Abstract
Objective:
To evaluate the benefit of adjuvant radiotherapy (RT) after surgical resection for extrahepatic bile duct (EHBD) cancer.
Methods:
From 1997 to 2015, 59 patients with EHBD cancer were the subject of this study; 36 patients not undergoing adjuvant treatment after surgery (observation group) and 23 patients receiving adjuvant RT (RT group) were compared. Microscopic residual disease (R1) was in 9 (25%) patients and 5 (22%) patients, and macroscopic residual disease (R2) was in 2 (6%) patients and 6 (26%) patients in the observation and RT groups, respectively. Adjuvant RT was delivered to the tumour bed and regional lymph nodes up to 50.4 Gy (range, 45–61 Gy).
Results:
With a median follow-up of 19 months, local recurrence was observed in 10 (28%) patients and 2 (9%) patients in the observation and RT groups, respectively. On univariate analysis, the 5-year local recurrence-free survival (LRFS) rates were 50% in the observation group and 54% in the RT group (p = 0.401). The 5-year overall survival (OS) rates were 29.3% in the observation group and 26.3% in the RT group (p = 0.602). On multivariable analysis, however, adjuvant RT significantly improved LRFS [hazard ratio (HR), 0.310; 95% confidence interval (CI), 0.100–0.963; p = 0.043] and had a trend towards increased OS (HR, 0.491; 95% CI, 0.219–1.102; p = 0.085). Resection margin (RM) status was also correlated with LRFS (HR for R1 6.134, 95% CI 2.051–18.344; and HR for R2 18.551, 95% CI 3.680–93.520; p < 0.001) and OS (HR for R1 1.816, 95% CI 0.853–3.867; and HR for R2 3.564, 95% CI 1.175–10.809; p = 0.054).
Conclusion:
RM status was a significant prognosticator of EHBD cancer, and adjuvant RT improved local control rate; thereby, survival rate might be increased.
Advances in knowledge:
The benefit of adjuvant RT in EHBD cancer was demonstrated via comparison with observation group.
INTRODUCTION
Extrahepatic bile duct (EHBD) cancer is a rare malignancy. However, the biliary tract cancer including gallbladder is the ninth common malignancy in Korea.1 Prognosis of EHBD cancer is generally poor; the median overall survival (OS) is about 20 months.2 Surgery provides the only chance for cure with varying resectability rates of 25–91% depending on tumour location.3–6 However, obtaining a negative resection margin (RM) is a challenge,7,8 and microscopic (R1) and macroscopic (R2) residual diseases are observed in 20–40% and 4–64%, respectively.9–15
Many studies have revealed that positive RM of EHBD cancer is directly associated with high local recurrence (LR) rate.9,11,15,16 As a result, LR is a major pattern of failure in EHBD cancer.17 In spite of the high LR rate, the utility of adjuvant radiotherapy (RT) for EHBD cancer has been sparse.2 Administration of adjuvant RT may increase local control rate, and improved local control might result in survival benefit.10,18,19 Because of the rarity of the disease, however, no prospective randomized controlled trials comparing adjuvant RT with observation have been performed, and retrospective studies have yielded conflicting results with insufficient evidences supporting the survival benefit of adjuvant RT.18,20–22
In this study, we retrospectively analyzed the effect of adjuvant RT on local relapse-free survival and OS for patients with EHBD cancer treated with surgical resection with or without adjuvant RT.
METHODS AND MATERIALS
Study population
This study was approved by the institutional review board (EUMC 2016-05-012). From 1997 to 2015, 59 patients who were diagnosed with adenocarcinoma of EHBD and underwent surgical resection followed by adjuvant RT or not were identified.
Treatment
All patients were restaged pathologically, according to American Joint Committee on Cancer 7th edn.23 There were no patients who received neoadjuvant treatment in this study. Surgeons decided the surgical procedure for patients in accordance with site and extension of the tumour. Referral for adjuvant RT was carried out at the discretion of the attending surgeon; but, RM, age, performance status and patient preference were considered in the decision-making.
Follow-up
Patients were followed up every 3 months for 2 years, and every 6 months thereafter. Routine follow-up methods included physical examination, laboratory screening and simple chest X-ray. Abdominal/pelvic CT scan was performed every 3 months in the initial 1–2 years and repeated every 6 months thereafter. If recurrence was suspected, whole-body positron emission tomography-CT scan and chest CT scan were performed for further evaluations.
Statistical analysis
Exact χ2 test was performed to compare categorical variables between the observation and RT groups. Cox proportional hazards regression was used to determine univariate and multivariable hazard ratios (HRs) for local recurrence-free survival (LRFS) and OS. LRFS was defined as the time period from the date of surgery to the date of treatment failure in the surgical bed. OS was defined as the time period from the date of surgery to the date of death or last follow-up. Analyses were carried out using the SPSS® Statistics software v. 18.0 (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL). A two-tailed p < 0.05 was considered statistically significant.
RESULTS
Patient and treatment characteristics
Patient and tumour characteristics according to receipt of adjuvant RT are summarized in Table 1. Median age of all patients was 65 years. Patients ≥65 years of age were more common in the observation group (67% vs 30%, p = 0.008).
Table 1.
Patient and tumour characteristics
| Variables | Number of patients (%) |
p-value | |
|---|---|---|---|
| Observation (n = 36) | RT (n = 23) | ||
| Age (years) | |||
| <65 | 12 (33.3) | 16 (69.6) | 0.008 |
| ≥65 | 24 (66.7) | 7 (30.4) | |
| Sex | |||
| Male | 21 (58.3) | 11 (47.8) | 0.593 |
| Female | 15 (41.7) | 12 (52.2) | |
| Performance status (ECOG) | |||
| 0–1 | 29 (80.6) | 21 (91.3) | 0.460 |
| 2–3 | 7 (19.4) | 2 ( 8.7) | |
| Surgery | |||
| Bile duct resection with hepatectomy | 6 (16.7) | 7 (30.4) | 0.136 |
| Bile duct resection | 5 (13.9) | 6 (26.1) | |
| Pancreaticoduodenectomy | 25 (69.4) | 10 (43.5) | |
| RM | |||
| R0 | 25 (69.4) | 12 (52.2) | 0.107 |
| R1 | 9 (25.0) | 5 (21.7) | |
| R2 | 2 (5.6) | 6 (26.1) | |
| Tumour location | |||
| Non-hilar | 30 (83.3) | 12 (52.2) | 0.017 |
| Hilar | 6 (16.7) | 11 (47.8) | |
| Differentiation | |||
| Well | 3 (8.3) | 3 (13.0) | 0.324 |
| Moderate | 22 (61.1) | 16 (69.6) | |
| Poor | 11 (30.6) | 3 (13.0) | |
| Unknown | 0 (0.0) | 1 (4.3) | |
| T stage | |||
| T1–2 | 19 (52.8) | 14 (60.9) | 0.599 |
| T3–4 | 17 (47.2) | 9 (39.1) | |
| N stage | |||
| N0 | 21 (58.3) | 15 (65.2) | 0.785 |
| N1 | 15 (41.7) | 8 (34.8) | |
| Perineural invasion | |||
| No | 5 (13.9) | 6 (26.1) | 0.730 |
| Yes | 20 (55.6) | 15 (65.2) | |
| Unknown | 11 (30.6) | 2 ( 8.7) | |
ECOG, Eastern Cooperative Oncology Group; RM, resection margin.
13, 11 and 35 patients underwent bile duct resection with hepatectomy, bile duct resection and pancreaticoduodenectomy, respectively. Clear RM (R0) was obtained in 25 (69%) patients in the observation group and 12 (52%) patients in the RT group. R1 resection was observed in 9 (25%) patients and 5 (22%) patients, and R2 resection was observed in 2 (6%) patients and 6 (26%) patients in the observation and RT groups, respectively. Even though RM status was not statistically different, more patients in the RT group underwent R2 resection (26% vs 6%).
In the RT group (n = 23), RT was delivered to the tumour bed and regional lymph nodes including the porta hepatis, pericholedochal, retrocaval and aortocaval lymph nodes according to the location of the primary tumour. The total dose was from 45 Gy to 61 Gy (median, 50.4 Gy) in 1.8–2.0 Gy/fraction for the tumour bed and 45 Gy in 1.8 Gy/fraction for the regional lymph nodes. 15 (65%) patients in the RT group received 5-fluorouracil- or gemcitabine-based chemotherapy during RT (n = 7), during and after RT (n = 6) or after RT (n = 2). Among eight patients who received adjuvant chemotherapy after RT, enteric-coated tegafur/uracil was given for 1 year after RT or until progression in four patients, 5-fluorouracil for four cycles in three patients and gemcitabine for six cycles in one patient.
Patients with hilar tumour were more likely to receive adjuvant RT than patients with more distally located tumour (65% vs 29%, p = 0.017). No differences were observed between the groups with respect to sex, T stage and N stage.
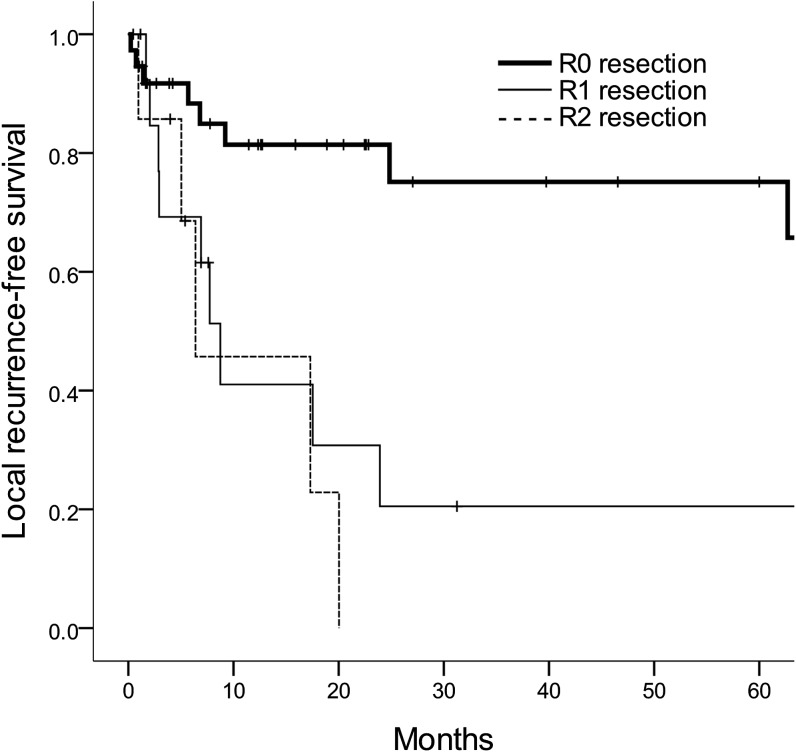
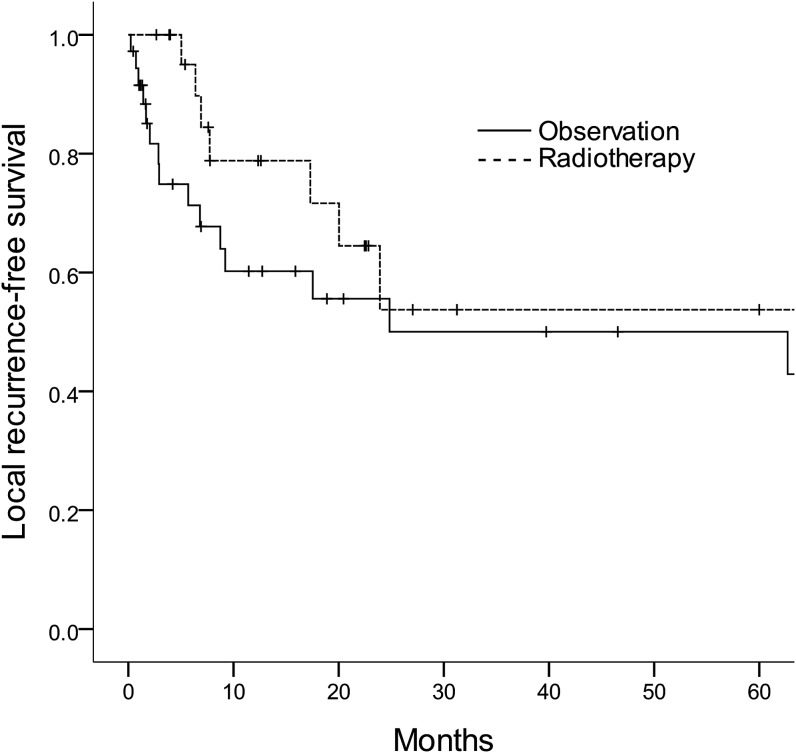
Treatment outcome
Median follow-up was 19 months (range, 1–222 months) for all patients and 43 months (range, 11–178 months) for survivors. The median LFRS and 5-year LRFS rate were 63 months and 52%, respectively. On univariate analysis for LRFS, RM status and T stage were significant prognostic factors (p = 0.003 and 0.002, respectively). When age, RM status, tumour location, T stage, N stage and RT were incorporated into a multivariable analysis, RM status was still correlated with LRFS; the 5-year LRFS rates of R0, R1 and R2 resection were 75%, 21% and 0%, respectively [HR for R1 6.134, 95% confidence interval (CI) 2.051–18.344; and HR for R2 18.551, 95% CI 3.680–93.520; p < 0.001] (Figure 1). Although adjuvant RT did not show significant effect on LFRS on univariate analysis, adjuvant RT revealed a significant association with improved LRFS after adjusting for other prognostic variables on multivariable analysis; the 5-year LRFS rates of the observation and RT groups were 50% and 54%, respectively (HR 0.310, 95% CI 0.100–0.963; p = 0.043) (Table 2) (Figure 2).
Figure 1.
Local recurrence-free survival curves according to the resection margin status.
Table 2.
Univariable and multivariable analyses for local recurrence-free survival
| Variables | Number of patients | 5-year rate (%) | Univariable | Multivariable |
||
|---|---|---|---|---|---|---|
| p-value | p-value | HR | 95% CI | |||
| Age (years) | ||||||
| <65 | 28 | 51.8 | 0.796 | 0.643 | 1 | |
| ≥65 | 31 | 52.1 | 1.281 | 0.449–3.657 | ||
| Sex | ||||||
| Male | 32 | 56.1 | 0.377 | |||
| Female | 27 | 47.9 | ||||
| Performance status (ECOG) | ||||||
| 0–1 | 50 | 52.7 | 0.122 | |||
| 2–3 | 9 | 47.6 | ||||
| Surgery | ||||||
| Bile duct resection with hepatectomy | 13 | 50.3 | 0.917 | |||
| Bile duct resection | 11 | 49.7 | ||||
| Pancreaticoduodenectomy | 35 | 53.4 | ||||
| RM | ||||||
| R0 | 37 | 75.1 | 0.003 | <0.001 | 1 | |
| R1 | 14 | 20.5 | 6.134 | 2.051–18.344 | ||
| R2 | 8 | 0.0 | 18.551 | 3.680–93.520 | ||
| Tumour location | ||||||
| Non-hilar | 42 | 53.0 | 0.700 | 0.966 | 1 | |
| Hilar | 17 | 52.1 | 1.025 | 0.329–3.194 | ||
| Differentiationa | ||||||
| Well | 6 | 100.0 | 0.502 | |||
| Moderate | 38 | 39.1 | ||||
| Poor | 14 | 63.1 | ||||
| T stage | ||||||
| T1–2 | 33 | 73.0 | 0.002 | 0.029 | 1 | |
| T3–4 | 26 | 24.5 | 3.079 | 1.121–8.461 | ||
| N stage | ||||||
| N0 | 36 | 56.8 | 0.183 | 0.039 | 1 | |
| N1 | 23 | 43.5 | 2.832 | 1.055–7.607 | ||
| Perineural invasionb | ||||||
| No | 11 | 69.3 | 0.445 | |||
| Yes | 35 | 35.6 | ||||
| RT | ||||||
| No | 36 | 50.0 | 0.401 | 0.043 | 1 | |
| Yes | 23 | 53.7 | 0.310 | 0.100–0.963 | ||
CI, confidence interval; ECOG, Eastern Cooperative Oncology Group; HR, hazard ratio; RM, resection margin; RT, radiotherapy.
In one patient, information on differentiation was unavailable.
In 13 patients, information on perineural invasion was unavailable.
Figure 2.
Local recurrence-free survival curves according to the receipt of radiotherapy.
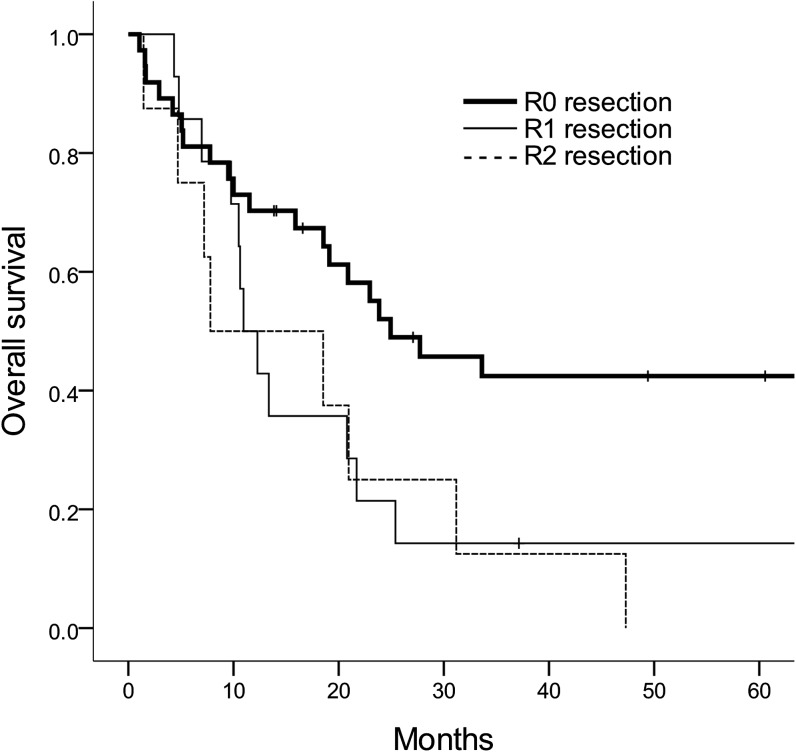
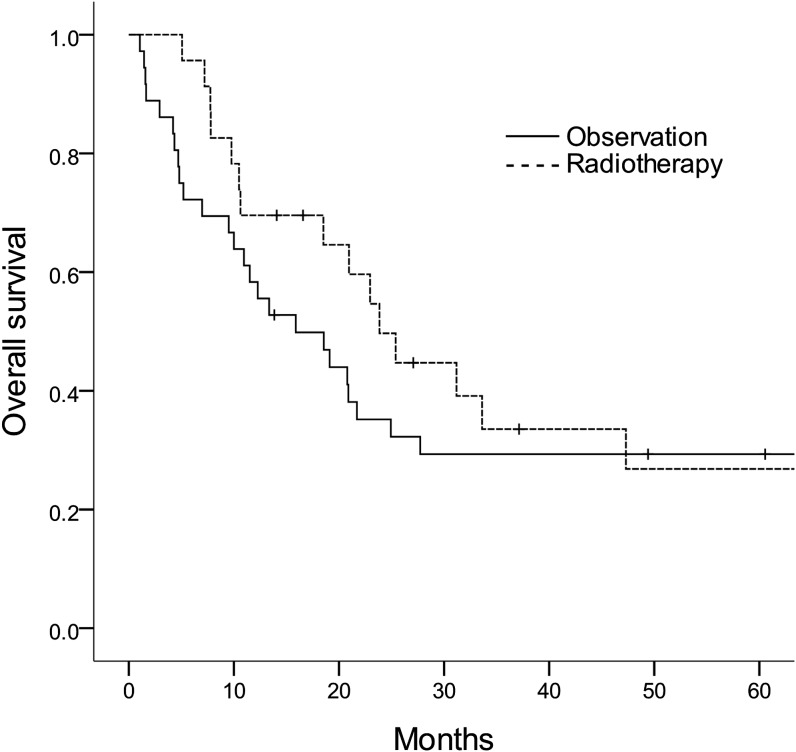
The median OS of all patients was 21 months and the 5-year OS rate was 29%. High T stage was a poor prognostic factor for OS in univariate analysis (p = 0.013). Adjuvant RT (HR 0.491, 95% CI 0.291–1.102; p = 0.085), RM status (HR for R1 1.816, 95% CI 0.853–3.867; and HR for R2 3.564, 95% CI 1.175–10.809; p = 0.054) and N stage (HR 1.956, 95% CI 0.983–3.892; p = 0.056) showed non-significant trends for OS on multivariable analysis incorporating age, RM status, tumour location, T stage, N stage and adjuvant RT (Table 3). The 5-year OS rates of R0, R1 and R2 resection were 42%, 14% and 0%, respectively (Figure 3). The 5-year OS rates were 29% for the observation group and 27% for the RT group (Figure 4).
Table 3.
Univariable and multivariable analyses for overall survival
| Variables | Number of patients | 5-year rate (%) | Univariable | Multivariable |
||
|---|---|---|---|---|---|---|
| p-value | p-value | HR | 95% CI | |||
| Age (years) | ||||||
| <65 | 28 | 27.6 | 0.851 | 0.962 | 1 | |
| ≥65 | 31 | 30.8 | 0.982 | 0.466–2.072 | ||
| Sex | ||||||
| Male | 32 | 29.7 | 0.786 | |||
| Female | 27 | 29.6 | ||||
| Performance status (ECOG) | ||||||
| 0–1 | 50 | 30.3 | 0.481 | |||
| 2–3 | 9 | 22.2 | ||||
| Surgery | ||||||
| Bile duct resection with hepatectomy | 13 | 30.8 | 0.981 | |||
| Bile duct resection | 11 | 15.9 | ||||
| Pancreaticoduodenectomy | 35 | 31.4 | ||||
| RM | ||||||
| R0 | 37 | 42.4 | 0.071 | 0.054 | 1 | |
| R1 | 14 | 14.3 | 1.816 | 0.853–3.867 | ||
| R2 | 8 | 0.0 | 3.564 | 1.175–10.809 | ||
| Tumour location | ||||||
| Non-hilar | 42 | 33.4 | 0.348 | 0.580 | 1 | |
| Hilar | 17 | 18.3 | 1.246 | 0.571–2.722 | ||
| Differentiationa | ||||||
| Well | 6 | 100.0 | 0.131 | |||
| Moderate | 38 | 23.5 | ||||
| Poor | 14 | 25.7 | ||||
| T stage | ||||||
| T1–2 | 33 | 41.9 | 0.013 | 0.101 | 1 | |
| T3–4 | 26 | 15.4 | 1.768 | 0.895–3.492 | ||
| N stage | ||||||
| N0 | 36 | 32.4 | 0.204 | 0.056 | 1 | |
| N1 | 23 | 24.2 | 1.956 | 0.983–3.892 | ||
| Perineural invasionb | ||||||
| No | 11 | 36.4 | 0.887 | |||
| Yes | 35 | 23.2 | ||||
| RT | ||||||
| No | 36 | 29.3 | 0.602 | 0.085 | 1 | |
| Yes | 23 | 26.3 | 0.491 | 0.219–1.102 | ||
CI, confidence interval; ECOG, Eastern Cooperative Oncology Group; HR, hazard ratio; RM, resection margin; RT, radiotherapy.
In one patient, information on differentiation was unavailable.
In 13 patients, information on perineural invasion was unavailable.
Figure 3.
Overall survival curves according to the resection margin status.
Figure 4.
Overall survival curves according to the receipt of radiotherapy.
Treatment failures were observed in 32 patients. As the first site failure, LR with or without distant metastasis was observed in 16 (44%) patients in the observation group and in 4 (17%) patients in the RT group (p = 0.021) (Table 4).
Table 4.
Patterns of the first treatment failure
| Site of failure | Number of patients/total failures |
p-value | |
|---|---|---|---|
| Observation (n = 36) | RT (n = 23) | ||
| LR with or without DM | |||
| No | 4/20 | 8/12 | 0.021 |
| Yes | 16/20 | 4/12 | |
| DM with or without LR | |||
| No | 10/20 | 2/12 | 0.075 |
| Yes | 10/20 | 10/12 | |
DM, distant metastasis; LR, local recurrence; RT, radiotherapy.
Treatment toxicity
Grade of toxicity was scored according to the Common Terminology Criteria for Adverse Events v. 4.03. Among 23 patients receiving adjuvant RT, acute complications of Grade ≥3 were observed in 2 (9%) patients; 1 patient (not receiving concomitant chemotherapy) experienced severe nausea and vomiting, and the other patient (receiving concomitant weekly gemcitabine) had decreased platelet and white blood cell count.
DISCUSSION
In this study, adjuvant RT showed an increase in LRFS as well as a non-significant improvement in OS of patients with EHBD cancer. Positive RM was associated with poor local control rate and adverse OS. LR was the predominant pattern of failure in the observation group, while distant metastasis was the dominant pattern in the RT group.
Poor prognosis of EHBD cancer was repeatedly observed in our study with a 5-year OS rate of 29%. It is noticeable that a treatment factor (i.e. RM status) had a greater impact on prognosis than any other patient or tumour characteristic. Many studies demonstrated that positive RM decreased median OS from 24–74 months (R0) to 12–13 months (R1 or R2).9,15,24 In our study, the 5-year OS rates according to RM status were 42% in R0 resection, 14% in R1 resection and 0% in R2 resection, suggesting that positive RM would drastically decrease the chance of cure by surgical treatment. Moreover, LR was the major pattern of failure without receiving adjuvant RT in the first site of failure pattern analysis. Also, the 5-year LRFS rate of R0 resection was 75% compared with 21% and 0% of R1 and R2 resections, respectively (p < 0.001). These findings suggest that more effective strategies for local control are mandatory to improve OS rate.
Additional resection of positive RM could be a reasonable option.25 Ribero et al26 demonstrated that reresection of positive proximal bile duct margin to gain secondary R0 resection in patients with hilar cholangiocarcinoma improved median OS to a level similar to that of patients who underwent primary R0 resection. However, the success rate of obtaining secondary R0 resection is limited because of procedural difficulties.9–15 Moreover, another author noted that additional resection of positive proximal bile duct RM in hilar cholangiocarcinoma did not improve OS, suggesting that further studies are indispensable to evaluate the role of additional resection of positive RM.7
Several studies investigated the benefit of adjuvant RT to countervail the adverse effect of positive RM.14,17–19,27–30 Small retrospective studies demonstrated that there was no significant OS difference between negative RM group without adjuvant RT and positive RM group with adjuvant RT.14,18 Gwak et al17 reported that patients with R1 resection who received adjuvant RT had significantly higher median disease-free survival than those who received R1 resection alone.
In our study, adjuvant RT group was compared with non-RT group, retrospectively. The RT group had more adverse features than its counterpart; among eight patients who had R2 resection, six patients were included in the RT group (26% of the RT group), whereas the remaining two patients were in the observation group (6% of the observation group). After incorporating RM status in multivariable analysis, adjuvant RT significantly improved LRFS (HR 0.310) and showed a trend towards increased OS (HR 0.491). Reduced LR rate by using adjuvant RT might result in OS improvement.
In spite of the high LR rate of EHBD cancer, RT has not yet been a well-established adjuvant treatment.31 An analysis of data from the Surveillance, Epidemiology, and End Results program demonstrated that only 32% of patients with EHBD cancer underwent adjuvant RT.2 Because of the rarity of this disease, only small retrospective studies were available in many institutions, resulting in limited statistical powers. One meta-analysis, however, revealed that adjuvant RT derived survival benefit in R1 resection (odds ratio 0.33), although this improvement was not observed in R0 resection.19
In the present study, median age for the observation group and RT group was 71 years and 61 years, respectively. In the elderly patient, adjuvant RT was less likely to be administered because of concerns regarding RT-related morbidity. On univariate and multivariable analyses, however, age was not a significantly poor prognostic factor for survival. Toxicity of adjuvant RT was minor; only 2 (9%) patients in RT group presented Grade ≥3 side effects. Therefore, more assertive utility of adjuvant RT might improve treatment outcomes in elderly patients with good performance status.
This study is a retrospective study with a small sample size in a single institution. While no patients received chemotherapy in the observation group, a major portion of patients in the RT group received chemotherapy with various regimens. Chemotherapy regimens and treatment durations were too heterogeneous to analyze. Benefits of adjuvant RT and chemotherapy could not be evaluated separately in this small study.
In conclusion, adjuvant RT improved LRFS for patients with localized EHBD cancer. RM status was a significant prognostic factor.
Contributor Information
Yi-Jun Kim, Email: kimyj.ro@gmail.com.
Kyubo Kim, Email: kyubokim.ro@gmail.com.
Seog Ki Min, Email: mp9666@ewha.ac.kr.
Eun Mi Nam, Email: enam34@ewha.ac.kr.
REFERENCES
- 1.Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee JK, et al. Prediction of cancer incidence and mortality in Korea, 2016. Cancer Res Treat 2016; 48: 451–7. doi: https://doi.org/10.4143/crt.2016.092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vern-Gross TZ, Shivnani AT, Chen K, Lee CM, Tward JD, MacDonald OK, et al. Survival outcomes in resected extrahepatic cholangiocarcinoma: effect of adjuvant radiotherapy in a surveillance, epidemiology, and end results analysis. Int J Radiat Oncol Biol Phys 2011; 81: 189–98. doi: https://doi.org/10.1016/j.ijrobp.2010.05.001 [DOI] [PubMed] [Google Scholar]
- 3.Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg 1996; 224: 463. doi: https://doi.org/10.1097/00000658-199610000-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsao JI, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, et al. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg 2000; 232: 166–74. doi: https://doi.org/10.1097/00000658-200008000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagorney DM, Donohue JH, Farnell MB, Schleck CD, Ilstrup DM. Outcomes after curative resections of cholangiocarcinoma. Arch Surg 1993; 128: 871–8. doi: https://doi.org/10.1001/archsurg.1993.01420200045008 [DOI] [PubMed] [Google Scholar]
- 6.Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, et al. Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg 1999; 230: 266. doi: https://doi.org/10.1097/00000658-199908000-00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shingu Y, Ebata T, Nishio H, Igami T, Shimoyama Y, Nagino M. Clinical value of additional resection of a margin-positive proximal bile duct in hilar cholangiocarcinoma. Surgery 2010; 147: 49–56. doi: https://doi.org/10.1016/j.surg.2009.06.030 [DOI] [PubMed] [Google Scholar]
- 8.Launois B, Reding R, Lebeau G, Buard JL. Surgery for hilar cholangiocarcinoma: French experience in a collective survey of 552 extrahepatic bile duct cancers. J Hepatobiliary Pancreat Surg 2000; 7: 128–34. doi: https://doi.org/10.1007/s005340050166 [DOI] [PubMed] [Google Scholar]
- 9.Rocha FG, Matsuo K, Blumgart LH, Jarnagin WR. Hilar cholangiocarcinoma: the Memorial Sloan-Kettering Cancer Center experience. J Hepatobiliary Pancreat Sci 2010; 17: 490–6. doi: https://doi.org/10.1007/s00534-009-0205-4 [DOI] [PubMed] [Google Scholar]
- 10.Kim K, Chie EK, Jang JY, Kim SW, Han SW, Oh DY, et al. Adjuvant chemoradiotherapy after curative resection for extrahepatic bile duct cancer: a long-term single center experience. Am J Clin Oncol 2012; 35: 136–40. doi: https://doi.org/10.1097/COC.0b013e318209aa29 [DOI] [PubMed] [Google Scholar]
- 11.Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery 2005; 137: 396–402. doi: https://doi.org/10.1016/j.surg.2004.10.008 [DOI] [PubMed] [Google Scholar]
- 12.Kim S, Kim SW, Bang YJ, Heo DS, Ha SW. Role of postoperative radiotherapy in the management of extrahepatic bile duct cancer. Int J Radiat Oncol Biol Phys 2002; 54: 414–9. doi: https://doi.org/10.1016/S0360-3016(02)02952-8 [DOI] [PubMed] [Google Scholar]
- 13.Pichlmayr R, Weimann A, Klempnauer J, Oldhafer KJ, Maschek H, Tusch G, et al. Surgical treatment in proximal bile duct cancer. A single-center experience. Ann Surg 1996; 224: 628–38. doi: https://doi.org/10.1097/00000658-199611000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oh D, Lim DH, Heo JS, Choi SH, Choi DW, Ahn YC, et al. The role of adjuvant radiotherapy in microscopic tumor control after extrahepatic bile duct cancer surgery. Am J Clin Oncol 2007; 30: 21–5. doi: https://doi.org/10.1097/01.coc.0000245467.97180.78 [DOI] [PubMed] [Google Scholar]
- 15.Ben-David MA, Griffith KA, Abu-Isa E, Lawrence TS, Knol J, Zalupski M, et al. External-beam radiotherapy for localized extrahepatic cholangiocarcinoma. Int J Radiat Oncol Biol Phys 2006; 66: 772–9. doi: https://doi.org/10.1016/j.ijrobp.2006.05.061 [DOI] [PubMed] [Google Scholar]
- 16.Higuchi R, Ota T, Araida T, Kobayashi M, Furukawa T, Yamamoto M. Prognostic relevance of ductal margins in operative resection of bile duct cancer. Surgery 2010; 148: 7–14. doi: https://doi.org/10.1016/j.surg.2009.11.018 [DOI] [PubMed] [Google Scholar]
- 17.Gwak HK, Kim WC, Kim HJ, Park JH. Extrahepatic bile duct cancers: surgery alone versus surgery plus postoperative radiation therapy. Int J Radiat Oncol Biol Phys 2010; 78: 194–8. doi: https://doi.org/10.1016/j.ijrobp.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 18.Borghero Y, Crane CH, Szklaruk J, Oyarzo M, Curley S, Pisters PW, et al. Extrahepatic bile duct adenocarcinoma: patients at high-risk for local recurrence treated with surgery and adjuvant chemoradiation have an equivalent overall survival to patients with standard-risk treated with surgery alone. Ann Surg Oncol 2008; 15: 3147–56. doi: https://doi.org/10.1245/s10434-008-9998-7 [DOI] [PubMed] [Google Scholar]
- 19.Horgan AM, Amir E, Walter T, Knox JJ. Adjuvant therapy in the treatment of biliary tract cancer: a systematic review and meta-analysis. J Clin Oncol 2012; 30: 1934–40. doi: https://doi.org/10.1200/JCO.2011.40.5381 [DOI] [PubMed] [Google Scholar]
- 20.Pitt HA, Nakeeb A, Abrams RA, Coleman J, Piantadosi S, Yeo CJ, et al. Perihilar cholangiocarcinoma. Postoperative radiotherapy does not improve survival. Ann Surg 1995; 221: 788. doi: https://doi.org/10.1097/00000658-199506000-00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Todoroki T, Ohara K, Kawamoto T, Koike N, Yoshida S, Kashiwagi H, et al. Benefits of adjuvant radiotherapy after radical resection of locally advanced main hepatic duct carcinoma. Int J Radiat Oncol Biol Phys 2000; 46: 581–7. doi: https://doi.org/10.1016/S0360-3016(99)00472-1 [DOI] [PubMed] [Google Scholar]
- 22.Hejna M, Pruckmayer M, Raderer M. The role of chemotherapy and radiation in the management of biliary cancer: a review of the literature. Eur J Cancer 1998; 34: 977–86. doi: https://doi.org/10.1016/S0959-8049(97)10166-6 [DOI] [PubMed] [Google Scholar]
- 23.Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010; 17: 1471–4. doi: https://doi.org/10.1245/s10434-010-0985-4 [DOI] [PubMed] [Google Scholar]
- 24.Sasaki R, Takeda Y, Funato O, Nitta H, Kawamura H, Uesugi N, et al. Significance of ductal margin status in patients undergoing surgical resection for extrahepatic cholangiocarcinoma. World J Surg 2007; 31: 1788–96. doi: https://doi.org/10.1007/s00268-007-9102-7 [DOI] [PubMed] [Google Scholar]
- 25.Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999; 230: 808. doi: https://doi.org/10.1097/00000658-199912000-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ribero D, Amisano M, Lo Tesoriere R, Rosso S, Ferrero A, Capussotti L. Additional resection of an intraoperative margin-positive proximal bile duct improves survival in patients with hilar cholangiocarcinoma. Ann Surg 2011; 254: 776–81; discussion 781–3. doi: https://doi.org/10.1097/SLA.0b013e3182368f85 [DOI] [PubMed] [Google Scholar]
- 27.Itoh H, Nishijima K, Kurosaka Y, Takegawa S, Kiriyama M, Dohba S, et al. Magnitude of combination therapy of radical resection and external beam radiotherapy for patients with carcinomas of the extrahepatic bile duct and gallbladder. Dig Dis Sci 2005; 50: 2231–42. doi: https://doi.org/10.1007/s10620-005-3040-8 [DOI] [PubMed] [Google Scholar]
- 28.Urego M, Flickinger JC, Carr BI. Radiotherapy and multimodality management of cholangiocarcinoma. Int J Radiat Oncol Biol Phys 1999; 44: 121–6. doi: https://doi.org/10.1016/S0360-3016(98)00509-4 [DOI] [PubMed] [Google Scholar]
- 29.Stein DE, Heron DE, Rosato EL, Anné PR, Topham AK. Positive microscopic margins alter outcome in lymph node-negative cholangiocarcinoma when resection is combined with adjuvant radiotherapy. Am J Clin Oncol 2005; 28: 21–3. doi: https://doi.org/10.1097/01.coc.0000139017.90599.f5 [DOI] [PubMed] [Google Scholar]
- 30.Kim MY, Kim JH, Kim Y, Byun SJ. Postoperative radiotherapy appeared to improve the disease free survival rate of patients with extrahepatic bile duct cancer at high risk of loco-regional recurrence. Radiat Oncol J 2016; 34: 297–304. doi: https://doi.org/10.3857/roj.2016.01879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet 2005; 366: 1303–14. doi: https://doi.org/10.1016/S0140-6736(05)67530-7 [DOI] [PubMed] [Google Scholar]