In this issue of the Journal, Raya Kheirbeck and colleagues present an analyses of a birth cohort-specific (1910–1915) sample of U.S. Veterans Administration-wide clinical data from community-dwelling deceased octogenarian (n≈31,000), nonagenarian (n≈52,000) and centenarian (n≈3,000) Veterans.1 With 97% of the centenarian sample being male, this study is by far and away the largest descriptive study of male centenarians to-date.
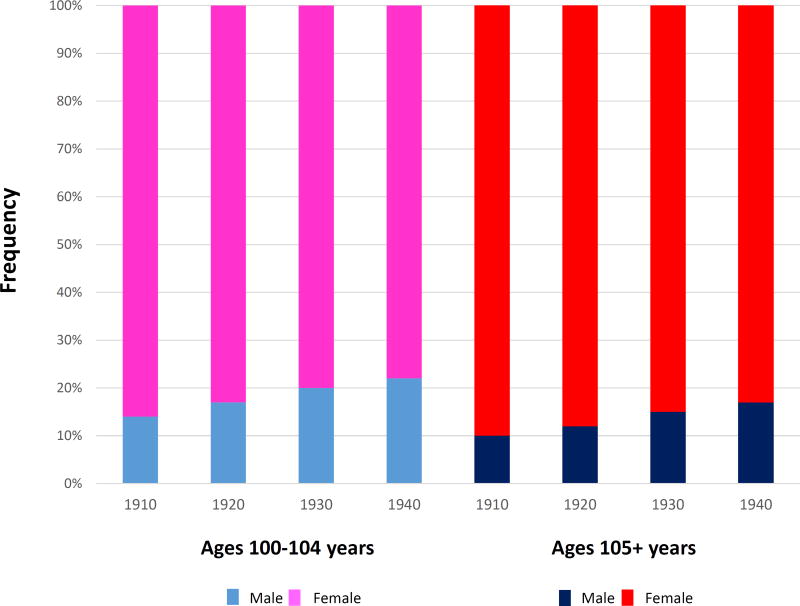
Perhaps nowhere is the difference between male and female survival more significant than when observing survival to 100+ years. According to the 2005 U.S. Social Security Administration’s birth cohort life tables2, for example, out of 100,000 people born in 1910, 3,795 were estimated to survive to 100 years old and older of which 14% were men and 86% were women. Figure 1 shows that the difference becomes even more pronounced for males and females surviving to age 105+ years, who for the 1910 birth cohort, for example, are comprised of 10% men and 90% women. Interestingly, new analyses reveal that with increasingly more recent birth cohorts, the life tables indicate that the relative proportion of men ages 100–104 years will steadily increase from 14% to 22% and for those 105+ years, their proportion will increase from 10% to 17%. This increase, if it is not some prediction artifact, would suggest some secular change(s) in health-related behaviors or environment that preferentially improves survival rates of men, compared to women, to these extreme ages.
Figure 1.
Birth year cohort-specific frequencies of males and females ages 100–104 and 105+ years according to 2005 U.S. Social Security cohort life table data.
One such secular change may be cigarette use where it has been noted that at earlier birth cohorts, men had higher rates of tobacco use, but with more recent cohorts the difference between sexes disappears.3 These sex and secular-associated differences in survival of the most extreme ages illustrate how very important it is to take into account these variables when investigating factors associated with survival to different ages and speak to the careful attention Kheirbeck and her colleagues paid to limiting their sample to a specific birth cohort. Thus, the lay public and scientists must keep in mind that the necessary combinations of genetic and environmental variants for people born in 1900 to survive to say, the oldest one percentile of survival, will be significantly different from what may be required for people born more recently.4,5 Furthermore, these genetic and environmental signatures certainly vary by sex, ethnicity and with more advanced age.6,7
Several characteristics of the Veteran’s sample must therefore be kept in mind when considering the generalizability of the presented findings. For example, 88% of the cohort is Caucasian. A very interesting and important race-related (and still somewhat controversial) difference for ages beyond approximately 90 years, at least for birth cohorts up through the early 1900’s, is a possible phenomenon called the Black-White mortality crossover. While mortality rates were higher for Blacks than for Whites at younger ages, in 1922 Raymond Pearl observed that according to 1916 U.S. mortality data, out of a total of approximately 1 million deaths at all ages, there were 649 centenarians, out of which 332 were Black and 317 where White (p. 26).8 Pearl remarked that some of these data had to be incorrect, such as a white person age 120 years and a black person, age 134 year.9 Still, there remained the possibility that after some older age, mortality rates for Blacks became less than for whites. The underlying mechanism would be that because Blacks are generally a more vulnerable population (e.g. due to poorer socioeconomic status, less access to medical care and public health measures etc.) they generally die at younger ages, but there is a select survivor cohort left behind with enhanced survival relative to the same birth cohort of Whites. The existence of a Black-White crossover has been hotly debated for years mostly because of suspect age records,10–12 but proponents also claim to observe the phenomenon amongst American Indians versus Whites and even more so among Hispanics compared to Whites.13 Cardiovascular disease-related mortality has been noted to be higher in Blacks at younger ages, but becomes relatively less frequent at much older ages.14
In considering their community dwelling sample, Kheirbek et al conclude that relative to octogenarians and nonagenarians from the same birth cohort, male centenarians demonstrate markedly reduced incidence rates of numerous diseases normally associated with increased risk of mortality. This finding is supported by our own work from the New England Centenarian Study, in which male centenarians are more likely to have delayed (age of onset after age 8015 or 85 years16) or to have escaped (age of onset after age 100 years) such age-related diseases rather than having developed them prior to the age of 65 years (“survivors”15 of disease). The Albert Einstein College of Medicine’s Longevity Genes Project and the Long Life Family Study noted the same amongst its male family members that are predisposed to healthy aging.17
Unlike men though, Women who live to around the oldest 1 percentile of survival (101 years for the U.S. 1900 birth cohort) are nearly just as likely to be survivors as they are delayers. The facts that 85%–90% of centenarians are women and that older women are, compared to men, more able to live with age-related diseases rather than die from them all speak to the realization that there are significant differences between men and women in the biological mechanisms that underlie healthy aging and exceptional longevity.18 The fact that women are more resilient however is a double-edged sword in that while women are more likely to live longer, at older ages they are also more likely than men to have chronic illnesses and disabilities. Male centenarians on the other hand, though far fewer, tend to be in better medical and functional condition because they are such a select survivor cohort. There may be an exception however to the different pathways of longevity in men and women. As they approach the limit of lifespan, that is, supercentenarians (ages 110+ years), our results suggest that the men and women in this most extreme and rare group are phenotypically much more alike, in that the majority of them are “escapers” and on average they delay both disability and mortality-associated age-related diseases until an average age of 106 years.19 Such phenotypic similarity might also suggest similar longevity-associated genetic and non-genetic variants. Generally speaking though, when one studies centenarians, they are studying almost entirely women. Therefore, when an opportunity like this Veterans study comes along, it truly affords us a unique opportunity to investigate how male centenarians are different from or similar to their female counterparts.
A possibility for why men and women are for the most part so different from one another in terms of “risk” for exceptional longevity might relate to what evolutionary mechanisms select for longevity-associated genetic variants. I propose that one such selective pressure would be to slow the rate of aging of the female reproductive system to increase the time span during which women can bear children, therefore having more children and a greater opportunity to pass the woman’s genes down to subsequent generations. These genes of course don’t stop slowing aging once reproduction ceases and thus they enable women (and men) to not only live long enough to ensure the survival of their children to reproductive age, but to live long enough to be grandparents and in some cases, even centenarians (and great-great grandparents). This hypothesis is supported by our finding that women who naturally bear children in their forties are 4–5 times more likely to live to become a centenarian compared to women with average age of child bearing.20 If women are the evolutionary driving force behind the development of longevity-enabling genes, perhaps this could explain in part why men and women age so differently.
Hopefully, the study by Raya Kheirbeck and colleagues, of the largest sample of male centenarians to date, will be just the first of many studies to follow. The rich and longitudinal nature of the medical data that typically accompany Veteran studies will allow for further study into specific subphenotypes of exceptional longevity. All the more exciting is the prospect of enrolling Veteran centenarians in a prospective longitudinal study to discover biological factors and pathways associated with what Kheirbeck and colleagues have very nicely characterized as an exceptionally healthy aging cohort that compresses disease towards the end of their very long lives.
Acknowledgments
Funding Sources: National Institute on Aging grants AG-023755 and AG-023122 and the William Wood Foundation
Sponsor: Support received from the William M. Wood Foundation and The Longevity Consortium (National Institute on Aging AG-023122). Sponsor’s Role: The Sponsors played no role in this work other than funding.
Footnotes
Dr. Perls has no conflict of interest to declare. Authors Contributions: Dr. Perls was the sole contributor to this work.
References
- 1.Kheirbek RA, Fokar A, Shara N, et al. Characteristics and incidence of chronic illness in community-dwelling predominantly male U.S. Veteran centenarians. J Amer Geriatr Soc. 2017 doi: 10.1111/jgs.14900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell FC, Miller ML. [accessed September 5, 2011];Life Tables for the United States Social Security Area 1900–2100, actuarial study no. 120. 2005 URL: http://www.ssa.gov/oact/NOTES/as120/LifeTables_Tbl_7_1900.html.
- 3.Anderson CM, Burns DM, Dodd KW, Feuer EJ. Birth-cohort-specific estimates of smoking behaviors for the U.S. populaion. Risk Analysis. 2012;32:S14–S24. doi: 10.1111/j.1539-6924.2011.01703.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaupel JW. Biodemography of human ageing. Nature. 2010;464:536–42. doi: 10.1038/nature08984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nygaard M, Lindahl-Jacobsen R, Soerensen M, et al. Birth cohort differences in the prevalence of longevity-associated variants in APOE and FOXO3A in Danish long-lived individuals. Exp Gerontol. 2014;57:41–6. doi: 10.1016/j.exger.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sebastiani P, Solovieff N, Dewan AT, et al. Genetic signatures of exceptional longevity in humans. PLoS One. 2012;7:e29848. doi: 10.1371/journal.pone.0029848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colchero F, Rau R, Jones OR, et al. The emergence of longevous populations. Proc Natl Acad Sci U S A. 2016;113:E7681–E90. doi: 10.1073/pnas.1612191113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pearl R. The Biology of Death. Philadelphia: J.B. Lippincott; 1922. https://books.google.com/books?id=puPUXw62Gq4C&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false. [Google Scholar]
- 9.Young TE. On Centenarians; the duration of the human race: A fresh and authentic inquiry. London: Charles and Edwin Layton; 1899. https://play.google.com/store/books/details?id=fAcFAAAAYAAJ&rdid=book-fAcFAAAAYAAJ&rdot=1. [Google Scholar]
- 10.Elo I, Preston SH. Estimating African American Mortality from inaccurate data. Demography. 1994;31:427–58. [PubMed] [Google Scholar]
- 11.Olshansky SJ. Mortality crossovers and selective survival in human and nonhuman populations. New developments in mortality. Gerontologist. 1995;35:583–7. doi: 10.1093/geront/35.5.583a. [DOI] [PubMed] [Google Scholar]
- 12.Manton KG, Sandomirsky S, Woing S. The black/white mortality crossover: Investigation from the persepctive of the components of aging. Geronotologist. 1979;19:291–300. doi: 10.1093/geront/19.3.291. [DOI] [PubMed] [Google Scholar]
- 13.Mohtashemi M, Levins R. Qualitative analysis of the all-cause Black-White mortality crossover. Bull Math Biol. 2002;64:147–73. doi: 10.1006/bulm.2001.0270. [DOI] [PubMed] [Google Scholar]
- 14.Corti M, Guralnik J, Ferrucci L, et al. Evidence for a black-white crossover in all-cause and coronary heart disease mortality in an older population: the North Carolina EPESE. Am J Pub Health. 1999;89:308–14. doi: 10.2105/ajph.89.3.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evert J, Lawler E, Bogan H, Perls T. Morbidity profiles of centenarians: survivors, delayers, and escapers. J Gerontol A Biol Sci Med Sci. 2003;58:232–7. doi: 10.1093/gerona/58.3.m232. [DOI] [PubMed] [Google Scholar]
- 16.Terry D, Sebastiani P, Andersen S, Perls T. Disentangling the roles of disability and morbidity in survival to exceptional old age. Arch Intern Med. 2008;168:277–83. doi: 10.1001/archinternmed.2007.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ismail K, Nussbaum L, Sebastiani P, et al. Compression of Morbidity Is Observed Across Cohorts with Exceptional Longevity. J Am Geriatr Soc. 2016;64:1583–91. doi: 10.1111/jgs.14222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Franceschi C, Motta L, Valensin S, Rapisarda R, Franzone A, Berardelli M, Motta M, Monti D, Bonafe M, Ferrucci L, Deiana L, Pes GM, Carru C, Desole MS, Barbi C, Sartoni G, Gemelli C, Lescai F, Olivieri F, Marchegiani F, Cardelli M, Cavallone L, Gueresi P, Cossarizza A, Troiano L, Pini G, Sansoni P, Passeri G, Lisa R, Spazzafumo L, Amadio L, Giunta S, Stecconi R, Morresi R, Viticchi C, Mattace R, De Benedictis G, Baggio G. Do men and women follow different trajectories to reach extreme longevity? Italian Multicenter Study on Centenarians (IMUSCE) Aging (Milano) 2000;12:77–84. doi: 10.1007/BF03339894. [DOI] [PubMed] [Google Scholar]
- 19.Andersen SL, Sebastiani P, Dworkis DA, Feldman L, Perls TT. Health span approximates life span among many supercentenarians: compression of morbidity at the approximate limit of life span. J Gerontol A Biol Sci Med Sci. 2012;67:395–405. doi: 10.1093/gerona/glr223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perls T, Alpert L, Fretts R. Middle aged mothers live longer. Nature. 1997;389:133. doi: 10.1038/38148. [DOI] [PubMed] [Google Scholar]