Abstract
Background/Objectives
Older adults with obesity are a high-need and growing segment of the population of the United States but little is known about disparities in caregiving. We assess the difference in activities of daily living (ADL) assistance for obese compared to normal weight older adults.
Design/Setting
Retrospective cohort study using the National Health & Aging Trends Study, 2011–2015.
Participants
10,168 observations of 5,612 adults aged ≥65 years old in the United States with disability in ADLs and body mass index (BMI) ≥18.5 kg/m2.
Measurements
BMI was classified as normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), or obese (≥30 kg/m2). Primary outcome was self-reported receipt of help for specific ADL disabilities. Models were adjusted for demographics (age, sex, race), degree of need (self-reported general health, severity of disability), household resources (income, marriage, people in household, number of children), and cognitive status (dementia, proxy respondent).
Results
Obese vs. normal weight older adults with disabilities had lower rates of assistance for walking inside (OR 0.63, 95% CI 0.50–0.81), walking outside (OR 0.76, 95% CI 0.59–0.97), toileting (OR 0.68, 95% CI 0.52–0.89), and getting in/out of bed (OR 0.67, 95% CI 0.50–0.87) after adjustment for respondent demographics. Associations were partially explained by level of need and cognitive status. In fully adjusted models, older adults with obesity still had significantly lower odds of assistance in getting in and out of bed than normal weight adults (OR 0.69, 95% CI 0.49–0.98).
Conclusion
Older adults with obesity are less likely to receive assistance for ADL disabilities than their normal weight counterparts—an important issue due to ongoing demographic changes in the United States.
Keywords: Obesity, caregiving, disability, aging
Background
In the coming decades, there are concerning medical, societal, and economic implications in the increasing prevalence and absolute number of older adults with obesity. From 2000 to 2014, the prevalence of obesity in adults aged 60 and over in the United States rose from 30.5% to 37.7%.1 At the same time, the projected growth in numbers of older adults in the United States, from 46 million in 2014 to 74 million in 2030, suggests that the number of older adults with obesity will continue to grow significantly.2 The costs of healthcare and caregiving for disabled older adults with obesity in the baby boomer generation is estimated at 68 billion dollars for long term care alone.3 One of the many challenges of these changing demographics is that older adults with obesity have higher rates of disability than normal weight counterparts and the prevalence of disability in this population is increasing over time.4–7 Yet, little is known about the particular barriers to caregiving and assistance for disabilities faced by older adults with obesity and disability.
It is well known that obesity challenges caregivers by increasing the difficulty of providing assistance with mobility, skin care, and personal hygiene for people with deficits in activities of daily living.8 In the inpatient setting, morbidly obese patients require a mean of 4.5 individuals to assist them with walking as opposed to 1.9 individuals for non-obese adults.9 Similar work has demonstrated higher personnel needs for care of obese adults in nursing homes.10–13 Obesity has been linked to high rates of musculoskeletal injuries in nurses and nursing assistants;14 these rates are already only surpassed by those of firefighters, psychiatric aides, and waste collectors in the United States.15
The absence of appropriate levels of assistance is a possible explanation for the association between obesity and lower quality of care at home for disabled adults. People with obesity are more likely to be admitted to a nursing home16–19 and more likely to fall.20 It is unclear if people with obesity in all care settings receive the same amount of assistance for deficits in activities of daily living as normal weight older adults. A single study demonstrated that obese adults of all ages with disability had lower rates of paid help than non-obese adults but this association was explained by differences in the younger age of disabled obese people and the analyses did not examine individual types of disability deficits.21
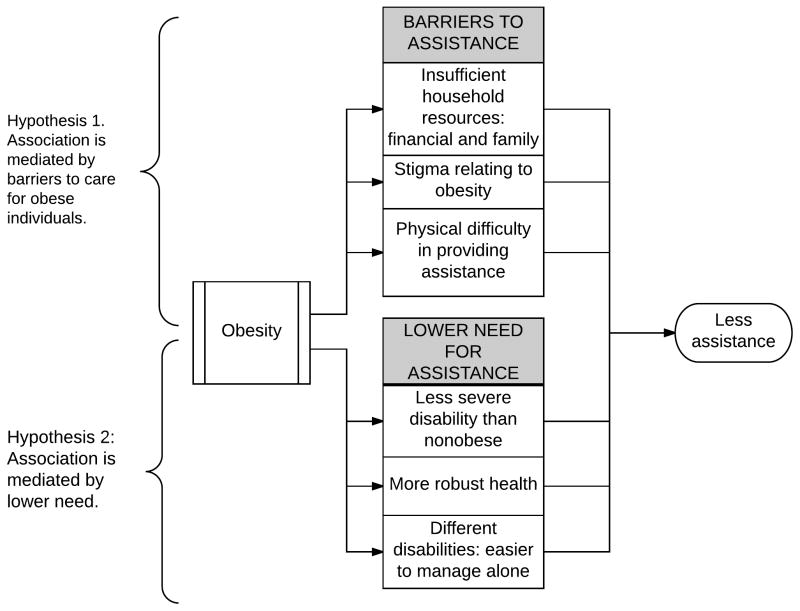
We hypothesized that there may be several potential pathways leading older adults with obesity to receive less assistance with disabled activities of daily living (ADLs) such as bathing, dressing, walking, and toileting than normal weight adults (Figure 1). First, they may have barriers to receiving the assistance they need. Obese, disabled individuals, who are generally younger than normal weight disabled individuals, may have fewer nonworking family members and may be less likely to ask for assistance. The difficulty of providing assistance, especially with physically demanding caregiving such as mobility or personal care, may lead to less available, qualified, capable caregiving than a similar normal weight individual.22 The presence of personal factors like poverty23 or the absence of factors like dementia24 may make accessing assistance more difficult or less preferred. Stigma surrounding obesity may serve as a barrier to requesting assistance and potential caregivers may have a bias against helping obese adults needing assistance because they are seen as less frail and more capable to do self-care.22
Figure 1.
Hypotheses for association between obesity and lower rates of assistance.
Alternatively, older disabled adults with obesity may have lower needs for assistance compared to normal weight counterparts. The nature (either the type or the severity) of the disabilities experienced by obese people may allow them to better compensate and so require less assistance. Given the younger age of onset of disability for obese adults, they may be physically healthier with less comorbid neurologic disease allowing them to manage mild disability with more independence.7 We therefore aim to both assess the differences in receipt of assistance for impaired ADLs between normal weight and older adults with obesity and explore the mediating pathways leading to this disparity in assistance for older, disabled, obese adults.
Methods
Data
We used survey data from the annual survey waves of the National Health and Aging Trends Study (NHATS), a nationally representative study of Americans age 65 and older, from 2011 to 2015.25 NHATs relies on the Medicare enrollment database as its sampling frame, and in 2011 enrolled 8,245 adults, achieving response rates ranging from 71% in 2011 to 90% in 2014.26 NHATs conducts annual in-person surveys with proxy reporters if the participant is unable to respond. The cohort was refreshed in 2015 in order to maintain representativeness. All NHATs data used was de-identified and all respondents provided informed consent under procedures approved by the Johns Hopkins Institutional Review Board.
Cohort
We included any observation where the respondent reported any difficulty, despite accommodations (such as using devices like walkers and grab bars) in performing ADLS, which include dressing, eating, bathing, toileting, walking inside, walking outside or getting in or out of bed. We excluded observations missing covariate data. We additionally excluded those with underweight body mass index (BMI), classified as <18.5 kg/m2, due to the potential reverse confounding as this population has higher levels of underlying illness and mortality risk.27
Measures
NHATS assesses several measures of performance of ADLS to consider a spectrum of disability and participation restriction.28 Our primary dependent variable was participants’ reported receipt of assistance for an ADL that they have any level of difficulty performing, for example the rate of reporting assistance with bathing for all those who reported difficulty bathing. The primary independent variable was body mass index (BMI), classified as normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), or obese (BMI ≥30 kg/m2) using World Health Organization classifications.
Covariates included proxy respondent status, age (in years), sex, race and ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), self-reported general health (excellent, good, average, below average, or poor),29 self-reported cancer and dementia diagnoses, total household income, marital status (married or not), number of people in the household, and number of living children. In addition, the level of difficulty that respondents report in performing each ADL was included, on a three-point scale (a little, some, or a lot of difficulty).
Analysis
We described demographic characteristics and prevalence of medical comorbidities for those in our cohort classified by BMI as normal weight, overweight and obese, and used χ2 and t tests to determine for significant differences between BMI groups. We then compared the prevalence of specific ADL disabilities for all individuals in each BMI group.
We used multivariable logistic regression models to determine the association with BMI class and odds of receiving assistance for a specific ADL for those reporting disability in that ADL and the effect of potential mediating factors and confounders on the overall association. The initial model was unadjusted. Further models sequentially added clusters of potential mediator covariates. Mediators were determined from our hypothesized theory as well as prior evidence around the role of demographics, stigma, household resources, and physical challenges to caregiving (Figure 1). The second model adjusted for age, race, and sex. The third model added covariates assessing the severity of need for assistance included general health and level of difficulty with performing the impaired ADL. The fourth model added covariates assessing personal resources included total household income, marital status, the number of people in the house, and number of children. The fifth model added, to all the covariates previously mentioned, covariates assessing cognitive status and if the respondent was a proxy. With each added cluster of variables, the odds ratio between obesity and receipt of assistance was assessed for statistical significance and relative size compared to the prior model.
All models applied survey weights30 and accounted for sampling strategy. Sensitivity analyses included a hierarchical mixed-effects model to account for repeated measures for individuals as well as modeling BMI as a fractional polynomial in order to allow it to be a continuous variable with flexibility of shape in relation to receipt of assistance. In addition, some alternative approaches were used to quantify the relative mediation effects of variable clusters. First, the coefficients were standardized without survey weights applied, then the indirect effects were computed as the product of the coefficients. Finally, bootstrapping was used to compute standard errors of the indirect effects of covariates and direct effect of BMI class.31 This study was assessed and determined to be exempt from review by the University of Michigan Institutional Review Board.
Results
Between 2010 and 2015 there were 11,359 observations of NHATs respondents reporting difficulty despite any accommodations in performing any ADLS, which include dressing, eating, bathing, toileting, walking inside, walking outside or getting in or out of bed. We excluded 436 observations (3.8%) missing BMI measurement for the individual during the current or prior survey wave, an additional 375 observations (3.4%) with underweight BMI and an additional 13 observations with missing covariates (1.0%). The final cohort was 10,535 observations of 5,639 individuals given that some (2,440) individuals were followed for multiple survey waves.
Demographic and comorbidities vary between individuals in different BMI classes as demonstrated in Table 1. Obese adults are younger, more likely to be women, more likely to be Hispanic and non-Hispanic blacks, less likely to describe excellent and very good health, and less likely to have a proxy respondent than normal weight individuals (all p values <0.05). Obese individuals have different comorbidities than normal weight adults with lower rates of dementia but higher rates of heart disease, hypertension and diabetes.
Table 1.
Baseline characteristics of adults age 65 with activities of daily living disability included in the cohort.
| Normal weight (n=1,919) | Overweight (n=1,948) | Obese (n=1,772) | p-value | |
|---|---|---|---|---|
|
|
||||
| Age, N (%): | ||||
| 65–69 | 14.3% | 21.2% | 32.5% | <0.001 |
| 70–74 | 17.9% | 20.7% | 27.7% | |
| 75–59 | 15.7% | 22.3% | 19.5% | |
| 80–84 | 21.6% | 17.0% | 11.5% | |
| 85–89 | 17.6% | 12.4% | 6.4% | |
| 90+ | 13.0% | 6.5% | 2.4% | |
| Sex, N (%): | ||||
| Men | 38.6% | 47.9% | 37.6% | <0.001 |
| Women | 61.4% | 52.1% | 62.4% | |
| Race, N (%): | ||||
| White, non-Hispanic | 77.1% | 78.2% | 74.4% | <0.001 |
| Black, non-Hispanic | 7.7% | 8.5% | 11.9% | |
| Other | 7.8% | 5.5% | 4.7% | |
| Hispanic | 7.4% | 7.8% | 9.0% | |
| Self-reported health, N(%): | ||||
| Excellent | 5.6% | 7.1% | 2.8% | <0.001 |
| Very good | 19.8% | 21.4% | 18.0% | |
| Good | 33.0% | 35.1% | 35.3% | |
| Fair | 27.9% | 26.6% | 30.9% | |
| Poor | 13.7% | 9.9% | 13.1% | |
| Proxy responder (%): | 13.7% | 8.5% | 4.8% | <0.001 |
| Medical conditions, N (%): | ||||
| Dementia | 12.5% | 8.1% | 4.5% | <0.001 |
| Heart disease | 23.3% | 22.0% | 25.6% | 0.04 |
| Hypertension | 62.9% | 71.7% | 81.1% | <0.001 |
| Diabetes | 18.9% | 29.2% | 45.6% | <0.001 |
| Osteoarthritis | 31.4% | 24.7% | 22.3% | <0.001 |
| Lung disease | 19.4% | 18.5% | 24.2% | 0.001 |
| Cancer | 21.4% | 21.8% | 20.8% | 0.81 |
Group percentages weighted according to National Health and Aging Trends Study analytic weights.
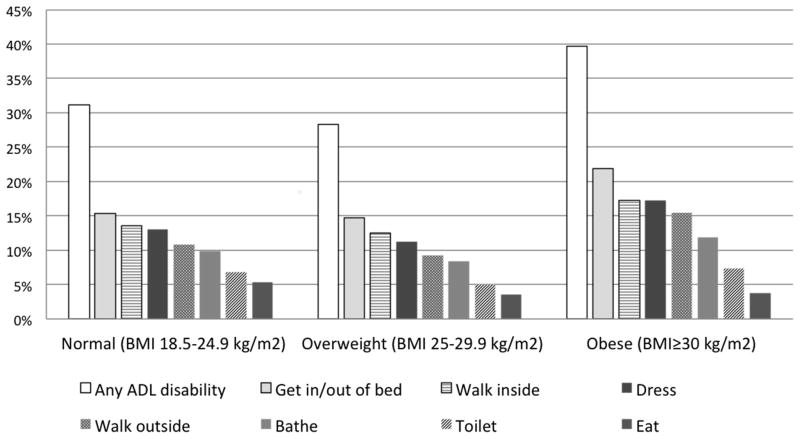
Figure 2 demonstrates the rates of specific ADL disabilities among adults age 65 and older with BMI measurements collected by NHATs. In comparing obese and normal weight adults, older adults with obesity reported higher rates of any ADL disability (39.7%) compared to overweight and normal weight older adults (28.3% and 31.2% respectively). Rates of disability in eating and toileting were similar but obese adults reported higher rates of difficulty getting in and out of bed (21.9% vs 15.30% of normal weight older adults), walking inside (17.3% vs. 13.6%), dressing (17.3% vs. 13.0%), and walking outside (15.5% vs. 10.8%).
Figure 2.
Prevalence of specific activities of daily living disabilities in adults age 65 and older by body mass index (BMI).
In our initial unadjusted logistic regression model (Table 2), obese older adults with difficulty walking inside had an odds ratio (OR) of 0.50 of receiving assistance (95% confidence interval (CI) 0.41 to 0.60) compared to those with normal weights. Obese older adults with disability had lower rates of assistance in walking outside (OR 0.57, 95% CI 0.47–0.69), toileting (OR 0.58, 95% CI 0.46–0.73), getting in/out of bed (OR 0.61, 95% CI 0.49–0.77), bathing (OR 0.61, 95% CI 0.48–0.77), and eating (OR 0.64, 95% CI 0.47–0.86). There was no significant difference in assistance for those with difficulty dressing (OR 1.06, 95% CI 0.89–1.25).
Table 2.
Odds of assistance for specific impaired activities of daily living by body mass index classification.
| Normal weight | Overweight | Obese | |
|---|---|---|---|
| Model 1: Unadjusted. | |||
| Walking inside | 1.00 (reference) | 0.57 (0.48–0.68) | 0.50 (0.41–0.60) |
| Walking outside | 1.00 (reference) | 0.74 (0.62–0.89) | 0.57 (0.47–0.69) |
| Toileting | 1.00 (reference) | 0.79 (0.62–1.01) | 0.58 (0.46–0.73) |
| Getting in/out of bed | 1.00 (reference) | 0.67 (0.55–0.81) | 0.61 (0.49–0.77) |
| Bathing | 1.00 (reference) | 0.70 (0.57–0.84) | 0.61 (0.48–0.77) |
| Eating | 1.00 (reference) | 0.72 (0.56–0.92) | 0.64 (0.47–0.86) |
| Dressing | 1.00 (reference) | 0.84 (0.69–1.03) | 1.06 (0.89–1.25) |
| Model 2: Adjusting for age, race, and sex. | |||
| Walking inside | 1.00 (reference) | 0.63 (0.51–0.77) | 0.63 (0.50–0.81) |
| Walking outside | 1.00 (reference) | 0.83 (0.68–1.01) | 0.76 (0.59–0.97) |
| Toileting | 1.00 (reference) | 0.89 (0.65–1.21) | 0.68 (0.52–0.89) |
| Getting in/out of bed | 1.00 (reference) | 0.71 (0.59–0.86) | 0.67 (0.50–0.87) |
| Bathing | 1.00 (reference) | 0.85 (0.69–1.05) | 0.91 (0.69–1.21) |
| Eating | 1.00 (reference) | 0.77 (0.59–1.00) | 0.73 (0.52–1.03) |
| Model 3: Adjusting for covariates from model above plus covariates for degree of need: general health and severity of disability. | |||
| Walking inside | 1.00 (reference) | 0.65 (0.51–0.82) | 0.65 (0.50–0.85) |
| Walking outside | 1.00 (reference) | 0.87 (0.68–1.10) | 0.85 (0.64–1.12) |
| Toileting | 1.00 (reference) | 0.90 (0.65–1.25) | 0.64 (0.45–0.91) |
| Getting in/out of bed | 1.00 (reference) | 0.72 (0.56–0.93) | 0.60 (0.43–0.83) |
| Bathing | 1.00 (reference) | 1.13 (0.84–1.52) | 1.23 (0.88–1.72) |
| Eating | 1.00 (reference) | 0.91 (0.70–1.19) | 0.92 (0.64–1.31) |
| Model 4: Adjusting for covariates from models above plus covariates for home resources: total income, married, number of people in household, number of children | |||
| Walking inside | 1.00 (reference) | 0.65 (0.51–0.82) | 0.64 (0.49–0.84) |
| Walking outside | 1.00 (reference) | 0.87 (0.69–1.11) | 0.83 (0.63–1.09) |
| Toileting | 1.00 (reference) | 0.90 (0.65–1.25) | 0.64 (0.45–0.90) |
| Getting in/out of bed | 1.00 (reference) | 0.71 (0.55–0.93) | 0.59 (0.43–0.83) |
| Bathing | 1.00 (reference) | 1.13 (0.84–1.54) | 1.22 (0.87–1.71) |
| Eating | 1.00 (reference) | 0.88 (0.67–1.15) | 0.87 (0.61–1.24) |
| Model 5: Adjusting for covariates from models above plus covariates for cognitive status: dementia, proxy respondent | |||
| Walking inside | 1.00 (reference) | 0.73 (0.57–0.94) | 0.78 (0.58–1.05) |
| Walking outside | 1.00 (reference) | 0.91 (0.70–1.17) | 0.87 (0.65–1.17) |
| Toileting | 1.00 (reference) | 1.05 (0.76–1.45) | 0.76 (0.53–1.08) |
| Getting in/out of bed | 1.00 (reference) | 0.82 (0.63–1.07) | 0.69 (0.49–0.98) |
| Bathing | 1.00 (reference) | 1.20 (0.90–1.60) | 1.39 (0.97–1.98) |
| Eating | 1.00 (reference) | 0.98 (0.69–1.39) | 1.04 (0.72–1.52) |
We sequentially added clusters of covariates to the model in order to test the mediating role of different factors described in our conceptual model (Table 2). Adjusting for demographic differences between obese and normal weight individuals (age, race, sex) reduced the association of obesity with assistance, although there were still significant differences in assistance for all ADLs other than bathing and eating. Adding covariates for degree of need which included general health and severity of disability reduced the association of obesity with assistance for walking outside (from OR 0.76 in prior model to 0.85 when adjusting for degree of need). Adding covariates for home resources which included total income, as well as, marriage, number of people in the household, and number of children, did not change the association of obesity with assistance. Adding covariates for cognitive status (dementia and proxy respondent) reduced the association of obesity with several ADLs to the degree that they were no longer statistically significant: assistance for walking inside (OR 0.64 in prior model, 0.78 when adjusting for cognitive status), toileting (OR 0.64 in prior model, 0.76 when adjusting for cognitive status). The association for getting in/out of bed remained statistically significant (OR 0.59 in prior model, 0.69 when adjusting for cognitive status, 95% CI 0.49–0.98).
Additional attempts to assess for mediation in this logistic regression model found that BMI had a significant direct effect on help walking inside as well as getting out of bed despite full adjustments, and that the cognitive status and demographics had the greatest mediating effects on the association (Appendix Table 1). In order to account for repeated observations, the full model was tested using a hierarchical modeling approach, and results did not differ (results not shown). In order to account for the range of BMIs as opposed to the standard categorization, BMI was modeled as a fractional polynomial while adjusting for all covariates including age. In these models, there are decreasing rates of assistance for walking inside, walking outside, and toileting as well as getting in/out of bed as BMI rises beyond a normal range of 18.5–24.9 (Appendix Figure 1).
Discussion
In a nationally representative cohort of older adults in the United States with ADL impairments, we demonstrated that older adults with obesity have higher rates of ADL impairments and lower rates of assistance compared to their normal weight counterparts. These gaps in assistance were largest for assistance with mobility and transfers. This has significant policy and healthcare implications given the predicted growing population of older adults with obesity. While part of the gap in assistance was explained by severity of disability and cognitive status, even in our fully adjusted models obese individuals reported significantly less assistance with walking indoors.
As we expected, the association of obesity with absent assistance with ADLs is particularly strong for mobility-related ADLs where providing assistance is more physically demanding. Unlike prior research,21 the finding persisted despite adjusting for demographics. We then explored potential mediating factors to delineate if the lower assistance was due to barriers to assistance versus lower need for assistance. Our analysis found partial mediation by degree of need, indicating that barriers to assistance may play a role. However, we did not find that insufficient household resources in terms of either assets or people to assist mediated the association as was hypothesized. Cognition appeared to have the largest effect of the association, although still as a partial and not complete mediator. This indicates that further research into the contributions of both stigma and the physical challenges of obesity caregiving will be important next steps.
The factors that explained the greatest proportion of the difference in receipt of care between obese and normal weight individuals was dementia and need for a proxy respondent, a related measure of cognitive impairment. There are two hypotheses for this finding. One is that older adults without cognitive impairment have increased ability to rally support from family or even gain access to nursing home care. An alternative explanation is that the lower prevalence of cognitive impairment in older adults with obesity enables them to cobble independent solutions at home alone despite disability and avoid the complexity of entering into a care recipient role, which may not be preferred despite the hardships of unmet needs. Therefore, dementia may indicate increased need for assistance, explaining this gap. Further research with more in-depth surveying and interviews is needed to establish if this is occurring and if it is a desired response to absent assistance by older adults with intact cognition.
This study has several limitations. This data was analyzed as a cross-sectional analysis, and further longitudinal analysis will be important to understand causal relationships. Our study relies on BMI as it is the most widely accepted and available measure of obesity, but we do not differentiate obesity subtypes such as sarcopenic obesity.32 The reliability of responses from our proxy respondents may be lower than non-proxies, especially regarding absent assistance and unmet needs in cases where they are a primary caregiver, although there is some evidence this is not the case from other studies.33 While we can capture the degree of difficulty that individuals report in performing an ADL as well as if they have had to go without that ADL, we would ideally have more information as to the level of needs that individuals have. Further, we have no measures of the implications of absent caregiving, both in terms of physical effects (pressure ulcers, poor hygiene, infections) and psychological effects (social isolation, perceiving weight bias, ADL-specific anxiety). Despite these limitations, the strength of our study is that we capture a nationally-representative population, base our analysis on a conceptual theory, and utilize data capturing both surveyed factors and measured BMI.
Research is needed to examine the implications of the lower rates of assistance received by the growing population of older adults with obesity and disability. While the nursing challenges of assisting obese individuals have been established,16 little is known about the patient and family experience. Even obese individuals with available family members to assist them might require extra help with safe transfers and mobility assistance. Given that Medicare and Medicaid generally do not reimburse for additional home health aides for obese patients, research should assesses if enriched personal aid funding for this population might offset high-cost nursing home care. Similarly, the possible ramifications of inadequate nursing and custodial assistance for this population such as lower physical function, higher rates of medical complications including depression, social isolation, infection, falls, malnutrition, and pressure ulcers; and higher costs of care, hospitalizations and emergency department visits are not well understood. Intervention and cost-effectiveness studies focusing on obese, disabled individuals should consider assessing the impacts of enriched home-based personal aid and medical equipment such as lifts, bariatric walkers and commodes, as well as no-lift policies in hospitals and nursing homes to increase utilization of mechanical lifts.34
This deficit in caregiving has policy implications given the cost of long term care and the high healthcare utilization of obese, disabled, older adults. Further work needs to be done to understand the evolving capacity of formal and informal long-term care to serve the needs of obese individuals. Addressing these issues will only be more pressing as older adults increasingly find themselves struggling with both obesity and disability.
Supplementary Material
Supplemental Figure S1: Partial residual plots of the association of BMI modeled as a fractional polynomial and activity of daily living assistance for disabled older adults.
Supplementary Table S1. Estimated indirect and direct effects of covariates with help with each ADL.
Acknowledgments
Funding sources: Dr. Ankuda is funded by the Robert Wood Johnson Foundation. Dr. Harris is funded by National Institute of Child Health and Human Development under grant K12HD063087. Dr. Levine is funded by the National Institute on Aging (NIA) under grant K23AG040278. Dr. Langa is supported by NIA grants P30AG024824 and P30AG053760. Dr. Ornstein is funded by NIA grant K01AG047923. Dr. Kelley is supported by the NIA K23AG040774 and the American Federation for Aging Research. The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Author contributions: Study concept and design: Claire K. Ankuda, John Harris, Katherine Ornstein, Deborah A. Levine, Kenneth M. Langa, Amy S. Kelley. Acquisition and management of data: Claire K. Ankuda, John Harris. Analysis and interpretation of data: Claire K. Ankuda, John Harris, Katherine Ornstein, Deborah A. Levine, Kenneth M. Langa, Amy S. Kelley. Preparation of manuscript: Claire K. Ankuda, John Harris. Revision of manuscript: Claire K. Ankuda, John Harris, Katherine Ornstein, Deborah A. Levine, Kenneth M. Langa, Amy S. Kelley.
References
- 1.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. 2015 http://www.ncbi.nlm.nih.gov/pubmed/26633046. [PubMed]
- 2.Ortman BJM, Velkoff Va, Hogan H. An Aging Nation: The Older Population in the United States. 2014 census.gov.
- 3.Yang Z, Zhang N. The Burden of Overweight and Obesity on Long-term Care and Medicaid Financing. Med Care. 2014;52(7):658. doi: 10.1097/MLR.0000000000000154. [DOI] [PubMed] [Google Scholar]
- 4.Lang IA, Llewellyn DJ, Alexander K, Melzer D. Obesity, physical function, and mortality in older adults. J Am Geriatr Soc. 2008;56(8):1474–1478. doi: 10.1111/j.1532-5415.2008.01813.x. [DOI] [PubMed] [Google Scholar]
- 5.Rillamas-Sun E, LaCroix AZ, Waring ME, et al. Obesity and late-age survival without major disease or disability in older women. JAMA Intern Med. 2014;174(1):98–106. doi: 10.1001/jamainternmed.2013.12051.Obesity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rejeski WJ, Marsh AP, Chmelo E, Rejeski JJ. Obesity, intentional weight loss and physical disability in older adults. Obes Rev. 2010;11(9):671–685. doi: 10.1111/j.1467-789X.2009.00679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alley DE, Chang VW. The Changing Relationship of Obesity and Disability, 1988–2004. JAMA. 2007;298(17) doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 8.Hahler B. Morbid obesity: a nursing care challenge. MEDSURG Nurs. 2002:85. [PubMed] [Google Scholar]
- 9.Rose MA, Baker G, Drake DJ, et al. Nurse Staffing Requirements for Care of Morbidly Obese Patients in the Acute Care Setting. Bariatr Nurs Surg Patient Care. 2006;1(2):115–121. doi: 10.1089/bar.2006.1.115. [DOI] [Google Scholar]
- 10.Lapane K, Resnik L. Weighing the Relevant Issues: Obesity in Nursing Homes. J Aging Soc Policy. 2006;18(2):1–9. doi: 10.1300/J031v18n02. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher S. Obesity and the aging adult: Ideas for promoting patient safety and preventing caregiver injury. Clin Geriatr Med. 2005;21(4):757–765. doi: 10.1016/j.cger.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Rotkoff N. Care of the Morbidly Obese Patient in a Long-term Care Facility. Geriatr Nurs (Minneap) 1999;20(6):309–313. doi: 10.1053/gn.1999.v20.103924001. [DOI] [PubMed] [Google Scholar]
- 13.Bradway C, Miller E, Heivly A, Fleshner I. Continence Care for Obese Nursing Home Residents. Urol Nurs. 2010;30(2):2–5. [PubMed] [Google Scholar]
- 14.Humphreys S. Obesity in Patients and Nurses Increases the Nurse’s Risk of Injury Lifting Patients. Bariatr Nurs Surg Patient Care. 2007;2(1):3–6. doi: 10.1089/bar.2006.9998. [DOI] [Google Scholar]
- 15.Bureau of Labor Statistics. Number, Incidence Rate, and Median Days Away from Work for Nonfatal Occupational Injuries and Illnesses Involving Days Away from Work and Musculoskeletal Disorders by Selected Worker Occupation and Ownership, 2013. 2013 http://www.bls.gov/news.release/osh2.t18.htm.
- 16.Bradway C, DiResta J, Fleshner I, Polomano RC. Obesity in nursing homes: A critical review. J Am Geriatr Soc. 2008;56(8):1528–1535. doi: 10.1111/j.1532-5415.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 17.Zizza CA, Herring A, Stevens J, Popkin BM. Obesity affects nursing-care facility admission among whites but not blacks. Obes Res. 2002;10(8):816–823. doi: 10.1038/oby.2002.110. [DOI] [PubMed] [Google Scholar]
- 18.Zizza C, Herring A, Domino M, Haines P, Stevens J, Popkin BM. The effect of weight change on nursing care facility admission in the NHANES I Epidemiologic Followup Survey. J Clin Epidemiol. 2003;56(9):906–913. doi: 10.1016/S0895-4356(03)00142-2. [DOI] [PubMed] [Google Scholar]
- 19.Valiyeva E, Russell LB, Miller JE, Safford MM. Lifestyle-related risk factors and risk of future nursing home admission. Arch Intern Med. 2006;166(9):985–990. doi: 10.1001/archinte.166.9.985. [DOI] [PubMed] [Google Scholar]
- 20.Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60(1):124–129. doi: 10.1111/j.1532-5415.2011.03767.x. [DOI] [PubMed] [Google Scholar]
- 21.Resnik L, Lapane KL, Allen SM. Obesity and receipt of personal care assistance for people with mobility impairments. ObesRes. 2005;13:1307–1310. doi: 10.1038/oby.2005.158.. [DOI] [PubMed] [Google Scholar]
- 22.Puhl R, Heuer C. The stigma of obesity: a review and update. Obesity. 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 23.Levine JA. Poverty and obesity in the U.S. Diabetes. 2011;60(11):2667–2668. doi: 10.2337/db11-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedditizi E, Peters R, Beckett N. The risk of overweight/obesity in mid-life and late life for the development of dementia: A systematic review and meta-analysis of longitudinal studies. Age Ageing. 2016;45(1):14–21. doi: 10.1093/ageing/afv151. [DOI] [PubMed] [Google Scholar]
- 25.Ornstein Ka, Leff B, Covinsky KE, et al. Epidemiology of the Homebound Population in the United States. JAMA Intern Med. 2015;175(7):1180–1186. doi: 10.1001/jamainternmed.2015.1849.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Montaquila J, Freedman VA, Edwards B, Kasper JD. National Health and Aging Trends Study Round 1 Sample Design and Selection. Baltimore, MD: 2011. www.nhats.org. [Google Scholar]
- 27.Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156. doi: 10.1136/bmj.i2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freedman VA, Kasper JD, Spillman BC, et al. Behavioral adaptation and late-life disability: A new spectrum for assessing public health impacts. Am J Public Health. 2014;104(2) doi: 10.2105/AJPH.2013.301687.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeSalvo K, Bloser N, Reynolds K, He J, Muntner P. Mortality Prediction with a Single General Self-Rated Health Question. J Gen Intern Med. 2005;20:267–275. doi: 10.1111/j.1525-1497.2005.0291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Montaquila J, Freedman Va, Kasper Judith D. NHATS Technical Paper # 6. 2014. National Health and Aging Trends Study Development of Round 2 Survey Weights. [Google Scholar]
- 31.Kenny D. [Accessed November 20, 2016];Mediation with Dichotomous Outcomes. http://davidakenny.net/cm/mediate.htm.
- 32.Roubenoff R. Sarcopenic obesity: the confluence of two epidemics. Obes Res. 2004;12(6):887–888. doi: 10.1038/oby.2004.107. [DOI] [PubMed] [Google Scholar]
- 33.Ahasic AM, Van Ness PH, Murphy TE, Araujo KLB, Pisani MA. Functional status after critical illness: Agreement between patient and proxy assessments. Age Ageing. 2015;44(3):506–510. doi: 10.1093/ageing/afu163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edlich RF, Hudson MA, Buschbacher RM, et al. Devastating injuries in healthcare workers: description of the crisis and legislative solution to the epidemic of back injury from patient lifting. J Long Term Eff Med Implants. 2005;15(August 2004):225–241. doi: 10.1615/JLongTermEffMedImplants.v15.i2.90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1: Partial residual plots of the association of BMI modeled as a fractional polynomial and activity of daily living assistance for disabled older adults.
Supplementary Table S1. Estimated indirect and direct effects of covariates with help with each ADL.