Abstract
Background
Anemia is highly prevalent in heart failure (HF) patients. However, the prevalence, clinical impact and prognostic factor of anemia in heart failure patients is widely varies. The aim of this study was to evaluate the prevalence of anemia in patients with HF, to compare baseline clinical characteristic and outcomes of severe HF patients with and without anemia admitted to Gondar University Referral Hospital (GURH), Gondar, Ethiopia.
Method
A retrospective cohort study was conducted and we assessed medical records of heart failure patients who were admitted Gondar University Referral Hospital in the period between December 02, 2010 and November 30, 2016. Kaplan Meier curve was used to analyze the survival status and log rank test was used to compare the curves. Multivariate Cox regression was used to analyze independent predictors of mortality in all HF patients. P value less than 0.05 was considered statistically significant.
Result
Three hundred and seventy patients participated in the study. The prevalence of anemia in the study cohorts was 41.90% and majority of the participants were females (64.59%). There was a significant difference in the level of hemoglobin, creatinine, and sodium among anemic and non-anemic patients. Anemic patients with HF tend to take angiotensin converting enzyme inhibitors (ACEI) less frequently. Kaplan Meier survival curves and Log rank test (P = 0.042) showed a significant difference in the prognosis of HF patients with anemia and non – anemic. More significant difference was observed (Log rank test, P = 0.001) in the study participants based on hemoglobin level. Furthermore, multivariate Cox regression showed: advanced age, levels of lower sodium and higher creatinine, and absences of medications like ACEI and Spironolactone independently predicted overall mortality.
Conclusion
HF patients with anemia tend to be older age, had lower hemoglobin and sodium level and higher creatinine value. Moreover, there was a significant difference in the prognosis between study cohorts, as anemic pateints tend to have a worse survival status . Even though, anemia is a significant risk marker, it is not an independent predictor of mortality in the current study.
Keywords: Heart Failure, Hemoglobin, Medical records, Survival, Mortality, Prognosis, Ethiopia
Background
Anemia is highly prevalent in heart failure (HF) patients. Its prevalence among patients with HF estimates can range from 30% to 70% in some studies depending on the cutoff value used to define its presence and on the population considered [1, 2]. Even though anemia is a commonly observed condition in HF, associated with significantly worse prognosis, there is no certain explanation, how it affects mortality, provokes HF exacerbation and influences the course of hospitalization [3–8]. Some of the proposed mechanism for anemia in HF include: iron deficiency due to reduced intestinal absorption or cytokine-related inflammatory changes, reduced erythropoietin production, simultaneous comorbidities such as renal failure, or even hemodilution [6, 9, 10]. The prevalence of anemia and its impact on patient’s survival outcome among reduced (HFrEF) and preserved (HFpEF) ejection fraction appears to be comparable, with comparable risks of mortality, readmission, hospitalization rates and loss of functional capacity [11, 12]. There are encouraging reports on the effectiveness of iron therapy in reducing HF symptoms, however, there are still no favorable results in terms of mortality in HF [13–16]. Thus, establishing the clinical importance of anemia in HF patients is imperative.
In Ethiopia, there is no study which demonstrated the overall prevalence of anemia in HF patients at national level; however, there are some studies which highlighted its prevalence in cardiovascular patients at institutional level to be between 3 and 25% depending on the diagnosis [17, 18].
The aim of this study was to evaluate the prevalence of anemia in patients with HF, to compare baseline clinical characteristic and outcomes of severe HF patients with and without anemia admitted to Gondar University Referral Hospital (GURH).
Methods
This study is adapted from a previous study conducted by Abebe et al. [18]. The study design and preliminary results were published previously [18]. Patients who had been admitted to GURH Internal Medicine department with the diagnosis of HF in the period from December 02, 2010 to November 30, 2016 were assessed retrospectively using their medical records. Patients who had been diagnosed HF, are 18 years of age or older, and met the adapted Framingham criteria for the diagnosis of heart failure were included [19].
Exclusion criteria were patients
Who had infection in addition to HF on admission,
Who did not have full laboratory and echocardiography data in their medical records and,
Who were not symptomatic on admission (New York Heart Association (NYHA) Class I and class II) as adapted from a study conducted by Mozaffarian et al. [20].
Based on the above criteria 370 patients met the inclusion criteria from 980 patients who were admitted during the study period.
Per hemoglobin level on hospital admission, patients were categorized into anemic and non-anemic groups. Hemoglobin concentration of less than 13 g/dl for male and less than 12 g/dl for female was used to define anemia according to the world health organization (WHO) criteria [21].
During the first admission to the internal medicine ward, patient’s ejection fraction was measured by a radiologist using echocardiography. Last hospital discharge or medication refill time was used as a vital status to assess study participants’ survival status. Definitions for etiologies of HF were taken from a previous study by Abebe et al. [18]. Hypertension was determined as blood pressure 140/90 mmHg or more.
Statistical analysis
Statistical analysis was carried out using the Statistical Package for Social Science, version 20.0 for Windows (SPSS, Chicago, IL, USA). Continuous variables were revealed as mean ± standard deviation and median (IQR) and discrete variables presented as percentage. Prior to additional analyses, Shapiro – Wilk and Levene test was performed to assess the data for normality and homogeneity. Patients were categorized based on their anemia status and further analysis was conducted using student t – test for Continuous variables and chi – square test for discrete variables to assess baseline characteristics, laboratory and echocardiography results and medication prescription among the study groups. Kaplan-Meier survival analysis was conducted to measure event free survival and the Mantel Log – rank test for between groups comparison. Cox proportional hazard ratio was used for the univariate analysis of predictor of events. The variables that had P values less than 0.2 in the univariate analysis were included in the Cox multivariate analysis. Hazard ratio and 95% confidence interval were shown. A type I error with P value less than 0.05 was considered significant.
During the study, patient’s data was de – identified to protect anonymity of medical records.
Result
Of 980 patients who were admitted to GURH due to HF, in the period between December 02, 2010 and November 30, 2016, 370 patients met the inclusion criteria. From the study group, 155 patients had anemia and the remaining participants (215) were non-anemic. Table 1 shows baseline clinical characteristics of the two groups. The mean age of the participants was 54.56 (±17.49) years with significant difference among the groups. There was no significant disparity among HF patients with and without anemia, hypertension, or AF, based on NYHA class, heart rate, or BP. Also, there was no difference between the two groups based on etiology of HF except for cor pulmonale (8.84% Vs. 0.65%, P = < 0.001).
Table 1.
Clinical characteristics of heart failure patients based on anemia status
| Variable | Non – anemic (215) | Anemic (155) | P – value | |
|---|---|---|---|---|
| Age, mean ± SD | 52.99 ± 17.15 | 56.47 ± 17.76 | 0.041* | |
| Gender, n (%) | 0.117 | |||
| Male | 69 (32.09%) | 62 (40.00%) | ||
| Female | 146 (67.91%) | 93 (60.00%) | ||
| Residency, n (%) | 0.075 | |||
| Urban | 99 (46.05%) | 57 (36.77%) | ||
| Rural | 116 (53.95%) | 98 (63.23%) | ||
| NYHA Class, n (%) | 0.339 | |||
| Class III | 55 (25.58%) | 33 (21.29%) | ||
| Class IV | 160 (74.42%) | 122 (78.71%) | ||
| Hypertension, n (%) | 63 (29.30%) | 54 (34.84%) | 0.258 | |
| AF, n (%) | 51 (23.72%) | 42 (27.10%) | 0.460 | |
| Heart Rate, mean ± SD | 91.06 ± 19.11 | 94.99 ± 19.64 | 0.056 | |
| Systolic BP, mean ± SD | 120.66 ± 22.29 | 123.74 ± 25.60 | 0.219 | |
| Diastolic BP, mean ± SD | 79.00 ± 14.30 | 79.50 ± 15.56 | 0.751 | |
| Etiology of HF, n (%) | ||||
| IHD | 36 (16.74%) | 22 (14.19%) | 0.506 | |
| VHD | 82 (38.14%) | 74 (47.74%) | 0.065 | |
| HHD | 33 (15.35%) | 24 (15.48%) | 0.972 | |
| DCMP | 25 (11.63%) | 21 (13.55%) | 0.581 | |
| CorPulmonale | 19 (8.84%) | 1 (0.65%) | <0.001* | |
| Other etiology | 20 (9.30%) | 13 (8.34%) | 0.761 |
AF Atrial Fibrillation, BP Blood Pressure, DCMP Dilated Cardiomyopathy, HF Heart Failure, HHD Hypertensive Heart Disease, IHD Ischemic Heart Disease, NYHA New York Heart Association, SD Standard Deviation, VHD Valvular Heart Disease
*p < 0.05
Results of laboratory analysis and echocardiograms
Per Table 2, higher hemoglobin (14.32 ± 2.16 Vs. 10.11 ± 2.17, P = < 0.0001), greater sodium (135.79 ± 6.48 Vs. 133.20 ± 6.18, P = < 0.0001) and lower creatinine (0.99 ± 0.50 Vs. 1.33 ± 1.02, P = < 0.0001) levels were measured in HF patients with non-anemic than anemic, respectively.
Table 2.
Laboratory and echocardiography results of heart failure patients based on anemia status
| Variable | Non – anemic (215) | Anemic (155) | P – value |
|---|---|---|---|
| Hemoglobin (mean ± SD) | 14.32 ± 2.16 | 10.11 ± 2.17 | <0.0001* |
| Creatinine (mean ± SD) | 0.99 ± 0.50 | 1.33 ± 1.02 | <0.0001* |
| Sodium (mean ± SD) | 135.79 ± 6.48 | 133.20 ± 6.18 | <0.0001* |
| LVEF (mean ± SD) | 52.56 ± 13.73 | 51.41 ± 13.75 | 0.425 |
| LVEDD in mm (mean ± SD) | 50.86 ± 10.87 | 51.92 ± 10.39 | 0.352 |
LVEF left ventricular ejection fraction, LVEDD left ventricular end diastolic dimension, SD standard deviation
*p < 0.05
Medical treatment
There was no significant disparity in the medication profile between the study groups except for angiotensin converting enzyme inhibitors (ACEIs) where they were more frequently prescribed in the non-anemic groups (52.56% Vs. 41.94%, P = 0.044) (Table 3).
Table 3.
Medication profile of heart failure patients based on anemia status
| Variable | Non – anemic (215) | Anemic (155) | P – value |
|---|---|---|---|
| Diuretics n (%) | 199 (92.56%) | 135 (87.10%) | 0.080 |
| Spironolactone n (%) | 148 (68.84%) | 100 (64.52%) | 0.383 |
| ACEI n (%) | 113 (52.56%) | 65 (41.94%) | 0.044* |
| Beta Blocker n (%) | 105 (48.84%) | 77 (49.68%) | 0.873 |
| Digoxin n (%) | 49 (22.79%) | 43 (27.74%) | 0.277 |
| CCB n (%) | 14 (6.51%) | 17 (10.97%) | 0.127 |
| Antiplatelet n (%) | 45 (20.93%) | 36 (23.23%) | 0.598 |
| Anticoagulants n (%) | 48 (30.97%) | 33 (21.29%) | 0.812 |
| Statin n (%) | 34 (15.81%) | 27 (17.42%) | 0.681 |
ACEI Angiotensin converting enzyme inhibitor, CCB calcium channel blocker
*p < 0.05
Survival analysis
The median (IQR) duration of follow up was 18(8 - 36) months. Mortality were 21.94% in HF patients with anemia (34 patients) and 9.78% in patients without anemia (21 patients). Kaplan Meier survival curves (Fig. 1) shows that there was significant difference in survival status of HF patients with and without anemia (Log Rank test, P = 0.042). Furthermore, a stronger significance differences (Log rank test, P = 0.001) were observed in the survival status of patients with HF when study participants were grouped based on their hemoglobin value (< 10.1 g/dl; 10.2 – 11.9 g/dl; 12–13.6 g/dl and ≥ 13.7 g/dl) (Fig. 2). On the other hand, univariate cox regression analysis showed that age, systolic blood pressure, diastolic pressure, Ischemic heart disease, anemia, creatinine level, sodium level, left ventricular ejection fraction, and use of spironolactone, ACEIs, beta blockers and anticoagulants were significantly associated with mortality in patients with HF. Multivariate cox regression analysis, showed that advanced age, lower sodium value, higher creatinine level and absence of medication use such as ACEI and spironolactone significantly predicted mortality in HF patients (Table 4). Even though, anemia is a significant risk marker, it is not an independent predictor of mortality in the current study.
Fig. 1.
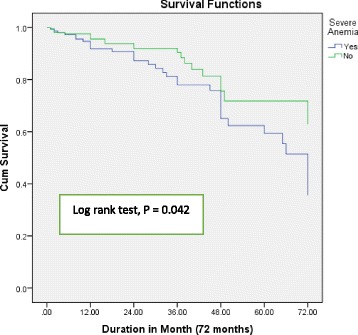
Kaplan Meier curves free from all causes of death in Heart Failure Patients based on anemia status
Fig. 2.
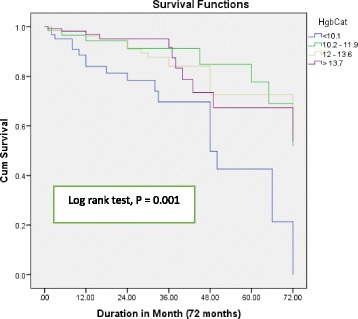
Kaplan Meier curves free from all causes of death in Heart Failure Patients based on hemoglobin status. Hgb Cat: Hemoglobin Category
Table 4.
Predictors of mortality to all causes of heart failure
| Variables | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| Hazard ratio (95% CI) | Hazard ratio (95% CI) | P- value | ||
| Gender | Female | 1.122 (0.643–1.958) | – | |
| Age, Years | 1.039 (1.021–1.058) | 1.041 (1.017–1.066) | 0.001* | |
| NYHA Class | Class IV | 1.622 (0.764–3.442) | 0.946 (0.402–2.227) | 0.899 |
| Heart Rate, bpm | 1.005 (0.992–1.017) | – | ||
| Systolic BP, mmHg | 1.017 (1.008–1.026) | 0.992 (0.975–1.009) | 0.367 | |
| Diastolic BP, mmHg | 1.031 (1.016–1.046) | 1.020 (0.997–1.044) | 0.089 | |
| Anemia | 1.740 (1.004–3.016) | 0.862 (0.439–1.693) | 0.666 | |
| Sodium, mEq/L | 0.937 (0.903–0.973) | 0.933 (0.882–0.987) | 0.016* | |
| Creatinine, mg/dl | 1.877 (1.636–2.155) | 1.869 (1.460–2.392) | <0.0001* | |
| AF | Yes | 0.535 (0.275–1.039) | 1.913 (0.583–6.272) | 0.284 |
| VHD | Yes | 0.635 (0.366–1.103) | 0.821 (0.418–1.612) | 0.566 |
| IHD | Yes | 2.261 (1.228–4.162) | 0.620 (0.256–1.501) | 0.289 |
| HHD | Yes | 0.918 (0.449–1.876) | – | |
| DCMP | Yes | 0.878 (0.346–2.227) | – | |
| Cor pulmonare | Yes | 0.776 (0.106–5.691) | – | |
| Other etiology | Yes | 1.237 (0.443–3.453) | – | |
| LVEF, % | 0.977 (0.955–0.998) | 0.984 (0.955–1.014) | 0.283 | |
| Diuretics | Yes | 0.586 (0.229–1.496) | – | |
| Spironolactone | Yes | 0.359 (0.210–0.613) | 0.527 (0.276–0.996) | 0.050* |
| ACEI | Yes | 0.546 (0.311–0.960) | 0.410 (0.197–0.852) | 0.017* |
| Beta Blocker | Yes | 0.555 (0.320–0.964) | 0.578 (0.295–1.132) | 0.110 |
| Digoxin | Yes | 0.401 (0.201–0.800) | 0.634 (0.225–1.791) | 0.390 |
| Antiplatelates | Yes | 0.895 (0.478–1.674) | – | |
| Anticoagulants | Yes | 0.400 (0.180–0.888) | 0.841 (0.277–2.558) | 0.760 |
| Statin | Yes | 1.431 (0.754–2.715) | – | |
| CCB | Yes | 1.524 (0744–3.119) | – |
ACEI Angiotensin converting enzyme inhibitor, AF Atrial Fibrillation, BP blood pressure, CCB calcium channel blocker, DCMP Dilated Cardiomyopathy, HHD hypertensive heart disease, IHD Ischemic heart disease, LVEF Left ventricular ejection fraction, NYHA New York Heart Association
*p < 0.05
Discussion
Anemia has lately been renowned as an imperative comorbidity and potential novel therapeutic target in heart failure patients [5]. To our knowledge, this study is the first to identify both the prevalence of anemia and its influence on survival status in patients with heart failure in Ethiopia. A meta-analysis conducted by Groenveld HF et al. reported the prevalence of anemia as 37.2% in patients with HF [5]. Furthermore, in a study of anemia in a population with heart failure (STAMINAHFP), the prevalence of anemia was 34% among outpatients with chronic heart failure, based on the WHO criteria for anemia [22]. In the current study, the prevalence of anemia was around 41.90% in HF patients. Our finding was higher than previous studies. This was attributable to patients’ characteristics such as gender, age, use of inconsistent definitions for anemia in patients with heart failure [23, 24] and inclusion of severely anemic patients in the study; unlike in most randomized clinical trials, severe anemia is an exclusion criterion, which makes it difficult to precisely assess this group of patients [25, 26].
In this study, age is significantly related with anemia with HF patients, which is a significant factor in most studies [27–29]. The mean age of anemic cohort in this study was (56.47 ± 17.76 years) which is younger than patients in the Swedish HF registry [30], the EVEREST trial [31], Valsartan heart failure (Val – HeFT) trial [25] and in IN – CHF registry [32]. This disparity might be due to the relative low sample size and younger population of the current study. Moreover, higher creatinine level, lower sodium and hemoglobin levels were significantly related with HF patients with anemia; these findings were in alignment with various studies [27–29, 33]. These all are substantially related with renal dysfunction, as glomerular filtration declines fluid volume in our body rises (hyponatremia) and creatinine clearance will decline. Moreover, renal dysfunction will result decreased erythropoietin synthesis which will affect red blood cell production and hemoglobin concentration [28, 33].
In the current study, left ventricular ejection fraction (LVEF) was not associated with degree of anemia. However, certain studies illustrated that the prevalence of anemia among patients with preserved left ventricular ejection fraction and among those with reduced ejection fraction is comparable [34, 35]. In an analysis of the Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity program (CHARM), lower Hemoglobin levels was associated with higher LVEF [33]. However, in a study of patients with restricted to impaired LVEF in the Valsartan Heart Failure Trial, the association between Hemoglobin and LVEF was not clear [25]. Further studies are required to clearly identify the association between anemia and LVEF.
Anemic patients are usually less likely to receive HF management according to guideline recommendations including ACEI, beta – blocker and Aldosterone antagonist, as it is evidenced by the EVEREST study [31], the IN – CHF registry [32] and the ANCHOR study [36]. In our study, at hospital discharge, ACEI were significantly less often prescribed to anemic patients. This might have been due to worse renal function in anemic patients.
HF patients with anemia and without anemia has a significant disparity in the long-term prognosis. Studies conducted by Agata Tyminska et al., Asa Jonsson et al. and the CHARM program, showed anemia has a poor prognostic outcome in patients with heart failure [28, 30, 33]. In the current study, Kaplan Meier survival curve showed (Log Rank test, P = 0.042) a significant difference in survival status which is in alignment with the above studies. Further survival curve analysis based on patient’s hemoglobin level indicated an even stronger difference (Log rank test, P = 0.001) in the overall mortality in the study group. This result was further supported by findings presented by various studies [29, 35, 37], as lower hemoglobin is strongly related with poor survival outcome.
In the current study, multivariate cox regression analysis showed that the independent factors of all causes of death in patients with HF were age (AHR = 1.041 (1.017 – 1.066), P = 0.001), sodium level (AHR = 0.933 (0.882 – 0.987), P = 0.016), creatinine level (AHR = 1.869 (1.460 – 2.392), P = < 0.0001), and prescription of medications like, ACEI (AHR = 0.410 (0.197–0.852), P = 0.017), and Spironolactone (AHR = 0.527 (0.276 – 0.996), P = 0.050). Our findings were in line with different studies; in studies investigated by Macín SM. et al. [38], and Ojeda S. et al. [39] in Spain, Agata Tymińska et al. [28] in Poland, Abebe et al. [18] in Ethiopia, a retrospective study in USA by Owan TE et al. [40] showed unfavorable prognosis in HF cohorts who were at advanced age, with lower level of sodium and higher serum creatinine level. Aldosterone blockers had a pivotal advantage in decreasing morbidity and mortality by lowering the atrial natriuretic peptide concentrations [41]. The polish cohort of two European society of cardiology heart failure registries determined that addition of ACEI in HF treatment had significantly decreased mortality in patients with HF [28].
The outcome of our study suggests that although anemia is a strong indicator of unfavorable prognosis in HF, it is not an independent risk factor for adverse outcomes. This may be dictated by the fact that most predictors of anemia, such as older age, higher NYHA class at hospital admission, kidney disease and diabetes overlapped with predictors of clinical endpoints [28].
Limitation of the study
Our study has several limitations. First, the study was conducted in single center so it might be difficult to represent the nationwide prevalence and prognosis outcome. Second, due to the small sample size, variables which might be statistically significant may not be evident. Third, due to the retrospective nature of the study and the sample size, generalizability to the other center might be taken in caution. Finally, last hospital discharge or medication refill was used to determine time for survival analysis and this could be affected by documentation or loss to follow-up.
Despite these limitations, we believe that our study provides prominent information on the clinical features and prognosis of HF patients with anemia. Moreover, it will provide a blue print for further clinical research in the area.
Conclusion
In the current study, HF patients with anemia tend to be older age, had lower hemoglobin and sodium level and higher creatinine value. On the other hand, patients without anemia were prescribed ACEI, beta – blocker and spironolactone more frequently than anemic patients. Age, sodium, creatinine and prescription of medication like ACEI and spironolactone predicted all causes of mortality in the study cohorts. Further survival analysis showed there was a significant difference in overall prognosis among anemic and non – anemic, and hemoglobin level. Even though, anemia is a significant risk marker, it is not an independent predictor of mortality in the current study.
Acknowledgements
We would like to acknowledge medical record department staffs for their support in searching and arranging study participants medical chart for the study. This publication has been produced during my scholarship period at Karolinska Institutet, thanks to a Swedish Institute Scholarship.
Funding
No financial support.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACEI
Angiotensin converting enzyme inhibitor
- AF
Atrial Fibrillation
- BP
Blood pressure
- CCB
Calcium channel blocker
- CHARM
the Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity program
- Cr
Creatinine
- DCMP
Dilated Cardiomyopathy
- GURH
Gondar University Referral Hospital
- Hct
Hematocrit
- HF
Heart failure
- HFpEF
Heart failure with preserved ejection fraction
- HFrEF
Heart failure with reduced ejection fraction
- Hg
Hemoglobin
- HHD
Hypertensive heart disease
- IHD
Ischemic Heart Disease
- LVEF
Left ventricular ejection fraction
- NYHA
New York Heart Association
- STAMINAHFP
Study of anemia in a population with heart failure
- Val – HeFT
Valsartan heart failure trial
- VHD
Valvular Heart Disease
- WHO
World health organization
Authors’ contributions
TBA – supervised and conceived the study, TBA and TMA – prepared study protocol, TBA, EAG and YGT – contributed in the data collection and analysis, TBA, ASB, TMA – wrote the manuscript, ASB and EAG – edited the manuscript. All authors have read and approved the Manuscript.
Ethics approval and consent to participate
Ethical clearance was obtained to access patient’s medical records from GURH ethical board of School of Pharmacy. Since the data collection was conducted retrospectively from patient medical records, and patients were not directly involved in data collection, informed consent was not sought from patients.
Consent for publication
Not applicable.
Competing interests
There are no perceived conflicts of interest for any of the authors related to this manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tamrat Befekadu Abebe, Phone: +251 913791302, Phone: +46 79 055 09 78, Email: Befekadutamrat@gmail.com, Email: tamrat.befekadu.abebe@stud.ki.se.
Eyob Alemayehu Gebreyohannes, Email: Justeyob@gmail.com.
Akshaya Srikanth Bhagavathula, Email: Akshaypharmd@gmail.com.
Yonas Getaye Tefera, Email: Yonas1get@gmail.com.
Tadesse Melaku Abegaz, Email: Abegaztadesse981@gmail.com.
References
- 1.Stamos TD, Silver MA. Management of anemia in heart failure. Curr Opin Cardiol. 2010;25(2):148–154. doi: 10.1097/HCO.0b013e3283357fe0. [DOI] [PubMed] [Google Scholar]
- 2.Anand IS. Anemia and chronic heart failure implications and treatment options. J Am Coll Cardiol. 2008;52(7):501–511. doi: 10.1016/j.jacc.2008.04.044. [DOI] [PubMed] [Google Scholar]
- 3.Tomaszuk-Kazberuk A, Bolinska S, Mlodawska E, Lopatowska P, Sobkowicz B, Musial W. Does admission anaemia still predict mortality six years after myocardial infarction? Kardiol Pol. 2014;72(6):488–493. doi: 10.5603/KP.a2014.0046. [DOI] [PubMed] [Google Scholar]
- 4.Young JB, Abraham WT, Albert NM, Gattis Stough W, Gheorghiade M, Greenberg BH, et al. Relation of low hemoglobin and anemia to morbidity and mortality in patients hospitalized with heart failure (insight from the OPTIMIZE-HF registry) Am J Cardiol. 2008;101(2):223–230. doi: 10.1016/j.amjcard.2007.07.067. [DOI] [PubMed] [Google Scholar]
- 5.Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008;52(10):818–827. doi: 10.1016/j.jacc.2008.04.061. [DOI] [PubMed] [Google Scholar]
- 6.Nanas JN, Matsouka C, Karageorgopoulos D, Leonti A, Tsolakis E, Drakos SG, et al. Etiology of anemia in patients with advanced heart failure. J Am Coll Cardiol. 2006;48(12):2485–2489. doi: 10.1016/j.jacc.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 7.Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013;34(11):816–829. doi: 10.1093/eurheartj/ehs224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kajimoto K, Sato N, Takano T. Association between anemia, clinical features and outcome in patients hospitalized for acute heart failure syndromes. Eur Heart J Acute Cardiovasc Care. 2015;4(6):568–576. doi: 10.1177/2048872614554199. [DOI] [PubMed] [Google Scholar]
- 9.O'Meara E, Rouleau JL, White M, Roy K, Blondeau L, Ducharme A, et al. Heart failure with anemia: novel findings on the roles of renal disease, interleukins, and specific left ventricular remodeling processes. Circ Heart Fail. 2014;7(5):773–781. doi: 10.1161/CIRCHEARTFAILURE.114.001100. [DOI] [PubMed] [Google Scholar]
- 10.Opasich C, Cazzola M, Scelsi L, De Feo S, Bosimini E, Lagioia R, et al. Blunted erythropoietin production and defective iron supply for erythropoiesis as major causes of anaemia in patients with chronic heart failure. Eur Heart J. 2005;26(21):2232–2237. doi: 10.1093/eurheartj/ehi388. [DOI] [PubMed] [Google Scholar]
- 11.Ather S, Chan W, Bozkurt B, Aguilar D, Ramasubbu K, Zachariah AA, et al. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol. 2012;59(11):998–1005. doi: 10.1016/j.jacc.2011.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moe GW, Ezekowitz JA, O'Meara E, Lepage S, Howlett JG, Fremes S, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol. 2015;31(1):3–16. doi: 10.1016/j.cjca.2014.10.022. [DOI] [PubMed] [Google Scholar]
- 13.Beck-da-Silva L, Piardi D, Soder S, Rohde LE, Pereira-Barretto AC, de Albuquerque D, et al. IRON-HF study: a randomized trial to assess the effects of iron in heart failure patients with anemia. Int J Cardiol. 2013;168(4):3439–3442. doi: 10.1016/j.ijcard.2013.04.181. [DOI] [PubMed] [Google Scholar]
- 14.Gutzwiller FS, Pfeil AM, Comin-Colet J, Ponikowski P, Filippatos G, Mori C, et al. Determinants of quality of life of patients with heart failure and iron deficiency treated with ferric carboxymaltose: FAIR-HF sub-analysis. Int J Cardiol. 2013;168(4):3878–3883. doi: 10.1016/j.ijcard.2013.06.045. [DOI] [PubMed] [Google Scholar]
- 15.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiencydagger. Eur Heart J. 2015;36(11):657–668. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jankowska EA, Tkaczyszyn M, Suchocki T, Drozd M, von Haehling S, Doehner W, et al. Effects of intravenous iron therapy in iron-deficient patients with systolic heart failure: a meta-analysis of randomized controlled trials. Eur J Heart Fail. 2016;18(7):786–795. doi: 10.1002/ejhf.473. [DOI] [PubMed] [Google Scholar]
- 17.Tefera YG, Abegaz TM, Abebe TB, Mekuria AB. The changing trend of cardiovascular disease and its clinical characteristics in Ethiopia: hospital-based observational study. Vasc Health Risk Manag. 2017;13:143–151. doi: 10.2147/VHRM.S131259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abebe TB, Gebreyohannes EA, Tefera YG, Abegaz TM. Patients with HFpEF and HFrEF have different clinical characteristics but similar prognosis: a retrospective cohort study. BMC Cardiovasc Disord. 2016;16(1):232. doi: 10.1186/s12872-016-0418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahmood SS, Wang TJ. The epidemiology of congestive heart failure: the Framingham Heart Study perspective. Glob Heart. 2013;8(1):77–82. doi: 10.1016/j.gheart.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mozaffarian D, Nye R, Levy WC. Anemia predicts mortality in severe heart failure. J Am Coll Cardiol. 2003;41(11):1933–1939. doi: 10.1016/S0735-1097(03)00425-X. [DOI] [PubMed] [Google Scholar]
- 21.WHO. UNICEF. UNU . Iron deficiency anaemia: assessment, prevention and control : a guide for programme managers. Geneva: World Health Organization; 2001. [Google Scholar]
- 22.Adams KF, Jr, Patterson JH, Oren RM, Mehra MR, O'Connor CM, Pina IL, et al. Prospective assessment of the occurrence of anemia in patients with heart failure: results from the Study of Anemia in a Heart Failure Population (STAMINA-HFP) Registry. Am Heart J. 2009;157(5):926–932. doi: 10.1016/j.ahj.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 23.Tang YD, Katz SD. Anemia in chronic heart failure: prevalence, etiology, clinical correlates, and treatment options. Circulation. 2006;113(20):2454–2461. doi: 10.1161/CIRCULATIONAHA.105.583666. [DOI] [PubMed] [Google Scholar]
- 24.Paul S, Paul RV. Anemia in heart failure: implications, management, and outcomes. J Cardiovasc Nursing. 2004;19(6 Suppl):S57–S66. doi: 10.1097/00005082-200411001-00008. [DOI] [PubMed] [Google Scholar]
- 25.Anand IS, Kuskowski MA, Rector TS, Florea VG, Glazer RD, Hester A, et al. Anemia and change in hemoglobin over time related to mortality and morbidity in patients with chronic heart failure: results from Val-HeFT. Circulation. 2005;112(8):1121–1127. doi: 10.1161/CIRCULATIONAHA.104.512988. [DOI] [PubMed] [Google Scholar]
- 26.Swedberg K, Young JB, Anand IS, Cheng S, Desai AS, Diaz R, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med. 2013;368(13):1210–1219. doi: 10.1056/NEJMoa1214865. [DOI] [PubMed] [Google Scholar]
- 27.Son Y-J, Kim BH. Prevalence of anemia and its influence on hospital readmissions and emergency department visits in outpatients with heart failure. Eur J Cardiovasc Nurs. doi:10.1177/1474515117710154. [DOI] [PubMed]
- 28.Tyminska A, Kaplon-Cieslicka A, Ozieranski K, Peller M, Balsam P, Marchel M, et al. Anemia at Hospital Admission and Its Relation to Outcomes in Patients With Heart Failure (from the Polish Cohort of 2 European Society of Cardiology Heart Failure Registries). Am J Cardiol. 2017; [DOI] [PubMed]
- 29.Hamaguchi S, Tsuchihashi-Makaya M, Kinugawa S, Yokota T, Takeshita A, Yokoshiki H, et al. Anemia is an independent predictor of long-term adverse outcomes in patients hospitalized with heart failure in Japan. A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD) Circ J. 2009;73(10):1901–1908. doi: 10.1253/circj.CJ-09-0184. [DOI] [PubMed] [Google Scholar]
- 30.Jonsson A, Hallberg AC, Edner M, Lund LH, Dahlstrom U. A comprehensive assessment of the association between anemia, clinical covariates and outcomes in a population-wide heart failure registry. Int J Cardiol. 2016;211:124–131. doi: 10.1016/j.ijcard.2016.02.144. [DOI] [PubMed] [Google Scholar]
- 31.Mentz RJ, Greene SJ, Ambrosy AP, Vaduganathan M, Subacius HP, Swedberg K, et al. Clinical profile and prognostic value of anemia at the time of admission and discharge among patients hospitalized for heart failure with reduced ejection fraction: findings from the EVEREST trial. Circ Heart Fail. 2014;7(3):401–408. doi: 10.1161/CIRCHEARTFAILURE.113.000840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maggioni AP, Opasich C, Anand I, Barlera S, Carbonieri E, Gonzini L, et al. Anemia in patients with heart failure: prevalence and prognostic role in a controlled trial and in clinical practice. J Card Fail. 2005;11(2):91–98. doi: 10.1016/j.cardfail.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 33.O'Meara E, Clayton T, McEntegart MB, McMurray JJ, Lang CC, Roger SD, et al. Clinical correlates and consequences of anemia in a broad spectrum of patients with heart failure: results of the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) Program. Circulation. 2006;113(7):986–994. doi: 10.1161/CIRCULATIONAHA.105.582577. [DOI] [PubMed] [Google Scholar]
- 34.Berry C, Poppe KK, Gamble GD, Earle NJ, Ezekowitz JA, Squire IB, et al. Prognostic significance of anaemia in patients with heart failure with preserved and reduced ejection fraction: results from the MAGGIC individual patient data meta-analysis. QJM. 2016;109(6):377–382. doi: 10.1093/qjmed/hcv087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anand I, McMurray JJ, Whitmore J, Warren M, Pham A, McCamish MA, et al. Anemia and its relationship to clinical outcome in heart failure. Circulation. 2004;110(2):149–154. doi: 10.1161/01.CIR.0000134279.79571.73. [DOI] [PubMed] [Google Scholar]
- 36.Go AS, Yang J, Ackerson LM, Lepper K, Robbins S, Massie BM, et al. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: the Anemia in Chronic Heart Failure: Outcomes and Resource Utilization (ANCHOR) Study. Circulation. 2006;113(23):2713–23. doi: 10.1161/CIRCULATIONAHA.105.577577. [DOI] [PubMed] [Google Scholar]
- 37.Redondo-Bermejo B, Pascual-Figal DA, Hurtado-Martinez JA, Montserrat-Coll J, Penafiel-Verdu P, Pastor-Perez F, et al. Clinical determinants and prognostic value of hemoglobin in hospitalized patients with systolic heart failure. Rev Esp de Cardiol. 2007;60(6):597–606. doi: 10.1157/13107116. [DOI] [PubMed] [Google Scholar]
- 38.Macin SM, Perna ER, Cimbaro Canella JP, Alvarenga P, Pantich R, Rios N, et al. Differences in clinical profile and outcome in patients with decompensated heart failure and systolic dysfunction or preserved systolic function. Rev Esp Cardiol. 2004;57(1):45–52. doi: 10.1016/S0300-8932(04)77060-8. [DOI] [PubMed] [Google Scholar]
- 39.Ojeda S, Anguita M, Munoz JF, Rodriguez MT, Mesa D, Franco M, et al. Clinical characteristics and medium-term prognosis of patients with heart failure and preserved systolic function. Do they differ in systolic dysfunction? Rev Esp Cardiol. 2003;56(11):1050–1056. doi: 10.1016/S0300-8932(03)77014-6. [DOI] [PubMed] [Google Scholar]
- 40.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 41.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341(10):709–717. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.


