Abstract
Objective:
Stroke guideline compliance of rural Canadian prehospital emergency medical services (EMS) care in acute stroke is unknown. In this quality assurance study, we sought to compare rural and urban care by prehospital EMS evaluation/management indicators from patients assessed at an urban Canadian stroke center.
Materials and Methods:
One hundred adult patients were randomly selected from the stroke registry. Patients were transported through Rural EMS bypass protocols or urban EMS protocols (both bypass and direct) to our stroke center between January and December 2013. Patients were excluded if they were first evaluated at any other health center. Prehospital care was assessed using ten indicators for EMS evaluation/management, as recommended by acute stroke guidelines.
Results:
Compliance with acute stroke EMS evaluation/management indicators were statistically similar for both groups, except administrating a prehospital diagnostic tool (rural 31.8 vs. urban 70.3%; P = 0.002). Unlike urban EMS, rural EMS did not routinely document scene time.
Conclusion:
Rural EMS responders’ compliance to prehospital stroke evaluation/management was similar to urban EMS responders. Growth areas for both groups may be with prehospital stroke diagnostic tool utilization, whereas rural EMS responders may also improve with scene time documentation.
KEYWORDS: Emergency medical services, rural health, stroke
INTRODUCTION
The time dependency of intravenous recombinant tissue plasminogen activator for acute ischemic stroke underscores the significance of prehospital delays and missed or delayed treatment windows. Efficient emergency medical services (EMS) systems have great potential in mitigating these delays by optimizing management from the onset of 9-1-1 activation to stroke center assessment.[1] Stroke guidelines have identified prehospital transport strategies such as EMS routing as important considerations.[2,3] This involves the direct transport of eligible stroke patients to only designated centers capable of hyperacute diagnoses and management. In some instances, air medical transport and bypassing closer health centers is required.[2] Implementation of these strategies has increased in both the US and Canada.[3,4,5]
Bypass protocols are also used for jurisdictions with large rural and remote communities. Such protocols have mitigated geography as a barrier for access to acute stroke management.[6,7] Physicians are often not involved in early bedside evaluations and management, and these responsibilities are placed on rural EMS. However, when compared to their urban counterparts,[8] rural EMS may be volunteers,[9] have less education,[10] have less training,[11] and fewer learning opportunities to maintain competency.[12] These may be important factors since an acute stroke in rural areas may be even more prevalent and carry a higher mortality than urban areas in developed countries.[13]
At present, whether rural Canadian prehospital EMS patient care is in compliance with best practice in acute stroke is unknown. Both American Heart Association/American Stroke Association (AHA/ASA) guidelines and Canadian stroke best practice recommendations discuss multiple prehospital EMS evaluation/management indicators that are later described. To identify potential growth areas in prehospital EMS care of acute stroke patients, we sought to use these indicators to compare rural responders on bypass protocol versus urban responders en route to a stroke center in Winnipeg, Canada.
MATERIALS AND METHODS
Study design
This retrospective chart audit examined acute stroke patients who presented according to “stroke protocol” and were evaluated by the Health Sciences Centre's (HSCs) neurology service in Winnipeg, Canada, between January and December 2013. The University of Manitoba granted ethical approval.
Setting
Patients with suspected acute stroke are assessed at the HSC if they are either picked up by urban EMS within the city of Winnipeg's HSC catchment area (approximate population of 350 000) or a northern rural catchment area that can accommodate predicted stroke center arrival <3.5 h of symptom onset. This equates to an approximate 150 km concentric and 70 000 people. Rural bypass protocols have been developed for patients demonstrating at least one sign on the Cincinnati Prehospital Stroke Scale (CPSS),[14] and ≥18 years of age. This may involve bypassing smaller urban centers not designated as stroke centers. Contraindications to bypass include unstable patients or unsuitable candidates for thrombolytics. Rural EMS responders within the concentric have a wide variation in training and expertise, generally ranging from emergency medical responders to unlicensed intermediate care paramedics.[15] Urban EMS responders are typically licensed as primary or advanced care paramedics.[15]
Selection of participants
One hundred patients were selected from our registry through computer-generated stratified random sampling to mirror our actual 75%–25% urban to rural acute stroke distribution pattern. Patients were included in this study if they were (a) ≥18 years of age; (b) transported through rural EMS bypass protocols or urban EMS protocols (both bypass and direct), and; (c) alive at the time of stroke center assessment. Patients were excluded if they were evaluated at any health center before stroke center assessment, as this may have altered EMS management. As variability of acute stroke practice in rural EMS has not been reported, 10 cases per measured outcome directed our quality assurance sample size.[16]
Outcome measures
Reviewed charts were coalesced from EMS records and stroke center entries. Data collected by a single nonblinded extractor included age, sex, and final diagnosis. All AHA/ASA prehospital EMS stroke evaluation and management recommendations were included: (1) Airway - Breathing-Circulation (ABCs) assessment and management; (2) utilization of a standardized out of hospital acute stroke screening tool; (3) recording the time of symptom onset; (4) continuous cardiac monitoring; (5) supplemental oxygen to maintain saturations >94%; (6) establishment of IV access; (7) determination of blood glucose; (8) brief history including comorbid conditions and current medications; (9) scene time; and (10) hospital prenotification of pending patient arrival.[2] Utilization of a stroke tool was evident on urban EMS computer charting by the hardcopy printout of a CPSS drop box, whereby rural paper charting required documentation of either the completed CPSS or facial droop, arm drift, and speech symptomology.
Analysis
The primary outcome was the proportion of prehospital EMS evaluation/management recommendations and indicators documented by EMS in suspected acute adult stroke patients. Proportions between groups were compared by a two-tailed Fischer's exact test. Statistical significance was considered as 0.05.
RESULTS
Of our 100 randomly selected charts, data were complied from 74 urban and 22 rural patients. Four charts were void of prehospital EMS documentation and thus were not included in the final analysis.
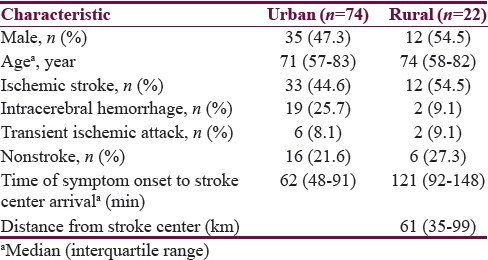
Patient characteristics were reported for both urban and rural EMS responders [Table 1], including male gender (47.3 vs. 54.5%), median age (71.0 vs. 74.0), and final diagnosis of acute stroke or transient ischemic attack (78.4 vs. 72.7%). The median distance of rural EMS transport was 61 km (interquartile range 35–99).
Table 1.
Patient characteristics, by emergency medical services responder
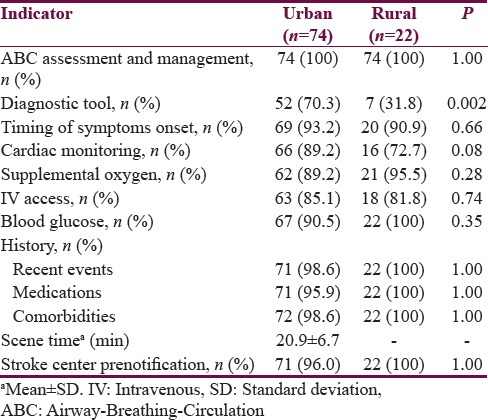
Compliance was over 80% in all acute stroke prehospital EMS evaluation/management indicators for both responders, with the exception of cardiac monitoring and administration of the CPSS [Table 2]. The only statistically significant difference between urban and rural EMS responders was in the administration of the CPSS (70.3 vs. 31.8%; P = 0.002). Rural EMS scene time was not routinely documented, whereas mean urban EMS scene time was 20.9 min (±6.7 min). A correct stroke diagnosis was similar between both groups (78.4 vs. 72.7%; P = 0.57).
Table 2.
Compliance to prehospital evaluation and management indicators, by emergency medical services responder
DISCUSSION
The purpose of this retrospective quality assurance chart audit was to compare acute stroke EMS assessment and management between urban and rural responders. We report similar compliance with best practice for both groups, with the exception of administrating a prehospital diagnostic tool. Unlike urban EMS, rural EMS did not routinely document scene times.
Compliance was over 90% for five indictors for both urban and rural EMS providers, including ABC assessment and management, determining blood glucose, brief history, documenting the timing of symptoms onset and stroke center prenotification. Comparatively, a recent US EMS urban study identified symptoms onset timing and prenotification as two key prehospital metrics, but a compliance of 68.3 and 56.5%, respectively, was reported.[17] Although not statistically significant, suboptimal cardiac monitoring was observed in our rural EMS cohort (72.7 vs. 89.2%). Our reported high compliance rates may be attributable to several related factors. First, both urban and rural EMS responders have developed similar acute stroke protocols and prehospital algorithms with our stroke center. Second, urban responders also utilize an embedded branching logic algorithm within their computer charting that may facilitate compliance through preprogrammed drop box prompting. Third, early communication with the stroke center neurologist also ensued if a patient was identified as a potential candidate for thrombolytics, allowing for prompt medical council and prenotification. Finally, prehospital management of acute stroke has become a regional training priority with regular quality assurance surveillance audits.
We observed a significantly higher reported administration of the CPSS in urban EMS responders (70.3 vs. 31.8%; P = 0.002). Both these values are suboptimal, but given that the discharge diagnosis of acute stroke was nearly 75% in both cohorts, other factors may have aided prehospital diagnoses. First, it may reflect accurate dispatch stroke diagnoses that increase the clinical index of stroke suspicion. However, unidentified stroke patients often have ambiguous dispatch diagnoses such as “fall” or “lying down,” reinforcing the need for clinical examination and patient differentiation.[18] Second, both responder groups utilized the CPSS, but its actual administration might not have been documented on the EMS records. Finally, a high stroke center prenotification rate might indicate that a patient with a queried acute stroke diagnosis was reviewed with the stroke center's neurologist. Given the imperfect diagnostic capabilities of the CPSS, a brief telephone review with a neurologist may have improved diagnostic precision.[19]
Rapid triage and transport of suspected acute stroke patients are critical components of prehospital time indicators.[2,3] Urban EMS responders demonstrated a scene time just over 20 min, with an average dispatch to the stroke center arrival time of 39.2 min. Rural EMS responders did not routinely document scene time, making comparisons and quality assurance very difficult. Although their paper charting may be inferior and more time consuming than computerized modalities, the importance of documenting scene times cannot be overstated. While their median time of symptom onset to stroke center arrival (121 min) was well within the treatment window, time is the brain, and every minute gained spares millions of neurons.[20]
Our study's main limitation is the assumption that charting was analogous to actual practice. Although we acknowledged this potential discrepancy in the discussion of CPSS utilization, under-reporting of actual practice is a plausible scenario with other prehospital indicators studied. Second, compliance with prehospital evaluation/management indicators might not directly equate with enhanced patient care. While prehospital care is complex, our variables nevertheless were based on AHA/ASA guidelines identifying the critical aspects of acute stroke care. Finally, although a sample size of 100 may be useful to identify potential growth areas of prehospital acute stroke care, larger studies would be necessary to confirm our results.
CONCLUSION
Despite lower acute stroke volume and generally lower certification, rural EMS responders’ compliance to prehospital evaluation\management guidelines was similar to urban EMS responders. Growth areas for both groups may be enhancing their CPSS utilization, while rural EMS responders may also improve with scene time documentation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fassbender K, Balucani C, Walter S, Levine SR, Haass A, Grotta J. Streamlining of prehospital stroke management: The golden hour. Lancet Neurol. 2013;12:585–96. doi: 10.1016/S1474-4422(13)70100-5. [DOI] [PubMed] [Google Scholar]
- 2.Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 3.Casaubon LK, Boulanger JM, Glasser E, Blacquiere D, Boucher S, Brown K, et al. Canadian stroke best practice recommendations: Hyperacute stroke care guidelines, update 2015. Int J Stroke. 2016;11:239–52. doi: 10.1177/1747493015622461. [DOI] [PubMed] [Google Scholar]
- 4.Song S, Saver J. Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke. 2012;43:1975–8. doi: 10.1161/STROKEAHA.112.657809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanks N, Wen G, He S, Song S, Saver JL, Cen S, et al. Expansion of U.S. emergency medical service routing for stroke care: 2000-2010. West J Emerg Med. 2014;15:499–503. doi: 10.5811/westjem.2014.2.20388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riopelle RJ, Howse DC, Bolton C, Elson S, Groll DL, Holtom D, et al. Regional access to acute ischemic stroke intervention. Stroke. 2001;32:652–5. doi: 10.1161/01.str.32.3.652. [DOI] [PubMed] [Google Scholar]
- 7.Sanossian N, Liebeskind DS, Eckstein M, Starkman S, Stratton S, Pratt FD, et al. Routing ambulances to designated centers increases access to stroke center care and enrollment in prehospital research. Stroke. 2015;46:2886–90. doi: 10.1161/STROKEAHA.115.010264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leira EC, Hess DC, Torner JC, Adams HP., Jr Rural-urban differences in acute stroke management practices: A modifiable disparity. Arch Neurol. 2008;65:887–91. doi: 10.1001/archneur.65.7.887. [DOI] [PubMed] [Google Scholar]
- 9.Thompson AM., 3rd Rural emergency medical volunteers and their communities: A demographic comparison. J Community Health. 1993;18:379–92. doi: 10.1007/BF01323968. [DOI] [PubMed] [Google Scholar]
- 10.Chng CL, Collins J, Eaddy S. A comparison of rural and urban Emergency Medical System (EMS) personnel: A Texas study. Prehosp Disaster Med. 2001;16:159–65. doi: 10.1017/s1049023x00025917. [DOI] [PubMed] [Google Scholar]
- 11.Brown LH, Copeland TW, Gough JE, Garrison HG, Dunn KA. EMS knowledge and skills in rural North Carolina: A comparison with the National EMS Education and Practice Blueprint. Prehosp Disaster Med. 1996;11:254–60. doi: 10.1017/s1049023x00043089. [DOI] [PubMed] [Google Scholar]
- 12.Becknell J, Ostrow LS. EMS in rural America. Emerg Med Serv. 2002;31:41. [PubMed] [Google Scholar]
- 13.Joubert J, Prentice LF, Moulin T, Liaw ST, Joubert LB, Preux PM, et al. Stroke in rural areas and small communities. Stroke. 2008;39:1920–8. doi: 10.1161/STROKEAHA.107.501643. [DOI] [PubMed] [Google Scholar]
- 14.Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: Reproducibility and validity. Ann Emerg Med. 1999;33:373–8. doi: 10.1016/s0196-0644(99)70299-4. [DOI] [PubMed] [Google Scholar]
- 15.Toews R. Manitoba EMS System Review: The Government of Manitoba, Minister of Health. [Last cited on 2016 Dec 21]. Available from: https://www.gov.mb.ca/health/documents/ems.pdf .
- 16.Sacket DL, Haynes RB, Guyatt GH, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. Boston, MA: Little, Brown * Company; 1991. [Google Scholar]
- 17.Oostema JA, Nasiri M, Chassee T, Reeves MJ. The quality of prehospital ischemic stroke care: Compliance with guidelines and impact on in-hospital stroke response. J Stroke Cerebrovasc Dis. 2014;23:2773–9. doi: 10.1016/j.jstrokecerebrovasdis.2014.06.030. [DOI] [PubMed] [Google Scholar]
- 18.Berglund A, von Euler M, Schenck-Gustafsson K, Castrén M, Bohm K. Identification of stroke during the emergency call: A descriptive study of callers’ presentation of stroke. BMJ Open. 2015;5:e007661. doi: 10.1136/bmjopen-2015-007661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brandler ES, Sharma M, Sinert RH, Levine SR. Prehospital stroke scales in urban environments: A systematic review. Neurology. 2014;82:2241–9. doi: 10.1212/WNL.0000000000000523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saver JL. Time is brain – Quantified. Stroke. 2006;37:263–6. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]


