Abstract
To investigate whether receiving US Department of Housing and Urban Development (HUD) housing assistance is associated with improved access to health care, we analyzed data on nondisabled adults ages 18–64 who responded to the 2004–12 National Health Interview Survey that were linked with administrative data from HUD for the period 2002–14. To account for potential selection bias, we compared access to care between respondents who were receiving HUD housing assistance at the time of the survey interview (current recipients) and those who received HUD assistance within twenty-four months of completing the survey interview (future recipients). Receiving assistance was associated with lower uninsurance rates: 31.8 percent of current recipients were uninsured, compared to 37.2 percent of future recipients. Rates of unmet need for health care due to cost were similarly lower for current recipients than for future recipients. No effect of receiving assistance was observed on having a usual source of care. These findings provide evidence that supports the effectiveness of housing assistance in improving health care access.
Exposure to substandard or unstable housing has been linked to adverse health outcomes.1–3 Conditions in substandard housing have been associated with increased rates of infectious and chronic diseases, injuries, poor mental health, and poor nutrition.1 Unaffordable housing has also been linked to poor health.4 People receiving public housing assistance are often in poor health,5 with increased need for mental health care6 and low levels of physical activity,7 despite having improved housing stability8,9 and more affordable housing than people in the private housing market. Compared to similarly poor people not in public housing, those in public housing have increased rates of smoking, hypertension, and poor health status in general.5 Poor health among those receiving public housing assistance may be due to myriad factors, which could include neighborhood effects,1,10 environmental factors,11 crowding,12 and social networks that increase financial and emotional stress and provide few employment or educational opportunities.13
Studies have measured the health of people in public housing,5 but few studies have examined whether assistance programs that improve housing lead to improved health. Some evidence points to health improvements from such programs,9,14–16 often through improved living conditions.17,18 Positive changes in health behaviors have also been observed in some studies.19 Other studies have assessed social and economic outcomes of improvements in housing.8
Access to health care has been shown to improve health,20–22 and housing instability is correlated with poor access to health care.23,24 For people with unstable housing, the competing demands of obtaining housing limit their ability to access health care.23–25 Hence, providing stable housing may reduce competing demands and improve access to care. However, little research exists concerning the effects of housing assistance programs on access to health care. The few studies on this topic have focused on special populations, such as homeless and HIV-positive people,26–30 rather than the general population.
The US Department of Housing and Urban Development (HUD) administers three structurally distinct main categories of housing assistance programs. First, in Housing Choice Voucher programs, local public housing agencies directly provide landlords with rent payment subsidies on behalf of participants, allowing recipients to select privately owned housing that meets program requirements.31 Second, public housing provides housing to eligible low-income families. Dwellings owned by local public housing agencies can range from single-family houses to high-rise apartment buildings. Third, in Multifamily Housing Programs, housing options are limited to private properties whose owners participate in the program. Participating owners receive subsidies from HUD but are required to provide a percentage of their housing units to low-income people at below-market-value rates.31 HUD programs in each of the three program categories are described in the online Appendix.32
The HUD-funded Moving to Opportunity for Fair Housing study compared different types of housing assistance programs in terms of their impacts on health and health care access, but the study did not include a group of participants that did not receive any housing assistance.33 Therefore, the effect of receiving housing assistance compared with not receiving any housing assistance could not be assessed. Whether receiving housing assistance results in improved access to health care has not been established.
We examined whether receiving HUD housing assistance was associated with improved health care access among nondisabled adults. We also examined differences in the magnitude of these effects across the three categories of HUD housing assistance programs.
Study Data And Methods
DATA
This study used data for the period 2004–12 from the National Health Interview Survey (NHIS) linked to administrative data for the period 2002–14 from HUD. Conducted annually by the National Center for Health Statistics, the NHIS is a nationally representative, cross-sectional, multistage survey of a sample of the US civilian noninstitutionalized population. Details of the survey design have been presented elsewhere.34,35 More information about the use of the survey for this study is in the Appendix.32
The HUD administrative data were collected by local public housing agencies and private building owners. The information included program participants’ dates of enrollment and participation, basic demographic characteristics, and detailed income information.31 Further information on HUD data collection for different program types is in the Appendix.32
Respondents to the sample adult module in the NHIS (referred to as sample adults) were eligible for linkage to HUD data if they provided sufficient identifying information (such as full or partial Social Security number, month and year of birth, sex, and first and last name), did not refuse to answer a question about housing assistance, and did not specifically refuse to have their data linked.31 For detailed information about consent for data linkage, see the Appendix.32 A deterministic linkage of HUD administrative data to NHIS data was based on the identifying information described above; this process has been described in detail elsewhere.36 In the period 2004–12, 52.5 percent of the sample adults from the NHIS were eligible for linkage. We selected those years for our study period because changes in the HUD administrative systems improved the data quality in the early 2000s, and the 2012 NHIS data were the most recent linked data available at the time of our study.31
The creation of the NHIS-HUD linked files was approved by the Research Ethics Review Board of the National Center for Health Statistics. The center required no additional approval for this analysis of the data.
DEPENDENT VARIABLES
We selected measures available in the NHIS that reflect access to health care, including insurance status (insured or uninsured);22,37 having a usual source of care;22,37 and having delayed getting or not receiving needed medical care,21,37 mental health care,38 specialist care,39 dental care,21,37 or prescription drugs due to cost in the previous year.21,37 For brevity, we refer to having delayed getting or not receiving care in any of these areas as “unmet need due to cost.” More information about, and the questions used to provide information for, our dependent variables is in the Appendix.32
MAIN INDEPENDENT VARIABLES
Our primary independent variable was housing status at the time of the NHIS interview, as determined from HUD administrative data. We used administrative data for housing assistance because they allowed us to assess the timing of assistance relative to that of the survey interview, and because self-reports of having housing assistance have been shown to be unreliable.40 For each linkage-eligible NHIS respondent, information on the receipt of housing assistance was available from HUD administrative data at the time of the NHIS interview and for at least two years afterward. Initially, we considered all housing program categories together, as a single dichotomous variable, and we divided survey respondents into two categories according to their housing status: current recipients, or those receiving HUD housing assistance at the time of the NHIS interview, regardless of the type of assistance program; and future recipients, or those who were not receiving HUD housing assistance at the time of the interview but would receive it within the next twenty-four months. We limited our analysis to these two groups to minimize selection bias, as described below.
Further analyses examined each category of housing assistance program separately. For these analyses, we categorized survey respondents as current or future recipients of public housing, Housing Choice Vouchers, and Multifamily Housing Programs assistance. Nearly all HUD housing assistance in this study was rental, not ownership, assistance (for information on ownership assistance programs in the analytic sample, see the Appendix).32
COVARIATES
All covariates were from the NHIS, including survey year, respondent’s age at the time of the survey interview, sex, and race/ethnicity; highest level of education in the respondent’s household; census region; and family size and income as a percentage of the federal poverty level. We controlled for self-reported health status, number of chronic physical conditions,41 and serious psychological distress (as measured by scores of at least 13 on the Kessler-6 questionnaire).42 Exact categorizations of covariates are in the Appendix.32
EXCLUSIONS
We limited our analysis to sample adults ages 18–64 years at the NHIS interview because nearly all adults ages sixty-five and older are enrolled in Medicare, and insurance status was one of our primary outcomes.
Similarly, we excluded respondents who received Supplemental Security Income or Social Security Disability Insurance benefits because of disability within the same calendar year as the NHIS interview. Receipt of these disability benefits confers eligibility for either Medicaid or Medicare.43,44 Specific HUD program categories and public housing agencies may also give preference for HUD housing assistance to people with disabilities.31,45 Subsequently, receipt of these disability benefits is highly related to both insurance status and receiving HUD housing assistance (for the insurance status of respondents receiving Social Security Administration disability benefits, see Appendix Exhibit 2).32
ANALYSIS
The effects of participation in social welfare programs in general are difficult to assess because of unobserved differences between those who participate and those who do not.46,47 Specifically, previous research suggests that people who receive housing assistance may differ in unmeasured ways from eligible people who do not apply for assistance.19 Hence, a direct comparison of people receiving assistance and those without it (at similar income levels, for example) may be problematic.
To address this selection bias, we considered the timing of housing assistance relative to that of the NHIS interview by comparing people receiving assistance at the time of the interview to those who were not receiving assistance then but would within twenty-four months. This approach accounted for unmeasured differences between people who obtain HUD housing assistance and those who do not by comparing individuals receiving assistance to a control group. The control group—people who would receive assistance within twenty-four months—represents our best estimate of those on the waiting list for receiving assistance (for a further discussion of the choice of control group and why a true waiting list was not used, see the Appendix).32 We chose two years as the length of time to determine future assistance because the mean time on the waiting list before obtaining HUD-assisted housing is approximately two years.48
For each dependent variable, we used bivariate logistic regression to examine the associations between each outcome and housing status (current or future recipients of housing assistance). Adjusted (multivariable) models included program category and the covariates presented above. To explore potential differences by HUD program category, we added interaction terms between category and our main independent variable of housing status (current or future recipients), using both unadjusted and fully adjusted models. Predictive margins from the models were used to obtain unadjusted and adjusted percentages (and 95 percent confidence intervals) for all outcomes by housing status and HUD program category.
All analyses used adjusted weights created by the National Center for Health Statistics. Weights for the sample adult file were adjusted for the unequal probability of selection and non-response.49 These weights were further adjusted by the center to account for linkage ineligibility and to create estimates that are representative of the national population of subgroups of interest.31 All analyses adjusted for the complex sample design of the surveys, using the SVY suite of commands in Stata, version 12.1 SE. Multiply imputed data for family income were analyzed using the MI suite of commands.
SENSITIVITY AND ADDITIONAL ANALYSES
We examined whether a relationship between HUD housing assistance and unmet need due to cost might be mediated through insurance by adding insurance as a covariate to the regression for unmet need due to cost. We also examined whether HUD assistance affected uptake of public insurance and private insurance differently by comparing the percentages of adults with each insurance type in the current recipient and future recipient groups. We also considered the possibility of heterogeneity within the latter group, which could have meant that some members of the group might not have been similar to the members of the current recipient group. We used actual waiting-list data (limited to the Housing Choice Voucher and public housing programs) to assess the possibility that members of the future recipient group might have different characteristics from people actually on the list. These two groups were very similar. We also used the waiting list data to compare people on the list to those in the current recipient group. Details about and results of all sensitivity analyses are presented in the Appendix.32
MISSING DATA
Fewer than 0.5 percent of linkage-eligible adults were missing data for any primary outcome variable or covariate, except race/ethnicity and income. Race/ethnicity information was missing for 7.2 percent of adults, but these data were singly imputed by the National Center for Health Statistics using a two-stage, hot-deck imputation procedure,49 and imputations were used in all analyses. Family income was missing for 10.1 percent of the adults, but multiply imputed values from the center were used in all analyses. The final analytic sample consisted of 4,014 adults (an inclusion and exclusion flow chart is in Appendix Exhibit 1).32
LIMITATIONS
This study had limitations. First, only 52.5 percent of adults in the 2004–12 NHIS were linkage-eligible, which could have introduced selection bias into our analysis. However, linkage-eligibility adjusted weights were used to account for this concern.
Second, homeless people who might live in HUD-assisted housing in the near future were not sampled in the NHIS. But the inclusion of this disadvantaged population would likely have strengthened our results.
Third, ideally a true waiting list for HUD assistance, instead of an estimated list (our future assistance group), would have been used (for a further discussion of existing waiting list data and why an estimated list was used as the main analysis, see the Appendix).32 Similarly, using time periods other than twenty-four months to define the future assistance group might have provided better comparison groups.
Study Results
In the period 2004–12, 4.4 percent (95% CI: 3.8, 5.0) of adults ages 18–64 years were receiving HUD housing assistance at the time of their NHIS interview (data not shown). Another 1.1 percent (95% CI: 0.5, 1.7) would be receiving assistance within twenty-four months of their interview.
The sociodemographic and health characteristics of the current recipients of housing assistance and of the future recipients did not differ significantly, with a few exceptions (Exhibit 1). The distribution of HUD program categories differed between the two groups, with a higher percentage of current recipients than of future recipients participating in Housing Choice Voucher programs (53.6 percent versus 44.8 percent). Future recipients were more likely than current recipients to be ages 18–24. And current recipients were more likely than future recipients to live in families with income levels of less than 100 percent of the federal poverty level, and less likely to live in families with income levels of 200 percent or more of poverty. Sociodemographic and health characteristics by housing assistance program category are in Appendix Exhibit 3.32
EXHIBIT 1.
Characteristics of adults receiving HUD housing assistance
| Characteristic | Current recipients (n = 3,179) |
SE | Future recipients (n = 835) |
SE |
|---|---|---|---|---|
| Type of assistance** | ||||
| Public housing | 22.7% | 2.3 | 27.5% | 2.2 |
| Housing choice vouchers | 53.6 | 2.3 | 44.8 | 2.2 |
| Multifamily housing | 23.7 | 2.5 | 27.7 | 2.0 |
|
| ||||
| SOCIODEMOGRAPHIC CHARACTERISTICS | ||||
|
| ||||
| Age range (years)** | ||||
| 18–24 | 26.9 | 1.2 | 33.2 | 2.2 |
| 25–44 | 50.1 | 1.2 | 45.7 | 2.1 |
| 45–64 | 23.0 | 1.1 | 21.1 | 1.7 |
| Sex* | ||||
| Male | 23.0 | 1.1 | 27.1 | 2.0 |
| Female | 77.0 | 1.1 | 72.9 | 2.0 |
| Race/ethnicity* | ||||
| Non-Hispanic white | 28.5 | 1.9 | 34.3 | 2.3 |
| Non-Hispanic black | 45.8 | 1.9 | 42.9 | 2.2 |
| Non-Hispanic other and multiracial | 4.3 | 0.8 | 2.6 | 0.7 |
| Hispanic | 21.4 | 1.3 | 20.1 | 2.0 |
| Highest level of education in family | ||||
| Less than high school | 21.7 | 0.9 | 20.3 | 1.7 |
| High school or GED | 35.2 | 1.2 | 35.3 | 2.2 |
| More than high school | 43.1 | 1.2 | 44.1 | 2.4 |
| Family income (percent of FPL)*** | ||||
| Less than 50% | 34.3 | 1.2 | 24.4 | 1.7 |
| 50%–<100% | 31.7 | 1.2 | 24.3 | 1.7 |
| 100%–<200% | 25.3 | 1.1 | 28.9 | 1.9 |
| 200% or more | 8.5 | 0.7 | 23.3 | 2.1 |
| Family size* | ||||
| 1 | 14.4 | 0.8 | 14.7 | 1.2 |
| 2 | 22.0 | 1.0 | 20.5 | 1.6 |
| 3 | 25.2 | 1.0 | 21.2 | 1.7 |
| 4 or more | 38.4 | 1.3 | 43.5 | 2.3 |
| Census region* | ||||
| Northeast | 20.8 | 1.9 | 17.9 | 1.9 |
| Midwest | 26.2 | 2.4 | 26.7 | 2.1 |
| South | 36.6 | 2.2 | 42.0 | 2.4 |
| West | 16.4 | 1.8 | 13.4 | 1.7 |
|
| ||||
| HEALTH | ||||
|
| ||||
| Serious psychological distress | ||||
| Yes | 9.8 | 0.8 | 10.4 | 1.3 |
| No | 90.2 | 0.8 | 89.6 | 1.3 |
| Number of chronic physical conditions | ||||
| 0 | 51.9 | 1.2 | 54.6 | 2.2 |
| 1 | 26.3 | 1.0 | 22.5 | 1.7 |
| 2–3 | 17.6 | 1.0 | 19.0 | 1.7 |
| 4 or more | 4.3 | 0.6 | 3.9 | 0.7 |
| Health status | ||||
| Excellent or very good | 43.9 | 1.3 | 46.7 | 2.3 |
| Good | 33.5 | 1.1 | 31.5 | 2.1 |
| Fair or poor | 22.6 | 1.1 | 21.9 | 1.7 |
SOURCE Authors’ analysis of data for 2004–12 from the National Health Interview Survey linked with administrative data for 2002–14 from the US Department of Housing and Urban Development (HUD). NOTES “Current recipients” are those who received assistance at the time they responded to the survey. “Future recipients” are those who received assistance within twenty-four months of responding to the survey. Percentages may not sum to 100 because of rounding. Significance was measured using a chi-square test of the difference in distributions of each variable between current and future recipients of housing assistance. SE is standard error. GED is general educational development test. FPL is federal poverty level.
p < 0.10
p < 0.05
p < 0.01
OVERALL HUD HOUSING ASSISTANCE
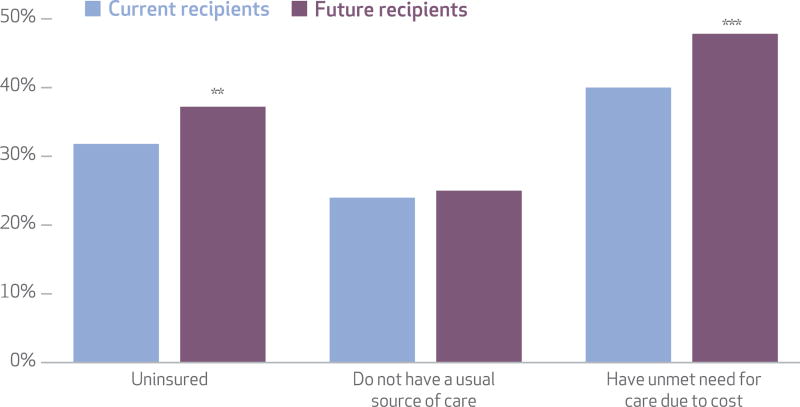
In adjusted analysis, we found that a smaller share of current recipients of HUD housing assistance were uninsured, compared to future recipients (31.8 percent versus 37.2 percent) (Exhibit 2). Unadjusted results were similar (Appendix Exhibit 4).32 The share of adults without a usual source of care was not significantly different between groups in either adjusted or unadjusted analysis. In the adjusted analysis, fewer current recipients than future recipients had unmet need due to cost (40.0 percent versus 47.8 percent) (Exhibit 2). Again, unadjusted results were similar (Appendix Exhibit 4).32
EXHIBIT 2. Adjusted percentages of adults receiving HUD housing assistance who are uninsured, who do not have a usual source of care, and who have unmet need for care due to cost.
SOURCE Authors analysis of data for 2004–12 from the National Health Interview Survey linked with administrative data for 2002–14 from the US Department of Housing and Urban Development (HUD). NOTES “Current” and “future” recipients are explained in the Notes to Exhibit 1. Percentages were adjusted for type of assistance (public housing, Housing Choice Vouchers, or Multifamily Housing), survey year, sociodemographic variables (age, sex, race/ethnicity, highest level of family education, family size, census region, and family income as a percentage of the federal poverty level), and health status variables (serious psychological distress, number of chronic physical conditions, and self-reported health status). **p < 0.05 ***p < 0.01
INDIVIDUAL PROGRAM CATEGORIES
The current and future recipient groups by program category did not generally differ significantly from one another in either unadjusted or adjusted analyses (Exhibit 3). The only exception was that adults currently in public housing were significantly less likely in adjusted analyses to have unmet need due to cost, compared to adults who would be in public housing in the near future (39.4 percent versus 50.2 percent). This pattern was similar in unadjusted analyses.
EXHIBIT 3.
Unadjusted and adjusted percentages of adults receiving HUD housing assistance who are uninsured, who do not have a usual source of care, and who have unmet need for care due to cost, by type of assistance
| Housing Choice Vouchers | Public housing | Multifamily Housing | ||||
|---|---|---|---|---|---|---|
| Current recipients (n = 1,633) |
Future recipients (n = 379) |
Current recipients (n = 761) |
Future recipients (n = 232) |
Current recipients (n = 785) |
Future recipients (n = 224) |
|
| PERCENTAGE UNINSURED | ||||||
|
| ||||||
| Unadjusted | 29.5% | 33.3% | 32.3% | 39.5% | 30.1% | 37.0% |
| Unadjusted differences | Ref | 3.8 | Ref | 7.2 | Ref | 6.9 |
| Adjusted | 29.6 | 34.0 | 33.1 | 38.6 | 29.5 | 35.9 |
| Adjusted differences | Ref | 4.5 | Ref | 5.6 | Ref | 6.5 |
|
| ||||||
| PERCENTAGE WITHOUT A USUAL SOURCE OF CARE | ||||||
|
| ||||||
| Unadjusted | 22.3% | 26.6% | 24.5% | 25.4% | 26.7% | 23.0% |
| Unadjusted differences | Ref | 4.3 | Ref | 1.8 | Ref | −3.8 |
| Adjusted | 22.7 | 26.4 | 25.5 | 26.0 | 25.5 | 22.3 |
| Adjusted differences | Ref | 3.6 | Ref | 0.6 | Ref | −3.2 |
|
| ||||||
| PERCENTAGE WITH UNMET NEED DUE TO COST | ||||||
|
| ||||||
| Unadjusted | 41.1% | 42.5% | 38.3% | 49.8%** | 41.0% | 48.5% |
| Unadjusted differences | Ref | 1.5 | Ref | 11.5** | Ref | 7.5 |
| Adjusted | 39.4 | 45.5* | 39.4 | 50.2** | 41.7 | 49.5* |
| Adjusted differences | Ref | 6.2* | Ref | 10.9** | Ref | 7.9* |
SOURCE Authors’ analysis of data for 2004–12 from the National Health Interview Survey linked with administrative data for 2002–14 from the US Department of Housing and Urban Development (HUD). NOTES “Current” and “future” recipients are explained in the Notes to Exhibit 1. Differences may not equal the percentage of current recipients subtracted from the percentage of future recipients because of rounding.
p < 0.10
p < 0.05
SENSITIVITY AND ADDITIONAL ANALYSES
We wondered whether the observed relationship between HUD housing assistance and unmet need due to cost might be mediated entirely by the reduction in uninsurance rates among people receiving assistance compared to those not receiving assistance. However, after we controlled for insurance status, we found that unmet need due to cost was still significantly lower among current recipients of assistance than among future recipients (40.4 percent versus 46.3 percent; p < 0.008), although the difference was slightly attenuated (data not shown).
We also examined whether the differences in insurance rates between current and future HUD assistance recipients would be consistent for public and for private insurance. In unadjusted analysis, we found that a higher percentage of current recipients of assistance had public insurance and a lower percentage of them had private insurance, compared to future recipients (for detailed results, see the Appendix).32
Discussion
Receiving HUD housing assistance was associated with a lower uninsurance rate and a lower rate of unmet need due to cost in both unadjusted and adjusted models. No effect of receiving assistance was observed on having a usual source of care. The sample size may have limited our ability to detect differences in the impact of individual program categories. However, the estimated differences for uninsurance and unmet need due to cost were consistently in the same direction across all program categories, which suggests that there were unlikely to be any categories with a directionally different effect.
Given our findings, future researchers might examine the downstream effects of housing assistance on other measures of access to and use of health care and of health, as well as the economic implications of each of those effects. Future housing policy and program evaluations, combined with findings from this study, could aid policy makers by providing evidence of the potential health-related impacts and cost-effectiveness of housing policies and programs. Such evidence is a critical component of HUD’s “health in all policies” approach.2
The competing demands theory states that people with limited economic resources place a higher priority on the basic needs of food and shelter than on access to health care.23–25 Consistent with this theory, some researchers have outlined specific pathways by which housing assistance might affect health care access. First, a “stability effect” could allow those with newly stable housing48 to focus on health care needs instead of housing.24,25 Second, housing assistance could have an “income effect,” as reduced housing costs free up financial resources to be spent on health care.19,31 A “gateway effect” may also exist, which would allow increased access to health care if subsidized housing is located close to social services such as public health clinics.19 In addition, some public housing programs conduct outreach to inform residents about public services. For instance, the Health Resources and Services Administration administers the Public Housing Primary Care Program, which provides grant funding to federally qualified health centers to provide public housing residents with improved access to primary health care services.50
Conclusion
This study provides evidence that receiving HUD housing assistance is associated with lower levels of both uninsurance and unmet need due to cost. Our study used nationally representative data, so its results are generalizable to the entire population ages 18–64 who receive HUD housing assistance but not Social Security disability benefits. Furthermore, by using a group of adults who will live in HUD-assisted housing in the near future as a comparison group, the study accounted for unobserved confounders related to obtaining HUD housing assistance. These findings provide data for policy makers to use in evaluating HUD housing assistance programs.
Supplementary Material
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official positions of the US Department of Health and Human Services, including the Office on Women’s Health and the Centers for Disease Control and Prevention (CDC), or of the US Department of Housing and Urban Development. Most of this research was conducted while Alan Simon was an employee of the Infant, Children, and Women’s Health Statistics Branch, Office of Analysis and Epidemiology, National Center for Health Statistics, CDC.
Contributor Information
Alan E. Simon, Office on Women’s Health in the US Department of Health and Human Services, in Washington, D.C..
Andrew Fenelon, Department of Health Services Administration, School of Public Health, at the University of Maryland, in College Park.
Veronica Helms, Office of Research, Evaluation, and Monitoring, Office of Policy Development and Research, in the US Department of Housing and Urban Development, in Washington, D.C..
Patricia C. Lloyd, Special Projects Branch, Office of Analysis and Epidemiology, at the National Center for Health Statistics, in Hyattsville, Maryland.
Lauren M. Rossen, Division of Vital Statistics at the National Center for Health Statistics.
NOTES
- 1.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–68. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bostic RW, Thornton RL, Rudd EC, Sternthal MJ. Health in all policies: the role of the US Department of Housing and Urban Development and present and future challenges. Health Aff (Millwood) 2012;31(9):2130–7. doi: 10.1377/hlthaff.2011.1014. [DOI] [PubMed] [Google Scholar]
- 3.Sharfstein J, Sandel M, Kahn R, Bauchner H. Is child health at risk while families wait for housing vouchers? Am J Public Health. 2001;91(8):1191–2. doi: 10.2105/ajph.91.8.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pollack CE, Griffin BA, Lynch J. Housing affordability and health among homeowners and renters. Am J Prev Med. 2010;39(6):515–21. doi: 10.1016/j.amepre.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Digenis-Bury EC, Brooks DR, Chen L, Ostrem M, Horsburgh CR. Use of a population-based survey to describe the health of Boston public housing residents. Am J Public Health. 2008;98(1):85–91. doi: 10.2105/AJPH.2006.094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Black BS, Rabins PV, German P, McGuire M, Roca R. Need and unmet need for mental health care among elderly public housing residents. Gerontologist. 1997;37(6):717–28. doi: 10.1093/geront/37.6.717. [DOI] [PubMed] [Google Scholar]
- 7.Lewis CE, Raczynski JM, Heath GW, Levinson R, Cutter GR. Physical activity of public housing residents in Birmingham, Alabama. Am J Public Health. 1993;83(7):1016–20. doi: 10.2105/ajph.83.7.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wood M, Turnham J, Mills G. Housing affordability and family well-being: results from the housing voucher evaluation. Hous Policy Debate. 2008;19(2):367–412. [Google Scholar]
- 9.Hayes MA, Zonneville M, Bassuk E. The SHIFT study: final report [Internet] Washington (DC): American Institutes for Research; [cited 2017 Mar 31]. Available from: http://www.air.org/sites/default/files/SHIFT_Service_and_Housing_Interventions_for_Families_in_Transition_final_report.pdf. [Google Scholar]
- 10.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–10. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann N Y Acad Sci. 2008;1136:276–88. doi: 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- 12.Coggon D, Barker DJ, Inskip H, Wield G. Housing in early life and later mortality. J Epidemiol Community Health. 1993;47(5):345–8. doi: 10.1136/jech.47.5.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Curley AM. Draining or gaining? The social networks of public housing movers in Boston. J Soc Pers Relat. 2009;26(2–3):227–47. [Google Scholar]
- 14.Thomson H, Petticrew M, Douglas M. Health impact assessment of housing improvements: incorporating research evidence. J Epidemiol Community Health. 2003;57(1):11–6. doi: 10.1136/jech.57.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown RT, Miao Y, Mitchell SL, Bharel M, Patel M, Ard KL, et al. Health outcomes of obtaining housing among older homeless adults. Am J Public Health. 2015;105(7):1482–8. doi: 10.2105/AJPH.2014.302539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breysse J, Dixon SL, Jacobs DE, Lopez J, Weber W. Self-reported health outcomes associated with green-renovated public housing among primarily elderly residents. J Public Health Manag Pract. 2015;21(4):355–67. doi: 10.1097/PHH.0000000000000199. [DOI] [PubMed] [Google Scholar]
- 17.Somerville M, Mackenzie I, Owen P, Miles D. Housing and health: does installing heating in their homes improve the health of children with asthma? Public Health. 2000;114(6):434–9. doi: 10.1038/sj.ph.1900687. [DOI] [PubMed] [Google Scholar]
- 18.Crocker DD, Kinyota S, Dumitru GG, Ligon CB, Herman EJ, Ferdinands JM, et al. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;41(2, Suppl 1):S5–32. doi: 10.1016/j.amepre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 19.Fertig AR, Reingold DA. Public housing, health and health behaviors: is there a connection? J Policy Anal Manage. 2007;26(4):831–59. doi: 10.1002/pam.20288. [DOI] [PubMed] [Google Scholar]
- 20.Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380(9845):917–23. doi: 10.1016/S0140-6736(12)61039-3. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Vital signs: core metrics for health care progress. Washington (DC): National Academies Press; 2015. [PubMed] [Google Scholar]
- 22.Access to health services [Internet] Washington (DC): US Department of Health and Human Services; [cited 2017 Mar 31]. HealthyPeople.gov. last updated 2017 Mar 30; Available from: http://www.healthypeople.gov/2020/topics-objectives/topic/Access-to-Health-Services. [Google Scholar]
- 23.Reid KW, Vittinghoff E, Kushel MB. Association between the level of housing instability, economic standing and health care access: a meta-regression. J Health Care Poor Underserved. 2008;19(4):1212–28. doi: 10.1353/hpu.0.0068. [DOI] [PubMed] [Google Scholar]
- 24.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–7. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–20. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conover CJ, Whetten-Goldstein K. The impact of ancillary services on primary care use and outcomes for HIV/AIDS patients with public insurance coverage. AIDS Care. 2002;14(Suppl 1):S59–71. doi: 10.1080/09540120220149957. [DOI] [PubMed] [Google Scholar]
- 27.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6, Suppl):85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- 28.Martinez TE, Burt MR. Impact of permanent supportive housing on the use of acute care health services by homeless adults. Psychiatr Serv. 2006;57(7):992–9. doi: 10.1176/ps.2006.57.7.992. [DOI] [PubMed] [Google Scholar]
- 29.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771–8. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 30.Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–57. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 31.Lloyd PC, Helms VE. NCHS-HUD linked data: analytic considerations and guidelines [Internet] Hyattsville (MD): National Center for Health Statistics; 2016. [cited 2017 Mar 31]. Available from: https://www.cdc.gov/nchs/data/datalinkage/nchs_hud_analytic_considerations.pdf. [Google Scholar]
- 32.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 33.Sanbonmatsu L, Ludwig J, Katz LF, Gennetian LA, Duncan GJ, Kessler RC, et al. Moving to Opportunity for Fair Housing Demonstration Program: final impacts evaluation [Internet] Washington (DC): US Department of Housing and Urban Development, Office of Policy Development and Research; 2011. Nov, [cited 2017 Mar 31]. National Bureau of Economic Research; Cambridge, MA. Available from: https://www.huduser.gov/publications/pdf/mtofhd_fullreport_v2.pdf. [Google Scholar]
- 34.Botman SL, Moore TF, Moriarity CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995–2004. [cited 2017 Mar 31];Vital and Health Statistics [serial on the Internet] 2000 Jun; Available from: https://www.cdc.gov/nchs/data/series/sr_02/sr02_130.pdf.
- 35.National Center for Health Statistics. 2014 National Health Interview Survey (NHIS) public use data release: survey description [Internet] Hyattsville (MD): NCHS; 2015. Jun, [cited 2017 Mar 31]. Available from: https://ftp.cdc.gov/pub/Health_Statistics/NCHs/Dataset_Documentation/NHIS/2014/srvydesc.pdf. [Google Scholar]
- 36.Lloyd P, Helms V, Golden C, Brittain J, Call E, Steffen B, et al. Linkage of 1999–2012 National Health Interview Survey (NHIS) and 1999–2012 National Health Examination Survey (NHANES) to administrative records from the US Department of Housing and Urban Development (HUD) Hyattsville (MD): National Center for Health Statistics; (Forthcoming) [PubMed] [Google Scholar]
- 37.Cohen RA, Bloom B. Access to and utilization of medical care for young adults ages 20–29 years, United States, 2008. NCHS Data Brief. 2010;(29):1–8. [PubMed] [Google Scholar]
- 38.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–55. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 39.Warfield ME, Gulley S. Unmet need and problems accessing specialty medical and related services among children with special health care needs. Matern Child Health J. 2006;10(2):201–16. doi: 10.1007/s10995-005-0041-3. [DOI] [PubMed] [Google Scholar]
- 40.Gordon EL, Chipungu S, Bagley LM, Zanakos SI. Improving housing subsidy surveys: data collection techniques for identifying the housing subsidy status of survey respondents [Internet] Washington (DC): US Department of Housing and Urban Development; 2005. Mar, [cited 2017 Mar 31]. ORC Macro, Calverton, MD. Available from: https://www.huduser.gov/Publications/pdf/datacollect.pdf. [Google Scholar]
- 41.Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10:E65. doi: 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10) Aust N Z J Public Health. 2001;25(6):494–7. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 43.Social Security Administration. Disability planner: Medicare coverage if you’re disabled [Internet] Baltimore (MD): The Administration; [cited 2017 Mar 31]. Available from: https://www.socialsecurity.gov/planners/disability/dapproval4.html. [Google Scholar]
- 44.Supplemental Security Income (SSI) Disability and Medicaid Coverage [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; [cited 2017 Mar 31]. HealthCare.gov. Available from: https://www.healthcare.gov/people-with-disabilities/ssi-and-medicaid/ [Google Scholar]
- 45.24 CFR 960.206(b)(3).
- 46.Long SK, Coughlin T, King J. How well does Medicaid work in improving access to care? Health Serv Res. 2005;40(1):39–58. doi: 10.1111/j.1475-6773.2005.00341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Björklund A, Moffitt R. The estimation of wage gains and welfare gains in self-selection models. Rev Econ Stat. 1987;69(1):42–9. [Google Scholar]
- 48.US Department of Housing and Urban Development. Assisted housing: national and local: picture of subsidized households [Internet] Washington (DC): HUD; [cited 2017 Mar 31]. Available from: https://www.huduser.gov/portal/datasets/picture/yearlydata.html. [Google Scholar]
- 49.National Center for Health Statistics. NHIS survey description [Internet] Hyattsville (MD): NCHS; 2013. Jun, [cited 2017 Mar 31]. 2012 National Health Interview Survey (NHIS) public use data release. Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2012/srvydesc.pdf. [Google Scholar]
- 50.Health Resources and Services Administration. HRSA Health Center Program: what is a health center? [Internet] Rockville (MD): HRSA; [cited 2017 Apr 26]. Available from: https://bphc.hrsa.gov/about/what-is-a-health-center/index.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.