Highlights
-
•
Internal supravesical hernia is very rare.
-
•
Most previous reports performed closure of the hernial sac by open laparotomy.
-
•
We could successfully repair intraoperatively-diagnosed internal supravesical hernia by the anterior approach alone.
Abbreviation: CT, computed tomography
Keywords: Internal supravesical hernia, Supravesical hernia, Anterior approach, Case report
Abstract
Introduction
Internal supravesical hernia is one of the rarest types of inguinal hernia. The hernial orifice is surrounded by the transverse vesical fold, median umbilical fold, and medial umbilical fold.
Presentation of case
A 75-year-old male presented with lower abdominal pain and nausea. Plain abdominal CT showed that the bladder was suppressed by small bowel near the left internal inguinal ring. A part of the small bowel wall seemed to be inlaid, and so the patient was diagnosed with a strangulated left inguinal hernia. The hernia repair operation was performed via the anterior approach. There was no internal hernial sac found, but there was a walnut-sized mass in the properitoneal space. A diagnosis was made intraoperatively of internal supravesical hernia with strangulated small bowel. Small bowel resection and hernial orifice closure were performed.
Discussion
Although internal supravesical hernia can present with distinctive CT findings, preoperative diagnosis is extremely difficult. Internal supravesical hernia in previous reports has been repaired via open laparotomy or laparoscopic surgery; however, we successfully repaired this intraoperatively-diagnosed internal supravesical hernia by the anterior approach alone.
Conclusion
The patient with internal supravesical hernia diagnosed intraoperatively could be treated via the anterior approach alone successfully. Depending on the situation, the anterior approach can be an option.
1. Introduction
Internal supravesical hernia is very rare and is not widely known by general surgeons. The low recognition of internal supravesical hernia makes preoperative diagnosis very difficult, although characteristic CT findings have been reported [1]. Most previous reports performed closure of the hernial sac by open laparotomy. There have been no recent report on repairing internal supravesical hernia without open laparotomy or laparoscopic surgery. This work has been reported in line with the SCARE criteria [2].
2. Presentation of case
A 75-year-old male presented with lower abdominal pain and nausea. His past medical history was significant for hypertension, and he had no history of previous abdominal surgery. On admission, the patient’s body temperature was 36.5 °C, heart rate was 58 beats/min, blood pressure was 162/89 mmHg, and SpO2 was 99% on room air. No tumor was detected in the abdomen, but there was tenderness in the hypogastric region without peritoneal signs. The bowel sounds were normal. Laboratory examination revealed that the patient’s C-reactive protein level was 1.00 mg/dL and white blood cell count was 8440 cells/μL. Abdominal radiography showed mildly dilated small intestines with a niveau (Fig. 1). Plain abdominal CT revealed that the bladder was being suppressed by small bowel near the left internal inguinal ring (Fig. 2). A part of the small bowel wall seemed to be inlaid, and so we diagnosed the patient with a strangulated left inguinal hernia (Fig. 3). The patient’s symptoms had improved since initial presentation at our hospital; hence, we thought that the strangulation had been released and the hernia repair operation was planned for the following day.
Fig. 1.
Preoperative abdominal X-ray image showing mildly dilated small intestine with niveau formation.
Fig. 2.
Preoperative plain CT image.
▽: Suppression of the bladder by small bowel near the left internal inguinal ring.
Fig. 3.
Preoperative plain CT image.
▽: A part of the small bowel wall seemed to be inlaid.
The operation was performed by a gastroenterological surgeon under general anesthesia via the anterior approach. After encircling the spermatic sheath, we attempted to explore the hernial sac. However, there was no internal or external hernial sac observed. After incising the transversal fascia, we could palpate a walnut-sized mass in the properitoneal space. We intraoperatively diagnosed an internal supravesical hernia with strangulated small bowel. After considering conversion to open laparotomy, we decided that it was possible to repair the hernial orifice via the anterior approach alone without making another abdominal incision. After incising the hernial sac, we resected the small bowel via the hernial orifice, resected the hernial sac, and closed the hernial orifice (Fig. 4). The posterior wall of the inguinal canal seemed to have become brittle during the operation, so we repaired it using McVay’s method. The patient was discharged on postoperative day 9 without any complications. No postoperative recurrence has occurred as of 22 months after surgery.
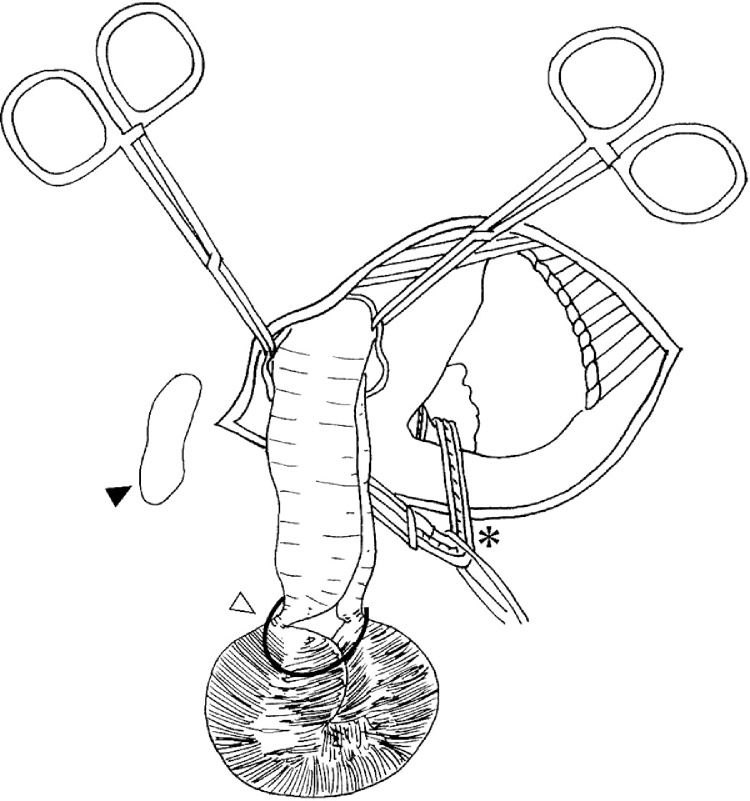
Fig. 4.
Schematic drawing of the operation.
After incision of the hernial sac, the necrotic small intestine was visible.
▽: strangulation of small intestine.
▼: pubis.
*: spermatic cord.
3. Discussion
Internal supravesical hernia is very rare. The first case was reported by Ring in 1814 [3]. While the exact number of cases is unknown, there have only been 13 documented cases in the past 30 years, including our case [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14] (summarized in Table 1). In previous reports of internal supravesical hernia, the median patient age was 74 years, and the male sex is dominant (10 of 11 cases). Internal supravesical hernia frequently occurs in men in their 60s [15]. The primary symptoms of supravesical hernia are often abdominal pain and vomiting. Almost all patients in previously reported internal supravesical hernia cases had digestive symptoms such as abdominal pain and vomiting caused by intestinal obstruction. Bladder irritation and dysuria can also be present, as the bladder is suppressed by the small bowel. Ischemic necrosis of the intestine frequently occurs as a consequence of strangulation; intestinal necrosis was present in four of the 13 reported cases. An accurate preoperative diagnosis was made in only one case. Two of the 13 cases were repaired laparoscopically (data were not fully available), while the other 10 cases were repaired by open laparotomy except for our case. Closure of the hernial sac was performed in all 13 cases, and resection of the hernial sac was performed in five of 13 cases.
Table 1.
Internal supravesical hernia cases reported in the past 30 years.
| Author | Year | Age/Sex | Presenting complaint | Accurate preoperative diagnosis (yes/no) | Operative method | Closure of sac (yes/no) | Resection of sac (yes/no) | Intestinal necrosis (yes/no) |
|---|---|---|---|---|---|---|---|---|
| Köksoy F.N. [4] | 1995 | 78/M | abdominal pain, vomitting | no (small bowel obstraction) | open laparotomy | yes | no | no |
| Yamaguchi R. [5] | 1996 | 74/M | abdominal pain, vomitting | no (small bowel obstraction) | open laparotomy | yes | yes | no |
| Gorgun E. [6] | ### | unknown | unknown | no | laparoscopic surgery | yes | no | no |
| Mehran A. [7] | ### | unknown | unknown | unknown | laparoscopic surgery | unknown | unknown | unknown |
| Jan Y.T. [8] | ### | 75/M | abdominal pain, vomitting | unknown | unknown | unknown | unknown | unknown |
| Saravanan B. [9] | ### | 62/M | abdominal pain, vomitting | no (small bowel obstraction) | open laparotomy | yes | no | yes |
| Cissé M. [10] | ### | 60/M | abdominal pain, vomitting | no (small bowel intussusception) | open laparotomy | yes | no | no |
| Bouassida M. [11] | 2012 | 36/M | abdominal pain, vomitting | no (small bowel obstraction) | open laparotomy | yes | yes | no |
| Bouassida M. [11] | 2012 | 58/F | abdominal pain, vomitting | yes | open laparotomy | yes | no | yes |
| Schwarz L. [12] | 2012 | 76/M | abdominal pain, vomitting | no (small bowel intussusception) | open laparotomy | yes | yes | yes |
| Khalid S. [13] | 2015 | 62/M | abdominal pain, constipation | no (small bowel obstraction) | open laparotomy | yes | yes | no |
| Sánchez Fuentes P.A. [14] | 2015 | 74/M | abodominal pain,distension | no (small bowel obstraction) | open laparotomy | yes | no | no |
| Our Case | ## | 75/M | abdominal pain, nausea | no(internal inguinal hernia) | anterior approach | yes | yes | yes |
| yes/no/unknown: 1/10/2 | open/laparoscopic/anterior/unknown: 9/2/1/1 | yes/no/unknown: 11/0/2 | yes/no/unknown: 5/6/2 | yes/no/unknown: 4/7/2 |
The orifice of a supravesical hernia is surrounded by the transverse vesical fold, median umbilical fold, and medial umbilical fold (Fig. 5). Supravesical hernia is classified into internal supravesical hernia and external supravesical hernia depending on the direction of extension. Internal supravesical hernia takes the form of an internal hernia, whereas external supravesical hernia takes the form of external hernia. It has been inferred that supravesical hernia is an acquired disease caused by diminution of peritoneal fat due to various factors (aging, malnutrition, and disease) or by dysraphism between Cooper’s ligament and the transversal fascia due to subperitoneal tissue-fibrillary contraction after inflammation [16]. Another theory is that supravesical hernia is caused by an extraordinarily large medial umbilical fold congenitally that creates a pocket above the bladder [17]. Ozturk et al. indicated that there was a developmental anomaly of the urinary system in their cadaveric case [18]. However, the pathogenesis has not yet been clarified.
Fig. 5.
Schematic drawing of the inside of the anterior lower abdominal wall.
The orifice of the supravesical hernia is surrounded by the transverse vesical fold, median umbilical fold, and medial umbilical fold.
Sasaya et al. reported that the distinguishing CT finding of strangulated small bowel in the supravesical fossa can help to diagnose internal supravesical hernia [1]. This CT finding was present in our case, but we misdiagnosed this as strangulation of a left inguinal hernia. A previous study reported that 45% of patients with internal supravesical hernia had experienced inguinal or femoral hernias [15], indicating that the patients may have a general vulnerability of the abdominal wall. Therefore, the diagnosis of internal supravesical hernia can be more difficult if another problem such as another hernia type is suspected. Our case was misdiagnosed as an inguinal hernia based on the preoperative CT findings, but no inguinal hernial sacs were revealed intraoperatively.
There is no gold standard surgical procedure for internal supravesical hernia; however, closure of the hernial orifice is generally considered important [15]. Removal of the hernial sac is reportedly not essential [19]. Almost all previous reports involved open laparotomy, whereas a few cases were repaired laparoscopically. As far as we know, there have been no recent reports of internal supravesical hernia repaired by the anterior approach alone. In our case, closure of the hernial orifice could be performed using the anterior approach alone without converting to laparotomy. In the case of intraoperatively-diagnosed internal supravesical hernia, closure of the hernial orifice may be performed by the anterior approach alone depending on the situation. If the operating field is anatomically deep due to patient factors such as the mobility or the size of the hernial sac, the surgical approach should be converted to open laparotomy or laparoscopic surgery. If it is suspected that the posterior wall of the inguinal canal is damaged, an additional repair should be considered. We subsequently performed McVay’s method, without mesh, because of the risk of infection from the intestinal necrosis.
If a precise preoperative diagnosis of internal supravesical hernia is made, the operator should consider the operative methods. As internal supravesical hernia is an uncommon disease and is frequently accompanied by intestinal necrosis, it may be better to select open laparotomy or laparoscopic surgery to enable determination of the patient’s anatomy. However, if the diagnosis of internal supravesical hernia is made unexpectedly during an operation being performed via the anterior approach, closure of the hernial orifice using the anterior approach alone may still be a viable option.
4. Conclusion
The patient with internal supravesical hernia diagnosed intraoperatively could be treated via the anterior approach alone successfully. Depending on the situation, the anterior approach can be an option.
Conflicts of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Author contribution
M. Morimoto carried out the acquisition of the data and drafted the manuscript. T. Sakamoto, N. Tokuyasu, E. Uchinaka, M. Amisaki, Y. Arai, Y. Kurisu, S. Nagai, H. Watanabe and S. Takahashi were involved in the drafting of the manuscript. S. Honjo revised the manuscript. Y. Fujiwara was the chief supervisor. All authors read and approved the final manuscript.
Guarantor
Soichiro Honjo.
References
- 1.Sasaya T., Yamaguchi A., Isogai M., Harada T., Kaneoka Y., Suzuki M. Supravesical hernia: CT diagnosis. Abdom. Imaging. 2001;26(1):89–91. doi: 10.1007/s002610000134. [DOI] [PubMed] [Google Scholar]
- 2.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Ring J. A case of internal inguinal hernia. Lond. Med. Reposit. 1814;2:204. [Google Scholar]
- 4.Koksoy F.N., Soybir G.R., Bulut T.M., Yalcin O., Aker Y., Kose H. Internal supravesical hernia: report of a case. Am. Surg. 1995;61(11):1023–1024. [PubMed] [Google Scholar]
- 5.Yamaguchi R., Yamaguchi A., Isogai M., Hori A., Kin Y., Kubota T. A case of internal supravesical hernia. Nihon Geka Gakkai Zasshi. 1996;97(11):1024–1026. [PubMed] [Google Scholar]
- 6.Gorgun E., Onur E., Baca B., Apaydin B., Yavuz N., Sirin F. Laparoscopic repair of an internal supravesical hernia: a rare hernia causing small bowel obstruction. Surg. Endosc. 2003;17(4):659. doi: 10.1007/s00464-002-4259-5. [DOI] [PubMed] [Google Scholar]
- 7.Mehran A., Szomstein S., Soto F., Rosenthal R. Laparoscopic repair of an internal strangulated supravesical hernia. Surg. Endosc. 2004;18(3):554–556. doi: 10.1007/s00464-003-4535-z. [DOI] [PubMed] [Google Scholar]
- 8.Jan Y.T., Jeng K.S., Liu Y.P., Yang F.S. Internal supravesical hernia. Am. J. Surg. 2008;196(4):e27–8. doi: 10.1016/j.amjsurg.2007.09.049. [DOI] [PubMed] [Google Scholar]
- 9.Saravanan B., Paramu M.K., Ranganathan E. Supravesical hernia–a rare cause of intestinal obstruction. Int. J. Surg. 2008;6(6):471–472. doi: 10.1016/j.ijsu.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 10.Cisse M., Konate I., Ka O., Dieng M., Dia A., Toure C.T. Internal supravesical hernia as a rare cauase of intestinal obstruction: a case report. J. Med. Case Rep. 2009;3:9333. doi: 10.1186/1752-1947-3-9333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouassida M., Sassi S., Touinsi H., Kallel H., Mighri M.M., Chebbi F. Internal supravesical hernia – a rare cause of intestinal obstruction: report of two cases. Pan Afr. Med. J. 2012;11:17. [PMC free article] [PubMed] [Google Scholar]
- 12.Schwarz L., Moszkowicz D., Peschaud F., Keilani K., Michot F., Scotte M. Internal supravesical hernia: an unusual cause of small bowel obstruction. Clin. Anat. 2012;25(5):663–667. doi: 10.1002/ca.21284. [DOI] [PubMed] [Google Scholar]
- 13.Khalid S., Burhanulhuq Bhatti A.A. Intestinal obstruction due to rare internal supravesical hernia. J. Ayub Med. Coll. Abbottabad. 2015;27(2):473–475. [PubMed] [Google Scholar]
- 14.Sanchez Fuentes P.A., Garcia Zamora C., Pinero Madrona A., Parrilla Paricio P. Intestinal obstruction due to internal supravesical hernia. Cir. Esp. 2015;93(1):e1. doi: 10.1016/j.ciresp.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Gray S.W., Skandalakis J.E. Supravesical hernia. In: LM N, RE C, editors. Hernia. 3rd edition. Lippincott; Philadelphia: 1989. pp. 388–398. [Google Scholar]
- 16.Skandalakis J.E., Gray S.W., Burns W.B., Sangmalee U., Sorg J.L. Internal and external supravesical hernia. Am. Surg. 1976;42(2):142–146. [PubMed] [Google Scholar]
- 17.Adler G.G. Die hernia supravesicalis. Bruns Beitr. Klin. Chir. 1970;218:225–233. [PubMed] [Google Scholar]
- 18.Ozturk N.C., Kurtoglu Z. Internal supravesical hernia accompanied with anomalous fold formations: a cadaveric case report. Surg. Radiol. Anat. 2014;36(10):1089–1092. doi: 10.1007/s00276-013-1252-8. [DOI] [PubMed] [Google Scholar]
- 19.Barnes D.R., Dreyer B.J. Internal supravesical hernia; report of a case presenting with bladder symptoms. Br. J. Surg. 1953;40(163):508–509. doi: 10.1002/bjs.18004016321. [DOI] [PubMed] [Google Scholar]