Abstract
To make them more responsive to their community’s needs, federally qualified health centers (FQHCs) are required to have a governing board comprised of at least 51% consumers. However, the extent to which consumer board members actually resemble the typical FQHC patient has not been assessed, which according to the political science literature on representation may influence the board’s ability to represent the community. This mixed-methods study uses four years of data from the Health Resources and Services Administration, combined with Uniform Data System, Bureau of Labor Statistics, and Area Resource File data to describe and identify factors associated with the composition of FQHC governing boards. Board members are classified into one of three groups: non-consumers, non-representative consumers (who do not resemble the typical FQHC patient), and representative consumers (who resemble the typical FQHC patient). The analysis finds that a minority of board members are representative consumers, and telephone interviews with a stratified random sample of 30 FQHC board members confirmed the existence of significant socioeconomic gaps between consumer board members and FQHC patients. This may make FQHCs less responsive to the needs of the predominantly low-income communities they serve.
Introduction
Federally qualified health centers (FQHCs) are primary care clinics first established in 1965 as part of President Lyndon Johnson’s War on Poverty. Located in underserved areas, they maintain an “open door” policy, providing care regardless of an individual’s ability to pay. Consequently, they serve a disproportionate share of uninsured individuals and Medicaid beneficiaries. Despite the challenges inherent in serving such vulnerable populations, FQHCs’ success in providing access to high quality, cost-effective health care is well documented (Proser 2005). Recognizing this, Congress made a significant investment in FQHCs, permanently authorizing the program and dedicating $11 billion in a new FQHC Trust Fund as part of the Affordable Care Act (Hall 2011).
A defining characteristic of FQHCs is their consumer governance mandate, which requires that at least 51% of the governing board must consist of consumers (i.e., patients) of the center. Furthermore, the board as a whole is required to “represent the individuals being served by the center” (Section 330 of the Public Health Service Act, 42 U.S.C. §254b). According to the Health Resources and Services Administration (HRSA), which administers the FQHC program:
“Since the intent is for consumer board members to give substantive input into the health center’s strategic direction and policy, these members should utilize the health center as their principal source of primary health care…[Additionally,] the board should be comprised of members with a broad range of skills and expertise. Finance, legal affairs, business, health, managed care, social services, labor relations and government are some examples of the areas of expertise needed by the board to fulfill its responsibilities (Bureau of Primary Health Care 1998a: 22).”
The requirement for FQHCs to have consumer-majority governing boards originated from the participatory democracy of the Civil Rights Movement, and a strong sentiment of “antiprofessionalism” that sought to empower the poor (Boone, 1972). More recently, consumer governance has been heralded as a way to make FQHCs more responsive to their community’s needs by giving a representative voice to a group of patients who are otherwise frequently under-represented (Phillips, 1998). In this view, the extent to which representatives share salient characteristics with those whom they represent (descriptive representation), is positively associated with the extent to which a representative advocates for the interests of those whom they represent (substantive representation) (Pitkin, 1967). Indeed, the positive relationship between descriptive and substantive representation has been well-established (Scherer and Curry 2010; Preuhs 2007; Wangnerud 2009; Herrick 2009). Descriptive representation may especially improve substantive representation of the interests of disenfranchised and under-represented groups in cases where disadvantaged groups are distrusting of those in power and where the views of the disadvantaged groups are not well known to persons outside of the group (Mansbridge, 1999; Dovi, 2003).
However, no formal process is mandated for the identification and selection of consumer board members, and little is known about who actually governs these increasingly important health care organizations (Hollister, 1974; Morone, 1998; Peterson, 1970). Prior studies have found consumer governance to be fraught with implementation challenges, including dominance by social elites (Robins and Blackburn 1974), low levels of consumer participation (Windle et al. 1974), and disparities in working knowledge between consumers and non-consumers (Paap 1978). More recent evidence suggests that FQHC board chairs and executive directors may undermine the intent of the consumer governance requirement by identifying potential board members for their expertise and encouraging them to become consumers (Bracken 2007).
Despite the challenges inherent in achieving descriptive representation (Chesney, 1982; Cross, 2002; Lipsky & Lounds, 1976) and the fact that disadvantaged groups lack the resources necessary to participate directly or engage their representatives to act on their behalf (Berinsky, 2002; Verba, Schlozman, and Brady, 1995), calls for direct citizen participation in health care persist (Morone & Kilbreth, 2003). Further complicating matters is the issue that, while consumer governance may make organizations more responsive to patient demands, the potential “technical expertise gap” between consumers and non-consumers may have important implications for organizational performance (LeRoux, 2009). FQHC governing boards are simultaneously required to have a consumer majority and the technical and professional expertise required for effective governance. Given a limited number of board seats, striking this balance may prove a challenge. As Gaventa (1998) writes, “Mandates for participation from ‘above’ must be linked with pre-existing capacities for participation ‘from below’.” The typical low-income, poorly educated FQHC consumer may be best able to identify the community’s needs, but is unlikely to possess the technical and/or professional skills required for the complex task of FQHC governance.
In the current study, I use mixed methods to describe the composition of FQHC governing boards, assess the extent to which consumer board members are socioeconomically representative of the FQHC patient population, and identify factors that predict variation in the consumer composition of FQHC governing boards. As FQHCs stand poised to play an even larger role in a reformed health care system, answering the decades-old question of who truly governs FQHCs is an important first step to better understanding the function of these important safety-net providers. This study also speaks to one potential role of consumers as “team members” in a modern health care system seeking to provide patient-centered care (Martin and Finn 2011), improve the cultural competence of health care organizations (Blustein et al. 2011), and allay concerns about government control of decision-making (Hsiao et al. 2011).
Study Data and Methods
Data on FQHC board members, including consumer status and occupation, are reported in Exhibit D of FQHC grant applications, which are filed annually with HRSA. These data for years 2003 – 2006 were obtained from HRSA in hard copy after filing a request under the Freedom of Information Act (FOIA). A second request was filed to obtain a more complete set of records. Using a high-volume scanner, in conjunction with specialized Able2Extract data extraction software (Investintech 2011), documents were converted into an electronic format and merged with FQHC-level data from HRSA’s Uniform Data System (UDS) and community-level data from the Area Resource File (ARF) for subsequent analysis in Stata 10 (StataCorp 2007).
Using the UDS data, some FQHCs were excluded from this study using a set of criteria designed to limit the analysis to fully operational, federally-funded FQHCs. At a minimum, such centers should have at least one full-time medical provider, at least one full-time administrative staff person, and at least 5,000 annual patient encounters (Wells et al. 2009). FQHCs not meeting these criteria were excluded. Additionally, FQHCs consist not only of community health centers (CHCs), but also include grantees of the migrant health, health care for the homeless, public housing, and school-based health center programs. These entities are eligible for a waiver of the consumer governance requirement if, and only if, they do not also receive funding from the CHC program (Bureau of Primary Health Care 1998b). Therefore, to ensure that all FQHCs in the sample were subject to the consumer governance requirement, non-CHC grantees were omitted from the sample. Finally, 164 FQHCs located in U.S. commonwealths and territories were excluded, because of the likelihood that these centers are substantively different from FQHCs located in the 50 United States or the District of Columbia.
Using these criteria, 615 FQHC-Year observations were excluded from the study. This left a starting sample of 3,143 FQHC-Years representing 824 unique FQHCs during the four years of the study. However, as shown in Table 1, the sample was limited to the 71.4% of total FQHC-Year observations in the UDS data for which corresponding grant application data were made available via the FOIA request.
Table 1.
Study Sample and FQHCs in Operation by Year
| Year | Total Number of FQHC Grantees | Number Excluded | Total FQHC Sample | Total Number of Grant Applications |
|---|---|---|---|---|
| 2003 | 890 | 154 | 736 | 397 (54%) |
| 2004 | 914 | 146 | 768 | 297 (39%) |
| 2005 | 952 | 155 | 797 | 767 (96%) |
| 2006 | 1,002 | 160 | 842 | 784 (93%) |
| Total | 3,758 | 615 | 3,143 | 2,245 (71.4%) |
Because FQHCs for which data are available may differ from FQHCs for which data are unavailable, a binary variable was created to indicate observations with missing FQHC grant data. A logistic regression of this variable on a set of variables available in the UDS for all 3,143 FQHCs in the sample indicated that FQHCs with and without missing data did not differ with respect to location, caseload, patient demographics, acuity, or payer mix.
On the grant applications, board member consumer status was recorded as a dichotomous variable, while board member occupation was reported in a free-response format. To standardize responses, the occupation data were coded to conform to Standard Occupational Classification (SOC) Codes used by the U.S. Bureau of Labor Statistics (BLS) (aU.S. Bureau of Labor Statistics 2010a). These codes uniquely identify occupations and allow them to be linked to data on average annual income, which are also available from the BLS (bU.S. Bureau of Labor Statistics 2010b). A table indicating how SOC codes were applied to the board member occupation data is available as an appendix.
After board members were assigned an SOC code, their occupations were dichotomized by income. Occupations with a mean annual income greater than 200% of the federal poverty level for a family of four in 2009 ($44,100) were considered high status, while occupations with incomes below this level were considered low status. This cutoff was selected to correspond with the socioeconomic status of the majority (>90%) of FQHC patients. An exception was made for social workers, whose average income would assign them to the low status category, because their field requires extensive training beyond college. In this way, based on their self-reported occupation and BLS data, each board member was assigned to a high or low status occupation. Then, because a low status board member is more descriptively representative of the typical FQHC patient than is a high status board member, the dichotomous consumer variable reported on FQHC grant applications was recoded categorically to include non-consumers, representative consumers, and non-representative consumers as shown in Figure 1.
Figure 1.
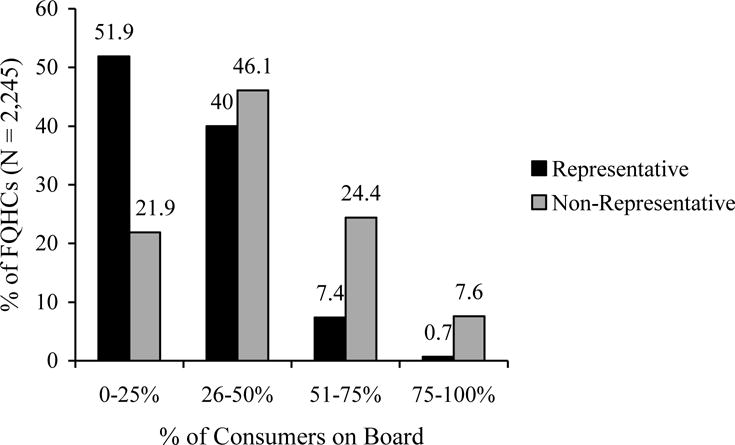
Categorization of FQHC Board Members
There were 293 cases where occupation was missing as well as 27 cases where occupation could not be clearly coded using the SOC codes. All of these cases (N = 320) were coded using an imputed value of “other” and treated as a low status occupation. This was done to code conservatively, making it more likely to assign someone of high socioeconomic status to a low status SOC than to assign someone of low socioeconomic status to a high status SOC. This is more likely to overestimate rather than underestimate the proportion of representative consumers, ensuring that results may be biased towards the null, but not overstated.
After examining the descriptive statistics to better understand board composition, a pair of ordinary least squares regression models were estimated to predict board composition as a function of various FQHC and community-level factors. The first model predicted the proportion of representative consumers on the board, while the second model predicted the proportion of non-representative consumers on the board. Both models were estimated using FQHC-level clustered standard errors to account for repeated observations of FQHCs over time. While a model with FQHC fixed effects would be ideal, these data represent a short panel with more variation in board composition between FQHCs than within FQHCs over time.
In addition to the quantitative analysis described above, semi-structured telephone interviews were conducted with 30 FQHC board members to assess their perception of the degree of descriptive representation on the board and provide additional context for interpreting the quantitative results. Using UDS data, all FQHCs were stratified into one of four cells representing all possible combinations of service provision (high vs. low) and financial performance (high vs. low). Using a random number generator, an FQHC was selected within each cell, and the CEO was contacted by email and asked to identify two board members (one consumer and one non-consumer, if possible) for interviews. If an FQHC declined to participate, it was replaced and another FQHC was randomly selected and contacted. A balance of census regions, urban and rural locations, and large and small FQHCs (cutoff of 9,293 users) was sought over time as respondents agreed to participate. Once a quota had been filled, a randomly selected FQHC that would exceed the quota was replaced and another FQHC was randomly selected. This process was continued as needed within each cell until enough FQHCs willing to participate in the study were identified.
Once an FQHC had agreed to participate in the study, the board members were contacted by email and/or telephone to schedule a mutually convenient time for the interviews. Telephone interviews were conducted and digitally recorded, and were kept semi-structured through the use of an interview guide containing a mixture of open-ended and fixed-response questions about the extent of consumer governance, its advantages and disadvantages, and the FQHC’s decision-making process. In practice, the interview guide was closely followed, although the question order was sometimes altered as the interview evolved and not all participants were asked all questions. The interviews generated approximately 23 hours of recorded audio and 363 pages of transcribed data.
All transcripts were reviewed once for accuracy and compared against the original audio file if necessary. Transcripts were reviewed a second time for substance, to increase familiarity with the interview content and better understand the data. In a third review, start codes were applied to the data using Atlas.ti (2009), with additional codes being created as dictated by the data. A 20% sample was independently coded by a research assistant as a validity check, with discrepancies resolved by consensus. Then, using Atlas.ti, the codes were linked to one another in an axial coding process to build a conceptual framework.
Study Results
The mean descriptive statistics for the sample are shown in Table 2, with selected variables broken out by year in Table 3. During the study period, the average FQHC board had between 12 and 13 members. Using the four years of data to categorize board members revealed that 30.9% of board members were non-consumers, while 69.1% were consumers. However, slightly more than 60% of self-reported consumers also self-identified high status occupations. As a result, 42.6% of board members are classified as non-representative consumers (whose socioeconomic status does not resemble the typical FQHC patient), while only 26.5% of board members are classified as representative consumers (whose socioeconomic status resembles the typical FQHC patient). By comparison, at least 66% of FQHC patients meet the criteria used to identify representative consumers, with income level unknown for an additional 27% of patients.
Table 2.
Summary Statistics (N=2,245)
| Variable | Mean | Std Dev |
|---|---|---|
| Board Size | 12.48 | 3.11 |
| % in Urban Location | 46.15 | 49.86 |
| Average Users per Delivery Site | 3609.26 | 2743.40 |
| Physicians as % of Staff | 8.15 | 3.62 |
| Physicians per 1,000 population | 1.76 | 1.14 |
| Nonprofits per 100,000 population | 10.12 | 13.22 |
| Grantee Type | ||
| % Migrant | 13.32 | 33.99 |
| % Homeless | 11.27 | 31.63 |
| % School-Based | 7.66 | 26.60 |
| % Public Housing | 3.07 | 17.26 |
| % Community Health | 100.0 | 0.0 |
| Census Region | ||
| % Midwest | 20.13 | 40.11 |
| % Northeast | 17.99 | 38.42 |
| % South | 36.26 | 48.09 |
| % West | 25.61 | 43.66 |
| % of Patients, Male | 40.51 | 5.49 |
| % of Patients, in Poverty | 48.59 | 23.23 |
| % of Patients, Non-white | 55.42 | 32.26 |
| % of Patients, Chronic Disease | 49.66 | 27.63 |
| Insurance Status | ||
| % Uninsured | 38.77 | 17.41 |
| % Medicaid | 31.87 | 14.33 |
| % Medicare | 9.01 | 6.01 |
| % Other Public | 1.84 | 3.97 |
| % Private | 18.51 | 13.81 |
| % of Population, Male | 49.30 | 1.87 |
| % of Population, in Poverty | 15.84 | 5.94 |
| % of Population, Uninsured | 15.45 | 4.93 |
| % of Population, Unemployed | 5.88 | 2.25 |
| % of Population, Non-white | 21.71 | 18.97 |
| % of Population, in Medicare | 15.01 | 3.96 |
Table 3.
Mean Descriptive Statistics for Select Variables by Year
| Variable | 2003 | 2004 | 2005 | 2006 | Overall |
|---|---|---|---|---|---|
| Board Size | 12.60 | 12.40 | 12.57 | 12.36 | 12.48 |
| % Non-Consumers | 31.43 | 31.56 | 30.61 | 30.64 | 30.89 |
| % Representative Consumers | 27.77 | 27.46 | 26.66 | 25.42 | 26.53 |
| % Non-Representative Consumers | 40.80 | 40.98 | 42.73 | 43.94 | 42.58 |
| % of Patients ≤ 200% FPL | 66.66 | 65.99 | 66.09 | 65.08 | 65.83 |
| % of Patients ≥ 201% FPL | 9.21 | 8.03 | 7.24 | 6.61 | 7.47 |
| % of Patients FPL Unknown | 24.13 | 25.98 | 26.66 | 28.31 | 26.70 |
|
| |||||
| Observations (N) | 397 | 297 | 767 | 784 | 2245 |
However, there is variation in the composition of governing boards between FQHCs. The distribution of FQHCs by the proportion of representative and non-representative consumers on the board is shown in Figure 2. While representative consumers are in the minority on nearly 92% of FQHC boards, a small number of FQHCs do have representative consumer majorities. Similarly, non-representative consumers are in the minority on 68% of FQHC boards. Together, it is evident that although some FQHCs meet the consumer governance requirement entirely with representative or non-representative consumers, most boards employ a mix of the two. The trend data in Table 3 suggest, however, that the consumer board member population is slowly becoming less representative over time.
Figure 2.
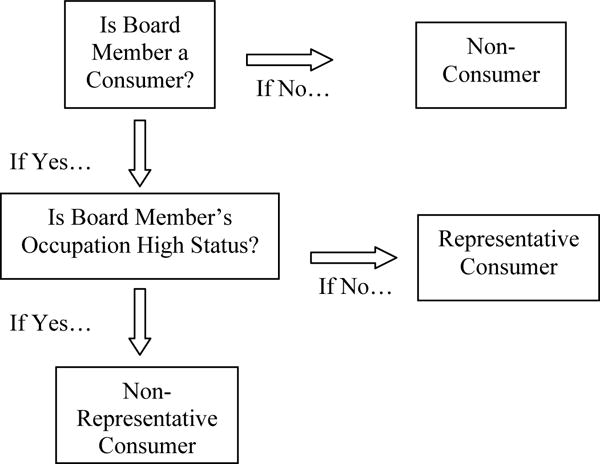
Distribution of FQHC Boards by Proportion of Representative and Non-Representative Consumer Members
Overall, the regression models explained 10% of the variation in the proportion of representative consumers on the board and 25% of the variation in the proportion of non-representative consumers on the board. While FQHC size (caseload) was not significantly associated with board composition, board size itself was an important factor. Each additional board member is associated with a decrease of nearly 0.6 percentage points in the composition of non-representative consumers on the board, but is not associated with the proportion of representative consumers. Staff composition was also important. Each 10 percentage point increase in the proportion of staff comprised of physicians is associated with a decrease of 4.9 percentage points in the proportion of representative consumers and an increase of 5.6 percentage points in the proportion of non-representative consumers on the board.
Location is one of the most important determinants of FQHC board composition. FQHCs in urban locations have nearly 3 percentage points fewer non-representative consumers on the board, though urbanicity is not associated with the proportion of representative consumers. Additionally, compared to FQHCs in the northeast, FQHCs in the south and west census regions have a lower proportion of non-representative consumers and a higher proportion of representative consumers on the board. Perhaps also related to location, FQHCs with a migrant health center grant have, on average, 8.6 percentage points fewer non-representative consumers and 6.4 percentage points more representative consumers on the board.
Case-mix by gender, poverty level, and race were not significant predictors of board composition. However, insurance status was an important predictor of the proportion of non-representative consumers on the board. FQHCs with a greater proportion of uninsured and/or Medicaid patients tended to have lower proportions of non-representative consumers, while FQHCs with a greater proportion of Medicare patients tended to have higher proportions of non-representative consumers. Insurance status did not affect the proportion of descriptive consumers. The year variables indicate that the proportion of non-representative consumers on the board increased by more than 3 percentage points between 2003 and 2006. Conversely, while there was a decreasing trend in the proportion of representative consumers, it was not statistically significant. None of the community-level population demographics were statistically significant in either model, however each additional nonprofit per 100,000 population is associated with an 0.21 percentage point increase in the proportion of non-representative consumers on the board.
The composition of FQHC governing boards identified in the quantitative analysis was generally confirmed by the qualitative interviews. All four U.S. Census regions were represented, with board members from FQHCs in Alaska, California, Florida, Illinois, Kentucky, Maine, Maryland, Massachusetts, Michigan, New York, Oklahoma, South Carolina, Virginia, and Wisconsin participating in the interviews. The respondents consisted of 12 men and 18 women ranging in age from 28 to 75, with a mean age of 56 years. The majority were white (n=16) or black (n=12). Six of the respondents were board chair, three were vice chair, seven were secretary, one was treasurer, and the remaining thirteen did not hold office.
The interview respondents themselves were not descriptively representative of the typical FQHC patient. Participants were highly educated, with 29 of the 30 completing at least some college, and 11 possessing graduate degrees. They were also generally high-income. Nearly 60% of respondents reported an annual household income greater than $80,000, while only five individuals reported an annual household income below $40,000.
Most respondents (80%) identified as FQHC patients. However, two of these patients indicated that they did not consider the FQHC to be their usual source of care, and three additional patients reported using dental services only. In essence, 19 board members (63%) were consumers who considered the FQHC to be their usual source of primary care, while 11 board members (37%) were either not consumers or consumers who did not meet HRSA’s definition of a consumer. A comparison of consumer and board member tenure revealed that 25% of the self-identified consumers interviewed had joined the board prior to becoming a patient.
When asked to assess the level of representativeness on their board, there was near-universal recognition of a socioeconomic gap between the board and the patients. Most common were responses like this one from a board member at an FQHC in New York City, expressing that the board members are not representative of the patients served in a number of ways:
“Basically, most of our board is full time working professionals who have private health insurance and who use various private sources of care. Our patients for the most part are low income people of color who live in inner-city neighborhoods….On our board, there’s a big class, race, socioeconomic, educational gulf between people like myself and most of the patients…I’m not really a patient the way the community health center governance requirements were set up. Now, not everybody has to be a patient, you want to have some people like me, but there should be more patient-patients, patients with a capital P as opposed to patients in quotation marks…”
Similarly representative responses came from a board member at an FQHC in Baltimore and a board member at an FQHC in rural Michigan who stressed differences in income and education between the board and patients:
“I think that we’re probably not quite as representative because our board is pretty well educated even though we’re lower to middle income. We’re probably on a little better heel than most of the clients that we see…I suspect that most of our client base is from the lower economic strata and I think our trustee-based clients is probably middle-income, moderate-income.”
“I think the new breed in particular tends to be a socioeconomic cut or cuts above the typical patient…You have to understand a financial statement or a legal document. You need to have a little education.”
A few respondents, like this one from an FQHC in rural Alaska, described their boards as being at least somewhat representative of the patients served, but still noted a socioeconomic divide:
“I think we’re relatively representative. The one thing that perhaps we may not be is that…most of those of us on the board are in an upper income bracket for the area…Many of the people on the other end of our sliding scale are up here in subsistence lifestyles and/or seasonal workers, sometimes unemployed…We’re not exactly representative of the lower end of the scale.”
While some respondents indicated that their board did a good job of representing the racial, gender, and geographic diversity of their patients, none of the respondents indicated that their board was very representative of the patients served, primarily citing substantial socioeconomic differences between the patients and the board members.
Discussion
Despite the requirement that a majority of board members must be consumers, the results of this study suggest that descriptive representation is lacking on most FQHC governing boards. While nearly two-thirds of board members are consumers, only about one-fourth are representative of typical FQHC patients. What is more, the method used to categorize consumer board members is likely to have overestimated the degree of descriptive representation. It is reasonable to assume that the true proportion of representative consumer board members may be closer to one-in-five. By contrast, the majority of consumer board members are not representative. While the board members in this group do report being FQHC patients, they also belong to a high status group that includes physicians, lawyers, and other professionals.
The predictive modeling suggests that FQHCs in urban areas of the northeast United States tend to have lower levels of consumer governance overall, especially as board size increases. Among consumers, certain factors seem to be associated with the representative/non-representative mix on the board. For example, the positive association of both Medicare case-mix and physicians as percentage of staff with non-representative consumer board members suggests that perhaps older, retired professionals and physicians themselves may be the ones serving on the board. The lack of an association between aggregate patient and community demographics and board composition suggests that board member selection is highly targeted and is not limited in any way by the pool of potential board members available to choose from. And, importantly, the regression models confirm that boards are becoming less descriptively representative over time.
Data from qualitative interviews confirm the lack of descriptive representation and suggest that it is driven more by socioeconomic gaps than by differences in race, gender, or geographic residence. They also indicate that self-reported consumer status may be less than ideal in other important ways, as some self-reported consumers did not consider the FQHC their usual source of care, did not utilize the FQHC for primary care, or did not become a consumer until after first joining the board. All of these characteristics suggest a lack of shared experiences between consumer board members and the typical FQHC patient that stands to make them less descriptively representative (Dovi 2003; Mansbridge 1999). This may have important implications for how well FQHCs are able to relate and respond to the needs of the communities they serve.
These findings are consistent with the well documented struggles to achieve descriptive representation in the early days of the health center program (Hochbaum 1969; Hollister 1974; Hollister et al. 1974; Paap 1978; Paap and Hanson 1982; Peterson 1970; Thompson 1980). However, more recent empirical studies did not identify deficiencies in descriptive representation (Bracken 2007; Latting 1983; Samuels and Xirasagar 2005). This can be explained by the fact that these more recent studies considered consumers to be a homogenous or nearly homogenous group.
The results of this study clearly demonstrate that consumer homogeneity is a strong assumption and that there are in fact considerable differences between consumer board members, especially with regards to socioeconomic status, which should be taken into consideration. The reality is that some consumer board members are more descriptively representative of the typical FQHC patient than others.
Yet, just because the level of descriptive representation is much lower than might be expected given the requirement of a consumer majority, it is important not to overlook the fact that FQHC boards are composed, on average, of 20 to 25% descriptively representative consumer board members. Given the obstacles to participation members of this group tend to face, this level of descriptive representation is a notable achievement in and of itself. One can imagine, for example, how different the United States Congress would look if it were to achieve this level of descriptive representation with regards to the electorate. What is more, even nominal consumer governance may yield community benefits (Banducci et al. 2004). Thus, the descriptive findings presented here should not be used to draw conclusions about the effectiveness of consumer governance.
This study has some limitations. While individual board members were coded into SOC groups as conservatively as possible, assumptions were made regarding the coding and categorization of board members. A cutoff of 200% FPL for a family of four was assumed as the indicator of a high status occupation. For single individuals or those in a smaller family, this will lead to a conservative estimate. However, for individuals from a larger family, this will tend to overstate income relative to poverty.
Furthermore, mean annual income for each occupation was used, although some occupations may have more variation in wages than others. For an individual at the lower end of the range, a higher mean income for the group may lead a descriptive consumer to be categorized as a non-descriptive consumer, while for individuals at the higher end of the range, a lower mean income for the group may lead a non-representative consumer to be categorized as a representative consumer.
Finally, the use of average annual occupational income only directly accounts for one dimension of representativeness. While this measure is likely correlated with other dimensions like education, it is not a perfect indicator. Consumer board members can be descriptively representative of the patient population in a variety of ways. Thus, a continuous index—rather than categorical measure—of descriptive representation would be the ideal solution. Unfortunately, no data were available to attempt this approach. The method used was conservative enough, however, to be confident that, if anything, the results may be understated.
Going forward, future studies of consumer governance should strive to identify relevant differences between consumer board members. While the BPHC requires consumer board members, as a whole, to “represent the individuals served by the health center in terms of race, ethnicity, and gender (Bureau of Primary Health Care 1998a: 22),” other important factors like insurance status, income, and education level have not been addressed. Health status might also be an important factor, as patients who utilize more services (e.g., those with a chronic illness) are more knowledgeable about the care they receive and more comfortable voicing their concerns to decision-makers, than are patients who rarely use services (Schlesinger et al. 2002).
Future studies might also focus on understanding barriers to descriptive representation and designing ways to enhance levels of descriptive representation in practice. Board composition is ultimately the result of board member selection. Prior qualitative research finds that FQHC staff often identify potential consumer board members without making their patient status a primary consideration in their selection, because it is challenging to find the expertise needed for governance among the FQHC’s patient population (Bracken 2007). While the current study reinforces these findings, a longitudinal case study of select FQHCs could provide valuable data on actual board member selection processes. At the very least, further inquiry into the role and contributions of descriptively representative consumer board members is warranted.
To be able to answer these questions well, there is a need for HRSA to collect and share better data on FQHCs. For instance, it would be useful to collect governance data on board member age, gender, race, education level and income. It would also be helpful to collect data on how long consumer board members have been receiving care at the center and how many visits for care they make annually. Finally, HRSA should consider making FQHC governance data publicly available in an electronic format to facilitate continued research into an important aspect of one of the nation’s most highly regarded safety net providers.
At the same time as the FQHC program has been permanently authorized and received the largest funding increase in its history, there is an ongoing debate about the effectiveness of consumer governance and the appropriateness of making certain federal funding contingent on having a consumer majority board. Many hospitals, free clinics, and other safety-net providers without consumer majority boards are ineligible for the federal grant funds and enhanced Medicaid reimbursement rate that FQHCs enjoy.
While this study cannot speak directly to the effectiveness of consumer governance, it provides the first empirical evidence regarding the composition of FQHC governing boards and, given the limited involvement of descriptively representative consumers on the board, raises questions about the potential of consumer governance to affect health center outcomes. Answering these questions is essential to informing the policy debate over consumer governance in health care.
Supplementary Material
Table 4.
Results of Linear Regression Models Predicting Board Composition (N=2,245)
| Model 1 | Model 2 | |
|---|---|---|
| % Representative Consumers | % Non-Representative Consumers | |
| Board Size | 0.15 (0.16) |
−0.59** (0.17) |
| Urban Location | 0.69 (0.93) |
−2.74** (1.05) |
| Average Users per Delivery Site (in thousands) | −0.14 (0.19) |
0.06 (0.22) |
| Physicians as % of Staff | −0.49** (0.16) |
0.56*** (0.16) |
| Physicians per 1,000 population | −0.96 (0.58) |
0.23 (0.71) |
| Nonprofits per 100,000 population | −0.01 (0.05) |
0.21** (0.06) |
| Grantee Type (CHC omitted) | ||
| Migrant | 6.43*** (1.67) |
−8.56*** (1.79) |
| Homeless | 1.50 (1.63) |
−3.44 (1.83) |
| School-Based | 0.88 (1.75) |
−1.22 (2.01) |
| Public Housing | 0.65 (2.71) |
1.27 (3.36) |
| Census Region (Northeast omitted) | ||
| Midwest | 1.69 (1.45) |
−3.50 (1.91) |
| South | 3.31* (1.62) |
−4.27* (2.01) |
| West | 4.90* (1.94) |
−6.25** (2.27) |
| % of Patients, Male | 0.16 (0.11) |
0.24 (0.12) |
| % of Patients, in Poverty | 0.01 (0.03) |
0.02 (0.03) |
| % of Patients, Non-white | −0.02 (0.03) |
0.001 (0.03) |
| % of Patients, Chronic Disease | 0.04 (0.02) |
−0.05* (0.02) |
| Insurance Status (Private omitted) | ||
| % Uninsured | 0.07 (0.06) |
−0.25*** (0.06) |
| % Medicaid | 0.11 (0.06) |
−0.30*** (0.07) |
| % Medicare | −0.17 (0.15) |
0.40* (0.17) |
| % Other Public | 0.07 (0.13) |
−0.23 (0.14) |
| % of Population, Male | 0.34 (0.36) |
−0.32 (0.39) |
| % of Population, in Poverty | 0.19 (0.16) |
−0.15 (0.18) |
| % of Population, Uninsured | −0.15 (0.23) |
0.45 (0.26) |
| % of Population, Unemployed | 0.40 (0.30) |
0.11 (0.30) |
| % of Population, Non-white | 0.004 (0.04) |
0.06 (0.04) |
| % of Population, in Medicare | −0.24 (0.18) |
0.08 (0.20) |
| Year (2003 Omitted) | ||
| 2004 | −0.25 (1.24) |
−0.12 (1.41) |
| 2005 | −1.06 (0.93) |
2.28* (1.07) |
| 2006 | −1.84 (1.04) |
3.28** (1.18) |
| Constant | −1.19 (19.90) |
63.15** (22.28) |
|
| ||
| R-Squared | 0.10 | 0.25 |
References
- ATLAS.ti. Version 6.1. Scientific Software Development; Berlin, Germany: 2009. [Google Scholar]
- Banducci Susan A, et al. Minority Representation, Empowerment and Participation. The Journal of Politics. 2004;66(2):534–56. [Google Scholar]
- Berinsky Adam J. Silent voices: Social welfare policy opinions and political equality in America. American Journal of Political Science. 2002;46(2):276–87. [Google Scholar]
- Blustein Jan, et al. Analysis Raises Questions on Whether Pay-For-Performance in Medicaid Can Efficiently Reduce Racial and Ethnic Disparities. Health Affairs. 2011;30(6):1165–75. doi: 10.1377/hlthaff.2010.1022. [DOI] [PubMed] [Google Scholar]
- Boone RW. Reflections on citizen participation and the economic opportunity act. Public Administration Review. 1972;32:444–456. Special Issue: Citizens Action in Model Cities and CAP Programs. [Google Scholar]
- Bracken Nancy J. The Impact of the User Board Majority Requirement on the Governance of Community Health Centers. Medical University of South Carolina; Charleston, SC: 2007. Unpublished Doctoral Dissertation. [Google Scholar]
- Bureau of Primary Health Care. Health Center Program Expectations. 1998a Aug 17; ftp://ftp.hrsa.gov/bphc/docs/1998pins/PIN98-23.PDF.
- Bureau of Primary Health Care. Implementation of the Section 330 Governance Requirements. 1998b Apr 28; http://bphc.hrsa.gov/policiesregulations/policies/pdfs/pin199812.pdf.
- Chesney JD. Strategies for building representative HSAs: The impact of legal structure. Journal of Health Politics, Policy and Law. 1982;7(1):96–110. doi: 10.1215/03616878-7-1-96. [DOI] [PubMed] [Google Scholar]
- Cross M. Should consumers be present on an HMO’s board of directors? Managed Care. 2002;11(11):22–28. [PubMed] [Google Scholar]
- Dovi Suzanne. Preferable Descriptive Representatives: Will Just Any Woman, Black, or Latino Do? American Political Science Review. 2003;96(04):729–43. [Google Scholar]
- Gaventa J. Poverty, participation and social exclusion in north and south. IDS Bulletin. 1998;29(1):50–57. [Google Scholar]
- Hall Mark A. The Mission of Safety Net Organizations Following National Insurance Reform. Journal of General Internal Medicine. 2011;26(7):802–5. doi: 10.1007/s11606-011-1654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick Rebekah. The Effects of Sexual Orientation on State Legislators’ Behavior and Priorities. Journal of Homosexuality. 2009;56(8):1117–33. doi: 10.1080/00918360903279361. [DOI] [PubMed] [Google Scholar]
- Hochbaum Godfrey M. Consumer Participation in Health Planning: Toward Conceptual Clarification. American Journal of Public Health. 1969;59(9):1698–1705. doi: 10.2105/ajph.59.9.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollister Robert M. Neighborhood Health Centers as Demonstrations. In: Hollister RM, Kramer BM, Bellin SS, editors. Neighborhood Health Centers. Lexington, MA: Lexington Books; 1974. [Google Scholar]
- Hollister Robert M, et al. Neighborhood Health Centers as a Social Movement. In: Hollister RM, Kramer BM, Bellin SS, editors. Neighborhood Health Centers. Lexington, MA: Lexington Books; 1974. [Google Scholar]
- Hsiao William C, et al. What Other States Can Learn from Vermont’s Bold Experiment: Embracing a Single-Payer Health Care Financing System. Health Affairs. 2011;30(7):1232–41. doi: 10.1377/hlthaff.2011.0515. [DOI] [PubMed] [Google Scholar]
- Investintech.com Inc. Able2Extract Professional. Toronto, Canada: 2011. [Google Scholar]
- Latting Jean E. Selecting Consumers for Neighborhood Health Center Boards. Journal of Community Health. 1983;9(2):110–22. doi: 10.1007/BF01349874. [DOI] [PubMed] [Google Scholar]
- LeRoux K. Paternalistic or participatory governance? Examining opportunities for client participation in nonprofit social service organizations. Public Administration Review. 2009;69(3):504–517. [Google Scholar]
- Lipsky M, Lounds M. Citizen participation and health care: Problems of government induced participation. Journal of Health Politics, Policy and Law. 1976;1(1):85–111. doi: 10.1215/03616878-1-1-85. [DOI] [PubMed] [Google Scholar]
- Mansbridge Jane. Should Blacks Represent Blacks and Women Represent Women? A Contingent “Yes”. Journal of Politics. 1999;61(3):628–57. [Google Scholar]
- Martin Graham P, Rachael Finn. Patients as Team Members: Opportunities, Challenges, and Paradoxes of Including Patients in Multi-Professional Healthcare Teams. Sociology of Health & Illness. 2011;33(7):1050–65. doi: 10.1111/j.1467-9566.2011.01356.x. [DOI] [PubMed] [Google Scholar]
- Morone JA. The democratic wish: Popular participation and the limits of American democracy. New Haven, CT: Yale University Press; 1998. [Google Scholar]
- Morone JA, Kilbreth EH. Power to the people? Restoring citizen participation. Journal of Health Politics, Policy and Law. 2003;28(2–3):271–288. doi: 10.1215/03616878-28-2-3-271. [DOI] [PubMed] [Google Scholar]
- Paap Warren R. Consumer-Based Boards of Health Centers: Structural Problems in Achieving Effective Control. American Journal of Public Health. 1978;68(6):578–82. doi: 10.2105/ajph.68.6.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paap Warren R, Bill Hanson. Unobtrusive Power: Interaction between Health Providers and Consumers at Council Meetings. Journal of Contemporary Ethnography. 1982;10(4):409–31. [Google Scholar]
- Peterson Paul E. Forms of Representation: Participation of the Poor in the Community Action Program. The American Political Science Review. 1970;64(2):491–507. [Google Scholar]
- Phillips A. Democracy and representation: Or, why should it matter who our representatives are? In: Phillips A, editor. Feminism and politics. New York: Oxford University Press; 1998. pp. 224–240. [Google Scholar]
- Pitkin Hanna F. The Concept of Representation. Berkeley: The University of California Press; 1967. [Google Scholar]
- Preuhs Robert R. Descriptive Representation as a Mechanism to Mitigate Policy Backlash: Latino Incorporation and Welfare Policy in the American States. Political Research Quarterly. 2007;60(2):277–92. [Google Scholar]
- Proser Michelle. Deserving the Spotlight: Health Centers Provide High-Quality and Cost-Effective Care. Journal of Ambulatory Care Management. 2005;28(4):321–30. doi: 10.1097/00004479-200510000-00007. [DOI] [PubMed] [Google Scholar]
- Robins Arthur J, Cheryl Blackburn. Governing Boards in Mental Health: Roles and Training Needs. Administration and Policy in Mental Health and Mental Health Services Research. 1974;2(1):37–45. [Google Scholar]
- Samuels Michael E, Xirasagar Sudha. National Survey of Community Health Center\Board Chairs. Kansas City, MO: National Rural Health Association; 2005. [DOI] [PubMed] [Google Scholar]
- Scherer Nancy, Brett Curry. Does Descriptive Race Representation Enhance Institutional Legitimacy? The Case of the US Courts. The Journal of Politics. 2010;72(1):90–104. [Google Scholar]
- Schlesinger Mark, et al. Voices Unheard: Barriers to Expressing Dissatisfaction to Health Plans. Milbank Quarterly. 2002;80(4):709–55. doi: 10.1111/1468-0009.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Section 330 of the Public Health Service Act, 42 U.S.C. §254b.
- StataCorp. Stata statistical software: Release 10. College Station, TX: 2007. [Google Scholar]
- Thompson Theodis. An Ordinal Evaluation of the Consumer Participation Process in Community Health Programs. Nursing Research. 1980;29(1):50–4. [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. 2010 SOC Definitions. 2010a http://www.bls.gov/soc/soc_2010_definitions.pdf.
- U.S. Bureau of Labor Statistics. May 2009 National Occupational Employment and Wage Estimates. 2010b http://www.bls.gov/oes/current/oes_nat.htm.
- Verba Sidney, Schlozman Kay L, Brady Henry E. Voice and Equality: Civic Voluntarism in American Politics. Cambridge: Harvard University Press; 1995. [Google Scholar]
- Wängnerud Lena. Women in Parliaments: Descriptive and Substantive Representation. Annual Review of Political Science. 2009;12:51–69. [Google Scholar]
- Wells Rebecca S, et al. Why Do Some Health Centers Provide More Enabling Services than Others? Journal of Health Care for the Poor and Underserved. 2009;20(2):507–23. doi: 10.1353/hpu.0.0151. [DOI] [PubMed] [Google Scholar]
- Windle Charles, et al. PR Aside: Initial Results from NIMH’s Service Program Evaluation Studies. American Journal of Community Psychology. 1974;2(3):311–27. doi: 10.1007/BF00880852. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


