Abstract
Background
Hospital readmission is common among patients with diabetes. Some readmissions, particularly for hypoglycemia and hyperglycemia, may be avoidable with better care transitions and post-discharge management.
Objective
To ascertain the most common reasons and risk factors for readmission among adults with diabetes, with specific consideration of severe dysglycemia.
Design
Retrospective analysis of data from the OptumLabs Data Warehouse, an administrative data set of commercially insured and Medicare Advantage beneficiaries across the U.S.
Participants
Adults ≥18 years of age with diabetes, discharged from a hospital between January 1, 2009, and December 31, 2014 (N = 342,186).
Main Measures
Principal diagnoses and risk factors for 30-day unplanned readmissions, subset as being for severe dysglycemia vs. all other causes.
Key Results
We analyzed 594,146 index hospitalizations among adults with diabetes: mean age 68.2 years (SD, 13.0), 52.9% female, and 67.8% white. The all-cause 30-day readmission rate was 10.8%. Heart failure was the most common cause for index hospitalization (5.5%) and readmission (8.9%). Severe dysglycemia accounted for 2.6% of index hospitalizations (48.1% hyperglycemia, 50.4% hypoglycemia, 1.5% unspecified) and 2.5% of readmissions (38.3% hyperglycemia, 61.0% hypoglycemia, 0.7% unspecified). Younger patient age, severe dysglycemia at index or prior hospitalization, and the Diabetes Complications Severity Index (DCSI) were the strongest risk factors predisposing patients to severe dysglycemia vs. other readmissions. Prior episodes of severe dysglycemia and the DCSI were also independent risk factors for other-cause readmissions, irrespective of the cause of the index hospitalization.
Conclusions
Adults with diabetes are hospitalized and readmitted for a wide range of health conditions, and hospitalizations for severe hypoglycemia and hyperglycemia remain common, with high rates of recurrence. Severe dysglycemia is most likely to occur among younger patients with multiple diabetes complications and prior history of such events.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-017-4095-x) contains supplementary material, which is available to authorized users.
KEY WORDS: diabetes, epidemiology, readmissions, hospital medicine, hypoglycemia, hyperglycemia, health services research, risk assessment
INTRODUCTION
Diabetes increases the risk of hospitalization and unplanned readmission,1 – 4 imposing a substantial burden on patients, caregivers, health systems, and the economy. Patients with diabetes are susceptible to a broad range of acute illnesses that can lead to hospitalization and readmission, including those related to co-existing chronic conditions as well as exacerbations of, and complications from, their underlying diabetes. Uniquely, patients with diabetes are vulnerable to severe hypoglycemia and hyperglycemia (“severe dysglycemia”), particularly during the post-discharge period when changes in activity, nutrition, and medications commonly occur.5 Efforts to reduce hospitalizations and readmissions among patients with diabetes require a broad and nuanced understanding of their most common causes, including the relative frequency of severe dysglycemic events, as well as the risk factors for these events.
Prior studies of hospital readmissions among patients with diabetes are limited, but show that all-cause readmission risk is higher among patients with multiple comorbidities1 – 3 , 6 , 7 and among racial minorities.1 – 3 , 8 , 9 Several studies focused on hospitalizations for hypoglycemia8 , 10 or hyperglycemia,8 but without placing them in the broader context of hospitalizations and readmissions. Severe dysglycemic events can be avoided with optimal transitional and ambulatory care,11 and understanding their relative importance may guide interventions for patients at high risk. Accordingly, our study addresses the following three questions in a large cohort of commercially insured and Medicare Advantage beneficiaries across the U.S.: (1) What are the principal reasons for which patients with diabetes are hospitalized and subsequently readmitted? (2) What is the relative burden of hospitalizations and readmissions for severe dysglycemia when considered in the context of all hospitalizations and readmissions experienced by this patient population? (3) What are the primary risk factors for unplanned 30-day readmissions in this high-risk population? This knowledge may facilitate the development and prioritization of individualized interventions for patients at highest risk for diabetes-related and unrelated readmissions.
METHODS
Study Design and Data Source
We conducted a retrospective analysis of medical and pharmacy claims data from the OptumLabs Data Warehouse (OLDW), an administrative database of more than 100 million privately insured and Medicare Advantage enrollees throughout the U.S. (Online Appendix 1).12 , 13 All study data were accessed after the data had been de-identified, consistent with the Health Insurance Portability and Accountability Act (HIPAA) expert de-identification determination and with appropriate legal, regulatory, and contractual permissions. Because this study involved analysis of pre-existing, de-identified data, it was exempt from institutional review board approval.14
Study Population
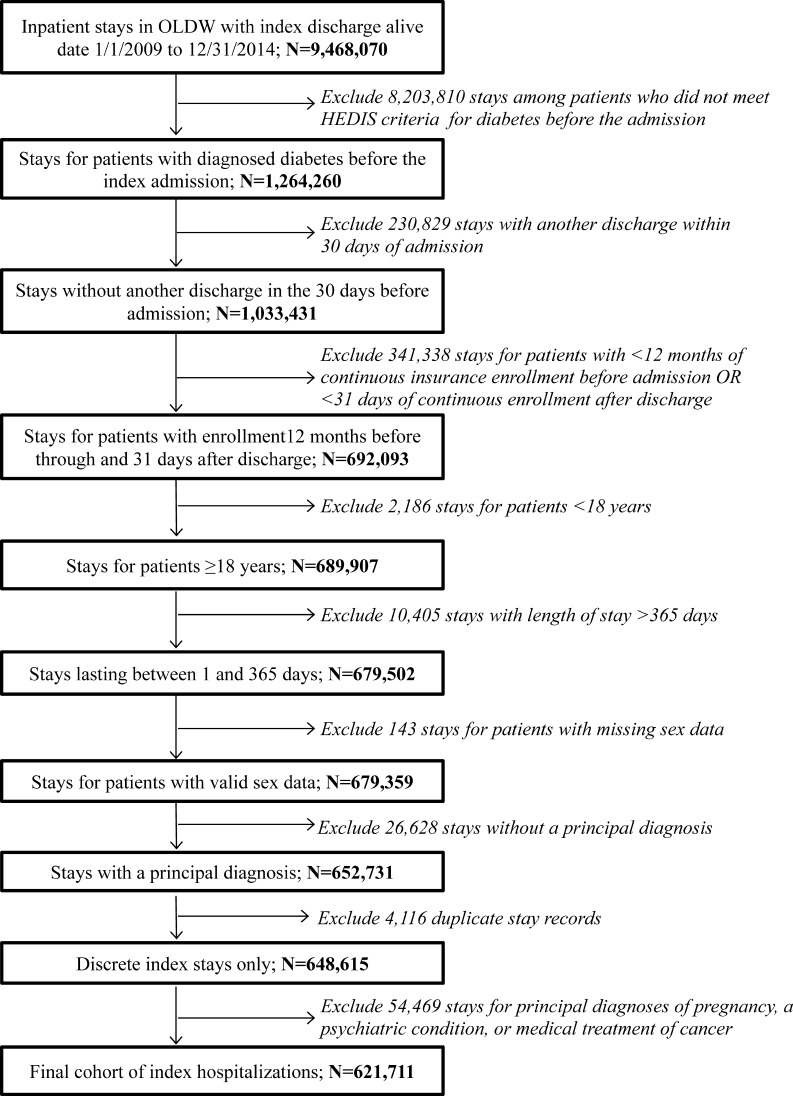
The study sample comprised all index hospitalizations among adults ≥18 years of age with diabetes in non-federal acute care hospitals lasting ≥1 night, with discharge alive date between January 1, 2009, and December 31, 2014 (Fig. 1). Diabetes was defined using Healthcare Effectiveness Data and Information Set (HEDIS) claims-computable criteria, excluding gestational diabetes (ICD-9-CM 648.0, 648.8).15 Included individuals had ≥12 months of enrollment before the index admission date and ≥31 days of enrollment after the index discharge date. In accordance with the Centers for Medicare & Medicaid Services (CMS) Hospital-Wide Readmission Measure (HWRM) and the National Committee for Quality Assurance criteria,16 , 17 hospitalizations for medical treatment of cancer, psychiatric disease, and pregnancy were excluded. We excluded admissions with length of stay (LOS) >365 days and readmissions within 1 day of discharge, which were counted as part of the original admission.
Figure 1.
Study cohort.
Explanatory Variables
Principal diagnoses for index admissions were identified using the first/primary diagnosis ICD-9-CM code from the hospitalization claim and grouped using categories identified by the Agency for Healthcare Research and Quality (AHRQ) Comorbidity and Clinical Classifications Software (CCS).18 Severe dysglycemic events were categorized as hypoglycemic, hyperglycemic, or unspecified (Online Appendix Table 1).19 – 21 CCS 50 (“diabetes mellitus with complications”) was not used, as it does not include hypoglycemia; it was included in the analyses but modified to exclude diagnoses included in the severe dysglycemia definitions.
Patient demographic characteristics were obtained from enrollment data, and included age at the index hospitalization, sex, race/ethnicity, and annual household income in US dollars. For each index hospitalization we determined the LOS (categorized as 1, 2–4, 5–7, 8–14, and ≥15 days), discharge year, and history of another hospitalization during the prior 12 months. Rather than assume a linear or monotone relationship between LOS and risk of readmission, we categorized this risk factor based on inspection of the distribution for our cohort. To determine whether a hospitalization was planned, we applied version 3 of the CMS HWRM planned readmission algorithm.16 , 22 , 23
To identify comorbidities, we used the Diabetes Complications Severity Index (DCSI), adapted for claims data,24 , 25 and the Charlson Comorbidity Index (CCI),26 all from within 12 months of the index admission. Treatment with insulin was ascertained from pharmacy claims within 120 days preceding the index admission.
Outcomes
The primary outcome was unplanned readmission within 30 days of discharge for any cause, categorized as a readmission for severe dysglycemia vs. other (Online Appendix Table 1). We also conducted a secondary analysis which stratified patients based on their index hospitalization (severe dysglycemia vs. other). Planned readmissions, defined using HWRM criteria,16 , 22 , 23 were excluded.
Statistical Analysis
We summarized patient and hospitalization characteristics for each index admission, overall and by readmission status (none, severe dysglycemia, other), and tested for differences in outcomes using χ2 tests of independence. We identified the 10 most common principal diagnosis CCS categories18 at index admission, overall and by readmission status.
In order to identify independent risk factors for severe dysglycemia vs. other readmissions, we estimated a multinomial logistic regression model using the primary outcome of no readmission, other readmission, or severe dysglycemia readmission as the dependent variable. To account for heterogeneity in index admission diagnoses between patients readmitted for severe dysglycemia and for other reasons, and the contribution of these diagnoses to subsequent readmission risk, we identified the 20 CCS groups that were most strongly associated with readmission for any cause based on bivariate analyses for all 46 CCS groups with a prevalence of at least 0.5% in the study cohort, and included these as risk factors in all models (Online Appendix Table 2). These 20 CCS groups were included in the multinomial logistic regression model, together with the explanatory variables listed above. We used the Huber–White sandwich variance estimator to account for correlation of outcomes by hospital.27 , 28 To account for missing income data (8.1% of total sample), we used multiple stochastic imputations, with 20 imputations.29 We report model effects as relative risk ratios (RRRs). To better interpret differences in RRRs across severe dysglycemia vs. other readmissions, we calculated ratios of RRRs for severe dysglycemia vs. other-cause readmissions, and the p-values for the test in which the ratio of RRRs differed from 1.0; that is, that the RRR for severe dysglycemia readmissions was not the same as the RRR for other readmissions. This P-value was based on a test which incorporated the variances in the RRRs. Thus, a severe dysglycemia/other RRR ratio >1 indicates that the particular covariate increases severe dysglycemia readmission risk more than other-cause readmission risk, and vice versa.
All analyses were conducted using Stata 14.1 (2015; StataCorp LP, College Station, TX). P-values <0.05 were considered statistically significant.
Results
Study Population and 30-Day Unplanned Readmission
Between January 1, 2009, and December 31, 2014, 342,186 adults with diabetes experienced 594,146 index hospitalizations, including 15,644 hospitalizations for severe dysglycemia (2.6% of index hospitalizations) among 13,161 patients (Table 1). Of these, 48.1% were for hypoglycemia, 50.4% for hyperglycemia, and 1.5% were unspecified. The most common cause for index hospitalization was heart failure (5.5% of index hospitalizations), while severe dysglycemic events were the 11th most common cause; the top 20 of 2621 diagnosis categories at index hospitalization are shown in Online Appendix Table 3.
Table 1.
Study Population
| Study cohort N (%) |
Not readmitted N (%) |
Readmitted | P-value | ||
|---|---|---|---|---|---|
| Severe dysglycemia N (%) |
Other cause N (%) |
||||
| Index discharges | 594,146 | 524,190 | 1744 | 68,212 | |
| Patient characteristics* | |||||
| Age, mean (SD) | 68.2 (13.0) | 68.0 (13.0) | 63.9 (18.0) | 69.7 (12.2) | |
| Age, N (%) | <0.001 | ||||
| <45 | 30,370 (5.1) | 27,694 (5.3) | 279 (16.0) | 2397 (3.5) | |
| 45–64 | 179,924 (30.3) | 161,069 (30.7) | 452 (25.9) | 18,403 (27.0) | |
| 65–74 | 173,279 (29.2) | 152,492 (29.1) | 431 (24.7) | 20,356 (29.8) | |
| ≥75 | 210,573 (35.4) | 182,935 (34.9) | 582 (33.4) | 27,056 (39.7) | |
| Sex | 0.83 | ||||
| Male | 279,651 (47.1) | 246,787 (47.1) | 812 (46.6) | 32,052 (47.0) | |
| Female | 314,495 (52.9) | 277,403 (52.9) | 932 (53.4) | 36,160 (53.0) | |
| Race | <0.001 | ||||
| White | 402,747 (67.8) | 356,824 (68.1) | 1090 (62.5) | 44,833 (65.7) | |
| Black | 109,670 (18.5) | 95,059 (18.1) | 445 (25.5) | 14,166 (20.8) | |
| Asian | 12,344 (2.1) | 10,956 (2.1) | 38 (2.2) | 1350 (2.0) | |
| Hispanic | 47,471 (8.0) | 41,910 (8.0) | 133 (7.6) | 5428 (8.0) | |
| Other/unknown | 21,914 (3.7) | 19,441 (3.7) | 38 (2.2) | 2435 (3.6) | |
| Annual income (US$) | <0.001 | ||||
| <40,000 | 242,291 (40.8) | 210,857 (40.2) | 795 (45.6) | 30,639 (44.9) | |
| 40,000–49,000 | 58,233 (9.8) | 51,567 (9.8) | 152 (8.7) | 6514 (9.5) | |
| 50,000–59,000 | 49,511 (8.3) | 43,775 (8.4) | 142 (8.1) | 5594 (8.2) | |
| 60,000–74,000 | 55,557 (9.4) | 49,492 (9.4) | 158 (9.1) | 5907 (8.7) | |
| 75,000–99,000 | 61,542 (10.4) | 55,114 (10.5) | 159 (9.1) | 6269 (9.2) | |
| ≥100,000 | 78,364 (13.2) | 71,033 (13.6) | 180 (10.3) | 7151 (10.5) | |
| Missing | 48,648 (8.2) | 42,352 (8.1) | 158 (9.1) | 6138 (9.0) | |
| Index hospitalization characteristics | |||||
| Planned status | <0.001 | ||||
| Unplanned | 500,750 (84.3) | 438,277 (83.6) | 1613 (92.5) | 60,860 (89.2) | |
| Planned | 93,396 (15.7) | 85,913 (16.4) | 131 (7.5) | 7352 (10.8) | |
| Reason for index hospitalization | |||||
| Severe dysglycemia | 15,644 (2.6) | 13,970 (2.7) | 483 (27.7) | 1191 (1.7) | |
| Hypoglycemia | 7528 (1.3) | 6686 (1.3) | 116 (6.7) | 726 (1.1) | <0.001 |
| Hyperglycemia | 7886 (1.3) | 7071 (1.3) | 363 (20.8) | 452 (0.7) | <0.001 |
| Unspecified | 230 (0.0) | 213 (0.0) | * (*) | 13 (0.0) | <0.001 |
| Other causes | 578,502 (97.4) | 510,220 (97.3) | 1261 (72.3) | 67,021 (98.3) | |
| Length of stay | <0.001 | ||||
| 1 day | 80,388 (13.5) | 74,637 (14.2) | 169 (9.7) | 5582 (8.2) | |
| 2–4 days | 314,962 (53.0) | 283,483 (54.1) | 822 (47.1) | 30,657 (44.9) | |
| 5–7 days | 118,193 (19.9) | 101,330 (19.3) | 403 (23.1) | 16,460 (24.1) | |
| 8–14 days | 63,392 (10.7) | 51,613 (9.8) | 265 (15.2) | 11,514 (16.9) | |
| ≥15 days | 17,211 (2.9) | 13,127 (2.5) | 85 (4.9) | 3999 (5.9) | |
| Prior hospitalizations | |||||
| None | <0.001 | ||||
| Other causes only | 351,468 (59.2) | 321,860 (61.4) | 693 (39.7) | 28,915 (42.4) | |
| Severe dysglycemia | 236,144 (39.7) | 196,958 (37.6) | 738 (42.3) | 38,448 (56.4) | |
| Diabetes characteristics | |||||
| Diabetes Complications Severity Index | <0.001 | ||||
| 0 | 143,755 (24.2) | 133,250 (25.4) | 153 (8.8) | 10,352 (15.2) | |
| 1–2 | 152,519 (25.7) | 137,598 (26.2) | 333 (19.1) | 14,588 (21.4) | |
| 3–6 | 198,156 (33.4) | 172,002 (32.8) | 695 (39.9) | 25,459 (37.3) | |
| 7–29 | 99,716 (16.8) | 81,340 (15.5) | 563 (32.3) | 17,813 (26.1) | |
| Diabetes treatment | <0.001 | ||||
| Non-insulin only | 435,861 (73.4) | 387,501 (73.9) | 47,563 (69.7) | 797 (45.7) | |
| Insulin | 158,285 (26.6) | 136,689 (26.1) | 20,649 (30.3) | 947 (54.3) | |
*Baseline patient characteristics at the time of index hospitalization. Each index admission was considered separately, and data were ascertained at the time of discharge
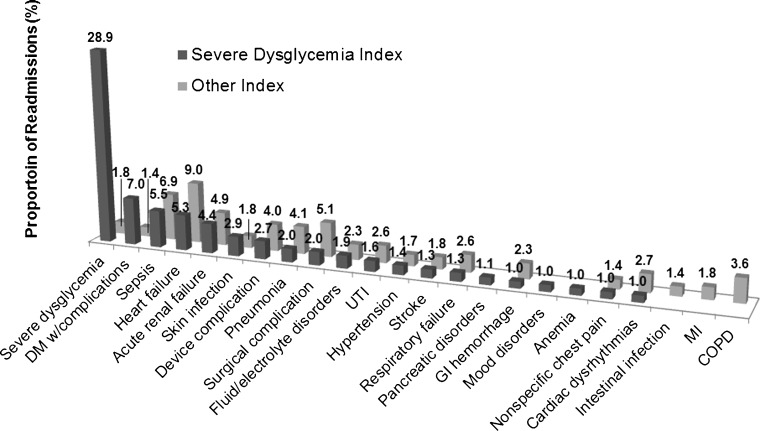
The all-cause unplanned readmission rate was 10.8%. Heart failure was the most common reason for readmission (8.9% of readmissions), while severe dysglycemic events accounted for 2.5% of readmissions (38.3% hyperglycemia, 61.0% hypoglycemia, 0.7% unspecified). The reason for readmission varied based on whether the index hospitalization was for severe dysglycemia or for other causes (Fig. 2; Online Appendix Tables 4, 5). Of those hospitalized for severe hypoglycemia, 6.7% were readmitted for another severe dysglycemic event and 1.1% were readmitted for other causes. Of those hospitalized for severe hyperglycemia, 20.8% were readmitted for another severe dysglycemic event and 0.7% were readmitted for other causes. Only 1.8% of patients hospitalized for other causes were readmitted for severe dysglycemia. Other causes for readmission following severe dysglycemia and other-cause hospitalizations are presented in Figure 2, highlighting the frequency of readmissions for heart failure, sepsis, and acute renal failure in both cohorts.
Figure 2.
Principal diagnoses at readmission. We present the percentage of patients readmitted for a specific principal diagnosis CCS category among all patients who were hospitalized for either a severe dysglycemic event (dark gray) or another cause (light gray) as their index hospitalization. The 20 most prevalent readmission diagnosis categories overall are presented.
General Risk Factors for Readmission
Certain variables increased readmission risk globally, for both severe dysglycemia and other-cause readmissions. Longer LOS during the index hospitalization increased the risk of all readmissions. Readmission risk was significantly lower following planned rather than unplanned hospitalizations: RRR 0.57 (95% CI, 0.47–0.69) for severe dysglycemia readmission and 0.79 (95% CI, 0.76–0.81) for other readmissions. Higher income was associated with reduced risk of all readmissions, with no significant difference in effect on the two types of readmission. African American patients had a slightly higher risk of all readmissions than did white patients.
Readmissions for Severe Dysglycemia
Many of the examined covariates had different effects on severe dysglycemia vs. other-cause readmissions (Table 2). The strongest risk factors for severe dysglycemia readmissions were patient age, DCSI, index hospitalization for severe dysglycemia (hyperglycemic events had a greater impact than hypoglycemic events), and prior history of severe dysglycemia hospitalizations (Table 2). The risk of readmission for severe dysglycemia was nearly twice as high among patients aged <45 years as those ≥45 years; age was not a strong risk factor for other-cause readmissions until age ≥75 years, when it began to rise. For all age groups, age was a stronger determinant of severe dysglycemia readmissions than other-cause readmissions. The DCSI was a significant risk factor for both categories of readmissions, but with greater impact on severe dysglycemia. Compared to patients with no diabetes complications, the risk of readmission for severe dysglycemia was 2.33-fold higher among patients with DCSI of 3–6, and 3.20-fold higher with DCSI ≥7. Compared to non-insulin-treated patients, patients using insulin were 80% more likely to be readmitted for severe dysglycemia and 6% more likely to be readmitted for other causes.
Table 2.
Risk Factors for Readmission for Severe Dysglycemia and Other Causes
| Readmission for severe dysglycemia | Readmission for other causes | Wald P* | Ratio of severe dysglycemia/other† | ||||
|---|---|---|---|---|---|---|---|
| RRR (95% CI) | P | RRR (95% CI) | P | P | |||
| Patient characteristics | |||||||
| Age, years | <0.001 | ||||||
| <45 | Ref | Ref | Ref | ||||
| 45–64 | 0.52 (0.43, 0.64) | <0.001 | 0.98 (0.94, 1.03) | 0.42 | 0.54 | <0.001 | |
| 65–74 | 0.56 (0.46, 0.69) | <0.001 | 1.00 (0.95, 1.06) | 0.96 | 0.56 | <0.001 | |
| ≥75 | 0.60 (0.49, 0.74) | <0.001 | 1.06 (1.00, 1.12) | 0.04 | 0.57 | <0.001 | |
| Sex | 0.93 | ||||||
| Male | Ref | Ref | Ref | ||||
| Female | 0.98 (0.88, 1.09) | 0.701 | 1.00 (0.98, 1.02) | 0.99 | 0.98 | 0.70 | |
| Race | <0.001 | ||||||
| White | Ref | Ref | Ref | ||||
| Black | 1.22 (1.07, 1.38) | 0.002 | 1.09 (1.06, 1.12) | <0.001 | 1.12 | 0.10 | |
| Asian | 1.30 (0.95, 1.78) | 0.106 | 1.05 (0.98, 1.11) | 0.15 | 1.24 | 0.23 | |
| Hispanic | 0.98 (0.81, 1.18) | 0.817 | 1.05 (1.01, 1.09) | 0.02 | 0.94 | 0.46 | |
| Other/unknown | 0.69 (0.50, 0.97) | 0.03 | 1.01 (0.96, 1.06) | 0.79 | 0.69 | 0.008 | |
| Annual income (US$) | <0.001 | ||||||
| <40,000 | Ref | Ref | Ref | ||||
| 40–49,000 | 0.77 (0.64, 0.93) | 0.007 | 0.94 (0.91, 0.97) | <0.001 | 0.82 | 0.03 | |
| 50–59,000 | 0.94 (0.79, 1.12) | 0.49 | 0.98 (0.95, 1.01) | 0.27 | 0.96 | 0.62 | |
| 60–74,000 | 0.89 (0.74, 1.07) | 0.21 | 0.95 (0.92, 0.98) | 0.001 | 0.94 | 0.47 | |
| 75–99,000 | 0.79 (0.66, 0.95) | 0.01 | 0.94 (0.91, 0.97) | <0.001 | 0.84 | 0.04 | |
| ≥100,000 | 0.77 (0.65, 0.91) | 0.003 | 0.90 (0.87, 0.93) | <0.001 | 0.85 | 0.05 | |
| Index hospitalization characteristics | |||||||
| Reason for index hospitalization | <0.001 | ||||||
| Other causes | Ref | Ref | Ref | ||||
| Hypoglycemia | 4.74 (3.81, 5.89) | <0.001 | 0.87 (0.81, 0.94) | 0.001 | 5.434 | <0.001 | |
| Hyperglycemia | 8.57 (7.08, 10.37) | <0.001 | 0.60 (0.55, 0.67) | <0.001 | 14.188 | <0.001 | |
| Unspecified | 5.81 (2.00, 16.83) | 0.001 | 0.61 (0.35, 1.07) | 0.082 | 9.564 | 0.137 | |
| Planned status | <0.001 | ||||||
| Unplanned | Ref | Ref | Ref | ||||
| Planned | 0.57 (0.47, 0.69) | <0.001 | 0.79 (0.76, 0.81) | <0.001 | 0.73 | <0.001 | |
| Length of stay | <0.001 | ||||||
| 1 day | 0.79 (0.67, 0.93) | 0.006 | 0.77 (0.75, 0.79) | <0.001 | 1.03 | 0.77 | |
| 2–4 days | Ref | Ref | Ref | ||||
| 5–7 days | 1.42 (1.25, 1.62) | <0.001 | 1.35 (1.32, 1.38) | <0.001 | 1.06 | 0.43 | |
| 8–14 days | 1.85 (1.60, 2.15) | <0.001 | 1.79 (1.74, 1.83) | <0.001 | 1.04 | 0.64 | |
| ≥15 days | 2.42 (1.91, 3.07) | <0.001 | 2.45 (2.35, 2.55) | <0.001 | 0.99 | 0.93 | |
| Prior hospitalizations | <0.001 | ||||||
| None | Ref | Ref | Ref | ||||
| Other causes | 1.27 (1.13, 1.42) | <0.001 | 1.58 (1.55, 1.61) | <0.001 | 0.81 | <0.001 | |
| Severe dysglycemia | 5.47 (4.60, 6.51) | <0.001 | 1.43 (1.33, 1.55) | <0.001 | 3.82 | <0.001 | |
| Diabetes characteristics | |||||||
| Diabetes Complications Severity Index | <0.001 | ||||||
| 0 | Ref | Ref | Ref | ||||
| 1–2 | 1.52 (1.25, 1.85) | <0.001 | 1.19 (1.15, 1.22) | <0.001 | 1.28 | 0.03 | |
| 3–6 | 2.33 (1.94, 2.81) | <0.001 | 1.41 (1.37, 1.45) | <0.001 | 1.65 | <0.001 | |
| 7–29 | 3.20 (2.60, 3.94) | <0.001 | 1.77 (1.72, 1.83) | <0.001 | 1.81 | <0.001 | |
| Diabetes treatment | <0.001 | ||||||
| Non-insulin | Ref | Ref | Ref | ||||
| Insulin | 1.79 (1.61, 1.99) | <0.001 | 1.06 (1.04, 1.08) | <0.001 | 1.68 | <0.001 | |
Note: Adjusted multinomial logit regression model showing the relative risk ratios (RRRs) for severe dysglycemia and other-cause 30-day readmission compared to no readmission. The severe dysglycemia/other ratio is a ratio of the RRRs of severe dysglycemia and other-cause readmission. Specifically, a severe dysglycemia/other ratio >1 signifies a greater impact of the covariate on readmissions for severe dysglycemia than for other causes, and vice versa. The model was adjusted for the Charlson comorbidities (dementia, chronic obstructive pulmonary disease, rheumatologic disease, peptic ulcer disease, liver disease, hemiplegia/paraplegia, cancer, and AIDS/HIV), the discharge year, and the 20 principal diagnosis CCS categories from the index discharge with the highest risk of all-cause 30-day readmission
*The Wald p-value is a test of overall (joint) effect of multi-category variables† P-value for a two-sided test of the severe dysglycemia/other RRR being different from 1
Patients whose index hospitalization was for severe dysglycemia were nearly nine times as likely to be readmitted for recurrent severe dysglycemia than for another reasons. Among patients hospitalized for hypoglycemia, the RRR for severe dysglycemia readmission was 4.74 (95% CI, 3.81–5.89) and other-cause readmission was 0.87 (95% CI, 0.81–0.94), with a severe dysglycemia/other RRR ratio of 5.43. Severe hyperglycemia index hospitalizations had an even greater impact on severe dysglycemia readmission risk, with an RRR of severe dysglycemia readmission of 8.57 (95% CI, 7.08–10.37) and other-cause readmission of 0.60 (95% CI, 0.55–0.67); the severe dysglycemia/other RRR ratio was 15.89. Having prior hospitalizations for severe dysglycemia was also a risk factor for all readmissions, but readmission for severe dysglycemia was nearly four times as likely: RRR for severe dysglycemia readmission of 5.47 (95% CI, 4.60–6.51) and other-cause readmission of 1.43 (95% CI, 1.33–1.55) compared to no prior hospitalizations.
Readmission Following Severe Dysglycemic vs. Other Events
In a secondary analysis examining patients hospitalized for severe dysglycemia separately from those hospitalized for other causes (Online Appendix Tables 6 and 7), most risk factors for severe dysglycemia and other-cause readmissions remained unchanged, with few notable differences. While higher DCSI increased the risk of all readmissions following all index hospitalizations, it had the greatest impact on readmission risk following index stays for other (not severe dysglycemia) causes: DCSI ≥7 (compared to DCSI = 0) increased the risk of severe dysglycemia readmissions by RRR 3.66 (95% CI, 2.87–4.66) and other-cause readmissions by RRR 1.77 (95% CI, 1.71–1.82) after an index hospitalization for other causes, compared to RRR 1.91 (95% CI, 1.27–2.88) and RRR 2.01 (95% CI, 1.58–2.56) for severe dysglycemia and other-cause readmissions, respectively, following index hospitalization for severe dysglycemia. Longer LOS did not affect the risk of readmission for severe dysglycemia following index severe dysglycemic events, while increasing it following index hospitalizations for other causes.
DISCUSSION
The all-cause readmission rate among 342,186 U.S. adults with diabetes was 10.8%, reflective of the wide age and morbidity distribution of this commercially and Medicare Advantage-insured population. The vast majority, 97.4%, of the index hospitalizations were for causes not directly related to diabetes, with only 2.6% being primarily for the management of severe dysglycemia (48.1% hypoglycemia and 50.4% hyperglycemia). Similarly, 97.5% of all readmissions were for causes unrelated to short-term glycemic control, and 2.5% were specifically for severe dysglycemia, though the relative frequency of hypoglycemic and hyperglycemic events was reversed, with 61.0% of these events for hypoglycemia and 38.3% for hyperglycemia. The most common cause for hospitalization and readmission among these diabetes patients was heart failure, which is consistent with studies conducted in the general U.S. population.4 Still, despite being potentially avoidable with optimal ambulatory and transitional care,11 severe dysglycemia was the 11th most common cause for index hospitalization, the 14th most common cause for readmission following non-diabetes-related index hospitalizations, and the most common cause for readmission following an index hospitalization for severe dysglycemia.
Younger patients were the most likely to be readmitted for severe dysglycemia, with 10% of all readmissions among patients aged 18–44 years being for severe dysglycemia vs. just over 2% in the older age groups. This may reflect greater clinical complexity and multi-morbidity of older patients, placing them at risk for multiple diseases and complications unrelated to diabetes. Younger patients may have worse glycemic control or greater glycemic variability, both of which raise the risk of severe dysglycemia but cannot be captured by administrative data. Younger patients are also more likely to have type 1 diabetes, though administrative data cannot reliably identify diabetes type. Conversely, older patients may be treated less intensively and/or have greater attention paid to their diabetes management during and following hospitalization, which would lower their risk of severe dysglycemia. Similarly, older patients with complex health or social needs may have closer outpatient follow-up after discharge, decreasing their risk of unnoticed and unaddressed glycemic deterioration. These variables could not be assessed in the context of this study, but would benefit from further examination.
An index or prior hospitalization for severe dysglycemia was the strongest predictor of readmission for severe dysglycemia. Prior hospitalizations for severe dysglycemia increased the risk of readmission for severe dysglycemia sixfold, irrespective of the reason for the index hospitalization. Additionally, nearly one-third of patients whose index hospitalization was for severe dysglycemia were later readmitted for a recurrent severe dysglycemic event. The risk of recurrent dysglycemia was higher after an index hyperglycemic event (8.6-fold increase compared to index hospitalizations for other causes) than hypoglycemic event (4.7-fold increase). Still, while prior hospital stays for severe dysglycemia had a very strong impact on the likelihood of severe dysglycemia readmissions, these hospitalizations also increased the risk of other-cause readmissions, suggesting that severe dysglycemia may be a global marker of patient complexity and illness. The DCSI and insulin therapy had similar effects on severe dysglycemia and other-cause readmissions, with readmission risk increasing linearly with the DCSI but more steeply for dysglycemia-specific readmissions. This reinforces the fact that diabetes severity is an important consideration for all readmissions, not just those directly related to glycemic control.
Hospitalization is likely to affect the post-discharge diabetes management and overall health of patients with diabetes, and thereby increases the risk for readmission for severe dysglycemia, irrespective of the reason for the index admission. Diabetes management is affected by the patient’s nutrition, physical activity, sleep, pain, and non-diabetic drugs—all of which are potentially altered during and after hospitalization. This, in turn, may result in increased susceptibility to severe dysglycemic events. While we initially hypothesized that the risk of readmission for severe dysglycemia might be elevated following index hospitalization for other causes due to the relative de-prioritization of diabetes management in the context of an unrelated acute illness, this was not substantiated by the data. Patients hospitalized for causes other than severe dysglycemia were less likely to be readmitted for severe dysglycemia, while those hospitalized for severe dysglycemia had the greatest risk of readmission for recurrent severe dysglycemia. This observation is important, because it reinforces both the relative frequency and the high probability of recurrent severe dysglycemia, despite that fact that these events may be avoidable. Inpatient diabetes education has been shown to reduce the risk of readmission30 and may benefit high-risk patients. Similarly, medication review and reconciliation, care transition programs, and follow-up telephone calls or appointments that specifically address diabetes management may reduce the risk of readmission for severe dysglycemia. Such interventions could not be identified in our data set, and accounting for these programs or any outpatient follow-up after discharge would be problematic due to endogeneity.
This study needs to be considered in light of its limitations stemming from the use of administrative data, which cannot capture all potential risk factors for severe dysglycemia and readmission, including clinical information (e.g., hemoglobin A1c),31 frailty,32 social support, and socioeconomic factors. We classified hospitalizations on the basis of principal discharge diagnoses, which may underestimate the incidence of severe dysglycemia by capturing only primary dysglycemic events rather than severe dysglycemia precipitated by another potentially unrelated illness. Because patients were required to have ≥31 days of enrollment following index hospitalization, patients who died during this period were excluded, even though their death may have been informative. Our study was also limited to people with commercial or Medicare Advantage health plans, and did not include patients who were uninsured or had public health coverage. The population studied here fills the gap in readmissions literature that has heretofore focused predominantly on selected states or health systems,1 – 4 , 33 or on the Medicare fee-for-service population,6 , 8 , 9 as it includes people from a wide range of ages, racial/ethnic groups, health systems, and geographic regions.
These findings constitute novel and important contributions to the management of diabetes. While patients with diabetes are hospitalized and readmitted for a large number of health conditions, hospitalizations for severe dysglycemia remain common and have a high rate of recurrence. Younger patients and those with diabetes complications are at highest risk for severe dysglycemia readmission, and may benefit from diabetes-specific interventions. History of severe dysglycemia and burden of diabetes complications are also independent risk factors for all-cause readmission, and should be considered in the management of all hospitalized patients with diabetes.
Electronic supplementary material
(DOCX 63 kb)
Author Contributions
McCoy and Shah had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: McCoy, Shah. Acquisition of data: Herrin, Jeffrey, Shah. Interpretation of data: McCoy, Lipska, Herrin, Shah. Drafting of the manuscript: McCoy. Critical revision of the manuscript for important intellectual content: McCoy, Lipska, Herrin, Krumholz, Jeffrey, Shah. Statistical analysis: Herrin. Obtaining funding: Shah. Administrative, technical, and material support: N/A. Study supervision: Shah.
Compliance with Ethical Standards
Funders
This publication was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Dr. Shah was funded in part through project number R18HS18339 from the Agency for Healthcare Research and Quality (AHRQ). Dr. McCoy receives support from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. Lipska receives support from the National Institute on Aging and the American Federation of Aging Research through the Paul Beeson Career Development Award (K23AG048359) and the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342). She also receives support from CMS to develop and maintain publicly reported quality measures.
Prior Presentations
Parts of this work were previously presented as poster presentations at the American Diabetes Association 75th Scientific Sessions in Boston, MA (June 7, 2015), and the AcademyHealth Annual Research Meeting in Minneapolis, MN (June 15, 2015).
Conflict of Interest
Dr. Krumholz is a recipient of research agreements from Medtronic and Johnson & Johnson (Janssen), through Yale, to develop methods of clinical trial data sharing; is the recipient of a grant from Medtronic and the Food and Drug Administration, through Yale, to develop methods for post-market surveillance of medical devices; works under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures; chairs a cardiac scientific advisory board for UnitedHealth; is a participant/participant representative of the IBM Watson Health Life Sciences Board; is a member of the Advisory Board for Element Science, the Physician Advisory Board for Aetna, and the Open Trials Advisory Board for the Laura and John Arnold Foundation; and is the founder of Hugo, a personal health information platform. All remaining authors declare that they do not have a conflict of interest.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-017-4095-x) contains supplementary material, which is available to authorized users.
References
- 1.Jiang HJ, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421–1426. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- 2.Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: the case of diabetes. Am J Public Health. 2005;95(9):1561–1567. doi: 10.2105/AJPH.2004.044222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim H, Ross JS, Melkus GD, Zhao Z, Boockvar K. Scheduled and unscheduled hospital readmissions among patients with diabetes. Am J Manag Care. 2010;16(10):760–767. [PMC free article] [PubMed] [Google Scholar]
- 4.Donze J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171. doi: 10.1136/bmj.f7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raval AD, Zhou S, Wei W, Bhattacharjee S, Miao R, Sambamoorthi U. 30-Day Readmission Among Elderly Medicare Beneficiaries with Type 2 Diabetes. Popul Health Manag. 2015. [DOI] [PMC free article] [PubMed]
- 7.Eby E, Hardwick C, Yu M, et al. Predictors of 30 day hospital readmission in patients with type 2 diabetes: a retrospective, case-control, database study. Curr Med Res Opin. 2015;31(1):107–114. doi: 10.1185/03007995.2014.981632. [DOI] [PubMed] [Google Scholar]
- 8.Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116–1124. doi: 10.1001/jamainternmed.2014.1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Neil SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010;38(4):381–388. doi: 10.1016/j.amepre.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 10.Emons MF, Bae JP, Hoogwerf BJ, Kindermann SL, Taylor RJ, Nathanson BH. Risk factors for 30-day readmission following hypoglycemia-related emergency room and inpatient admissions. BMJ Open Diabetes Res Care. 2016;4(1):e000160. doi: 10.1136/bmjdrc-2015-000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.AHRQ QITM Research Version 5.0, Prevention Quality Indicators #1, Technical Specifications, Diabetes Short-Term Complications Admission Rate. March 2015. Available at: http://www.qualityindicators.ahrq.gov/. Accessed May 18, 2017.
- 12.Optum. Optum Research Data Assets. June 2015. Available at: https://www.optum.com/content/dam/optum/resources/productSheets/5302_Data_Assets_Chart_Sheet_ISPOR.pdf. Accessed May 18, 2017.
- 13.Wallace PJ, Shah ND, Dennen T, Bleicher PA, Crown WH. Optum Labs: Building A Novel Node In The Learning Health Care System. Health Aff (Millwood) 2014;33(7):1187–1194. doi: 10.1377/hlthaff.2014.0038. [DOI] [PubMed] [Google Scholar]
- 14.Privacy of Individually Identifiable Health Information: Other requirements relating to uses and disclosures of protected health information. 45 CFR 164.514(b)(1) (June 7, 2013). Available at: http://www.ecfr.gov/cgi-bin/retrieveECFR?gp=1&SID=ff85fb032e00c1b6d135ecf0767f18a0&ty=HTML&h=L&mc=true&r=PART&n=pt45.1.164#se45.1.164_1514. Accessed May 18, 2017.
- 15.National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) Comprehensive Diabetes Care. Washington, D.C.: National Committee for Quality Assurance; 2015:74–98.
- 16.Horwitz LI, Grady JN, Dorsey KB, et al. 2014 Measures Updates and Specifications Report: Hospital-Wide All-Cause Unplanned Readmission (Version 3.0). Submitted by Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). Prepared for Centers for Medicare & Medicaid Services (CMS). Available at file:///C:/Users/m070233/Downloads/Hosp-Wide_Rdmsn_Msr_Updts_032114.pdf2014.
- 17.National Quality Measures Clearinghouse. All-cause readmissions: the number of acute inpatient stays during the measurement year that were followed by an acute readmission for any diagnosis within 30 days and the predicted probability of an acute readmission, for patients 18 years of age and older. 2015; http://www.qualitymeasures.ahrq.gov/content.aspx?id=48857. Accessed May 18, 2017.
- 18.HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). Rockville: Agency for Healthcare Research and Quality; 2006–2009. [PubMed]
- 19.National Quality Measures Clearinghouse (NQMC). Measure summary: Diabetes short term complications admission: percentage of admissions for a principal diagnosis of diabetes with short-term complications per 100,000 population, ages 18 years and older. In: National Quality Measures Clearinghouse (NQMC) [Web site]. Rockville (MD): Agency for Healthcare Research and Quality (AHRQ); March 1, 2015. Available at: https://www.qualitymeasures.ahrq.gov/summaries/summary/49498. Accessed on May 18, 2017.
- 20.National Quality Measures Clearinghouse (NQMC). Measure summary: Uncontrolled diabetes admission: percentage of admissions for a principal diagnosis of diabetes without mention of short-term or long-term complications per 100,000 population, ages 18 years and older. In: National Quality Measures Clearinghouse (NQMC) [Web site]. Rockville (MD): Agency for Healthcare Research and Quality (AHRQ); March 1, 2015. Available at: https://www.qualitymeasures.ahrq.gov/summaries/summary/49503. Accessed on May 18, 2017.
- 21.Ginde AA, Blanc PG, Lieberman RM, Camargo CA., Jr Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord. 2008;8:4. doi: 10.1186/1472-6823-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.2015 Measure Updates and Specifications Report Hospital-Wide All-Cause Unplanned Readmission Measure – Version 4.0. Submitted by Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). Prepared for Centers for Medicare & Medicaid Services (CMS). March 2015. 22.; http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed May 18, 2017.
- 23.CMS. Centers for Medicare & Medicaid Services. Hospital Quality Initiative. Measure Methodology. 2016; https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed May 18, 2017.
- 24.Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008;14(1):15–23. [PMC free article] [PubMed] [Google Scholar]
- 25.Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care. 2012;18(11):721–726. [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KA, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 27.White HLJ. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–838. doi: 10.2307/1912934. [DOI] [Google Scholar]
- 28.Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. Berkeley: University of California Press; 1967. [Google Scholar]
- 29.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: Wiley; 1987. [Google Scholar]
- 30.Healy SJ, Black D, Harris C, Lorenz A, Dungan KM. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013;36(10):2960–2967. doi: 10.2337/dc13-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tomlin AM, Dovey SM, Tilyard MW. Risk factors for hospitalization due to diabetes complications. Diabetes Res Clin Pract. 2008;80(2):244–252. doi: 10.1016/j.diabres.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 32.Morandi A, Bellelli G, Vasilevskis EE, et al. Predictors of rehospitalization among elderly patients admitted to a rehabilitation hospital: the role of polypharmacy, functional status, and length of stay. J Am Med Dir Assoc. 2013;14(10):761–767. doi: 10.1016/j.jamda.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bennett KJ, Probst JC, Vyavaharkar M, Glover SH. Lower rehospitalization rates among rural Medicare beneficiaries with diabetes. J Rural Health. 2012;28(3):227–234. doi: 10.1111/j.1748-0361.2011.00399.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 63 kb)