Abstract
The accuracy of cup position in total hip arthroplasty is essential for a satisfactory result as malpositioning increases the risk of complications including dislocation, high wear rate, loosening, squeaking, edge loading, impingement and ultimately failure.
We studied 166 patients in a single-surgeon-series of matched cohorts of patients who underwent total hip arthroplasties. Four separate groups were identified comprising of the posterior approach +/- navigation and the direct anterior approach +/- navigation.
We found a significant difference between the direct anterior navigated group and the posterior non-navigated group for both anteversions (P < 0.05, confidence interval (CI) -3.86 to -1.73) and inclination (P < 0.05, CI -3.08 to -1.08). Almost, 72% of anterior navigated patients fell within 5o of the navigation software set target cup position of 45o inclination and 20o anteversion and 100% were within 10o. Only 30% of posterior non-navigated were within 5o of both anteversion and inclination and 73% were within 10o.
There was also a significant difference between the direct anterior navigated and non-navigated group with respect to anteversion only (p < 0.05, CI 1.50 to 1.30). There were no other significant differences between approaches +/- navigation.
The direct anterior approach allows ease of access to both anterior-superior iliac spines for navigation and a supine patient allows anteversion and inclination to be measured in the frontal plane. We conclude that the direct anterior approach with navigation improves the accuracy of cup position compared to the conventional posterior approach without navigation.
Keywords: orthopaedic surgery, total hip arthroplasty, total hip replacement, intraoperative navigation, arthroplasty, outcome measures
Introduction
Improper positioning of the acetabular component in total hip arthroplasties (THA) has been shown to increase the dislocation rate [1-6], increase bearing surface wears [7-8], decrease the range of motion [9-10], increase revision rates [11] and contributes to squeaking [12]. Many factors have been described which contribute to accurate cup positioning. There are patient factors including body mass index (BMI) [13], age [14-16], gender [14, 16] and primary diagnosis for total hip arthroplasty (THA) [16-17]. There are surgical factors including the performing surgeon's experience [16, 18], the surgical approach [16, 19-24], the prosthetic components [14, 16, 25-28], the acetabular cup fixation method [17] and the orientation of the acetabular cup [14, 16, 27]. We designed this study to determine if there was a difference in acetabulum orientation when performed via the direct anterior approach (DAA) or the posterior approach (PA) with and without using navigation. We studied 166 patients comparing matched cohorts who underwent THA by the same surgeon at our institution. Four separate groups of patients were identified: Group 1 – PA with navigation; Group 2 – PA without navigation; Group 3 – DAA with navigation; Group 4 – DAA without navigation. Informed consent statement was obtained for this study.
Materials and methods
A standardized statistical computer program developed by the University of Tennessee [29] was used to perform a prospective power calculation of a continuous response variable from cohorts containing the matched patients. Prior data from an unpublished pilot study indicated a sample size of 14 pairs of subjects to reject the null hypothesis that this response difference is zero with probability (power) 0.8. The Type I error probability associated with this test of this null hypothesis is 0.05.
All total hip arthroplasties performed by the senior author (WLW) from January 2004 to February 2013 were analyzed retrospectively. This included 650 PA THAs and 111 DAA. Only 13 of the PA group were navigated and only 21 of the DAA group were without navigation. Due to relatively small numbers in these two groups, the study was divided into two arms. Both arms matched patients according to gender, side, body mass index (BMI) and age. The first arm contained the 13 PA navigated group which was matched to 48 PA without navigation and 33 DAA with navigation (Table 1). The second arm contained the 21 DAA without navigation group which was matched to 26 PA without navigation and 25 DAA with navigation (Table 2).
Table 1. Table representing the demographics of the study's first arm.
| Category | NAV Posterior | NO NAV Posterior | NAV Anterior |
| Sex (Male:Female) | 13 (8:5) | 48 (24:24) | 33 (10:23) |
| Body Mass Index | 30 | 29 | 29 |
| Age | 65 | 70 | 71 |
Table 2. Table representing the demographics of the study's second arm.
| Category | NO NAV Anterior | NO NAV Posterior | NAV Anterior |
| Sex (Male:Female) | 21 (4:17) | 26 (5:21) | 25 (7:18) |
| Body Mass Index | 26 | 26 | 25 |
| Age | 66 | 68 | 68 |
All anteroposterior (AP) hip radiographs were exported or scanned into a validated computer program and the anteversion and inclination were measured.
Results
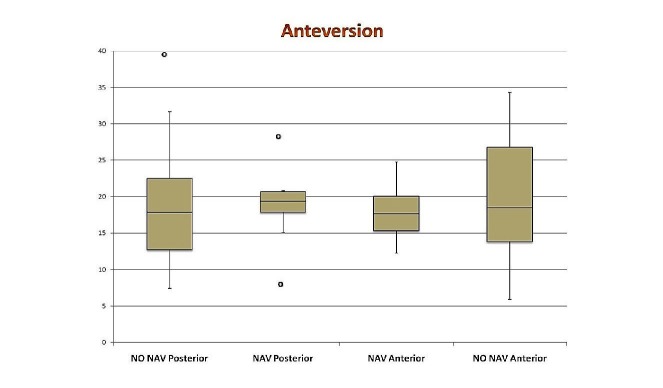
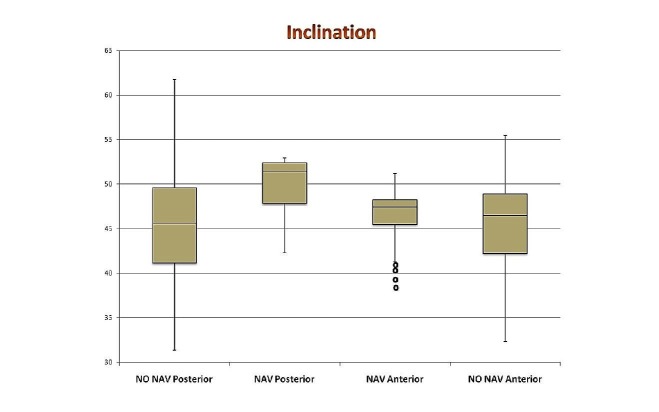
The results of mean anteversion and inclination for all four groups are shown in Table 3, in addition to the absolute difference of these values from a target of 20 degrees anteversion and 45 degrees inclination. Box and whisker plots for all four groups are shown in Figure 1 -2. A two-sample Student’s T-test for two independent means was used to compare cup position within each arm of the study. Consequently, no comparison can be made between PA navigated and DAA without navigation as they were in different arms of the study. We found a significant difference between the DAA navigated group and the PA non-navigated group for both anteversions (P < 0.05, CI -3.86 to -1.73) and inclination (P < 0.05, CI -3.08 to -1.08). Almost 72% of anterior navigated patients fell within 5 degrees of the target cup position of 45 degrees inclination and 20 degrees anteversion and 100% were within 10 degrees. Only 30% of posterior non-navigated were within 5 degrees of both anteversion and inclination and 73% were within 10 degrees.
Table 3. Table representing the cup position for all four groups and absolute difference from the target.
| Category | NAV Posterior | NO NAV Posterior | NAV Anterior | NO NAV Anterior |
| Anteversion | 20o | 18o | 18o | 20o |
| Absolute anteversion difference from 20o | 4o | 6o | 3o | 6o |
| Inclination | 50o | 46o | 47o | 46o |
| Absolute inclination difference from 45o | 5o | 5o | 3o | 5o |
Figure 1. Box and whisker plot showing anteversion (degrees) in all four groups.
Figure 2. Box and whisker plot showing inclination (degrees) in all four groups.
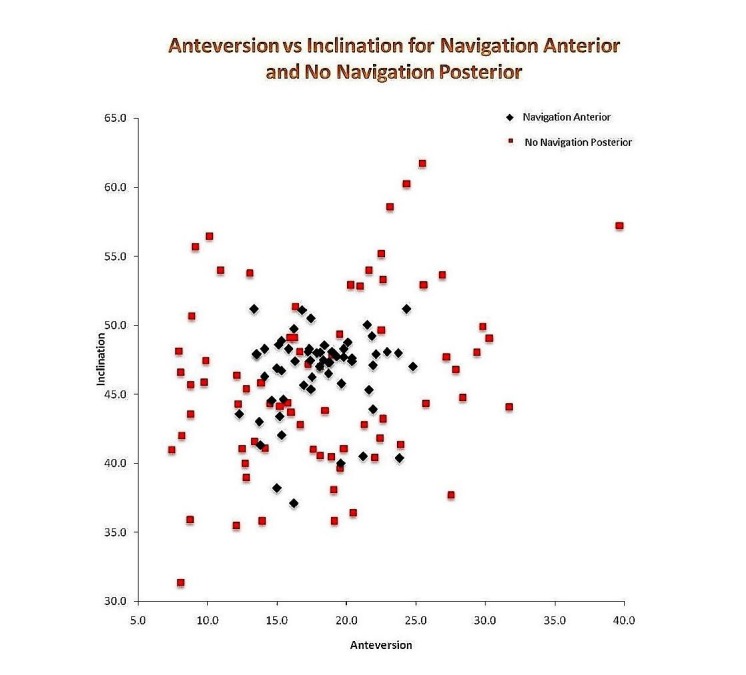
There was also a significant difference between the direct anterior navigated and non-navigated group with respect to anteversion only (p < 0.05, CI 1.50 to 1.30). There were no other significant differences between approaches +/- navigation. The figure 3 shows a scatter plot comparing cup position between DAA navigated group and PA non-navigated group, which highlights the difference in precision.
Figure 3. Scatterplot showing cup position of direct anterior approach (DAA) navigated vs posterior approach (PA) without navigation.
Discussion
This study was designed to gain objective evidence of the accuracy of cup position whilst controlling as many of the variables as possible. All the patients were operated on by the same surgeon and all patients were rigorously matched with respect to gender, side, BMI, and age. The initial hypothesis was that the anterior approach allowed more accurate positioning of the cup for two reasons. Firstly, because it involves surgery in the frontal plane when the patient is supinely allowing an unobstructed view of both anterior superior iliac spines (ASIS) to assess the horizontal plane of the pelvis to reference off for inclination and the coronal plane of the pelvis can be inferred as being parallel to the floor to reference off for anteversion. Secondly, the supine position allows the contralateral ASIS to be prepared and draped allowing intraoperative navigation markers to be sited in a way not possible in a laterally positioned patient for the posterior approach.
There were several limitations to this study including the available numbers of patients in the two groups. The PA navigated and DAA non-navigated groups were small and did not allow for rigorous direct matching between the two groups. Since we could not draw statistical conclusion directly between these two groups, we elected to create two arms with rigorous matching between PA navigated and the two remaining groups (excluding DAA non-navigated) in one arm and the other arm containing DAA non-navigated and the two remaining groups (excluding PA navigated). This did not affect the comparison of PA non-navigated with DAA navigated as these were in the same arm of the study. Another potential limitation was the DAA non-navigated group included some cases in the first 30 DAA procedures that were performed by the senior author and therefore may be affected by the learning curve bias.
Our study showed that the DAA with navigation was significantly more accurate than the PA without navigation. The authors acknowledge that there is no robustly proven ideal position of the acetabular implant and the deviation from the target position of 45 degrees inclination and 20 degrees anteversion is based on the currently available literature and surgeon preference. Analysis of the level of deviation from this target revealed figures for outliers defined here as an absolute difference of greater than 10 degrees from the target position for both inclination and anteversion. Almost 72% of DAA navigated group was accurate within 5 degrees of the target and there were no outliers, compared to 30% of PA non-navigated group within 5 degrees and 27% were outliers.
Conclusions
The direct anterior approach with navigation is more accurate when compared to the non-navigated posterior approach. It allows for improved visualization of the pelvic landmarks and along with the navigation, eliminates outliers and improves the accuracy of acetabular cup placement during total hip arthroplasties. The direct anterior approach with navigation allows for reproducible results and by decrease outliers hopefully, decreases the risk of potential complications related to the malposition of acetabular cups in total hip arthroplasties.
Acknowledgments
The findings of this research have been summarized as an abstract in the Orthopaedic Proceedings Abstract Catalog printed on the 31st of December 2013 as a part of the collective submission following its presentation at the International Society for Technology in Arthroplasty Congress of that same year. No formal journal publications have been published using this data prior to this submission. The abstract is of the same title and can be accessed via http://www.bjjprocs.boneandjoint.org.uk/content/95-B/SUPP_34/195.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Animal Ethics
Animal subjects: This study did not involve animal subjects or tissue.
References
- 1.Instability following total hip arthroplasty. DeWal H, Su E, DiCesare PE. https://www.researchgate.net/profile/Paul_Dicesare/publication/10594281_Instability_following_total_hip_arthroplasty/links/00b4952daf989a40a5000000.pdf. Am J Orthop. 2003;32:377–382. [PubMed] [Google Scholar]
- 2.Factors predisposing to dislocation after primary total hip arthroplasty: A multivariate analysis. Jolles BM, Zangger P, Leyvraz PF. http://www.arthroplastyjournal.org/article/S0883-5403(02)88481-9/fulltext. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 3.Dislocations after total hip-replacement arthroplasties. Lewinnek GE, Lewis JL, Tarr R, et al. https://www.ncbi.nlm.nih.gov/pubmed/641088. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 4.Dislocation after total hip arthroplasty causes, and prevention. McCollum DE, Gray WJ. http://journals.lww.com/corr/Abstract/1990/12000/Dislocation_After_Total_Hip_Arthroplasty_Causes.19.aspx. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 5.The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. Paterno SA, Lachiewicz PF, Kelley SS. https://www.ncbi.nlm.nih.gov/pubmed/?term=The+influence+of+patient-related+factors+and+the+position+of+the+acetabular+component+on+the+rate+of+dislocation+after+total+hip+replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Causes of dislocation of total hip arthroplasty. CT study of component alignment. Pierchon F, Pasquier G, Cotten A, et al. http://www.bjj.boneandjoint.org.uk/content/76-B/1/45. J Bone Joint Surg Br. 1994;76:45–48. [PubMed] [Google Scholar]
- 7.Effects of acetabular abduction on cup wear rates in total hip arthroplasty. Del Schutte H Jr, Lipman AJ, Bannar SM, et al. http://www.arthroplastyjournal.org/article/S0883-5403(98)80003-X/abstract. J Arthroplasty. 1998;13:621–626. doi: 10.1016/s0883-5403(98)80003-x. [DOI] [PubMed] [Google Scholar]
- 8.Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. Kennedy JG, Rogers WB, Soffe KE, et al. http://www.arthroplastyjournal.org/article/S0883-5403(98)90052-3/pdf. J Arthroplasty. 1998;13:530–534. doi: 10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 9.The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. D’Lima DD, Urquhart AG, Buehler KO, et al. https://www.ncbi.nlm.nih.gov/pubmed/10724224. J Bone Joint Surg Am. 2000;82:315–321. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 10.The effect of acetabular cup orientations on limiting hip rotation. Kummer FJ, Shah S, Iyer S, et al. http://www.arthroplastyjournal.org/article/S0883-5403(99)90110-9/pdf. J Arthroplasty. 1999;14:509–513. doi: 10.1016/s0883-5403(99)90110-9. [DOI] [PubMed] [Google Scholar]
- 11.Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. Sugano N, Nishii T, Miki H, et al. http://www.bjj.boneandjoint.org.uk/content/89-B/4/455.full.pdf. J Bone Joint Surg Br. 2007;89:455–460. doi: 10.1302/0301-620X.89B4.18458. [DOI] [PubMed] [Google Scholar]
- 12.A review of squeaking hips. Walter WL, Yeung E, Esposito C. http://journals.lww.com/jaaos/Abstract/2010/06000/A_Review_of_Squeaking_Hips.4.aspx. J Am Acad Orthop Surg. 2010;18:319–326. doi: 10.5435/00124635-201006000-00004. [DOI] [PubMed] [Google Scholar]
- 13.High body mass index is associated with increased risk of implant dislocation following primary total hip replacement:2,106 patients followed for up to 8 years. Azodi SO, Adami J, Lindstrom D, et al. http://www.tandfonline.com/doi/abs/10.1080/17453670710014897. Acta Orthop. 2008;79:141–147. doi: 10.1080/17453670710014897. [DOI] [PubMed] [Google Scholar]
- 14.Difficult complications after hip joint replacement: Dislocation. Morrey BF. http://journals.lww.com/corr/Abstract/1997/11000/Difficult_Complications_After_Hip_Joint.19.aspx. Clin Orthop Relat Res. 1997;344:179–187. [PubMed] [Google Scholar]
- 15.Primary total hip replacement in patients over 80 years of age. Newington DP, Bannister GC, Fordyce M. http://www.bjj.boneandjoint.org.uk/content/72-B/3/450.full.pdf. J Bone Joint Surg Br. 1990;72:450–452. doi: 10.1302/0301-620X.72B3.2341446. [DOI] [PubMed] [Google Scholar]
- 16.Epidemiology of instability after total hip replacement. Sanchez-Sotelo J, Berry DJ. http://www.orthopedic.theclinics.com/article/S0030-5898(05)70225-X/pdf. Orthop Clin North Am. 2001;32:543–552. doi: 10.1016/s0030-5898(05)70225-x. [DOI] [PubMed] [Google Scholar]
- 17.Risk factors for revision for early dislocation in total hip arthroplasty. Conroy JL, Whitehouse SL, Graves SE, et al. http://www.sciencedirect.com/science/article/pii/S0883540307004433. J Arthroplasty. 2008;23:867–872. doi: 10.1016/j.arth.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Poor accuracy of freehand cup positioning during total hip arthroplasty. Bosker BH, Verheyen CC, Horstmann WG, et al. https://link.springer.com/article/10.1007/s00402-007-0294-y. Arch Orthop Trauma Surg. 2007;127:375–379. doi: 10.1007/s00402-007-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prosthesis survival after total hip arthroplasty—does surgical approach matter? Analysis of 19,304 Charnley and 6,002 exeter primary total hip arthroplasties reported to the Norwegian Arthroplasty Register. Arthursson AJ, Furnes O, Espehaug B, et al. http://www.tandfonline.com/doi/abs/10.1080/17453670710014482. Acta Orthop. 2007;78:719–729. doi: 10.1080/17453670710014482. [DOI] [PubMed] [Google Scholar]
- 20.Instability after total hip arthroplasty. Colwell CWJ. http://journals.lww.com/c-orthopaedicpractice/Abstract/2009/01000/Instability_after_total_hip_arthroplasty.3.aspx Curr Orthop Pract. 2009;20:8–14. [Google Scholar]
- 21.Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Enocson ATJ, Tornkvist H, Lapidus L. http://www.tandfonline.com/doi/abs/10.1080/17453670710014996. Acta Ortho. 2008;79:211–217. doi: 10.1080/17453670710014996. [DOI] [PubMed] [Google Scholar]
- 22.Dislocation after total hip arthroplasty using the anterolateral abductor split approach. Mallory TH, Lombardi AV, Fada RA, et al. http://journals.lww.com/corr/Abstract/1999/01000/Dislocation_After_Total_Hip_Arthroplasty_Using_the.20.aspx. Clin Orthop Relat Res. 1999;358:166–172. [PubMed] [Google Scholar]
- 23.Instability after total hip arthroplasty. Morrey BF. http://europepmc.org/abstract/med/1570136. Orthop Clin North Am. 1992;23:237–248. [PubMed] [Google Scholar]
- 24.The effect of femoral component head size on posterior dislocation of the artificial hip joint. Bartz RL, Noble PC, Kadakia NR, et al. https://www.ncbi.nlm.nih.gov/pubmed/11005521. J Bone Joint Surg Am. 2000;82:1300–1307. doi: 10.2106/00004623-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Wear of polyethylene acetabular components in total hip arthroplasty. An analysis of one hundred and twenty-eight components retrieved at autopsy or revision operations. Jasty M, Goetz DD, Bragdon CR, et al. http://journals.lww.com/jbjsjournal/pages/articleviewer.aspx?year=1997&issue=03000&article=00005&type=Fulltext. J Bone Joint Surg Am. 1997;79:349–358. [PubMed] [Google Scholar]
- 26.Relationship of femoral head and acetabular size to the prevalence of dislocation. Kelley SS, Lachiewicz PF, Hickman JM, et al. http://journals.lww.com/corr/Abstract/1998/10000/Relationship_of_Femoral_Head_and_Acetabular_Size.17.aspx. Clin Orthop Relat Res. 1998;355:163–170. doi: 10.1097/00003086-199810000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Influence of femoral head size on impingement, dislocation and stress distribution in total hip replacement. Kluess D, Martin H, Mittelmeier W, et al. https://www.ncbi.nlm.nih.gov/pubmed/16901743. Med Eng Phys. 2007;29:465–471. doi: 10.1016/j.medengphy.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Larger diameter femoral heads used in conjunction with a highly cross-linked ultra-high molecular weight polyethylene: A new concept. Muratoglu OK, Bragdon CR, O’Connor D, et al. http://www.sciencedirect.com/science/article/pii/S0883540301414811. J Arthroplasty. 2001;16:24–30. doi: 10.1054/arth.2001.28376. [DOI] [PubMed] [Google Scholar]
- 29.Power and sample size calculations: A review and computer program. Dupont WD, Plummer WD. http://www.sciencedirect.com/science/article/pii/019724569090005M. Controlled Clin Trials. 1990;11:116–128. doi: 10.1016/0197-2456(90)90005-m. [DOI] [PubMed] [Google Scholar]