Abstract
Background
Anticoagulation is the therapeutic paradigm for stroke prevention in patients with atrial fibrillation (AF). It is unknown how physicians make treatment decisions in primary stroke prevention for patients with AF.
Objectives
To evaluate the association between family physicians’ risk preferences (aversion risk and ambiguity) and therapeutic recommendations (anticoagulation) in the management of AF for primary stroke prevention by applying concepts from behavioral economics.
Methods
Overall, 73 family physicians participated and completed the study. Our study comprised seven simulated case vignettes, three behavioral experiments, and two validated surveys. Behavioral experiments and surveys incorporated an economic framework to determine risk preferences and biases (e.g., ambiguity aversion, willingness to take risks). The primary outcome was making the correct decision of anticoagulation therapy. Secondary outcomes included medical errors in the management of AF for stroke prevention.
Results
Overall, 23.3% (17/73) of the family physicians elected not to escalate the therapy from antiplatelets to anticoagulation when recommended by best practice guidelines. A total of 67.1% of physicians selected the correct therapeutic options in two or more of the three simulated case vignettes. Multivariate analysis showed that aversion to ambiguity was associated with appropriate change to anticoagulation therapy in the management of AF (OR 5.48, 95% CI 1.08–27.85). Physicians’ willingness to take individual risk in multiple domains was associated with lower errors (OR 0.16, 95% CI 0.03–0.86).
Conclusion
Physicians’ aversion to ambiguity and willingness to take risks are associated with appropriate therapeutic decisions in the management of AF for primary stroke prevention. Further large scale studies are needed.
Keywords: atrial fibrillation, decision making, therapeutic decisions, anticoagulants, risk, physicians
Background
The advent of precision medicine promises a paradigm shift to medical practice by improving physicians’ abilities to more accurately prevent, diagnose, and treat medical conditions by factoring in the biological variability of individuals and differences in their environments and lifestyles.1 This “potential”, for precision medicine to improve health and patient outcomes, will likely be realized in the years ahead, however, both in the present and future, physicians will undoubtedly continue to use medical judgments and make treatment decisions by processing information that, by virtue of being human, will employ biases and heuristics.2–4 A systematic review by Blumenthal-Barby and Krieger reported that 34% of studies investigating cognitive biases and heuristics in medical decision making focused on medical professionals; bias and heuristics were confirmed in 80% of these studies, thereby attesting to their prominence within medical decision making.5 There are over 30 types of biases in decision making; the most commonly assessed ones include ambiguity aversion, anchoring, ascertainment bias, default bias, framing, overconfidence, and outcome bias.2 The scientific literature on biases in medical decision making is mainly descriptive, thereby hindering the interpretation of causal inferences.2 In an attempt to alleviate some of the uncertainty, the practice of medicine uses tools for risk stratification of patients and visual aids for the communication of expected outcomes based on the current available evidence.6–8
The management of atrial fibrillation (AF), the most prevalent type of cardiac arrhythmia in adults, highlights the current paradigm of decision making under uncertainty. One of the main complications of AF is stroke.9,10 The risk of stroke that is associated with AF is preventable through the use of antiplatelet agents and anticoagulants, which, once prescribed to a patient with AF, are taken lifelong.9,10 More recently, new oral anticoagulants (NOACs) have been introduced in the market which are similar or more efficacious than the traditional comparator coumadin, and they do not require monthly blood monitoring.11 A recent meta-analysis revealed that NOACs significantly reduced stroke or systemic embolic events by 20% compared with warfarin (relative risk [RR] 0.81, 95% CI 0.73–0.91; P<0.0001), all-cause mortality (RR 0.90, 95% CI 0.85–0.95; P=0.0003), and intracranial hemorrhage (RR 0.48, 95% CI 0.39–0.59; P<0.0001), but increased gastrointestinal bleeding (RR 1.25, 95% CI 1.01–1.55; P=0.04).11 Although funding varies by country and insurance status, the daily cost is approximately US$3. However, there is also a trade-off between the risk of serious complications, like bleeding, and the efficacy of oral anticoagulants.9,11,12
To assist physicians in the management of AF and in guiding the therapeutic strategy, a number of risk assessment scoring systems are available to stratify the risk of stroke in patients with AF; the two commonly used and validated risk scores are CHADS2 and CHA2DS2-Vasc.13–17 The CHA2DS2-Vasc score includes age, sex, history of stroke, hypertension, diabetes, vascular disease, and heart failure or left ventricular dysfunction and provides an annual stroke risk of ~1% for the very low risk and over 9.6% for those with a high risk (score of 7 points or higher).17 Interestingly, a substantial proportion of the population falls in the low risk category (CHA2DS2-Vasc of 0 or 1), where guidelines for treatment vary and the benefits of anticoagulation are less certain.18 Although physicians are trained to quickly recognize critical aspects of particular situations under uncertainty,19 there is little knowledge of how they behave and the decisions they make in circumstances surrounded with unknown probability or uncertainty of outcomes. The current study aims to assess individual risk attitude (aversion to risk and ambiguity) among family physicians and whether there is any influence in their treatment decisions (anticoagulation) and recommendations for stroke prevention.
Methods
Participants
Family physicians from the Greater Toronto Area (GTA), Ontario, Canada, were invited to participate in a single, monitored session to individually complete a paper-based pilot survey. The short, pilot survey included case vignettes, behavioral experiments, and validated surveys from behavioral economics, and collected physician self-reported demographics: age, sex, medical specialty, practice setting, time spent in clinical practice (%), and total years in practice.
The session was conducted in a quiet room and electronic devices were permitted for access to clinical tools routinely used in practice, to mimic the clinic setting as close as possible.
Participants completing the survey provided informed consent to participate in the study. This survey study was approved by the Research Ethics Board of St. Michael’s Hospital, University of Toronto (Toronto, ON, Canada).
Case vignettes
The survey had seven case vignettes involving patients with AF, with three of these case vignettes having one correct response based on the current best practice guidelines;20–22 for each, the CHA2DS2-Vasc scores ranged from 0 to 7 (http://www.mdcalc.com/cha2ds2-vasc-score-for-atrial-fibrillation-stroke-risk/) and the case vignettes outlined common clinical scenarios, phrased from the perspective of stroke prevention at the individual level with a time horizon of 20 years and with the main outcome of interest being number of stroke-free months. The case vignettes were devised and reviewed in a face-to-face meeting of methodologists, statisticians, general practitioners, neurologists, and cardiologists.
Experiments and validated surveys assessing cognitive factors
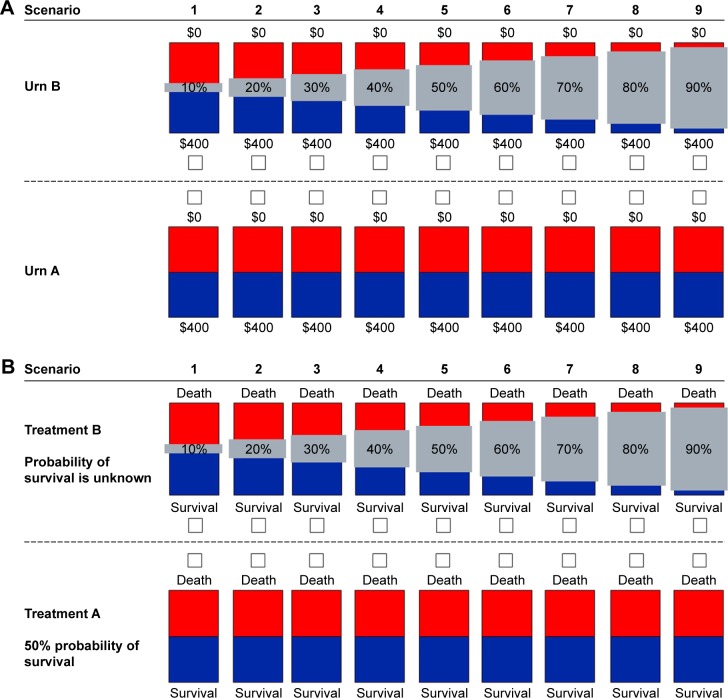
Behavioral experiments were designed to assess ambiguity aversion in the financial and health domains (Figure 1A and B).23–25 Ambiguity aversion is defined as dislike for events with unknown probability over events with known probability.24 For example, an ambiguity-averse individual would rather choose a treatment where the probability of benefits or side effects are known (even if these are some-what unfavorable) over one where these probabilities are unknown. Specifically, physicians were asked to choose between a visual option with known 50/50 probability of winning US$400 or US$0 (Urn A, Figure 1A) versus an option with unknown probability of the same outcomes. Gray bars represented the degree to which the winning probability was unknown (UrnB, Figure 1A). The degree of ambiguity aversion was defined as the proportion of times physicians chose the 50/50 option over the ambiguous option involving the same outcomes. To avoid using an arbitrary criterion, we classified physicians as total ambiguity averse if they chose the 50/50 (known probability) option in each of the nine scenarios (Figure 1A) as we did in previous studies.26,27 A similar visual design and methodology were used to elicit aversion to ambiguity in the health domain (Figure 1B).23 Physicians were asked to choose between “Treatment A” (50% probability of survival) and “Treatment B” (the probability of survival is unknown), with the gray bars quantifying how much is unknown about the probability of survival.
Figure 1.
Aversion to ambiguity in the financial (Panel A) and health (Panel B) domains.
Notes: (A) Representation of the experiment for ambiguity aversion in the financial domain. The amounts are shown in US$. In the administered survey, the family physicians saw the occluders (gray rectangles) without the level (percentage) of uncertainty. Urn A represents a visual option with known 50/50 probability of winning US$400 or US$0. Urn B represents an option with unknown degree of winning probability. (B) Representation of the experiment for ambiguity aversion in the health domain. In this domain also, the family physicians saw the occluders (gray rectangles) without the level of uncertainty in survival.
We also used a standardized survey to assess family physicians’ willingness to take risk in multiple activity-related domains. The German Socio-Economic Panel (SOEP) is a validated survey that evaluates individual willingness to take risk in different domains (financial matters, own health, driving, own occupation, etc.).28 We used questions of the form: “How would you rate your willingness to take risks in the following areas….” Areas included financial matters, driving, occupation, etc., and responses could range from 0 (not at all) to 10 (very much). The six activity domains were summed and dichotomized to low risk attitude (scores of ≤30) and high risk attitude (scores of >30).
Outcome measures
The primary outcome was the proportion of physicians who correctly chose initiating anticoagulation therapy for a 76-year-old man with hypertension who was recently diagnosed with AF (CHA2DS2-Vasc =3) and recommended aspirin in the emergency department.
A secondary outcome included the number of errors in decision of anticoagulation for case vignettes with CHA2DS2-Vasc =3.
Statistical analysis
Descriptive statistics were completed on the physicians’ demographic data, frequency tables tabulated the responses for each case vignette, and a two-sample Student’s t-test was used to compare the demographic characteristics (continuous variables) with cognitive factors. We used median split (above and below the median value) to determine the association between demographic variables (e.g., age) with risk preferences and outcomes of interest. Logistic regression was completed to examine whether there was any relationship between demographic or cognitive factors and the responses provided for each case vignette and the case vignettes on aggregate. All the analyses were completed using Stata (version 13; StataCorp LP, College Station, TX, USA).
Results
The pilot survey was completed within 25 minutes by 73 participants, all of whom were family medicine practitioners (female, n=39; mean age 51.6±11.9 years). The demographics of the participating physicians are summarized in Table 1. Three physicians (4.1%) did not complete all case vignettes.
Table 1.
Demographics of family physicians surveyed
| Demographics | Total n=73 (%) |
|---|---|
| Age | |
| Number of family physicians | 71 |
| Mean ± SD, years | 51.6±11.9 |
| Median (min–max), years | 50 (27–74) |
| <50 years | 36 (50.7%) |
| >51 years | 35 (49.3%) |
| Sex | |
| Number of family physicians | 72 |
| Female | 39 (54.2) |
| Male | 33 (45.8) |
| Practice setting | |
| Number of family physicians | 73 |
| Community | 62 (84.9) |
| Other | 11 (15.1) |
| Percentage of time in clinical practice | |
| Number of family physicians | 73 |
| ≤75% | 19 (26.0) |
| >75% | 54 (74.0) |
| Years in clinical practice | |
| Number of family physicians | 68 |
| Mean ± SD, years | 20.8±14.0 |
| Median (min–max) | 22.5 (0–50) |
Abbreviations: min, minimum; max, maximum.
Overall, 23.3% (17/73) of the family physicians elected not to escalate therapy to anticoagulation when indicated by best practice guidelines (CHA2DS2-Vasc =3). On the other hand, 67.1% of family physicians selected the correct therapeutic options in two or more of the three simulated case vignettes. There was no relationship observed between any of the demographic characteristics of the physicians and the correct selection of treatment in the case vignettes.
Ambiguity aversion
Ambiguity aversion was examined in the: 1) financial domain, where 65.8% of physicians selected the lottery with unknown probability for the range of all nine varying levels of uncertainty (10%–90%), and 2) the health domain, where a larger number of physicians (83.6% [61/73]) than in the financial domain selected the no treatment option for all nine unknown levels of survival (instead of the treatment with known estimates of survival and side effects).
Figure 2 represents the relationship between ambiguity aversion and age, stratified into two age groups (median split): <50 years and >51 years. The overall trend in both the financial and health domains are that the physicians <50 years were more averse to ambiguity than their older counterparts (Figure 2; P<0.008). The multivariate analysis adjusting for demographic data and time in clinical practice revealed that aversion to ambiguity in the financial domain was associated with correctly recommending anti-coagulation for the case vignettes assessing treatment of AF (odds ratio [OR] 5.48, 95% CI 1.08–27.85).
Figure 2.
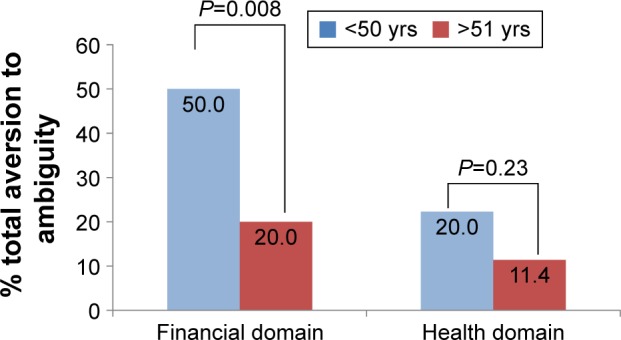
Prevalence of total aversion to ambiguity by age.
Notes: The figure presents ambiguity aversion by respondent age (median split, in years). In the financial domain, physicians were ambiguity averse if they selected all 50/50, and in the health domain, physicians were ambiguity averse if they selected all treatment with known survival of 20 years and 20% side effects instead of the uncertain probability options.
Abbreviation: yrs, years.
Willingness to take risk in multiple domains
The majority of family physicians (75.3% [55/73]) were not willing to take risks and had a cumulative score of ≤30 for all the indicators on risk aversion. Figure 3 shows the percentage of physicians who indicated ≥6 on the linear 10-point scale for each of the domains (where 10= “very much” willing to take risk). The multivariate analysis revealed that physicians indicating willingness to take individual risk in multiple domains (as reflected by the SOEP cumulative score >30) were less likely to make errors in the management of AF (OR 0.16, 95% CI 0.03–0.86).28,29
Figure 3.
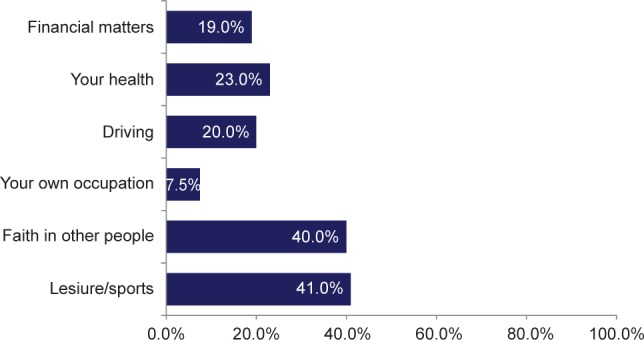
Family physicians’ willingness to take risk in multiple domains (SOEP survey).
Notes: The figure presents the results of the German Socio-Economic Panel (SOEP) indicators of risk aversion. The percentages indicate family physicians willing to take risks based on a rating of ≥6 for each indicator (domain), where 10= “very much” willing to take the risk.
Discussion
In this study we used simulated case vignettes, validated behavioral experiments, and surveys to evaluate the association of family physicians’ risk preferences with treatment decisions for primary stroke prevention in the context of AF. We found that the family physicians with aversion to ambiguity were more likely to correctly recommend anti-coagulation in simulated case vignettes with AF. We also found that total aversion to ambiguity was more common among younger practitioners. Furthermore, willingness to take risk (elicited by the SOEP survey) was associated with a reduction in medical errors.
Medical decisions are a unique paradigm in neuroeconomics and consumer research, given that the decision makers (e.g., physicians) provide recommendations that will affect someone else instead of themselves. This phenomenon, in conjunction with physicians’ biases and risk preferences, has practical implications in the selection of diagnostic and therapeutic options.30
Our findings are in agreement with recent studies. In a study conducted by our group, an association was found between ambiguity aversion in the financial domain and therapeutic inertia in the management of patients with multiple sclerosis by specialists.27 Similarly, Han et al found that younger physicians were more averse to ambiguity.31 This finding may suggest that an increased exposure to medical practice, and gaining experience with treatment decisions under uncertainty, results in lower aversion to ambiguity. Yee et al found that tolerance to ambiguity was associated with optimal management (reflected by lower instrumental vaginal deliveries) and lower medical errors (P<0.006).30 Moreover, the finding that three fourths of the family physicians in our study elected anticoagulants for the patients in the case vignettes is similar to another survey study that found 73% of general practitioners prescribing anticoagulants to hypothetical AF patients, suggesting there is a continued care gap in stroke prevention among general practitioners.32
Recent studies showed that continuing medical education including academic detailing and personalized feedback yielded improvements in prescribing competency (knows how) or performance (shows how).33,34
Limitations
Our study has some limitations that deserve comment: 1) this study should be seen as a pilot study given the small sample size; 2) we used simulated cases which may not truly reflect routine clinical practice; 3) the number of case vignettes is small to address specific questions regarding therapeutic agents in the management of AF; 4) given our aim of maintaining a short study, we have limited information on the physicians’ reasoning process behind treatment decisions. Notwithstanding these limitations, our study applied novel concepts from neuroeconomics to better understand medical decisions in primary care.
In order to make clinical decisions, physicians combine scientific evidence, individual expertise, and a risk-benefit assessment for patients’ overall utility from the potential management and treatment. Established guidelines and validated patient risk assessment tools exist to assist in the process. On the other hand, physicians should be aware that their own risk preferences affect therapeutic decisions. As such, our study constitutes the first step in understanding how cognitive factors (aversion to ambiguity) and personality attributes (willingness to take risk in multiple domains) affect therapeutic decisions in primary care. This is more relevant considering the known knowledge-to-action gaps in the management of AF despite the recent availability of novel therapeutic options (e.g., NOACs).
The next steps include conduction of a larger scale study and identification of other cognitive factors associated with suboptimal decisions and medical errors that, together, may guide the development of educational tools to optimize stroke prevention.
Acknowledgments
We would like to express our thanks and gratitude to Mr. Steve Dempsey, Vice President, Medical Group, Diversified Communications Canada (Markham, ON, Canada), and his team at Diversified Communications Canada for helping to organize and facilitate the survey administration at a Pri-Med Canada conference session (Toronto, ON, Canada), and to the family physicians who participated in the study. We are indebted to Professors Christian Ruff and Philippe Tobler (Department of Economics at the University of Zurich) for the support. This study was sponsored by Boehringer Ingelheim (Canada) Ltd.
Footnotes
Disclosure
None of the authors received personal compensation. Dr. G. Saposnik is supported by the Heart and Stroke Foundation Career Award following an open and peer-reviewed competition. Dr. A. Liuni is an employee of Boehringer Ingelheim (Canada) Ltd. The authors report no other conflicts of interest in this work.
References
- 1.Saposnik G, Johnston SC. Decision making in acute stroke care: learning from neuroeconomics, neuromarketing, and poker players. Stroke. 2014;45:2144–2150. doi: 10.1161/STROKEAHA.114.005462. [DOI] [PubMed] [Google Scholar]
- 2.Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak. 2016;16:138. doi: 10.1186/s12911-016-0377-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mamede S, van Gog T, van den Berge K, van Saase JL, Schmidt HG. Why do doctors make mistakes? A study of the role of salient distracting clinical features. Acad Med. 2014;89:114–120. doi: 10.1097/ACM.0000000000000077. [DOI] [PubMed] [Google Scholar]
- 4.van den Berge K, Mamede S. Cognitive diagnostic error in internal medicine. Eur J Intern Med. 2013;24:525–529. doi: 10.1016/j.ejim.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Blumenthal-Barby JS, Krieger H. Cognitive biases and heuristics in medical decision making: a critical review using a systematic search strategy. Med Decis Making. 2015;35:539–557. doi: 10.1177/0272989X14547740. [DOI] [PubMed] [Google Scholar]
- 6.Hong HJ, Kim YD, Cha MJ, et al. Early neurological outcomes according to chads2 score in stroke patients with non-valvular atrial fibrillation. Eur J Neurol. 2012;19:284–290. doi: 10.1111/j.1468-1331.2011.03518.x. [DOI] [PubMed] [Google Scholar]
- 7.Lip GY, Halperin JL. Improving stroke risk stratification in atrial fibrillation. Am J Med. 2010;123:484–488. doi: 10.1016/j.amjmed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Saposnik G, Joundi RA. Visual aid tool to improve decision making in anticoagulation for stroke prevention. J Stroke Cerebrovasc Dis. 2016;25(10):2380–2385. doi: 10.1016/j.jstrokecerebrovasdis.2016.05.037. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 10.January CT, Wann LS, Alpert JS, et al. 2014 aha/acc/hrs guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the heart rhythm society. Circulation. 2014;130:2071–2104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 11.Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–962. doi: 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 12.Lega JC, Bertoletti L, Gremillet C, et al. Consistency of safety and efficacy of new oral anticoagulants across subgroups of patients with atrial fibrillation. PLoS One. 2014;9:e91398. doi: 10.1371/journal.pone.0091398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cha MJ, Kim YD, Nam HS, Kim J, Lee DH, Heo JH. Stroke mechanism in patients with non-valvular atrial fibrillation according to the chads2 and cha2 ds2-vasc scores. Eur J Neurol. 2012;19:473–479. doi: 10.1111/j.1468-1331.2011.03547.x. [DOI] [PubMed] [Google Scholar]
- 14.Dzeshka MS, Lip GY. Specific risk scores for specific purposes: use cha2ds2-vasc for assessing stroke risk, and use has-bled for assessing bleeding risk in atrial fibrillation. Thromb Res. 2014;134:217–218. doi: 10.1016/j.thromres.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Giralt-Steinhauer E, Cuadrado-Godia E, Ois A, et al. Comparison between chads2 and cha2 ds2-vasc score in a stroke cohort with atrial fibrillation. Eur J Neurol. 2013;20:623–628. doi: 10.1111/j.1468-1331.2012.03807.x. [DOI] [PubMed] [Google Scholar]
- 16.Larsen TB, Lip GY, Skjoth F, Due KM, Overvad K, Hvilsted Rasmussen L. Added predictive ability of the cha2ds2vasc risk score for stroke and death in patients with atrial fibrillation: the prospective danish diet, cancer, and health cohort study. Circ Cardiovasc Qual Outcomes. 2012;5:335–342. doi: 10.1161/CIRCOUTCOMES.111.964023. [DOI] [PubMed] [Google Scholar]
- 17.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 18.Joundi RA, Cipriano LE, Sposato LA, Saposnik G, Stroke Outcomes Research Working Group Ischemic stroke risk in patients with atrial fibrillation and cha2ds2-vasc score of 1: systematic review and meta-analysis. Stroke. 2016;47:1364–1367. doi: 10.1161/STROKEAHA.115.012609. [DOI] [PubMed] [Google Scholar]
- 19.Ye S. Medical decision making and the counting of uncertainty. Circulation. 2014;129:2500–2502. doi: 10.1161/CIRCULATIONAHA.114.010152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson JL, Halperin JL, Albert NM, et al. Management of patients with atrial fibrillation (compilation of 2006 accf/aha/esc and 2011 accf/aha/hrs recommendations): a report of the american college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. 2013;61(18):1935–1944. doi: 10.1016/j.jacc.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 21.January CT, Wann LS, Alpert JS, et al. 2014 aha/acc/hrs guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the heart rhythm society. Circulation. 2014;130:e199–e267. doi: 10.1161/CIR.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verma A, Cairns JA, Mitchell LB, et al. 2014 focused update of the canadian cardiovascular society guidelines for the management of atrial fibrillation. Can J Cardiol. 2014;30:1114–1130. doi: 10.1016/j.cjca.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Saposnik G, Sempere AP, Raptis R, Prefasi D, Selchen D, Maurino J. Decision making under uncertainty, therapeutic inertia, and physicians’ risk preferences in the management of multiple sclerosis (discutir ms) BMC Neurol. 2016;16:58. doi: 10.1186/s12883-016-0577-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levy I, Snell J, Nelson AJ, Rustichini A, Glimcher PW. Neural representation of subjective value under risk and ambiguity. J Neurophysiol. 2010;103:1036–1047. doi: 10.1152/jn.00853.2009. [DOI] [PubMed] [Google Scholar]
- 25.Anderson LR, Mellor JM. Predicting health behaviors with an experimental measure of risk preference. J Health Econ. 2008;27:1260–1274. doi: 10.1016/j.jhealeco.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Binmore KSL, Voorhoeve A. How much ambiguity aversion? Finding indifferences between ellsberg’s risky and ambiguous bets. J Risk Uncertain. 2012;45:215–238. [Google Scholar]
- 27.Saposnik G, Sempere AP, Prefasi D, et al. Decision-making in multiple sclerosis: the role of aversion to ambiguity for therapeutic inertia among neurologists (discutir ms) Front Neurol. 2017;8:65. doi: 10.3389/fneur.2017.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dohmen TFA, Huffman D, Sunde U, Schupp J, Wagner GG. Individual risk attitudes: measurement, determinants, and behavioral consequences. J Eur Econ Assoc. 2011;9:522–550. [Google Scholar]
- 29.Wagner GG, Frick JR, Schupp J. The German Socio-Economic Panel study (SOEP) – scope, evolution and enhancements. JASS. 2007;127(1):139–169. [Google Scholar]
- 30.Yee LM, Liu LY, Grobman WA. The relationship between obstetricians’ cognitive and affective traits and their patients’ delivery outcomes. Am J Obstet Gynecol. 2014;211:692.e691–e696. doi: 10.1016/j.ajog.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Han PK, Schupack D, Daggett S, Holt CT, Strout TD. Temporal changes in tolerance of uncertainty among medical students: insights from an exploratory study. Med Educ Online. 2015;20:28285. doi: 10.3402/meo.v20.28285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frankel DS, Parker SE, Rosenfeld LE, Gorelick PB. Hrs/nsa 2014 survey of atrial fibrillation and stroke: gaps in knowledge and perspective, opportunities for improvement. J Stroke Cerebrovasc Dis. 2015;24:1691–1700. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.026. [DOI] [PubMed] [Google Scholar]
- 33.Kamarudin G, Penm J, Chaar B, Moles R. Educational interventions to improve prescribing competency: a systematic review. BMJ Open. 2013;3:e003291. doi: 10.1136/bmjopen-2013-003291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petre B, Gagnayre R, De Andrade V, Ziegler O, Guillaume M. From therapeutic patient education principles to educative attitude: the perceptions of health care professionals – a pragmatic approach for defining competencies and resources. Patient Prefer Adherence. 2017;11:603–617. doi: 10.2147/PPA.S121892. [DOI] [PMC free article] [PubMed] [Google Scholar]