Abstract
Background
Electronic cigarette (e-cigarette) use is rising in both the general and clinical populations. Little is known about e-cigarette use in primary care, where physicians report discussing e-cigarette use with patients.
Objective
Identify how and why smokers in primary care use e-cigarettes.
Design
Cross-sectional secondary data analysis from a randomized controlled trial of a tablet intervention to deliver the 5As for smoking cessation in primary care.
Participants
Current smokers aged 18 and older in three primary care clinics in San Francisco, CA (N = 788).
Main measures
Patients reported sociodemographics, cigarette smoking habits, quitting readiness, and ever and current use of e-cigarettes. We also asked reasons they have used or would use e-cigarettes. ICD-9 codes from the medical record determined comorbidities.
Key results
Fifty-two percent (n = 408) of patients reported ever using an e-cigarette, and 20% (n = 154) reported past-30-day use. Ever e-cigarette use was associated with younger age and negatively associated with being seen at practices at a public safety-net hospital compared to a practice at University-affiliated hospital. The most common reason for having used e-cigarettes among ever e-cigarette users, and for interest in future use of e-cigarettes among never e-cigarette users, was to cut down cigarette use. The mean number of days of e-cigarette use in the past 30 increased with duration of e-cigarette use. Most current e-cigarette users did not know the nicotine content of their e-cigarettes.
Conclusions
Over half of smokers in primary care have ever used e-cigarettes, and one-fifth are currently using them. Most reported using e-cigarettes to cut down or quit cigarettes. Primary care providers should be prepared to discuss e-cigarettes with patients. Screening for e-cigarette use may help identify and treat patients interested in changing their cigarette smoking habits.
Key words: substance abuse, primary care, comorbidity, alcoholism and addictive behavior
Introduction
As the prevalence of e-cigarette use increases in the general US population,1 , 2 a similar trend is emerging among clinical populations and those with comorbid medical conditions. A study of hospitalized smokers showed that past-30-day e-cigarette use rose from 1.1% to 18.4% between 2010 and 2013.3 Between 2012 and 2013, prevalence of e-cigarette use in a population of cancer patients who smoke tripled from 10.6% to 38.5%.4 High prevalence of use has also been seen in smokers after acute coronary syndrome5 and in smokers who are preoperative for elective surgery.6 As of 2014, the prevalence of ever and current e-cigarette use among adult smokers in the US was 47.6% and 15.9%, respectively.7
The most commonly reported reasons for e-cigarette use among adults are smoking cessation and smoking-induced health concerns.8 , 9 Smokers perceive e-cigarettes as significantly less harmful than conventional cigarettes.10 Cessation and health-related claims are also prevalent in e-cigarette marketing.11 – 13 While e-cigarettes have been found to contain lower amounts of many toxicants than conventional cigarettes,14 , 15 the long-term health effects of e-cigarettes are unknown. Furthermore, concerns remain about the potential toxicity of some components of e-cigarettes, such as flavorings.16 – 18
Many patients receive tobacco cessation treatment and counseling in primary care settings, where discussions about e-cigarettes also take place.19 – 22 However, many providers report lacking confidence in their knowledge about e-cigarettes and their ability to talk to their patients about these new products.22 Identifying e-cigarette users in primary care and understanding how and why they use the products can better inform conversations between providers and patients. Furthermore, it may help to identify more smokers who are interested in, or in the process of, making changes in their cigarette smoking behavior, and provide opportunities to assist smokers in quit attempts.
Given the paucity of data on e-cigarette use among patients in primary care settings, we aimed to (1) identify the prevalence of e-cigarette use among patients in primary care clinics, (2) describe these e-cigarette users and how they are using e-cigarettes, and (3) explore the reasons for e-cigarette use and interest in future use in this population. Since most smokers report having seen a health care provider in the past 12 months,23 we hypothesized that the prevalence of ever and current e-cigarette use in this primary care population would be similar to that of the general adult population7 and hospitalized adults.3 However, since prevalence of e-cigarette use varies by medical comorbidity,24 the patterns of use in this primary care population may be influenced by the prevalence of chronic medical conditions in study participants. Specifically, our study participants have a high prevalence of HIV, and little is known about e-cigarette use in this population. We also hypothesized that e-cigarette use would be more prevalent in younger adults, as has been seen in the general adult population and hospitalized patients,3 , 7 and that the most common reason for use would be to quit or cut down cigarettes.8 , 9
Methods
Study population
From 2014 to 2015, we collected cross-sectional data from current cigarette smokers enrolled in a randomized controlled trial (RCT) of a tablet intervention to deliver the 5As for smoking cessation in adult primary care clinics in San Francisco, California.25 Participants could participate in the RCT up to three times; however, only data from each participant’s first attempt were included in the present study. We recruited patients from three adult academic primary care practices 1: University of California San Francisco General Internal Medicine Clinic (UCSF GIM), 2: San Francisco General Hospital General Medicine Clinic (SFGH GMC), which is located at a public safety-net hospital, and 3: the UCSF Positive Health Program (PHP) at SFGH, an HIV primary care practice at a public safety-net hospital. Inclusion criteria included: age 18 years or older, English- or Spanish-speaking, and having smoked at least 100 cigarettes in their lifetime with the most recent cigarette use in the past 7 days.
Measures
Participants completed a baseline questionnaire on a computer tablet just prior to their acute or primary care appointment at one of the three study sites. On the tablet, patients self-reported information about sociodemographics (age, sex, race/ethnicity, and education), type of health insurance, smoking habits, and level of readiness to quit. Within 72 h of their office visit, patients had either a telephone or in-person interview during which they were asked questions about their provider visit, smoking habits, and e-cigarette use. Specifically, participants reported the number of days per week they smoke cigarettes, cigarettes smoked per day, time to first cigarette in the morning (30 min or less or more than 30 min), and whether they were interested in quitting cigarettes (responses categorized as already quit/will quit in the next month, may quit in next 6 months, and not interested/do not know).
Participants self-reported whether they had ever heard of e-cigarettes and had ever used even one puff of an e-cigarette. We classified ever e-cigarette users who had used e-cigarettes in the past 30 days as current e-cigarette users and those who had not used any e-cigarettes in the past 30 days as former e-cigarette users. Ever e-cigarette users reported how long they have been using (for current users) or had used (for former users) e-cigarettes (< 1 month, 1–6 months, 6–12 months, or > 12 months) and what concentration of nicotine they usually use or used in their e-cigarette (0 mg, 1-12 mg, 12-24 mg, 25 + mg, or do not know). Current e-cigarette users reported on how many of the past 30 days they used an e-cigarette. Participants were asked whether they ever used or ever would use e-cigarettes for each of the following seven reasons (all response options were yes or no, and participants could answer yes for more than one reason): “to help me quit smoking,” “curious and interested in trying something new,” “to cut down the number of cigarettes I smoke,” “because I think they are less harmful than tobacco cigarettes,” “for use in places where smoking is banned,” “because they are inexpensive,” and “because the vapor does not smell.” We asked about these specific reasons based on prior studies.26 – 28 Participants who reported never using an e-cigarette were asked whether they would ever use e-cigarettes for the above reasons.
We determined patient comorbidities from electronic heath records using ICD-9 codes. Specific comorbidities that we extracted included: mental illness (ICD-9 295.xx, 296.xx, 300.xx, 309.81, 311), alcohol dependence (303.xx), drug dependence (304.xx), HIV (V08, 042), hypertension (401.xx-405.xx), ischemic heart disease (410.xx-414.xx), cancer excluding non-melanoma skin cancer (140.xx-172.xx, 174.xx-195.8, 200.xx-208.xx, 238.6), asthma (493.xx), COPD (491.xx, 492.xx, 496.xx), and cerebrovascular disease (362.34, 430.xx-438.xx). Comorbidities were available for approximately half of participants, because participants were not routinely asked to provide medical record numbers by all study staff. Specifically, data on mental illness, alcohol and drug dependence, cancer, asthma, COPD, and cerebrovascular disease were missing in 331 participants (42%); data on hypertension and ischemic heart disease were missing in 425 participants (54%); data on HIV were missing in 426 participants (54%).
Analysis
We compared ever e-cigarette users to never e-cigarette users using t-tests for continuous variables and chi-square tests for categorical variables. Any variable with a p value <0.20 in these univariate analyses was included in a multivariable logistic regression model with sociodemographic variables to examine factors associated with ever e-cigarette use. We also compared current versus former e-cigarette users using univariate and multivariable analyses as above. Primary analyses excluded individuals with missing data. We also conducted sensitivity analyses on the full study sample excluding the comorbidity variables that were missing in over 40% of participants. In exploratory analyses, current and former e-cigarette users who used e-cigarettes for at least 1 month were also compared to those who used e-cigarettes for less than 1 month.
Results
Prevalence of E-cigarette use
A total of 788 unique participants were included in the analyses. Over half of participants (52%) reported ever use of e-cigarettes (n = 408): 20% were current e-cigarette users (n = 154), and 32% were former users (n = 253). In descriptive analyses, compared to never e-cigarette users, ever e-cigarette users were younger, non-Hispanic white, more educated, seen at UCSF GIM, more likely to be daily smokers, smoked more cigarettes per day, and smoked their first cigarette within 30 min of waking (Table 1). Fewer ever e-cigarette users had ICD-9 diagnoses of hypertension, ischemic heart disease, and alcohol dependence compared to never e-cigarette users. In multivariable logistic regression, odds of e-cigarette ever use were lower among those who were older (p = 0.001) and those receiving care from SFGH GMC (p = 0.03) and PHP (p = 0.04) (Table 3). The sensitivity analysis found similar findings in terms of age, but also higher odds of ever e-cigarette use among participants of non-Hispanic race/ethnicity (p = 0.04) and lower odds of ever e-cigarette use in those with low interest quitting cigarettes (p = 0.02).
Table 1.
Characteristics of Study Participants by E-cigarette Use Status
| Never e-cigarette use (n = 380) |
Ever e-cigarette use* (n = 408) |
P value | |
|---|---|---|---|
| Age, mean (SD) | 53.8 (10.3) | 48.4 (11.2) | <0.001 |
| Female sex, n(%) | 138 (37) | 148 (36) | 0.9 |
| Race/ethnicity, n(%) | <0.001 | ||
| Non-Hispanic white | 86 (26) | 126 (36) | |
| Non-Hispanic black | 153 (46) | 105 (30) | |
| Hispanic | 57 (17) | 67 (19) | |
| Other non-Hispanic | 24 (7) | 36 (10) | |
| Multiple race, non-Hispanic | 12 (4) | 17 (5) | |
| Level of education, n(%) | 0.002 | ||
| Less than high school | 99 (28) | 68 (17) | |
| High school diploma/GED | 97 (27) | 111 (28) | |
| Some college | 107 (30) | 159 (40) | |
| 4 Year degree or higher | 56 (16) | 57 (14) | |
| Insurance, n(%) | 0.07 | ||
| HMO/PPO | 12 (3) | 25 (6) | |
| Medicare | 96 (26) | 73 (18) | |
| Medicaid | 211 (58) | 244 (62) | |
| Healthy SF/Healthy Workers | 39 (11) | 49 (12) | |
| Other | 3 (1) | 3 (1) | |
| None | 3 (1) | 2 (1) | |
| Clinic site, n(%) | 0.009 | ||
| UCSF GIM | 88 (23) | 123 (30) | |
| SFGH GMC | 131 (34) | 103 (25) | |
| PHP | 161 (42) | 182 (45) | |
| Daily smoker, n(%) | 293 (77) | 340 (83) | 0.03 |
| Cigarettes per day, mean (SD) | 9.2 (7.9) | 10.9 (8.5) | 0.004 |
| Interest in quitting, n(%) | 0.1 | ||
| Within next month/already quit | 112 (30) | 140 (34) | |
| Maybe in 6 months | 168 (44) | 184 (45) | |
| Do not know/not interested | 99 (26) | 84 (21) | |
| First cigarette within 30 min of waking, n(%) | 207 (54) | 258 (63) | 0.01 |
| Comorbid conditions, n(%)† | |||
| Hypertension | 137 (78) | 112 (60) | <0.001 |
| Chronic obstructive pulmonary disease | 59 (28) | 72 (30) | 0.6 |
| Asthma | 44 (21) | 57 (23) | 0.5 |
| Ischemic heart disease | 45 (26) | 31 (16) | 0.03 |
| Stroke | 27 (13) | 28 (12) | 0.7 |
| Cancer | 40 (19) | 30 (12) | 0.06 |
| HIV | 86 (49) | 110 (59) | 0.07 |
| Mental illness | 153 (72) | 192 (79) | 0.06 |
| Drug dependence | 80 (37) | 98 (40) | 0.5 |
| Alcohol dependence | 49 (23) | 38 (16) | 0.049 |
GED = General Educational Development; UCSF GIM = University of California San Francisco General Internal Medicine Clinic; SFGH GMC = San Francisco General Hospital General Medicine Clinic; PHP = UCSF Positive Health Practice at San Francisco General Hospital; HIV = human immunodeficiency virus
*Defined as having ever used even one puff of an e-cigarette
†Data on mental illness, alcohol and drug dependence, cancer, asthma, COPD, and cerebrovascular disease were missing in 331 participants; data on hypertension and ischemic heart disease were missing in 425 participants; data on HIV were missing in 426 participants
Table 3.
Predictors of Ever and Current E-cigarette Use*
| Ever vs. never use aOR (95% CI) | Current vs. former use aOR (95% CI) | |
|---|---|---|
| Age | 0.95 (0.93–0.98) | 1.01 (0.98–1.03) |
| Female sex | 1.13 (0.63–2.01) | 0.52 (0.25–1.07) |
| Non-Hispanic white race/ethnicity | 1.01 (0.56–1.82) | 1.17 (0.61–2.25) |
| Level of education | ||
| Less than high school | 0.66 (0.27–1.63) | 1.74 (0.53–5.73) |
| High school diploma/GED | 1.13 (0.47–2.75) | 1.24 (0.40–3.80) |
| Some college | 1.11 (0.49–2.50) | 1.23 (0.43–3.56) |
| 4 Year degree or higher | ref | ref |
| Medicaid insurance | 1.36 (0.82–2.26) | 1.88 (0.97–3.62) |
| Clinic site | ||
| UCSF GIM | ref | ref |
| SFGH GMC | 0.40 (0.17–0.92) | 1.02 (0.43–2.46) |
| PHP | 0.45 (0.21–0.97) | 0.96 (0.44–2.09) |
| Daily smoker | 1.38 (0.68–2.80) | 0.69 (0.29–1.64) |
| Cigarettes per day | 1.02 (0.99–1.06) | -- |
| Interest in quitting | ||
| Within next month/already quit | ref | -- |
| Maybe in 6 months | 0.81 (0.45–1.47) | -- |
| Do not know/not interested | 0.59 (0.30–1.15) | -- |
| First cigarette within 30 min of waking | 1.06 (0.59–1.90) | 0.69 (0.36–1.34) |
| Comorbid conditions† | ||
| Hypertension | 0.59 (0.33–1.07) | -- |
| Ischemic heart disease | 1.13 (0.58–2.19) | -- |
| Cancer | 0.68 (0.33–1.38) | 0.58 (0.21–1.61) |
| Mental illness | 1.11 (0.60–2.04) | -- |
| Alcohol dependence | 0.92 (0.51–1.69) | -- |
GED = General Educational Development; UCSF GIM = University of California San Francisco General Internal Medicine Clinic; SFGH GMC = San Francisco General Hospital General Medicine Clinic; PHP = UCSF Positive Health Practice at San Francisco General Hospital; ref. = referent group
*Ever e-cigarette use is defined as having ever tried even one puff of an e-cigarette; former e-cigarette use is defined as having ever tried an e-cigarette, but no use in the past 30 days; current e-cigarette use is defined as use within the past 30 days
†HIV not included in regression models because almost all participants with HIV were seen in the PHP clinic
--: Not included in model because p > 0.2 in univariate analyses
Boldface indicates statistical significance (p < 0.05)
In univariate analyses, fewer current e-cigarette users were daily cigarette smokers compared to former e-cigarette users (Table 2). No variables were significantly associated with current e-cigarette use versus former use in multivariable analyses (Table 3) and in the sensitivity analysis.
Table 2.
Characteristics of Former and Current E-cigarette Users* †
| Former e-cigarette use (n = 253) |
Current e-cigarette use (n = 154) |
P value | |
|---|---|---|---|
| Age, mean (SD) | 48.8 (11.5) | 47.7 (10.7) | 0.3 |
| Female sex, n(%) | 100 (40) | 48 (31) | 0.08 |
| Race/ethnicity, n(%) | 0.9 | ||
| Non-Hispanic white | 81 (37) | 45 (34) | |
| Non-Hispanic black | 62 (28) | 43 (33) | |
| Hispanic | 42 (19) | 25 (19) | |
| Other non-Hispanic | 22 (10) | 13 (10) | |
| Multiple race, non-Hispanic | 11 (5) | 6 (5) | |
| Level of education, n(%) | 0.98 | ||
| Less than high school | 42 (17) | 26 (18) | |
| High school diploma/GED | 69 (28) | 42 (28) | |
| Some college | 98 (40) | 60 (41) | |
| 4 Year degree or higher | 37 (15) | 20 (14) | |
| Insurance, n(%) | 0.3 | ||
| HMO/PPO | 16 (7) | 8 (5) | |
| Medicare | 44 (18) | 29 (19) | |
| Medicaid | 145 (59) | 99 (66) | |
| Healthy SF/Healthy Workers | 36 (15) | 13 (9) | |
| Other | 3 (1) | 0 (0) | |
| None | 1 (0.4) | 1 (1) | |
| Clinic site, n(%) | 0.2 | ||
| UCSF GIM | 84 (33) | 38 (25) | |
| SFGH GMC | 60 (24) | 43 (28) | |
| PHP | 109 (43) | 73 (47) | |
| Daily smoker, n(%) | 221 (87) | 118 (77) | 0.005 |
| Cigarettes per day, mean (SD) | 11.1 (8.8) | 10.6 (8.0) | 0.5 |
| Interest in quitting, n(%) | 0.2 | ||
| Within next month/already quit | 82 (32) | 58 (38) | |
| Maybe in 6 months | 123 (49) | 61 (40) | |
| Do not know/not interested | 48 (19) | 35 (23) | |
| First cigarette within 30 min of waking, n(%) | 161 (64) | 97 (63) | 0.9 |
| Comorbid conditions, n(%)†† | |||
| Hypertension | 72 (59) | 40 (61) | 0.8 |
| Chronic obstructive pulmonary disease | 49 (31) | 23 (27) | 0.6 |
| Asthma | 34 (21) | 23 (27) | 0.3 |
| Ischemic heart disease | 22 (18) | 9 (14) | 0.4 |
| Stroke | 16 (10) | 12 (14) | 0.3 |
| Cancer | 23 (14) | 7 (8) | 0.17 |
| HIV | 70 (58) | 40 (60) | 0.9 |
| Mental illness | 128 (81) | 64 (76) | 0.4 |
| Drug dependence | 60 (38) | 38 (45) | 0.3 |
| Alcohol dependence | 23 (14) | 15 (18) | 0.5 |
GED = General Educational Development; UCSF GIM = University of California San Francisco General Internal Medicine Clinic; SFGH GMC = San Francisco General Hospital General Medicine Clinic; PHP = UCSF Positive Health Practice at San Francisco General Hospital; HIV = human immunodeficiency virus
*Total N = 787; one ever e-cigarette user was missing data on past 30-day use and was excluded from these analyses
†Former e-cigarette use is defined as having ever tried an e-cigarette, but no use in the past 30 days; current e-cigarette use is defined as use within the past 30 days
††Data on mental illness, alcohol and drug dependence, cancer, asthma, COPD, and cerebrovascular disease were missing in 331 participants; data on hypertension and ischemic heart disease were missing in 425 participants; data on HIV were missing in 426 participants
Patterns of E-cigarette use
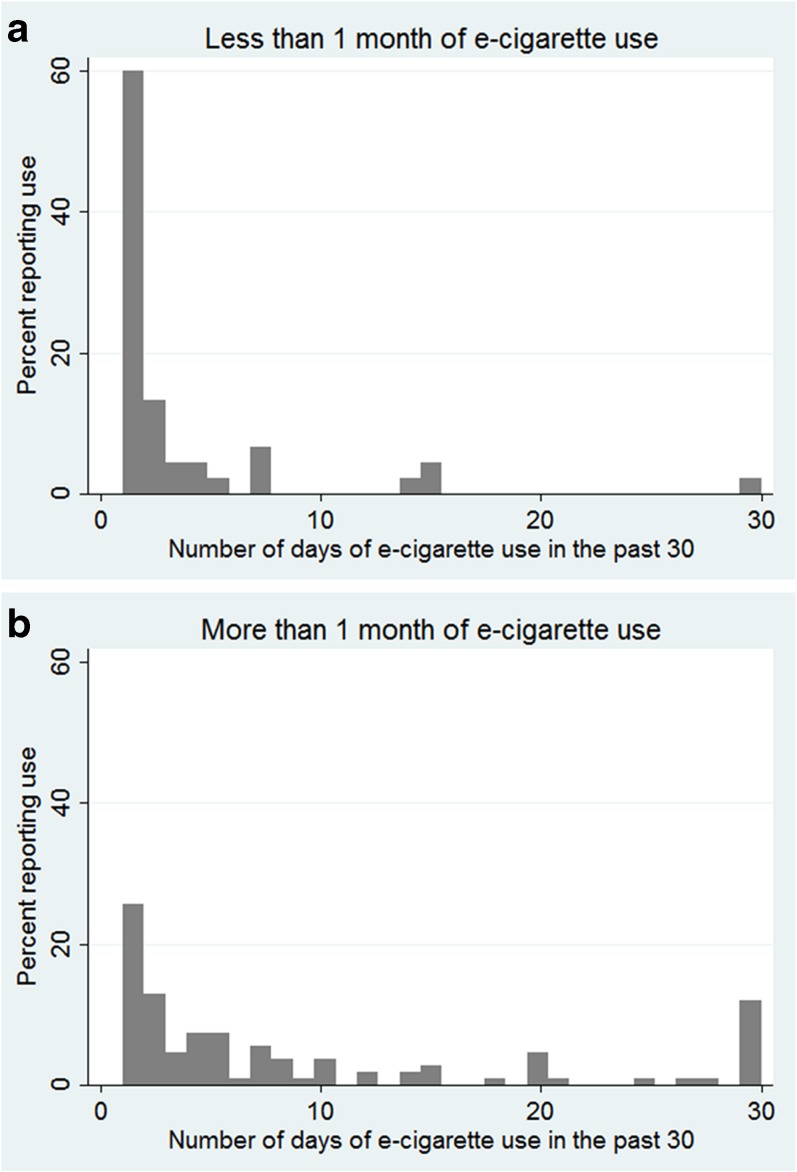
The mean number of days of e-cigarette use in the past 30 days was 7.3 among current e-cigarette users. Nine percent of current e-cigarette users reported daily e-cigarette use, and 66% reported 5 or fewer days of e-cigarette use in the past 30 days. Among current e-cigarette users, 29% reported e-cigarette use for less than 1 month, 34% reported use for 1–6 months, 15% reported use for 6–12 months, and 21% reported use for over 12 months. Distribution of days of e-cigarette use by duration of e-cigarette use is shown in Fig. 1. The percentage of current e-cigarette users who reported less than 1 month of e-cigarette use who used 5 or fewer e-cigarettes per day was 84% compared to 62% of those reporting 1–6 months of use, 48% of those reporting 6–12 months of use, and 58% of those reporting over 12 months of use. Only 2% of those reporting less than 1 month of e-cigarette use were daily users compared to 13% of those reporting 1–6 months of use, 9% of those reporting 6–12 months of use, and 12% of those reporting over 12 months of use.
Fig. 1.
Number of days of e-cigarette use in the past 30 in current e-cigarette users who report (a) less than 1 month of e-cigarette use and (b) more than 1 month of e-cigarette use
Most (60%) current e-cigarette users did not know the concentration of nicotine used in their e-cigarettes, 7% reported using no-nicotine e-cigarettes, 10% reported using 1-12 mg of nicotine, 19% reported using 12-24 mg of nicotine, and 4% reported using 25 mg or more of nicotine.
In exploratory analyses, there was no significant difference in sociodemographics among current e-cigarette users who reported over 1 month of e-cigarette use (n = 311) compared to those reporting less than 1 month of use (n = 97). A higher percentage of participants who reported over 1 month of e-cigarette use was receiving care from SFGH PHP (50% versus 27%; p < 0.001; data not shown in tables).
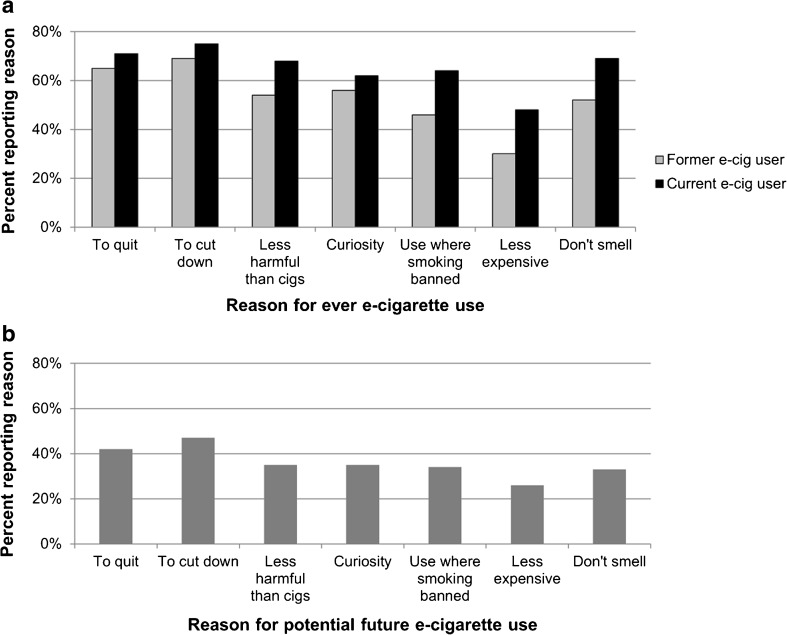
Reasons for E-cigarette use
The reasons that current and former e-cigarette users report for using e-cigarettes are shown in Fig. 2a. Among current e-cigarette users, 84% reported using e-cigarettes to quit cigarettes, to cut down on cigarettes, or because they believe they are less harmful than cigarettes. The least common reason for use was cost (48%). Among former e-cigarette users, 78% reported using e-cigarettes to quit cigarettes, to cut down on cigarettes, or because they believe they are less harmful than cigarettes, and the least common reason was also cost (30%).
Fig. 2.
Reasons for ever e-cigarette use among current and former e-cigarette users (a) and for potential future use among never e-cigarette users (b)
Over half of never e-cigarette users (57%) reported that they would use e-cigarettes for at least one reason. To cut down cigarettes was the most common reason for interest in future use among never e-cigarette users (47%), while cost was the least common reason for future e-cigarette use (27%) (Fig. 2b).
In exploratory analyses, compared to those using e-cigarettes for less than 1 month, more participants who used e-cigarettes for over 1 month reported using e-cigarettes to cut down on cigarettes (74% versus 62%, p = 0.02), because they are less expensive than cigarettes (40% versus 25%, p = 0.01), and because e-cigarettes do not smell (62% versus 48%, p = 0.02; data not shown in tables).
Discussion
Cigarette smokers in adult primary care clinics report high rates of e-cigarette use. In this sample of current cigarette smokers in San Francisco, California, the prevalence of ever and current e-cigarette use were 52% and 20%, respectively. Similar to other studies and as we hypothesized, those who reported using e-cigarettes in this study were younger.2 , 3 , 7 , 29 Most e-cigarette users reported using e-cigarettes to cut down or quit cigarettes, and over half of never e-cigarette users reported that they would use e-cigarettes in the future.
As hypothesized, the estimates of e-cigarette use in primary care populations we obtained in this study were consistent with estimates of ever (48%) and current (16%) e-cigarette use in the general US population.7 Additionally, as we hypothesized, the most common reasons for e-cigarette use among current e-cigarette users in our study were to reduce or quit cigarette use, because they perceive e-cigarettes as less harmful than cigarettes, and because the vapor does not smell, which is similar to a national sample of US adults in 2014 in which 84.5% reported use for cessation/health and 71.5% for consideration of others.8 Patients should be counseled that the long-term health effects of e-cigarette use and secondhand exposure to e-cigarette vapor are unknown. Additionally, with few clinical trials on the use and efficacy of e-cigarettes for smoking cessation,30 and the varied quality and results from observational studies on this topic,31 whether e-cigarettes help smokers quit cigarettes is uncertain. Until more data are available, primary care providers and smoking cessation counselors should encourage patients to use existing evidence-based tools to improve success of cigarette quit attempts.
The overall number of days of e-cigarette use among current users was low, with two-thirds of current e-cigarette users reporting 5 or fewer days of e-cigarette use in the past 30 days. This is in contrast to a previous study of adults in Minnesota in 2014, where most current smokers used e-cigarettes between 6 to 29 of the past 30 days.32 In our study, patients who reported longer durations of e-cigarette use (e.g., over 1 month) used e-cigarettes on more days than those who used e-cigarettes for shorter durations; however, even among those who reported over 12 months of use, over half were using e-cigarettes on 5 or fewer days per month. One potential reason for the infrequent use in our study population is the high percentage of people of non-Hispanic black race/ethnicity who have been shown to use e-cigarettes less frequently compared to non-Hispanic white and Hispanic individuals in a previous study.33
The majority of current e-cigarette users in this study did not know the concentration of nicotine used in their e-cigarettes. This is concerning because it suggests that patients may not pay attention to the labels on e-cigarettes. It is important for consumers to know the concentration, because if patients do not realize that they are using a nicotine-containing product, they (and their physicians) may not be aware that they are continuing to use an addictive product. As of 2018, new FDA regulations will require a warning statement that indicates when a product contains nicotine and that nicotine is addictive.34 This may increase consumers’ awareness of the contents of the products that they are consuming.
Primary care providers need to be aware of the high rates of dual product use (i.e., use of both cigarettes and e-cigarettes) among cigarette smokers, as this may impact their communication with patients around tobacco use and treatment in clinical settings. Patients are already talking to primary care providers and specialists about e-cigarettes.19 , 20 , 22 One recent study of 561 US physicians (33% primary care, 36% pulmonology, and 31% surgery) found that 70% reported that their patients ask them about e-cigarettes at least 25% of the time.22 Another study of 150 physicians found that 65% of physicians (including primary care, oncology, cardiology, and pulmonology) had been asked about e-cigarettes by their patients.19 Physicians should therefore be prepared for discussions on the topic, which may be challenging with many physicians lacking confidence in their ability to answer patients’ questions about e-cigarettes.22 Further guidance from professional organizations in general medicine and educational efforts can help physicians faced with these questions to improve their confidence in communicating with patients more effectively. Providers should also incorporate screening for e-cigarette use into screening of patients for tobacco use. Since patients who endorse e-cigarette use are often using them for smoking cessation or reduction, screening can provide an opportunity to identify and assist patients interested in quitting cigarettes and taking steps toward improving their health. Academic detailing, which has been effective in primary care populations in improving use of alcohol screening and brief interventions,35 providing tobacco dependence treatment to underserved populations,36 and in increasing referrals to tobacco quitlines,37 may also be an effective tool for improving physician screening and knowledge.
This study has a number of limitations. First, we do not have detailed information about the characteristics of smokers in these practices, and the sampling design of the parent RCT was not probability-based; therefore, the participants may not be representative of all smoking patients at these sites. Since the data were collected in one city and over 70% of patients were from public safety-net hospital-based practices, findings may not be generalizable to other populations. Second, data other than comorbidities were collected by patient self-report and are thus subject to bias. Third, we only have data on the frequency of use of e-cigarettes for current e-cigarette users, and what percentage of ever e-cigarette users tried e-cigarettes only once is not known. Most former e-cigarette users, however, reported having used e-cigarettes for over 1 month (30% used for 1–6 months, 16% used for 6–12 months, and 34% used for over 12 months), suggesting more than just one use in the past. Fourth, participants responded to seven yes/no questions about reasons for e-cigarette use; however, there could have been other reasons for use that were not captured by these measures. Finally, data on comorbidities were missing on over 40% of participants. Our sensitivity analyses suggest that factors in addition to age, such as race/ethnicity and interest in quitting cigarettes, may be important predictors of e-cigarette use in this population and should be addressed in future research.
Over half of smokers in adult primary care clinics have used e-cigarettes at least once, with one in five reporting current use. Current e-cigarette use is intermittent in this population, with most patients reporting non-daily use. Most patients who smoke cigarettes use e-cigarettes to quit or cut down on cigarettes or because they view them as a less harmful product than cigarettes. Screening of patients for e-cigarette use along with other tobacco use may help identify those interested in changing their smoking habits and provide an opportunity for evidence-based smoking cessation treatment and counseling.
Acknowledgements
This work was supported by NIH National Institute on Drug Abuse R01DA034253. The funding source had no role in the study design, in the collection, analysis, and interpretation of the data, in the writing of the manuscript, or in the decision to submit for publication.
Compliance with ethical standards
Conflicts of interest
Dr. Kalkhoran receives royalties from Uptodate, Inc., for contributing to a chapter on electronic cigarettes. All remaining authors declare that they do not have a conflict of interest.
References
- 1.King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010-2013. Nicotine Tob Res. 2015;17(2):219–27. doi: 10.1093/ntr/ntu191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McMillen RC, Gottlieb MA, Shaefer RM, Winickoff JP, Klein JD. Trends in electronic cigarette use among US adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17(10):1195–202. doi: 10.1093/ntr/ntu213. [DOI] [PubMed] [Google Scholar]
- 3.Rigotti NA, Harrington KF, Richter K, Fellows JL, Sherman SE, Grossman E, et al. Increasing prevalence of electronic cigarette use among smokers hospitalized in 5 US cities, 2010-2013. Nicotine Tob Res. 2015;17(2):236–44. doi: 10.1093/ntr/ntu138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borderud SP, Li Y, Burkhalter JE, Sheffer CE, Ostroff JS. Electronic cigarette use among patients with cancer: characteristics of electronic cigarette users and their smoking cessation outcomes. Cancer. 2014;120(22):3527–35. doi: 10.1002/cncr.28811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Busch AM, Leavens EL, Wagener TL, Buckley ML, Tooley EM. Prevalence, reasons for use, and risk perception of electronic cigarettes among post-acute coronary syndrome smokers. J Cardiopulm Rehabil Prev. 2016;36(5):352–7. doi: 10.1097/HCR.0000000000000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kadimpati S, Nolan M, Warner DO. Attitudes, beliefs, and practices regarding electronic nicotine delivery systems in patients scheduled for elective surgery. Mayo Clin Proc. 2015;90(1):71–6. doi: 10.1016/j.mayocp.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Schoenborn CA, Gindi RM. Electronic cigarette use among adults: United States. NCHS Data Brief. 2014;2015(217):1–8. [PubMed] [Google Scholar]
- 8.Patel D, Davis KC, Cox S, Bradfield B, King BA, Shafer P, et al. Reasons for current E-cigarette use among US adults. Prev Med. 2016. doi:10.1016/j.ypmed.2016.09.011 [DOI] [PMC free article] [PubMed]
- 9.Rutten LJ, Blake KD, Agunwamba AA, Grana RA, Wilson PM, Ebbert JO, et al. Use of e-cigarettes among current smokers: associations among reasons for use, quit intentions, and current tobacco use. Nicotine Tob Res. 2015;17(10):1228–34. doi: 10.1093/ntr/ntv003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pepper JK, Emery SL, Ribisl KM, Rini CM, Brewer NT. How risky is it to use e-cigarettes? Smokers’ beliefs about their health risks from using novel and traditional tobacco products. Journal of behavioral medicine. 2015;38(2):318–26. doi: 10.1007/s10865-014-9605-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein EG, Berman M, Hemmerich N, Carlson C, Htut S, Slater M. Online e-cigarette marketing claims: a systematic content and legal analysis. Tobacco regulatory science. 2016;2(3):252–62. doi: 10.18001/TRS.2.3.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grana RA, Ling PM. "Smoking revolution": a content analysis of electronic cigarette retail websites. Am J Prev Med. 2014;46(4):395–403. doi: 10.1016/j.amepre.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramamurthi D, Gall PA, Ayoub N, Jackler RK. Leading-brand advertisement of quitting smoking benefits for e-cigarettes. Am J Public Health. 2016:e1-e7. doi:10.2105/ajph.2016.303437 [DOI] [PMC free article] [PubMed]
- 14.Margham J, McAdam K, Forster M, Liu C, Wright C, Mariner D, et al. Chemical composition of aerosol from an e-cigarette: a quantitative comparison with cigarette smoke. Chem Res Toxicol. 2016. doi:10.1021/acs.chemrestox.6b00188 [DOI] [PubMed]
- 15.Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–9. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kosmider L, Sobczak A, Prokopowicz A, Kurek J, Zaciera M, Knysak J, et al. Cherry-flavoured electronic cigarettes expose users to the inhalation irritant, benzaldehyde. Thorax. 2016;71(4):376–7. doi: 10.1136/thoraxjnl-2015-207895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barrington-Trimis JL, Samet JM, McConnell R. Flavorings in electronic cigarettes: an unrecognized respiratory health hazard? Jama. 2014;312(23):2493–4. doi: 10.1001/jama.2014.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tierney PA, Karpinski CD, Brown JE, Luo W, Pankow JF. Flavour chemicals in electronic cigarette fluids. Tob Control. 2016;25(e1):e10–5. doi: 10.1136/tobaccocontrol-2014-052175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinberg MB, Giovenco DP, Delnevo CD. Patient–physician communication regarding electronic cigarettes. Preventive Medicine Reports. 2015;2:96–8. doi: 10.1016/j.pmedr.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Shahawy O, Brown R, Elston LJ. Primary care physicians’ beliefs and practices regarding e-cigarette use by patients who smoke: a qualitative assessment. International Journal of Environmental Research and Public Health. 2016;13(5):445. doi: 10.3390/ijerph13050445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kandra KL, Ranney LM, Lee JGL, Goldstein AO. Physicians’ attitudes and use of e-cigarettes as cessation devices, North Carolina, 2013. PLoS ONE. 2014;9(7):e103462. doi: 10.1371/journal.pone.0103462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nickels AS, Warner DO, Jenkins SM, Tilburt J, Hays JT. Beliefs, practices, and self-efficacy of US physicians regarding smoking cessation and electronic cigarettes: a national survey. Nicotine Tob Res. 2016. doi:10.1093/ntr/ntw194 [DOI] [PubMed]
- 23.Danesh D, Paskett ED, Ferketich AK. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev Chronic Dis. 2014;11:E131. doi: 10.5888/pcd11.140053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kruse GR, Kalkhoran S, Rigotti NA. Use of electronic cigarettes among US adults with medical comorbidities. Am J Prev Med. 2017. doi:10.1016/j.amepre.2016.12.004 [DOI] [PMC free article] [PubMed]
- 25.Kalkhoran S, Appelle NA, Napoles AM, Munoz RF, Lum PJ, Alvarado N, et al. Beyond the ask and advise: implementation of a computer tablet intervention to enhance provider adherence to the 5As for smoking cessation. J Subst Abuse Treat. 2016;60:91–100. doi: 10.1016/j.jsat.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vickerman KA, Carpenter KM, Altman T, Nash CM, Zbikowski SM. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15(10):1787–91. doi: 10.1093/ntr/ntt061. [DOI] [PubMed] [Google Scholar]
- 27.Pepper JK, Brewer NT. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review. Tob Control. 2014;23(5):375–84. doi: 10.1136/tobaccocontrol-2013-051122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pepper JK, Ribisl KM, Emery SL, Brewer NT. Reasons for starting and stopping electronic cigarette use. Int J Environ Res Public Health. 2014;11(10):10345–61. doi: 10.3390/ijerph111010345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu SS, Neff L, Agaku IT, Cox S, Day HR, Holder-Hayes E, et al. Tobacco product use among adults—United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(27):685–91. doi: 10.15585/mmwr.mm6527a1. [DOI] [PubMed] [Google Scholar]
- 30.Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:Cd010216. doi: 10.1002/14651858.CD010216.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–28. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amato MS, Boyle RG, Levy D. How to define e-cigarette prevalence? Finding clues in the use frequency distribution. Tob Control. 2016;25(e1):e24–9. doi: 10.1136/tobaccocontrol-2015-052236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pulvers K, Hayes RB, Scheuermann TS, Romero DR, Emami AS, Resnicow K, et al. Tobacco use, quitting behavior, and health characteristics among current electronic cigarette users in a national tri-ethnic adult stable smoker sample. Nicotine Tob Res. 2015;17(9):1085–95. doi: 10.1093/ntr/ntu241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.United States Food and Drug Administration. FDA’s New Regulations for E-cigarettes, Cigars, and All Other Tobacco Products. 2016. http://www.fda.gov/TobaccoProducts/Labeling/RulesRegulationsGuidance/ucm394909.htm. Accessed April 25 2017.
- 35.Ornstein SM, Miller PM, Wessell AM, Jenkins RG, Nemeth LS, Nietert PJ. Integration and sustainability of alcohol screening, brief intervention, and pharmacotherapy in primary care settings. J Stud Alcohol Drugs. 2013;74(4):598–604. doi: 10.15288/jsad.2013.74.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leone FT, Evers-Casey S, Graden S, Schnoll R, Mallya G. Academic detailing interventions improve tobacco use treatment among physicians working in underserved communities. Ann Am Thorac Soc. 2015;12(6):854–8. doi: 10.1513/AnnalsATS.201410-466BC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sheffer MA, Baker TB, Fraser DL, Adsit RT, McAfee TA, Fiore MC. Fax referrals, academic detailing, and tobacco quitline use: a randomized trial. Am J Prev Med. 2012;42(1):21–8. doi: 10.1016/j.amepre.2011.08.028. [DOI] [PubMed] [Google Scholar]