Abstract
No widely used pediatric standards for hospital discharge care exist, despite nearly 10,000 pediatric discharges per day in the U.S. This lack of standards undermines the quality of pediatric hospital discharge, hinders quality improvement efforts, and adversely affects the health and wellbeing of children and their families after they leave the hospital. In this article, we first review guidance regarding the discharge process for adult patients, including federal law within the Social Security Act that outlines standards for hospital discharge, a variety of toolkits aimed to improve discharge care, and the research evidence that supports the discharge process. We then outline a framework within which to organize the diverse activities that constitute discharge care to be executed throughout the hospitalization of a child from admission to the actual discharge. In the framework, we describe processes to 1) initiate pediatric discharge care, 2) develop discharge care plans, 3) monitor discharge progress, and 4) finalize discharge. We contextualize these processes with a clinical case of a child undergoing hospital discharge. Use of this narrative review will help pediatric healthcare providers move forward to better understand what works and what does not during hospital discharge for children, while steadily improving their quality of care and health outcomes.
Keywords: children, hospital discharge, readmission, transitions of care
INTRODUCTION
Katie, a two-year-old girl hospitalized five days prior with a retropharyngeal abscess, has responded well to intravenous antibiotics. She will finish oral antibiotic treatment at home and follow-up with her primary care pediatrician in a few days. During morning rounds on the final day of her hospitalization, Katie’s parents and inpatient care team pause to think about all the work that was needed to get her ready for a successful hospital discharge.
Every day in the United States, an average of 9,706 pediatric patients are discharged from hospitals – not including 7,811 healthy newborns.1 Despite the unrelenting frequency of pediatric hospital discharge, key questions about the discharge process are unanswered. What is discharge care? What constitutes a “good” pediatric hospital discharge? How should discharge planning proceed from start to finish? What roles should parents play in shaping the discharge plan that, post-hospitalization, they will have to implement? How do we assure that the discharge process is done well? The lack of consensus on answers to these questions has inhibited the development of useful standards for pediatric discharge care. This lack of standards undermines the quality of pediatric hospital discharge, hinders quality improvement efforts, and adversely affects child health and wellbeing after leaving the hospital.2–5
This article aims to 1) inform pediatric providers about key elements of excellent discharge planning and execution, legislation that bears on discharge care, and tools available to address discharge planning; and 2) offer a framework of pediatric discharge planning that can help guide pediatric-specific discharge care guidelines, regulations, planning tools, quality improvement, and research.
HOSPITAL DISCHARGE RESEARCH, LEGISLATION, & PRACTICE FOR ADULT PATIENTS
The regulations and tools that guide and govern discharge planning are based on research of adult patients. A variety of studies have demonstrated that during hospital discharge: 1) care varies within and across hospitals and regions6, 7; 2) care is fraught with inconsistencies, omissions, and duplications of care8–11; 3) patient-provider and provider-provider communication are often substandard8, 12–14; 4) discrepancies in medication information exist and medical errors occur7, 9, 13, 15–17; 5) when discharge plans exist, patients, families, and outpatient healthcare providers have difficulty understanding and executing them11, 13, 18, 19; 6) documentation of important health information is often incomplete, late, and unnoticed20–22; and 7) patients leave the hospital unprepared and not ready for the transition.23 Poor quality of discharge care contributes to worsening health and an increased likelihood of hospital readmission.10, 13, 24, 25
The Social Security Act sets and protects standards and guidelines for hospital discharge care.26 The Act is the basis for Conditions of Participation - Discharge Planning, which describes the discharge processes required to meet the standards.27 The Conditions of Participation are the basis for the Interpretive Guidelines for Hospitals, which detail how hospitals are to be reviewed to determine whether they are compliant with the processes and standards.28, 29 Although written predominately with adult patients in mind, the Interpretive Guidelines provide structured guidance on the initiation, planning, and execution of high quality discharge planning to all hospitalized patients of any age.
The ability of this legislation to influence and improve discharge care depends on frontline providers to implement the recommended care processes. Various discharge care toolkits have been developed for adult patients.7 Toolkits like the Society of Hospital Medicine’s Better Outcomes by Optimizing Safe Transitions (BOOST)30, Boston University’s Project Re-Engineered Discharge (RED)31, the Institute for Healthcare Improvement’s (IHI) Improving Transitions Guide32, and Eric Coleman’s Care Transition Program33 assist patients and providers in discharge planning. These toolkits include questionnaires to help identify patients at risk for worsening health after discharge, conceptual models for developing and implementing a discharge care plan, checklists of essential processes that should be completed at hospital discharge, and guides to communicate with, educate, and empower patients for their hospital discharge. Although developed for adult patients, these toolkits can be adapted to pediatric hospital discharge in a framework to help guide the modifications.
A FRAMEWORK OF THE PEDIATRIC HOSPITAL DISCHARGE PROCESS
Rather than existing simply as a transient clinical event that occurs as the child and family leave the hospital, the pediatric discharge process is best conceptualized – in accordance with legislation, research, and clinical practice – as a set of care processes to be executed throughout the child’s full hospital course.7, 26–28, 34 The care processes may not be equivocally important for all children. The nature and complexity of the child’s health problems and needs will dictate which processes to emphasize as well as which inpatient health providers (e.g., physicians, nurses, social workers, etc.) are responsible for each process. Central to all processes is involvement and an on-going dialogue among the child, family, and healthcare providers through which the pathway to a high quality discharge can be visualized and traversed (Figure).5, 32, 35, 36
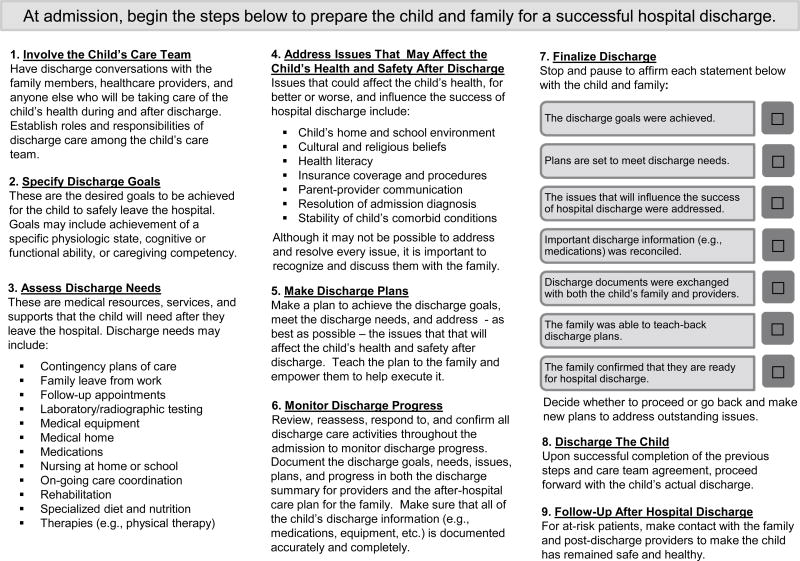
Figure. A Framework of Pediatric Hospital Discharge Care.
The figure portrays the steps to complete when preparing a child and family for a successful hospital discharge.
Initiating Pediatric Discharge Care
Discharge care for Katie had begun at admission, when her family and hospital care team systematically assessed and projected what tasks had to be performed for Katie to be healthy enough to leave the hospital with her discharge needs met and with plans in place to address things that could affect her health after leaving (Textbox 1).
Textbox 1. Initiating Pediatric Hospital Discharge Care for Katie, a 2-Year-Old Girl with a Retropharyngeal Abscess.
| Setting Katie’s Discharge Goals |
|
|
| Katie is a 2-year-old with hypoxic brain injury (from a difficult birth), epilepsy, and mild developmental delay. She was admitted to the hospital following 3 days of high fever, stiff neck, and drooling. Her pediatrician evaluated her and referred her to the emergency department. A C.T. scan showed a retropharyngeal abscess and a staple that she had swallowed that was stuck deep in her throat. After the staple was removed by flexible endoscopy, she was admitted to the hospitalist service for monitoring and treatment of the abscess. |
| During her admission history and physical, Katie’s inpatient care team talked with her family about the treatment plan for her abscess and the health goals that she needed to achieve to leave the hospital. The team explained that Katie would need antibiotics and fluids given intravenously (IV) until her fever had improved, her neck felt better, her drooling had gone away, and the swelling in the back of her throat had subsided enough that she could safely eat and drink again. They thought it might take 4–5 days to achieve those things. At that point, Katie’s IV antibiotic could be changed to one that she could take by mouth and she could leave the hospital as long as she was recovering well and had no troubles taking the antibiotic. Katie’s family understood all of these things and agreed with the plan. |
| On a whiteboard in Katie’s room, the team wrote her discharge goals: 1) to no longer need IV antibiotics, 2) to eat and drink enough to stay hydrated and nourished; and 3) to take the oral antibiotic without difficulty. |
|
|
| Assessing Katie’s Discharge Needs |
|
|
| The team and family then discussed the needs that Katie would have when going home. She would need a prescription for the oral antibiotic accompanied by instructions on how to take it and a list of what side effects to watch for. She would also need a follow-up appointment with her pediatrician. Aside from those obvious needs, the team wondered whether Katie might need anything else when going home. The pediatrics resident on the care team took out a card from his coat pocket that had a list of potential discharge needs for children. One by one, the resident reviewed each need on the list with the team and family to make sure no discharge needs had been overlooked. When thinking about medication needs, the family remembered that Katie needed a new prescription for a refill of her epilepsy medication; her supply would run out tomorrow. They informed the team that Katie would seize if she missed a dose after she went home. |
| The team wrote Katie’s discharge needs on the whiteboard in her room: 1) she needs a prescription for an oral antibiotic, 2) she needs a prescription for refills of her seizure medication, and 3) she needs a follow-up appointment with her pediatrician. |
|
|
| Identifying Factors Influencing Katie’s Health After Discharge |
|
|
| Next, the team and family discussed factors that might influence Katie’s health after leaving the hospital. The team mentioned that the abscess could get worse if the oral antibiotic does not kill the bacteria inside of it. They planned to use the antibiotic amoxicillin with clavulanic acid. Katie’s parents replied that she gets very bad diarrhea from the bacteria clostridium difficile (c. diff) when taking that antibiotic. The diarrhea causes her to get dehydrated and she sometimes needs to be hospitalized for IV fluids. Her parents also remembered that Katie’s seizures tend to get worse when she is sick and they were concerned that she might have a seizure in the hospital or after discharge. |
| The team wrote the factors that might influence Katie’s health after discharge on the whiteboard: 1) she could experience severe diarrhea from taking the oral antibiotic after discharge; 2) she could have a seizure while recovering from her abscess. |
Hospital discharge legislation mandates that discharge planning should begin well in advance of the patient’s actual discharge.26–28 Soong, et. al.’s discharge checklist, a standard list used by some hospitals for adult patients, asserts that discharge care begin at admission and continue on subsequent days before the day of discharge.34 Because most hospitalized children spend, on average, 2-to-3 days in the hospital, admission may be the most opportune time to begin discharge care.1 The plan for hospital care is routinely crafted at admission through healthcare providers’ communication with the child and family and their review of existing health records and other sources of information. The knowledge gained from this dialogue and health information review at admission could be used to make discharge planning more efficient and effective.
Three processes should be completed when initiating discharge care for a hospitalized child: 1) specify discharge goals, 2) assess discharge healthcare needs, and 3) identify factors that could influence the child’s health after leaving the hospital. Hospital discharge legislation declares that the purpose of these processes is to screen and identify individual patients for whom the lack of an adequate discharge plan will likely result in an unnecessary delay in discharge or an adverse impact on their health after discharge.26–28 In addition, these processes are essential to create a foundation of knowledge about the child, their family, and healthcare providers from which effective discharge plans can be efficiently created and executed.
Specify Discharge Goals
Specify discharge goals - the desired health results to be achieved for the child to safely leave the hospital - early in the admission to guide the final decisions about when and to which level of care (e.g., to home with hospice) the child will be discharged. Discharge goals may include achievement of a physiologic state (e.g., no fever for 24 hours), a cognitive or functional ability (e.g. the ability to eat and drink by mouth without difficulty), or a caregiving competency (e.g., a parent’s competency to give an oral medication to their child). Discharge goals may evolve and change during the hospitalization. Reconciling differences in preferences of the discharge goals is important. Children whose parents believe that they are not healthy enough to be discharged are more likely to experience an unplanned readmission.2
Assess Discharge Needs
Assess discharge needs - the items and services that must be in place to optimize the health and well-being of the child and family after leaving the hospital – in a systematic, comprehensive manner to drive discharge planning.37 Although most hospitalized children have few discharge needs, the list of possible needs is extensive, including post-discharge medications, medical equipment and supplies, nutrition, and health services (e.g., primary care, therapists, home nursing).26–28, 32 Absent a standardized systematic assessment, overlooked discharge needs can lead to adverse health consequences after discharge. Accordingly, experts – and the Institute for Healthcare Improvement (IHI), in particular – emphasize the importance of involving patients, families, and post-discharge providers of all kinds (e.g., primary care providers, home and school nurses, etc.) as full partners in this process.32, 35
Spot Issues that Could Influence the Child’s Health after Discharge
Identify all of the issues that will affect the child’s health, for better or worse, after leaving the hospital. The Interpretive Guidelines identify several of these key issues, such as the patient and caregiver’s understanding of discharge needs, the patient’s post-discharge environment, transportation to access post-discharge health services, and community resources.28 Project BOOST and IHI’s Transition Guide identify additional issues to consider, including the patient’s primary health problem, underlying comorbid conditions, psychological functioning, and health trajectory.30, 32 While there may seem to be an endless number of issues to consider, time spent identifying and addressing key factors can further improve the discharge planning process.38 IHI’s Transition Guide has questions that, when adapted for children, may facilitate the identification of these issues (e.g., “Why might this child experience an unplanned readmission after they are discharged?”).2 Accurately identifying these issues enables the development of plans to address them.30
Developing Discharge Plans
Katie’s family and hospital care team had worked together to make plans to achieve her discharge goals, meet her health care needs, and address factors that could influence her health after discharge (Textbox 2).
Textbox 2. Developing Hospital Discharge Plans and Monitoring Discharge Progress in Katie, an 18-month-old Girl with a Retropharyngeal Abscess.
| Developing Katie’s Discharge Plans |
|
|
| On hospital day 2, Katie’s inpatient care team and family huddled to think about what plans she would need to achieve her discharge goals, meet her discharge needs, and address the factors that could influence her health after discharge. They prioritized the development of two plans: |
| Oral Antibiotic Plan. Choosing the oral antibiotic, in particular, was something Katie’s care team wanted to get right. They wanted to choose an antibiotic that would likely kill the bacteria in her abscess without putting her at risk for c. diff-related diarrhea. The team decided they needed help from a hospital pharmacist and an otolaryngology surgeon who was familiar with treatment of retropharyngeal abscess. They also decided to review the evidence behind the treatment and prevention of recurrent c. diff in children. |
| Plans for Diarrhea and Seizure. Both the team and the family felt it important to develop plans for what to do and whom to call for help should Katie develop diarrhea or seizures after leaving the hospital. They thought that Katie’s pediatrician and neurologist could also help develop these plans with them. In speaking more with the family about this, they learned that Katie was not followed by a gastroenterologist for her recurrent c. diff infections. They decided to refer her to a gastroenterologist for help managing that problem. |
|
|
| Monitoring Katie’s Discharge Progress |
|
|
| On hospital day 3, Katie’s inpatient care team collaborated with a pharmacist, an otolaryngologist, a gastroenterologist, and Katie’s neurologist to solidify her discharge plans. They discussed and confirmed the plans with Katie’s parents. |
| Oral Antibiotic Plan. Katie’s oral antibiotic will be clindamycin instead of amoxicillin with clavulanic acid. Per otolarlyngology, clindamycin should effectively treat her abscess. Although clindamycin has been associated with c. diff infection, Katie’s records – confirmed by her parents and primary care pediatrician – report that she has received clindamycin twice in the past for treatment of aspiration pneumonia without experiencing c. diff diarrhea. |
| Plans for Diarrhea and Seizures. For the diarrhea plan, Katie will be started on the medication, lactobacillus, a probiotic that has been shown to decrease the risk of recurrent c. diff diarrhea. Should she develop diarrhea, the family will 1) collect a stool sample (a kit to collect the sample was sent to them) and bring it to the hospital laboratory for c. diff testing (the family was given the laboratory paperwork for this); 2) they will call the gastroenterologist on call to decide whether to give her an additional antibiotic to treat the suspected c. diff while the test is pending; and 3) they will change Katie’s regular diet to one with pedialyte and toast to keep her hydrated. For the seizures, Katie’s neurologist called in refills for her seizure medication to her local pharmacy. Aside from giving Katie diazepam for a seizure lasting longer than 5 minutes – a plan already in place for her – the neurologist did not have further recommendations on what do to should she have a seizure. |
| By the end of hospital day 4, Katie was feeling great. She was moving her neck around and she was smiling and talking. Her IV fluids were discontinued and she was eating and drinking well. Her family and inpatient care team decided together that if she continued to do well overnight, then the next morning they would discontinue her IV antibiotics, give her a dose of her oral antibiotic, and get everything ready for her go home from the hospital. The family was thrilled to hear this news. In anticipation of Katie’s hospital discharge, the inpatient team started to work on the discharge summary that they would share with all of her post-discharge providers and the after hospital care plan that they would share with Katie and her family before leaving the hospital. |
The Interpretive Guidelines specify that discharge plans should be created to achieve each discharge goal, to meet each discharge need, and to address each issue that could influence discharge success.28 According to IHI, good discharge plans contain components that specify particular actions (e.g., tasks to complete, such as scheduling a follow-up appointment or making a follow-up phone call after discharge), contingencies (e.g., instructions on how to address a post-discharge health problem), things to teach and learn (e.g., teaching the caregiver a new home treatment skill), and things to remember (e.g., the result of a lab test that should not be forgotten).30 Relatedly, the Interpretive Guidelines mandate that the plans include clear instructions regarding what to do when concerns, issues, or problems arise after discharge and whom to call and when patients should seek emergency assistance; providing a patient with only the advice to “return to the ED” when problems arise is unacceptable.28
When developing discharge plans, hospital clinicians are charged to provide patients, families, and post-discharge providers with choices; indeed, hospital discharge legislation declares that these persons have the right to participate in this process.26–28 Hospitals are expected to know the capabilities of the patient’s post-discharge providers so that feasible discharge plans are developed.26–28 Each component of the plan should have a sound reason for why it is important to execute.7, 39, 40 Furthermore, each component should be delegated to one or more of the child’s family or healthcare team members with explicit delineation of role and responsibility and with an assigned timeline of execution (e.g., within 3 days after discharge).7, 39, 40
Patient and family education is critical to the success of developing and implementing a successful discharge plan. In randomized clinical trials of hospitalized adult patients, discharge planning interventions that included a formal teaching facet (e.g., access to a discharge educator in Project RED41 or a discharge coach in the Care Transitions Program42) were associated with decreased hospital readmission. Among children, discharge education (e.g., with a booklet or dedicated teaching session) is the most common feature of interventions that have improved hospital discharge success.43–47 Educating the child’s family members who will actually be caring for the child after discharge is crucial, as is assessing their primary language and health literacy.48–50 Discharge teaching should include a discussion of the rationale and importance of each component of the plan as well as confirmation that the child and family understand and can execute each component for which they are responsible.51
Monitoring Discharge Progress
On a whiteboard in her room, Katie’s hospital care team wrote her discharge goals, needs, and factors that could influence her health after discharge. Together with Katie’s family, they reviewed, each day, the progress made on the plans that were developed to get Katie ready and prepared for hospital discharge. Katie’s team began documenting her discharge plans so that they could be shared with her family and post-discharge providers (Textbox 2).
Because the child’s discharge goals, needs, and factors influencing the child’s health after discharge may change during the hospitalization, the inpatient care team needs to regularly reassess the appropriateness and responsiveness of discharge plans and to revise the plans accordingly.27, 28 The Interpretive Guidelines mandate that discharge plans that have to be enacted or completed during the child’s hospitalization be done so.28 A dedicated system (e.g., a whiteboard in the patient’s room, a tracking system in the health record, etc.) should be used to monitor the progress in developing, updating, and executing discharge plans.52 The system should also monitor the counseling, teaching, and preparation that has occurred to get the child and family ready for the approaching hospital discharge.
Written documentation of discharge progress is central to the monitoring process; this documentation can be used to generate the discharge documents that will be exchanged with the child’s family and post-discharge care providers as discharge is finalized. At a minimum, discharge information to document includes, but is not limited to, the reason for hospitalization and principal diagnosis; description of the hospital course of treatment; patient’s condition at discharge, including cognitive and functional status; medication list; list of food, drug, and other allergies; experienced and potential drug interactions; pending laboratory work and test results with information on how results will be furnished.28, 53 In addition, critical to document are clear description of discharge plans with instructions regarding what to do when concerns, issues, or problems arise after discharge; whom to call; when patients should seek emergency assistance; and who is responsible for individual components of the plan.7, 19
Finalizing Pediatric Discharge
Now, on this last day of hospitalization, Katie’s care team and family took time to review all of her hospital discharge preparation and to assure that everything was in place for her to leave the hospital. Katie’s discharge documentation was shared with her family and post-discharge providers and was carefully reviewed for completeness and accuracy. After final confirmation that Katie and her family understood the discharge care plan and were ready for hospital discharge, Katie left the hospital. Everyone was hopeful that she would do well (Textbox 3).
Textbox 3. Finalizing Hospital Discharge Care for Katie, an 18-month-old Girl with a Retropharyngeal Abscess.
| Finalizing Katie’s Hospital Discharge |
|
|
| During rounds, mid-morning of hospital day 5, Katie’s inpatient team and family took time out to review Katie’s hospital course and to make sure that it was safe to proceed with her hospital discharge. |
| Together, they confirmed that Katie had achieved her discharge goals. Katie no longer needed IV antibiotics. She was able to eat and drink enough to stay hydrated and nourished. She took her oral antibiotic this morning without difficulty. |
| Next, they confirmed plans to meet Katie’s discharge needs. The team confirmed that they had called in the prescription for her oral antibiotic, that her neurologist had called in refills for her seizure medication, and that the family had scheduled an appointment for Katie to be seen by her pediatrician two days later. |
| After that, they confirmed that they had addressed the factors that might influence Katie’s discharge success. They were glad that they had thought about Katie’s history of recurrent c. diff infections. Although they were hopeful that the oral antibiotic would not lead to another infection, they were reassured that a post-discharge plan to manage diarrhea and dehydration was in place. The family wished that a stronger plan could be made to mitigate the risk of Katie having a seizure, but they were reassured that no seizures had occurred thus far during her acute illness. |
| The team exchanged a family-centered, discharge document with Katie’s family. The family read through the document carefully. Katie’s health information was checked to see if any of it needed to be reconciled. The information on her diagnoses, past medical history, medications, and contact information was accurate and complete. |
| The team then asked Katie’s family to describe the discharge care plan in their own words. During this teach-back process, the family described the plan perfectly aside from one perception. They family forgot that they were to change Katie’s diet should she develop diarrhea. The team went through this part of the plan with them again and it was clear that the family understood how to do it. |
| Finally, the team asked the family how ready and prepared they were to leave the hospital. Both parents responded that they were very ready and felt very prepared. Katie’s inpatient care team agreed that the Katie and her family were ready to go. |
As discharge is finalized, the family and inpatient care team should take a “time out” (i.e., a stop and pause) to ensure that the child is safe and ready to leave the hospital.36, 54 During the time out, everyone can survey the discharge work to date in light of the child’s current health status, raising the question of whether to proceed with discharge as planned, or extend the hospitalization to work on an important outstanding issue that had been overlooked. Furthermore, discharge documentation can be reviewed and revised to correct information inaccuracies and to clarify understanding of the plan going forward. A checklist or related tool can help standardize how discharge care is finalized.34
Confirm Discharge Goal Achievement, Needs Attainment, and Attention to Factors Influencing the Child’s Health after Discharge
This confirmation ensures consensus among the child, family, and healthcare providers that the time is right to start the final process of discharging the child. As with informed consent, the family should fully understand the risks and benefits of hospital discharge, including the likelihood of hospital readmission, especially in a situation where an issue that could affect the health of the child after discharge cannot be fully resolved.55 They should also confirm the completion of tasks (for instance, that follow-up appointments have been scheduled to meet a discharge need) that must be carried through before hospital discharge occurs.
Exchange Discharge Documentation
The Conditions of Participation and Interpretive Guidelines mandate that necessary discharge information be exchanged so that patients and the family and post-discharge provider taking care of them know the outcome of hospital treatment and the discharge plan.27, 28 Every hospitalized patient should leave the hospital with discharge instructions written in their preferred language and at their education level.7 The Internal Guidelines mandate that all discharge information must be organized and delivered to patients’ post-discharge providers prior to the first follow-up appointment.28
Reconcile Health Information
Reconciliation is the process of verifying with the child and family vital health information that, if incomplete or inaccurate, could adversely affect the child’s health. Medication reconciliation at hospital discharge for adult patients, when evaluated in randomized trials that bundled reconciliation with other interventions aiming at improving discharge care, has been associated with decreased adverse drug events56, 57 as well as decreased emergency department visits and readmissions.58 Reconciliation of other types of health information, such as a list of chronic health problems or the contact information of the child’s family and post-discharge providers, may also be beneficial.
Confirm Understanding of the Discharge Plans with Teach-back
Teach-back is a question and answer activity during which the child (if capable) and family can verbalize, in their own words, the specific elements of the discharge plan, including the discharge goals, needs, and factors that will influence the child’s health after discharge.51 Teach-back can also be used to verify caregiving skills, such as demonstrating the ability to use home medical equipment.59 This process allows the person educating to verify, reinforce, and maximize understanding of these things while addressing any misconceptions. Teach-back may begin by a hospital provider asking the family, “Why do you think [the child] has been in the hospital?” Discharge education methods using teach-back have been associated with increased health literacy50, 60, better knowledge acquisition and retention of discharge plans61, and decreased readmission rates.62, 63
Assess Readiness for Hospital Discharge
Discharge readiness - the ability to understand and execute the intended discharge care plan and the perception that it is safe to proceed with the child’s actual discharge - is the culmination of all the preceding processes of discharge care.30, 59, 64, 65 The child, family, and post-discharge healthcare providers should feel comfortable with and be prepared for hospital discharge. Discharge success is more likely for children whose parents who believe that their child is healthy enough to leave the hospital and that they understand how to manage their child’s health after discharge.2 For these reasons, identifying, discussing, and addressing low or divergent perceptions of discharge readiness are crucial to complete before discharge. Engaging patients and families in completing a discharge checklist or short questionnaire (e.g., the Care Transitions Program’s patient and family-facing discharge preparation checklist and care transition measure) can confirm discharge preparedness and readiness.2, 33
Following-Up after Hospital Discharge
After hospital discharge, when Katie was seen by her post-discharge healthcare providers, her parents brought with them the hospital discharge summaries that they had received at the hospital. Her parents each reported that they had felt well prepared to go home, and while the transition home had involved much work, the way that the work had been broken down and tackled piece-by-piece made the transition home manageable. And most important, Katie was doing great.
Consideration of the continuation of hospital discharge care after the child leaves the hospital should occur, especially for children at increased risk for readmission (e.g., children with medical complexity66–68). After discharge, Project BOOST recommends phone contact with at risk patients and their principal provider.30 During contact, assessment can occur of the patient’s condition as well as the comprehension of and adherence to the discharge plan.30 New or unresolved health problems can be addressed19, pending test results reviewed21, 22, and attendance at follow-up appointments reiterated.3
CONCLUSION
Without doubt – for reasons ranging from patient safety to parental satisfaction, and from payor reimbursement to regulatory requirements – the time has come to focus on, standardize, and improve the pediatric hospitalization discharge process. We offer this discharge framework to help organize the many diverse activities that make up the discharge process, enabling pediatric healthcare providers to move forward to a better understanding of what works and what does not. The framework and its activities will evolve as new findings emerge from on-going research, quality improvement, and policy experiments on pediatric discharge care. With testing, refinement, and implementation,, we hope that use of this framework will steadily improve pediatric quality of care and outcomes for children and their families.
Acknowledgments
Mr. Blaine and Drs. Berry, Feudtner, McBride, and Schuster were supported by the Lucile Packard Foundation for Children’s Health to complete this work. The funder was not involved in the design and conduct of the work; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Agency for Healthcare Research and Quality. HCUPnet: Healthcare Cost and Utilization Project. [Accessed January 1, 2014]; http://hcupnet.ahrq.gov/
- 2.Berry JG, Ziniel SI, Freeman L, et al. Hospital readmission and parent perceptions of their child's hospital discharge. Int J Qual Health Care. 2013 Aug 20; doi: 10.1093/intqhc/mzt051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frei-Jones MJ, Field JJ, DeBaun MR. Risk factors for hospital readmission within 30 days: a new quality measure for children with sickle cell disease. Pediatr Blood Cancer. 2009 Apr;52(4):481–485. doi: 10.1002/pbc.21854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones C, Missanelli M, Dure L, et al. Anticonvulsant medication errors in children with epilepsy during the home-to-hospital transition. J Child Neurol. 2013 Mar;28(3):314–320. doi: 10.1177/0883073812446632. [DOI] [PubMed] [Google Scholar]
- 5.Mahant S, Keren R, Localio R, et al. Variation in Quality of Tonsillectomy Perioperative Care and Revisit Rates in Children's Hospitals. Pediatrics. 2013 Jan 20; doi: 10.1542/peds.2013-1884. [DOI] [PubMed] [Google Scholar]
- 6.Audet A-MJ. A Call for Standardized Rehospitalization Measures and Information Systems. [9/27/2010];The Commonwealth Fund Blog. 2010 [Google Scholar]
- 7.Jack B, Greenwald J, Forsythe S, et al. Developing the Tools to Administer a Comprehensive Hospital Discharge Program: The ReEngineered Discharge (RED) Program (Vol. 3: Performance and Tools) 2008 Aug; [PubMed] [Google Scholar]
- 8.Bourgeois FC, Olson KL, Mandl KD. Patients treated at multiple acute health care facilities: quantifying information fragmentation. Arch Intern Med. 2010 Dec 13;170(22):1989–1995. doi: 10.1001/archinternmed.2010.439. [DOI] [PubMed] [Google Scholar]
- 9.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Feb 4;138(3):161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 10.Bradley EH, Curry L, Horwitz LI, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol. 2012 Aug 14;60(7):607–614. doi: 10.1016/j.jacc.2012.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007 Sep;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 12.Arora VM, Prochaska ML, Farnan JM, et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010 Sep;5(7):385–391. doi: 10.1002/jhm.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008 Aug;23(8):1228–1233. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007 Feb 28;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 15.Anderson GF, Steinberg EP. Hospital readmissions in the Medicare population. N Engl J Med. 1984 Nov 22;311(21):1349–1353. doi: 10.1056/NEJM198411223112105. [DOI] [PubMed] [Google Scholar]
- 16.Burns R, Nichols LO. Factors predicting readmission of older general medicine patients. J Gen Intern Med. 1991 Sep-Oct;6(5):389–393. doi: 10.1007/BF02598158. [DOI] [PubMed] [Google Scholar]
- 17.Huynh C, Wong IC, Tomlin S, et al. Medication discrepancies at transitions in pediatrics: a review of the literature. Paediatr Drugs. 2012 Jun;15(3):203–215. doi: 10.1007/s40272-013-0030-8. [DOI] [PubMed] [Google Scholar]
- 18.Berry JG, Ziniel SI, Freeman L, et al. Hospital Readmission and Parent Perceptions of Their Child's Hospital Discharge. International Journal for Quality in Health Care. 2012 doi: 10.1093/intqhc/mzt051. Under review, October 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007 Jun 25;167(12):1305–1311. doi: 10.1001/archinte.167.12.1305. [DOI] [PubMed] [Google Scholar]
- 20.Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013 Mar 22; doi: 10.1002/jhm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poon EG, Gandhi TK, Sequist TD, Murff HJ, Karson AS, Bates DW. "I wish I had seen this test result earlier!": Dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004 Nov 8;164(20):2223–2228. doi: 10.1001/archinte.164.20.2223. [DOI] [PubMed] [Google Scholar]
- 22.Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005 Jul 19;143(2):121–128. doi: 10.7326/0003-4819-143-2-200507190-00011. [DOI] [PubMed] [Google Scholar]
- 23.Weiss ME, Costa LL, Yakusheva O, Bobay KL. Validation of Patient and Nurse Short Forms of the Readiness for Hospital Discharge Scale and Their Relationship to Return to the Hospital. Health Serv Res. Jul 16; doi: 10.1111/1475-6773.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009 Mar;24(3):381–386. doi: 10.1007/s11606-008-0882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bautista J. 2012 American Association of Neurology Meeting. New Orleans: 2012. Identifying Reasons for Readmission from the Epilepsy Monitoring Unit Compared to a General Neurology Hospital Service. P04.017. [Google Scholar]
- 26.Social Security Act. 42 U.S. C. §1395x(ee), 42 U.S.C. §1395a(a), 42 U.S.C. §1395cc(a)(1)(S) United States: 1965. [Google Scholar]
- 27.Federal Register 69 49268. 42 C.F.R. §482.13, 42 C.F.R. §482.43(a–e) United States: 2004. Condition of Participation: Discharge Planning. [Google Scholar]
- 28.Centers for Medicare and Medicaid Services. State Operations Manual. Appendix A - Survey Protocol, Regulations and Interpretive Guidelines for Hospitals. 2013 [Google Scholar]
- 29.Birmingham J. Discharge Planning Guide: Tools for Compliance. 3. Danvers, MA: HCPro, Inc; 2010. [Google Scholar]
- 30.Williams MV, Coleman E. BOOSTing the hospital discharge. J Hosp Med. 2009 Apr;4(4):209–210. doi: 10.1002/jhm.525. [DOI] [PubMed] [Google Scholar]
- 31.Boston University Medical Center. Project RED (Re-Engineering Discharge) [Accessed November 27, 2013]; http://www.bu.edu/fammed/projectred/index.html.
- 32.Rutherford P, Nielsen GA, Taylor J, Bradke P, Coleman E. How-to-Guide: Improving transitions from the hospital to community settings to reduce avoidable rehospitalizations. Cambridge, MA: Institute for Healthcare Improvement; 2012. [Google Scholar]
- 33.Coleman E. The Care Transitions Program: Health Care Services for Improving Quality and Safety During Care Hand-offs. [Accessed November 27, 2014]; http://www.caretransitions.org/ctm_main.asp.
- 34.Soong C, Daub S, Lee J, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013 Aug;8(8):444–449. doi: 10.1002/jhm.2032. [DOI] [PubMed] [Google Scholar]
- 35.Harlan GA, Nkoy FL, Srivastava R, et al. Improving transitions of care at hospital discharge--implications for pediatric hospitalists and primary care providers. J Healthc Qual. 2010 Sep-Oct;32(5):51–60. doi: 10.1111/j.1945-1474.2010.00105.x. [DOI] [PubMed] [Google Scholar]
- 36.Noyes J, Lewis M. From Hospital to Home: Guidance on Discharge Management and Community Support for Children Using Long-Term Ventilation. Essex, UK: Barnardo's Children's Charity; 2005. [Google Scholar]
- 37.Holland DE, Bowles KH. Standardized discharge planning assessments: impact on patient outcomes. J Nurs Care Qual. 2012 Jul-Sep;27(3):200–208. doi: 10.1097/NCQ.0b013e31824ebc59. [DOI] [PubMed] [Google Scholar]
- 38.Anthony D, Chetty VK, Kartha A, McKenna K, DePaoli MR, Jack B. Re-engineering the Hospital Discharge: An Example of a Multifaceted Process Evaluation and Methodology) 2005 Feb; [PubMed] [Google Scholar]
- 39.Anthony D, Chetty VK, Kartha A, McKenna K, DePaoli MR, Jack B. Re-engineering the Hospital Discharge: An Example of a Multifaceted Process Evaluation. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation. Vol 2: Concepts and Methodology. 2011/01/21 ed. Rockville, MD: Agency for Healthcare Research and Quality; 2005. [PubMed] [Google Scholar]
- 40.Alpers A. Key legal principles for hospitalists. Am J Med. 2001 Dec 21;111(9B):5S–9S. doi: 10.1016/s0002-9343(01)00962-7. [DOI] [PubMed] [Google Scholar]
- 41.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009 Feb 3;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 43.Ng DK, Chow PY, Lai WP, Chan KC, And BL, So HY. Effect of a structured asthma education program on hospitalized asthmatic children: a randomized controlled study. Pediatr Int. 2006 Apr;48(2):158–162. doi: 10.1111/j.1442-200X.2006.02185.x. [DOI] [PubMed] [Google Scholar]
- 44.Wesseldine LJ, McCarthy P, Silverman M. Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child. 1999 Feb;80(2):110–114. doi: 10.1136/adc.80.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Madge P, McColl J, Paton J. Impact of a nurse-led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax. 1997 Mar;52(3):223–228. doi: 10.1136/thx.52.3.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taggart VS, Zuckerman AE, Sly RM, et al. You Can Control Asthma: evaluation of an asthma education program for hospitalized inner-city children. Patient Educ Couns. 1991 Feb;17(1):35–47. doi: 10.1016/0738-3991(91)90049-b. [DOI] [PubMed] [Google Scholar]
- 47.Broyles RS, Tyson JE, Heyne ET, et al. Comprehensive follow-up care and life-threatening illnesses among high-risk infants: A randomized controlled trial. Jama. 2000 Oct 25;284(16):2070–2076. doi: 10.1001/jama.284.16.2070. [DOI] [PubMed] [Google Scholar]
- 48.Coleman EA, Chugh A, Williams MV, et al. Understanding and Execution of Discharge Instructions. Am J Med Qual. 2013 Jan 25; doi: 10.1177/1062860612472931. [DOI] [PubMed] [Google Scholar]
- 49.Chugh A, Williams MV, Grigsby J, Coleman EA. Front Health Serv Manage. 3. Vol. 25. Spring; 2009. Better transitions: improving comprehension of discharge instructions; pp. 11–32. [PubMed] [Google Scholar]
- 50.Weiss M. Health literacy and patient safety: Help patients understand. Chicago, IL: American Hospital Association Foundation; 2007. [Google Scholar]
- 51.Kornburger C, Gibson C, Sadowski S, Maletta K, Klingbeil C. Using "teach-back" to promote a safe transition from hospital to home: an evidence-based approach to improving the discharge process. J Pediatr Nurs. 2013 May-Jun;28(3):282–291. doi: 10.1016/j.pedn.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 52.Sehgal NL, Green A, Vidyarthi AR, Blegen MA, Wachter RM. Patient whiteboards as a communication tool in the hospital setting: a survey of practices and recommendations. J Hosp Med. 2010 Apr;5(4):234–239. doi: 10.1002/jhm.638. [DOI] [PubMed] [Google Scholar]
- 53.Kind AJH, Smith MA. Documentation of Mandated Discharge Summary Components in Transitions from Acute to Subacute Care Culture and Redesign) 2008 Aug; [PubMed] [Google Scholar]
- 54.Beardsley JR, Schomberg RH, Heatherly SJ, Williams BS. Implementation of a Standardized Discharge Time-out Process to Reduce Prescribing Errors at Discharge. Hosp Pharm. 2013 Jan;48(1):39–47. doi: 10.1310/hpj4801-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lidz CW, Appelbaum PS, Meisel A. Two models of implementing informed consent. Arch Intern Med. 1988 Jun;148(6):1385–1389. [PubMed] [Google Scholar]
- 56.Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009 Apr 27;169(8):771–780. doi: 10.1001/archinternmed.2009.51. [DOI] [PubMed] [Google Scholar]
- 57.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006 Mar 13;166(5):565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 58.Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med. 2013 Mar 5;158(5 Pt 2):397–403. doi: 10.7326/0003-4819-158-5-201303051-00006. [DOI] [PubMed] [Google Scholar]
- 59.Smith VC, Hwang SS, Dukhovny D, Young S, Pursley DM. Neonatal intensive care unit discharge preparation, family readiness and infant outcomes: connecting the dots. J Perinatol. 2013 Jun;33(6):415–421. doi: 10.1038/jp.2013.23. [DOI] [PubMed] [Google Scholar]
- 60.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003 Jan 13;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 61.White M, Garbez R, Carroll M, Brinker E, Howie-Esquivel J. Is "teach-back" associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J Cardiovasc Nurs. 2013 Mar-Apr;28(2):137–146. doi: 10.1097/JCN.0b013e31824987bd. [DOI] [PubMed] [Google Scholar]
- 62.Re-engineered discharge cuts readmissions. Hosp Case Manag. 2012 May;20(5):70–75. [PubMed] [Google Scholar]
- 63.Multi-faceted program cuts HF readmissions. Hosp Case Manag. 2012 Jun;20(6):92–93. [PubMed] [Google Scholar]
- 64.Weiss M, Johnson NL, Malin S, Jerofke T, Lang C, Sherburne E. Readiness for discharge in parents of hospitalized children. J Pediatr Nurs. 2008 Aug;23(4):282–295. doi: 10.1016/j.pedn.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 65.Lerret SM, Weiss ME. How ready are they? Parents of pediatric solid organ transplant recipients and the transition from hospital to home following transplant. Pediatr Transplant. 2011 Sep;15(6):606–616. doi: 10.1111/j.1399-3046.2011.01536.x. [DOI] [PubMed] [Google Scholar]
- 66.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011 Feb 16;305(7):682–690. doi: 10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013 Jan 23;309(4):372–380. doi: 10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Berry JG, Graham DA, Graham RJ, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009 Aug;124(2):563–572. doi: 10.1542/peds.2008-3491. [DOI] [PMC free article] [PubMed] [Google Scholar]