Abstract
The objective of the study was to examine the mediating effect of child dental use on the effectiveness of North Carolina Early Head Start (EHS) in improving oral health–related quality of life (OHRQoL). In total, 479 parents of children enrolled in EHS and 699 parents of Medicaid-matched children were interviewed at baseline when children were approximately 10 mo old and 24 mo later. In this quasi-experimental study, mediation analysis was performed using the counterfactual framework analysis, which employed 2 logit models with random effects: 1) for the mediator as a function of the treatment and covariates and 2) for the outcome as a function of the treatment, mediator, and covariates. The covariates were baseline dental OHRQoL, dental need, survey language, and a propensity score. We used in-person computer-assisted, structured interviews to collect information on demographic characteristics and dental use and to administer the Early Childhood Oral Health Impact Scale, a measure of OHRQoL. Dental use had a mediation effect in the undesired direction with a 2–percentage point increase in the probability of any negative impact to OHRQoL (95% confidence interval [CI], 0.3%–3.9%). Even with higher dental use by EHS participants, the probability of any negative impact to OHRQoL was approximately 8 percentage points lower if an individual were moved from the non-EHS group to the EHS group (95% CI, −13.9% to −1.2%). EHS increases child dental use, which worsens family OHRQoL. However, EHS is associated with improved OHRQoL overall.
Knowledge Transfer Statement: Study results can inform policy makers that comprehensive early childhood education programs improve oral health–related quality of life (OHRQoL) for disadvantaged families with young children in pathways outside of clinical dental care. This awareness and its promotion can lead to greater resource investments in early childhood education programs. Information about the negative impacts of dental use on OHRQoL should lead to the development and testing of strategies in dentistry and Early Head Start to improve dental care experiences.
Keywords: community health services, child health services, early intervention (education), health status disparities, health care disparities, North Carolina
Introduction
Early Head Start (EHS) is a national comprehensive early education program designed to improve the lives of low-income families and children birth to 3 y of age (The Early Head Start National Resource Center 2016). EHS operates according to comprehensive federal performance standards that integrate oral health into their activities. The oral health performance standards include toothbrushing with fluoridated toothpaste, oral health education for the parent and child, and determination of a child’s oral health status by a dental professional (Head Start Bureau 2006; American Academy of Pediatrics 2008; American Academy of Pediatric Dentistry 2013).
Oral health–related quality of life (OHRQoL) is defined as “the impact of oral disorders on aspects of everyday life that are important to patients and persons, with those impacts being of sufficient magnitude, whether in terms of severity, frequency or duration, to affect an individual’s perception of their life overall” (Locker and Allen 2007). Dental caries, the most common dental disease in childhood, is associated with worse OHRQoL (Barbosa and Gavião 2008; Wong et al. 2011; Kramer et al. 2013; Scarpelli et al. 2013; Onoriobe et al. 2014), particularly when moderate to severe and left untreated (Scarpelli et al. 2013). Treatment of dental caries is associated with improved OHRQoL (Almaz et al. 2014; Jankauskiene et al. 2014; Abanto et al. 2016). However, its treatment can be associated with high treatment costs and distress to the family, potentially resulting in negative physical and psychological impacts on the child and family (Locker 1997; Oral Health in America 2000).
An important goal of EHS performance standards is to help ensure that children get comprehensive, age-appropriate dental care (Head Start Bureau 2016). By facilitating access to dental services, EHS may lead to improved OHRQoL. In a previous study, we confirmed that enrollment in EHS is associated with improved OHRQoL (Burgette et al. 2017a). We also found that enrollment in EHS had a strong positive effect on dental use by children younger than 3 y (Burgette et al. 2017b). It is unknown whether child’s dental use influences the effect of EHS on OHRQoL. We expect dental use to mediate the effect of EHS on OHRQoL because of our previous observations on the association of EHS with both improved dental use (Burgette et al. 2017b) and improved OHRQoL (Burgette et al. 2017a). In addition, existing literature supports an association between dental treatment and improved OHRQoL (Almaz et al. 2014; Jankauskiene et al. 2014; Abanto et al. 2016).
This study’s aim was to determine if the improvement in OHRQoL experienced by EHS families was mediated by dental use. We hypothesized that EHS activities connect EHS parent-child dyads with dental providers, which may increase dental use in compliance with EHS oral health performance standards, reduce oral health symptoms, and improve function. Thereby, dental use facilitated by EHS can improve OHRQoL. We seek to understand the role of pediatric dental use, an important pathway through which EHS enrollment might improve OHRQoL among families at increased risk for poor oral health. These findings will provide insight into how to improve OHRQoL for low-resource families through early childhood education programs.
Methods
Overview of Study Design and Data Source
We used data from the Zero Out Early Childhood Caries (ZOE) study, a 24-mo longitudinal prospective nonrandomized study to determine the effect of EHS on oral health outcomes. In the ZOE study, the EHS group is compared with a control group of Medicaid-enrolled children not enrolled in EHS. Teachers and staff in EHS programs received minimal training in oral health and communication techniques to bolster awareness of EHS performance standards and facilitate their implementation. The study was approved by the Institutional Review Board at the University of North Carolina and by the NC Head Start State Collaboration Office.
Study Population
Subjects were recruited using a 3-step process described in detail in a previous publication (Born et al. 2016): 1) enrollment of EHS programs, 2) enrollment of parent-child dyads within EHS programs, and 3) enrollment of community-matched parent-child dyads to serve as controls. In step 1, all North Carolina EHS programs were invited to participate; all except 1 were enrolled. In step 2, parents of EHS children <19 mo of age were recruited from all participating EHS programs. In step 3, children serving as controls were randomly selected from a population of Medicaid-enrolled children of the same age, language, and ZIP codes as already enrolled EHS subjects. The controls were recruited through direct mailings from the North Carolina Medicaid program. Our final sample included EHS and non-EHS parent-child dyads clustered within 25 of the 26 North Carolina EHS programs.
Trained personnel conducted in-person, computer-assisted, structured interviews with parents of eligible children at baseline and approximately 24 mo later (the time children aged out of the EHS program). The outcome variable of interest (OHRQoL) and the hypothesized mediator (dental use) were assessed during the 1-h interviews at both baseline and follow-up. Interviews were conducted in English or Spanish, as appropriate.
Conceptual Framework
We used a general health-related quality of life conceptual model developed by Ferrans and colleagues (2005) to study the impact of EHS on OHRQoL. In this model, both individual and environmental characteristics affect factors (biological function, symptoms, functional status, and general health perceptions) that led to health-related quality of life. We consider early childhood education programs to be part of the environmental characteristics domain that can affect health-related quality of life for the child. For example, EHS provides multiple services for the child and parent (e.g., education, nutrition, toothbrushing, and dental health care referrals) that can affect symptoms, functional status, and general health perceptions for the child. Within the environmental characteristics, we are specifically examining the impact of dental health care referrals and the facilitation of dental appointments by EHS. These direct effects on the child and family are supported by an early education and childcare framework proposed by Friedman-Krauss and Barnett (2013).
Variables
The main independent variable, EHS enrollment, was supplied by EHS staff and confirmed by the parent at the baseline enrollment screening and interview. It was treated as a binary variable in the analysis (1 = enrolled in EHS; 0 = not enrolled).
The dependent variable, OHRQoL, was measured using the 13-item Early Childhood Oral Health Impact Scale (ECOHIS), the most frequently used scale for assessing OHRQoL among preschool children and their families (Pahel et al. 2007; Kumar et al. 2014). ECOHIS items queried parents about the frequency of lifetime impacts of child dental problems or treatments on the child and family as 0 = never, 1 = hardly ever, 2 = occasionally, 3 = often, and 4 = very often. The sum score for the 13 items can range from 0 (best) to 52 (worst) OHRQoL. We excluded observations with missing responses to >2 child items or >1 family item (n = 22); otherwise, we performed simple imputation of the average of the remaining items for missing values (baseline, n = 128; follow-up, n = 49).
The specific outcome used in this study was ECOHIS impact, a dichotomous variable defined as having any negative impacts on OHRQoL at follow-up (ECOHIS ≥1 due to any reason at the level of hardly ever/occasionally/often/very often). No convention for defining the prevalence of OHRQoL exists, particularly for assessing OHRQoL in young children. We arbitrarily chose our threshold for prevalence because of the high frequency of “never” responses for all of the ECOHIS items and the potential for greater measurement sensitivity of the ECOHIS scale in detecting any negative impacts to OHRQoL.
We included 2 baseline covariates in the models because of their potential impact on follow-up OHRQoL: baseline ECOHIS score and survey language. The Spanish-language version of ECOHIS has not been as widely used and tested for its psychometric properties as the English version, but its construct validity and internal consistency were demonstrated (Talekar et al. 2005). A cross-sectional analysis of baseline interviews in the ZOE study found that Spanish-speaking parents reported a lower severity of ECOHIS impacts (Born et al. 2016). Because of differences between the Spanish- and English-speaking families in the baseline scores, we included interview language (Spanish or English) as a covariate.
The potential mediator, dental use of any type, was also a binary variable defined as a positive response from the parent to “Has your child ever been to a dentist or dental clinic?” at follow-up.
Analytical Approach
We used descriptive statistics to explore the distribution of the children’s demographic characteristics by EHS enrollment and describe the distribution of the overall ECOHIS scores by EHS group. We used an as-assigned “intent-to-treat” analysis of EHS because it is more generalizable and estimates the impact of EHS policies as implemented.
We tested whether dental use mediated the relationship between EHS and OHRQoL using causal mediation analysis (Imai, Keele, and Tingley 2010; Glymour and Spiegelman 2017). In particular, this approach described below required fitting 2 logistic random-effects models: 1) for the mediator, dental use, as a function of the treatment and covariates, and 2) for the outcome, any negative impact of OHRQoL, as a function of the treatment, mediator, and covariates. This approach was chosen because it is not limited to a particular statistical model and, therefore, is applicable to a wide range of situations (Imai, Keele, and Tingley 2010). In our study, it allowed for the analysis of dental use as a mediator while accounting for covariates and random effects.
Regression models
In both the aforementioned models, we controlled for clustering of subjects within EHS programs (n = 25) using random effects and estimated the effect of EHS on the respective outcome. We also controlled for baseline negative impact on OHRQoL, survey language (Spanish, English), and a generalized boosted model propensity score covariate (Burgette et al. 2016). We used logistic regression with random effects to examine the effect of the binary independent variable, EHS, on the respective outcomes. Specifically,
where πij is the probability of the outcome at follow-up for the jth child in the ith EHS program cluster conditional on the cluster-specific effect, bi. In particular, bi is a normally distributed random effect for each EHS program cluster (n = 25) where bi ~ N(0, σ12). Model equation (1) includes the following independent variables:
x1i = EHS enrollment (treatment indicator, dichotomous)
x2ij = any negative impact to OHRQoL (ECOHIS ≥1) at baseline (dichotomous)
x3ij = survey language (dichotomous: Spanish, English)
x4ij = generalized boosted model propensity score (continuous)
In the first model based on equation (1) that had the mediator as the outcome, we estimated the EHS cluster-specific odds ratio, eβ1, as the odds of having any dental use by a child in EHS relative to the odds for a child not in EHS, which, due to the random effect, is conditional on the EHS and non-EHS child being from the same geographic area. In the second model, we estimated the EHS cluster-specific odds ratio, eβ1, as the odds of having any negative impact to OHRQoL (ECOHIS ≥1) by a child in EHS relative to the odds for a child not in EHS while also adjusting for any dental use as a covariate.
Mediation test for dental use
Causal mediation analysis uses the counterfactual framework of causal inference (Tingley et al. 2014; Glymour and Spiegelman 2017). In this framework, each individual has 4 possibilities for the outcome (OHRQoL) and the mediator (dental use): A) outcome and mediator as if in the EHS group; B) outcome as if in the EHS group, mediator as if in the non-EHS group; C) outcome as if in the non-EHS group, mediator as if in the EHS group; and D) outcome and mediator as if in the non-EHS group. Of these 4 potential outcomes, we observe only 1 for each person in the data set.
The mediation effect was measured using 3 parameters: average indirect effect, average direct effect, and total effect (Imai, Keele, and Tingley 2010; Tingley et al. 2014). The average indirect effect, also known as the average causal mediation effect, is the effect of the treatment (EHS) on the outcome (OHRQoL) through the mediating variable (overall dental use) (Robins and Greenland 1992). Using the above 4 potential outcomes, the average indirect effect is A minus B or C minus D, averaged over the sample of interest.
The average direct effect is the effect of the treatment (EHS) on the outcome (OHRQoL) while holding the mediator (overall dental use) constant at the level that would be realized under one fixed treatment status (EHS or non-EHS). Using the above 4 potential outcomes, the direct effect is A minus C or B minus D.
The total effect is the sum of the average indirect and average direct effects (Imai, Keele, and Tingley 2010). Using the above 4 potential outcomes, the total effect is A minus D, which is any negative impact to OHRQoL to individuals in the EHS group if they had their dental use in the EHS group minus any negative impact to OHRQoL to individuals in the non-EHS group if they had their dental use in the non-EHS group.
To estimate the causal effects described above, we employed an algorithm that used the results from the 2 regression models to combine the “prediction[s] of the mediator values under different treatment regimens [based on model (1)] as well as the prediction of the different outcome values under different treatment and mediator values [based on model (2)]” (Imai, Keele, Tingley, and Yamamoto 2010, p. 133). We used the R package called “mediation” version 4.4.5 (Tingley et al. 2014) and, in particular, its implementation of an algorithm for the causal mediation analysis of multilevel data. This software is freely available at the Comprehensive R Archive Network and has been used for mediation analyses (Bergh et al. 2015; Serrano-Pozo et al. 2015; Yao et al. 2015). Confidence intervals for the indirect, direct, and total effects were obtained using bootstrap resampling with 1,000 replications.
Results
The study enrolled 1,567 child-parent dyads, an estimated 60% of the eligible EHS sample and 9% of the non-EHS comparison sample. Follow-up interviews were completed with 468 parent-child dyads from EHS programs and 688 parent-child dyads not enrolled in EHS. Baseline characteristics of the EHS and non-EHS children were similar with respect to age, sex, enrollment in public health insurance, and physical, learning, or mental health limitations; however, significantly (P < 0.05) more children in EHS had been homeless and were minority race and ethnicity compared with children not enrolled in EHS (Table 1). On average, children in EHS also had more children in the household and fewer adults in the household compared with non-EHS children (Table 1).
Table 1.
Baseline Child Characteristics of the Zero Out Early Childhood Caries Study Population, by EHS and Non-EHS Groups.
| Characteristic | EHS (n = 468) | Non-EHS (n = 688) | P Valuea |
|---|---|---|---|
| Age, mean, SD (range), mo | 10.6, 4.8 (0–19) | 10.4, 4.6 (1–19) | 0.351 |
| Sex, % | 0.226 | ||
| Male | 54.17 | 50.4 | |
| Female | 45.9 | 49.6 | |
| Race and ethnicity, % | <0.001 | ||
| Non-Hispanic white | 17.5 | 36.8 | |
| Non-Hispanic black | 37.8 | 19.5 | |
| Non-Hispanic Native American | 2.4 | 1.2 | |
| Non-Hispanic other, single race/ethnicity | 0.0 | 1.0 | |
| Non-Hispanic other, multiple races/ethnicities | 7.5 | 10.9 | |
| Hispanic | 34.2 | 30.4 | |
| Missing | 0.6 | 0.3 | |
| Language, % | 0.633 | ||
| English | 74.8 | 76.0 | |
| Spanish | 25.2 | 24.0 | |
| Enrolled in public health insurance, % | 0.441 | ||
| Yes | 98.3 | 98.8 | |
| No | 1.7 | 1.2 | |
| Physical, learning, or mental health limitations, % | 0.160 | ||
| Yes | 4.5 | 2.9 | |
| No | 94.9 | 95.8 | |
| Don’t know | 0.6 | 1.3 | |
| Ever been homeless or not had a regular place to live, % | 0.002 | ||
| Yes | 4.7 | 1.6 | |
| No | 95.1 | 98.3 | |
| Don’t know | 0.2 | 0.1 | |
| Number of children in the household under 5 y old, mean, SD (range) | 1.8, 1.0 (1–7) | 1.4, 0.6 (1–5) | <0.001 |
| Number of children in the household between 5 and 17 y old, mean, SD (range) | 1.0, 1.2 (0–5) | 0.7, 1.1 (0–5) | 0.0014 |
| Number of adults in the household over 17 y old, mean, SD (range) | 2.1, 1.0 (0–7) | 2.2, 1.0 (1–9) | 0.0044 |
EHS, early head start; SD, standard deviation. n = number of subjects in stratum. Due to rounding, percentages may not add to exactly 100%.
The P values are for chi-square tests or t tests comparing EHS and non-EHS groups. For the chi-square test, “don’t know” and “missing” values were excluded, and categories were combined if the expected count for a particular cell was less than 5 to satisfy the test’s assumptions.
The causal mediation analysis fit 2 logistic random-effects models: one for the mediator, dental use, and one for the outcome, OHRQoL (Table 2). In the mediator model, there was a significant association between EHS and dental use, controlling for survey language, baseline OHRQoL, and the propensity score (P < 0.001). In the outcomes model, both EHS and the mediator, dental use, had significant associations with OHRQoL, controlling for survey language, baseline OHRQoL, and the propensity score (P < 0.01).
Table 2.
Mediator and Outcome Models Fit Using Generalized Linear Mixed Models in the Causal Mediation Analysis (N = 1,156).
| Model 1 (Mediator Model, Dependent Variable: Any Dental Use)a |
Model 2 (Outcome Model, Dependent Variable: Oral Health–Related Quality of Life)b |
|||||
|---|---|---|---|---|---|---|
| Estimate (SE) | OR (95% CI) | P Value | Estimate (SE) | OR (95% CI) | P Value | |
| Early Head Start | 1.11 (0.18) | 3.04 (2.15–4.29) | <0.001 | −0.44 (0.15) | 0.64 (0.48–0.87) | 0.004 |
| Any dental use | 0.48 (0.18) | 1.62 (1.14–2.30) | 0.008 | |||
| Survey language | −0.61 (0.19) | 0.54 (0.38–0.78) | 0.001 | 0.49 (0.16) | 1.64 (1.21–2.23) | 0.002 |
| Baseline oral health–related quality of lifec | 0.01 (0.02) | 1.01 (0.98–1.04) | 0.65 | 0.07 (0.01) | 1.07 (1.04–1.10) | <0.001 |
| Propensity score | 0.71 (0.44) | 2.04 (0.86–4.86) | 0.11 | 0.13 (0.39) | 1.14 (0.53–2.43) | 0.73 |
| Constant | 0.61 (0.27) | 1.84 (1.09–3.10) | 0.02 | −1.18 (0.26) | 0.31 (0.19–0.51) | <0.001 |
| Random effect standard deviation (intercept)d | 0.62 | 0.55 | ||||
| Random effect standard deviation (slope)e | 0.46 | |||||
CI, confidence interval; OR, odds ratio; SE, standard error.
Model 1 is the logistic random-effects model for the mediator (any dental use) as a function of the treatment (Early Head Start) and covariates (survey language, baseline oral health–related quality of life, propensity score).
Model 2 is the logistic random-effects model for the outcome of any negative impact on follow-up oral health–related quality of life as a function of the treatment (Early Head Start), mediator (any dental use), and covariates (survey language, baseline oral health–related quality of life, propensity score).
Oral health–related quality of life (OHRQoL) was measured using the Early Childhood Oral Health Impact Scale (ECOHIS), which is a 0 to 52 continuous variable with a higher score indicating worse OHRQoL and a score of 0 indicating no negative impact to OHRQoL. Therefore, any negative impact to OHRQoL is an ECOHIS score ≥1.
Both the mediator (model 1) and outcomes (model 2) models included random effects for each of the 25 Early Head Start program clusters.
The outcomes model (model 2) included random slopes for any dental visit, similar to the example provided in section 4.1 by Tingley et al. (2014).
Dental Use as Mediator of EHS Effect on Any Negative Impact to OHRQoL
The outcome (ECOHIS ≥1 at follow-up) used in the mediator analysis is binary, so all estimated effects are expressed as the increase in probability that the adult study participant reported any negative impact on OHRQoL. The estimated total effect was −0.075 (95% confidence interval [CI], −0.139 to −0.012). Thus, on average, the probability of any negative impact to OHRQoL is approximately 8 percentage points lower if the individual were moved from the non-EHS group to the EHS group (Table 3, Fig.).
Table 3.
Causal Mediation Analysis for the Mediating Effect of Any Dental Use in the Association between EHS Enrollment on Any Impact to Follow-up OHRQoLa (N = 1,156).
| Estimate (95% CI) | |
|---|---|
| Total effectb | −0.075* (−0.139, −0.012) |
| Indirect effectc (average across EHS and non-EHS groups) | 0.020* (0.003, 0.039) |
| Non-EHS | 0.020* (0.003, 0.041) |
| EHS | 0.019* (0.002, 0.037) |
| Direct effectd (average across EHS and non-EHS groups) | −0.095** (−0.158, −0.032) |
| Non-EHS | −0.094** (−0.156, −0.032) |
| EHS | −0.096** (−0.159, −0.032) |
The model included random effects for each of the 25 Early Head Start program clusters and adjusted for survey language, baseline oral health–related quality of life (OHRQoL), and the propensity score covariates. CI, confidence interval; EHS, Early Head Start.
OHRQoL was measured using the Early Childhood Oral Health Impact Scale (ECOHIS), which is a 0 to 52 continuous variable with a higher score indicating worse OHRQoL and a score of 0 indicating no negative impact to OHRQoL. Therefore, any negative impact to OHRQoL is an ECOHIS score ≥1.
The total effect is the sum of the indirect effect and the direct effect.
The indirect effect is the effect of the treatment (EHS) on the outcome (follow-up OHRQoL) through the mediating variable (any dental use).
The direct effect is the effect of the treatment (EHS) on the outcome (follow-up OHRQoL) while holding the mediator (any dental use) constant at the level that would be realized under 1 fixed treatment status (EHS or non-EHS).
P < 0.05. **P < 0.01.
Figure.
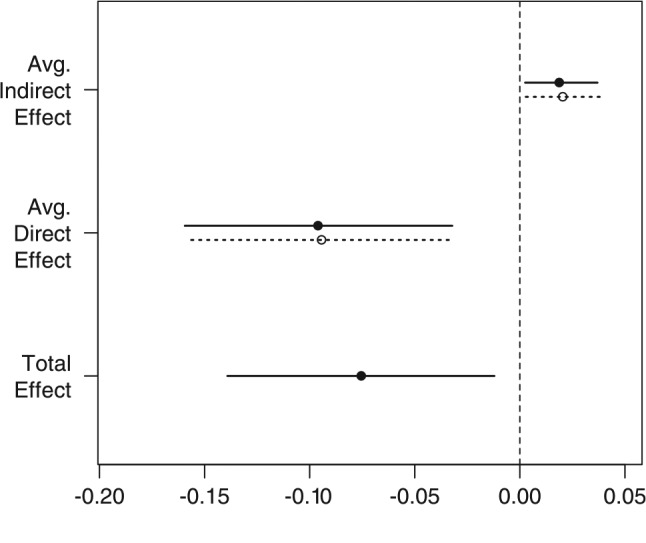
Causal mediation analysis using the average indirect effect, average direct effect, and total tffect. Circles represent estimates. Bars represent 95% CI. Filled circles and solid bars represent the Early Head Start group. Open circles and dashed bars represent the Non–Early Head Start group. Avg., average.
The estimated average indirect effect was 0.020 (95% CI, 0.003–0.039), indicating that, on average, the probability of any negative impact to OHRQoL is 2 percentage points higher if everyone had the dental use they would have received if enrolled in EHS versus not being in EHS, if all other aspects of their treatment assignment were unchanged (Table 3, Fig.). According to the indirect effect averaged within the non-EHS group, individuals in the non-EHS group who are changed only to receive the dental use they would have had if they were in EHS (but receive no other aspects of EHS exposure) would have their probability of any negative impact to OHRQoL increase by 2 percentage points on average (Table 3). The average indirect effect suggests that the increased dental use arising from EHS enrollment has a deleterious impact on OHRQoL.
The estimated average direct effect was −0.095 (95% CI, −0.158 to −0.032), which can be interpreted as follows: on average, the probability of any negative impact to OHRQoL is approximately 10 percentage points lower if the individual were moved from the non-EHS group to the EHS group, while keeping his or her observed dental use fixed (Table 3, Fig.). For the direct effect averaged within the non-EHS group, if an individual’s dental use were held constant at the observed value but the treatment group were changed to EHS in all other respects, then the probability of any negative impact to OHRQoL would be 10 percentage points lower on average (Table 3). The average direct effect suggests that EHS enrollment has a beneficial impact on OHRQoL.
Discussion
Previously, we found that EHS enrollment had positive effects on dental use (Burgette et al. 2017b) and OHRQoL (Burgette et al. 2017a). In the current study, we extend those findings by examining whether dental use mediates the effects of EHS on OHRQoL. We found that dental use, which was improved through EHS participation, mediated some of the EHS intervention effects on OHRQoL but in an unexpected way: dental use made OHRQoL worse. Notably, this indirect effect was not of sufficient magnitude to counterbalance the direct effect of EHS on improved OHRQoL. The overall indirect effect in the mediation analysis showed that dental use was a statistically significant and positive mediator of the effects of EHS on the prevalence of negative OHRQoL impacts.
Most studies on the effects of dental visits on OHRQoL in young children involve the treatment of severe dental disease in a tertiary care center (Jankauskiene and Narbutaite 2010; Almaz et al. 2014; Jankauskiene et al. 2014; Arrow and Klobas 2015; Arrow 2016). These studies generally show improved OHRQoL with dental use. In contrast, a population-based survey of low-income parents of 3-y-old children in 20 North Carolina counties found that treating children with moderate-to-high caries experience measured with decay, missing, and filled (dmf) scores was associated with higher mean ECOHIS scores compared with no treatment (Abraham et al. 2010). Dental visits without any disease treatment also can affect OHRQoL. Nelson and colleagues (2015) found that over a third of parents of children under 3 y old reported that their children experienced severe distress during preventive dental visits consisting of an examination, cleaning, and fluoride treatment.
Qualitative studies provide insights into the possible reasons for our unexpected results by revealing parents’ opinions about the entire dental care experience, not just the dental visit itself. For example, in 1 study, parents reported being misunderstood and unfairly judged for how they balanced their demanding lives with their sincere but frustrating efforts to care for their children’s teeth (Mofidi et al. 2009). In another study, parents described negative experiences when obtaining dental care for their children, such as time spent searching for dental providers who would see Medicaid patients, the availability of limited appointment times aligned with their work schedules, difficulty with transportation, long waiting times on the day of the appointment, and judgmental, disrespectful, and discriminatory behavior because of their race and public assistance status (Mofidi et al. 2002).
Based upon our study results and the literature, we conclude that the effect of dental use on OHRQoL depends on the severity of dental disease, the type of care received during the entire care-seeking experience, and its quality. EHS programs are successful in improving access to dental care but do so only partially (U.S. Department of Health and Human Services 2005; Martin et al. 2012). Enrolled children are more likely to receive preventive oral health services compared with nonenrolled children; however, they still can lack comprehensive treatment of existing disease in a patient-centered dental home. Some characteristics of the pediatric dental home have been outlined (Nowak and Casamassimo 2002), but little is known about how widespread these characteristics might be in dental practice or whether they are causally associated with oral health outcomes, including OHRQoL.
Despite our findings on the role of dental use in mediating the relationship between EHS and OHRQoL, we found improvements in OHRQoL from both direct and total EHS effects (Table 3, Fig.). We tested a single mediator model in our study. However, multiple processes may be responsible for the overall improvement in OHRQoL resulting from EHS enrollment. The additional oral health activities provided in classrooms and other supportive family services provided by EHS likely compensated for the observed effect of use and resulted in an overall positive effect on OHRQoL. Additional research is needed to identify and understand the factors and pathways that contribute to our finding on EHS overall effects on OHRQoL.
Research also is needed to test strategies that might help prevent negative impacts from dental visits. The quality of the dental care experience of young children in EHS should be studied. EHS programs can develop strategies, including acclimation and preparation for in-office dental use targeted to parents of young children to help reduce the negative impacts of dental visits. One example is to add oral health to existing programs such as home-visiting programs that provide medical and psychosocial services during pregnancy and up to 2 years postpartum for first-time mothers who are often young, are unmarried, and have low socioeconomic status (Karoly et al. 2005). Additional interventions could be modeled after childhood health promotion activities, such as vaccination campaigns in which infants and toddlers are expected to experience negative outcomes, like a fever, that can affect their short-term quality of life.
Mediation analysis is growing in popularity as a way to understand causal pathways, particularly as new analytical approaches and tools become available to the scientific community. Some of the newer methods such as the causal mediation analysis framework used in this study have not yet received broad use, even though these new methods resolve some of the shortcomings of older methods (Imai, Keele, and Tingley 2010; Glymour and Spiegelman 2017) such as the classic Baron and Kenny (1986) approach, through an alternative utilization of regression model outputs.
Limitations
We note several limitations of our study. First, we could not randomize families; however, we used a Medicaid-matched control group and propensity scores to reduce the potential for bias. Second, the study was conducted in a single state, which limits generalizability. However, it is important to note that we did not enroll a health care–seeking population; therefore, our study sample likely includes parents who might not have wanted to take their child to the dentist or families who might not value oral health. Third, the equivalence of the English and Spanish ECOHIS scores has not been established for very young children. Future research is needed to establish the comparability between the English and Spanish ECOHIS. Fourth, some health-related quality-of-life scales use thresholds for prevalence other than the one we chose. However, in a previous study, we found no qualitative change in the results when we conducted a sensitivity analysis that set the threshold for prevalence at the level of “occasionally” or more frequently (Burgette et al. 2017a). In addition, future research is needed to determine whether the difference in impacts between the EHS and non-EHS groups is clinically significant. There is a need to define the minimally important difference for oral health impacts in children, particularly to inform the dichotomization of OHRQoL prevalence in future research.
Conclusion
Federally funded social programs, such as EHS, represent an important infrastructure through which socioeconomically vulnerable families can benefit. We found that OHRQoL was negatively affected by one of the successes of the EHS program: increased child dental use. Although the direction of the mediation effect was not as expected, the net prevalence scores for OHRQoL were still improved by EHS enrollment. These results call attention to the effectiveness of improving OHRQoL for low-resource families through comprehensive early childhood education programs. Our findings also suggest the need for future research to reduce the potential for negative impacts of dental use on children from disadvantaged families.
Author Contributions
J.M. Burgette, contributed to conception, data analysis, and interpretation, drafted and critically revised the manuscript; J.S. Preisser, contributed to conception, design, data analysis, and interpretation, critically revised the manuscript; M. Weinberger, contributed to conception, critically revised the manuscript; R.S. King, contributed to conception and data acquisition, critically revised the manuscript; R.G. Rozier, contributed to conception, design, data acquisition, analysis, and interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Footnotes
This research is supported by a grant from the National Institute of Dental and Craniofacial Research, Prevention of Dental Caries in Early Head Start Children, R01 DE018236. This research was partially supported by a National Research Service Award Post-Doctoral Traineeship from the Agency for Health Care Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, T32 HS000032.
The views expressed in the article are those of the authors and do not necessarily reflect the views of the National Institute of Dental and Craniofacial Research or the University of North Carolina at Chapel Hill.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Abanto J, Paiva SM, Sheiham A, Tsakos G, Mendes FM, Cordeschi T, Vidigal EA, Bönecker M. 2016. Changes in preschool children’s OHRQoL after treatment of dental caries: responsiveness of the B-ECOHIS. Int J Paediatr Dent. 26(4):259–265. [DOI] [PubMed] [Google Scholar]
- Abraham J, Rozier R, Pahel B. 2010. Early childhood caries, treatment and oral health–related quality of life. J Dent Res. 89(Spec Iss A):850. [Google Scholar]
- Almaz ME, Sonmez IS, Oba AA, Alp S. 2014. Assessing changes in oral health–related quality of life following dental rehabilitation under general anesthesia. J Clin Pediatr Dent. 38(3):263–267. [PubMed] [Google Scholar]
- American Academy of Pediatric Dentistry. 2013. Policy on the dental home. American Academy of Pediatric Dentistry Reference Manual 2013–2014 [accessed 2017 April 19]. http://www.aapd.org/media/policies_guidelines/p_dentalhome.pdf.
- American Academy of Pediatrics. 2008. Guidelines for health supervision of infants, children, adolescents. In: Holt K., Cassamassimo P, editors. Bright futures in practice: oral health—pocket guide. 3rd ed. Elk Grove Village (IL): American Academy of Pediatrics. [Google Scholar]
- Arrow P. 2016. Responsiveness and sensitivity of the early childhood oral health impact scale to primary dental care for early childhood caries. Community Dent Oral Epidemiol. 44(1):1–10. [DOI] [PubMed] [Google Scholar]
- Arrow P, Klobas E. 2015. Child oral health–related quality of life and early childhood caries: a non-inferiority randomised control trial. Aust Dent J. 61(2):227–235. [DOI] [PubMed] [Google Scholar]
- Barbosa TS, Gavião MB. 2008. Oral health–related quality of life in children: Part II. Effects of clinical oral health status. A systematic review. Int J Dent Hyg. 6(2):100–107. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. 1986. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- Bergh C, Udumyan R, Fall K, Almroth H, Montgomery S. 2015. Stress resilience and physical fitness in adolescence and risk of coronary heart disease in middle age. Heart. 101(8):623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Born CD, Divaris K, Zeldin LP, Rozier RG. 2016. Influences on preschool children’s oral health–related quality of life as reported by English and Spanish-speaking parents and caregivers. J Public Health Dent. 76(4):276–286. [DOI] [PubMed] [Google Scholar]
- Burgette JM, Preisser JS, Weinberger M, King RS, Lee JY, Rozier RG. 2017. a. Enrollment in Early Head Start and oral health–related quality of life. Qual Life Res [epub ahead of print] in press. doi: 10.1007/s11136-017-1584-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgette JM, Preisser JS, Weinberger M, King RS, Lee JY, Rozier RG. 2017. b. The impact of Early Head Start in North Carolina on dental care use among children younger than 3 years. Am J Public Health. 107(4):614–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgette JM, Preisser JS, Rozier RG. 2016. Propensity score weighting: an application to an Early Head Start dental study. J Public Health Dent. 76(1):17–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Early Head Start National Resource Center, Office of Head Start, Administration for Children and Families, U.S. Department of Health and Human Services. 2016. About Early Head Start. Washington (DC): Office of Planning, Research, and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; [accessed 2017 April 19]. http://eclkc.ohs.acf.hhs.gov/hslc/tta-system/ehsnrc/about-ehs/about.html#about. [Google Scholar]
- Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. 2005. Conceptual model of health–related quality of life. J Nurs Scholarsh. 37(4):336–342. [DOI] [PubMed] [Google Scholar]
- Friedman-Krauss A, Barnett WS. 2013. Early childhood education: pathways to better health. New Brunswick (NJ): National Institute for Early Education Research. Policy Brief Issue 25; [accessed 2017 April 19]. https://eric.ed.gov/?id=ED556248. [Google Scholar]
- Glymour MM, Spiegelman D. 2017. Evaluating public health interventions: 5. Causal inference in public health research—do sex, race, and biological factors cause health outcomes? Am J Public Health. 107(1):81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head Start Bureau, Administration on Children, Youth and Families, U.S. Department of Health and Human Services. 2016. Oral health—revision ACF-PI-HS-06-03. Washington (DC): Office of Planning, Research, and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; [accessed 2017 April 19]. http://eclkc.ohs.acf.hhs.gov/hslc/standards/PIs/2006/resour_pri_00109_122006.html. [Google Scholar]
- Imai K, Keele L, Tingley D. 2010. A general approach to causal mediation analysis. Psychol Methods. 15(4):309–334. [DOI] [PubMed] [Google Scholar]
- Imai K, Keele L, Tingley D, Yamamoto T. 2010. Causal mediation analysis using R. In: Vinod HD, editor. Advances in social science research using R. New York (NY): Springer (Lecture Notes in Statistics) p. 129–154. [Google Scholar]
- Jankauskiene B, Narbutaite J. 2010. Changes in oral health–related quality of life among children following dental treatment under general anaesthesia: a systematic review. Stomatologija. 12(2):60–64. [PubMed] [Google Scholar]
- Jankauskiene B, Virtanen JI, Kubilius R, Narbutaite J. 2014. Oral health–related quality of life after dental general anaesthesia treatment among children: a follow-up study. BMC Oral Health. 14:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karoly L, Kilburn M, Cannon J. 2005. Early childhood interventions: proven results, future promise. Santa Monica (CA): RAND Corporation. [Google Scholar]
- Kramer PF, Feldens CA, Ferreira SH, Bervian J, Rodrigues PH, Peres MA. 2013. Exploring the impact of oral diseases and disorders on quality of life of preschool children. Community Dent Oral Epidemiol. 41(4):327–335. [DOI] [PubMed] [Google Scholar]
- Kumar S, Kroon J, Lalloo R. 2014. A systematic review of the impact of parental socio-economic status and home environment characteristics on children’s oral health related quality of life. Health Qual Life Outcomes. 12:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locker D. 1997. Concepts of oral health, disease and the quality of life. In: Slade GD, editor. Measuring oral health and quality of life. Chapel Hill: University of North Carolina, Dental Ecology. [Google Scholar]
- Locker D, Allen F. 2007. What do measures of ‘oral health–related quality of life’ measure? Community Dent Oral Epidemiol. 35(6):401–411. [DOI] [PubMed] [Google Scholar]
- Martin AB, Hardin JW, Veschusio C, Kirby HA. 2012. Differences in dental service utilization by rural children with and without participation in Head Start. Pediatr Dent. 34(5):107-111. [PubMed] [Google Scholar]
- Mofidi M, Rozier RG, King RS. 2002. Problems with access to dental care for Medicaid-insured children: what caregivers think. Am J Public Health. 92(1):53-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mofidi M, Zeldin LP, Rozier RG. 2009. Oral health of early head start children: a qualitative study of staff, parents, and pregnant women. Am J Public Health. 99(2):245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TM, Huebner CE, Kim A, Scott JM, Pickrell JE. 2015. Parent-reported distress in children under 3 years old during preventive medical and dental care. Eur Arch Paediatr Dent. 16(3):283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak AJ, Casamassimo PS. 2002. The dental home: a primary care oral health concept. J Am Dent Assoc. 133(1): 93-98. [DOI] [PubMed] [Google Scholar]
- Onoriobe U, Rozier RG, Cantrell J, King RS. 2014. Effects of enamel fluorosis and dental caries on quality of life. J Dent Res. 93(10):972–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oral Health in America: a report of the Surgeon General. 2000. Rockville (MD): U.S. Department of Health and Human Services. [Google Scholar]
- Pahel BT, Rozier RG, Slade GD. 2007. Parental perceptions of children’s oral health: the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes. 5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins JM, Greenland S. 1992. Identifiability and exchangeability for direct and indirect effects. Epidemiology. 3(2):143–155. [DOI] [PubMed] [Google Scholar]
- Scarpelli AC, Paiva SM, Viegas CM, Carvalho AC, Ferreira FM, Pordeus IA. 2013. Oral health–related quality of life among Brazilian preschool children. Community Dent Oral Epidemiol. 41(4):336–344. [DOI] [PubMed] [Google Scholar]
- Serrano-Pozo A, Qian J, Monsell SE, Betensky RA, Hyman BT. 2015. APOEepsilon2 is associated with milder clinical and pathological Alzheimer disease. Ann Neurol. 77(6):917–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talekar B, Rozier R, Zeldin L. 2005. Spanish version of the early childhood oral health impact scale. J Dent Res. 84(Spec Iss A):2653. [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. 2014. Mediation: R package for causal mediation analysis. J Stat Software. 59(5):1–40. [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children and Families. 2005. Head Start impact study: first year findings. Washington (DC): Office of Planning, Research, and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services. [Google Scholar]
- Wong HM, McGrath CP, King NM, Lo EC. 2011. Oral health–related quality of life in Hong Kong preschool children. Caries Res. 45(4):370–376. [DOI] [PubMed] [Google Scholar]
- Yao C, Chen BH, Joehanes R, Otlu B, Zhang X, Liu C, Huan T, Tastan O, Cupples LA, Meigs JB, et al. 2015. Integromic analysis of genetic variation and gene expression identifies networks for cardiovascular disease phenotypes. Circulation. 131(6):536–549. [DOI] [PMC free article] [PubMed] [Google Scholar]


