Abstract
Background/Objective
Most older adults have multiple chronic conditions which lead to costly care that requires coordination across specialties. Yet many in the U.S. use a specialist physician rather than primary care as their predominant provider of ambulatory visits (PPC). As new physician payment models are designed under the Medicare and Chip Reauthorization Act (MACRA), information on whether specialists deliver care as efficiently as primary care to this high cost, high need population is needed. We test whether primary care versus specialty PPC is associated with better outcomes for older adults with multimorbidity.
Design
Observational study using propensity-score matching.
Setting
Fee-for-service Medicare, 2011–2012.
Participants
Beneficiaries over age 65 with multimorbidity.
Measurements
The independent variable was an indicator for having a specialty (versus primary) care PPC. Main outcomes were one-year mortality, hospitalization, and standardized expenditures, ambulatory visit patterns.
Results
In 3,934,942 beneficiaries with multimorbidity, two-thirds had a primary care provider as their PPC. Patients with a specialty PPC compared to primary care PPC had higher hospitalizations (40.3 more per 1,000) and higher spending ($1,781 more per beneficiary) but little meaningful difference in mortality (0.2% higher) or preventable hospitalizations. Spending differences stemmed from professional fees ($769 higher per beneficiary), inpatient stays ($572 higher per beneficiary) and outpatient facilities ($510 higher per beneficiary). All p-values <.001. In addition, people with a specialist versus primary care PPC had lower continuity of care and saw a greater number of providers.
Conclusions
Older adults with multimorbidity with a specialist as their main ambulatory care provider had higher spending and lower continuity of care but similar clinical outcomes as patients whose PPC was in primary care.
Keywords: Multimorbidity, Physician Specialty, Spending, Quality, Continuity
INTRODUCTION
New payment models, such accountable care organizations (ACOs) and patient-centered medical homes (PCMH), put a premium on people using primary care providers, as opposed to specialty care, as their longitudinal provider of care. In the United States, family practice and general internal medicine are commonly considered the primary care providers for adults, although other specialties have advocated for taking on that role.1–3 A recent Dartmouth Atlas report, however, shows that 43% of older fee-for-service Medicare beneficiaries see a specialty physician for the majority of their outpatient visits.4 Using a specialist as the predominant provider varied widely across the US, from 27–58% across hospital referral regions.4 In this context, shifting the organization of care toward primary care may be challenging in some areas of the country, which may limit diffusion of alternative payment models.
While the idea that primary care providers are better positioned to coordinate care and generate better outcomes at lower costs is appealing, the evidence suggesting that specialty matters in achieving those outcomes is controversial. A series of studies attempted to determine whether the quality of care delivered by primary care specialties is different from that delivered by specialists.5–11 Broadly summarized, there are some differences within specific domains, such as better disease-specific guideline adherence if treated by specialists but better global preventive care if treated by primary care. Yet, firm conclusions about quality remain elusive and the effect on spending has not been evaluated.5,7,12–15
One group of patients for whom use of primary care as the predominant provider may be particularly important is people with multimorbity, having more than one major chronic illness.16 Several disparate clinical specialties are involved in the care of people with multimorbidity, which creates the need to align competing disease management recommendations.17 Such patients are also high risk for preventable hospitalizations and are among the costliest to treat.18,19 The existing literature about physician care focuses on one disease at time and cannot address the additional complexity posed by multimorbid patients. 15
In this study, we test whether having a primary care provider versus all other specialies as the predominant provider of care was associated with better outcomes among older adults with multimorbidity. The predominant provider of care (PPC) is defined as the doctor or nurse practitioner the patient saw most for ambulatory visits. Our analysis does not consider which specialty the provider or patient believes holds this role, but instead the provider who likely has the most influence over care by virtue of having the most contact. We test whether having primary care PPC is associated with lower mortality, hospitalization, or spending compared to having a specialist as PPC. We also evaluate whether ambulatory care visit patterns and fragmentation differ based on specialty of PPC.
METHODS
Study population
We first identified Medicare beneficiaries who were age 65 or older on January 1, 2011, and had full Parts A and B coverage without any Medicare Advantage enrollment. We then used 2011 inpatient and outpatient claim records to identify whether they had each of 18 chronic conditions (see Appendix Table 1, ICD-9 Codes for Chronic Conditions). Conditions were identified by the presence of selected ICD-9 codes on two outpatient claims 7 days apart or one inpatient claim.
Participants were included in the study if they resided in the community (i.e. spent fewer than 100 days in a nursing home according to the Minimum Data Set20) and had two or more chronic conditions. We also required participants to be alive on January 1, 2012 with the same Medicare enrollment criteria while alive in 2012.
Predominant provider of care
We adapted methods from previous work to identify the PPC21 for each patient in 2011 as the provider seen most for ambulatory visits. We classified the specialty of PPC as primary care providers (family or internal medicine, geriatrics or nurse practitioner (NP)) versus all other specialties. For NPs, administrative data do not distinguish those who practice in a specialty versus primary care setting. We categorized them as primary care because 86.5% of NPs have primary care focus.22
Outcome Measures
Outcomes measured in 2012 included mortality, utilization of inpatient and outpatient services, and Medicare expenditures. Death was obtained from the Beneficiary Summary File. Hospitalizations were categorized as medical or surgical admissions based on Medicare Severity Diagnosis Related Groups. Ambulatory care sensitive condition (ACSC) hospitalizations, which represent conditions for which hospitalization might be avoided if the patient receives timely and adequate outpatient care, were identified using the Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQI).23 We used the overall composite (PQI 90), the acute composite (PQI 91), the chronic composite (PQI 92) and each PQI condition separately.
We standardized Medicare payments to adjust for differences in Medicare reimbursement24 and examined spending by category: total, inpatient (MedPAR), physician/supplier (Carrier), outpatient facility, home health, hospice, and durable medical equipment. We further report Medicare Part B payments by Berenson-Eggers Type of Service (BETOS) category.25
As a secondary analysis, we characterized the ambulatory care patterns including differences in number of total, primary care, and specialty care visits, number of different clinicians seen, percent of visits to the predominant provider (called usual provider of care in other studies26) and continuity of care (measured by the Bice-Boxerman continuity of care index which ranges from 0 to 1 from lowest to highest27). These ambulatory care measures were based on evaluation and management visits.
Covariates
From the 2011 Beneficiary Summary File, we obtained patients’ birthdate, sex, race/ethnicity, Medicare-Medicaid dual eligibility and ZIP Code of residence. We linked patients’ ZIP Code of residence to hospital referral region (HRR) and the 2010 Census Tract to obtain median household income.
Statistical Analysis
We first examined characteristics of the study population by specialty type of the predominant provider of care (PPC) using descriptive statistics. We applied propensity score matching methods to balance the differences in observable patient characteristics. Propensity scores are an approach used in non-randomized studies to get the comparison groups as similar as possible based on observable characteristics. We used a logistic regression model to estimate the probability (propensity score) that the PPC was a primary care provider versus specialist. Covariates in the baseline year were selected based upon their potential to predict specialty of PPC including patients’ age, sex, race, dual eligible status, median census tract income, 18 pre-existing chronic conditions, number of ambulatory visits, medical admissions, surgical admissions, and hospital referral region.
We then performed 1-to-1 nearest neighbor matching with replacement based on the propensity score. To test our approach and maximize number of matches, we repeated the matching process without the replacement option, using calipers, and using the logit of the propensity score, each of which impacted fewer than 100 cases of the matched sample. Outcome comparisons based on the propensity-score matched groups are valid only if the groups have similar distributions of measured baseline covariates. We tested balance by comparing baseline characteristics in the matched groups using the standardized difference. A value greater than 0.1 difference indicates potentially meaningful imbalance.28 Based on the matched sample, differences in average outcomes between primary care and specialist PPC were evaluated by t-statistics.
Analyses were conducted using SAS V9.3 (SAS Institute Inc., Cary, NC) or STATA v13.1 (Stata Corp, College Station, TX). The Dartmouth College Committee on the Protection of Human Subjects approved this study.
RESULTS
Among 25.7 million Medicare fee-for-service elderly beneficiaries in 2011, 22.3% had multimorbidity. After restricting to those with multimorbidity living in the community and eligible in 2012 as well, our final sample included 3,924,942 beneficiaries. Two-thirds of patients with multimorbidity had a primary care provider as their PPC (Table 1); 14% saw only primary care and 18% saw only specialties. Overall, without propensity score matching, patients with primary care PPC were older (77.3 vs. 76.1 years old), less likely to be male (43.8% vs. 51.3%), more likely to be dually eligible for Medicare and Medicaid (20.4% vs. 14.5%), more likely to have diabetes (56.9% vs. 49.3%) or dementia (25.0% vs. 16.5%), more likely to live in communities with lower incomes (average median household income $53,866 vs. $58,563) and had higher rates of medical and lower rates of surgical discharges in 2011 compared to patients of specialty PPC. All p-values for differences are < 0.01. The propensity-score matching successfully balanced the observable patient characteristics when comparing primary care PPC and specialty PPC groups in the baseline year (Table 1).
Table 1.
Characteristics of Older Adults in Medicare with Multimorbidity whose Predominant Provider of Care is Primary Care vs Other Specialties Before & After Propensity Matching (2011)
| Unmatched
|
Std Diff* | Matched
|
Std Diff | ||||
|---|---|---|---|---|---|---|---|
| Overall | Primary care | Other Specialty | Primary care | Other Specialty | |||
|
|
|
||||||
| N | 3,924,942 | 2,648,500 | 1,276,442 | ||||
| 67.5% | 32.5% | ||||||
| Age | |||||||
| Mean (%) | 76.9 | 77.3 | 76.1 | .162 | 77.3 | 77.2 | .000 |
| 65–69 | 20.1 | 19.1 | 22.4 | −.081 | 19.1 | 18.4 | .018 |
| 70–74 | 21.8 | 21.0 | 23.4 | −.060 | 21.0 | 21.0 | −.002 |
| 75–79 | 21.3 | 21.0 | 21.9 | −.022 | 21.0 | 21.7 | −.018 |
| 80–84 | 19.2 | 19.7 | 18.2 | .039 | 19.7 | 20.2 | −.014 |
| 85-Up | 17.7 | 19.3 | 14.2 | .139 | 19.3 | 18.7 | .017 |
| Male (%) | 46.3 | 43.8 | 51.3 | −.150 | 43.8 | 43.9 | −.001 |
| Race (%) | |||||||
| White | 82.0 | 81.6 | 82.9 | −.034 | 81.6 | 81.2 | .010 |
| Black | 9.3 | 9.4 | 8.9 | .018 | 9.4 | 9.6 | −.007 |
| Hispanic | 5.5 | 5.6 | 5.2 | .019 | 5.6 | 5.8 | −.006 |
| Other | 3.3 | 3.4 | 3.0 | .021 | 3.4 | 3.4 | −.003 |
| Dual-Eligible (%) | 18.5 | 20.4 | 14.5 | .156 | 20.4 | 20.7 | − −.008 |
| Median household income | $55,394 | $53,866 | $58,563 | −.180 | $53,866 | $53,793 | .002 |
| Number of chronic conditions (%) | |||||||
| 2 | 56.7 | 56.7 | 56.7 | −.001 | 56.7 | 55.5 | .023 |
| 3 | 24.1 | 24.0 | 24.4 | −.009 | 24.0 | 24.4 | −.010 |
| 4 | 11.1 | 11.2 | 11.1 | .003 | 11.2 | 11.4 | −.008 |
| ≥5 | 8.1 | 8.2 | 7.8 | .013 | 8.2 | 8.6 | −.016 |
| Selected Chronic Conditions (%) | |||||||
| Coronary artery disease | 18.1 | 17.2 | 20.1 | −.075 | 17.2 | 17.4 | −.007 |
| Congestive heart Failure | 34.9 | 34.9 | 35.0 | −.003 | 34.9 | 35.3 | −.010 |
| Diabetes Mellitus | 54.5 | 56.9 | 49.3 | .153 | 56.9 | 57.1 | −.004 |
| Dementia | 22.3 | 25.0 | 16.5 | .211 | 25.0 | 25.0 | .001 |
| HCC score | 2.0 | 1.9 | 2.1 | −.128 | 1.9 | 2.0 | −.034 |
| Baseline utilization | |||||||
| Number of Visits | 15.1 | 14.5 | 16.4 | −.191 | 14.5 | 14.6 | −.008 |
| Hospital Discharges (per 1,000) | |||||||
| Total | 833.4 | 842.1 | 815.5 | .023 | 842.1 | 862.6 | −.012 |
| Medical Discharges | 616.8 | 639.2 | 570.3 | .069 | 639.2 | 653.6 | −.010 |
| Surgical Discharges | 216.6 | 202.8 | 245.1 | −.085 | 202.8 | 209.0 | −.009 |
Std diff = Standardized Difference compares the difference in means (or proportions) in the units of the pooled standard deviations between treated and controls and is the recommended measure for comparing balance between propensity-matched groups. A value of greater than 0.1 suggests potentially meaningful lack of balance
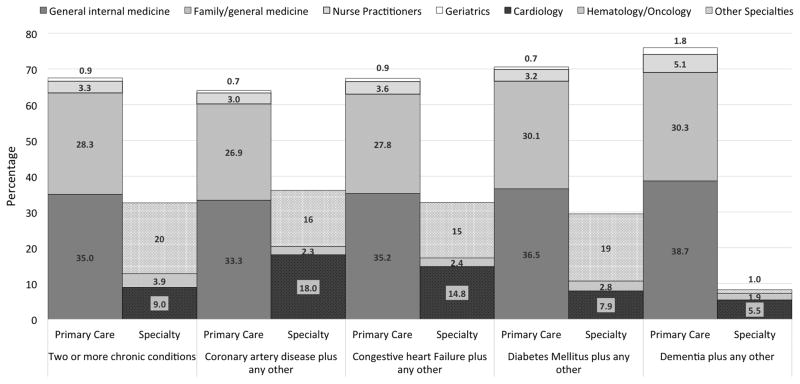
Figure 1 shows that the majority of patients with multimorbidity had one of two primary care specialties as their PPC: 35.0% had general internal medicine and 28.3% had family medicine. The specialists used most commonly as a PPC were cardiologists (9.0%), followed by hematologists/oncologists (3.9%) and a mix of other specialties each under 2% (20.0%). The specific conditions a person with multimorbidity had influenced use of a specialist as PPC. For example, cardiologists were the PPC for 18.0% of patients with coronary artery disease and 14.8% of patients with congestive heart failure, but were the PPC for only 7.9% of patient with diabetes and 5.5% of patients with dementia.
Figure 1.
Specialty of the Predominant Provider of Care for Older Medicare Beneficiaries with Multimorbidity, Overall and Stratified by Presence of Specific Conditions
Table 2 shows the difference in outcomes between primary care PPC and specialty PPC based on the matched samples. For each of the clinical outcomes, primary care is favored but the differences are quite small albeit statistically significant due to the large sample size. Compared to patients with a primary care PPC, patients with a specialty PPC had higher mortality (0.2% absolute p<.001, or 2% relative difference), higher hospitalizations (40.3 per 1,000 higher, p<.001) and ambulatory care sensitive admisions (7.8 per 1,000 higher, p<.001). The lack of a strong association with ACSC admissions is further shown by differences that are dependent on the specific type of ACSC. While the clinical differences are small, the spending differences are large with $1,781 higher (p<.001) per beneficiary total spending among people whose PPC was a specialist.
Table 2.
Quality & Cost Outcomes for Propensity-Matched Older Medicare Benefiaries with Multimorbidity whose Predominant Provider of Care is Primary Care vs. Other Specialty (2012)
| Specialty of Predominant Provider of Care
|
|||||
|---|---|---|---|---|---|
| Primary care | Other Specialty | Abs Diff | % Diff | p-value | |
|
|
|||||
| Mortality (%) | 10.2 | 10.4 | −0.2 | −2% | <.001 |
| Hospitalizations, per 1,000 | |||||
| Total discharges | 649.1 | 689.4 | −40.3 | −6% | <.001 |
| All medical discharges | 524.1 | 553.1 | −29.0 | −6% | <.001 |
| All surgical discharges | 125.0 | 136.3 | −11.3 | −9% | <.001 |
| Ambulatory Care Sensitive Admissions | |||||
| Composites | |||||
| PQI 90 Prevention Quality Overall Composite | 178.3 | 186.0 | −7.8 | −4% | <.001 |
| PQI 91 Prevention Quality Acute Composite | 62.1 | 59.6 | 2.5 | 4% | <.001 |
| PQI 92 Prevention Quality Chronic Composite | 116.2 | 126.4 | −10.3 | −9% | <.001 |
| Individual Components | |||||
| PQI 01 Diabetes Short-Term Complications | 1.1 | 1.3 | −0.2 | −20% | <.001 |
| PQI 02 Perforated Appendix | 0.4 | 0.3 | 0.1 | 14% | 0.097 |
| PQI 03 Diabetes Long-Term Complications | 8.3 | 9.7 | −1.4 | −17% | <.001 |
| PQI 05 COPD or Asthma | 43.4 | 44.5 | −1.1 | −3% | <.001 |
| PQI 07 Hypertension | 3.6 | 3.5 | 0.2 | 4% | 0.077 |
| PQI 08 Heart Failure | 57.1 | 64.5 | −7.4 | −13% | <.001 |
| PQI 10 Dehydration | 10.1 | 9.4 | 0.7 | 7% | <.001 |
| PQI 11 Bacterial Pneumonia | 31.6 | 30.7 | 0.9 | 3% | <.001 |
| PQI 12 Urinary Tract Infection | 20.4 | 19.5 | 0.9 | 4% | <.001 |
| PQI 13 Angina Without Procedure | 0.9 | 0.9 | 0.0 | −3% | 0.516 |
| PQI 14 Uncontrolled Diabetes | 1.0 | 1.0 | −0.1 | −5% | 0.280 |
| PQI 16 Lower-Extremity Amputation Diabetes | 1.4 | 1.8 | −0.4 | −30% | <.001 |
| Standardized price payment | |||||
| Total | $19,398 | $21,178 | −$1,781 | −9% | <.001 |
| Inpatient | $9,468 | $10,040 | −$572 | −6% | <.001 |
| Professional Fees (Carrier file) | $4,388 | $5,157 | −$769 | −18% | <.001 |
| Outpatient facility | $2,378 | $2,887 | −$510 | −21% | <.001 |
| Hospice | $710 | $626 | $85 | 12% | <.001 |
| Home Health | $1,795 | $1,747 | $47 | 3% | <.001 |
| Durable Medical Equipment | $659 | $720 | −$62 | −9% | <.001 |
| Standardized Part B payment by BETOS Type | |||||
| E/M visits | $1,752 | $1,885 | −$133 | −8% | <.001 |
| Procedures | $1,063 | $1,241 | −$177 | −17% | <.001 |
| Tests | $428 | $492 | −$64 | −15% | <.001 |
| Imaging | $386 | $435 | −$49 | −13% | <.001 |
| Durable Medical Equipment | $5 | $6 | −$1 | −21% | <.001 |
| Other | $748 | $1,112 | −$364 | −49% | <.001 |
The lower spending of primary care PPC patients stemmed from professional fee payments ($769 less per beneficiary, p<.001), hospitals ($572 less per beneficiary, p<.001) and outpatient facilities ($510 less per beneficiary, p<.001). On the other hand, patients with primary care PPCs spent more on services devoted to late stage disease or disability: hospice ($85 more per beneficiary, p<.001) and home health ($47 more per beneficiary, p<.001). The difference in professional fees was driven largely by visits, procedures, and the miscellaneous category of “other” that includes services such as ambulance transfers, vision and hearing care, chemotherapy or other drugs, and chiropractic care.
We examined further how visit patterns differed between people with a primary care versus specialty care PPC. While having only slightly higher number of total ambulatory visits, people with a specialist as their PPC had lower continuity of care measured both by the continuity of care index (24% lower, p<.001) and the percentage of visits delivered by the patient’s PPC (48.3% vs 55.7%, p<.001), and they saw a greater number of unique providers (5.1 vs 4.6, p<.001).
Sensitivity analysis
We tested the sensitivity of results to patients changing specialty of PPC between 2011 and 2012. Of the 24.5% of patients for whom this occurred, 12.9% changed from primary care to specialty and 11.7% changed from specialty to primary care. The number that switched into primary care and into specialty were about equal and these two groups had complementary characteristics such that the distribution of sociodemographic and illness characteristics do not change between the baseline and outcome year. People who switched to or from a specialist PPC were younger, more likely to have surgical admissions, more likely to live in wealthier ZIP codes, more likely to be white, were less likely to be dual-eligible, and had slightly higher HCC than those who did not switch (Appendix Table 2, Comparison of Characteristics when Switched PPC). When we excluded people who switched, the association between specialty of PPC and spending was similar to the main results but the slight differences in mortality and hospitalizations now favored specialists PPC over primary care (Appendix Table 3, Outcomes Excluding Beneficiaries who Switched PPC). The magnitude of the mortality difference was small, as in the main analyses, which we interpret in both the analyses as having limited, if any, clinical importance.
Discussion
Among older adults who have multiple chronic conditions, having a specialists as the predominant provider of care is common (32% of people). Using a primary care provider as the clinician seen most in the ambulatory setting had similar clinical outcomes as measured by potentially preventable hospitalizations and mortality, with a slightly favorable difference of 0.2% compared with the baseline mortality of about 10%. Medicare expenditures, however, were higher when the predominant provider of care was a specialist, due largely to use of visits, tests and imaging but also due to higher risk of hospitalization. If the $1800 spending difference were applied to all 4 million Medicare fee-for-service beneficiaries in the community with multiple conditions, it would translate into $7 billion.
Limitations of Interpretation
The biggest challenge to interpreting our findings is the potential for selection bias based on how and why patients may choose (or be referred) to see primary care or specialists. We used propensity score matching techniques to address any differences on observable characteristics. The balance in observable factors was excellent, achieved partly because the groups were similar even before the match. The limitation of this approach, however, is that there may be unmeasured factors, such as severity of illness or functional impairment, and local unmeasured factors, such as availability of specialities, that influence who a patient sees. We addressed the second concern by including hospital referral region of residence in the propensity model to account for differences in access and norms around use of specialty services that are difficult to measure directly.34 In Medicare claims, we are unable to measure disease severity or presence of functional impairment so there is the potential for residual confounding, that is, one group could have higher unmeasured illness burden. But the near identical number of chronic conditions and similar HCC scores even before applying matching suggests that any residual confounding is not likely to be large.
Another factor that could influence the results is the use of a prospective design which was necessary to overcome endogeneity of results. Patients could change from predominantly seeing a primary care provider to a specialist from year one to two. This is most likely to occur when a person has had a new, serious diagnosis such as an acute myocardial infarction or cancer during the period. The sensitivity analysis excluding people who switch predominant provider specialty is likely more subject to selection bias than the main study, but, the results of this sensitivity analysis were largely consistent with the main results. While the results on mortality and total hospitalizations changed sign such that specialty care was now favored, the magnitude was small, as in our baseline analysis, which we interpret as showing little, if any, clinical importance in both analyses.
Interpretation in Context of Prior Research
In terms of clinical outcomes, prior studies suggest that specialty has mixed results on disease-specific quality measures29 and we find that on clinical outcomes of mortality and ACSC hospitalization there appears to be little difference between having primary care versus a specialist at the predominant provider. Prior studies, however, have not assessed spending. Our findings suggest that while clinical outcomes are not substantially dfferent, spending is 9% lower when primary care providers act as the predominant provider of ambulatory care. Primary care providers are achieving similar clinical outcomes with fewer resource inputs, or said another way, appear to be more efficient in the use of resources and hence may provide better value. The magnitude of these savings is greater than many reforms designed to achieve savings in Medicare.30,31
Positioning primary care as the central provider for people with multimorbidity has intuitive strength as a solution to better coordination. In fact, we find that in usual fee-for-service practice as it occurs across the U.S., continuity of care is higher and number of unique physicians involved in care is lower when primary care is the predominant provider, but those visit patterns do not directly equate with providing better care coordination. It remains possible that a provider who is seen less frequently may be providing a coordinating role through asynchronous care (such as phone calls and email). Our inability to observe these behaviors and inability to know how a patient views each provider is why we chose to use the new term of “predominant provider” which highlights opportunity for influence through visits rather than assuming that any given provider, regardless of specialty, is taking on the primary role of coordination.
Implications for Clinical Care and Policy
The implications of these results for people seeking care are important to consider. People with a higher burden of chronic disease may be using specialists as their main source of care 4,32: the question is whether the specialist themselves recognize that they are in that role. Survey evidence shows that specialists are less likely to self-identify as the primary provider of care than they did in years past.32 Specialist may find themselves managing conditions far from their area of expertise and needing to connect with disciplines that are not central to their usual practice, such as home health services, behavioral health care and social services. Importantly, there may be a trade-off between the expertise of primary care in coordinating care and the expertise of specialists in disease-specific management, although our study does not find a difference in mortality.
The spending differences when primary care versus specialists are the predominant provider also have implications for initiatives such as ACOs and PCMH that are based on primary care specialties being in a central role. This study suggests that major clinical outcomes like mortality and hospitalization may not be improved by reorienting local care systems around primary care, but spending may be lower. Many initiatives focus on disease management to reduce hospitalizations and readmissions. Yet our findings suggest additional value may be gained by focusing on the efficiency of ambulatory care delivery itself.
The high frequency of specialists as the PPC also has implications for efforts to increase participation in Alternative Payment Methods under the Medicare and Chip Reauthorization Act (MACRA).33 Under MACRA, physician incentives are designed to encourage participation in Alternative Payment Models which currently include ACOs and Comprehensive Primary Care models, both of which place high value on primary care. Yet specialty of the predominant provider of care varies strongly across hospital referral regions as shown in The Dartmouth Atlas – there are some regions in Louisana, Texas, and Florida where the majority of older adults see a specialist as their predominant care provider.4 The proportion of older adults with multimorbidity who see a specialist as their PPC varies from 21–57% across hospital referral regions.4 New payment incentives that encourage organization around primary care may face steeper challenges to dissemination in regions where specialists play a more dominant role.
In summary, one third of older adults with multimorbidity use specialty physicians as their predominant provider of care. Clinical outcomes of mortality and ACSC admissions are similar, but these patients tend to use more resources to achieve these results at higher cost. This study suggests that expansion of new models of care that encourage concentration of visits in primary care may not be associated with better clinical outcomes but may achieve cost savings among elders with multimorbidity.
Supplementary Material
Supplementary Table S1: Definition of Chronic Conditions Based on Hierarchical Condition Categories (HCC) developed by the Centers of Medicare & Medicaid Services. Categories chosen for chronic nature, association with mortality and costs, and prevalence greater than 2%.
Supplementary Table S2: Characteristics of Older Adults in Medicare with Multimorbidity whose Predominant Provider of Care is Primary Care versus Other Specialties Before and After Propensity Matching excluding those who Changed Specialty of PPC between Years 1 & 2 (2011)
Supplementary Table S3: Quality & Cost Outcomes for Propensity-Matched Older Medicare Beneficiaries with Multimorbidity whose Predominant Provider of Care is Primary Care vs. Other Specialty excluding those who changed Specialty of PPC between Year 1 and 2 (2012)
Table 3.
Patterns of Ambulatory Visits when Primary Care vs Specialty Care is the predominant provider of care (PPC).
| Specialty of Predominant Provider of Care
|
|||||
|---|---|---|---|---|---|
| Primary care | Other Specialty | p-value | |||
|
|
|||||
| Ambulatory care visits per person | 13.1 | 13.5 | <.001 | ||
| Number Visits to Primary Care | 7.3 | 4.4 | <.001 | ||
| Number Visits to Specialists | 5.3 | 8.7 | <.001 | ||
| Number of unique doctors seen | 4.6 | 5.1 | <.001 | ||
| Continuity of care score | 0.37 | 0.28 | <.001 | ||
| Percent of visits to PPC | 55.7% | 48.3% | <.001 | ||
| Percentage of Visits to Specialty Care | 37.5% | 65.0% | <.001 | ||
Acknowledgments
Funding: This study was funded by The John A. Hartford Foundation and NIA P01 AG19783.
This study was funded by The John A. Hartford Foundation and NIA P01 AG19783. The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. No authors had any potential conflicts of interest, including financial interests, activities, relationships, and affiliations. Drs. Bynum and Meara were responisible for study concept and acquisition of data, and all authors were involved in the design, analysis and interpretation of data, and preparation of the manuscript.
Footnotes
Presentation: This study was presented at the American Geriatrics Society Meeting 2015
References
- 1.Scholle SH, Chang J, Harman J, McNeil M. Characteristics of patients seen and services provided in primary care visits in obstetrics/gynecology: Data from NAMCS and NHAMCS. American Journal of Obstetrics and Gynecology. 2004;190(4):1119–1127. doi: 10.1016/j.ajog.2003.09.059. [DOI] [PubMed] [Google Scholar]
- 2.Kirschner N, Barr MS. Specialists/subspecialists and the patient-centered medical home. 1372010:200–204. doi: 10.1378/chest.09-0060. [DOI] [PubMed] [Google Scholar]
- 3.Casalino LP, Rittenhouse DR, Gillies RR, Shortell SM. Specialist physician practices as patient-centered medical homes. The New England journal of medicine. 2010;362(17):1555–1558. doi: 10.1056/NEJMp1001232. [DOI] [PubMed] [Google Scholar]
- 4.Bynum JPW, Meara ER, Chang CH, Rhoads JM, Bronner KK. Our Parents Ourselves: Health Care for an Aging Population. Lebanon, NH: The Dartmouth Institute for Health Policy and Clinical Practice; 2016. p. 57. [PubMed] [Google Scholar]
- 5.Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and specialties. Results from the medical outcomes study. JAMA. 1995;274(18):1436–1444. [PubMed] [Google Scholar]
- 6.Franks P, Fiscella K. Primary care physicians and specialists as personal physicians - Health care expenditures and mortality experience. J Fam Pract. 1998;47(2):105–109. [PubMed] [Google Scholar]
- 7.Chen J, Radford MJ, Wang Y, Krumholz HM. Care and outcomes of elderly patients with acute myocardial infarction by physician specialty: the effects of comorbidity and functional limitations. American Journal of Medicine. 2000;108(6):460–469. doi: 10.1016/s0002-9343(00)00331-4. [DOI] [PubMed] [Google Scholar]
- 8.De Berardis G, Pellegrini F, Franciosi M, et al. Quality of care and outcomes in type 2 diabetic patients: a comparison between general practice and diabetes clinics. Diabetes Care. 2004;27(2):398–406. doi: 10.2337/diacare.27.2.398. [DOI] [PubMed] [Google Scholar]
- 9.Pellegrini F, Belfiglio M, De Berardis G, et al. Role of organizational factors in poor blood pressure control in patients with type 2 diabetes: the QuED Study Group--quality of care and outcomes in type 2 diabetes. Arch Intern Med. 2003;163(4):473–480. doi: 10.1001/archinte.163.4.473. [DOI] [PubMed] [Google Scholar]
- 10.Lewis BG, Halm EA, Marcus SM, et al. Preventive services use among women seen by gynecologists, general medical physicians, or both. Obstet Gynecol. 2008;111(4):945–952. doi: 10.1097/AOG.0b013e318169ce3e. [DOI] [PubMed] [Google Scholar]
- 11.Ayanian JZ, Landrum MB, Guadagnoli E, Gaccione P. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. N Engl J Med. 2002;347(21):1678–1686. doi: 10.1056/NEJMsa020080. [DOI] [PubMed] [Google Scholar]
- 12.Greenfield S. Dividing up the turf. Generalists versus specialists. Journal of General Internal Medicine. 1996;11(4):245–246. doi: 10.1007/BF02642484. [DOI] [PubMed] [Google Scholar]
- 13.Greenfield S, Kaplan SH, Kahn R, Ninomiya J, Griffith JL. Profiling care provided by different groups of physicians: effects of patient case-mix (bias) and physician-level clustering on quality assessment results. Annals of Internal Medicine. 2002;136(2):111–121. doi: 10.7326/0003-4819-136-2-200201150-00008. [DOI] [PubMed] [Google Scholar]
- 14.Kravitz RL, Greenfield S, Rogers W, et al. Differences in the mix of patients among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992;267(12):1617–1623. [PubMed] [Google Scholar]
- 15.Smetana G, Landon B, Bindman AB, et al. A comparison of outcomes resulting from generalist vs specialist care for a single discrete medical condition: A systematic review and methodologic critique. Arch Intern Med. 2007;167(1):10–20. doi: 10.1001/archinte.167.1.10. [DOI] [PubMed] [Google Scholar]
- 16.Starfield B, Lemke KW, Herbert R, Pavlovich WD, Anderson G. Comorbidity and the use of primary care and specialist care in the elderly. Annals of Family Medicine. 2005;3(3):215–222. doi: 10.1370/afm.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical Practice Guidelines and Quality of Care for Older Patients With Multiple Comorbid Diseases: Implications for Pay for Performance. JAMA. 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 18.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 19.Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for High-Need, High-Cost Patients — An Urgent Priority. New England Journal of Medicine. 2016;375(10):909–911. doi: 10.1056/NEJMp1608511. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Medicare and Medicaid Services. [Accessed July 28, 2016];Long Term Care Minimum Data Set (MDS) https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/IdentifiableDataFiles/LongTermCareMinimumDataSetMDS.html.
- 21.Bynum JPW, Bernal-Delgado E, Gottlieb D, Fisher E. Assigning Ambulatory Patients and Their Physicians to Hospitals: A Method for Obtaining Population-Based Provider Performance Measurements. Health Services Research. 2007;42(1):45–62. doi: 10.1111/j.1475-6773.2006.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Association of Nurse Practitioners. [Accessed July 28, 2016];NP Fact Sheet. 2016 https://www.aanp.org/all-about-nps/np-fact-sheet.
- 23.Agency for Healthcare Research and Quality. [Accessed July 28, 2016];Prevention Quality Indicators. http://www.qualityindicators.ahrq.gov/modules/pqi_resources.aspx.
- 24.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices Don’t Drive Regional Medicare Spending Variations. Health Aff. 29(3):537–543. doi: 10.1377/hlthaff.2009.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Medicare and Medicaid Services. [Accessed March 9, 2009];Berenson-Eggers Type of Services. http://www.cms.hhs.gov/hcpcsreleasecodesets/20_betos.asp.
- 26.Jee SH, Cabana MD. Indices for continuity of care: A systematic review of the literature. Med Care Res Rev. 2006;63(2):158–188. doi: 10.1177/1077558705285294. [DOI] [PubMed] [Google Scholar]
- 27.Nyweide DJ, Anthony DL, Bynum JP, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879–1885. doi: 10.1001/jamainternmed.2013.10059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in Medicine. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harrold LR, Field TS, Gurwitz JH. Knowledge, Patterns of Care, and Outcomes of Care for Generalists and Specialists. Journal of General Internal Medicine. 1999;14(8):499–511. doi: 10.1046/j.1525-1497.1999.08168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early Performance of Accountable Care Organizations in Medicare. N Engl J Med. 2016;374(24):2357–2366. doi: 10.1056/NEJMsa1600142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Colla CH, Lewis VA, Kao LS, O’Malley AJ, Chang CH, Fisher ES. Association Between Medicare Accountable Care Organization Implementation and Spending Among Clinically Vulnerable Beneficiaries. JAMA Intern Med. 2016;176(8):1167–1175. doi: 10.1001/jamainternmed.2016.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Edwards ST, Mafi JN, Landon BE. Trends and quality of care in outpatient visits to generalist and specialist physicians delivering primary care in the United States, 1997–2010. Journal of General Internal Medicine. 2014;29(6):947–955. doi: 10.1007/s11606-014-2808-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for medicare and Medicaid Services. [Accessed July 28, 2016];Quality Payment Program: Delivery System Reform, Medicare Payment Reform, & MACRA. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html.
- 34.Yasaitis LC, Bynum JP, Skinner JS. Association between physician supply, local practice norms, and outpatient visit rates. Med Care. 2013;51(6):524–531. doi: 10.1097/MLR.0b013e3182928f67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Definition of Chronic Conditions Based on Hierarchical Condition Categories (HCC) developed by the Centers of Medicare & Medicaid Services. Categories chosen for chronic nature, association with mortality and costs, and prevalence greater than 2%.
Supplementary Table S2: Characteristics of Older Adults in Medicare with Multimorbidity whose Predominant Provider of Care is Primary Care versus Other Specialties Before and After Propensity Matching excluding those who Changed Specialty of PPC between Years 1 & 2 (2011)
Supplementary Table S3: Quality & Cost Outcomes for Propensity-Matched Older Medicare Beneficiaries with Multimorbidity whose Predominant Provider of Care is Primary Care vs. Other Specialty excluding those who changed Specialty of PPC between Year 1 and 2 (2012)