Abstract
Objective:
This study was undertaken to examine the characteristics of cancers detected at the earliest possible point on MRI and to determine their significance.
Methods:
This institutional review board-approved Health Insurance Portability and Accountability Act-compliant retrospective study evaluated invasive breast cancers ≤1 cm histologically. MRI was performed within 6 months before diagnosis. Between 1 January 2005 and 31 December 2015, 163 cancers in 161 patients were evaluated. Breast Imaging-Reporting and Data System lesion characteristics were assessed by two radiologists independently. In cases of disagreement, arbitration by a third reader was performed.
Results:
Cancers ≤1 cm became more obviously malignant as they enlarged with regard to shape (p = 0.021), margin (p = 0.0006), internal enhancement (p = 0.0158) and kinetics (p = 0.0001). Cancers ≤5 mm had benign characteristics of circumscribed margins in 71% (71/100), round/oval shape in 67% (67/100) and persistent enhancement in 41% (41/100). High T2 signal was found in 17% (28/62), distributed equally among different sizes (p = 0.3920). In ≤5-mm cancers (59%, 12/29), a comparison study to show interval growth was more often needed to determine the need for biopsy. When interval growth determined biopsy, this was evident within 24 months and cancers remained node negative despite this delay.
Conclusion:
Benign characteristics are present in most invasive cancers ≤5 mm. Small cancers on MRI may need to demonstrate growth to determine need for biopsy.
Advances in knowledge:
MR lesion characteristics may not be helpful in determining whether small lesions on MR are benign or malignant. However, as 97% of cancers in our study showed interval change when a prior MR for comparison was available, new lesions or increasing size should lead to consideration of biopsy.
INTRODUCTION
Optimal screening for the detection of invasive breast cancer occurs when tumours are small, unifocal, node negative and without metastatic disease.1,2 Early breast cancer detection remains a challenge because small cancers may be less conspicuous than larger tumours on mammography, particularly in females with increased breast density.
The best technology to detect all cancers is MRI.3,4 Breast MRI has been demonstrated to have the highest sensitivity for breast cancer detection, ranging from 94% to 100%, and it can depict small invasive cancers measuring <5 mm.5–10 However, prior studies have shown that the ability of MRI to characterize a lesion as malignant increases with increasing size. In a study of 666 lesions, of which 149 were malignant, only 1/37 (3%) lesions <5 mm were cancerous, whereas 17% (44/254) of those between 5 and 10 mm were cancerous and the likelihood of malignancy increased with further increases in the lesion size up to 31% of 2-cm or larger lesions.8 In another study of MRI for high-risk screening, although the mean size of cancers found was 4 mm, some tumours were as large as 1.2 cm before they were diagnosed.5 Diagnosis of these tumours was made difficult by T2 hyperintensity in 2/6 invasive cancers and plateau kinetics in 3/6. Additionally, cancers on MRI may be possibly more biologically aggressive and of a higher grade than those detected on conventional imaging.11
This study was undertaken to examine the characteristics of cancers detected at the earliest possible point on MRI and to determine their characteristics.
METHODS AND MATERIALS
Patients
This Health Insurance Portability and Accountability Act-compliant retrospective study was undertaken with approval from the institutional review board. The need for informed consent was waived by the institutional review board. A search of medical records was undertaken to identify females with newly diagnosed single-site invasive breast cancer measuring ≤1 cm on pathology between 01 January 2005 and 31 December 2015, regardless of the histopathological subtype in whom breast MRI had been performed within 6 months prior to diagnosis. Of the 257 patients meeting these criteria, excluded from this study were patients with recurrent cancers (N = 50), patients with post-biopsy changes due to biopsy being performed before MRI (N = 20), patients with microinvasive ductal carcinoma in situ (N = 15) and patients whose cancers were not seen on MRI (N = 11). Therefore, 161 females with 163 newly diagnosed single site invasive breast cancers measuring ≤1 cm constituted the population of this study. In two patients, there was synchronous bilateral invasive cancer.
Patient characteristics are reported in Table 1.
Table 1.
Characteristics in females at the time of diagnosisa
| Patient age in years (N = 161) | Mean ± SD Median (range) |
56 ± 11 55 (32–81) |
| Interval in days between MRI and biopsy/excision (N = 161) | Mean ± SD Median (range) |
17 ± 14.5 13 (0–89) |
| Risk factors (N = 161) | None At least one reported |
28/161 (17) 133/161 (83) |
| Family history (N = 161) | Negative Positive 1st age ≤40 years 1st age >40 years 2nd degree Other |
57/161 (35) 104/161 (65) 25/104 (24) 52/104 (50) 15/104 (14) 12/104 (12) |
| Prior high-risk lesion (N = 161) | None Present ADH LCIS Papilloma Combination of above |
134/161 (83) 27/161 (17) 8/27 (30) 13/27 (48) 2/27 (7) 4/27 (15) |
| PH (N = 161) | Negative Positive PH ≤ age 40 PH > age 40 |
126/161 (78) 35/161 (22) 8/35 (23) 27/35 (77) |
| BRCA status (N = 161) | BRCA 1/2 tested negative BRCA 1 positive BRCA 2 positive Unknown |
47/161 (29) 14/161 (9) 7/161 (4) 93/161 (58) |
| History of mantle radiation to the chest (N = 161) | Negative Positive |
154/161 (96) 7/161 (4) |
| MR indication (N = 161) | Screening Extent of disease Symptoms Short term follow-up (BI-RADS 3) Architectural distortion on MG Asymmetry on MG Equivocal mass on MG |
90/161 (56) 41/161 (25) 8/161 (5) 6/161 (4) 6/161 (4) 4/161 (2) 6/161 (4) |
| Symptoms (N = 8) | Palpable lump Pain Nipple discharge |
4/8 (50) 2/8 (25) 2/8 (25) |
1st, first-degree relative; 2nd degree, second-degree relative; ADH, atypical ductal hyperplasia; BI-RADS, Breast Imaging-Reporting and Data System; LCIS, lobular carcinoma in situ; MG, mammogram; PH, personal history; SD, standard deviation.
Differences to 100% are due to rounding.
Data in parentheses are percentages, unless stated otherwise.
In two patients, there were synchronous bilateral lesions included in the study.
Tumour characteristics including size, histopathological results, oestrogen, progesterone, ERRB2 and nodal status were retrieved from the pathology reports. Tumour subtypes were categorized as luminal A (ER+ and/or PR+ and ERRB−), luminal B (ER+ and/or PR+ and ERRB+), triple negative (ER−, PR−, ERRB−) and ERRB+ (ER−, PR−, ERRB+) subtypes.
Breast MRI and imaging analysis
Breast MRI was performed either at the authors' institution (a tertiary cancer institution) in 135 cases or an outside facility in 28 cases where afterwards the patients were referred to the author's institution where MR images were reviewed. In-house MR examinations were performed while the patient lay prone on a commercially available 1.5-T system in 92 cases or 3-T systems in the remaining 43 cases (Sigma; GE Medical Systems, Milwaukee, WI). All in-house studies were carried out with a dedicated breast coil. Recorded sequences included a localizing sequence, a sagittal T2 weighted sequence with fat suppression and a T1 weighted three-dimensional, fat-suppressed fast spoiled gradient-echo sequence before and three times after rapid bolus injection of 0.1 mmol l−1 gadopentetate dimeglumine (Magnevist®; Berlex, Wayne, NJ) per kilogram of body weight.
Breast MR examinations were independently reviewed for this study on a dedicated workstation by two readers with 20 (initials blinded for review) and 3 (initials blinded for review) years' experience in breast MRI and who were blinded to the pathology reports. For those cases in which there was not an initial agreement, a joint reading by the two readers was performed to obtain a consensus. For cases in which a consensus was not reached, arbitration reading was performed by a third reader (initials blinded for review) with 8 years' breast MR experience. All images were reviewed based on the 2013 Breast Imaging-Reporting and Data System (BI-RADS®) MRI lexicon.12 Lesion type, size on MR as the single largest diameter, signal intensity on T2 weighted images, shape, margin and internal enhancement characteristics in masses, and distribution and internal enhancement characteristics in non-masses were evaluated for each case. In cases with a prior breast MR, the lesion was assessed for interval change vs stability, and the interval to the prior MR examination in months was noted.
Time–intensity kinetic curve analysis was performed on a dedicated workstation with a commercially available computer-aided diagnosis system (Sentinelle Aegis Breast 3.0 software; Sentinelle Medical Inc., Toronto, ON) by one reader (MM). The kinetic curve pattern was grouped into three types (washout, plateau and persistent). However, in 12 lesions, kinetic data analysis could not be performed due to severe motion artefacts or technical difficulties with the outside MR examinations.
Statistical analysis
All parameters were entered into an MS Excel® (Microsoft®, Redmond, WA) spreadsheet. Univariate analysis was conducted and used to report summary statistics, including frequencies, means, medians and ranges of patient characteristics at the time of diagnosis. MR and pathological lesion characteristics were examined using χ2 or Fisher's exact test for categorical variables and t-tests for continuous variables. All p-values were two-tailed and p-values < 0.05 were considered statistically significant. The kappa coefficient was used to measure the concordance of lesion characteristics on MRI readings. All statistical analyses were performed using SAS statistical software v. 9.4 (SAS Institute, Cary, NC).
RESULTS
MR characteristics according to lesion size
136/163 (83%) cases were invasive ductal cancer with or without other histologies, 26/163 (16%) were invasive lobular cancer and there was 1 case of invasive matrix-producing cancer. 20/163 (13%) were triple negative cancers, which would be expected in this high-risk population. Patients showed no evidence for nodal micro- or macrometastases, although four cases showed single tumour cells in axillary lymph nodes.
MR characteristics according to lesion size
Lesion characteristics on MR for all lesions and according to their size on MR are given in Table 2.
Table 2.
MR characteristics according to lesion size on MR
| Lesion size on MR in millimetres | All | ≤5 | >5 to ≤10 | >10 to ≤15 | >15 | p-value | |
|---|---|---|---|---|---|---|---|
| Number of cases (N = 163) |
163 (100) | 29 (18) | 111 (68) | 17 (10) | 6 (4) | ||
| MR lesion type (N = 163) | Focus Mass Non-mass |
8/163 (5) 129/163 (79) 26/163 (16) |
8/29 (28) 21/29 (72) 0/29 (0) |
− 95/111 (86) 16/111 (14) |
− 13/17 (76) 4/17 (24) |
− 0/6 (0) 6/6 (100) |
0.001 |
| Shape in masses (N = 129) | Round Oval Irregular |
14/129 (11) 35/129 (27) 80/129 (62) |
5/21 (24) 9/21 (43) 7/21 (33) |
9/95 (9) 24/95 (25) 62/95 (65) |
0/13 (0) 2/13 (15) 11/13 (85) |
No masses | 0.021 |
| Margin in masses (N = 129) | Circumscribed Non-circumscribed |
44/129 (34) 85/129 (66) |
15/21 (71) 6/21 (29) |
26/95 (27) 69/95 (73) |
3/13 (23) 10/13 (77) |
No masses | 0.0006 |
| Mass—internal enhancement (N = 129) | Homogeneous N-e. int. sept. Heterogeneous Rim-enhanc. |
9/129 (7) 1/129 (1) 97/129 (75) 22/129 (17) |
6/21 (29) 0/21 (0) 12/21 (57) 3/21 (14) |
3/95 (3) 1/95 (1) 74/95 (78) 17/95 (18) |
0/13 (0) 0/13 (0) 11/13 (85) 2/13 (15) |
No masses | 0.0158 |
| Non-mass—distribution (N = 26) | Linear Focal Regional Segmental Multiple region Diffuse |
15/26 (58) 11/26 (42) 0/26 (0) 0/26 (0) 0/26 (0) 0/26 (0) |
None | 11/16 (69) 5/16 (31) 0/16 (0) 0/16 (0) 0/16 (0) 0/16 (0) |
2/4 (50) 2/4 (50) 0/4 (0) 0/4 (0) 0/4 (0) 0/4 (0) |
2/6 (33) 4/6 (67) 0/6 (0) 0/6 (0) 0/6 (0) 0/6 (0) |
0.3396 |
| Non-mass—internal enhancement (N = 26) | Homogeneous Clumped Heterogeneous Clustered ring |
3/26 (12) 13/26 (50) 9/26 (35) 1/26 (4) |
None | 3/16 (19) 10/16 (63) 3/16 (19) 0/16 (0) |
0/4 (0) 2/4 (50) 2/4 (50) 0/4 (0) |
0/6 (0) 1/6 (17) 4/6 (67) 1/6 (17) |
0.1027 |
| Kinetics (N = 151, NA in 12 cases) | Washout Plateau Persistent |
81/151 (54) 24/151 (16) 46/151 (30) |
11/27 (41) 5/27 (19) 11/27 (41) |
56/101 (55) 16/101 (16) 29/101 (29) |
10/17 (59) 2/17 (12) 5/17 (29) |
4/6 (67) 1/6 (17) 1/6 (17) |
0.0001 |
| T2 signal (N = 162, NA in 1 case) | High Iso Low |
28/162 (17) 45/162 (28) 89/162 (55) |
6/29 (21) 7/29 (24) 16/29 (55) |
18/110 (16) 28/110 (25) 64/110 (58) |
3/17 (18) 8/17 (47) 6/17 (35) |
1/6 (17) 2/6 (33) 3/6 (50) |
0.3920 |
NA, not available or not applicable; N-e. int. sept., non-enhancing internal septations; Rim-enhanc., rim enhancing.
Lesion size on MR defined as the single largest diameter in millimetres. Differences to 100% are due to rounding.
Data in parentheses are percentages, unless otherwise stated.
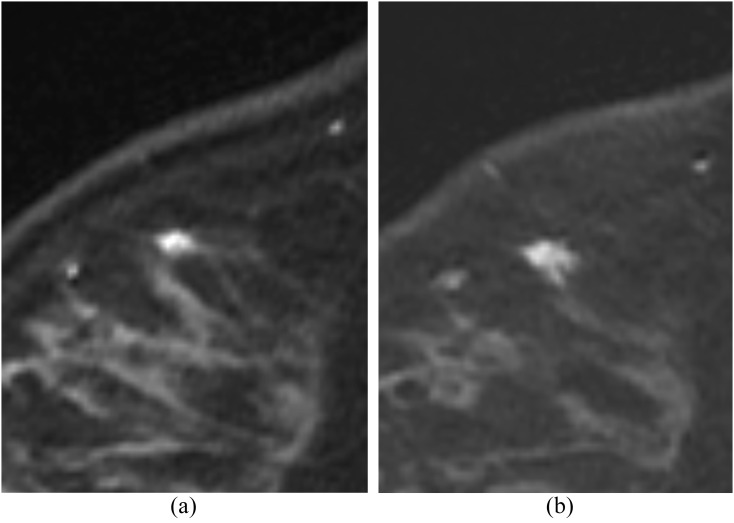
Masses ≤5 mm showed typically benign MR indicators including circumscribed margins (15/21, 71%), oval or round shape (14/21, 67%) (Figure 1). Kinetics was evaluable for 27 of 29 malignant masses, and persistent enhancement was seen in 41% (11/27). As masses increased to >10 mm, they became increasingly irregular (11/13, 85%), increasingly non-circumscribed (10/13, 77%) and increasingly heterogeneously enhancing (11/13, 85%) (Figure 2).
Figure 1.
A 64-year-old patient with positive family history of breast cancer and new nipple discharge for diagnostic MRI. T1 post-contrast study shows a focus that was a 3-mm invasive ductal carcinoma.
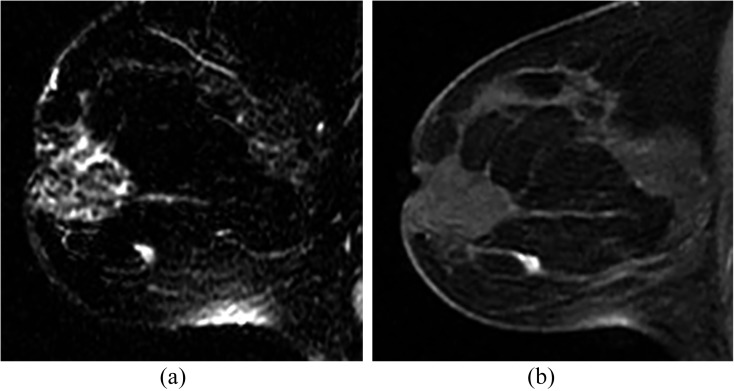
Figure 2.
A 33-year-old BRCA-positive female for screening. T1 fat suppressed first post-contrast images. (a) Baseline study showing indeterminate solitary focus of enhancement. (b) 6 months later, the lesion is now slightly larger and spiculated. Biopsy showed a 5-mm invasive ductal carcinoma.
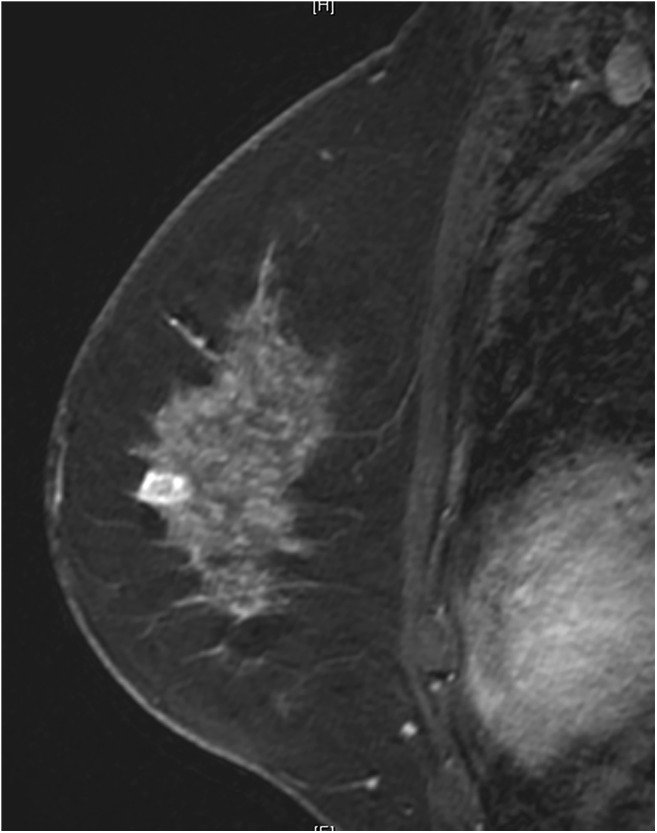
For non-mass enhancement of >10 mm, internal enhancement became increasingly heterogeneous (6/10, 60%) as the size increased to >10 mm vs 19% (3/16) in smaller non-mass enhancing lesions (Figure 3). Non-mass distribution of a linear pattern decreased from 69% (11/16) for non-mass enhancement ≤10 mm, to 40% (4/10) for non-mass enhancement >10 mm and larger lesions were increasingly described as focal. More suspicious characteristics were found with increasing size on MR, and these were statistically significant for shape (p = 0.021), margin (p = 0.0006) and internal enhancement pattern (p = 0.0158) in masses and kinetics among all lesion types (p = 0.0001) (Figure 4).
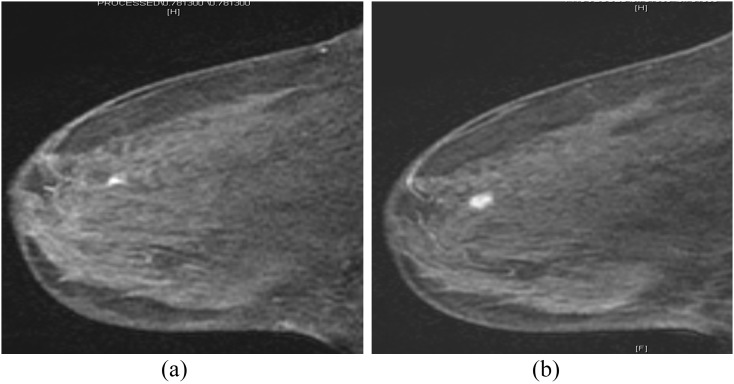
Figure 3.
A 60-year-old BRCA-positive female with personal history of breast cancer for screening. T1 post-contrast fat-suppressed study show solitary enhancing mass which, when windowed and levelled, has non-enhancing septations. Biopsy showed a 5-mm invasive ductal carcinoma (arrow).
Figure 4.
A 50-year-old female with positive family history and the initial screening MRI showing rim-enhancing mass which was a 6-mm invasive ductal carcinoma on biopsy.
Unexpectedly high percentages of lesions with characteristically benign findings were distributed among all lesions, including persistent kinetics (30%, 46/151). Additionally, high T2 signal was present in 17% (28/162), independent of size (p = 0.3920) (Figure 5).
Figure 5.
A 43-year-old female with extensive ductal carcinoma in situ in the opposite breast; work-up for extent of disease. (a) T2 weighted image shows solitary lesion with high signal. (b) Irregular enhancing mass on T1 fat-suppressed first post-contrast image. Biopsy showed a 6-mm poorly differentiated invasive ductal carcinoma.
In malignant foci, kinetics and T2 signal characteristics were not useful in determining that they were not benign. 2/8 (25%) showed high T2 signal. Of 7 for which kinetics were evaluable, 4/7 (57%) had persistent enhancement.
MR characteristics according to histological grade
MR characteristics according to histological grade are given in Table 3. Although more malignant kinetics were more likely associated with higher histological grade (p = 0.0298), there was no significant association between other suspicious BI-RADS descriptors and a higher histological grade. Of 73 lesions with washout for which histological grading was available, 36 (49%) were of a high histological grade, 25 (34%) of intermediate grades and 12 (16%) of low histological grades. Among 38 lesions with persistent kinetics, only 8 (21%) were of a high histological grade compared with 16 (42) intermediate and 14 (37%) low histological grades.
Table 3.
MR characteristics according to histological grade (N = 140, grading NA in 23 cases)
| MR characteristic | Grade 1 | Grade 2 | Grade 3 | p-value | |
|---|---|---|---|---|---|
| Number of cases (N = 140) |
30/140 (21) | 55/140 (39) | 55/140 (39) | ||
| Lesion type (N = 140) | Focus Mass Non-mass |
4/8 (50) 22/112 (19) 4/20 (20) |
3/8 (38) 45/112 (40) 7/20 (35) |
1/8 (13) 45/112 (40) 9/20 (45) |
0.3255 |
| T2 signal (N = 140) | High Iso Low |
5/27 (19) 8/42 (19) 17/71 (24) |
9/27 (33) 18/42 (43) 28/71 (39) |
13/27 (48) 16/42 (38) 26/71 (37) |
0.8315 |
| Delayed kinetic enhancement (N = 130) | Washout Plateau Persistent |
12/73 (16) 3/19 (16) 14/38 (37) |
25/73 (34) 8/19 (42) 16/38 (42) |
36/73 (49) 8/19 (42) 8/38 (21) |
0.0298 |
| Masses—shape (N = 112) | Round Oval Irregular |
2/12 (17) 8/31 (25) 12/69 (17) |
6/12 (50) 9/31 (29) 30/69 (43) |
4/12 (33) 14/31 (45) 27/69 (39) |
0.6110 |
| Masses—margin (N = 112) | Circumscribed Non-circumscribed |
8/37 (22) 14/75 (19) |
14/37 (38) 31/75 (41) |
15/37 (41) 30/75 (40) |
0.9649 |
| Masses—internal enhancement pattern (N = 112) | Heterogeneous Rim-enhancement Homogeneous Non-enhancing internal septation |
18/86 (21) 3/18 (17) 1/7 (14) 0/1 (0) |
32/86 (37) 8/18 (44) 5/7 (71) 0/1 (0) |
36/86 (42) 7/18 (39) 1/7 (14) 1/1 (100) |
0.6132 |
| Non-mass—distribution (N = 20) | Linear Focal Segmental Regional Multiple regions Diffuse |
3/11 (27) 1/9 (11) 0/0 (0) 0/0 (0) 0/0 (0) 0/0 (0) |
4/11 (36) 3/9 (33) 0/0 (0) 0/0 (0) 0/0 (0) 0/0 (0) |
4/11 (36) 5/9 (56) 0/0 (0) 0/0 (0) 0/0 (0) 0/0 (0) |
0.8425 |
| Non-mass—internal enhancement pattern (N = 20) | Clumped Heterogeneous Homogeneous Clustered ring |
2/9 (22) 1/8 (13) 1/2 (50) 0/1 (0) |
3/9 (33) 3/8 (38) 1/2 (50) 0/1 (0) |
4/9 (44) 4/8 (50) 0/2 (0) 1/1 (100) |
0.9041 |
NA, not available or not applicable.
Lesion size defined as the single largest diameter in millimetres. Differences to 100% are due to rounding.
Data in parentheses are percentages.
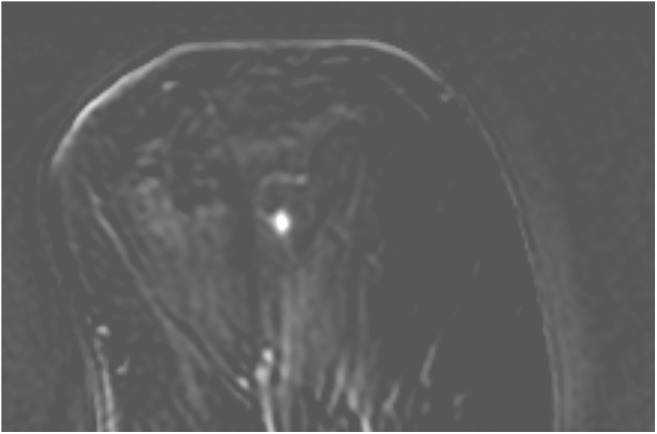
Reference standard
The recommendation to biopsy lesions was based on changes on a follow-up MRI in 72 cases. Interval changes of new lesion, increasing size or conspicuity was present in 70/72 (97%) of cases (Figure 6). Interval change of lesions vs stability over interval to prior MR examination is shown in Figure 3. In none of these small cancers was a follow-up study of more than 24 months needed to demonstrate interval growth.
Figure 6.
A 46-year-old female with positive family history and the initial screening MRI showing (a) enhancing focus interpreted as Breast Imaging-Reporting and Data System 3. (b) 6 months later, some enlargement noted. Biopsy showed a 4-mm invasive ductal carcinoma.
In 91 cases, the recommendation to biopsy was based on a single MRI study (Table 4). Of these, 39 (39/91, 43%) were studies carried out for the extent of disease that found suspicious enhancing lesions in the contralateral breast. Biopsy was performed based on a single study showing suspicious morphology or kinetics in only 17% (2/12) of cancers ≤5 mm but in 43% (34/79) of larger tumours.
Table 4.
Indication for biopsy in cases with a single MRI
| Lesion size on MR in millimetres | All | ≤5 | >5 to ≤10 | >10 to ≤15 | >15 | p-value |
|---|---|---|---|---|---|---|
| Number of cases (N = 91) | 91 (100) | 12 | 63 | 12 | 4 | |
| Known cancer on contralateral side (extent of disease) Suspicious morphology/kinetics on MR Indeterminate single dominant lesion Suspicious mammographic correlate Palpable lesion |
3934 8 9 1 |
4 (33) 2 (17) 6 (50) 0 (0) 0 (0) |
30 (47) 24 (38) 2 (3) 6 (10) 1 (2) |
5 (42) 6 (50) 0 (0) 1 (8) 0 (0) |
0 (0) 4 (100) 0 (0) 0 (0) 0 (0) |
0.036 |
Differences to 100% are due to rounding.
Data in parentheses are percentages.
Although follow-up examinations of up to 24 months were required to identify some of these cancers, nodal status was negative in all cases. Of note, four cases showed single cells in axillary nodes, but this was not clinically significant and did not impact treatment.
Except for foci which by definition were all ≤5 mm, MRI tended to overestimate lesion size compared with histopathology, more so for non-mass enhancement than masses. For masses, the mean size and standard deviation on MR were 7.8 ± 2.2 mm vs pathological measurement of 6.5 ± 2.3 mm. For non-mass enhancement, the MR size was 12.6 ± 6.6 mm vs pathological measurement of 6.1 ± 2.1 mm. Overestimation by MR was statistically significant for both masses and non-mass enhancement (p < 0.0001). The reason for overestimation in MR-measured lesions >10 mm may be the co-existent ductal carcinoma in situ (DCIS) which was present in 9/10 (90%) non-mass lesions and 12/13 mass lesions >10 mm (92%). DCIS was also present in many smaller lesions including 8/16 (50%) non-mass lesions and 91/116 (78%) mass lesions ≤10 mm. For non-masses, the increased presence of DCIS among MR-measured lesions >10 mm compared with those ≤10 mm on MR was statistically significant (p = 0.037), but this was not statistically significant for masses (p = 0.237).
It is also interesting to note that magnet strength did not appear to have an impact on the ability to discover these small, invasive cancers. Of the 135 studies that were performed in-house and in which the magnet strength was known, 92 (68%) were performed with 1.5-T magnet.
DISCUSSION
Breast MRI is superior to mammography and ultrasound in detecting suspicious lesions, and sensitivities of MRI for invasive cancer approach 94–100%.5–10,13,14 Historically, breast MRI has been recommended for females at >20% lifetime risk for breast cancer.15
Because MRI is a functional examination depicting blood flow and is not only based on anatomical changes but also can depict cancers measuring only a few millimetres.16 The problem is that these lesions are benign in the vast majority of cases, resulting in a low specificity of MRI for these small cancers.8,16–19 Cancers >1 cm have been well characterized on MRI. Criteria for malignancy include irregular shape, non-circumscribed margins, hypervascularity and washout kinetics.5–9,19,20
In our study, correlation of tumour size on MR and histopathology was not always reliable. In cancers >1 cm, we hypothesize that this may be due to co-existent enhancing DCIS. In smaller lesions, the reason is uncertain, but those who are accustomed to measuring small lesions on MR know that minimal movements of electronic calibres can result in measurement changes of several millimetres. This may at least partially account for these differences.
Our data show that cancers measuring ≤5 mm typically have benign margin (71%), shape (67%) and kinetic characteristics (41%). Cancers ≤1 cm demonstrate a high frequency of benign persistent enhancement (30%) and high T2 signal (17%). This is greater than in series with larger cancers.5–9,19,20
Whether cancers need to grow beyond a certain size in order to establish the characteristic malignant findings such as irregularity in shape and margin or T2 hypointensity or whether the limited resolution of MRI for lesions measuring only a few millimetres is the more important factor accounting for their more benign pattern was not assessed in our study.
The question remains that if there is a difference in the MRI pattern of subcentimetre malignancy compared with larger cancers, is there an effective method of differentiating the smallest enhancing cancers from mundane benign foci? According to the current American College of Radiology BI-RADS lexicon, the smallest lesion type in MRI is a focus, which is defined as an enhancing lesion measuring 5 mm or less.12 In its original definition, a focus is too small to reliably apply morphological characteristics or region of interest dynamic data for characterization. Most foci represent a benign finding such as a small fibroadenoma, an intramammary lymph node or fibrocystic changes.16 However, invasive malignancy has been reported, and the likelihood of finding cancer on biopsy of a solitary enhancing focus ranges from 0.6% to 2.3%, including one study demonstrating this likelihood is significantly higher with increasing proximity to known cancer.8,16,21,22 As the spatial resolution increases in MRI, it has been suggested to consider foci measuring 4–5 mm as small masses and apply lesion morphological criteria such as unsharp margin and low signal on T2 weighted images.12,22 However, according to our data, morphological characteristics, T2 signal and kinetics in malignant foci and masses ≤5 mm were not useful in determining if these were benign or malignant.
Characteristically benign kinetics may be present in malignant lesions, making their diagnosis difficult. However, in our study, malignant enhancement characteristics (washout) were found in 54% of these cancers, facilitating the diagnosis of tumours which were more likely of a higher histological grade (p = 0.0298).
The decision to biopsy a solitary lesion based on a single MR study because of its suspicious morphology or kinetics was increasingly likely as lesion size increased, progressing from 17% (2/12) of ≤5-mm lesions to 38% (2410 mm/63) of >5- to ≤10-mm lesions to 63% (10/16) of cancers >10 mm on MRI.
The decision to biopsy a cancer ≤5 mm was only performed based on a single study in 41% (12/29) vs 59% (79/134) for larger cancers, almost a 50% increase. Conversely, a prior MRI was necessary to show interval change before ≤5-mm lesions underwent biopsy in 59% (17/29) vs only 41% (55/134) of larger cancers.
Among cases for which prior MR examinations were available, invasive cancers disclosed themselves by interval change within 2 years of initial appearance on MR. It seems unlikely that continued short-term follow-up (6-month interval) is useful in diagnosing after lesions have been observed for 2 years. Annual follow-up to detect small malignancies seems adequate. The appearance of new enhancing findings should lead to consideration of biopsy.
The study is limited by the small number of lesions in the groups of foci and lesions ≤5 mm. It is hoped that studies from other institutions can expand the published experience with these very small lesions. Additionally, data derived from the experience of a single institution invariably need confirmation from other sites.
CONCLUSION
As invasive breast cancers approach 1 cm, characteristics on MRI become increasingly typical of malignancy, but those cancers ≤5 mm are difficult to distinguish from the more usual, benign lesions with which they share similar characteristics. If the clinical setting does not suggest that their immediate biopsy is appropriate, short-term follow-up studies are useful to identify the need for their biopsy as they develop more worrisome patterns.
FUNDING
This research was funded in part through the National Institutes of Health/National Cancer Institute Cancer Centre Support Grant P30 CA008748. MM received financial support for travel and accommodation expenses related to the project from the Paracelsus Medical University Research Fund—under the number S-16/02/009—MEI.
Contributor Information
Matthias Meissnitzer, Email: m.meissnitzer@salk.at.
D David Dershaw, Email: dershawd@mskcc.org.
Kimberly Feigin, Email: feigink@mskcc.org.
Blanca Bernard-Davila, Email: bernardb@mskcc.org.
Filipe Barra, Email: Filipebarra@gmail.com.
Elizabeth A Morris, Email: morrise@mskcc.org.
REFERENCES
- 1.Elkin EB, Hudis C, Begg CB, Schrag D. The effect of changes in tumor size on breast carcinoma survival in the U.S.: 1975–1999. Cancer 2005; 104: 1149–57. [DOI] [PubMed] [Google Scholar]
- 2.Narod SA. Age of diagnosis, tumor size, and survival after breast cancer: implications for mammographic screening. Breast Cancer Res Treat 2011; 128: 259–66. doi: https://doi.org/10.1007/s10549-010-1318-9 [DOI] [PubMed] [Google Scholar]
- 3.Lee CH, Dershaw DD, Kopans D, Evans P, Monsees B, Monticciolo D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol 2010; 7: 18–27. doi: https://doi.org/10.1016/j.jacr.2009.09.022 [DOI] [PubMed] [Google Scholar]
- 4.Berg WA, Gutierrez L, NessAiver MS, Carter WB, Bhargavan M, Lewis RS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology 2004; 233: 830–49. doi: https://doi.org/10.1148/radiol.2333031484 [DOI] [PubMed] [Google Scholar]
- 5.Morris EA, Liberman L, Ballon DJ, Robson M, Abramson AF, Heerdt A, et al. MRI of occult breast carcinoma in a high-risk population. AJR Am J Roentgenol 2003; 181: 619–26. doi: https://doi.org/10.2214/ajr.181.3.1810619 [DOI] [PubMed] [Google Scholar]
- 6.Bluemke DA, Gatsonis CA, Chen MH, DeAngelis GA, DeBruhl N, Harms S, et al. Magnetic resonance imaging of the breast prior to biopsy. JAMA 2004; 292: 2735–42. doi: https://doi.org/10.1001/jama.292.22.2735 [DOI] [PubMed] [Google Scholar]
- 7.Orel SG, Schnall MD. MR imaging of the breast for the detection, diagnosis, and staging of breast cancer. Radiology 2001; 220: 13–30. doi: https://doi.org/10.1148/radiology.220.1.r01jl3113 [DOI] [PubMed] [Google Scholar]
- 8.Liberman L, Mason G, Morris EA, Dershaw DD. Does size matter? Positive predictive value of MRI-detected breast lesions as a function of lesion size. AJR Am J Roentgenol 2006; 186: 426–30. doi: https://doi.org/10.2214/ajr.04.1707 [DOI] [PubMed] [Google Scholar]
- 9.Eby PR, DeMartini WB, Gutierrez RL, Saini MH, Peacock S, Lehman CD. Characteristics of probably benign breast MRI lesions. AJR Am J Roentgenol 2009; 193: 861–7. doi: https://doi.org/10.2214/ajr.08.2096 [DOI] [PubMed] [Google Scholar]
- 10.Weinstein SP, Hanna LG, Gatsonis C, Schnall MD, Rosen MA, Lehman CD. Frequency of malignancy seen in probably benign lesions at contrast-enhanced breast MR imaging: findings from ACRIN 6667. Radiology 2010; 255: 731–7. doi: https://doi.org/10.1148/radiol.10081712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sung JS, Stamler S, Brooks J, Kaplan J, Huang T, Dershaw DD, et al. Breast cancers detected at screening MR imaging and mammography in patients at high risk: method of detection reflects tumor histopathologic results. Radiology 2016; 280: 716–22. doi: https://doi.org/10.1148/radiol.2016151419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris E, Comstock C, Lee C. ACR BI-RADS® magnetic resonance imaging. In: ACR BI-RADS®Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology; 2013. [Google Scholar]
- 13.Kuhl CK, Schrading S, Leutner CC, Morakkabati-Spitz N, Wardelmann E, Fimmers R, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol 2005; 23: 8469–76. [DOI] [PubMed] [Google Scholar]
- 14.Warner E, Messersmith H, Causer P, Eisen A, Shumak R, Plewes D. Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann Intern Med 2008; 148: 671–9. [DOI] [PubMed] [Google Scholar]
- 15.Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57: 75–89. doi: https://doi.org/10.3322/canjclin.57.2.75 [DOI] [PubMed] [Google Scholar]
- 16.Ha R, Sung J, Lee C, Comstock C, Wynn R, Morris E. Characteristics and outcome of enhancing foci followed on breast MRI with management implications. Clin Radiol 2014; 69: 715–20. doi: https://doi.org/10.1016/j.crad.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 17.Nunes LW, Schnall MD, Orel SG, Hochman MG, Langlotz CP, Reynolds CA, et al. Breast MR imaging: interpretation model. Radiology 1997; 202: 833–41. doi: https://doi.org/10.1148/radiology.202.3.9051042 [DOI] [PubMed] [Google Scholar]
- 18.Kuhl CK, Mielcareck P, Klaschik S, Leutner C, Wardelmann E, Gieseke J, et al. Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology 1999; 211: 101–10. doi: https://doi.org/10.1148/radiology.211.1.r99ap38101 [DOI] [PubMed] [Google Scholar]
- 19.Kinkel K, Helbich TH, Esserman LJ, Barclay J, Schwerin EH, Sickles EA, et al. Dynamic high-spatial-resolution MR imaging of suspicious breast lesions: diagnostic criteria and interobserver variability. AJR Am J Roentgenol 2000; 175: 35–43. doi: https://doi.org/10.2214/ajr.175.1.1750035 [DOI] [PubMed] [Google Scholar]
- 20.Kuhl CK, Klaschik S, Mielcarek P, Gieseke J, Wardelmann E, Schild HH. Do T2 weighted pulse sequences help with the differential diagnosis of enhancing lesions in dynamic breast MRI? J Magn Reson Imaging 1999; 9: 187–96. [DOI] [PubMed] [Google Scholar]
- 21.Raza S, Sekar M, Ong EM, Birdwell RL. Small masses on breast MR: is biopsy necessary? Acad Radiol 2012; 19: 412–9. doi: https://doi.org/10.1016/j.acra.2011.12.014 [DOI] [PubMed] [Google Scholar]
- 22.Ha R, Comstock CE. Breast magnetic resonance imaging: management of an enhancing focus. Radiol Clin 2014; 52: 585–9. doi: https://doi.org/10.1016/j.rcl.2014.01.001 [DOI] [PubMed] [Google Scholar]