Abstract
Objective
Accumulation of epicardial adipose tissue (EAT) is considered to be a cardiovascular risk factor independent from visceral adiposity, obesity, hypertension and diabetes. We explored the parameters related to EAT accumulation, aiming to clarify the novel pathophysiological roles of EAT in subjects with type 2 diabetes (T2DM).
Methods
We examined the laboratory values, including cystatinC, and surrogate markers used for evaluating atherosclerosis. EAT was measured as the sum of the adipose tissue area, obtained by plain computed tomography scans in 208 subjects with T2DM but no history of coronary artery disease.
Results
EAT correlated positively with age, body mass index (BMI), visceral fat area, leptin, cystatin C and C-peptide, while correlating negatively with adiponectin, estimated glomerular filteration rate (eGFR) and the liver-to-spleen ratio. Multiple linear regression analysis revealed serum cystatin C (β = 0.175), leptin (β = 0.536), BMI (β = 0.393) and age (β = 0.269) to be the only parameters showing independent statistically significant associations with EAT. When cystatin C was replaced with eGFR, eGFR showed no significant correlation with EAT. In reverse analysis, serum cystatin C was significantly associated with EAT after adjustment in multivariate analysis.
Discussion
EAT accumulation and elevated cystatin C have been independently regarded as risk factors influencing atherosclerosis. The strong association between EAT and cystatin C demonstrated herein indicates that EAT accumulation may play an important role in Cystatin C secretion, possibly contributing to cardiometabolic risk in T2DM patients.
Introduction
Epicardial adipose tissue (EAT) has recently been recognized not only as fat deposited around the pericardium, but also as a metabolically active tissue, secreting various humoral factors [1]. The volume of EAT accumulation is, in fact, associated with parameters related to obesity, especially the visceral fat area, as well as markers of insulin resistance [2]. In this decade, the pathophysiological roles of EAT have been attracting attention based on their relevance to both atherosclerotic surrogate markers [3, 4] and cardiovascular disease [5, 6], independent of obesity, hypertension and type 2 diabetes mellitus (T2DM). Moreover, a case-control study showed increased EAT volume to be related to major adverse cardiac events in subjects who have no prior history of coronary artery disease (CAD) [7].
EAT is a source of bioactive molecules, including adipocyokines and growth factors, directly impacting inflammation of the myocardium and coronary arteries. Similar to visceral fat, increasing obesity accompanied by epicardial adipocyte enlargement, leads to deterioration of adipocytokine signaling, including enhancement of plasminogen activator inhibitor (PAI)-1, tumor necrosis factor (TNF)-α and leptin expressions and a decrease in adiponectin expression [8]. This potential for local production of various cytokines is regarded as a major mechanism underlying the effects of EAT accumulation on the development of atherosclerosis. The profile of adipocytokine expression in EAT is reportedly comparable to that in visceral fat, as exemplified by the reduced expression of adiponectin in adipose tissue from CAD subjects [9].
The recent advances in imaging technology enable us to quantify EAT using modalities such as echocardiography [10], magnetic resonance imaging [11] and multi-detector computed tomography (MDCT) [12]. Among these modalities, MDCT provides the most reproducible determination of EAT because of its higher spatial resolution, resulting in accurate quantification. Obtaining information on calcification of coronary arteries, an established predictor of CAD, is another merit of performing cardiac CT.
While several studies have shown the importance of EAT accumulation in the development of atherosclerosis, the EAT associated factors influencing atherosclerosis as not as yet fully understand. Thus, we designed this cross-sectional study to examine associations among EAT, humoral factors and atherosclerotic surrogate markers in T2DM patients, who are known to be at risk for CAD. In this study, we explored the parameters related to EAT accumulation, aiming to clarify the novel pathophysiological roles of EAT in subjects with T2DM.
Materials and methods
Study subjects
The study subjects were T2DM patients admitted to Iwate Medical University Hospital during the period from January 2014 to July 2016. Two hundred and eight subjects, all of whom underwent cardiac MDCT, were enrolled in this study. Patients were excluded if they had renal dysfunction (estimated glomerular filtration rate with serum creatinine [eGFRcre] below 45 mL min-1 1.73 m-2), any malignancy, an infectious disorder, collagen disease or a past history of CAD. This study was approved by the Institutional Review Board of Iwate Medical University (Approval number: H27-30). The concent of the study was informed and obtained by written form.
Quantification of EAT
EAT and the coronary artery calcification score (CACS) were quantified on ECG-gated diagnostic cardiac CT scans with some modification [13, 14]. A VCT 240 slice MDCT (Aquillion ONE, Toshiba Medical, Tokyo, Japan) was used to obtain plain multi-slice CT scans, performed with a 0.5 mm collimation width, a gantry rotation speed of 0.4 s/rotation, 120 kV and 300 mA, using prospective ECG-gated axial scanning.
Measurements of EAT were performed by CT scanning with cross-sectional axial views employing imageswith 3mm gaps. The range for measurement of EAT was set as the origin of the left main coronary trunk for the superior border and 6cm below the superior border for the basal border [15]. Quantification of the EAT area (cm2) was performed using software programs (Slim Vision 5, Cybernet Systems, Japan). The EAT area was calculated by manually tracing a region of interest (ROI), which was placed outside the line of the visceral pericardium to exclude pericardial fluid. A density range between -200 and -30 Hounsfield Units was used to isolate adipose tissue [14, 16]. The EAT area of each slice was summed from 20 slices and multiplied by the slice number to evaluate the EAT volume (cm3). A representative image is shown in Fig 1. The EAT values obtained from 20 slices were validated by assessing the correlation with those of whole cardiac scanning image from the same person, in a portion of the subjects enrolled in this study (n = 105, r = 0.974, p < 0.01).
Fig 1. The representative image of CT image evaluating EAT.
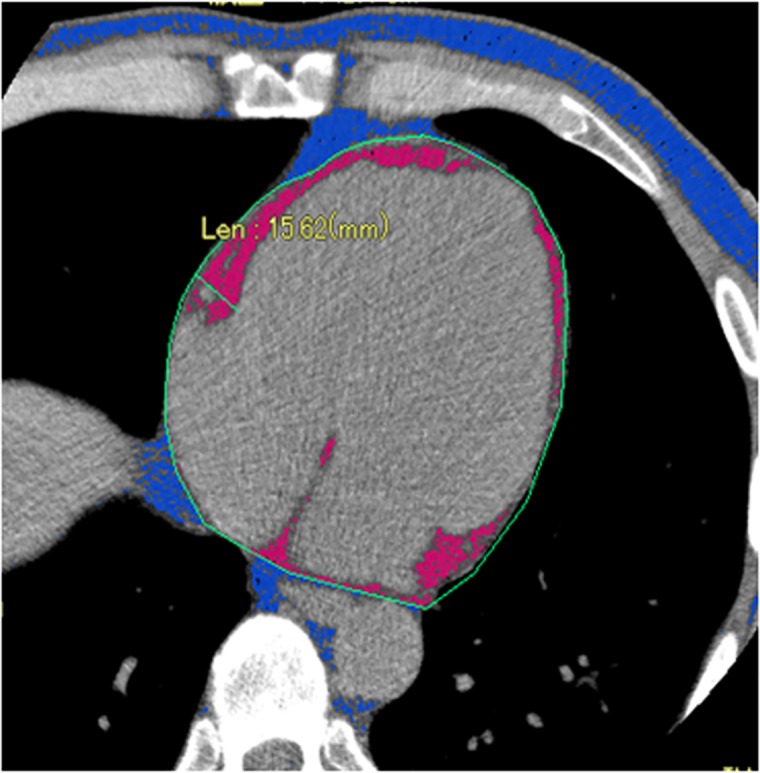
A region of interest (ROI) was manually traced along the visceral pericardium as indicated green line. A density range between -200 and -30 Hounsfield Units was used to isolate adipose tissue displayed as pink area.
CT imaging analyses
The total CACS were analyzed according to the Agatston method [15] and were determined as previously reported [17]. The volume of abdominal fat, divided into visceral fat area and subcutaneous fat area, was obtained from CT images scanned at the level of the fourth lumbar vertebra [18]. Hepatic steatosis was defined as a liver to spleen density ratio below 0.9, based on plain abdominal CT [19].
Measurements of ABI, baPWV and carotid artery IMT
The ABI (ankle brachial pressure index) and brachial ankle pulse wave velocity (baPWV) were measured using an automatic waveform analyzer (BP-203RPE; Colin Co., Komaki, Japan). The intima-media thickness (IMT) of the carotid arteries was measured using ultrasound diagnostic equipment (LOGIQ 500, GE Yokogawa Medical Systems Corp., Hino, Tokyo, Japan) and the max IMT, i.e. the thickest portion detected in the scanned regions, was determined as described previously [17]. These measurement values and CACS were evaluated in order to screen for asymptomatic atherosclerosis in T2DM patients.
Laboratory data analysis
Laboratory values were measured employing routine techniques on blood and urine samples obtained after a 12-h overnight fast in T2DM patients. The value of low dencity lipoprotein cholesterol (LDL-C) was measured using a direct assay method (Sekisui Medical Co., Tokyo, Japan). The serum levels of adipocytekines, including leptin and adiponectin, as well as those of oxidative stress markers, such as urinary 8-isoprostane and 8-hydroxydeoxyguanosine, and serum malondialdehyde-LDL cholesterol, and various unsaturated fatty acid were measured by SRL, Inc. (Tokyo, Japan).
Estimated glomerular filtration rates (eGFR) were calculated as shown below [20]. Serum creatinine (cre) based eGFR was defined as eGFRcre (mL/min/1.73m2) = 194 x cre-1.094 x age-0.287 (male), 194 x cre-1.094 x age-0.287 x 0.739 (female). Serum cystatin C (cys) based eGFR was defined as eGFRcys (mL/min/1.73m2) = (104 x cys-1.019 x 0.996 age) - 8 (male), (104 x cys-1.019 x 0.996 age x 0.929) - 8 (female).
Statistical analysis
Quantitative data are presented as means ± standard deviation (SD) or as medians with inter quartile range when the data showed a non-normal distribution. Comparisons between the subjects were performed employing the student t test and the chi-square test or, when the data showed a non-normal distribution, the Mann–Whitney U-test. The level of significance was set at P < 0.05. Multiple linear regression analyses were performed to evaluate parameters independently showing significant correlations with EAT and cystatin C. Clinical parameters, showing significant simple correlations with EAT or cystatin C, were assigned as independent variables in multivariate linear regression analysis, unless there was extreme collinearity. All statistical analyses were carried out using SPSS version 21 (SPSS Japan Inc., Tokyo, Japan).
Results
The clinical characteristics of the 208 enrolled subjects are shown in Table 1. Mean age was 58 years, mean diabetes duration was 9.7 years and 125 subjects were males. The mean body mass index (BMI), visceral fat area and homeostasis model assessment (HOMA) -R were 27.0, 160.2 cm2 and 3.1, respectively, indicating moderately obesity and the presence of insulin resistance as compared to Japanese subjects with T2DM in general. The mean EAT values was 52.4 cm3.
Table 1. Baseline characteristics of the study subjects.
| n = 208 | |
|---|---|
| Gender (male / female) | 125 / 83 |
| Age (years) | 58.0 ± 14.3 |
| BMI (kg/m2) | 27.0 ± 6 |
| Diabetes duration (years) | 9.7 ± 9.6 |
| Hypertension, n (%) | 115 (55) |
| Dyslipidemia, n (%) | 152 (73) |
| SBP (mmHg) | 127.8 ± 19.2 |
| DBP (mmHg) | 76.0 ± 12.8 |
| Total cholesterol (mg/dL) | 193.9 ± 49.3 |
| Triglyceride (mg/dL) | 150.8 ± 92.5 |
| HDL cholesterol (mg/dL) | 46.1 ± 13.8 |
| LDL cholesterol (mg/dL) | 119.3 ± 38.7 |
| eGFRcre (mL/min/ 1.73 m2) | 74.8 ± 15.2 |
| eGFRcys (mL/min / 1.73 m2) | 81.1 ± 22.6 |
| 24hrs creatinine clearance (mL/min) | 87.3 ± 30.1 |
| Cystatin C (mg/L) | 0.96 ± 0.24 |
| Fasting blood glucose (mg/dL) | 172.7 ± 79.1 |
| HbA1c (%) | 10.4 ± 2.4 |
| HOMA-R | 3.1 ± 2.9 |
| C-peptide (ng/mL) | 1.64 ± 1.00 |
| Urinary 8-isoprostane (pg/mgCr) | 245.8 ± 124.7 |
| Urinary 8-OHdG (pg/mgCr) | 11.1 ± 5.5 |
| MDA-LDL (U/dL) | 134.5 ± 47.5 |
| Leptin (ng/mL) | 12.2 ± 9.6 |
| Adiponectin (μg/mL) | 3.2 ± 3.3 |
| High-sensitivity C-reactive protein (mg/dL) | 0.11 (0.04–0.31) |
| DGLA (μg/mL) | 37.6 ± 18.8 |
| AA (μg/mL) | 193.8 ± 58.7 |
| EPA (μg/mL) | 73.5 ± 46.7 |
| DHA (μg/mL) | 149.8 ± 59.6 |
| EPA/AA | 0.4 ± 0.3 |
| max IMT (mm) | 1.45 (1.00–2.00) |
| baPWV (cm/s) | 1499 (1251–1749) |
| ABI | 1.12 (1.06–1.18) |
| Coronary artery calcification score, (AU) | 20.0 (0–143.8) |
| Visceral Fat Area (cm2) | 156.4 (112.8–200.0) |
| Subcutaneous Fat Area (cm2) | 175.0 (121.2–267.1) |
| EAT (cm3) | 52.4 ± 29.5 |
| Liver spleen ratio | 1.12 ± 0.28 |
| Diabetic retinopathy, n (%) | 58 (28) |
| Peripheral neuropathy, n (%) | 94 (46) |
| History of smoking, n (%) | 110 (53) |
| Af, n (%) | 18 (9) |
| History of CVD, n (%) | 25 (12) |
| Family history of CVD, n (%) | 82 (39) |
| Diabetic nephropathy Normoalbuminuria (<30 mg/ gCre) | 140 (77.4) |
| Microalbuminuria (30–299 mg/ gCre) | 51 (24.5) |
| Overtalbuminuria (≥300 mg/ gCre) | 17 (8.1%) |
| DPP-4 inhibitors, n (%) | 101 (49) |
| Insulin, n (%) | 96 (46) |
| Metformin, n (%) | 53 (25) |
| Sulfonylurea, n (%) | 37 (18) |
| Alpha-glucosidase inhibitor, n (%) | 30 (14) |
| Glinide, n (%) | 6 (3) |
| Glucagon-like peptide-1, n (%) | 9 (4) |
| Thiazolidinedione, n (%) | 13 (6) |
| SGLT inhibitor, n (%) | 5 (2) |
| Statins, n (%) | 86 (41) |
| RAS inhibitors, n (%) | 84 (40) |
| Calcium channel blocker, n (%) | 57 (27) |
| Diuretics, n (%) | 31 (15) |
SBP: systolic blood pressure, DBP: diastolic blood pressure, HbA1c: hemoglobin A1c, DGLA: dihomo-gamma-linolenic acid, AA: arachidonic acid, EPA: eicosapentaenoic acid, DHA: docosahexaenoic acid, CVD: cerebral vascular disease, DPP: dipeptidyl peptidase, RAS: renin-angiotensin system, SGLT: Sodium-dependent glucose transporter, 8-OHdG: 8-hydroxydeoxyguanosine
The volume of EAT correlated positively with age (r = 0.206, p < 0.01), BMI (r = 0.488, p < 0.01), visceral fat area (r = 0.603, p < 0.01), levels of serum dihomo-gamma-linolenic acid levels (DGLA) (r = 0.184, p < 0.01), leptin (r = 0.496, p < 0.01), cystatin C (r = 0.320, p < 0.01) and C-peptide (r = 0.263, p < 0.01), as well as with HOMA-R (r = 0.262 p < 0.01) (Table 2). The EAT values showed negative correlations with adiponectin (r = -0.173, p < 0.05), eGFRcre (r = -0.218, p < 0.01), eGFRcys (r = -0.362, p < 0.01) and the liver-to-spleen ratio (r = -0.186, p < 0.01). Consistent with previous reports, EAT values correlated with the parameters known to be related to metabolic syndrome in Japanese subjects. In addition, the EAT values were higher in females and in the subjects with hypertension.
Table 2. Correlations of clinical parameters with EAT.
| Variable | Correlation coefficient | EAT values | P value |
|---|---|---|---|
| Age, (years) | 0.206 | 0.003 | |
| BMI (kg/m2) | 0.488 | < 0.001 | |
| Diabetes duration (years) | 0.111 | 0.114 | |
| SBP (mmHg) | 0.080 | 0.253 | |
| DBP (mmHg) | -0.006 | 0.929 | |
| Total cholesterol (mg/dL) | -0.077 | 0.266 | |
| Triglyceride (mg/dL) | 0.045 | 0.516 | |
| HDL cholesterol (mg/dL) | -0.123 | 0.076 | |
| LDL cholesterol (mg/dL) | -0.048 | 0.487 | |
| eGFRcre (ml/min /1.73 m2) | -0.218 | 0.002 | |
| eGFRcys (ml/min / 1.73 m2) | -0.362 | < 0.001 | |
| 24hrs creatinine clearance (mL/min) | 0.011 | 0.877 | |
| Cystatin C (mg/L) | 0.320 | < 0.001 | |
| Fasting blood glucose (mg/dL) | -0.079 | 0.258 | |
| HbA1c (%) | -0.112 | 0.110 | |
| HOMA-R | 0.262 | < 0.001 | |
| C-peptide (ng/mL) | 0.264 | < 0.001 | |
| Urinary 8-isoprostane (pg/mgCr) | -0.029 | 0.681 | |
| Urinary 8-OHdG (pg/mgCr) | 0.024 | 0.728 | |
| MAD-LDL (U/dL) | 0.018 | 0.795 | |
| Leptin (ng/mL) | 0.496 | < 0.001 | |
| Adiponectin (μg/mL) | -0.173 | 0.012 | |
| High-sensitivity C-reactive protein (mg/L) | 0.137 | 0.062 | |
| DGLA (μg/mL) | 0.184 | 0.008 | |
| AA (μg/mL) | -0.010 | 0.890 | |
| EPA (μg/mL) | 0.095 | 0.171 | |
| DHA (μg/mL) | 0.039 | 0.580 | |
| EPA/AA | 0.090 | 0.194 | |
| max IMT (mm) | -0.013 | 0.856 | |
| baPWV (cm/s) | 0.095 | 0.173 | |
| ABI | 0.066 | 0.344 | |
| Coronary artery calcification score (AU) | 0.074 | 0.288 | |
| Visceral Fat Area (cm2) | 0.603 | < 0.001 | |
| Liver-to-spleen ratio | -0.186 | 0.009 | |
| Male vs Female* | 48.5±27.2 vs58.5±32.0 | 0.022 | |
| Hypertension (Yes vs No)* | 55.8±29.0 vs 48.3±29.9 | 0.048 | |
| Dyslipidemia (Yes vs No)* | 51.7±28.0 vs 54.5±33.5 | 0.577 |
Spearman rank correlation coefficient
* analyzed by Mann-Whitney U-test, values are mean±SD
Next, we performed multiple linear regression analyses to identify variables independently related to EAT values (Table 3). Multivariate analysis, adjusted for sex, adiponectin, the liver-to-spleen ratio, DGLA and HOMA-R, revealed age, BMI, serum leptin level, the presence of hypertension and the cystatin C level to be positively related to EAT values. Since the serum cystatin C level is an established marker of renal function, to assess whether the effect of cystatin C on EAT values reflects glomerular filtration, we performed multivariate analysis employing Model 2, switching one of the dependent variables from cystatin C to eGFRcre. Intriguingly, this multiple linear regression analysis revealed eGFRcre to not be independently associated with EAT values. This result suggested the association between cystatin C and EAT values to be independent of glomerular filtration rate evaluated by serum creatinine level.
Table 3. Multiple regression analysis for EAT.
| Model 1. | Model 2. | |||
|---|---|---|---|---|
| Variables | β | P value | β | P value |
| Age | 0.335 | < 0.001 | 0.373 | < 0.001 |
| Leptin | 0.260 | 0.011 | 0.346 | 0.001 |
| BMI | 0.393 | < 0.001 | 0.363 | < 0.001 |
| Cystatin C | 0.199 | 0.003 | ||
| eGFRcre | -0.079 | 0.238 | ||
Model 1: independent variables: Age, Leptin, Sex, Adiponectin, Liver-to-spleen ratio, HOMA-R, BMI, DGLA, presence of hypertension and Cystatin-C
Model 2: independent variables: Age, Leptin, Sex, Adiponectin, Liver-to-spleen ratio, HOMA-R, BMI, DGLA, presence of hypertension and eGFRcre
β; the standard coefficient
the multiple coefficient of determination (R2) = 0.408 (Model 1) and 0.413 (Model 2)
To investigate the effects of cystatin C on clinical parameters in our study subjects, we performed simple and multiple linear regression analyses for cystatin C. The serum cystatin C level showed significant correlation with age, diabetes duration, visceral fat area, EAT, IMT, PWV and CACS (Table 4). Furthermore, cystatin C correlated negatively with the parameters reflecting renal function, including eGFRcre, eGFRcys and 24hrCcr, and HbA1c. The EAT values were higher in the subjects with hypertension. Interestingly, cystatin C showed associations with the parameters related to metabolic syndrome and with the surrogate markers of atherosclerosis. Multiple linear regression analysis, adjusted for age, gender, EAT, max IMT, CACS, baPWV, HbA1c and the presence of hypertension, revealed age, male, EAT and the presence of hypertension to show independent statistically significant associations with cystatin C (Table 5).
Table 4. Correlations of clinical parameters with cystatin C.
| Variable | Correlation cofficient | Cystatin C value | P value |
|---|---|---|---|
| Age (years) | 0.450 | < 0.001 | |
| BMI (kg/m2) | -0.040 | 0.565 | |
| Diabetes duration (years) | 0.290 | < 0.001 | |
| SBP (mmHg) | -0.059 | 0.394 | |
| DBP (mmHg) | 0.390 | 0.775 | |
| Total cholesterol (mg/dL) | -0.045 | 0.516 | |
| Triglyceride (mg/dL) | 0.122 | 0.080 | |
| HDL cholesterol (mg/dL) | -0.130 | 0.062 | |
| LDL cholesterol (mg/dL) | -0.102 | 0.141 | |
| eGFRcre (ml/min/ 1.73 m2) | -0.759 | < 0.001 | |
| eGFRcys (ml/min/ 1.73 m2) | -0.963 | < 0.001 | |
| 24hrs creatinine clearance (mL/min) | -0.489 | < 0.001 | |
| Fasting blood glucose (mg/dL) | -0.166 | 0.017 | |
| HbA1c (%) | -0.204 | 0.003 | |
| HOMA-R | -0.026 | 0.712 | |
| C-peptide (ng/mL) | 0.183 | 0.008 | |
| Urinary 8-isoprostane (pg/mgCr) | -0.086 | 0.223 | |
| Urinary 8-OHdG (pg/mgCr) | 0.063 | 0.367 | |
| MDA-LDL (U/dL) | -0.027 | 0.703 | |
| Leptin (ng/mL) | 0.090 | 0.196 | |
| Adiponectin (μg/mL) | 0.074 | 0.290 | |
| High-sensitivity C-reactive protein (mg/L) | 0.138 | 0.060 | |
| DGLA (μg/mL) | 0.084 | 0.228 | |
| AA (μg/mL) | -0.147 | 0.034 | |
| EPA (μg/mL) | 0.151 | 0.029 | |
| DHA (μg/mL) | 0.093 | 0.179 | |
| EPA/AA | 0.214 | 0.002 | |
| max IMT (mm) | 0.285 | < 0.001 | |
| baPWV (cm/s) | 0.340 | < 0.001 | |
| ABI | 0.065 | 0.351 | |
| Coronary artery calcification score (AU) | 0.320 | < 0.001 | |
| Visceral Fat Area (cm2) | 0.199 | 0.006 | |
| Subcutaneous Fat Area (cm3) | -0.057 | 0.440 | |
| EAT (cm3) | 0.320 | < 0.001 | |
| Liver-to-spleen ratio | 0.058 | 0.445 | |
| Male vs Female* | 0.98±0.26 vs 0.92±0.20 | 0.138 | |
| Hypertension (Yes vs No)* | 1.01±0.27 vs 0.89±0.18 | <0.001 | |
| Dyslipidemia (Yes vs No)* | 0.97±0.25 vs 0.93±0.22 | 0.361 |
Spearman rank correlation coefficient
* analyzed by Mann-Whitney U-test, values are mean±SD
Table 5. Multiple regression analysis for cystatin C.
| Factors | β | P value |
|---|---|---|
| Age | 0.243 | 0.005 |
| Sex | -0.188 | < 0.001 |
| EAT | 0.306 | < 0.001 |
| max IMT | 0.074 | 0.334 |
| CACS | 0.042 | 0.559 |
| PWV | -0.045 | 0.576 |
| Hypertension | 0.142 | 0.039 |
| HbA1c | -0.043 | 0.525 |
β; the standard coefficient
the multiple coefficient of determination (R2) = 0.259
In addition, there were no significant differences either EAT volume or cystatin C values between users and non-users of various medications, including drugs for diabetes, statins and renin-angiotensin system inhibitors.
Discussion
This study is the first, to our knowledge, to demonstrate a close relationship between EAT accumulation and the serum level of cystatin C, independent from glomerular filtration rate in Japanese T2DM. Because the incidence of CAD in the Japanese population has been rising in recent decades, identification of factors contributing to the development of atherosclerosis resulting from adiposity is important. Our present observations shed light on the mechanism of atherosclerosis development in T2DM patients with fat accumulation.
EAT arises from brown adipose tissue as well as visceral adipose tissue [21] and possesses biological characteristics to similar those of visceral fat [22]. While the volume of EAT accounts for only one percent of whole fat mass [1], adipocytes in the epicardium are able to synthesize, produce and secrete bioactive humoral factors which are transported into the myocardium via vasocrine and/or paracrine pathways [23]. These bioactive molecules, including inflammatory cytokines, secreted from EAT might interact directly with coronary arteries and the myocardium. In addition, expressions and secretions of inflammatory cytokines, such as resistin, monocyte chemotactic protein (MCP)-1 and TNF-α, are higher in EAT than in subcutaneous fat tissue (SAT) [24] and inflammatory cells markedly infiltrate EAT as compared to SAT in CAD subjects [1]. Moreover, expressions of mRNA involved in oxidative stress are higher in EAT than in SAT [25]. Taken together, our results and those of other investigators indicate that EAT has distinctive pathogenic and pathophysiological characteristics with exacerbate inflammation and oxidative stress, leading to the development of atherosclerosis.
The volume of EAT reportedly showed association with surrogate markers of atherosclerosis, including CACS [5], carotid IMT [3], carotid stiffness [4] and the degree of coronary artery stenosis [26]. However, in this study, there was no association between EAT volume and surrogate markers of atherosclerosis, including CACS, max IMT, baPWV and ABI. A meta-analysis [27] and a multicenter study [28] also found no associations between EAT and atherosclerotic markers, such as CACS. In contrast, CACS was found to have a strong association with CAD and future cardiovascular events in subjects with chronic kidney disease (CKD) [29] and in a large prospective study [30]. Kaikita et al reported EAT to correlate positively not with calcified, but rather with non-calcified coronary plaque in subjects at high risk for CAD [31], suggesting that EAT may reflect early stage atherosclerosis and serve as a predictive marker of CAD progression. Statins administered to 41% of enrolled subjects, were reported to possibly impact the association between EAT and CACS, though whether statin usage promotes vascular calcification remains controvercial [32]. In addition, taking the T2DM population as a whole, wherein atherosclerosis development is attributable to multiple factors, we can reasonably specurate that the association between EAT and atherosclerotic markers might be obscured.
Cystatin C, a 13-kD endogenous cysteine proteinase inhibitor, is ubiquitously expressed, mainly in the brain, testis, lung, spleen and adipose tissue [33]. Cystatin C is freely filtered by the glomeruli, and catabolized in the proximal tubules. As muscle mass, gender and protein intake exert no influence on serum cystatin C, it is a more reliable marker of renal function than eGFR which is based on creatinine [34, 35].
Epidemiological studies have shown serum cystatin C to be increased in humans with obesity [36]. Naour et al showed cystatin C mRNA expression to be significantly elevated in omental and subcutaneous adipose tissue and increased three-fold in obese as compared to lean subjects [37]. Consistent with our result, a relationship between EAT and serum cystatin C was demonstrated in subjects with acromegaly [38]. Taken together with the previous findings of an association between visceral fat and EAT, cystatin C might be expressed in EAT and is then probably secreted into the circulation. Our present study demonstrated a strong association between EAT and serum cystatin C independent of glomerular filtration rate, supporting this hypothesis.
On the other hand, elevated cystatin C is reportedly associated with the presence or likely development of cardiovascular disease in subjects without chronic kidney disease [39, 40]. Moreover, the serum cystatin C level showed strong correlations with the degree of CAD [41, 42] and all-cause mortality [43]. Taken together, these results indicate that cystatin C is not simply a marker of impaired kidney function but also a marker of cardiovascular disease. Cystatin C is an endogenous inhibitor of cysteine protease, including cathepsin B, K and S, which are involved in degradation of the extracellular matrix and migration of monocytes and macrophages into the intima [44]. An imbalance between cysteine proteases and their inhibitor, cystatin C, may affect vascular inflammation, potentially leading to the development of atherosclerosis and inflammatory disorders [45]. Associations of serum cystatin C with inflammatory parameters, C-reactive protein and fibrinogen, were demonstrated, suggesting a role of cystatin C in systemic inflammation [46]. Furthermore, plasma cystatin C levels correlated with a build-up of amyloid deposits in the vascular walls in myocardial ischemic model mice [47]. In this study, elevated serum cystatin C showed a simple correlation with surrogate markers of atherosclerosis, such as max IMT, baPWV and CACS, while these relationships disappeared with adjustment for age on multiple regression analysis. This result supports the hypothesis that cystatin C exerts an effect on atherosclerosis development in T2DM.
The strengths of this study include the employment of numerous surrogate markers for atherosclerosis and other obesity-related disease as independent variables in conducting correlation analyses focusing on EAT. Among the obesity-related markers, such as adipocytokines, inflammatory cytokines and polyunsaturated fatty acids, studied herein, a particularly strong association between cystatin C and EAT was revealed. Serum cystatin C showed a significant association with EAT even after adjustment for several confounding factors. This study supports the hypothesis, and its clinical implications, that cystatin C elevation, related to EAT accumulation, exerts an additional impact on atherosclerosis development. Surrogate markers for evaluating atherosclerosis, including EAT volume, are informative but somewhat inconvenient and expensive to obtain, due to the equipment necessary for performing the measurement. In contrast, measuring serum cystatin C is non-invasive and low-cost. Therefore, assessment of serum cystatin C may allow early detection of atherosclerosis.
The major limitation of this study is its cross-sectional design, raising the possibility that our results show only associations. Therefore, the possible casual relationships between EAT and cystatin C cannot be confirmed, and further prospective study is required. Second, the extent of cardiac CT scanning for EAT evaluation is restricted, to within a range of 6cm from the origin of the left main coronary trunk. Third, the sample size was rather small for performing multivariate analysis incorporating large number of variables. In addition, despite the various clinical characteristics of the enrolled subjects varying rather markedly, the subjects were analyzed as a single group.
EAT accumulation and a high cystatin C concentration have been independently regarded as risk factors influencing atherosclerosis. This study showed a strong association between EAT and cystatin C independent of several confounders, including renal function parameters and several humoral factors. EAT accumulation may play an important role in Cystatin C secretion, thereby possibly contributing to cardiometabolic risk in T2DM.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by Grants-in-Aid for Scientific Research (15K09416) to Y.I., from the Japan Society for the Promotion of Science and a Grant-in-Aid for Strategic Medical Science Research (S1491001, 2014–2018) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
References
- 1.Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108(20):2460–6. Epub 2003/10/29. doi: 10.1161/01.CIR.0000099542.57313.C5 01.CIR.0000099542.57313.C5 [pii]. . [DOI] [PubMed] [Google Scholar]
- 2.Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. The Journal of clinical endocrinology and metabolism. 2003;88(11):5163–8. Epub 2003/11/07. doi: 10.1210/jc.2003-030698 . [DOI] [PubMed] [Google Scholar]
- 3.Fracanzani AL, Pisano G, Consonni D, Tiraboschi S, Baragetti A, Bertelli C, et al. Epicardial Adipose Tissue (EAT) Thickness Is Associated with Cardiovascular and Liver Damage in Nonalcoholic Fatty Liver Disease. PloS one. 2016;11(9):e0162473 Epub 2016/09/15. doi: 10.1371/journal.pone.0162473 ; PubMed Central PMCID: PMCPMC5023162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Natale F, Tedesco MA, Mocerino R, de Simone V, Di Marco GM, Aronne L, et al. Visceral adiposity and arterial stiffness: echocardiographic epicardial fat thickness reflects, better than waist circumference, carotid arterial stiffness in a large population of hypertensives. European journal of echocardiography: the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2009;10(4):549–55. Epub 2009/02/13. jep002 [pii] doi: 10.1093/ejechocard/jep002 . [DOI] [PubMed] [Google Scholar]
- 5.Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117(5):605–13. Epub 2008/01/24. CIRCULATIONAHA.107.743062 [pii] doi: 10.1161/CIRCULATIONAHA.107.743062 . [DOI] [PubMed] [Google Scholar]
- 6.Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, et al. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J. 2009;30(7):850–6. Epub 2009/01/13. ehn573 [pii] doi: 10.1093/eurheartj/ehn573 ; PubMed Central PMCID: PMC3693564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng VY, Dey D, Tamarappoo B, Nakazato R, Gransar H, Miranda-Peats R, et al. Pericardial fat burden on ECG-gated noncontrast CT in asymptomatic patients who subsequently experience adverse cardiovascular events. JACC Cardiovascular imaging. 2010;3(4):352–60. Epub 2010/04/17. doi: 10.1016/j.jcmg.2009.12.013 ; PubMed Central PMCID: PMCPMC2946639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzgibbons TP, Czech MP. Epicardial and perivascular adipose tissues and their influence on cardiovascular disease: basic mechanisms and clinical associations. J Am Heart Assoc. 2014;3(2):e000582 Epub 2014/03/07. jah3448 [pii] doi: 10.1161/JAHA.113.000582 ; PubMed Central PMCID: PMC4187500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker AR, Silva NF, Quinn DW, Harte AL, Pagano D, Bonser RS, et al. Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovasc Diabetol. 2006;5:1 Epub 2006/01/18. 1475-2840-5-1 [pii] doi: 10.1186/1475-2840-5-1 ; PubMed Central PMCID: PMC1352345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeong JW, Jeong MH, Yun KH, Oh SK, Park EM, Kim YK, et al. Echocardiographic epicardial fat thickness and coronary artery disease. Circulation journal: official journal of the Japanese Circulation Society. 2007;71(4):536–9. Epub 2007/03/27. JST.JSTAGE/circj/71.536 [pii]. . [DOI] [PubMed] [Google Scholar]
- 11.Fluchter S, Haghi D, Dinter D, Heberlein W, Kuhl HP, Neff W, et al. Volumetric assessment of epicardial adipose tissue with cardiovascular magnetic resonance imaging. Obesity (Silver Spring, Md). 2007;15(4):870–8. Epub 2007/04/12. doi: 10.1038/oby.2007.591 . [DOI] [PubMed] [Google Scholar]
- 12.Shimabukuro M, Hirata Y, Tabata M, Dagvasumberel M, Sato H, Kurobe H, et al. Epicardial adipose tissue volume and adipocytokine imbalance are strongly linked to human coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 2013;33(5):1077–84. Epub 2013/03/09. ATVBAHA.112.300829 [pii] doi: 10.1161/ATVBAHA.112.300829 . [DOI] [PubMed] [Google Scholar]
- 13.Nichols JH, Samy B, Nasir K, Fox CS, Schulze PC, Bamberg F, et al. Volumetric measurement of pericardial adipose tissue from contrast-enhanced coronary computed tomography angiography: a reproducibility study. J Cardiovasc Comput Tomogr. 2008;2(5):288–95. Epub 2008/12/17. S1934-5925(08)00559-5 [pii] doi: 10.1016/j.jcct.2008.08.008 ; PubMed Central PMCID: PMC3041941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorter PM, van Lindert AS, de Vos AM, Meijs MF, van der Graaf Y, Doevendans PA, et al. Quantification of epicardial and peri-coronary fat using cardiac computed tomography; reproducibility and relation with obesity and metabolic syndrome in patients suspected of coronary artery disease. Atherosclerosis. 2008;197(2):896–903. Epub 2007/09/22. S0021-9150(07)00496-0 [pii] doi: 10.1016/j.atherosclerosis.2007.08.016 . [DOI] [PubMed] [Google Scholar]
- 15.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32. Epub 1990/03/15. 0735-1097(90)90282-T [pii]. . [DOI] [PubMed] [Google Scholar]
- 16.Chun H, Suh E, Byun AR, Park HR, Shim KW. Epicardial fat thickness is associated to type 2 diabetes mellitus in Korean men: a cross-sectional study. Cardiovasc Diabetol. 2015;14:46 Epub 2015/05/04. doi: 10.1186/s12933-015-0210-7 [pii]. ; PubMed Central PMCID: PMC4432519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hangai M, Takebe N, Honma H, Sasaki A, Chida A, Nakano R, et al. Association of Advanced Glycation End Products with coronary Artery Calcification in Japanese Subjects with Type 2 Diabetes as Assessed by Skin Autofluorescence. Journal of atherosclerosis and thrombosis. 2016;23(10):1178–87. Epub 2016/03/11. doi: 10.5551/jat.30155 ; PubMed Central PMCID: PMCPMC5098918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakano NT R., Ono M., Hangai M., Nakagawa R., Yashiro S., Murai T., Nagasawa K., Takahashi Y., Satoh J. and Ishigaki Y. Involvement of oxidative stress in atherosclerosis development in subjects with sarcopenic obesity. Obesity, Science & Practice. 2017. Epub 27 JAN 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ono M, Takebe N, Oda T, Nakagawa R, Matsui M, Sasai T, et al. Association of coronary artery calcification with MDA-LDL-C/LDL-C and urinary 8-isoprostane in Japanese patients with type 2 diabetes. Intern Med. 2014;53(5):391–6. Epub 2014/03/04. DN/JST.JSTAGE/internalmedicine/53.9549 [pii]. . [DOI] [PubMed] [Google Scholar]
- 20.Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2009;53(6):982–92. Epub 2009/04/03. doi: 10.1053/j.ajkd.2008.12.034 . [DOI] [PubMed] [Google Scholar]
- 21.Marchington JM, Mattacks CA, Pond CM. Adipose tissue in the mammalian heart and pericardium: structure, foetal development and biochemical properties. Comparative biochemistry and physiology B, Comparative biochemistry. 1989;94(2):225–32. Epub 1989/01/01. . [DOI] [PubMed] [Google Scholar]
- 22.Bertaso AG, Bertol D, Duncan BB, Foppa M. Epicardial fat: definition, measurements and systematic review of main outcomes. Arq Bras Cardiol. 2013;101(1):e18–28. Epub 2013/08/07. S0066-782X2013002700020 [pii] doi: 10.5935/abc.20130138 ; PubMed Central PMCID: PMC3998169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iacobellis G. Local and systemic effects of the multifaceted epicardial adipose tissue depot. Nat Rev Endocrinol. 2015;11(6):363–71. Epub 2015/04/09. nrendo.2015.58 [pii] doi: 10.1038/nrendo.2015.58 . [DOI] [PubMed] [Google Scholar]
- 24.Kremen J, Dolinkova M, Krajickova J, Blaha J, Anderlova K, Lacinova Z, et al. Increased subcutaneous and epicardial adipose tissue production of proinflammatory cytokines in cardiac surgery patients: possible role in postoperative insulin resistance. The Journal of clinical endocrinology and metabolism. 2006;91(11):4620–7. Epub 2006/08/10. doi: 10.1210/jc.2006-1044 . [DOI] [PubMed] [Google Scholar]
- 25.Salgado-Somoza A, Teijeira-Fernandez E, Fernandez AL, Gonzalez-Juanatey JR, Eiras S. Proteomic analysis of epicardial and subcutaneous adipose tissue reveals differences in proteins involved in oxidative stress. American journal of physiology Heart and circulatory physiology. 2010;299(1):H202–9. Epub 2010/05/04. doi: 10.1152/ajpheart.00120.2010 . [DOI] [PubMed] [Google Scholar]
- 26.Ueno K, Anzai T, Jinzaki M, Yamada M, Jo Y, Maekawa Y, et al. Increased epicardial fat volume quantified by 64-multidetector computed tomography is associated with coronary atherosclerosis and totally occlusive lesions. Circulation journal: official journal of the Japanese Circulation Society. 2009;73(10):1927–33. Epub 2009/08/20. JST.JSTAGE/circj/CJ-09-0266 [pii]. . [DOI] [PubMed] [Google Scholar]
- 27.Xu Y, Cheng X, Hong K, Huang C, Wan L. How to interpret epicardial adipose tissue as a cause of coronary artery disease: a meta-analysis. Coron Artery Dis. 2012;23(4):227–33. Epub 2012/03/01. doi: 10.1097/MCA.0b013e328351ab2c . [DOI] [PubMed] [Google Scholar]
- 28.Tanami Y, Jinzaki M, Kishi S, Matheson M, Vavere AL, Rochitte CE, et al. Lack of association between epicardial fat volume and extent of coronary artery calcification, severity of coronary artery disease, or presence of myocardial perfusion abnormalities in a diverse, symptomatic patient population: results from the CORE320 multicenter study. Circulation Cardiovascular imaging. 2015;8(3):e002676 Epub 2015/03/11. doi: 10.1161/CIRCIMAGING.114.002676 ; PubMed Central PMCID: PMCPMC4355954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerr JD, Holden RM, Morton AR, Nolan RL, Hopman WM, Pruss CM, et al. Associations of epicardial fat with coronary calcification, insulin resistance, inflammation, and fibroblast growth factor-23 in stage 3–5 chronic kidney disease. BMC Nephrol. 2013;14:26 Epub 2013/01/29. 1471-2369-14-26 [pii] doi: 10.1186/1471-2369-14-26 ; PubMed Central PMCID: PMC3571879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elkeles RS. Coronary artery calcium and cardiovascular risk in diabetes. Atherosclerosis. 2010;210(2):331–6. Epub 2009/12/09. S0021-9150(09)00983-6 [pii] doi: 10.1016/j.atherosclerosis.2009.11.026 . [DOI] [PubMed] [Google Scholar]
- 31.Kaikita K. Epicardial Adipose Tissue as a Predictor for the Development of Non-Calcified Coronary Plaque. Journal of atherosclerosis and thrombosis. 2016. Epub 2016/10/14. doi: 10.5551/jat.ED062 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puri R, Nicholls SJ, Shao M, Kataoka Y, Uno K, Kapadia SR, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am Coll Cardiol. 2015;65(13):1273–82. Epub 2015/04/04. doi: 10.1016/j.jacc.2015.01.036 . [DOI] [PubMed] [Google Scholar]
- 33.Abrahamson M, Olafsson I, Palsdottir A, Ulvsback M, Lundwall A, Jensson O, et al. Structure and expression of the human cystatin C gene. Biochem J. 1990;268(2):287–94. Epub 1990/06/01. ; PubMed Central PMCID: PMC1131430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–9. Epub 2012/07/06. doi: 10.1056/NEJMoa1114248 ; PubMed Central PMCID: PMC4398023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2002;40(2):221–6. Epub 2002/07/31. S0272-6386(02)00034-3 [pii] doi: 10.1053/ajkd.2002.34487 . [DOI] [PubMed] [Google Scholar]
- 36.Luc G, Bard JM, Lesueur C, Arveiler D, Evans A, Amouyel P, et al. Plasma cystatin-C and development of coronary heart disease: The PRIME Study. Atherosclerosis. 2006;185(2):375–80. Epub 2005/07/28. doi: 10.1016/j.atherosclerosis.2005.06.017 . [DOI] [PubMed] [Google Scholar]
- 37.Naour N, Fellahi S, Renucci JF, Poitou C, Rouault C, Basdevant A, et al. Potential contribution of adipose tissue to elevated serum cystatin C in human obesity. Obesity (Silver Spring, Md). 2009;17(12):2121–6. Epub 2009/04/11. oby200996 [pii] doi: 10.1038/oby.2009.96 . [DOI] [PubMed] [Google Scholar]
- 38.Aulinas A, Crespo I, Vilades D, Leta R, Urgell E, Biagetti B, et al. Cystatin-C and epicardial adipose tissue as noninvasive predictors of cardiovascular risk in acromegaly. Clin Endocrinol (Oxf). 2016. Epub 2016/12/03. doi: 10.1111/cen.13273 . [DOI] [PubMed] [Google Scholar]
- 39.Dandana A, Gammoudi I, Chalghoum A, Chahed H, Addad F, Ferchichi S, et al. Clinical utility of serum cystatin C in predicting coronary artery disease in patients without chronic kidney disease. J Clin Lab Anal. 2014;28(3):191–7. Epub 2014/01/31. doi: 10.1002/jcla.21665 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niccoli G, Conte M, Della Bona R, Altamura L, Siviglia M, Dato I, et al. Cystatin C is associated with an increased coronary atherosclerotic burden and a stable plaque phenotype in patients with ischemic heart disease and normal glomerular filtration rate. Atherosclerosis. 2008;198(2):373–80. Epub 2007/11/07. S0021-9150(07)00561-8 [pii] doi: 10.1016/j.atherosclerosis.2007.09.022 . [DOI] [PubMed] [Google Scholar]
- 41.Silva D, Cortez-Dias N, Jorge C, Marques JS, Carrilho-Ferreira P, Magalhaes A, et al. Cystatin C as prognostic biomarker in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2012;109(10):1431–8. Epub 2012/02/24. S0002-9149(12)00456-0 [pii] doi: 10.1016/j.amjcard.2012.01.356 . [DOI] [PubMed] [Google Scholar]
- 42.Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, et al. Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med. 2005;352(20):2049–60. Epub 2005/05/20. 352/20/2049 [pii] doi: 10.1056/NEJMoa043161 . [DOI] [PubMed] [Google Scholar]
- 43.Ristiniemi N, Lund J, Tertti R, Christensson A, Ilva T, Porela P, et al. Cystatin C as a predictor of all-cause mortality and myocardial infarction in patients with non-ST-elevation acute coronary syndrome. Clin Biochem. 2012;45(7–8):535–40. Epub 2012/03/08. S0009-9120(12)00089-6 [pii] doi: 10.1016/j.clinbiochem.2012.02.012 . [DOI] [PubMed] [Google Scholar]
- 44.Chapman HA, Riese RJ, Shi GP. Emerging roles for cysteine proteases in human biology. Annual review of physiology. 1997;59:63–88. Epub 1997/01/01. doi: 10.1146/annurev.physiol.59.1.63 . [DOI] [PubMed] [Google Scholar]
- 45.Lafarge JC, Naour N, Clement K, Guerre-Millo M. Cathepsins and cystatin C in atherosclerosis and obesity. Biochimie. 2010;92(11):1580–6. Epub 2010/04/27. S0300-9084(10)00149-5 [pii] doi: 10.1016/j.biochi.2010.04.011 . [DOI] [PubMed] [Google Scholar]
- 46.Singh D, Whooley MA, Ix JH, Ali S, Shlipak MG. Association of cystatin C and estimated GFR with inflammatory biomarkers: the Heart and Soul Study. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2007;22(4):1087–92. Epub 2007/01/11. doi: 10.1093/ndt/gfl744 ; PubMed Central PMCID: PMCPMC2770338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xie L, Terrand J, Xu B, Tsaprailis G, Boyer J, Chen QM. Cystatin C increases in cardiac injury: a role in extracellular matrix protein modulation. Cardiovascular research. 2010;87(4):628–35. Epub 2010/05/22. doi: 10.1093/cvr/cvq138 ; PubMed Central PMCID: PMCPMC2920813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.


