Abstract
Purpose:
To investigate the clinical and neuroradiographic features of Chinese patients with optic nerve hypoplasia (ONH).
Methods:
This was a retrospective case series study. The medical records and magnetic resonance imaging (MRI) studies of patients diagnosed with ONH from September 2001 to December 2013 in the neuro-ophthalmology clinic of Taipei Veterans General Hospital were reviewed.
Results:
A total of eight eyes of five patients with ONH were enrolled in this study (1 male, 4 females). The mean age at diagnosis was 14.5 ± 12.0 years (range 0.25–30 years). Ocular examination revealed approximately half of the eyes had tortuous retinal vessels. In MRI studies, all patients had midline brain abnormalities including ectopic posterior pituitary gland (60%), agenesis of septum pellucidum (20%), and Rathke's cleft cyst (20%). Two patients had endocrinopathies—one suffered from hypopituitarism and the other had hyperprolactinemia. Both of them showed ocular findings of tortuous retinal vessels.
Conclusion:
A high prevalence of midline brain abnormalities was noted in ONH patients of Chinese ethnicity. The presence of tortuous retinal vessels in patients with a midline brain anomaly may indicate the occurrence of endocrinopathy.
Keywords: endocrinopathy, magnetic resonance imaging, optic nerve hypoplasia
1. Introduction
Optic nerve hypoplasia (ONH) is one of the leading causes of childhood blindness worldwide.1 It is a congenital anomaly with subnormal numbers of axons in the optic nerve.2 ONH was first described by Schwarz in 1915 or even earlier.3 Reeves subsequently reported an infant with bilateral ONH and absence of septum pellucidum in 1941.4 The clinical spectrum extends to include hypopituitarism after Hoyt et al5 discovered the presence of pituitary dwarfism in ONH patients in 1970. In recent decades, the numbers of reported cases increased with an estimated prevalence of 7.2 per 100,000 in Sweden and of 10.9 per 100,000 in England (2006).6,7 Studies regarding ONH mainly concern western society, whereas reports from Asian countries are scarce.4
The purpose of this study was to investigate the clinical and neuroradiographic features of Chinese patients with ONH in Taiwan.
2. Methods
We conducted a retrospective study of patients diagnosed with ONH from September 2001 to November 2013 in the neuro-ophthalmology clinic of Taipei Veterans General Hospital, Taipei, Taiwan. All case participants were Taiwan residents of Chinese ethnicity. The study protocol complied with the provisions of the Declaration of Helsinki, and was approved by the institutional review boards of the hospital.
All patients received comprehensive examination by one neuro-ophthalmologist (A.-G. Wang). The diagnosis of ONH was defined as a ratio of ≤0.35 for the horizontal disc diameter/disc-macula distance (DD/DM).8,9 Data included in the analysis were age, sex, laterality, Snellen visual acuity, intraocular pressure, refraction status, eye position and movement, anterior segment examinations, pupil response, and fundus photography. Magnetic resonance imaging (MRI) of the brain was obtained from all enrolled participants and reported by the neuro-radiologists. A systematic review of the literature was carried out.
3. Results
A total of eight eyes of five patients with ONH were enrolled in this study (1 male, 4 females). The mean age (±standard deviation) at diagnosis was 14.5 ± 12.0 years (range 0.25–30 years). Of the five eyes having refraction examinations, the mean spherical power was −7.90 ± 3.38 diopters (D) (range −2.00 to −10.25 D) and the mean astigmatism was −2.60 ± 2.31 D (range −0.75 to −6.00 D). Four of the five eyes attained high myopia and two of the five eyes had high astigmatism. Snellen visual acuity ranged from light perception to 1.0. Approximately half (3/8) of the diseased eyes had tortuous retinal vessels, and two eyes of one patient showed diffuse changes in the retinal pigment epithelium (Table 1).
Table 1.
Demographic data, ophthalmologic characteristics, and findings on MRI of patients with ONH.
| No. | Sex | Age at diagnosis (y) | Eye | Snellen visual acuity | IOP (mmHg) | Spherical power (D) | Astigmatism (D) | Anterior segment and pupil | Fundus | MRI findings | Others | FU (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 3 mo | OD | N/A | N/A | N/A | N/A | WNL | Diffuse RPE change | Agenesis of septum pellucidum, small size of bilateral optic nerve | Right congenital ptosis | 12.8 |
| OS | N/A | N/A | N/A | N/A | WNL | Diffuse RPE change | Roving eye | |||||
| 2 | M | 21 | OD | CF | 22 | –9.75 | –4.0 | WNL | Ectopic posterior pituitary gland | Nystagmus OU | 1.6 | |
| OS | LP | 23 | –8.25 | –6.0 | RAPD+ | Tortuous vein | Hypopituitarism | |||||
| 3 | F | 30 | OD | 1 | 12 | N/A | N/A | WNL | Ectopic posterior pituitary gland | SLE, PRES, lupus nephritis | 0 | |
| 4 | F | 5 | OD | LP | 12 | –2.00 | –1.00 | RAPD+ | Atrophy of right optic nerve, optic chiasma, and left optic tract | Exotropia | 7.6 | |
| Ectopic posterior pituitary gland | ||||||||||||
| 5 | F | 16 | OD | 0.5 | 16 | –10.25 | –1.25 | WNL | Tortuous vessel | Intrasellar Rathke’s cleft cyst | Exophoria, scoliosis, laryngeal cleft, mild hyperprolactinemia | 130.8 |
| OS | 0.4 | 17 | –9.25 | –0.75 | WNL | Tortuous vessel |
CF = counting finger; (D) = diopters; F = female; FU = follow up; IOP = intraocular pressure; LP = light perception; M = male; MRI = magnetic resonance imaging; N/A = not available; OD = right eye; ONH = optic nerve hypoplasia; OS = left eye; OU = bilateral eyes; PRES = posterior reversible encephalopathy syndrome; RAPD = relative afferent pupillary defect; RPE = retinal pigment epithelium; SLE = systemic lupus erythematosus; WNL = within normal limit.
In the MRI analysis, ectopic posterior pituitary gland was the most prevalent finding (3 of 5 patients, 60%), followed by agenesis of septum pellucidum (1/5, 20%) and Rathke's cleft cyst (1/5, 20%) (Figs. 1–3). The diagnosis of ectopic posterior pituitary gland was established when a hyperintense nodule at the median eminence and absence of the normal posterior pituitary bright spot were noted on a T1-weighted MRI.10 Of the three patients with ectopic posterior pituitary gland, one had hypopituitarism. Another patient with intrasellar Rathke's cleft cyst had hyperprolactinemia (prolactin level 53.75 ng/mL; normal range 3.0–26.0 ng/mL).
Fig. 1.
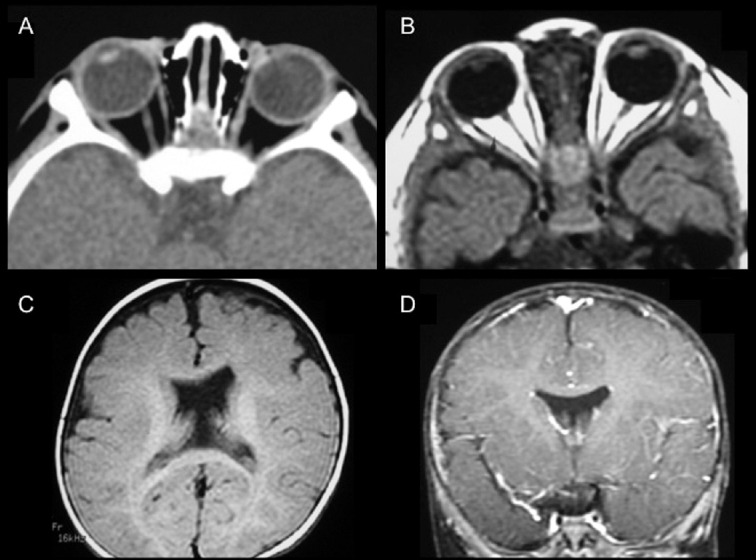
Bilateral optic nerve hypoplasia (ONH) with agenesis of septum pellucidum on neuroimaging (Case 1). (A) Computer tomography showed atrophy of the right optic nerve. (B) T1-weighted magnetic resonance imaging (MRI) revealed atrophy of bilateral optic nerves. Absent septum pellucidum was demonstrated on (C) axial view (T1-weighted MRI) and (D) coronal view (T1-weighted contrast MRI).
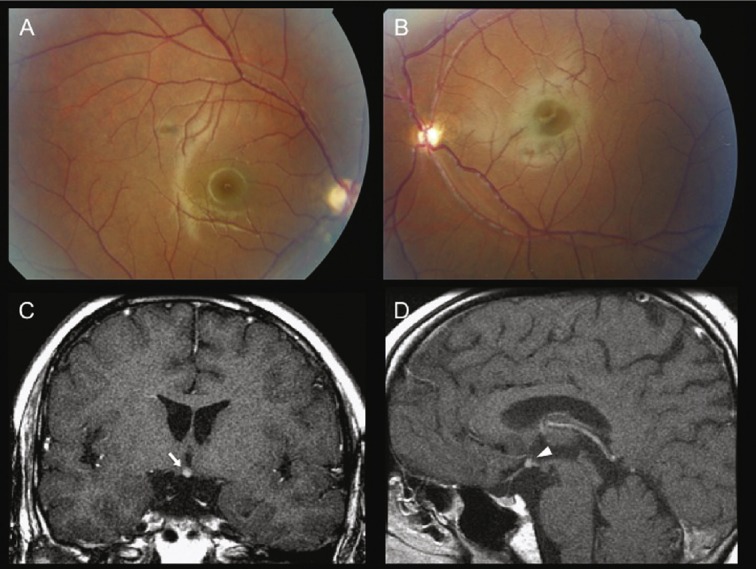
Fig. 3.
Bilateral optic nerve hypoplasia (ONH) with tortuosity of retinal vessels and intrasellar Rathke's cleft cyst on magnetic resonance imaging (MRI) (Case 5). (A, B) Fundus photography showed tortuous retinal vessels, which were more prominent in the right eye. (C, D) T1-weighted contrast MRI showed intrasellar Rathke's cleft cyst on coronal view (arrow) and sagittal view (arrowhead).
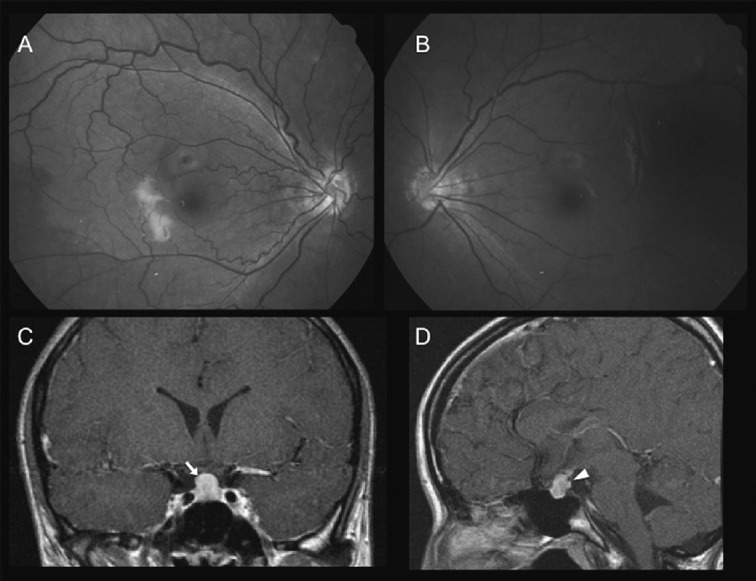
Fig. 2.
Bilateral optic nerve hypoplasia (ONH) with ectopic posterior pituitary gland on magnetic resonance imaging (MRI) (Case 2). (A, B) Fundus photography showed a small optic disc in both eyes and tortuous retinal veins in the left eye. (C, D) T1-weighted contrast MRI showed ectopic posterior pituitary gland on coronal view (arrow) and sagittal view (arrowhead).
Additional ocular findings included unilateral congenital ptosis in one patient with bilateral ONH, exotropia/exophoria in two patients, and nystagmus in one patient. A female patient with ectopic posterior pituitary gland also had systemic lupus erythematosus (SLE) with lupus nephritis.
4. Discussion
This study demonstrated ONH in eight eyes of five patients of Chinese ethnicity. All of them had midline brain abnormalities on MRI, such as ectopic posterior pituitary gland (60%), agenesis of septum pellucidum (20%), and Rathke's cleft cyst (20%). These patients presented with a wide range of visual acuity from 1.0 on the Snellen visual acuity scale to light perception, and possible association with high myopia (50%), high astigmatism (25%), and exodeviation (40%).
ONH is a nonprogressive congenital disc anomaly characterized by a small optic disc with a double-ring sign. It may result from excessive apoptosis of retinal ganglion cells during visual pathway development.2,11 A 90% reduction of optic nerve fibers without degenerated axons has been noted on histopathologic examination.2 Visual acuity may range from no light perception to normal vision. Associated ophthalmological features include nystagmus (26–86%), strabismus (42–52%), axial myopia, and astigmatism.3,12,13,14,15 Approximately 80% of the ONH patients had bilateral involvement, compared to 60% in our study.3,13 The most consistently reported maternal factors were young maternal age and primiparity. Other factors such as maternal smoking, maternal diabetes, poor maternal weight gain, premature labor, medication use, and family unemployment had been advocated but still need further validation.3,7,13,16,17,18,19
The most prevalent findings on neuroimaging included absent septum pellucidum (53%), corpus callosum hypoplasia and abnormalities of the pituitary gland (13–34%), such as ectopic pituitary gland, empty sella, and infundibular hypoplasia.20,21 Other neuro-radiographic features included schizencephaly, arachnoid cysts, pachygyria, polymicrogyria, cortical heterotopia, white matter hypoplasia, and hydrocephalus.19,20 In our series, cases included ectopic posterior pituitary gland (60%), agenesis of septum pellu-cidum (20%), and Rathke's cleft cyst (20%). Rathke's cleft cysts are believed to derive from remnants of the Rathke's pouch, which normally regress after primitive pituitary cell proliferation and differentiation.22 The enlargement of the Rathke's cleft may lead to symptomatic Rathke's cleft cyst.22,23,24 From the literature search, there were no reports regarding Rathke's cleft cyst and ONH. Given the previous study that Rathke's cleft cyst may occur in 13–22% of normal pituitary glands, whether Rathke's cleft cyst and ONH have real association or not still needs further investigation.22,23,24
Over the last few decades, numerous studies have placed great emphasis on neuroimaging in the diagnosis of ONH. An associated brain anomaly may imply a variety of functional disorders such as the occurrence of hypopituitarism, metabolic crisis, seizure, developmental delay, and so on. Corpus callosum hypoplasia was identified as having an association with developmental delay.9 Isolated absent septum pellucidum was associated with normal developmental and endocrinologic features.9,14,20 Pituitary abnormalities may strongly suggest hypopituitarism.9,20 In fact, patients with ONH may have hypopituitarism (26–82%) even without visible pituitary abnormalities.13,14,25 A normal pituitary gland on MRI does not preclude the possibility of endocrinopathy. In our study, one patient with ectopic posterior pituitary gland had hypopituitarism. The other patient with Rathke's cleft cyst had hyperprolactinemia—the most commonly associated endocrine disorder that is postulated to be the result of compression of the hypothalamic-infundibular system by the cyst.22,23,24
Additionally, Hellstrom et al found a significant association between tortuosity of retinal veins and endocrinopathy in patients with ONH, which was also true in our patients.26 Pituitary abnormalities together with tortuosity of retinal vessels may be highly predictive of endocrine disorders in these patients.
The limitations of this study included its small cohort size and its retrospective nature. However, all patients were evaluated by one neuro-ophthalmologist and had documented fundus photography and brain MRI. These data may be valuable to determine the clinical features in ONH patients of Chinese ethnicity.
In conclusion, this study demonstrated a high prevalence of midline brain abnormalities in ONH patients of Chinese ethnicity. The presence of tortuous retinal vessels in patients with a midline brain anomaly may indicate the occurrence of endocrinopathy. Due to the limited case numbers, further studies are needed to characterize the clinical and neuroradiographic features of patients with ONH.
Footnotes
Conflicts of interest: All contributing authors declare no conflicts of interest.
References
- 1.Steinkuller PG, Du L, Gilbert C, Foster A, Collins ML, Coats DK. Childhood blindness. J AAPOS. 1999;3:26–32. doi: 10.1016/s1091-8531(99)70091-1. [DOI] [PubMed] [Google Scholar]
- 2.Saadati HG, Hsu HY, Heller KB, Sadun AA. A histopathologic and morphometric differentiation of nerves in optic nerve hypoplasia and Leber hereditary optic neuropathy. Arch Ophthalmol. 1998;116:911–916. doi: 10.1001/archopht.116.7.911. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Filion P, Borchert M. Optic nerve hypoplasia syndrome: a review of the epidemiologyand clinical associations. Curr Treat OptionsNeurol. 2013;15:78–89. doi: 10.1007/s11940-012-0209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borchert M, Garcia-Filion P. The syndrome of optic nerve hypoplasia. Curr Neurol Neurosci Rep. 2008;8:395–403. doi: 10.1007/s11910-008-0061-7. [DOI] [PubMed] [Google Scholar]
- 5.Hoyt WF, Kaplan SL, Grumbach MM, Glaser JS. Septo-optic dysplasia and pituitary dwarfism. Lancet. 1970;1:893–894. doi: 10.1016/s0140-6736(70)91717-4. [DOI] [PubMed] [Google Scholar]
- 6.Blohme J, Bengtsson-Stigmar E, Tornqvist K. Visually impaired Swedish children. Longitudinal comparisons 1980–1999. Acta Ophthalmol Scand. 2000;78:416–420. doi: 10.1034/j.1600-0420.2000.078004416.x. [DOI] [PubMed] [Google Scholar]
- 7.Patel L, McNally RJ, Harrison E, Lloyd IC, Clayton PE. Geographical distribution of optic nerve hypoplasia and septo-optic dysplasia in Northwest England. J Pediatr. 2006;148:85–88. doi: 10.1016/j.jpeds.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Borchert M, McCulloch D, Rother C, Stout AU. Clinical assessment, optic disk measurements, and visual-evoked potential in optic nerve hypoplasia. Am J Ophthalmol. 1995;120:605–612. doi: 10.1016/s0002-9394(14)72207-x. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Filion P, Epport K, Nelson M, Azen C, Geffner ME, Fink C, et al. Neuro-radiographic, endocrinologic, and ophthalmic correlates of adverse developmental outcomes in children with optic nerve hypoplasia: a prospective study. Pediatrics. 2008;121:e653–e659. doi: 10.1542/peds.2007-1825. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell LA, Thomas PQ, Zacharin MR, Scheffer IE. Ectopic posterior pituitary lobe and periventricular heterotopia: cerebral malformations with the same underlying mechanism? Am J Neuroradiol. 2002;23:1475–1481. [PMC free article] [PubMed] [Google Scholar]
- 11.Zeki SM, Dutton GN. Optic nerve hypoplasia in children. Br J Ophthalmol. 1990;74:300–304. doi: 10.1136/bjo.74.5.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeki SM. Optic nerve hypoplasia and astigmatism: a new association. Br J Ophthalmol. 1990;74:297–299. doi: 10.1136/bjo.74.5.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohney BG, Young RC, Diehl N. Incidence and associated endocrine and neurologic abnormalities of optic nerve hypoplasia. JAMA Ophthalmol. 2013;131:898–902. doi: 10.1001/jamaophthalmol.2013.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siatkowski RM, Sanchez JC, Andrade R, Alvarez A. The clinical, neuroradio-graphic, and endocrinologic profile of patients with bilateral optic nerve hy-poplasia. Ophthalmology. 1997;104:493–496. doi: 10.1016/s0161-6420(97)30286-3. [DOI] [PubMed] [Google Scholar]
- 15.Weiss AH, Ross EA. Axial myopia in eyes with optic nerve hypoplasia. Graefe's Arch Clin Exp Ophthalmol. 1992;230:372–377. doi: 10.1007/BF00165948. [DOI] [PubMed] [Google Scholar]
- 16.Tornqvist K, Ericsson A, Kallen B. Optic nerve hypoplasia: risk factors and epidemiology. Acta Ophthalmol Scand. 2002;80:300–304. doi: 10.1034/j.1600-0420.2002.800313.x. [DOI] [PubMed] [Google Scholar]
- 17.Garcia-Filion P, Borchert M. Prenatal determinants of optic nerve hypoplasia: review of suggested correlates and future focus. Survey Ophthalmol. 2013;58:610–619. doi: 10.1016/j.survophthal.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia-Filion P, Fink C, Geffner ME, Borchert M. Optic nerve hypoplasia in North America: a re-appraisal of perinatal risk factors. Acta Ophthalmol. 2010;88:527–534. doi: 10.1111/j.1755-3768.2008.01450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia ML, Ty EB, Taban M, Rothner AD, Rogers D, Traboulsi EI. Systemic and ocular findings in 100 patients with optic nerve hypoplasia. J Child Neurol. 2006;21:949–956. doi: 10.1177/08830738060210111701. [DOI] [PubMed] [Google Scholar]
- 20.Brodsky MC, Glasier CM. Optic nerve hypoplasia. Clinical significance of associated central nervous system abnormalities on magnetic resonance imaging. Arch Ophthalmol. 1993;111:66–74. doi: 10.1001/archopht.1993.01090010070029. [DOI] [PubMed] [Google Scholar]
- 21.Zeki SM, Hollman AS, Dutton GN. Neuroradiological features of patients with optic nerve hypoplasia. J Pediatr Ophthalmol Strabismus. 1992;29:107–112. doi: 10.3928/0191-3913-19920301-11. [DOI] [PubMed] [Google Scholar]
- 22.Noh SJ, Ahn JY, Lee KS, Kim SH. Pituitary adenoma and concomitant Rathke's cleft cyst. Acta Neurochir (Wien) 2007;149:1223–1228. doi: 10.1007/s00701-007-1295-x. [DOI] [PubMed] [Google Scholar]
- 23.Isono M, Kamida T, Kobayashi H, Shimomura T, Matsuyama J. Clinical features of symptomatic Rathke's cleft cyst. Clin Neurol Neurosurg. 2001;103:96–100. doi: 10.1016/s0303-8467(01)00121-4. [DOI] [PubMed] [Google Scholar]
- 24.Nishioka H, Haraoka J, Izawa H, Ikeda Y. Magnetic resonance imaging, clinical manifestations, and management of Rathke's cleft cyst. Clin Endocrinol. 2006;64:184–188. doi: 10.1111/j.1365-2265.2006.02446.x. [DOI] [PubMed] [Google Scholar]
- 25.Haddad NG, Eugster EA. Hypopituitarism and neurodevelopmental abnormalities in relation to central nervous system structural defects in children with optic nerve hypoplasia. J Pediatr Endocrinol Metab. 2005;18:853–858. doi: 10.1515/jpem.2005.18.9.853. [DOI] [PubMed] [Google Scholar]
- 26.Hellström A, Wiklund LM, Svensson E, Albertsson-Wikland K, Stromland K. Optic nerve hypoplasia with isolated tortuosity of the retinal veins: a marker of endocrinopathy. Arch Ophthalmol. 1999;117:880–884. doi: 10.1001/archopht.117.7.880. [DOI] [PubMed] [Google Scholar]


