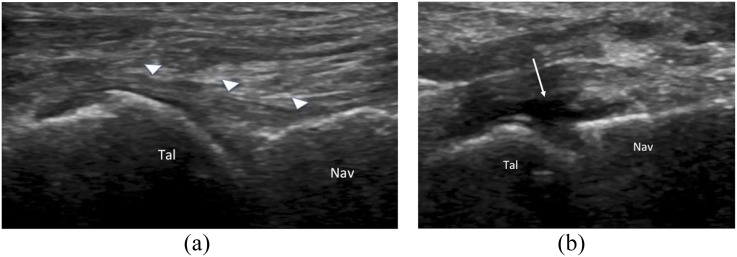
The ligamentous injuries were divided into three patterns: sprain, partial tear and complete tear. A complete tear was identified by showing discontinuity with torn ends or by the presence of a full thickness hypoechoic lesion. It is common that the ends of the torn ligament are seen in different planes and are therefore not necessarily visible in a single ultrasound section.
A partial tear was represented by a partial thickness hypoechoic lesion. A sprained ligament was represented as a ligament with increased thickness and/or irregular contours and/or inhomogeneity of its fibrillary structure. Dynamic assessment using gentle mechanical loading helped to differentiate partial from complete tears.
Cadaveric study—anatomy
One embalmed and six fresh-frozen cadaveric feet and ankles from four different cadavers were examined. All were female with an average age of 86 years. The embalmed cadaver was perfused and fixed with a mixture of ethanol, glycerol, formalin and phenol. The fresh-frozen specimens were thawed for 24 h in preparation for the study. No specimens had any apparent deformity or scars on external examination. A soft-tissue window including tendons was removed from the dorsum of the foot and part of the ankle to expose the articulations of the ankle, midtarsal, naviculocuneiform and tarsometatarsal joints to allow identification of the talonavicular articulation. Photographs were obtained of the TNL from all specimens. The TNL was dissected off the talus and navicular bone of the fresh-frozen specimens and the dimensions were measured with a ruler before being fixed in formalin for histological analysis. The specimens were sampled along both the short (transverse) and long (longitudinal) axis and embedded in paraffin wax and routinely processed. 5-µm sections were cut and stained with haematoxylin–eosin and toluidine blue.
Cadaveric study—stability
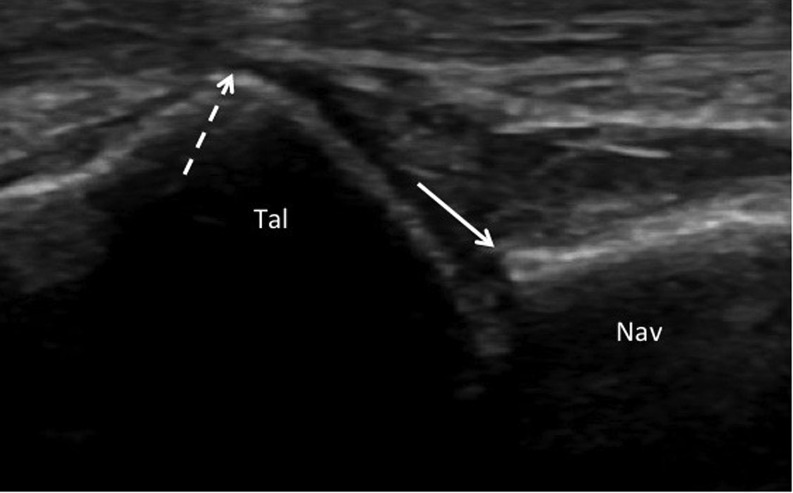
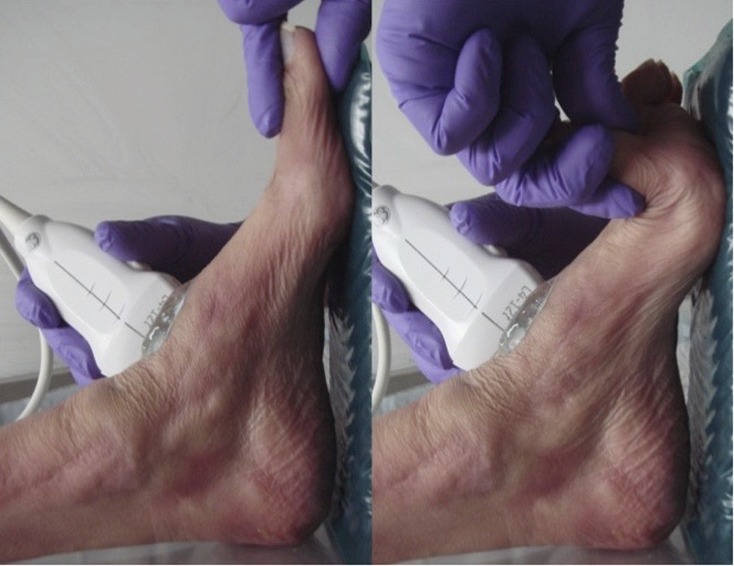
A further six fresh-frozen specimens from three different cadavers with an average age of 80 years (two females and 1 male) without any evident deformity or functional impairment of the first metatarsophalangeal joint were positioned on a 90° ankle support, and the TNL was imaged using a portable GE Healthcare Logic e ultrasound system with 4- to 12-MHz linear array probe. As landmarks for the ultrasound measurement, we identified the dorsal proximal angle of the navicular bone and the proximal edge of the talar head cartilage at the level of the dorsal lip (Figure 2). The probe was positioned on the dorsal aspect of the TNJ where a greater exposure of talar cartilage was observed. The distance between our two landmarks [the talonavicular distance (TD)] was measured with the big toe metatarsophalangeal joint at rest and following full extension (“stress” test) to reproduce loading at the TNJ as per the windlass mechanism during the push-off phase of walking (Figure 3). The TNL was then divided percutaneously under ultrasound guidance via a medial stab incision with a No 15 blade and the same measurements were obtained at rest and after stress of the joint. TNJ displacement was defined as the difference between the stressed TD with the ligament intact and then divided. At the end of this set of measurements, the TNL and joint were openly exposed to ensure that the ligament was completely divided. The TD was measured on ten random ultrasound images by three independent observers and repeated twice by a single observer to determine inter- and intraobserver reliability.
Figure 2.
Ultrasound image of the talonavicular joint during “stress” test. The solid white arrow shows the proximal aspect of the cortical bone of the navicular, and the dashed white arrow shows the edge of the cartilage at the level of the dorsal lip of the talar head. Nav, navicular; Tal, talus.
Figure 3.
Demonstration of the “stress” test by extending the big toe metatarsophalangeal joint.
Statistics
Results were described with a mean and standard deviation. Paired t-test and repeated-measures analysis of variance (paired) and Tukey multiple comparisons post-test were used. The inter- and intraobserver reliability were calculated using the intraclass correlation. The intraclass correlation under 0.2 was defined as slight agreement, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial and 0.81–1.0 as almost perfect.9 Statistics were calculated using GraphPad® Instat software (GraphPad Software Inc., La Jolla, CA) and MedCalc® statistical software (MedCalc Software bvba, Ostend, Belgium).
RESULTS
Patient study
The mean age of our patients was 33 years, with a range from 18 to 68 years. 55 patients (55%) were males. TNL injury was the fourth commonest (21%) after injuries to the lateral (ATFL, CFL) and medial ankle (DL) ligaments (Table 1). A complete tear of the TNL occurred in 43% of the patients with an injury to the TNL (Table 1 and Figure 4).
Table 1.
Number of patients with ligamentous injuries out of our 100-patient cohort, rounded to the nearest integer
| Ligament | Total | c | %c | p | %p | s | %s |
|---|---|---|---|---|---|---|---|
| ATFL | 83 | 67 | 81% | 9 | 11% | 7 | 8% |
| DL | 39 | 3 | 8% | 12 | 31% | 24 | 61% |
| CFL | 26 | 8 | 31% | 8 | 31% | 10 | 38% |
| TNL | 21 | 9 | 43% | 2 | 9% | 10 | 48% |
| ATiFL | 19 | 15 | 79% | 0 | 0% | 4 | 21% |
| SL | 14 | 3 | 21% | 3 | 21% | 8 | 58% |
| CCL | 3 | 3 | 100% | 0 | 0% | 0 | 0% |
%c, %p and %s, the prevalence of the type of injury in the relative subpopulation of each ligament; ATFL, anterior talofibular ligament; ATiFL, anterior tibiofibular ligament; c, number of patients with complete tear; CCL, calcaneocuboid ligament; CFL, calcaneofibular ligament; DL, deltoid ligament; p, number of patients with a partial tear; s, number of patients with a sprained ligament; SL, spring ligament; TNL, talonavicular ligament.
Figure 4.
Ultrasound images showing (a) a normal talonavicular ligament (TNL) and (b) a complete tear of the TNL. Solid white arrow heads show ligament and fine white arrow shows effusion and site of ligamentous injury. Nav, navicular; Tal, talus.
In the subpopulation of patients with TNL injury (Table 2), 86% had an associated ATFL injury. In one of the three patients without an associated acute ATFL lesion, there was a chronic one. An associated DL injury was found in 48% of the patients and 38% had both ATFL and DL injury. SL injury occurred in 14% of the patients. In two cases where no TNL injury was identified, a joint effusion was detected. Of the 37 patients with ATFL and DL injuries, 12 (32%) had a concomitant injury to the TNL or joint effusion.
Table 2.
Nature of talonavicular ligament (TNL) injuries and association with other ligamentous injury
| Case | TNL | ATFL | CFL | DL | SL |
|---|---|---|---|---|---|
| 1 | s | c | c | ||
| 2 | s | c | |||
| 3 | c | c | c | p | |
| 4 | c | c | |||
| 5 | s | s | |||
| 6 | p | c | p | p | s |
| 7 | c | ||||
| 8 | s | c | c | ||
| 9 | s | c | |||
| 10 | c | c | |||
| 11 | c | c | s | ||
| 12 | c | p | s | ||
| 13 | c | p | s | ||
| 14 | p | c | |||
| 15 | c | s | |||
| 16 | s | c | |||
| 17 | s | c | p | s | |
| 18 | c | c | s | ||
| 19 | s | c | s | ||
| 20 | s | s | |||
| 21 | s | s | c |
ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; DL, deltoid ligament; c, complete tear; p, partial tear; s, sprain; SL, spring ligament.
Cadaveric study—anatomy
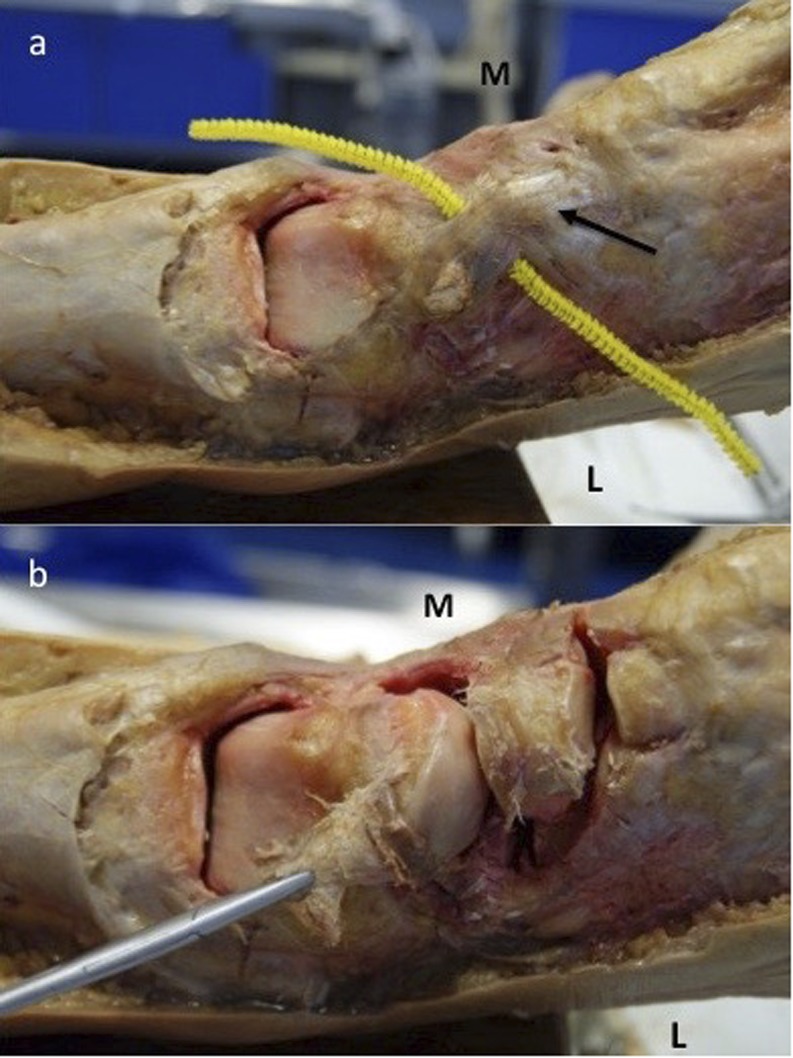
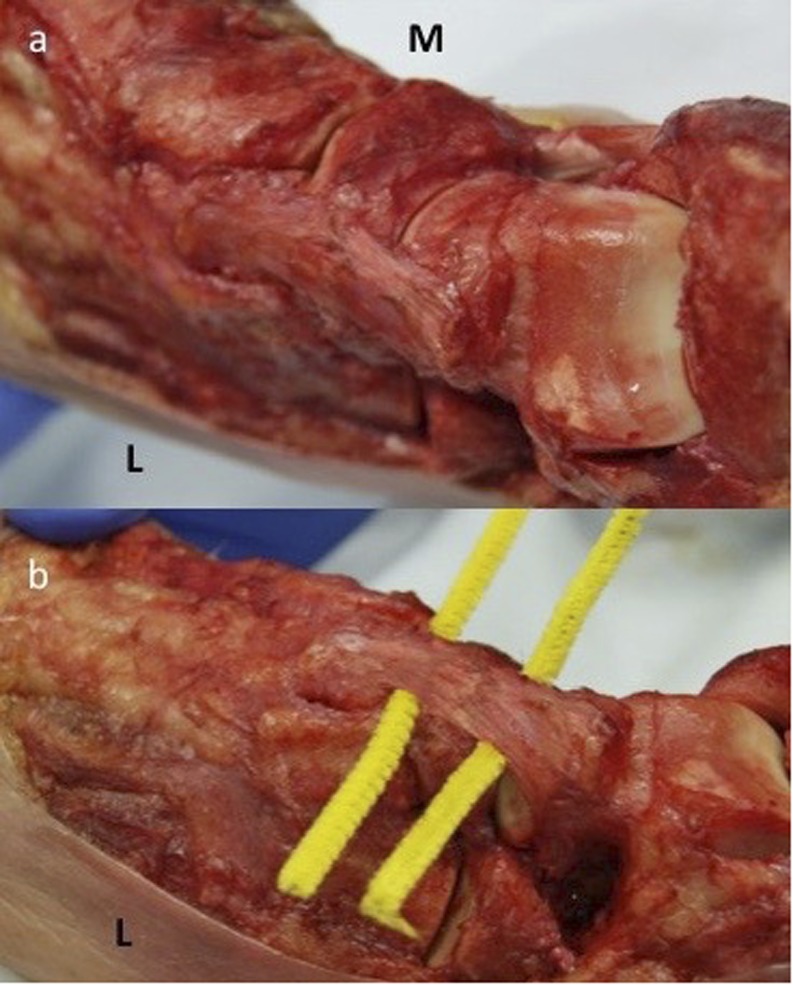
From our cadaveric dissections, the TNL had a well-defined and typical structure. It originated from the distal dorsolateral aspect of the talar neck and inserted into the dorsal mid-portion of the navicular where it continued as the naviculointermediate cuneiform ligament (Figures 5 and 6). It had a broader proximal origin and narrower distal insertion almost trapezoid shaped. The width at the origin was 2.1 ± 0.2 cm; the width at the insertion was 1.3 ± 0.2 cm; and the overall length was 2.6 ± 0.2 cm.
Figure 5.
Talonavicular ligament (TNL) of an embalmed cadaver. (a) Front view with a pipecleaner marker underneath the TNL and naviculocuneiform ligaments intact. (b) Front view with the TNL dissected off its insertion and naviculocuneiform ligaments divided. Arrow demonstrates the naviculointermediate cuneiform ligament. L, lateral; M, medial.
Figure 6.
Talonavicular ligament of a fresh-frozen cadaver. (a) Front/medial view with the naviculointermediate cuneiform ligament intact. (b) Front/lateral view with pipecleaner markers at the talonavicular and naviculointermediate cuneiform joint showing its dorsolateral origin. L, lateral; M, medial.
Histological examination of six of the fresh frozen specimens showed that the structure of the ligament was not uniform, with differences in collagen structure and fibroblast cellularity. Samples of two specimens included an area of ligament insertion into the navicular bone. Dense connective tissue composed of bundles of collagen was seen along the length of the ligament, particularly centrally (Figure 7); these contained scattered fibroblast-like cells with spindle-shaped nuclei and indistinct cytoplasm. There was a parallel arrangement of collagen fibres. More superficially, there was more ground substance and collagen bundles were less prominent. Where the ligament inserted into the bone, there was loss of parallel arrangement of collagen bundles and cells had more ovoid nuclei; there was fibrocartilaginous metaplasia above the line of calcification where the ligament inserted into the bone (Figure 8).
Figure 7.
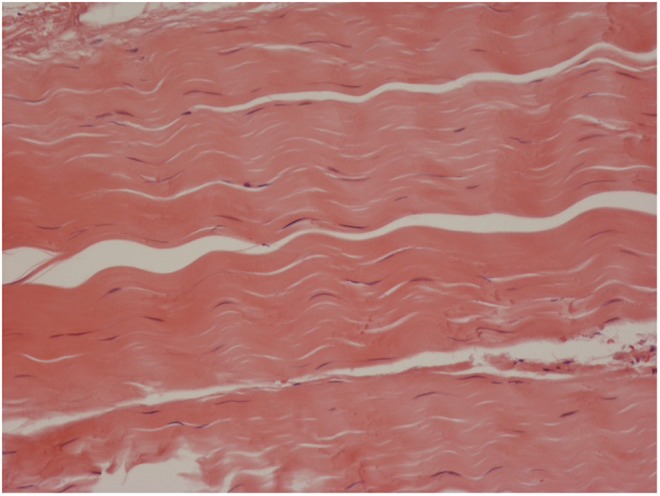
Dense connective tissue in talonavicular ligament composed of collagen bundles with a parallel arrangement of collagen fibres. Haematoxylin–eosin: original magnification ×400.
Figure 8.
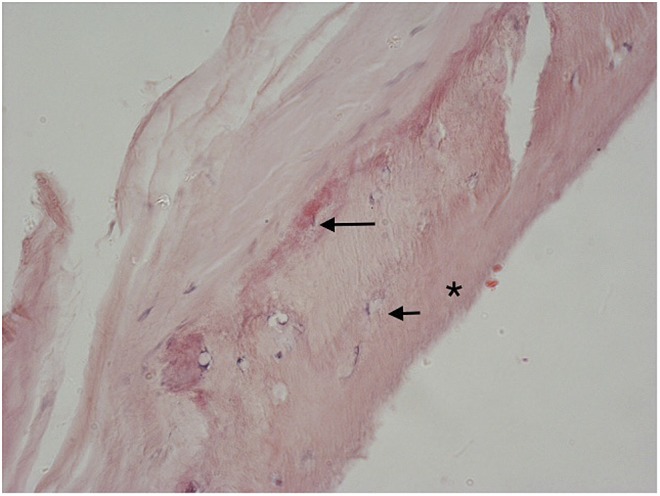
Area of talonavicular ligament insertion into bone (*) in which there are osteocyte nuclei (short arrow). There is a line of calcification (long arrow) at the point of insertion into bone above which there is loss of the parallel arrangement of collagen fibres in the ligament. Haematoxylin–eosin: original magnification ×400.
Cadaveric study—stability
The TD of the six specimens with the ligament intact measured 0.82 ± 0.10 cm at rest [intact rest (IR)] and 1.0 ± 0.16 cm with stress [intact stress (IS)]. With the ligament divided, it measured 0.88 ± 0.16 cm at rest [divided rest (DR)] and 1.16 ± 0.18 cm with stress [divided stress (DS)]. Significant differences were found between all pair comparisons apart from IR vs DR (IR vs IS p < 0.01, DR vs DS p < 0.001, IS vs DS p < 0.01, IR vs DS p < 0.001, IS vs DR p < 0.05). TNJ displacement measured 0.18 ± 0.08 cm when the ligament was intact and 0.29 ± 0.07 cm when the ligament was divided (p < 0.005). The inter- and intraobserver reliability of our ultrasound measure (TD) showed almost perfect agreement (Table 3).
Table 3.
Inter- and intraobserver reliability (intraclass correlation ± 95% confidence interval)
| Observer reliability | Talonavicular distance |
|---|---|
| Interobserver | 0.999 (0.996, 0.999) |
| Intraobserver | 0.999 (0.991, 0.998) |
DISCUSSION
We have found that TNL injury is surprisingly common (21%) following an ankle sprain with 43% of the cases being complete tears. SL injury was less common (14%), with 22% of these being complete tears. The prevalence of injury of the other ligaments such as the ATFL was in keeping with existing literature.2,3 A series of nine cases of acquired flat foot due to isolated SL insufficiency has been previously described with two of those requiring reconstructive surgery.10 Therefore, early diagnosis and treatment of such ligament injuries may improve patient outcomes and reduce the risk of surgical intervention.
Ultrasonography is a relatively inexpensive and valid method to assess ankle ligaments, and there are several studies regarding its accuracy. In a study published in 2010 using arthroscopy as the gold standard, ultrasound with a 8-MHz probe showed a 91% diagnostic accuracy for an acute ATFL injury where MRI gave a 97% accuracy.11 This article used a low-frequency ultrasound probe which will diminish accuracy and did not rely on dynamic or colour Doppler assessment. The reliability of MRI for detection of ATFL injuries in chronic lateral instability compared with arthroscopic findings as interpreted by two observers showed an accuracy of 86.1% and 78.5%, respectively.12 In this study, the sensitivity was found to be 100% for mid-substance tears but poor for injuries at the talar and fibular attachments.12 More recently, the sensitivity, specificity and accuracy of ultrasound using 5- to 17-MHz probes for detecting chronic injury to the ATFL were 98.9%, 96.2% and 84.2%, respectively, using intraoperative findings as the Cheng et al13 study. These figures rival the best reported for MRI. The accuracy of ultrasound in the study of TNL injury has never been studied since it is not a ligament that was known to be injured or ever repaired to provide an intraoperative reference standard. It is likely, however, due to its superficial position, that ultrasound has a diagnostic accuracy similar to that of ATFL in assessing TNL injuries.
In our study, we have used colour Doppler to differentiate acute injuries from chronic although the value of colour Doppler has not been described and clearly recognized for this purpose. The use of colour Doppler is widely recognized in rheumatology to assess synovial vascularity and more in general to assess the vascularity of a lesion.14 Using these criteria, we have considered those with some neovascularity as new injuries and those without as old. We have not found any studies describing the use of colour or power Doppler to differentiate old from new ligamentous injuries in ankle sprains. Ultrasonography can also identify TNJ effusion but cannot study the whole joint, cartilage or bone oedema; for these structures, MRI examination is better than ultrasound.
The TNJ is the only joint in the foot with a ball-and-socket shape, whereas the others are hinge joints.15 The structures forming the socket, sometimes called “acetabulum tali”, are the navicular bone, the calcaneus and the superomedial part of the calcaneonavicular ligament, better known as the SL.16 This gives the TNJ multiaxial degrees of movement, whereas the other joints have limited movements, determined by their structure.15 The TNJ forms part of the mid-tarsal joint complex, and together with the calcaneocuboid joint, they provide rotation between anterior and posterior parts of the foot.15
In normal walking, there is a continuous alternate passage from a condition where the foot has a low arch, is relaxed and is freely moving with an unlocked mobile mechanism in order to adapt to uneven surfaces, to a condition in which the foot is packed in a rigid position of high arch and locked with a stiff lever arm to push-off with. The longitudinal arch of the foot rises through the windlass mechanism applied to the plantar aponeurosis (PA), as first explained by Hicks4 many years ago in “The mechanics of foot”. The PA divides in the forefoot into five bundles that connect the calcaneus to the proximal phalanges through the plantar plates, most importantly to the big toe.17 When the big toe is extended, which is the position in which the big toe is in prior to the push-off of walking, the PA is pulled forward, with a consequent shortening and tightening that determines a rise of the longitudinal arch in a closed packed position.
The rising of the arch, even of just a few degrees, implies a change in the shape of the foot and a movement in the mid-tarsal bones, particularly at the level of the TNJ (Figure 1).15 The mechanical stress produced by the change in shape through the windlass mechanism, consistent with a triangular truss getting tighter, with a more acute apical angle (increased height and shorter base), may be absorbed also by the TNJ.
In our study, we found that the TNL has a typical structure composition to other foot and ankle ligaments consisting of collagen bundles in the central area of the ligament.16 We also found a parallel arrangement of the collagen bundles along the length of the ligament, particularly centrally where they were densely packed, suggesting a role in tensile force transmission such as when the longitudinal arch of the foot is raised during gait. In supination-adduction and supination-external rotation ankle injuries, the foot is in a position of supination with a high arch.18 These circumstances may overstress and acutely damage the TNL. This could also explain the lower prevalence of SL injuries, as that ligament is in a lower position with respect to the apex of the triangular truss, which in inversion injuries to the ankle will not be placed under such stress. Ligaments around the foot and ankle were previously divided into having three different morphological configurations: densely packed parallel collagen bundles, mixed (tight and loose) parallel bundles of collagen and interlaced.6 Dense ligaments can resist high tensile forces and were found mostly in the lateral compartment, in the tarsal canal and the anterior tibiofibular ligament. Mixed ligaments, which include the talocalcaneal oblique ligament, have a possible role to support the dynamic positioning of the foot on the ground and proprioception. Interlaced ligaments, seen at the insertion of the DL, have an arrangement of fibres that has evolved to counteract tension in multiple directions.
The landmarks for measuring the TD are relatively easy to identify with ultrasound and this “new” measure has shown an excellent reliability. Once identified with ultrasound the two landmarks it is important to maintain the exact same position of the probe before and after the “stress” test to ensure that the TD is only the result of the test and not of the movement of the probe. This can be achieved by holding the probe aligned in the same direction while keeping the dorsal proximal angle of the navicular bone always focused in the ultrasound image while performing the test at a moderate to slow speed.
We have demonstrated by ultrasound examination that division of the TNL results in increased TNJ movement and displacement when the joint is stressed by extending the big toe at the metatarsophalangeal joint compared with when the ligament is intact. Although the difference was statistically significant, it was small, averaging just over 1 mm. This “instability” following division of the TNL, which is a static stabiliser, can occur on every step the patient takes especially during the push-off phase. The displacement at the TNJ could therefore be considerably greater when accounting for the axial loading and the weight of the body whilst walking, although we could not investigate this in our study. A limitation of our study is the relatively small and poorly representative population in terms of age and gender for the cadaver study. The consequences of a TNL injury on foot and ankle disease and patient outcomes are unknown. Injury/insufficiency of the TNL may alter the biomechanics of the foot, cause symptoms and result in later degenerative changes necessitating surgical intervention.
An interesting study from primary care included 206 patients with an average age of 37 years who underwent radiological investigations (conventional radiographs and MRI) of the foot and ankle, 6 months to 1 year after sustaining an ankle sprain.7 This demonstrated the presence of osteophytes at the TNJ in 10.2% of the cases, sclerosis in 36.5%, joint space narrowing in 8.6%, and Kellgren and Lawrence arthritis score of ≥2 in 5.6%. No radiological differences were found between patients with and without complaints, although the results were not analysed for specific complaints and the physical examination findings were not presented.
Arthritis of the TNJ can have consequences on the subtalar and calcaneocuboid joint movement and foot and ankle function since we know that fusion of the TNJ can limit subtalar and calcaneocuboid motion to <8%.19
The TNL is surprisingly commonly injured in ankle sprains. Its anatomy and histology suggest a role in tensile force transmission during the windlass mechanism in gait. Its complete tear causes increased displacement of the TNJ when under stress and may be implicated in later joint arthritis and foot and ankle symptomatology. It may be useful to include the TNL in the checklist of ankle and foot examination and imaging, and if injured, early treatment might include immobilization. Further studies are required to assess the significance of TNL injury in the outcome of ankle sprains.
Contributor Information
Miriam De Dea, Email: dedeamiriam@gmail.com.
Constantinos L Loizou, Email: con.loizou@doctors.org.uk.
Georgina M Allen, Email: georgina.allen@gtc.ox.ac.uk.
David J Wilson, Email: davidwilson.stlukes@btconnect.com.
Nick Athanasou, Email: nick.athanasou@ouh.nhs.uk.
Yoshinobu Uchihara, Email: y-uchihara@naramed-u.ac.jp.
Paul Cooke, Email: oxfordfoot@aol.com.
Thomas Cosker, Email: thomas.cosker@dpag.ox.ac.uk.
REFERENCES
- 1.Langner I, Frank M, Kuehn JP, Hinz P, Ekkernkamp A, Hosten N, et al. Acute inversion injury of the ankle without radiological abnormalities: assessment with high-field MR imaging and correlation of findings with clinical outcome. Skeletal Radiol 2011; 40: 423–30. doi: https://doi.org/10.1007/s00256-010-1017-y [DOI] [PubMed] [Google Scholar]
- 2.Khor YP, Tan KJ. The anatomic pattern of injuries in acute inversion ankle sprains: a magnetic resonance imaging study. Orthop J Sports Med 2013; 1: 2325967113517078. doi: https://doi.org/10.1177/2325967113517078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chun KY, Choi YS, Lee SH, Kim JS, Young KW, Jeong MS, et al. Injury in chronic lateral ankle instability: magnetic resonance imaging evaluation at 3T and comparison with arthroscopy. Korean J Radiol 2015; 16: 1096–103. doi: https://doi.org/10.3348/kjr.2015.16.5.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hicks JH. The mechanics of the foot. II. The plantar aponeurosis and the arch. J Anat 1954; 88: 25–30. [PMC free article] [PubMed] [Google Scholar]
- 5.Sammarco VJ. The talonavicular and calcaneocuboid joints: anatomy, biomechanics, and clinical management of the transverse tarsal joint. Foot Ankle Clin 2004; 9: 127–45. doi: https://doi.org/10.1016/S1083-7515(03)00152-9 [DOI] [PubMed] [Google Scholar]
- 6.Rein S, Hagert E, Schneiders W, Fieguth A, Zwipp H. Histological analysis of the structural composition of ankle ligaments. Foot Ankle Int 2015; 36: 211–24. doi: https://doi.org/10.1177/1071100714554003 [DOI] [PubMed] [Google Scholar]
- 7.van Ochten JM, Mos MC, van Putte-Katier N, Oei EH, Bindels PJ, Bierma-Zeinstra SM, et al. Structural abnormalities and persistent complaints after an ankle sprain are not associated: an observational case control study in primary care. Br J Gen Pract 2014; 64: e545–53. doi: https://doi.org/10.3399/bjgp14X681349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Reardon M, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA 1993; 269: 1127–32. doi: https://doi.org/10.1001/jama.269.9.1127 [DOI] [PubMed] [Google Scholar]
- 9.Landis JR, Koch GC. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. doi: https://doi.org/10.2307/2529310 [PubMed] [Google Scholar]
- 10.Tryfonidis M, Jackson W, Mansour R, Cooke PH, Teh J, Ostlere S, et al. Acquired adult flat foot due to isolated plantar calcaneonavicular (spring) ligament insufficiency with a normal tibialis posterior tendon. Foot Ankle Surg 2008; 14: 89–95. doi: https://doi.org/10.1016/j.fas.2007.11.005 [DOI] [PubMed] [Google Scholar]
- 11.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol 2010; 39: 41–7. doi: https://doi.org/10.1007/s00256-009-0767-x [DOI] [PubMed] [Google Scholar]
- 12.Kim YS, Kim YB, Kim TG, Lee SW, Park SH. Reliability and validity of magnetic resonance imaging for evaluation of the anterior talofibular ligament in patients undergoing ankle arthroscopy. Arthroscopy 2015; 31: 1540–7. doi: https://doi.org/10.1016/j.arthro.2015.02.024 [DOI] [PubMed] [Google Scholar]
- 13.Cheng Y, Cai Y, Wang Y. Value of ultrasonography for detecting chronic injury of the lateral ligaments of the ankle joint compared with ultrasonography findings. Br J Radiol 2014; 87: 20130406. doi: https://doi.org/10.1259/bjr.20130406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fukae J, Tanimura K, Atsumi T, Koike T. Sonographic synovial vascularity of synovitis in rheumatoid arthritis. Rheumatology (Oxford) 2014; 53: 586–91. doi: https://doi.org/10.1093/rheumatology/ket311 [DOI] [PubMed] [Google Scholar]
- 15.Hicks JH. The mechanics of the foot. I. The joints. J Anat 1953; 87: 345–57. [PMC free article] [PubMed] [Google Scholar]
- 16.Davis WH, Sobel M, DiCarlo EF, Torzilli PA, Deng X, Geppert MJ, et al. Gross, histological, and microvascular anatomy and biomechanical testing of the spring ligament complex. Foot Ankle Int 1996; 17: 95–102. doi: https://doi.org/10.1177/107110079601700207 [DOI] [PubMed] [Google Scholar]
- 17.Chen DW, Li B, Aubeeluck A, Yang YF, Huang YG, Zhou JQ, et al. Anatomy and biomechanical properties of the plantar aponeurosis: a cadaveric study. PLoS One 2014; 9: e84347. doi: https://doi.org/10.1371/journal.pone.0084347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg 1950; 60: 957–85. [PubMed] [Google Scholar]
- 19.Astion DJ, Deland JT, Otis JC, Kenneally S. Motion of the hindfoot after simulated arthrodesis. J Bone Joint Surg Am 1997; 79: 241–6. doi: https://doi.org/10.2106/00004623-199702000-00012 [DOI] [PubMed] [Google Scholar]