Abstract
Minimally invasive spine surgeries (MISS) are becoming increasingly favored as alternatives to open spine procedures because of the reduced blood loss, postoperative pain, and recovery time. Studies have shown mixed results regarding the efficacy and safety of minimally invasive procedures compared to the traditional, open counterparts. The objectives of this systematic analysis are to compare clinical outcomes between the three MISS and open procedures: (1) laminectomy/discectomy, (2) transforaminal lumbar interbody fusion (TLIF), and (3) posterior lumbar interbody fusion (PLIF). The Cochrane and PubMed databases were queried according to the preferred reporting items for systematic review and meta-analyses (PRISMA) statement. The primary outcome measures included the visual analog scale (VAS), the Oswestry disability index (ODI), and blood loss. A total of 32 studies were included in the analysis. Of the three procedures investigated, only MISS TLIF showed significantly improved VAS for leg pain (p = 0.02), ODI (p = 0.05), and reduced blood loss (p = 0.005). MISS-laminectomy/discectomy, TLIF, and PLIF appear to be similar in terms of postoperative pain and perioperative blood loss. MISS TLIF is perhaps more effective in specific outcome measures and results in less intraoperative blood loss than open TLIF.
Keywords: systematic review, minimally invasive spine surgery, neurosurgery
Introduction and background
In recent years, minimally invasive spine surgery (MISS) has become an increasingly attractive alternative to open spine surgery because of a combination of technological advances and a continued desire to reduce tissue injury, complications, and recovery time through the use of minimal incisions and specialized instruments [1-2]. First introduced in 1997 by Foley and Smith for the microscopic decompression of spinal stenosis, MISS is now being applied to a broad spectrum of pathologies, including, but not limited to, adult spinal deformities, trauma, and malignancies [3-6]. In the surgical treatment of lumbar stenosis and degenerative lumbar spondylolisthesis, MISS procedures, including unilateral laminotomy, bilateral laminectomy for bilateral decompression, and transforaminal lumbar interbody fusion (TLIF) have become popular procedures [4,7,8]. Posterior lumbar interbody fusion (PLIF) is another procedure that can be performed using minimally invasive techniques [9].
Despite the widespread and accepted use of MISS, many surgeons still question their safety compared to their traditional, open counterparts. Three criteria have been put forward to evaluate this point: (1) equal or superior treatment of symptoms; (2) reduction in perioperative tissue trauma, physiologic stress, and disturbance of biomechanics; and (3) reduction in complications, infections, and need for subsequent surgeries [3]. With regard to the first criteria, a review by Skovrlj et al. compared the minimally invasive versus the open procedure for laminectomy, TLIF, and direct lateral interbody fusion (DLIF). The authors reported MISS to be as effective as the analogous open procedures [10]. With respect to the second criteria, MISS procedures have also been shown to decrease injury to the multifidus muscle [2], decrease physiologic stress [11], as well as maintain the biomechanical properties of the spine [12].
Controversy remains, however, regarding the third criteria: perioperative outcomes. While studies addressing this concern are available for a number of these procedures, many are inherently limited in their design as prospective/retrospective cohort studies or national database analyses [13-16]. Recently, however, a number of randomized and nonrandomized clinical trials comparing minimally invasive to open procedures have been published [14-23]. In an effort to more accurately characterize the effectiveness of MISS versus open analogs, we conducted a systematic review looking at the perioperative and postoperative outcomes for three spine procedures: (1) laminectomy/discectomy, (2) TLIF, and (3) PLIF.
Review
Study Inclusion
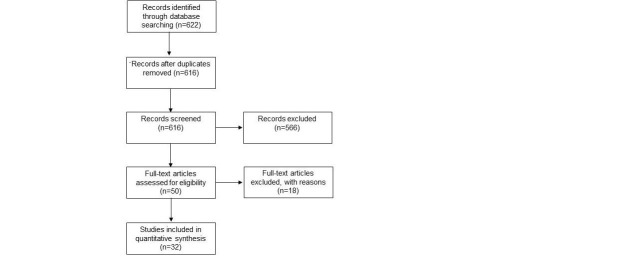
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines were adhered to throughout this study. Our workflow is summarized in Figure 1. This systematic review is registered under the PROSPERO International prospective register of the National Institute for Health Research (CRD42017060375). Institutional review board approval was not required for this study. Electronic searches of the Cochrane Library and PubMed databases were performed by two independent authors (AI and TH) through November of 2016. Strategic search term combinations were utilized and included "minimally invasive" and "spine" and "surgery" and "outcomes." English, full-text clinical studies/trials involving human adults ages 19 and over were included. The title and abstract views were screened for relevance to the topic and duplicate articles were removed. A total of 32 quantitative studies were included in the analysis. Procedures were categorized based on their description in individual studies as open or MISS laminectomy/discectomy, TLIF, or PLIF.
Figure 1. Flowchart According to the PRISMA Statement .
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist was followed for study selection and the 2009 flow diagram is shown.
Outcome Measures
The postoperative values were recorded at the final follow-up for each study, and these included the visual analog scale (VAS) for leg pain and the Oswestry disability index (ODI). VAS scores were scaled across studies to be 0-10 centimeters, to allow for comparison. Estimated intraoperative blood loss was also recorded. We focused on these three outcome measures because they were the most prevalent across the studies analyzed.
Statistical Analysis
Descriptive statistics were ascertained for the included studies. Means and standard deviations were calculated for all outcomes of interest. Paired, parametric t-tests and single factor analyses of variance (ANOVAs) were used to evaluate for significant differences between procedural groups using IBM Statistical Package for the Social Sciences (SPSS), version 23.
Laminectomy/Discectomy
A total of 18 studies were identified involving open and MISS laminectomy/discectomy: 12 analyzed MISS laminectomy/discectomy, 1 analyzed open laminectomy/discectomy, and 5 compared open versus MISS laminectomy/discectomy (Table 1) [15-18,21,24-36]. The mean follow-up time was 20.47; range: 12-40.2 months with an average of 119.44; and range: 8-721 patients. There were no significant differences in terms of VAS for leg pain (mean = 4.56 ± 1.04 vs. 4.58 ± 0.96, p = 0.98); no significant difference in ODI (mean = 31.84 ± 11.30 vs. 17.40 ± 0.57, p = 0.10); and no significant difference in intraoperative blood loss (mean = 70 ± 51 vs. 139 ± 71, p = 0.10; Table 2).
Table 1. Characteristics of Included Studies.
RCT: randomized controlled trial; RC: retrospective cohort; PC: prospective cohort; PELD: percutaneous endoscopic lumbar discectomy; PDD: percutaneous disc decompression; PLDD: percutaneous laser disc decompression; physio: physical therapy; X-STOP: interspinous process decompression system; PEDTA: posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty; PCS: percutaneous cervical discectomy; PCN: percutaneous cervical disc nucleoplasty; PCDN: percutaneous cervical discectomy and nucleoplasty; LDH: lumbar disc herniation; LSS: lumbar spinal stenosis; discogenic lower back pain; cervical disc herniation; sacroiliac joint dysfunction; DS: degenerative spondylolisthesis; IS: isthmic spondylolisthesis; DDD: degenerative disc disease; TJF: thoracolumbar junction fractures; PS: post laminectomy syndrome; CLBP: chronic lower back pain
| Authors & Year | Study Type | Included Cases | Diagnosis | Follow-Up (months) | Technique Used |
| Laminectomy/Discectomy | |||||
| Ying et al., 2006 [24] | RCT | 45 | LDH | 12 | PELD |
| Nikoobakht et al., 2015 [25] | RCT | 177 | LDH | 12 | PDD vs. physio |
| Nerland et al., 2015 [15] | RC | 721 | LSS | 12 | Microdecompression vs. open laminectomy |
| Brouwer et al., 2015 [17] | RCT | 115 | LDH | 12 | PLDD vs. open discectomy |
| Lonne et al., 2015 [26] | RCT | 96 | LSS | 24 | Microdecompression vs. X-STOP |
| Cheng et al., 2014 [27] | PC | 113 | LDH | 36 | PEDTA |
| Mobbs et al., 2014 [18] | RCT | 54 | LSS | 40.2 | MI vs open laminectomy |
| Yang et al., 2014 [28] | RC | 171 | CDH | 40.2 | PCS vs. PCDN vs. both |
| Majeed et al., 2013 [16] | RC | 66 | LDH | 24 | Microdecompression vs. open discectomy |
| Wong et al., 2012 [29] | CS | 17 | LSS | 12 | Mild interlaminar decompression |
| Gerszten et al., 2010 [30] | RCT | 90 | LDH | 12 | PDD vs. epidural corticosteroids |
| Yagi et al., 2009 [21] | RCT | 41 | LSS | 18 | Microdecompression vs. open laminectomy |
| Pao et al., 2009 [31] | PC | 53 | LSS | 16 | Microendoscopic laminotomy |
| Matsumoto et al., 2007 [32] | PC | 36 | LDH | 21 | Microdiscectomy |
| Dewing et al., 2008 [33] | PC | 197 | LDH | 26 | Microdiscectomy |
| Cho et al., 2007 [34] | RCT | 70 | LSS | 15 | Open laminectomy vs. marmot operation |
| Sasaki et al., 2006 [35] | PC | 8 | LSS | 24 | Laminotomy |
| Kim et al., 2007 [36] | RCT | 80 | LSS | 12 | Laminotomy |
| Mean = 119.44; range [8 – 721] | Mean = 20.47; range [12 – 40.2] | ||||
| Transforaminal Lumbar Interbody Fusion | |||||
| Gu et al., 2015 [12] | PC | 74 | SIJD | 32 | MI-TLIF |
| Shen et al., 2014 [37] | RCT | 65 | DDD | 27 | MI-TLIF |
| Nandyala et al., 2014 [38] | RCT | 52 | LSS, DS | 12 | MI-TLIF |
| Perez-Cruet et al., 2014 [39] | PC | 304 | IS, DS, LSS, LDH | 47 | MI-TLIF |
| Choi et al., 2013 [40] | RCT | 53 | DDD | 28 | MI-TLIF |
| Rodriguez-Vela et al., 2013 [41] | PC | 41 | DDD | 45 | open-TLIF |
| Tsahtsarlis et al., 2012 [42] | PC | 34 | DDD | 28 | MI-TLIF |
| Wang et al., 2014 [20] | NRCT | 81 | LSS, DS, IS, PS | 12 | MI vs. open-TLIF |
| Sembrano et al., 2016 [43] | RCT | 55 | DS, LSS | 24 | MI-TLIF |
| Gandhoke et al., 2016 [23] | PC | 74 | DS | 24 | MI vs. open-TLIF |
| Wang et al., 2011 [19] | RCT | 79 | DDD | 24 | MI vs. open-TLIF |
| Mean = 82.91; range [34 – 304] | Mean = 27.54; range [12 – 47] | ||||
| Posterior Lumbar Interbody Fusion | |||||
| Li et al., 2015 [14] | PC | 30 | TJF | 24 | MI vs. open-PLIF |
| Song et al., 2015 [44] | PC | 54 | IS | 27 | Open PLIF |
| Kasis et al., 2009 [22] | PC | 323 | CLBP, DS | 24 | MI vs. open-PLIF |
| Mean = 135.67; range [30 – 323] | Mean = 25; range [24 – 27] |
Table 2. Summary of Analysis Comparing Outcome Measures in Open Versus Minimally Invasive Procedures.
* indicates p-value < 0.05
| Outcome Measures | Minimally Invasive – Laminectomy/Discectomy | Open –Laminectomy/Discectomy | p -value | Minimally Invasive –Transforaminal Lumbar Interbody Fusion | Open – Transforaminal Lumbar Interbody Fusion | p -value | Minimally Invasive – Posterior Lumbar Interbody Fusion | Open – Posterior Lumbar Interbody Fusion |
| VAS for leg pain | 0.98 | 0.02* | ||||||
| Mean | 4.56 | 4.58 | 5.36 | 3.75 | 5.1 | 4 | ||
| SD | 1.04 | 0.96 | 0.85 | 0.74 | 0 | 0.3 | ||
| ODI | 0.10 | 0.05* | ||||||
| Mean | 31.84 | 17.40 | 24.21 | 17.20 | 28.6 | 36.57 | ||
| SD | 11.13 | 0.57 | 5.52 | 5.94 | 0 | 12.76 | ||
| Blood loss | 0.13 | 0.005* | ||||||
| Mean | 70 | 139 | 158 | 452 | 323 | 595 | ||
| SD | 51 | 71 | 77 | 273 | 0 | 93 |
While we found no statistical differences in the three outcome measures of interest between open and MI laminectomy/discectomy, the raw difference seems to be considerable with regards to ODI, yet fails to reach statistical significance (ODI mean = 31.84 ± 11.30 vs. 17.40 ± 0.57, p = 0.10). This is most likely because of a lack of statistical power, as only two studies reported ODI. A recent review by Phan et al. in 2016 showed significantly improved VAS scores and reduced blood loss [45]. Contrastingly, Skovrlj et al. in 2015 reported no significant difference in blood loss between MISS and open laminectomy [10]. Nerland et al. in 2015 and Mobb et al. in 2014 showed equivalence between MISS and open laminectomy ODI scores [15,18]. Further, higher-powered, randomized controlled trials are necessary to determine whether or not MISS laminectomy/discectomy is superior to its open counterpart.
Transforaminal Lumbar Interbody Fusion
A total of 11 studies involving TLIF were identified: 1 analyzed open TLIF, 7 analyzed MISS TLIF, and 2 compared open vs. MISS TLIF [12,19-20,23,37-43]. The mean follow-up time was 27.54; range: 12-47 months on an average with 82.9; and range: 34-304 patients. MISS TLIF had significantly improved VAS scores for leg pain compared to open TLIF (mean = 5.36 ± 0.85 vs. 3.75 ± 0.74, p = 0.02; Table 2). The improvement in ODI was significantly greater in MISS TLIF (mean = 24.21 ± 5.52 vs. 17.20 ± 5.94, p = 0.05). MISS TLIF showed significantly reduced average blood loss compared to open TLIF (mean = 157 ± 77 mL vs. 452 ± 273 mL, p = 0.005).
Our significant findings are consistent with other systematic reviews comparing open and MI TLIF procedures. Goldstein et al. reported significantly reduced blood loss and ODI in the MI TLIF and PLIF procedures [46]. Similarly, Skovrlj et al. also reported significantly reduced blood loss in MISS procedures [10]. TLIF can be approached in several different ways, which include a midline incision with a Taylor retractor (Sklar Instruments, West Chester, PA), the Wiltse approach with and without a tubular retractor, and endoscopic TLIF. Neither of the above reviews nor we in this present study control for these differences, which may account for differences in our findings. Further targeted studies should compare these different approaches.
Posterior Lumbar Interbody Fusion
Three studies were identified analyzing PLIF performed open (one) or comparing MISS versus open techniques (two) [14,22,44]. The mean follow-up time was 25; range: 24-27 months with 135.67; and range: 30-323 patients on an average. Of these three studies, only one of them reported one or more of our three outcome measures of interest, and, consequently, statistical analysis and comparison could not be performed for this group. However, individual studies showed significant improvements in ODI scores and VAS for leg pain, as well as estimated reduced blood loss [14]. Sidhu et al. reported decreased blood loss, shorter hospital stays, and longer operative times in the MI PLIF groups [47]. Li et al. also reported significantly reduced blood loss in the MISS PLIF group. Further randomized trials are needed to determine whether or not MISS PLIF is superior to its open counterpart.
Overall Benefits of Minimally Invasive Spine Surgery
Of the procedures evaluated, only MISS TLIF demonstrated advantages in terms of VAS for leg pain, ODI, and blood loss. Several factors have been postulated behind the benefits of MISS, including smaller portals and reduced muscle stripping, which have been shown to reduce blood loss [19-20]. One study specifically showed significantly improved T2 relaxation time of the multifidus muscle, improved average discharge amplitude, and improved frequency of the sacrospinalis muscle in the MI group [19]. Mobbs et al. showed that patients having undergone MISS consumed significantly less mean total morphine equivalents and fewer patients required opioids after MISS [18]. It is unclear, however, what factors might distinguish TLIF from discectomy and PLIF, whether it be related to procedure or study design. No significant differences in study size (p = 0.73) between all three groups were appreciated.
Limitations
The limitations of this study are inherent to systematic reviews, and we remain cognizant of them. Selection bias was a key obstacle given the range of preoperative outcome measures reported and the baseline differences in the demographics of included studies. Since we were specifically interested in comparing the effectiveness of the open and minimally invasive versions of the three surgeries of interest, we based this analysis on procedure rather than on indication. As a result, our results may have been confounded through heterogeneity among the study populations, specifically in terms of diagnosis and indication for surgery. Specific approach techniques for each procedure were not accounted for due to variation and lack of description in specific studies. Furthermore, different surgeons at different institutions performing the surgeries may have added variability to clinical outcomes. It is unclear whether VAS is comparable from study to study because it is a subjective measure. Oswestry scoring is more standardized and, consequently, presumably more robust. Reported blood loss is highly dependent on surgeons and anesthesia practitioners and, as a result, should be interpreted carefully. Finally, this study only looked at end-point outcome measures, which might have led us to miss any potential early improvement. A plethora of validated quality of life and back pain scores to evaluate recovery exists, but questions remain as to which measures are appropriate when comparing MISS to open spine procedures.
Conclusions
This systematic review suggests that out of laminectomy/discectomy, PLIF, and TLIF, only MI TLIF may be superior to its open analog in terms of VAS score, ODI, and intraoperative blood loss. While individual studies have demonstrated advantages in favor of MISS over traditional techniques, more highly powered, randomized clinical trials are needed to establish MISS techniques as standardized treatment strategies.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Minimally invasive spine surgery. O'Toole JE, Eichholz KM, Fessler RG. Neurosurg Clin N Am. 2006;17:0. doi: 10.1016/j.nec.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Kim CW. http://journals.lww.com/spinejournal/pages/articleviewer.aspx?year=2010&issue=12151&article=00003&type=abstract. Spine. 2010;35:281–286. doi: 10.1097/BRS.0b013e3182022d32. [DOI] [PubMed] [Google Scholar]
- 3.Paradigm changes in spine surgery: evolution of minimally invasive techniques. Smith ZA, Fessler RG. Nat Rev Neurol. 2012;8:443–450. doi: 10.1038/nrneurol.2012.110. [DOI] [PubMed] [Google Scholar]
- 4.Microendoscopic discectomy: surgical technique and initial clinical results. Foley KT, Smith MM. Clin Neurol Neurosurg. 1997;3:301–307. [Google Scholar]
- 5.Minimally invasive treatment of spine trauma. McGowan JE, Ricks CB, Kanter AS. Neurosurg Clin N Am. 2017;28:157–162. doi: 10.1016/j.nec.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Minimally invasive approaches in metastatic spinal tumor surgery. Dalbayrak S, Yaman O, Ozer AF. Turk Neurosurg. 2015;25:357–361. doi: 10.5137/1019-5149.JTN.8990-13.1. [DOI] [PubMed] [Google Scholar]
- 7.Minimally invasive lumbar decompression. Tredway TL. Neurosurg Clin N Am. 2006;17:467–476. doi: 10.1016/j.nec.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Minimally invasive fusion and fixation techniques. Powers CJ, Isaacs RE. Neurosurg Clin N Am. 2006;17:477–489. doi: 10.1016/j.nec.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Posterior lumbar interbody fusion: indications, techniques, and results. McLaughlin MR, Haid RW Jr, Rodts GE Jr, et al. https://www.ncbi.nlm.nih.gov/pubmed/11197722. Clin Neurosurg. 2000;47:514–527. [PubMed] [Google Scholar]
- 10.Perioperative outcomes in minimally invasive lumbar spine surgery: A systematic review. Skovrlj B, Belton P, Zarzour H, et al. World J Orthop. 2015;6:996–1005. doi: 10.5312/wjo.v6.i11.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minimally invasive surgery for traumatic fractures in ankylosing spinal diseases. Nayak NR, Pisapia JM, Abdullah KG, et al. Global Spine J. 2015;5:266–273. doi: 10.1055/s-0034-1397341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clinical and radiological outcomes of unilateral versus bilateral instrumentation in two-level degenerative lumbar diseases. Gu G, Zhang H, Fan G, et al. Eur Spine J. 2015;24:1640–1648. doi: 10.1007/s00586-015-4031-x. [DOI] [PubMed] [Google Scholar]
- 13.Comparative analysis of perioperative surgical site infection after minimally invasive versus open posterior/transforaminal lumbar interbody fusion: analysis of hospital billing and discharge data from 5170 patients. McGirt MJ, Parker SL, Lerner J, et al. J Neurosurg Spine. 2011;14:771–778. doi: 10.3171/2011.1.SPINE10571. [DOI] [PubMed] [Google Scholar]
- 14.Comparison between posterior short-segment instrumentation combined with lateral-approach interbody fusion and traditional wide-open anterior-posterior surgery for the treatment of thoracolumbar fractures. Li X, Zhang J, Tang H, et al. Medicine. 2015;94:1946. doi: 10.1097/MD.0000000000001946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. Nerland US, Jakola AS, Solheim O, et al. BMJ. 2015;350:1603. doi: 10.1136/bmj.h1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comparison of outcomes between conventional lumbar fenestration discectomy and minimally invasive lumbar discectomy: an observational study with a minimum 2-year follow-up. Majeed SA, Vikraman CS, Mathew V, et al. J Orthop Surg Res. 2013;8:34. doi: 10.1186/1749-799X-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Percutaneous laser disc decompression versus conventional microdiscectomy in sciatica: a randomized controlled trial. Brouwer PA, Brand R, van den Akker-van Marle ME, et al. Spine J. 2015;15:857–865. doi: 10.1016/j.spinee.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. Mobbs RJ, Li J, Sivabalan P, et al. J Neurosurg Spine. 2014;21:179–186. doi: 10.3171/2014.4.SPINE13420. [DOI] [PubMed] [Google Scholar]
- 19.Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: a prospective randomized clinical trial. Wang HL, Lu FZ, Jiang JY, et al. https://www.ncbi.nlm.nih.gov/pubmed/22340311. Chin Med J (Engl) 2011;124:3868–3874. [PubMed] [Google Scholar]
- 20.Comparison of the clinical outcome in overweight or obese patients after minimally invasive versus open transforaminal lumbar interbody fusion. Wang J, Zhou Y, Feng Zhang Z, et al. J Spinal Disord Tech. 2014;27:202–206. doi: 10.1097/BSD.0b013e31825d68ac. [DOI] [PubMed] [Google Scholar]
- 21.Postoperative outcome after modified unilateral-approach microendoscopic midline decompression for degenerative spinal stenosis. Yagi M, Okada E, Ninomiya K, et al. J Neurosurg Spine. 2009;10:293–299. doi: 10.3171/2009.1.SPINE08288. [DOI] [PubMed] [Google Scholar]
- 22.Significantly improved outcomes with a less invasive posterior lumbar interbody fusion incorporating total facetectomy. Kasis AG, Marshman LA, Krishna M, et al. Spine. 2009;34:572–577. doi: 10.1097/BRS.0b013e3181973e35. [DOI] [PubMed] [Google Scholar]
- 23.A cost-effectiveness comparison between open transforaminal and minimally invasive lateral lumbar interbody fusions using the incremental cost-effectiveness ratio at 2-year follow-up. Gandhoke GS, Shin HM, Chang YF, et al. Neurosurgery. 2016;78:585–595. doi: 10.1227/NEU.0000000000001196. [DOI] [PubMed] [Google Scholar]
- 24.The effect and feasibility study of transforaminal percutaneous endoscopic lumbar discectomy via superior border of inferior pedicle approach for down-migrated intracanal disc ferniations. Ying J, Huang K, Zhu M, et al. Medicine. 2016;95:2899. doi: 10.1097/MD.0000000000002899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Plasma disc decompression compared to physiotherapy for symptomatic contained lumbar disc herniation: A prospective randomized controlled trial. Nikoobakht M, Yekanineajd MS, Pakpour AH, et al. Neurol Neurochir Pol. 2016;50:24–30. doi: 10.1016/j.pjnns.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Comparing cost-effectiveness of X-stop with minimally invasive decompression in lumbar spinal stenosis: a randomized controlled trial. Lonne G, Johnsen LG, Aas E, et al. Spine. 2015;40:514–520. doi: 10.1097/BRS.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 27.Posterolateral transforaminal selective endoscopic diskectomy with thermal annuloplasty for discogenic low back pain: a prospective observational study. Cheng J, Zheng W, Wang H, et al. Spine. 2014;39:60–65. doi: 10.1097/BRS.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 28.Treatment of cervical disc herniation through percutaneous minimally invasive techniques. Yang B, Xie J, Yin B, et al. Eur Spine J. 2014;23:382–388. doi: 10.1007/s00586-013-3063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mild interlaminar decompression for the treatment of lumbar spinal stenosis: procedure description and case series with 1-year follow-up. Wong WH. Clin J Pain. 2012;28:534–538. doi: 10.1097/AJP.0b013e31823aaa9d. [DOI] [PubMed] [Google Scholar]
- 30.Plasma disc decompression compared with fluoroscopy-guided transforaminal epidural steroid injections for symptomatic contained lumbar disc herniation: a prospective, randomized, controlled trial. Gerszten PC, Smuck M, Rathmell JP, et al. J Neurosurg Spine. 2010;12:357–371. doi: 10.3171/2009.10.SPINE09208. [DOI] [PubMed] [Google Scholar]
- 31.Clinical outcomes of microendoscopic decompressive laminotomy for degenerative lumbar spinal stenosis. Pao JL, Chen WC, Chen PQ. Eur Spine J. 2009;18:672–678. doi: 10.1007/s00586-009-0903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Microendoscopic discectomy for lumbar disc herniation with bony fragment due to apophyseal separation. Matsumoto M, Watanabe K, Tuji T, et al. Minim Invasive Neurosurg. 2007;50:335–339. doi: 10.1055/s-2007-993202. [DOI] [PubMed] [Google Scholar]
- 33.The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Dewing CB, Provencher MT, Riffenburgh RH, et al. Spine. 2008;33:33–38. doi: 10.1097/BRS.0b013e31815e3a42. [DOI] [PubMed] [Google Scholar]
- 34.Split-spinous process laminotomy and discectomy for degenerative lumbar spinal stenosis: a preliminary report. Cho DY, Lin HL, Lee WY, et al. J Neurosurg Spine. 2007;6:229–239. doi: 10.3171/spi.2007.6.3.229. [DOI] [PubMed] [Google Scholar]
- 35.Microscopic bilateral decompression through unilateral laminotomy for lumbar canal stenosis in patients undergoing hemodialysis. Sasaki M, Abekura M, Morris S, et al. J Neurosurg Spine. 2006;5:494–499. doi: 10.3171/spi.2006.5.6.494. [DOI] [PubMed] [Google Scholar]
- 36.Minimally invasive lumbar spinal decompression: a comparative study between bilateral laminotomy and unilateral laminotomy for bilateral decompression. Kim SW, Ju CI, Kim CG, et al. https://www.koreamed.org/SearchBasic.php?DT=1&RID=1032JKNS%2F2007.42.3.195 J Korean Neurosurg Soc. 2007;42:195–199. [Google Scholar]
- 37.Unilateral versus bilateral pedicle screw instrumentation for single-level minimally invasive transforaminal lumbar interbody fusion. Shen X, Zhang H, Gu X, et al. J Clin Neurosci. 2014;21:1612–1616. doi: 10.1016/j.jocn.2013.11.055. [DOI] [PubMed] [Google Scholar]
- 38.Prospective, randomized, controlled trial of silicate-substituted calcium phosphate versus rhBMP-2 in a minimally invasive transforaminal lumbar interbody fusion. Nandyala SV, Marquez-Lara A, Fineberg SJ, et al. Spine. 2014;39:185–191. doi: 10.1097/BRS.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 39.Quality-of-life outcomes with minimally invasive transforaminal lumbar interbody fusion based on long-term analysis of 304 consecutive patients. Perez-Cruet MJ, Hussain NS, White GZ, et al. Spine. 2014;39:191–198. doi: 10.1097/BRS.0000000000000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Unilateral versus bilateral percutaneous pedicle screw fixation in minimally invasive transforaminal lumbar interbody fusion. Choi UY, Park JY, Kim KH, et al. J Neuro Surg. 2013;35:0. doi: 10.3171/2013.2.FOCUS12398. [DOI] [PubMed] [Google Scholar]
- 41.Clinical outcomes of minimally invasive versus open approach for one-level transforaminal lumbar interbody fusion at the 3- to 4-year follow-up. Rodriguez-Vela J, Lobo-Escolar A, Joven E, et al. Eur Spine J. 2013;22:2857–2863. doi: 10.1007/s00586-013-2853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minimally invasive transforaminal lumbar interbody fusion and degenerative lumbar spine disease. Tsahtsarlis A, Wood M. Eur Spine J. 2012;21:2300–2305. doi: 10.1007/s00586-012-2376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Two-year comparative outcomes of MIS lateral and transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: part II: radiographic findings. Sembrano JN, Tohmeh A, Isaacs R, et al. https://www.ncbi.nlm.nih.gov/pubmed/26839992. Spine (Phila Pa 1976) 2016;41:133–144. doi: 10.1097/BRS.0000000000001472. [DOI] [PubMed] [Google Scholar]
- 44.Comparison of posterior lumbar interbody fusion (PLIF) with autogenous bone chips and PLIF with cage for treatment of double-level isthmic spondylolisthesis. Song D, Chen Z, Song D, et al. Clin Neurol Neurosurg. 2015;138:111–116. doi: 10.1016/j.clineuro.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 45.Minimally invasive versus open laminectomy for lumbar stenosis: a systematic review and meta-analysis. Phan K, Mobbs RJ. Spine (Phila Pa 1976) 2016;41:91–100. doi: 10.1097/BRS.0000000000001161. [DOI] [PubMed] [Google Scholar]
- 46.Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. Goldstein CL, Macwan K, Sundararajan K, et al. J Neurosurg Spine. 2016;24:416–427. doi: 10.3171/2015.2.SPINE14973. [DOI] [PubMed] [Google Scholar]
- 47.Minimally invasive versus open posterior lumbar interbody fusion: a systematic review. Sidhu GS, Henkelman E, Vaccaro AR, et al. Clin Orthop Relat Res. 2014;472:1792–1799. doi: 10.1007/s11999-014-3619-5. [DOI] [PMC free article] [PubMed] [Google Scholar]