Abstract
The incidence and prevalence of cardiovascular disease is highest among the elderly, in part, due to deleterious effects of advancing age on the heart and blood vessels. Aging, a known cardiovascular risk factor, is progressively associated with structural and functional changes to the vasculature including hemodynamic disturbance due to increased oxidative stress, premature cellular senescence and impairments in synthesis and/or secretion of endothelium-derived vasoactive molecules. These molecular and physiological changes lead to vessel wall stiffening and thickening, as well as other vascular complications that culminate to loss of vascular tone regulation and endothelial function. Intriguingly, the vessel wall, a biochemically active structure composed of collagen, connective tissue, smooth muscle and endothelial cells, is adversely affected by processes involved in premature or normal aging. Notably, the inner most layer of the vessel wall, the endothelium, becomes senescent and dysfunctional with advancing age. As a result, its ability to release vasoactive molecules such as acetylcholine (ACh), prostacyclin (PGI2), endothelium-derived hyperpolarizing factor (EDHF), and nitric oxide (NO) is reduced and the cellular response to these molecules is also impaired. By contrast, the vascular endothelium increases its generation and release of reactive oxygen (ROS) and nitrogen (RNS) species, vasoconstrictors such as endothelin (ET) and angiotensin (AT), and endogenous inhibitors of NO synthases (NOSs) to block NO. This skews the balance of the endothelium in favor of the release of highly tissue reactive and harmful molecules that promote DNA damage, telomere erosion, senescence, as well as stiffened and hardened vessel wall that is prone to the development of hypertension, diabetes, atherosclerosis and other cardiovascular risk factors. This Review discusses the impact of advancing age on cardiovascular health, and highlights the cellular and molecular mechanisms that underlie age-associated vascular changes. In addition, the role of pharmacological interventions in preventing or delaying age-related cardiovascular disease is discussed.
Keywords: Vascular aging, Endothelium, Endothelial senescence, Vascular rejuvenation, Vascular function, Vascular pharmacology, Cardiovascular health
Introduction
More than three centuries ago, a famous English physician and author, Thomas Sydenham, said “A man is as old as his arteries”. This popular quote signifies a correlation between aging and the cardiovascular system including the susceptibility of this system to age-associated changes. Indeed, cardiovascular diseases such as atherosclerosis, hypertension, diabetes and heart attack are the leading causes of morbidity and mortality in the elderly population. In line with this, premature or normal aging is a major cardiovascular risk factor. According to the National Institute of Aging (NIA), about 40% of all deaths in the elderly (age 65 and older) are related to cardiovascular disease [1]. The risk for cardiovascular morbidity between the ages of 50 and 80 increases by about 10-fold. Meanwhile, premature aging syndromes such as Hutchinson-Gilford progeria syndrome (HGPS) and Werner syndrome (WRN) are disproportionally affected by cardiovascular disease including heart attack and stroke [2]. As a result, healthcare expenses related to cardiovascular care is much higher in the accelerated aging syndromes and advancing age population and has mounted profound economic and public health burden. Therefore, understanding the molecular and cell biological processes underlying age-associated structural and functional changes to the cardiovascular system including the heart and blood vessels is of significant importance.
The effect of aging on cardiovascular health is in part because aging perturbs a number of metabolic and hemodynamic mechanisms in the cardiovascular system in general and the vascular endothelium in particular [3–5]. Some of these perturbations include increased oxidative stress and reduced telomere length resulting in DNA damage, impaired replicative capacity of cells and upregulated cardiovascular tissue senescence [6]. These changes expose the heart and its vascular network to a series of risk factors that impair physiological repair mechanisms, and accelerate vascular dysfunction and cardiovascular disease.
Vascular endothelium, a diaphanous film of tissue, is the inner-most structure that coats the interior walls (tunica intima) of the cardiovascular and lymphatic systems covering a surface area of over 4,000 m2 [7,8]. This structure is laid with a monolayer of about one trillion endothelial cells throughout its lumen [9]. Vascular endothelial cells (ECs) have a distinct cobblestone-like morphology and are involved in the regulation of de novo formation of blood vessels (vasculogenesis), blood vessel sprouting (angiogenesis), vascular tone (vasodilation and vasoconstriction), vascular permeability, blood clotting, as well as inflammation and immune defense [8–10]. In addition, ECs are actively involved in the suppression of middle vascular layer (tunica media) cells (i.e. vascular smooth muscle cells) from outgrowing into the tunica intima layer and interfering with normal vascular function. Furthermore, ECs synthesize and release vasoactive molecules including endothelium-derived relaxing factor (EDRF) to promote relaxation of vascular smooth muscle. With advancing age, ECs have depleted anti-inflammatory and antioxidant defense mechanisms and are subjected to augmented inflammatory and oxidative stress that impairs their number, morphology and function [11]. As a result, older subjects have increased susceptibility to cardiovascular morbidity and death. The present review discusses the contribution of advancing age to vascular endothelial dysfunction, and the sequelae of aged and dysfunctional endothelium in the development and progression of cardiovascular diseases. The review also discusses current and future perspectives in the treatment of vascular aging.
Vascular endothelium: senescence and aging
Healthy endothelium chiefly regulates cardiovascular physiology including fine tuning vascular tone, tissue perfusion and oxygenation, resistance to thrombosis, inhibition of underlying smooth muscle cell proliferation, adhesion of inflammatory cells to vessel wall and vascular fibrosis [8].
By contrast, dysfunctional or aged endothelium is characterized by several phenotypic changes and molecular patterns that include impaired replicative capacity of cells, increased cellular senescence, reduced generation of anti-inflammatory molecules, antioxidants and other salutary mechanisms that are involved in vascular homeostasis [11,12]. Physiologically, endothelial function is mediated by shear stress and the release of vasodilating molecules such as acetylcholine (ACh), prostacyclin (PGI2), adenosine, bradykinin, vascular endothelial growth factor (VEGF), nitric oxide (NO), and guanosine 3′, 5′-cyclic monophosphate (cGMP), as well as simultaneous regulation of mediators involved in vasoconstriction, inflammation and thrombosis including endothelin (ET), angiotensin (AT), prostaglandins (PGs), leukotrienes (LTs), thromboxanes (TXs), and endogenous inhibitors of NO synthases (NOSs) to block NO. Failure of the senescing endothelium to maintain the physiological balance between these opposing functions is the basis for increased cardiovascular risk in the elderly. Below is a description of how vascular aging is associated with cardiovascular morbidity and mortality.
Is vascular senescence a risk factor for cardiovascular disease?
Cellular senescence and vascular aging are perpetrated and/or accelerated by several factors that induce oxidative stress and DNA damage. Some of the common predisposing factors include aging, tobacco smoke, chemotherapeutic drugs and exposure to radiation. For example, ionizing radiation depopulates stem cell reserve and induces premature replicative senescence (i.e. arrests cell division) of somatic cells through increased generation of free radicals and subsequent DNA damage [13–15]. In addition, some of the commonly used chemotherapeutic drugs such as doxorubicin and cisplatin induce cellular senescence by altering DNA structure and function [16]. In the cardiovascular system, some chemotherapeutic drugs and radiation therapy are associated with increased risk of cardiotoxicity and vascular damage [16–18]. In particular, the administration of radiation therapy to the chest wall is a significant cause of vascular endothelial dysfunction including impaired perfusion, fibrous thickening of the pericardium and myocardial fibrosis [19,20]. These cardiac and vascular lesions culminate to senescence of resident cardiomyocytes and endothelial cells leading to hardening of the heart muscle and stiffening of vascular wall to trigger angina, dyspnea and heart failure that leads to sudden death [21].
In the absence of history of exposure to chemotherapy or radiation therapy, traditional risk factors such as chronological aging play significant role in promoting processes involved in biological aging including oxidative stress, DNA methylation, telomere shortening, as well as structural and functional changes to the vasculature. As a result, the endothelium compromises its ability to secrete many of its vasoactive molecules such as growth factors, hormones, NO and microRNA (miRNA). In addition, the number and function of endothelial progenitor cells (EPCs) is reduced with advancing age. Taken together, the endothelium becomes senescent and prone to cardiovascular disease including hypertension, atherosclerosis and diabetes [22–24].
Regulation of endothelial function
Exogenously, endothelial function is influenced by several factors including smoking, diet and exercise. Endogenously, the expression and/or activity of several mediators determine the integrity and optimal function of vascular endothelium including its bidirectional response to aging, disease onset and progression. Below is a description of how some key endogenous molecules, endothelial progenitor cells, as well as exercise and diet, are involved in vascular pathobiology.
Growth factors
A number of angiogenic growth factors and their receptors are centrally involved in the formation and maturation of blood vessels, regulation of endothelial cell proliferation and migration. Some of the main factors include vascular endothelial growth factors (VEGFs) and their receptors (VEGFR-I, VEGFR-II and VEGFR-III), platelet-derived growth factors (PDGFs) and their receptors (PDGFRalpha and PDGFRbeta), as well as fibroblast growth factors (FGFs) and their receptors (FGFR-I to FGFR-IV). By far, VEGF is the most potent and highly specific mitogen for endothelial cells. So far, five isoforms of VEGF have been identified and characterized [25,26]. The first two tyrosine-kinase receptors, VEGFR-I (Flt-1) and VEGFR-II (Flk-1/KDR), are predominantly expressed in endothelial cells and efficiently recognize most of the members of the VEGF family in order to promote cell proliferation, migration and inhibition of apoptosis. In vivo, VEGF is absolutely required in the modulation of angiogenesis and vasculogenesis and its genetic suppression in animals leads to embryonic lethality due to failure of the cardiovascular system to develop [27,28].
Similarly, targeted disruption of Flt-1 or Flk-1 causes severe defects in endothelial differentiation and formation of functional blood vessels [29,30]. By contrast, overexpression of Flt-1 may promote abnormal cell migration, cell-cell and cell-matrix interactions leading to severely defective blood vessels [29]. Thus, optimal levels of VEGF and its tyrosine kinase receptors is required for homeostasis of the vascular system. However, chronological aging is unable to maintain physiological levels of VEGF. As a result, endothelial cells isolated from aged subjects show downregulation of VEGF mRNA and protein expression and impairment in their angiogenic capacity [31]. Restoration of VEGF expression using recombinant protein promotes angiogenesis in senescent rat heart [32]. Similar to VEGF, aging has been implicated in the downregulation of PDGF receptor and impairment of cell proliferation whereas re-expression of its levels enhances cell proliferation and function [33]. The FGF signaling is also normally involved in suppression of cellular senescence and vascular dysfunction [34,35]. However, inhibition of this signaling pathway results in loss of endothelial barrier function [34].
Cytokines and adhesion molecules
Several cytokines can modulate vascular function directly or indirectly by regulating the expression of growth factors such as VEGF [36–39]. For example, systemically secreted or locally released tumor necrosis factor alpha (TNFα) induces macrovascular and microvascular dysfunction in part through transcriptional upregulation of pro-inflammatory cytokines including interleukins (e.g. IL6 and IL8), adhesion molecules (e.g. VCAM1, ICAM1 and MCP1), nuclear factor kB (NFkB), inducible NOS (iNOS), nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, and by increasing intravascular production of ROS [40]. With age, the expression of TNFα increases, in part due to accumulation of advanced glycation end-product (AGEs), and is associated with superoxide (O2−) production and vascular oxidative stress [41–43]. The oxidative stress in the vessel walls is likely caused and/or exacerbated by NADPH oxidases, xanthine oxidase and uncoupled NOS [44–46]. The increase in NADPH-dependent free radical production is involved in the biotransformation of NO into tissue reactive and harmful nitrogenous species including peroxynitrite (OONO−). As a result of this TNFα-induced NO depletion and upregulation of pro-inflammatory gene expression, the vasculature is unable to optimally maintain its ability to relax and becomes exposed to the onset of vascular diseases including atherogenesis, thrombosis, vascular inflammation and fibrosis. By contrast, anti-TNFα treatment suppresses several markers of endothelial dysfunction including oxidative stress, pro-apoptotic markers and pro-inflammatory gene expression including iNOS. As a result, response of the endothelium to vasoactive molecules such as acetylcholine is improved [47].
Nitric oxide synthases
In mammalian cells, three isoforms of NOS are differentially expressed in neurons (neuronal NOS; nNOS), immune cells (inducible NOS; iNOS) and vascular cells (endothelial NOS; eNOS) [48–50]. In the cardiovascular system, eNOS is a multisubstrate enzyme and plays a significant role in catalyzing the production of NO from its substrate L-arginine in the presence of cosubstrates and cofactors [49]. Bioactive eNOS is tightly regulated and requires dimerization and phosphorylation by a protein kinase [51]. The eNOS-derived NO is multifunctional and significantly contributes to vascular homeostasis including atheroprotection, inhibition of vascular inflammation, and suppression of neointimal lesion and thickening. These protective effects of NO are important in opposing vascular diseases such as restenosis, atherosclerosis and vasculopathy. Aging of the vascular system disrupts many of these physiological processes and causes and/or accelerates eNOS uncoupling where the enzyme is involved in generating superoxide radicals and inducing vascular oxidative stress. In addition, eNOS expression and/or activity are impaired by cytokines that are pathologically upregulated with advancing age. For example, in aortic and microvascular ECs, cytokines such as TNFα and IL1β selectively downregulate eNOS expression and upregulate iNOS levels. These imbalances in NOS expression reduce bioactive NO and increase iNOS-driven OONO− and ROS production to favor vascular oxidative and nitrosative stress and eventually lead to endothelial dysfunction [52–54]. By contrast, inhibition of iNOS expression in aged animals reduced nitrosative stress and reversed endothelial dysfunction [55].
Other age-associated factors that influence NOS expression and/or activity to quench NO levels include: i) reduction in the levels of NOS cosubstrates and cofactors including flavin adenine dinucleotide (FAD), Flavin mononucleotide (FMN) and tetrahydrobiopterin (BH4) [49]; ii) increased arginase activity and alternate metabolism of L-arginine [56]; iii) replicative senescence of vascular cells including endothelial and smooth muscle cells [57–59]; and iv) elevation of asymmetric dimethylarginine (ADMA) levels [60,61]. ADMA is a methylated arginine that endogenously and competitively inhibits eNOS to reduce bioavailability of NO and accelerate endothelial cell senescence [62]. Plasma level of ADMA is an independent predictor of major adverse cardiovascular events [63]. Physiologically, ADMA is metabolized by dimethylarginine dimethylaminohydrolase (DDAH) [64]. However, DDAH expression and/or activity is impaired by oxidative stress including oxidized lipids and TNFα [64,65]. Thus, each of these factors could lead to increased vascular stiffness, reduced endothelium-dependent vasodilation and accelerated vascular dysfunction.
MicroRNAs
MicroRNAs (miRNAs), single-stranded RNAs of about 25 nucleotides that endogenously suppress protein expression by destabilizing target mRNAs, play profound role in the pathobiology of the cardiovascular system. Several gain- and loss- of function preclinical studies have shown that miRNAs are useful in understanding molecular mechanisms of cardiovascular disease and as novel drug targets to treat cardiac and vascular pathologies. In addition, pharmacologic manipulation of miRNAs using oligonucleotides have shown some promise in attenuating cardiovascular disease and in defining a path for miRNA-based therapeutics. Mechanistically, miRNAs interact with Argonaute (AGO) protein that is complexed with RNA-induced silencing complex (RISC) proteins in the cytosol of cells in order to recognize and target the 3′ untranslated regions (UTRs) of mRNA transcripts and inhibit their protein translation; several targets at a time. In order to mount their sustained effect in the cardiovascular system, miRNAs are loaded into vesicles, lipid particles and exosomes before being released into the bloodstream. Of the nearly 1000 miRNAs in the human genome, several are implicated in the pathogenesis of heart and vascular disorders including angiogenesis, vessel growth, inflammation and fibrosis. Some of the well-characterized vascular miRNAs include miR-17-92 cluster, miR-29, miR-30, miR-31, miR-34a, miR-43a, miR-126, miR-143, miR-145, miR-146 family, miR-216, miR-217 and miR-299 [66–68]. Each of these miRNAs target critical cellular processes that are involved in senescence.
During endothelial senescence and dysfunction, the family members of miR-29 and miR-34a are significantly upregulated. For example, the miR-29 family of miRNAs is overexpressed in senescent ECs and cardiovascular tissue [69,70] likely due to DNA damage-mediated dysregulation of tumor suppressor mechanisms and cell senescence mediators [71,72]. In a senescence mouse model of Klotho-deficiency, induction of miR-29 expression was associated with decreased expression of matrix proteins and accelerated tissue aging [70]. Similarly, miR-34a overexpression inhibits EC proliferation and induces senescence by suppressing the expression of sirtuin 1 (SIRT1); a histone deacetylase that controls various cellular processes including cellular plasticity and senescence [73]. In addition, the expression of miR-34a is upregulated in tissues explanted from older animals [73–76].
Sex steroid hormones
Chronological and vascular aging are known to be distinctively regulated in men and women. This gender-based difference in vascular (dys)function culminates to differences in cardiovascular risk [77,78]. Sex hormones in general, and estrogen and testosterone in particular are primarily implicated in these pathophysiological differences. Several clinical studies indicate that estrogen plays a protective role in women during their child-bearing age. As a result, the prevalence of heart disease is differentially higher in men than women until at least menopause and advancing age dampen endogenous estrogen production and negate the differences [78]. In this regard, other studies also report that estrogen has vasoprotective function in premenopausal women [79–81]. As part of this protective mechanism, it has been demonstrated that estrogen increases the expression and activity of eNOS [82], reduces ADMA levels [83] and scavenges free radicals [84]. This modulation of endothelium-derived vasoactive molecules together with the action of estrogen on lipid metabolism may be the mechanism of action for estrogen’s cardioprotective effect.
In a mechanistic study to understand the vascular effect of estrogen pre- and post-menopause, Novella et al. [85] exposed uterine arteries from postmenopausal women to vehicle, synthetic estrogen or raloxifene (anti-estrogenic molecule on the uterus). The data from this study shows that estrogen reduced the levels of several classic proinflammatory markers including TNFα and IL1β. Interestingly, this study revealed biphasic effect of estrogen as a function of aging where 5 years postmenopausal age was associated with a reversed function of estrogen from anti-inflammatory to a pro-inflammatory modulator of vascular inflammation. This switched effect of estrogen has been linked to increased expression of estrogen receptors with aging [85]. This phenomenon likely explains the mixed effect of estrogen replacement therapy in aged postmenopausal women [86,87].
Meanwhile, some studies have reported that testosterone induces endothelium-independent relaxation of vascular beds [88,89] and endothelial release of NO through extracellular signal-regulated kinase (ERK)/mitogen-associated protein kinase (MAPK) pathway [90]. The later effect is likely mediated by the endogenous conversion of testosterone into estrogen [91]. With aging, testosterone levels decrease by about 2% per year and this sustained reduction may contribute to vascular aging. This possibility is supported by preclinical data that found resistance of vessels isolated from aged animals to testosterone-mediated vasodilation compared to blood vessels from younger animals [92] and by clinical data that demonstrate regulation of vascular function by testosterone replacement therapy [93,94].
Endothelial progenitor cells
Endothelial progenitor cells (EPCs) are presumed as the precursor cells for mature ECs and are, albeit controversially, reported to be involved in the repair and regeneration of denuded endothelium including in neovascularization [95,96]. EPCs, characterized by the expression of a set of molecular markers including CD34, CD133 and KDR, are normally isolated from bone marrow and blood (peripheral or umbilical cord). In vitro, they can be differentiated into mature CD31-expressing ECs in the presence of appropriate growth factors including VEGF, FGF and EGF [97]. In vivo, EPCs secrete angiogenic factors such as VEGF and HGF, migrate and adhere to injured vessels to promote revascularization and repair of ischemic tissue [98]. Several studies report that the number and function of EPCs including their proliferative and migratory capacity is reduced with age in part due to activation of pro-senescent and pro-oxidant pathways [99]. In addition, cardiovascular risk factors such as diabetes, atherosclerosis and hypertension also accelerate premature senescence of EPCs and impair the function of mature ECs [100]. As a result, injury to the endothelium fails to physiologically repair in older subjects or patients with cardiovascular disease.
In a mouse model of hindlimb ischemia, transplantation of bone marrow-derived EPC-like cells isolated from patients with chronic ischemic cardiomyopathy showed poor function in restoring tissue perfusion compared to the same number of cells isolated from normal subjects [101]. Clinically, transplantation of EPCs in patients with peripheral arterial disease (PAD) have been demonstrated to increase the number of collateral vessels, and improve blood flow [102].
Overall, based on preclinical and early phase clinical studies, it appears that EPCs actively participate in vascular homeostasis, and their function is significantly impaired by age and other cardiovascular risk factors in part due to suppression of angiogenic cytokines and growth factors, as well as co-influence of age and cardiovascular disease on EPC senescence including telomere length and antioxidant defense mechanisms. In this regard, several studies demonstrated that there is increased loss of telomere length and/or upregulated expression of senescence markers in EPCs treated with pro-oxidant molecules such as high glucose, angiotensin II and oxidized LDL [102]. By contrast, treatment with antioxidants or forced expression of telomerase increases EPC proliferation and vasculogenesis [103,104].
Progeroid syndromes and the endothelium
Premature aging syndromes such as Fanconi anemia, dyskeratosis congenita (DKC), Hutchinson-Gilford progeria syndrome (HGPS), Bloom syndrome (BS), Cockayne syndrome (CS) and Werner syndrome (WRN) are characterized by accelerated aging phenotype that affects several mesodermal tissue types including the vascular endothelium. One common feature of all these syndromes is that they result from genetic mutations of corresponding genes encoding DNA repair machinery or translation of lamin A protein (progerin); as in HGPS [105]. In HGPS, cardiovascular disease is the leading cause of death in part due to derangement of vascular tissue including decellularization of the intimal and medial layer and calcification of the vessel wall [106,107]. In this regard, the transgenic mouse model created by Francis Collins’ group at the NIH [107] provided significant insights into understanding the vascular pathobiology of human progerin overexpression. Structurally, examination of blood vessels revealed that the medial layer became thick and lost its resident vascular smooth muscle cells. In addition, the explanted arteries were found to be calcified and fibrosed [107]. Functionally, the blood vessels lacked response to the vasoactive molecule sodium nitroprusside.
Mechanistically, HGPS is caused by accumulation of truncated lamin A protein that has a farnesyl modification [108–110]. The truncation and uncleaved farnesyl moiety impedes the protein from being released out of the nuclear membrane causing destabilization of the nuclei, DNA damage, oxidative stress and telomere erosion [111]. Recently, pharmacological agents that block the farnesylation of lamin A precursor (prelamin A) and its truncated version progerin have been developed and shown to reduce many of the cardiovascular features seen in progeroid children [112–114].
Diet, exercise and vascular health
The pathobiologic effect of metabolic diseases such as atherosclerosis and diabetes on the cardiovascular system in general, and the endothelium in particular is well characterized [115]. As such, hypercholesterolemia and hyperglycemia have long been known to induce oxidative stress, promote vascular inflammation, and increase the risk of coronary arterial disease [115,116]. For example, high-fat diet has been shown to impair vascular function, and dyslipidemic patients have more severe endothelial dysfunction than healthy controls with normal baseline plasma triglyceride profile [117]. Dysfunctional endothelium increases the risk of developing insulin resistance, which further augments the risk for hypertension, type 2 diabetes and other metabolic syndromes [116,118].
In diabetics, high-fat and/or carbohydrate-enriched diet increase circulating levels of several pro-inflammatory molecules including iNOS, TNFα, interleukins and adhesion molecules; chemicals that are known to potentiate processes involved in endothelial dysfunction including vascular inflammation and senescence [119]. By contrast, inhibition of these pro-inflammatory cytokines using antibodies or small molecules have been shown to reduce adhesion of inflammatory cells into ECs and restore endothelial responsiveness to vasoactive molecules [47,120].
While high fat/carbohydrate diet may accelerate endothelial dysfunction, epidemiological studies have mounted evidence that traditional Mediterranean diets that limit saturated fats, and enrich fruits and leafy green vegetables reduce endothelial dysfunction and cardiovascular risk [121].
In addition to plant-based diets and pharmacological therapy, regular physical exercise (45 min to 1 hour per day to burn about 300 Kcal of energy) has been shown to reduce levels of circulating proinflammatory molecules and favor sustained release of endogenous factors that are associated with good endothelial health including anti-inflammatory molecules, antioxidants, hormones and vasodilators such as NO, prostacyclin and adenosine. Among the mechanisms by which physical exercise improves vascular health are induction of laminar shear stress and improved blood flow [122–124]. These are endothelial-dependent mechanisms that significantly affect vascular structure and function including favorable changes in vessel diameter, as well as endothelial NOS expression and activity [125].
Regular physical exercise has therefore been linked to lean body mass, normal blood pressure, improved plasma sugar, insulin and lipid profiles [126–128]. Accordingly, physically active individuals have relatively reduced loss of vascular function and lower risk of cardiovascular morbidity and mortality [129,130].
Pharmacological regulation of vascular senescence and aging
Several molecular and cell biological studies have unraveled genes and pathways that drive and/or accelerate vascular senescence [131,132]. The studies have also identified druggable targets to improve vascular compliance including endothelium-dependent vasodilation, and thereby reduce cardiovascular morbidity. By extension, preclinical and clinical studies have tested the efficacy of several FDA-approved drugs and new chemical entities (NCEs) to modify chronological aging- or premature aging-associated vascular dysfunction.
Among the mainstream targets of currently pursued drug therapy are the NOS pathway, cyclooxygenase (COX) pathway, the renin-angiotensin system (RAS), pro-inflammatory pathways and telomerase [40,131,133]. One common goal of these therapeutic modalities is to preserve or improve vascular function and structure by suppressing interdependent processes including oxidative stress, inflammation and telomere attrition. For example, HMG-CoA reductase inhibitors (e.g. statins) have been shown to prevent senescence and improve proliferative capacity of EPCs through modulation of cell cycle genes, pro-oxidants, and pro-inflammatory pathways [134,135]. Similarly, the COX-2 inhibitor aspirin has been reported to attenuate replicative senescence of ECs through inhibition of oxidative stress, as well as induction of NO. Interestingly, the effect of aspirin on NO was found to be due to modulation of the endogenous NOS inhibitor ADMA [136]. Another study has demonstrated that ADMA induces vascular senescence by accelerating telomere shortening and reducing telomerase activity in ECs [62].
In addition to HMG-CoA reductase and COX inhibitors, inhibitors of RAS have shown some beneficial effect on the vascular system. Treatment of vascular cells with angiotensin II (Ang II) accelerates senescence and its pharmacological inhibition with olmesartan prevents the onset of Ang II-induced vascular inflammation and premature senescence [137]. Clinical studies also showed that treatment with valsartan (Ang II inhibitor) or quinapril (ACE inhibitor) improved vascular compliance in elderly subjects [133,138]. Among the pleiotropic mechanisms of statins and ACE inhibitors in modulating vascular inflammation is the inhibition of circulating TNFα levels [139,140]. In this regard, several TNFα inhibitors including etanercept and infliximab have been demonstrated to inhibit intravascular TNFα and reverse endothelial dysfunction [141,142].
In principle, another intriguing target to slow or reverse vascular aging is the telomerase enzyme complex including telomerase reverse transcriptase (TERT), telomerase RNA (TERC), dyskerin, and subunits of the shelterin complex. This conviction stems from the common occurrence of telomere shortening with advancing age or in premature aging syndromes [143]. Short telomeres increase the likelihood of DNA damage, genomic instability and mutagenesis. In addition, almost every post-mitotic cell type, with the exception of germline cells, express negligible levels of telomerase rendering them to be exquisitely susceptible to telomere-dependent replicative senescence; a phenotype that enhances the generation of ROS and pro-inflammatory molecules in vascular cells [58,144]. By contrast, endothelium-derived NO delays the onset of EC senescence through TERT activation [145]. Proof-of-concept genetic studies have reported that TERT reactivation increases longevity and favorably modulates cardiovascular disease including insulin sensitivity [146]. Similarly, activation of telomerase using phytochemicals such as resveratrol has been reported to delay EPC senescence and improve their proliferative and migratory capacity [147].
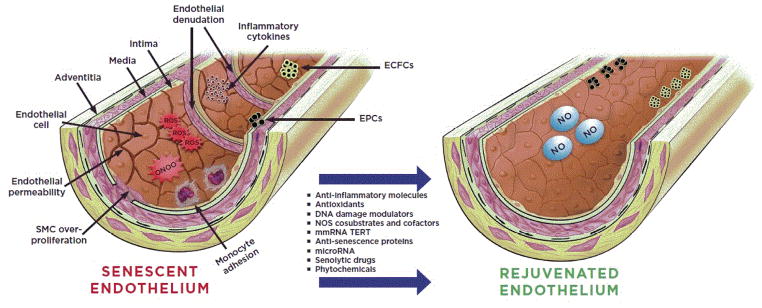
More recently, it has been demonstrated that introduction of exogenously expressed TERT in the form of modified messenger RNA (mmRNA) increases TERT enzymatic activity and transiently extends telomere length in primary human cells [148]. This technology may be able to delay cellular and tissue senescence, and increase the proliferative capacity of cells without immortal transformation. Systemic and transient delivery of such mmRNA formulated with suitable carriers to senescent endothelium is expected to slow or even reverse vascular aging and dysfunction (Figure 1).
Figure 1.
Senescence and rejuvenation of vascular endothelium. A) Aging or vascular injury contributes to endothelial dysfunction and senescence including increased endothelial permeability, over-proliferation of smooth muscle cells (SMCs), adhesion of inflammatory monocytes, accumulation of reactive oxygen species (ROS), peroxynitrite (OONO−), and inflammatory cytokines. In addition, the number of endothelial precursor cell reserve such as endothelial progenitor cells (EPCs) and endothelial colony-forming cells (ECFCs) is markedly reduced. In B) a rejuvenated vascular endothelium, as a result of pharmacological intervention, characterized by continuous monolayer of endothelial cells and production of beneficial vasoactive molecules such as nitric oxide (NO), as well as enriched EPCs and ECFCs is shown.
Conclusion and Perspectives
Currently, considerable efforts are being made to delay aging and age-associated diseases including cardiovascular morbidity. Endothelial dysfunction is one of the earliest indicators of cardiovascular disease. In line with this, the endothelium has emerged as one of the most important targets for the prevention and treatment of cardiovascular disease including hypertension, diabetes, atherosclerosis, and insulin resistance syndrome. ECs, mature or progenitor, are the building blocks of the vascular endothelium and are involved in active secretion of paracrine factors to modulate vascular homeostasis. Unfortunately, aging exerts several pathological changes in the vascular system including apoptosis, inflammation, DNA damage and telomere attrition. As a result, ECs lose their ability to proliferate and secrete vasoactive molecules. Several of the existing strategies attempt to restore key EC functions including production of NO (through exogenous supplementation or reactivation of co-substrates and cofactors) and other vasodilators while decreasing inflammation, oxidative and nitrosative stress through anti-inflammatory, antioxidants and restoration of eNOS coupling. However, these strategies have not been able to rejuvenate denuded or senescent endothelium in a meaningfully way.
In order to effectively overcome the exhausted number and function of mature ECs, endothelial lineage progenitors such as EPCs and endothelial colony-forming cells (ECFCs) [149,150] may be isolated from circulation or from niches within the vascular wall and rejuvenated through ectopic expression of factors that halt senescence and other age-associated phenotypes. In this regard, transient extension of telomere length through non-viral and non-integrating approaches ex vivo is particularly appealing. This cell-based strategy may be combined with other mechanisms involved in the regulation of cellular senescence such as microRNA, senolytic drugs and/or NCEs that modulate DNA damage repair for preventative or therapeutic vascular rejuvenation (Figure 1).
Acknowledgments
Funding Support
YTG was a recipient of the Stanford School of Medicine Dean’s fellowship (grant number 1049528-149-KAVFB), Stanford SPARK Translational Research Program, the Tobacco-Related Disease Research Program of the University of California (grant number 20FT-0090) and the Houston Methodist Research Institute (project ID 25150001). He is currently supported by NHLBI (grant number K01HL118683), by the Caroline Weiss Law Fund for Research in Molecular Medicine at Baylor College of Medicine (BCM), and by intramural funding from BCM.
Footnotes
Disclosure
YTG is an inventor on patents, owned by Stanford University, that protect the use of NOS/ADMA/DDAH modulators for therapeutic use. He is also a co-founder of Altitude Pharma, Inc; a biotechnology Company that is developing therapeutic products for airway diseases. YTG and EY are co-founders of phaRNA comprehensive RNA Technology including mmRNA-based therapeutics.
References
- 1.National Institutes of Aging. Blood Vessels and Aging: The Rest of the Journey in Health and Aging 2005 [Google Scholar]
- 2.Capell BC, Collins FS, Nabel EG. Mechanisms of cardiovascular disease in accelerated aging syndromes. Circ Res. 2007;101:13–26. doi: 10.1161/CIRCRESAHA.107.153692. [DOI] [PubMed] [Google Scholar]
- 3.Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a “set up” for vascular disease. Circulation. 2003;107:139–146. doi: 10.1161/01.cir.0000048892.83521.58. [DOI] [PubMed] [Google Scholar]
- 4.Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation. 2003;107:346–354. doi: 10.1161/01.cir.0000048893.62841.f7. [DOI] [PubMed] [Google Scholar]
- 5.Ferrari AU, Radaelli A, Centola M. Invited review: aging and the cardiovascular system. J Appl Physiol. 2003;95:2591–2597. doi: 10.1152/japplphysiol.00601.2003. [DOI] [PubMed] [Google Scholar]
- 6.Minamino T, Komuro I. Vascular aging: insights from studies on cellular senescence, stem cell aging, and progeroid syndromes. Nat Clin Pract Cardiovasc Med. 2008;5:637–48. doi: 10.1038/ncpcardio1324. [DOI] [PubMed] [Google Scholar]
- 7.Wolinsky H. A proposal linking clearance of circulating lipoproteins to tissue metabolic activity as a basis for understanding atherogenesis. Circ Res. 1980;47:301–311. doi: 10.1161/01.res.47.3.301. [DOI] [PubMed] [Google Scholar]
- 8.Aird WC. Spatial and temporal dynamics of the endothelium. J Thromb Haemost. 2005;3:1392–406. doi: 10.1111/j.1538-7836.2005.01328.x. [DOI] [PubMed] [Google Scholar]
- 9.Galley HF, Webster NR. Physiology of the endothelium. Br J Anaesth. 2004;93:105–113. doi: 10.1093/bja/aeh163. [DOI] [PubMed] [Google Scholar]
- 10.Cines DB, Pollak ES, Buck CA, Loscalzo J, Zimmerman GA, et al. Endothelial cells in physiology and in the pathophysiology of vascular disorders. Blood. 1998;91:3527–3561. [PubMed] [Google Scholar]
- 11.Brandes RP, Fleming I, Busse R. Endothelial aging. Cardiovasc Res. 2005;66:286–294. doi: 10.1016/j.cardiores.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 12.Feletou M, Vanhoutte PM. Endothelial dysfunction: a multifaceted disorder (The Wiggers Award Lecture) Am J Physiol Heart Circ Physiol. 2006;291:H985–1002. doi: 10.1152/ajpheart.00292.2006. [DOI] [PubMed] [Google Scholar]
- 13.Paris F, Fuks Z, Kang A, Capodieci P, Juan G, et al. Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science. 2001;293:293–297. doi: 10.1126/science.1060191. [DOI] [PubMed] [Google Scholar]
- 14.Folkman J, Camphausen K. What does radiotherapy do to endothelial cells? Science. 2001;293:227–228. doi: 10.1126/science.1062892. [DOI] [PubMed] [Google Scholar]
- 15.Dong X, Tong F, Qian C, Zhang R, Dong J, et al. NEMO modulates radiation-induced endothelial senescence of human umbilical veins through NF-kappaB signal pathway. Radiat Res. 2015;183:82–93. doi: 10.1667/RR13682.1. [DOI] [PubMed] [Google Scholar]
- 16.Yeh ET, Tong AT, Lenihan DJ, Yusuf SW, Swafford J, et al. Cardiovascular complications of cancer therapy: diagnosis, pathogenesis, and management. Circulation. 2004;109:3122–3131. doi: 10.1161/01.CIR.0000133187.74800.B9. [DOI] [PubMed] [Google Scholar]
- 17.Chatterjee K, Zhang J, Honbo N, Karliner JS. Doxorubicin cardiomyopathy. Cardiology. 2010;115:155–162. doi: 10.1159/000265166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patane S. Cardiotoxicity: cisplatin and long-term cancer survivors. Int J Cardiol. 2014;175:201–202. doi: 10.1016/j.ijcard.2014.04.238. [DOI] [PubMed] [Google Scholar]
- 19.Brosius FC, Waller BF, Roberts WC. Radiation heart disease. Analysis of 16 young (aged 15 to 33 years) necropsy patients who received over 3,500 rads to the heart. Am J Med. 1981;70:519–530. doi: 10.1016/0002-9343(81)90574-x. [DOI] [PubMed] [Google Scholar]
- 20.Veinot JP, Edwards WD. Pathology of radiation-induced heart disease: a surgical and autopsy study of 27 cases. Hum Pathol. 1996;27:766–773. doi: 10.1016/s0046-8177(96)90447-5. [DOI] [PubMed] [Google Scholar]
- 21.Orzan F, Brusca A, Conte MR, Presbitero P, Figliomeni MC. Severe coronary artery disease after radiation therapy of the chest and mediastinum: clinical presentation and treatment. Br Heart J. 1993;69:496–500. doi: 10.1136/hrt.69.6.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinto E. Blood pressure and ageing. Postgrad Med J. 2007;83:109–114. doi: 10.1136/pgmj.2006.048371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barzilai N, Huffman DM, Muzumdar RH, Bartke A. The critical role of metabolic pathways in aging. Diabetes. 2012;61:1315–1322. doi: 10.2337/db11-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang JC, Bennett M. Aging and atherosclerosis: mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ Res. 2012;111:245–259. doi: 10.1161/CIRCRESAHA.111.261388. [DOI] [PubMed] [Google Scholar]
- 25.Park JE, Keller GA, Ferrara N. The vascular endothelial growth factor (VEGF) isoforms: differential deposition into the subepithelial extracellular matrix and bioactivity of extracellular matrix-bound VEGF. Mol Biol Cell. 1993;4:1317–1326. doi: 10.1091/mbc.4.12.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA. Vascular endothelial growth factor and angiogenesis. Pharmacol Rev. 2004;56:549–580. doi: 10.1124/pr.56.4.3. [DOI] [PubMed] [Google Scholar]
- 27.Carmeliet P, Ferreira V, Breier G, Pollefeyt S, Kieckens L, et al. Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele. Nature. 1996;380:435–439. doi: 10.1038/380435a0. [DOI] [PubMed] [Google Scholar]
- 28.Ferrara N, Carver-Moore K, Chen H, Dowd M, Lu L, et al. Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature. 1996;380:439–442. doi: 10.1038/380439a0. [DOI] [PubMed] [Google Scholar]
- 29.Fong GH, Rossant J, Gertsenstein M, Breitman ML. Role of the Flt-1 receptor tyrosine kinase in regulating the assembly of vascular endothelium. Nature. 1995;376:66–70. doi: 10.1038/376066a0. [DOI] [PubMed] [Google Scholar]
- 30.Shalaby F, Rossant J, Yamaguchi TP, Gertsenstein M, Wu XF, et al. Failure of blood-island formation and vasculogenesis in Flk-1-deficient mice. Nature. 1995;376:62–66. doi: 10.1038/376062a0. [DOI] [PubMed] [Google Scholar]
- 31.Ahluwalia A, Jones MK, Szabo S, Tarnawski AS. Aging impairs transcriptional regulation of vascular endothelial growth factor in human microvascular endothelial cells: implications for angiogenesis and cell survival. J Physiol Pharmacol. 2014;65:209–215. [PubMed] [Google Scholar]
- 32.Besse S, Boucher F, Linguet G, Riou L, De Leiris J, et al. Intramyocardial protein therapy with vascular endothelial growth factor (VEGF-165) induces functional angiogenesis in rat senescent myocardium. J Physiol Pharmacol. 2010;61:651–661. [PubMed] [Google Scholar]
- 33.Chen H, Gu X, Liu Y, Wang J, Wirt SE, et al. PDGF signalling controls age-dependent proliferation in pancreatic beta-cells. Nature. 2011;478:349–355. doi: 10.1038/nature10502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murakami M, Nguyen LT, Zhuang ZW, Moodie KL, Carmeliet P, et al. The FGF system has a key role in regulating vascular integrity. J Clin Invest. 2008;118:3355–3366. doi: 10.1172/JCI35298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coutu DL, Galipeau J. Roles of FGF signaling in stem cell self-renewal, senescence and aging. Aging (Albany NY) 2011;3:920–933. doi: 10.18632/aging.100369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li J, Perrella MA, Tsai JC, Yet SF, Hsieh CM, et al. Induction of vascular endothelial growth factor gene expression by interleukin-1 beta in rat aortic smooth muscle cells. J Biol Chem. 1995;270:308–312. doi: 10.1074/jbc.270.1.308. [DOI] [PubMed] [Google Scholar]
- 37.Cohen T, Nahari D, Cerem LW, Neufeld G, Levi BZ. Interleukin 6 induces the expression of vascular endothelial growth factor. J Biol Chem. 1996;271:736–741. doi: 10.1074/jbc.271.2.736. [DOI] [PubMed] [Google Scholar]
- 38.Matsumoto K, Ohi H, Kanmatsuse K. Interleukin 10 and interleukin 13 synergize to inhibit vascular permeability factor release by peripheral blood mononuclear cells from patients with lipoid nephrosis. Nephron. 1997;77:212–218. doi: 10.1159/000190275. [DOI] [PubMed] [Google Scholar]
- 39.Ohba T, Haro H, Ando T, Wako M, Suenaga F, et al. TNF-alpha-induced NF-kappaB signaling reverses age-related declines in VEGF induction and angiogenic activity in intervertebral disc tissues. J Orthop Res. 2009;27:229–235. doi: 10.1002/jor.20727. [DOI] [PubMed] [Google Scholar]
- 40.Zhang H, Park Y, Wu J, Chen X, Lee S, et al. Role of TNF-alpha in vascular dysfunction. Clin Sci (Lond) 2009;116:219–230. doi: 10.1042/CS20080196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Csiszar A, Ungvari Z, Koller A, Edwards JG, Kaley G. Proinflammatory phenotype of coronary arteries promotes endothelial apoptosis in aging. Physiol Genomics. 2004;17:21–30. doi: 10.1152/physiolgenomics.00136.2003. [DOI] [PubMed] [Google Scholar]
- 42.Bruunsgaard H, Skinhoj P, Pedersen AN, Schroll M, Pedersen BK. Ageing, tumour necrosis factor-alpha (TNF-alpha) and atherosclerosis. Clin Exp Immunol. 2000;121:255–260. doi: 10.1046/j.1365-2249.2000.01281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kirwan JP, Krishnan RK, Weaver JA, Del Aguila LF, Evans WJ. Human aging is associated with altered TNF-alpha production during hyperglycemia and hyperinsulinemia. Am J Physiol Endocrinol Metab. 2001;281:E1137–E1143. doi: 10.1152/ajpendo.2001.281.6.E1137. [DOI] [PubMed] [Google Scholar]
- 44.Cave AC, Brewer AC, Narayanapanicker A, Ray R, Grieve DJ, et al. NADPH oxidases in cardiovascular health and disease. Antioxid Redox Signal. 2006;8:691–728. doi: 10.1089/ars.2006.8.691. [DOI] [PubMed] [Google Scholar]
- 45.Minhas KM, Saraiva RM, Schuleri KH, Lehrke S, Zheng M, et al. Xanthine oxidoreductase inhibition causes reverse remodeling in rats with dilated cardiomyopathy. Circ Res. 2006;98:271–279. doi: 10.1161/01.RES.0000200181.59551.71. [DOI] [PubMed] [Google Scholar]
- 46.Thum T, Fraccarollo D, Schultheiss M, Froese S, Galuppo P, et al. Endothelial nitric oxide synthase uncoupling impairs endothelial progenitor cell mobilization and function in diabetes. Diabetes. 2007;56:666–674. doi: 10.2337/db06-0699. [DOI] [PubMed] [Google Scholar]
- 47.Csiszar A, Labinskyy N, Smith K, Rivera A, Orosz Z, et al. Vasculoprotective effects of anti-tumor necrosis factor-alpha treatment in aging. Am J Pathol. 2007;170:388–398. doi: 10.2353/ajpath.2007.060708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Forstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012;33:829–837. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sukhovershin RA, Yepuri G, Ghebremariam YT. Endothelium-Derived Nitric Oxide as an Antiatherogenic Mechanism: Implications for Therapy. Methodist Debakey Cardiovasc J. 2015;11:166–71. doi: 10.14797/mdcj-11-3-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lai L, Ghebremariam YT. Modulating DDAH/NOS Pathway to Discover Vasoprotective Insulin Sensitizers. J Diabetes Res. 2016;2016:1982096. doi: 10.1155/2016/1982096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R, et al. Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature. 1999;399:601–605. doi: 10.1038/21224. [DOI] [PubMed] [Google Scholar]
- 52.MacNaul K, Hutchinson NI. Differential expression of iNOS and cNOS mRNA in human vascular smooth muscle cells and endothelial cells under normal and inflammatory conditions. Biochem Biophys Res Commun. 1993;196:1330–1334. doi: 10.1006/bbrc.1993.2398. [DOI] [PubMed] [Google Scholar]
- 53.Anderson HD, Rahmutula D, Gardner DG. Tumor necrosis factor-alpha inhibits endothelial nitric-oxide synthase gene promoter activity in bovine aortic endothelial cells. J Biol Chem. 2004;279:963–969. doi: 10.1074/jbc.M309552200. [DOI] [PubMed] [Google Scholar]
- 54.Yan G, You B, Chen SP, Liao JK, Sun J. Tumor necrosis factor-alpha downregulates endothelial nitric oxide synthase mRNA stability via translation elongation factor 1-alpha 1. Circ Res. 2008;103:591–597. doi: 10.1161/CIRCRESAHA.108.173963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zanetti M, Gortan Cappellari G, Burekovic I, Barazzoni R, Stebel M, et al. Caloric restriction improves endothelial dysfunction during vascular aging: Effects on nitric oxide synthase isoforms and oxidative stress in rat aorta. Exp Gerontol. 2010;45:848–855. doi: 10.1016/j.exger.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 56.Vanhoutte PM. Arginine and arginase: endothelial NO synthase double crossed? Circ Res. 2008;102:866–868. doi: 10.1161/CIRCRESAHA.108.175570. [DOI] [PubMed] [Google Scholar]
- 57.Erusalimsky JD, Kurz DJ. Cellular senescence in vivo: its relevance in ageing and cardiovascular disease. Exp Gerontol. 2005;40:634–642. doi: 10.1016/j.exger.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 58.Minamino T, Komuro I. Vascular cell senescence: contribution to atherosclerosis. Circ Res. 2007;100:15–26. doi: 10.1161/01.RES.0000256837.40544.4a. [DOI] [PubMed] [Google Scholar]
- 59.Erusalimsky JD, Skene C. Mechanisms of endothelial senescence. Exp Physiol. 2009;94:299–304. doi: 10.1113/expphysiol.2008.043133. [DOI] [PubMed] [Google Scholar]
- 60.Cooke JP. Does ADMA cause endothelial dysfunction? Arterioscler Thromb Vasc Biol. 2000;20:2032–2037. doi: 10.1161/01.atv.20.9.2032. [DOI] [PubMed] [Google Scholar]
- 61.Cooke JP. ADMA: its role in vascular disease. Vasc Med. 2005;10(Suppl 1):S11–S17. doi: 10.1177/1358836X0501000103. [DOI] [PubMed] [Google Scholar]
- 62.Bode-Boger SM, Scalera F, Martens-Lobenhoffer J. Asymmetric dimethylarginine (ADMA) accelerates cell senescence. Vasc Med. 2005;1:S65–71. doi: 10.1177/1358836X0501000110. [DOI] [PubMed] [Google Scholar]
- 63.Mittermayer F, Krzyzanowska K, Exner M, Mlekusch W, Amighi J, et al. Asymmetric dimethylarginine predicts major adverse cardiovascular events in patients with advanced peripheral artery disease. Arterioscler Thromb Vasc Biol. 2006;26:2536–2540. doi: 10.1161/01.ATV.0000242801.38419.48. [DOI] [PubMed] [Google Scholar]
- 64.Palm F, Onozato ML, Luo Z, Wilcox CS. Dimethylarginine dimethylaminohydrolase (DDAH): expression, regulation, and function in the cardiovascular and renal systems. Am J Physiol Heart Circ Physiol. 2007;293:H3227–3245. doi: 10.1152/ajpheart.00998.2007. [DOI] [PubMed] [Google Scholar]
- 65.Ito A, Tsao PS, Adimoolam S, Kimoto M, Ogawa T, et al. Novel mechanism for endothelial dysfunction: dysregulation of dimethylarginine dimethylaminohydrolase. Circulation. 1999;99:3092–3095. doi: 10.1161/01.cir.99.24.3092. [DOI] [PubMed] [Google Scholar]
- 66.Bonauer A, Boon RA, Dimmeler S. Vascular microRNAs. Curr Drug Targets. 2010;11:943–949. doi: 10.2174/138945010791591313. [DOI] [PubMed] [Google Scholar]
- 67.Yamakuchi M. MicroRNAs in Vascular Biology. Int J Vasc Med. 2012;2012:794898. doi: 10.1155/2012/794898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Badi I, Burba I, Ruggeri C, Zeni F, Bertolotti M, et al. MicroRNA-34a Induces Vascular Smooth Muscle Cells Senescence by SIRT1 Downregulation and Promotes the Expression of Age-Associated Pro-inflammatory Secretory Factors. J Gerontol A Biol Sci Med Sci. 2015;70:1304–1311. doi: 10.1093/gerona/glu180. [DOI] [PubMed] [Google Scholar]
- 69.Boon RA, Seeger T, Heydt S, Fischer A, Hergenreider E, et al. MicroRNA-29 in aortic dilation: implications for aneurysm formation. Circ Res. 2011;109:1115–1119. doi: 10.1161/CIRCRESAHA.111.255737. [DOI] [PubMed] [Google Scholar]
- 70.Takahashi M, Eda A, Fukushima T, Hohjoh H. Reduction of type IV collagen by upregulated miR-29 in normal elderly mouse and klotho-deficient, senescence-model mouse. PLoS One. 2012;7:e48974. doi: 10.1371/journal.pone.0048974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martinez I, Cazalla D, Almstead LL, Steitz JA, DiMaio D. miR-29 and miR-30 regulate B-Myb expression during cellular senescence. Proc Natl Acad Sci USA. 2011;108:522–527. doi: 10.1073/pnas.1017346108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wan G, Mathur R, Hu X, Zhang X, Lu X, et al. miRNA response to DNA damage. Trends Biochem Sci. 2011;36:478–484. doi: 10.1016/j.tibs.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ito T, Yagi S, Yamakuchi M. MicroRNA-34a regulation of endothelial senescence. Biochem Biophys Res Commun. 2010;398:735–740. doi: 10.1016/j.bbrc.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 74.Smith-Vikos T, Slack FJ. MicroRNAs and their roles in aging. J Cell Sci. 2012;125:7–17. doi: 10.1242/jcs.099200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smit-McBride Z, Forward KI, Nguyen AT, Bordbari MH, Oltjen SL, et al. Age-dependent increase in miRNA-34a expression in the posterior pole of the mouse eye. Mol Vis. 2014;20:1569–1578. [PMC free article] [PubMed] [Google Scholar]
- 76.Boon RA, Iekushi K, Lechner S, Seeger T, Fischer A, et al. MicroRNA-34a regulates cardiac ageing and function. Nature. 2013;495:107–110. doi: 10.1038/nature11919. [DOI] [PubMed] [Google Scholar]
- 77.Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18:598–602. doi: 10.1007/s12471-010-0841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation. 2011;124:2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shaw LJ, Bairey Merz CN, Pepine CJ, Reis SE, Bittner V, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. 2006;47:S4–S20. doi: 10.1016/j.jacc.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 80.Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. 2006;47:S21–29. doi: 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 81.Xing D, Nozell S, Chen YF, Hage F, Oparil S. Estrogen and mechanisms of vascular protection. Arterioscler Thromb Vasc Biol. 2009;29:289–295. doi: 10.1161/ATVBAHA.108.182279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sumi D, Ignarro LJ. Estrogen-related receptor alpha 1 up-regulates endothelial nitric oxide synthase expression. Proc Natl Acad Sci USA. 2003;100:14451–14456. doi: 10.1073/pnas.2235590100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Holden DP, Cartwright JE, Nussey SS, Whitley GS. Estrogen stimulates dimethylarginine dimethylaminohydrolase activity and the metabolism of asymmetric dimethylarginine. Circulation. 2003;108:1575–1580. doi: 10.1161/01.CIR.0000091083.61609.DF. [DOI] [PubMed] [Google Scholar]
- 84.Ruiz-Larrea MB, Martin C, Martinez R, Navarro R, Lacort M, et al. Antioxidant activities of estrogens against aqueous and lipophilic radicals; differences between phenol and catechol estrogens. Chem Phys Lipids. 2000;105:179–188. doi: 10.1016/s0009-3084(00)00120-1. [DOI] [PubMed] [Google Scholar]
- 85.Novella S, Heras M, Hermenegildo C, Dantas AP. Effects of estrogen on vascular inflammation: a matter of timing. Arterioscler Thromb Vasc Biol. 2012;32:2035–2042. doi: 10.1161/ATVBAHA.112.250308. [DOI] [PubMed] [Google Scholar]
- 86.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 87.Moreau KL, Donato AJ, Seals DR, DeSouza CA, Tanaka H. Regular exercise, hormone replacement therapy and the age-related decline in carotid arterial compliance in healthy women. Cardiovasc Res. 2003;57:861–868. doi: 10.1016/s0008-6363(02)00777-0. [DOI] [PubMed] [Google Scholar]
- 88.Yue P, Chatterjee K, Beale C, Poole-Wilson PA, Collins P. Testosterone relaxes rabbit coronary arteries and aorta. Circulation. 1995;91:1154–1160. doi: 10.1161/01.cir.91.4.1154. [DOI] [PubMed] [Google Scholar]
- 89.Kelly DM, Jones TH. Testosterone: a vascular hormone in health and disease. J Endocrinol. 2013;217:R47–71. doi: 10.1530/JOE-12-0582. [DOI] [PubMed] [Google Scholar]
- 90.Goglia L, Tosi V, Sanchez AM, Flamini MI, Fu XD, et al. Endothelial regulation of eNOS, PAI-1 and t-PA by testosterone and dihydrotestosterone in vitro and in vivo. Mol Hum Reprod. 2010;16:761–769. doi: 10.1093/molehr/gaq049. [DOI] [PubMed] [Google Scholar]
- 91.Longcope C, Kato T, Horton R. Conversion of blood androgens to estrogens in normal adult men and women. J Clin Invest. 1969;48:2191–2201. doi: 10.1172/JCI106185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.English KM, Jones RD, Jones TH, Morice AH, Channer KS. Aging reduces the responsiveness of coronary arteries from male Wistar rats to the vasodilatory action of testosterone. Clin Sci (Lond) 2000;99:77–82. [PubMed] [Google Scholar]
- 93.Khaw KT, Barrett-Connor E. Blood pressure and endogenous testosterone in men: an inverse relationship. J Hypertens. 1988;6:329–332. [PubMed] [Google Scholar]
- 94.Corona G, Petrone L, Fisher AD, Mansani R, Bandini E, et al. Six-month administration of 1% testosterone gel is able to restore erectile function in hypogonadal patients with erectile dysfunction. Arch Ital Urol Androl. 2008;80:103–108. [PubMed] [Google Scholar]
- 95.Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–967. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 96.Yoder MC, Ingram DA. Endothelial progenitor cell: ongoing controversy for defining these cells and their role in neoangiogenesis in the murine system. Curr Opin Hematol. 2009;16:269–273. doi: 10.1097/MOH.0b013e32832bbcab. [DOI] [PubMed] [Google Scholar]
- 97.Caiado F, Dias S. Endothelial progenitor cells and integrins: adhesive needs. Fibrogenesis Tissue Repair. 2012;5:4. doi: 10.1186/1755-1536-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jujo K, Ii M, Losordo DW. Endothelial progenitor cells in neovascularization of infarcted myocardium. J Mol Cell Cardiol. 2008;45:530–544. doi: 10.1016/j.yjmcc.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Williamson K, Stringer SE, Alexander MY. Endothelial progenitor cells enter the aging arena. Front Physiol. 2012;3:30. doi: 10.3389/fphys.2012.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shantsila E, Watson T, Lip GY. Endothelial progenitor cells in cardiovascular disorders. J Am Coll Cardiol. 2007;49:741–752. doi: 10.1016/j.jacc.2006.09.050. [DOI] [PubMed] [Google Scholar]
- 101.Heeschen C, Lehmann R, Honold J, Assmus B, Aicher A, et al. Profoundly reduced neovascularization capacity of bone marrow mononuclear cells derived from patients with chronic ischemic heart disease. Circulation. 2004;109:1615–1622. doi: 10.1161/01.CIR.0000124476.32871.E3. [DOI] [PubMed] [Google Scholar]
- 102.Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani S, et al. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002;360:427–435. doi: 10.1016/S0140-6736(02)09670-8. [DOI] [PubMed] [Google Scholar]
- 103.Fiorito C, Rienzo M, Crimi E, Rossiello R, Balestrieri ML, et al. Antioxidants increase number of progenitor endothelial cells through multiple gene expression pathways. Free Radic Res. 2008;42:754–762. doi: 10.1080/10715760802357057. [DOI] [PubMed] [Google Scholar]
- 104.Murasawa S, Llevadot J, Silver M, Isner JM, Losordo DW, et al. Constitutive human telomerase reverse transcriptase expression enhances regenerative properties of endothelial progenitor cells. Circulation. 2002;106:1133–1139. doi: 10.1161/01.cir.0000027584.85865.b4. [DOI] [PubMed] [Google Scholar]
- 105.Navarro CL, Cau P, Levy N. Molecular bases of progeroid syndromes. Hum Mol Genet. 2006;2:R151–161. doi: 10.1093/hmg/ddl214. [DOI] [PubMed] [Google Scholar]
- 106.Hennekam RC. Hutchinson-Gilford progeria syndrome: review of the phenotype. Am J Med Genet A. 2006;140:2603–2624. doi: 10.1002/ajmg.a.31346. [DOI] [PubMed] [Google Scholar]
- 107.Varga R, Eriksson M, Erdos MR, Olive M, Harten I, et al. Progressive vascular smooth muscle cell defects in a mouse model of Hutchinson-Gilford progeria syndrome. Proc Natl Acad Sci USA. 2006;103:3250–3255. doi: 10.1073/pnas.0600012103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pereira S, Bourgeois P, Navarro C, Esteves-Vieira V, Cau P, et al. HGPS and related premature aging disorders: from genomic identification to the first therapeutic approaches. Mech Ageing Dev. 2008;129:449–459. doi: 10.1016/j.mad.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 109.Eriksson M, Brown WT, Gordon LB, Glynn MW, Singer J, et al. Recurrent de novo point mutations in lamin A cause Hutchinson-Gilford progeria syndrome. Nature. 2003;423:293–298. doi: 10.1038/nature01629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sinha JK, Ghosh S, Raghunath M. Progeria: a rare genetic premature ageing disorder. Indian J Med Res. 2014;139:667–674. [PMC free article] [PubMed] [Google Scholar]
- 111.Decker ML, Chavez E, Vulto I, Lansdorp PM. Telomere length in Hutchinson-Gilford progeria syndrome. Mech Ageing Dev. 2009;130:377–383. doi: 10.1016/j.mad.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 112.Capell BC, Olive M, Erdos MR, Cao K, Faddah DA, et al. A farnesyltransferase inhibitor prevents both the onset and late progression of cardiovascular disease in a progeria mouse model. Proc Natl Acad Sci USA. 2008;105:15902–15907. doi: 10.1073/pnas.0807840105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gordon LB, Kleinman ME, Miller DT, Neuberg DS, Giobbie-Hurder A, et al. Clinical trial of a farnesyltransferase inhibitor in children with Hutchinson-Gilford progeria syndrome. Proc Natl Acad Sci USA. 2012;109:16666–16671. doi: 10.1073/pnas.1202529109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gordon LB, Massaro J, D’Agostino RB, Campbell SE, Brazier J, et al. Impact of farnesylation inhibitors on survival in Hutchinson-Gilford progeria syndrome. Circulation. 2014;130:27–34. doi: 10.1161/CIRCULATIONAHA.113.008285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fornoni A, Raij L. Metabolic syndrome and endothelial dysfunction. Curr Hypertens Rep. 2005;7:88–95. doi: 10.1007/s11906-005-0080-6. [DOI] [PubMed] [Google Scholar]
- 116.Tziomalos K, Athyros VG, Karagiannis A, Mikhailidis DP. Endothelial dysfunction in metabolic syndrome: prevalence, pathogenesis and management. Nutr Metab Cardiovasc Dis. 2010;20:140–146. doi: 10.1016/j.numecd.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 117.Giannattasio C, Zoppo A, Gentile G, Failla M, Capra A, et al. Acute effect of high-fat meal on endothelial function in moderately dyslipidemic subjects. Arterioscler Thromb Vasc Biol. 2005;25:406–410. doi: 10.1161/01.ATV.0000152231.93590.17. [DOI] [PubMed] [Google Scholar]
- 118.Pinkney JH, Stehouwer CD, Coppack SW, Yudkin JS. Endothelial dysfunction: cause of the insulin resistance syndrome. Diabetes. 1997;2:S9–13. doi: 10.2337/diab.46.2.s9. [DOI] [PubMed] [Google Scholar]
- 119.Nappo F, Esposito K, Cioffi M, Giugliano G, Molinari AM, et al. Postprandial endothelial activation in healthy subjects and in type 2 diabetic patients: role of fat and carbohydrate meals. J Am Coll Cardiol. 2002;39:1145–1150. doi: 10.1016/s0735-1097(02)01741-2. [DOI] [PubMed] [Google Scholar]
- 120.Csiszar A, Smith K, Labinskyy N, Orosz Z, Rivera A, et al. Resveratrol attenuates TNF-alpha-induced activation of coronary arterial endothelial cells: role of NF-kappaB inhibition. Am J Physiol Heart Circ Physiol. 2006;291:H1694–699. doi: 10.1152/ajpheart.00340.2006. [DOI] [PubMed] [Google Scholar]
- 121.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. [Google Scholar]
- 122.Francescomarino SD, Sciartilli A, Valerio VD, Baldassarre AD, Gallina S. The effect of physical exercise on endothelial function. Sports Med. 2009;39:797–812. doi: 10.2165/11317750-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 123.Niebauer J, Cooke JP. Cardiovascular effects of exercise: role of endothelial shear stress. J Am Coll Cardiol. 1996;28:1652–1660. doi: 10.1016/S0735-1097(96)00393-2. [DOI] [PubMed] [Google Scholar]
- 124.Maiorana A, O’Driscoll G, Taylor R, Green D. Exercise and the nitric oxide vasodilator system. Sports Med. 2003;33:1013–1035. doi: 10.2165/00007256-200333140-00001. [DOI] [PubMed] [Google Scholar]
- 125.Dyakova EY, Kapilevich LV, Shylko VG, Popov SV, Anfinogenova Y. Physical exercise associated with NO production: signaling pathways and significance in health and disease. Front Cell Dev Biol. 2015;3:19. doi: 10.3389/fcell.2015.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.McTiernan A, Sorensen B, Irwin ML, Morgan A, Yasui Y, et al. Exercise effect on weight and body fat in men and women. Obesity (Silver Spring) 2007;15:1496–1512. doi: 10.1038/oby.2007.178. [DOI] [PubMed] [Google Scholar]
- 127.Marliss EB, Vranic M. Intense exercise has unique effects on both insulin release and its roles in glucoregulation: implications for diabetes. Diabetes. 2002;51:S271–283. doi: 10.2337/diabetes.51.2007.s271. [DOI] [PubMed] [Google Scholar]
- 128.Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, et al. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36:533–553. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 129.Walther C, Gielen S, Hambrecht R. The effect of exercise training on endothelial function in cardiovascular disease in humans. Exerc Sport Sci Rev. 2004;32:129–134. doi: 10.1097/00003677-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 130.Pal S, Radavelli-Bagatini S, Ho S. Potential benefits of exercise on blood pressure and vascular function. J Am Soc Hypertens. 2013;7:494–506. doi: 10.1016/j.jash.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 131.Rodriguez-Manas L, El-Assar M, Vallejo S, Lopez-Doriga P, Solis J, et al. Endothelial dysfunction in aged humans is related with oxidative stress and vascular inflammation. Aging Cell. 2009;8:226–238. doi: 10.1111/j.1474-9726.2009.00466.x. [DOI] [PubMed] [Google Scholar]
- 132.Malinin NL, West XZ, Byzova TV. Oxidation as “the stress of life”. Aging. 2011;3:906–910. doi: 10.18632/aging.100385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rajagopalan S, Kariisa M, Dellegrottaglie S, Bard RL, Kehrer C, et al. Angiotensin receptor blockade improves vascular compliance in healthy normotensive elderly individuals: results from a randomized double-blind placebo-controlled trial. J Clin Hypertens (Greenwich) 2006;8:783–790. doi: 10.1111/j.1524-6175.2006.05797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Assmus B, Urbich C, Aicher A, Hofmann WK, Haendeler J, et al. HMG-CoA reductase inhibitors reduce senescence and increase proliferation of endothelial progenitor cells via regulation of cell cycle regulatory genes. Circ Res. 2003;92:1049–1055. doi: 10.1161/01.RES.0000070067.64040.7C. [DOI] [PubMed] [Google Scholar]
- 135.Margaritis M, Channon KM, Antoniades C. Statins as regulators of redox state in the vascular endothelium: beyond lipid lowering. Antioxid Redox Signal. 2014;20:1198–1215. doi: 10.1089/ars.2013.5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bode-Boger SM, Martens-Lobenhoffer J, Tager M, Schroder H, Scalera F. Aspirin reduces endothelial cell senescence. Biochem Biophys Res Commun. 2005;334:1226–1232. doi: 10.1016/j.bbrc.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 137.Kunieda T, Minamino T, Nishi J, Tateno K, Oyama T, et al. Angiotensin II induces premature senescence of vascular smooth muscle cells and accelerates the development of atherosclerosis via a p21-dependent pathway. Circulation. 2006;114:953–960. doi: 10.1161/CIRCULATIONAHA.106.626606. [DOI] [PubMed] [Google Scholar]
- 138.Mancini GB, Henry GC, Macaya C, O’Neill BJ, Pucillo AL, et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. The TREND (Trial on Reversing ENdothelial Dysfunction) Study. Circulation. 1996;94:258–265. doi: 10.1161/01.cir.94.3.258. [DOI] [PubMed] [Google Scholar]
- 139.Tikiz C, Utuk O, Pirildar T, Bayturan O, Bayindir P, et al. Effects of Angiotensin-converting enzyme inhibition and statin treatment on inflammatory markers and endothelial functions in patients with longterm rheumatoid arthritis. J Rheumatol. 2005;32:2095–2101. [PubMed] [Google Scholar]
- 140.Radaelli A, Loardi C, Cazzaniga M, Balestri G, DeCarlini C, et al. Inflammatory activation during coronary artery surgery and its dose-dependent modulation by statin/ACE-inhibitor combination. Arterioscler Thromb Vasc Biol. 2007;27:2750–2755. doi: 10.1161/ATVBAHA.107.149039. [DOI] [PubMed] [Google Scholar]
- 141.Bilsborough W, Keen H, Taylor A, O’Driscoll GJ, Arnolda L, et al. Anti-tumour necrosis factor-alpha therapy over conventional therapy improves endothelial function in adults with rheumatoid arthritis. Rheumatol Int. 2006;26:1125–1131. doi: 10.1007/s00296-006-0147-y. [DOI] [PubMed] [Google Scholar]
- 142.Cardillo C, Schinzari F, Mores N, Mettimano M, Melina D, et al. Intravascular tumor necrosis factor alpha blockade reverses endothelial dysfunction in rheumatoid arthritis. Clin Pharmacol Ther. 2006;80:275–281. doi: 10.1016/j.clpt.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 143.Shammas MA. Telomeres, lifestyle, cancer, and aging. Curr Opin Clin Nutr Metab Care. 2011;14:28–34. doi: 10.1097/MCO.0b013e32834121b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Minamino T, Miyauchi H, Yoshida T, Tateno K, Komuro I. The role of vascular cell senescence in atherosclerosis: antisenescence as a novel therapeutic strategy for vascular aging. Curr Vasc Pharmacol. 2004;2:141–148. doi: 10.2174/1570161043476393. [DOI] [PubMed] [Google Scholar]
- 145.Vasa M, Breitschopf K, Zeiher AM, Dimmeler S. Nitric oxide activates telomerase and delays endothelial cell senescence. Circ Res. 2000;87:540–542. doi: 10.1161/01.res.87.7.540. [DOI] [PubMed] [Google Scholar]
- 146.Bernardes de Jesus B, Vera E, Schneeberger K, Tejera AM, Ayuso E, et al. Telomerase gene therapy in adult and old mice delays aging and increases longevity without increasing cancer. EMBO Mol Med. 2012;4:691–704. doi: 10.1002/emmm.201200245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Xia L, Wang XX, Hu XS, Guo XG, Shang YP, et al. Resveratrol reduces endothelial progenitor cells senescence through augmentation of telomerase activity by Akt-dependent mechanisms. Br J Pharmacol. 2008;155:387–394. doi: 10.1038/bjp.2008.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ramunas J, Yakubov E, Brady JJ, Corbel SY, Holbrook C, et al. Transient delivery of modified mRNA encoding TERT rapidly extends telomeres in human cells. FASEB J. 2015;29:1930–1939. doi: 10.1096/fj.14-259531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ingram DA, Mead LE, Moore DB, Woodard W, Fenoglio A, et al. Vessel wall-derived endothelial cells rapidly proliferate because they contain a complete hierarchy of endothelial progenitor cells. Blood. 2005;105:2783–2786. doi: 10.1182/blood-2004-08-3057. [DOI] [PubMed] [Google Scholar]
- 150.Yoder MC. Is endothelium the origin of endothelial progenitor cells? Arterioscler Thromb Vasc Biol. 2010;30:1094–1103. doi: 10.1161/ATVBAHA.109.191635. [DOI] [PubMed] [Google Scholar]