Abstract
Background/Purpose:
To evaluate the relationship between refractive error and vision-related quality of life in 16-year-old students in Taiwan.
Methods:
A cross-sectional study was designed for 16-year junior-high-school students in Taiwan. Myopia was defined as a spherical refractive error (SRE) < −0.50 D, hyperopia as SRE > +1.0 D, and emmetropia as SRE −0.5–+1.0 D in the better eye. Vision-related quality of life was assessed using the Taiwan Chinese version of the 25-Item National Eye Institute Visual Functioning Questionnaire.
Results:
Of the 688 participants, 466 (68%) had myopia and 22 (3%) had hyperopia. In logistic-regression models adjusted for gender, parents’ education, family income, and parental refractive error, myopia was an independent risk factor of poorer vision-related quality of life for both near vision (odds ratio 1.73, 95% confidence interval 1.22–2.45) and distance vision (odds ratio 3.11, 95% confidence interval 2.23–4.35). Hyperopia was not associated with near- or distance-vision difficulty.
Conclusion:
In this study population, myopia was associated with difficulties in near and distance vision compared to emmetropia. Further studies are needed to confirm our findings in other populations.
Keywords: distance vision, myopia, near vision, refractive error, vision-related quality of life
1. Introduction
Refractive error is a major eye problem throughout the world, especially in Asia. Without adequate correction, refractive error can become the main cause of vision impairment. Previous studies indicated that the rate of myopia was up to 84% among schoolchildren aged 16–18 years in Taiwan.1,2,3 The prevalence of myopia in school-age children in Taiwan has been increasing over recent years,1 and refractive error is associated with lower levels of family income and parental education, as well as the number of myopic parents.4,5 Myopia and hyperopia can increase the risk of developing some ocular diseases and have impact on vision-related quality of life; however, for schoolchildren, refractive errors can have a more direct influence on quality of life and learning ability than other ocular diseases.
The 25-Item National Eye Institute Visual Functioning Questionnaire (NEIVFQ-25) has been used as a tool to evaluate vision-related quality of life or visual function.6,7 These studies reported that corrected refractive errors remained a negative effect on vision-related quality of life; however, data regarding school-age children are still lacking. Therefore, this study aimed to determine the effect of corrected refractive error on vision-related quality of life in school age children, by using the score of near-and distance-activity subscales.
2. Methods
2.1. Study population
This cross-sectional study enrolled all ninth-grade students from a junior high school in Taiwan. Students with histories of previous ocular surgery; diagnosed ocular diseases like amblyopia, glaucoma, congenital cataracts, or retina dystrophy; or wearing orthokeratology lens were excluded. The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Taipei City Hospital, Taipei, Taiwan. After obtaining informed consent, these students received a detailed ocular examination, including measurements of presenting visual acuity and refractive errors, as well as face-to-face interviews for assessments of the NEIVFQ-25 (Taiwan Chinese version) and demographic information using questionnaires. Presenting visual acuities were obtained for students wearing their glasses as usual.
2.2. Refractive error
Refractive error was measured using an auto refractometer (Canon RK-5 Auto Ref-Keratometer; Canon Inc., Ltd., Tokyo, Japan) under cycloplegic conditions. Five consecutive measurements were obtained for each eye of all students, and the mean of measurements was used for analysis. Cycloplegia was preceded with one drop of 0.5% proparacaine, and then two drops of 1% cyclopentolate within a 5-minute interval. If the pupil size was < 6 mm or reflective to light, an additional drop of cyclopentolate was administered every 5 minutes until an acceptable dilation occurred. Myopia was defined as spherical refractive error (SRE) < −0.50 D, hyperopia was defined as SRE > +1.0 D, and emmetropia as SRE −0.5–+1.0 D. This study used the better eye when determining SRE.
2.3. Vision-related quality of life
The Taiwan Chinese version of the NEIVFQ-25 was used to obtain objective measure of visual impairment. The subscores within the NEIVFQ-25 have been validated in our previous studies,6,7 in which the near-vision subscore as the individual visual function of near activities and the distance-vision subscore as the visual function of distance activities were established.
2.4. Statistical analysis
Because the distributions of near- and distance-vision function scores were highly skewed, the scores were transformed into an ordinal variable for analysis. According to the median values, the cutoff value of 100 was used to create a “no difficulty” group (score = 100) and a “difficulty” group (score < 100) for both near-and distance-vision function scores. Cutoff values of < 90 were also determined by a sensitivity test.
A multivariate logistic-regression model was performed to analyze the relationship between the SRE categories and the visual-function difficulty, and was adjusted according to gender, parental education, family income, and the number of myopic parents. Significant associations were reported as odds ratios (ORs) with 95% confidence intervals (CIs). A p value of < 0.05 was considered statistically significant. Statistical analyses were conducted with IBM SPSS 20.0 software (IBM, Chicago, IL, USA).
3. Results
A total of 688 students were included in the final analysis. Of those, 466 (68%) had myopia and 22 (3%) had hyperopia, 49.8% were boys, 54.9% had both parents with an education lower than university level, 56.8% had a family income of < $2000, and 28.2% had no myopic parents (Table 1).
Table 1.
Demographic data and refractive errors in each group.
| Parameter | Spherical refractive error | ||
|---|---|---|---|
| Emmetropia | Myopia | Hyperopia | |
| N | 200 | 466 | 22 |
| Refractive error (D) | –0.25 ± 1.03 | –3.92 ± 2.06 | 1.57 ± 1.34 |
| Gender | |||
| Boy | 92 (46) | 241 (52) | 12 (55) |
| Girl | 108 (54) | 225 (48) | 10 (45) |
| Parental educational level | |||
| High school | 112 (56) | 247 (53) | 13 (59) |
| University | 88 (44) | 219(47) | 9 (41) |
| Family income (monthly) | |||
| < US $2000 | 104 (52) | 269 (58) | 14 (64) |
| > US $2000 | 96 (48) | 197 (42) | 8 (36) |
| Number of myopic parents | |||
| 0 | 63 (32) | 116 (25) | 11 (50) |
| 1 | 88 (44) | 218 (47) | 6 (27) |
| 2 | 49 (24) | 132 (28) | 5 (23) |
Data are presented as n (%) or mean ± standard deviation.
The median NEIVFQ subscale scores in each group are shown in Table 2. The distributions of subscores of near activities and distance activities were highly skewed (Figure 1). A significant difference in the refractive errors between the no-difficulty group and the difficulty group was found in distance-vision score (Table 3). Furthermore, 55.5% of the students reported no difficulty in near visual function, and 42.5% reported no difficulty in distance visual function (Table 4).
Table 2.
The 25-Item National Eye Institute Visual Functioning Questionnaire composite and the subscores of refractive errors for different groups.
| Subscores | Emmetropia (N = 200) | Myopia (N = 466) | Hyperopia (N = 22) | p |
|---|---|---|---|---|
| Median (25–75a) | Median (25–75a) | Median (25–75a) | ||
| Composite | 80.5 (73.7–85.2) | 77.2 (68.3–81.9) | 79.0 (69.8–84.8) | < 0.01b |
| General health | 50 (50–75) | 50 (25–75) | 50 (50–75) | 0.14 |
| General vision | 80 (60–100) | 60 (60–80) | 80 (60–80) | < 0.01b |
| Ocular pain | 62.5 (50–75) | 62.5 (50–75) | 68.75 (50–87.5) | 0.33 |
| Near activities | 100 (91.6–100) | 100 (83.3–100) | 100 (83.3–100) | 0.09 |
| Distance activities | 100 (91.6–100) | 87.5 (75–100) | 95.8 (75–100) | < 0.01b |
| Social functioning | 100 (100–100) | 100 (87.5–100) | 100(100–100) | < 0.01 |
| Mental health | 56.2 (43.7–68.7) | 50 (43.7–62.5) | 56.2 (50–62.5) | 0.03 |
| Role difficulties | 62.5 (37.5–75) | 50 (37.5–75) | 62.5 (37.5–75) | 0.53 |
| Dependency | 58.3 (41.6–75) | 50 (41.6–75) | 66.6 (50–75) | 0.18 |
| Driving | 100 (70.8–100) | 91.6 (66.6–100) | 75 (50–100) | 0.18 |
| Color vision | 100 (100–100) | 100(100–100) | 100(100–100) | 0.06 |
| Peripheral vision | 100 (100–100) | 100(75–100) | 100(75–100) | < 0.01b |
aIndicates the 25th and 75th percentiles, or the lower and higher quartiles.
b Indicates significant higher subscale scores in the emmetropia group compared to the myopia group (p < 0.01) by χ2 test analysis.
Figure 1.
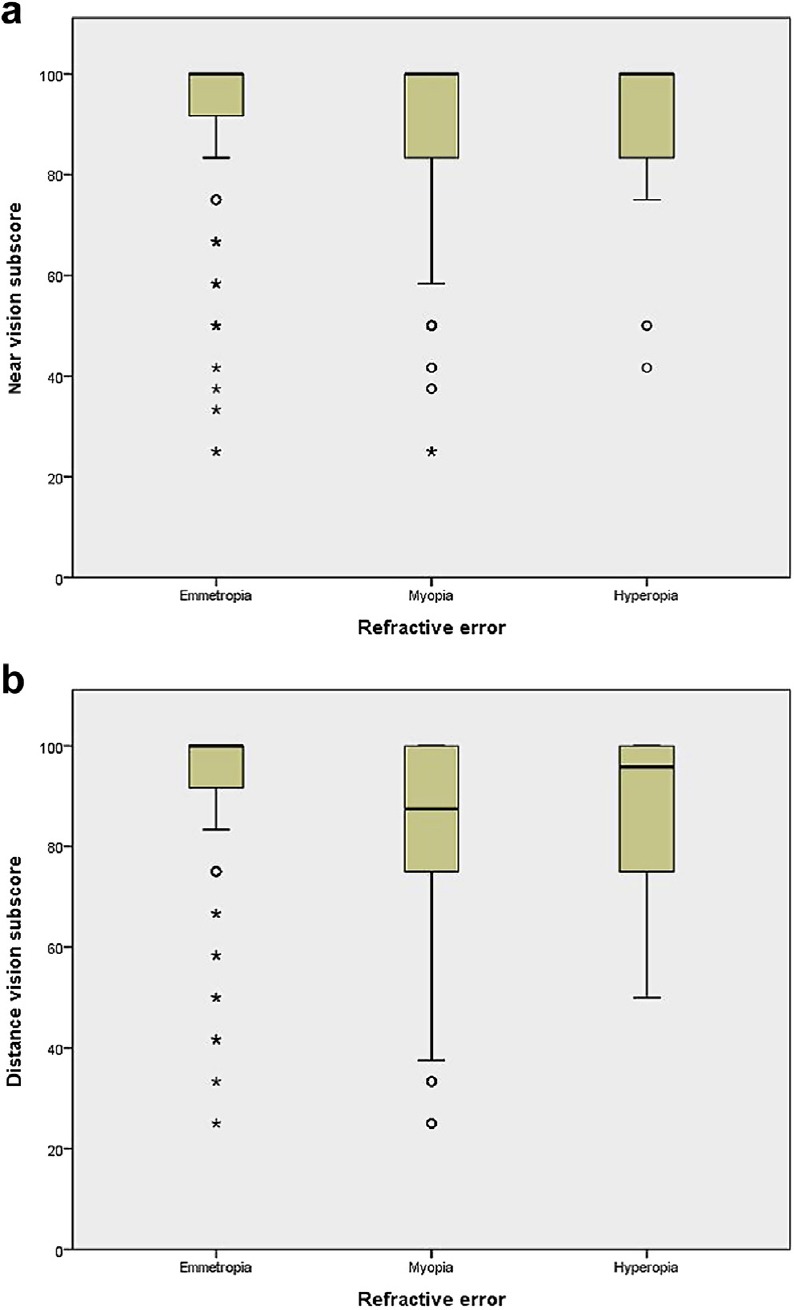
The distribution of scores in near activities (1A) and distance activities (1B) are displayed. The boxes represent the 25th–75th percentile; the whiskers represent a 1.5 interquartile range outside the boxes; the circle markers (B) represent mild outliers, and the asterisks (*) represent extreme outliers. There are obvious ceiling effects in all groups in both subscores.
Table 3.
Population characteristics by vision score category.
| Near-vision score | Distance-vision score | |||||
|---|---|---|---|---|---|---|
| No difficulty | Difficulty | p | No difficulty | Difficulty | p | |
| Refractive error (D) | –2.54 | –2.88 | 0.09 | –2.24 | –3.01 | < 0.01* |
| Female | 53.7 | 45.7 | 0.03* | 49.5 | 50.7 | 0.75 |
| Below university | 46.4 | 43.4 | 0.42 | 44.7 | 45.3 | 0.85 |
| Income < US $2000 | 42.1 | 44.3 | 0.54 | 41.5 | 44.2 | 0.47 |
| Myopic parents | ||||||
| 1 | 46.2 | 42.2 | 0.28 | 42.1 | 45.8 | 0.32 |
| 2 | 25.7 | 29.8 | 0.21 | 28.9 | 26.6 | 0.49 |
Data are presented as %, unless otherwise indicated.
*p < 0.05.
Table 4.
Distribution of refractive errors by the vision score category.
| Group | N | Near-vision score | Distance-vision score | ||
|---|---|---|---|---|---|
| No difficultya | Difficultyb | No difficultya | Difficultyb | ||
| All participants | 688 | 55.5 | 44.5 | 42.5 | 57.5 |
| Emmetropia | 200 | 64.7 | 35.3 | 62.2 | 37.8 |
| Myopia | 466 | 51.3 | 48.7 | 33.3 | 66.7 |
| Hyperopia | 22 | 63.6 | 36.4 | 50.0 | 50.0 |
Data are presented as %.
a Score = 100.
b Score < 100.
After adjustment for gender, parental education, family income, and the number of myopic parents, students with myopia were significantly more likely to report difficulties of both near vision (OR 1.73, 95% CI 1.22–2.45) and distance vision (OR 3.11, 95% CI 2.23–4.35; Table 5). By contrast, no significant association with either near or distance visual-function difficulty was observed in those with hyperopia.
Table 5.
Results of logistic regression.
| Group | Near-vision impairment | Distance-vision impairment | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Emmetropia | Ref | Ref | Ref | Ref |
| Myopia | 1.7* | 1.2–2.4 | 3.1* | 2.2–4.3 |
| Hyperopia | 1 | 0.4–2.6 | 1.8 | 0.7–4.3 |
* The p value < 0.05 after adjustment for gender, family income, parental education, and number of myopic parents.
CI = confidence interval; OR = odds ratio; Ref = reference.
4. Discussion
In this study, we found that students with myopia had more difficulties in near and distance activities. They reported uncomfortable, some inconvenience, or other problems in their usual daily lives even with visual aids. By contrast, no significant difficulty with activities related to near or distance vision was reported by those with hyperopia. The students with refractive errors might usually wear glasses or contact lenses for both myopia and hyperopia groups, which could lead to a similar array of inconvenience or uncomfortable experience while using visual aids for both groups.
The mean value of NEIVFQ composite score in the emmetropia group was 76.7 (data not shown), lower than 80.7 reported in a previous study for a healthy adult group in Taiwan.7 In another previous study that analyzed the subscores of NEIVFQ in Taiwanese adults,8 the median value of the near-vision subscore was 75, lower than 100 from that found in our study group. In the distance-vision subscore, the median value was 95 in our study in contrast to the value of 83 found in the previous study. The observations based on these results suggested that younger students clearly have higher scores than adults in the subscores of both near and distance vision.
Previous research has also reported that refractive errors, such as myopia or hyperopia, were associated with increased difficulties in visual function, even after the problems were corrected.9,10,11 However, to our knowledge, the negative effect of refractive errors has only been reported in adults, but not in children.
This study found that school-age children with myopia had a greater risk of having difficulties in distance- and near-vision functions. Similar to adults, they may have a difficulty in reading newspapers and street signs, finding objects at arm’s length, and going down steps in dim light. However, further research is needed to determine whether visual-function difficulty has a negative effect on the learning abilities of these students.
In our study, the students with hyperopia were not associated with difficulty in near- or distance-vision function compared to those with emmetropia. Due to the use of cycloplegic refraction in our participants, the hyperopia group might have similar outcomes to the emmetropia group in normal circumstances and under appropriate accommodations, since they are younger than adults. The negative effect of excessive accommodation noted by the students might not be detectable in the near or distance subscore by the questionnaire.
This study had some limitations. First, the participants were only recruited from a junior high school in a densely populated city in Taiwan, and the results may require further confirmation by more studies in other populations. Second, as the NEIVFQ was used as an evaluation tool, the skewed distribution of scores was transformed into ordinal categories by cutoff values according to the experiences reported in previous studies.7,9 Third, because the lack of standardized definitions for myopia and hyperopia presented a challenge in the classification of participants in this study, the cutoff values were only based on prior studies.9
In conclusion, myopia was found to be associated with difficulties in near and distance visual function in school-age children in this study. However, further study is necessary to determine the relationship between visual-function difficulty and learning ability. This study also suggests that the programs and policies aimed at reducing the prevalence of myopia in our populations have a positive public-health impact.
Footnotes
Conflicts of interest: There is no financial conflict of interest for this study.
References
- 1.Lin LL, Shih YF, Hsiao CK, Chen CJ, Lee LA, Hung PT. Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Assoc. 2001;100:684–691. [PubMed] [Google Scholar]
- 2.Lin LL, Chen CJ, Hung PT, Ko LS. Nationwide survey of myopia among schoolchildren in Taiwan, 1986. Acta Ophthalmol Scand Suppl. 1988;185:29–33. doi: 10.1111/j.1755-3768.1988.tb02657.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin LK, Shih YF, Tsai CB, et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom Vis Sci. 1999;76:275–281. doi: 10.1097/00006324-199905000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Cheng CY, Hsu WM, Liu JH, Tsai SY, Chou P. Refractive errors in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Invest Ophthalmol Vis Sci. 2003;44:4630–4638. doi: 10.1167/iovs.03-0169. [DOI] [PubMed] [Google Scholar]
- 5.Saw SM. A synopsis of the prevalence rates and environmental risk factors for myopia. Clin Exp Optom. 2003;86:289–294. doi: 10.1111/j.1444-0938.2003.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 6.Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-Item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001 Jul;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 7.Lin JC, Chie WC. Psychometric validation of the Taiwan Chinese version of the 25-Item National Eye Institute Visual Functioning Questionnaire. J Eval Clin Pract. 2010;16:619–626. doi: 10.1111/j.1365-2753.2009.01253.x. [DOI] [PubMed] [Google Scholar]
- 8.Lin JC, Yu JH. Assessment of quality of life among Taiwanese patients with visual impairment. J Formos Med Assoc. 2012;111:572–579. doi: 10.1016/j.jfma.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Sandhu RK, Munoz BE, Swenor BK, West SK. Refractive error and visual function difficulty in a Latino population. Ophthalmology. 2012;119:1731–1736. doi: 10.1016/j.ophtha.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lamoureux EL, Saw SM, Thumboo J, et al. The impact of corrected and un-corrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2009;50:2614–2620. doi: 10.1167/iovs.08-2164. [DOI] [PubMed] [Google Scholar]
- 11.Coleman AL, Yu F, Keeler E, Mangione CM. Treatment of uncorrected refractive error improves vision-specific quality of life. J Am Geriatr Soc. 2006;54:883–890. doi: 10.1111/j.1532-5415.2006.00817.x. [DOI] [PubMed] [Google Scholar]


