Abstract
A 47-year-old man presented with epiphora and a mass around the lacrimal sac in his left eye. Imaging studies revealed a favorable diagnosis of sinusitis-related mucocele. However, the pathological study of the excised tumor demonstrated a diffuse large B cell lymphoma. The patient was consequently referred to the oncology department for further management. Malignant lymphomas of the lacrimal sac are rare and they can mimic mucoceles. As such, they should be included in the list of differential diagnoses for lacrimal sac mass.
Keywords: diffuse large B cell lymphoma, lacrimal sac, mucocele
1. Introduction
Tumors of the lacrimal sac are rare. Malignant lymphomas account for approximately 6% of all lacrimal sac tumors.1 They are usually secondary to systemic lymphoreticular malignancies. Primary non-Hodgkin's lymphoma of the lacrimal sac is extremely rare. Its symptoms are usually nonspecific, and thus easy to misdiagnose. We report a patient with primary diffuse large B cell lymphoma (DLBCL) of the lacrimal sac, which was initially mis-diagnosed as a mucocele.
2. Case report
A 47-year-old man with a history of chronic sinusitis presented with epiphora in his left eye for 4 months and had an elastic mass around the left lacrimal sac for 2 months. The ophthalmic examinations revealed an elastic, nontender, and nonmovable mass around the left lacrimal sac (Fig. 1). Lacrimal irrigation was patent. Orbital computed tomography (CT; Fig. 2A) and magnetic resonance (MR) imaging (Fig. 2B and C) revealed chronic paranasal sinusitis and a homogeneous cystic lesion (17 mm × 12 mm × 20 mm) over the left lacrimal sac. The radiologist suggested that sinusitis-related mucocele be ruled out. The patient was then referred to an otolaryngologist. Functional endoscopic sinus surgery and Monoka tube insertion were performed. Polyps in the left osteomeatal complex and inflammatory contents over the left maxillary sinus opening were found during the operation. The Monoka tube was inserted smoothly. The pathological report showed chronic sinusitis only. However, the epiphora persisted and the mass enlarged gradually. During the tumor excision, a capsularized homogenous pink soft mass over the lacrimal sac was observed. The lacrimal sac was totally removed. The pathological results revealed a diffuse infiltration of medium-size to large neoplastic cells with high mitotic activity (Fig. 3A). The immunohistochemical stains showed the characteristic CD20 (+), CD3 (−), CD5 (−), and CK (−), compatible with the diagnosis of diffuse large B cell lymphoma (Fig. 3B). The patient was then referred to the oncology department. A whole-body fludeoxyglucose (FDG) positron emission tomography scan demonstrated focal increased FDG uptake in the inferior medial aspect of the left orbital cavity without metastasis (Fig. 4A). A bone marrow examination revealed no bone marrow involvement. The patient's serum lactate dehydrogenase (LDH) level was 154 U/L. Six cycles of chemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) were subsequently conducted. No abnormal glucose metabolic region was found in the whole-body FDG positron emission tomography scan 1 year after the chemotherapy (Fig. 4B).
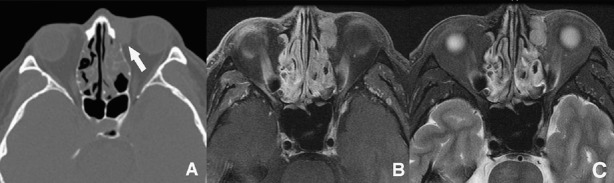
Fig. 1.
There is an elastic, nontender, and nonmovable mass around left lacrimal sac without inflammatory signs (arrow).
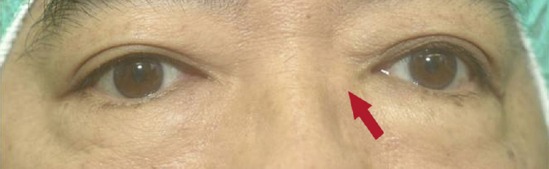
Fig. 2.
(A) Facial paranasal sinus computed tomography reveals a homogeneous high-density cyst-like lesion over the left lacrimal sac (arrow). Marked periosteal mucosal thickening of the nasal cavity with polypoid lesions is also noted. (B) Head orbits postgadolinium T1-weighted magnetic resonance imaging (MRI) reveals an iso- to hyperintense homogeneous lesion (17 mm × 12 mm × 20 mm) with contrast enhancement over left lacrimal sac. Paranasal sinusitis is also noted. (C) T2-weighted MRI reveals slightly hyperintense signal of the lesion.
Fig. 3.
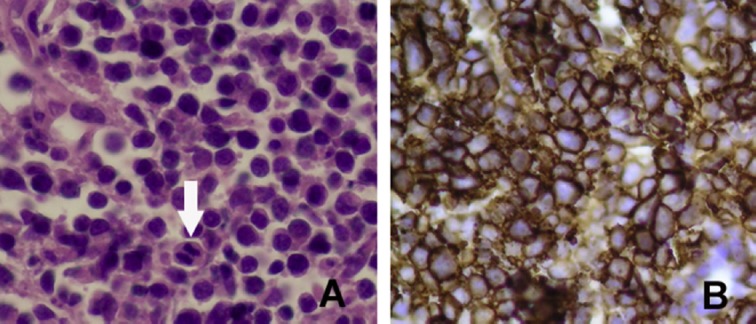
(A) Histopathological studies reveal diffuse infiltration of medium-sized to large neoplastic cells with high mitotic activity (arrow; hematoxylin and eosin stain, ×400). (B) The immunohistochemical stain shows the neoplastic cells with CD20 (+) (×400).
Fig. 4.
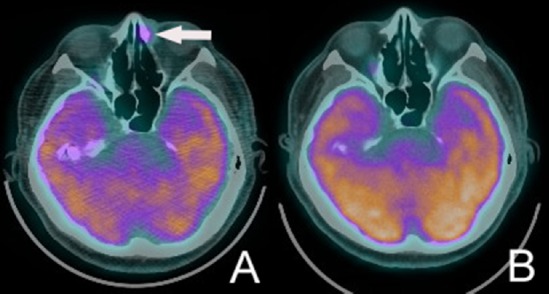
(A) Whole-body fludeoxyglucose positron emission tomography (FDG PET) scan demonstrates focal increased FDG uptake in the inferior medial aspect of left orbital cavity (arrow). (B) One year after rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) therapy, no abnormal glucose metabolic region is found in the whole-body FDG PET scan.
3. Discussion
In clinical practice, one rarely encounters primary tumor of the lacrimal sac. Among the recorded cases, 55% are considered malignant and 71% are of epithelial origin.1 Malignant lymphomas account for approximately 6% of all lacrimal sac tumors.1 They are usually secondary to systemic lymphoreticular malignancies. Primary non-Hodgkin's lymphoma of lacrimal sac is extremely rare in the literature.2
Primary lacrimal sac lymphomas usually occur in elderly people.2 Previous studies demonstrated that the 5-year overall survival rate was about between 20% and 65% and showed a poor prognosis for patients with DLBCL involving the ocular adnexal region.2,3,4 The symptoms are usually nonspecific, and therefore some were initially misdiagnosed as dacryocystitis.3,4 In the present case, our initial diagnosis was a mucocele. One report showed that a correct and prompt diagnosis occurs in < 15% of cases with malignant lacrimal sac tumors.5 Some patients were inadvertently diagnosed during dacryocystorhinostomy or other procedures.6 Biopsy should be confirmed in lacrimal sac tumors. CT and MR images can aid in making a definite diagnosis, staging, and planning treatment.5 The mucocele or inflammatory dacryocystitis on CT scan displays a nonenhancing homogenous mass with expansion of the bony walls and reveals a hyperintense mass on T2-weighted MR images.7 However, the lymphoma shows a hypointense signal on T2-weighted images instead.5 Our case had a slightly hyperintense lesion on T2 images. Moreover, the lesion was just adjacent to the nasal cavity. Discriminating between mucoceles and lymphomas using MR images may require pathological tests for confirmation in certain cases.
Meunier et al8 reported that certain factors, such as age (older than 59 years), elevated LDH level, stage IV, high-grade histological subgroup, and presence of B symptoms (fever, night sweats, and weight loss), had a negative impact on the overall survival of patients with ocular non-Hodgkin's lymphoma. Rasmussen et al9 found that concordant bone marrow involvement was an independent poor prognostic factor in ocular adnexal DLBCL. In the present case, the patient was younger with normal LDH level and had no bone marrow metastasis. His treatment prognosis is favorable.
Systemic chemotherapy is effective in the treatment of localized DLBCL.9 The recently introduced R-CHOP regimen has improved the survival rate.10 Rituximab is a monoclonal chimeric anti-CD20 antibody that has been extensively used in treatment of B cell non-Hodgkin's lymphoma.10 Its combination with chemotherapy has a significant benefit compared with chemotherapy alone in terms of response rate, progression-free survival, and overall survival in patients with DLBCLs.10
In conclusion, malignant lymphomas of the lacrimal sac are rare and they can mimic mucoceles or dacryocystitis. A differential diagnosis using neuroimages and biopsy is essential in making an accurate diagnosis. The current treatment of choice for lacrimal sac DLBCL is the R-CHOP regimen.
Footnotes
Conflicts of interest: None for all authors.
References
- 1.Stefanyszyn MA, Hidayat AA, Pe’er JJ, Flanagan JC. Lacrimal sac tumors. Ophthal Plast Reconstr Surg. 1994;10:169–184. doi: 10.1097/00002341-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Sjo LD, Ralfkiaer E, Juhl BR, Prause JU, Kivelä T, Auw-Haedrich C, et al. Primary lymphoma of the lacrimal sac: an EORTC ophthalmic oncology task force study. Br J Ophthalmol. 2006;90:1004–1009. doi: 10.1136/bjo.2006.090589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Palma P, Ravalli L, Modestino R, Grisanti F, Casillo F, Marzola A. Primary lacrimal sac B-cell immunoblastic lymphoma simulating an acute dacryocys-titis. Orbit. 2003;22:171–175. doi: 10.1076/orbi.22.3.171.15620. [DOI] [PubMed] [Google Scholar]
- 4.Palamar M, Midilli R, Ozsan N, Egrilmez S, Sahin F, Yagci A. Primary diffuse large B-cell lymphoma of the lacrimal sac simulating chronic dacryocystitis. Auris Nasus Larynx. 2011;38:643–645. doi: 10.1016/j.anl.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Montalban A, Lietin B, Louvrier C, Russier M, Kemeny JL, Mom T, et al. Malignant lacrimal sac tumors. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:165–172. doi: 10.1016/j.anorl.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Tucker N, Chow D, Stockl F, Codere F, Burnier M. Clinically suspected primary acquired nasolacrimal duct obstruction: clinicopathologic review of 150 patients. Ophthalmology. 1997;104:1882–1886. doi: 10.1016/s0161-6420(97)30012-8. [DOI] [PubMed] [Google Scholar]
- 7.Capra GG, Carbone PN, Mullin DP. Paranasal sinus mucocele. Head Neck Pathol. 2012;6:369–372. doi: 10.1007/s12105-012-0359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meunier J, Lumbroso-Le Rouic L, Vincent-Salomon A, Dendale R, Asselain B, Arnaud P, et al. Ophthalmologic and intraocular non-Hodgkin's lymphoma: a large single centre study of initial characteristics, natural history, and prognostic factors. Hematol Oncol. 2004;22:143–158. doi: 10.1002/hon.741. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen PK, Ralfkiaer E, Prause JU, Sjö LD, Toft PB, Siersma VD, et al. Diffuse large B-cell lymphoma of the ocular adnexal region: a nation-based study. Acta Ophthalmol. 2013;91:163–169. doi: 10.1111/j.1755-3768.2011.02337.x. [DOI] [PubMed] [Google Scholar]
- 10.Decaudin D, de Cremoux P, Vincent-Salomon A, Dendale R, Rouic LL. Ocular adnexal lymphoma: a review of clinicopathologic features and treatment options. Blood. 2006;108:1451–1460. doi: 10.1182/blood-2006-02-005017. [DOI] [PubMed] [Google Scholar]