Abstract
We reported the spectral-domain optical coherence tomography (SD-OCT) findings of a subinternal limiting membrane hemorrhage in the macula in one patient with Valsalva retinopathy and in one patient with macroaneurysm before and after neodymium-doped yttrium aluminum garnet (Nd:YAG) laser membranotomy. Within 1 week, the Nd:YAG laser treatment facilitated rapid absorption of the hemorrhage in both patients. Spectral-domain optical coherence tomography was helpful before laser treatment to evaluate the exact location of the blood and after laser treatment to confirm the amount and location of residual hemorrhage, which was hard to confirm by only indirect ophthalmoscopy.
Keywords: Nd:YAG laser treatment, spectral-domain optical coherence tomography, subinternal limiting membrane hemorrhage
1. Introduction
Hemorrhagic detachment of the internal limiting membrane (ILM) in the macula causes sudden profound visual loss. Spontaneous resorption of the entrapped blood tends to be slow and may result in longstanding visual impairment. Major etiological factors are Valsalva retinopathy, macroaneurysms, retinal vein occlusions, and diabetic retinopathy.1 Dense premacular hemorrhage is traditionally managed by observation or vitrectomy. Puncturing the posterior hyaloid face or ILM by neodymium-doped yttrium aluminum garnet (Nd:YAG) laser photodisruption to facilitate rapid absorption of the hemorrhage has been described as an alternative treatment.1,2,3,4,5 However, the exact location of the hemorrhage before or after laser treatment is hard to confirm using only indirect ophthalmoscopy. In this paper, we report the spectral-domain optical coherence tomography (SD-OCT) findings of two patients with a sub-ILM hemorrhage before and after Nd:YAG laser membranotomy.
2. Case reports
2.1. Case 1
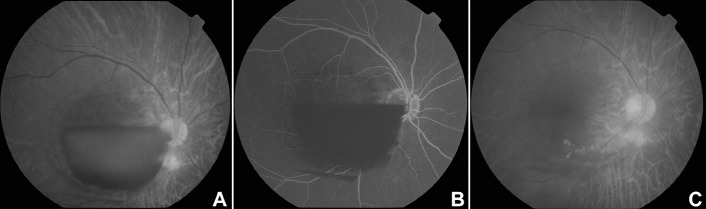
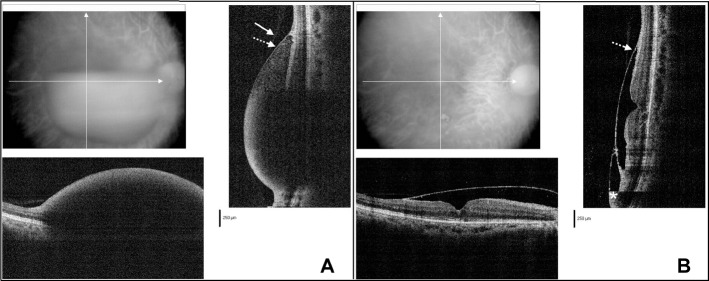
A 62-year-old man with hypertension suffered from sudden blurred vision in his right eye after severe coughing a few days before. A sudden decrease of vision to counting fingers resulted from a large premacular hemorrhage. The boat-shaped hemorrhage, which extended over the optic disc was a typical subhyaloid hemorrhage (Fig. 1A). No neovascularization, venous occlusion, or macroaneurysm was detected by fluorescein angiography (Fig. 1B). The SD-OCT scan (RTVue-100 OCT; Optovue Inc., CA, USA) of the region just at the upper margin of the hemorrhage revealed two distinct membranes overlying the preretinal hemorrhage (Fig. 2A). A very faint overlying membrane was identified as the posterior hyaloid. The more reflective membrane on the retina aspect was the ILM. Posterior vitreous detachment had not developed. After the OCT examinations, the hemorrhage was identified under the ILM. Valsalva retinopathy with mixed-type hemorrhage (i.e., sub-hyaloid and sub-ILM hemorrhage) was diagnosed. Seven days later, Nd:YAG laser (6–8 mJ) was performed at the inferior margin of the anterior surface of the hemorrhage. The blood was immediately drained into the vitreous cavity; by 1 week, it was mostly eliminated (Fig. 1C). His visual acuity improved to 20/40. The SD-OCT distinguished the detached hyperreflective ILM from the underlying retinal layers and the remaining blood in the subhyaloidal space (Fig. 2B).
Fig. 1.
Fundus photographs before and after Nd:YAG laser membranotomy in Case 1. (A) Right eye with a dense and large premacular hemorrhage. (B) Late-phase fluorescein angiogram confirms Valsalva retinopathy. (C) One week after Nd:YAG laser membranotomy, the right eye showed very little residual hemorrhage.
Fig. 2.
Optical coherence tomography (OCT) findings before and after Nd:YAG laser membranotomy in Case 1. (A) The very faint overlying membrane is the posterior hyaloid (solid arrow), and on the retina aspect is the more reflective internal limiting membrane (ILM) (dotted arrow). The infrared image shows the location of the vertical and horizontal spectral domain-OCT (SD-OCT) scan area. (B) One week after Nd:YAG laser membranotomy, the detached ILM (dotted arrow) was present and residual blood was found in the subhyaloidal space (asterisk) in the lower part.
2.2. Case 2
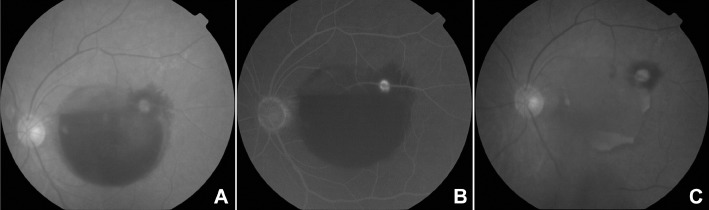
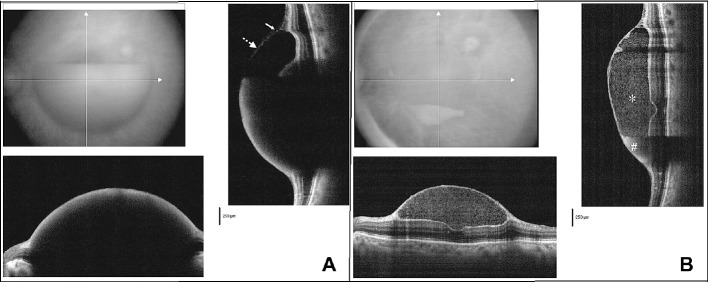
A 75-year-old woman with hypertension noticed sudden blurred vision in her left eye 1 month previously. Visual acuity was reduced to hand motion. A dense dark-red premacular hemorrhage with macroaneurysm was confirmed by fluorescein angiography (Fig. 3A and B). The SD-OCT scan also revealed a faint overlying membrane (i.e., posterior hyaloid) fused with the hyperreflective membrane (i.e., ILM) around the upper margin of the hemorrhage (Fig. 4A). Nd:YAG laser photodisruption (8–10 mJ) was performed. The blood rapidly dispersed into the vitreous cavity. One week later, her visual acuity improved to 20/200 with a substantially decreased hemorrhage, but a residual yellowish hematoma was in the para-central area (Fig. 3C). The OCT image showed a blood clot in the lower part under the hyperreflective ILM and remaining blood in the upper part, which were not easily detected by indirect ophthalmoscopy (Fig. 4B). The patient did not return to our clinic because of a recent stroke.
Fig. 3.
Fundus photographs before and after Nd:YAG laser membranotomy in Case 2. (A) Macroaneurysm in the left eye with a dense premacular hemorrhage. (B) Late-phase fluorescein angiogram shows dye leaking from the macroaneurysm on the upper macular branch artery. (C) One week after Nd:YAG laser membranotomy, a residual yellowish hematoma was present in the paracentral area of the left eye.
Fig. 4.
Optical coherence tomography (OCT) findings before and after Nd:YAG laser membranotomy in Case 2. (A) spectral domain-OCT (SD-OCT) reveals that the fainter reflecting posterior hyaloid in the upper border (solid arrow) is fused with the internal limiting membrane (ILM) (dotted arrow) over the preretinal hemorrhage. The infrared image shows the location of the vertical and horizontal SD-OCT scan area. (B) The SD-OCT image shows a residual sub-ILM hemorrhage (asterisk) and a dense blood clot (pound sign) in the lower part.
3. Discussion
It is hard to differentiate sub-ILM hemorrhage or subhyaloid hemorrhage using only fundoscopic examination. Therefore, it is usually unclear that the precise anatomic layer of the laser puncture is the ILM or the posterior hyaloid membrane. A boat-shaped hemorrhage, as our first patient had, usually—but not always—indicates a subhyaloid hemorrhage. If the space within the ILM is substantially large, blood cell components would enter the lower part and create a boat-like image. The fundoscopic image of Case 1 revealed a subhyaloid hemorrhage; however, with the help of OCT scans, we found the patient also had a sub-ILM hemorrhage. Schuman6 and associates in their OCT findings reported subhyaloid hemorrhage in Valsalva retinopathy and sub-ILM hemorrhage in macroaneurysm. Shukla et al7 demonstrated a sub-ILM hemorrhage in Valsalva retinopathy using OCT scans. They found the highly reflective ILM and an overlying patchy membrane with low optical reflectivity, which was consistent with the posterior hyaloid. Our two cases demonstrated that the best area to differentiate between a sub-ILM hemorrhage and a subhyaloid hemorrhage on an OCT scan was the upper border of the hemorrhage. This is because a dense blood clot disturbing an OCT scan usually condenses in the lower part because of gravity. Spectral-domain optical coherence tomography reportedly localizes Nd:YAG laser spots in Valsalva retinopathy.2 However, we only routinely focused on the central macular area and we did not have the OCT pictures showing the site of membranotomy which was usually in the lower part of macula. This may be the future direction of OCT studies in the follow up of premacular hemorrhage after Nd-YAG laser treatment. However, our cases emphasized the importance of SD-OCT evaluation after ND:YAG laser treatment. This could determine the amount of residual sub-ILM hemorrhage, which would otherwise be hard to define only by fundoscopic examination. Optical coherence tomography could also confirm the exact location of the remaining hemorrhage. Mixed-type hemorrhage (i.e., sub-ILM and subhyoloid hemorrhage) could be demonstrated clearly before and after Nd: YAG laser treatment, as in Case 1.
The Nd:YAG laser power required to achieve perforation varies from 1 mJ to 50 mJ.3,4 The laser energy (6–10 mJ) was lower in our patients. In Case 2, incomplete drainage of the hemorrhage did not result from insufficient laser energy or from failure of laser perforation since the hemorrhage leaked into the vitreous cavity soon after the laser treatment. Delayed treatment by more than 1 month after the onset of hemorrhage may have been a cause and suggested a poor prognostic sign.4,5 Case 2 demonstrated that yellowish clotted blood may be hidden in the dark-red hemorrhage. It was harder to disperse into the vitreous cavity, even after successful laser photodisruption. On the contrary, since the natural history of macular hemorrhage secondary to a macroaneurysm is usually spontaneous involution with a good visual outcome, the typical management consists of observation.8 Some patients may initially choose observation; however, we suggest that if Nd:YAG laser is considered, it should be performed as early as possible. Once the blood becomes clotted, complete drainage is hard to achieve, despite successful laser perforation.
In conclusion, Nd:YAG laser may be considered for treating a recent premacular hemorrhage. Before and after laser treatment, SD-OCT is helpful in evaluating the exact location of the blood and in confirming the amount of residual hemorrhage. Larger case studies are required to confirm this finding, and randomized prospective studies are needed to evaluate the timing and effectiveness of laser treatment.
Footnotes
Conflicts of interest: The authors have no conflicts of interest relevant to this article.
References
- 1.Rennie CA, Newman DK, Snead MP, Flanagan DW. Nd:YAG laser treatment for premacular subhyaloid haemorrhage. Eye (Lond) 2001;15:519–524. doi: 10.1038/eye.2001.166. [DOI] [PubMed] [Google Scholar]
- 2.Sabella P, Bottoni F, Staurenghi G. Spectral-domain OCT evaluation of Nd:YAG laser treatment for Valsalva retinopathy. Graefes Arch Clin Exp Ophthalmol. 2010;248:599–601. doi: 10.1007/s00417-009-1252-x. [DOI] [PubMed] [Google Scholar]
- 3.Iijima H, Satoh S, Tsukahara S. Nd:YAG laser photodisruption for preretinal hemorrhage due to retinal macroaneurysm. Retina. 1998;18:430–434. doi: 10.1097/00006982-199805000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Gabel VP, Birngruber R, Gunther-Koszka H, Puliafito CA. Nd:YAG laser photo-disruption of hemorrhagic detachment of the internal limiting membrane. Am J Ophthalmol. 1989;107:33–37. doi: 10.1016/0002-9394(89)90811-8. [DOI] [PubMed] [Google Scholar]
- 5.Mansour A. Nd:YAG laser photodisruption of hemorrhagic detachment of the internal limiting membrane. Am J Ophthalmol. 1989;107:566–568. doi: 10.1016/0002-9394(89)90519-9. [DOI] [PubMed] [Google Scholar]
- 6.Schuman JS, Puliafito CA, Fujimoto JG. Optical coherence tomography of ocular diseases. Thorofare NJ: Slack; 2004:1–698. [Google Scholar]
- 7.Shukla D, Naresh KB, Kim R. Optical coherence tomography findings in Valsalva retinopathy. Am J Ophthalmol. 2005;140:134–136. doi: 10.1016/j.ajo.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Rabb MF, Gagliano DA, Teske MP. Retinal arterial macroaneurysms. Surv Ophthalmol. 1988;33:73–96. doi: 10.1016/0039-6257(88)90160-9. [DOI] [PubMed] [Google Scholar]