Abstract
Objectives
We compared incidence of falls in an emergency department (ED) cohort using a traditional ICD-9 code-based scheme and an expanded definition that included chief complaint information. We further examined the clinical characteristics of those visits “missed” in the ICD-9-based scheme.
Design
Retrospective Electronic Record Review
Setting
Academic medical center ED
Participants
All ED visits of individuals aged 65 and older between 1/1/2013 and 9/30/2015.
Measurements
Two fall definitions were applied (both individually and in unison) to the cohort: an ICD-9-based definition, and a chief complaint definition. Admission and 30-day mortality rates (per encounter) were measured for each definition.
Results
23,880 older adult visits occurred during the study period. Using the most inclusive definition (either ICD-9 code or chief complaint indicating a fall) 4,363 visits (18%) were fall related. Among these visits, 3,506 (80%) met the ICD-9 definition for a fall related visit, while 2,664 (61%) met the chief complaint definition. Among visits meeting the chief complaint definition, 857 (19.6%) were missed when applying the ICD-9 definition alone. Encounters missed by the ICD-9 definition had a lower admission rate (42.9%, 95% CI 39.7–46.3) than those identified (54.4%, 95% CI 52.7–56.0).
Conclusion
Identifying ED fall patients based on diagnosis codes underestimates the true burden of disease. Patients missed by the code-based definition were less likely to have been admitted than those captured. These findings call attention to the value of using chief complaint information to identify fall patients in the ED setting, whether it be for research, clinical care, or policy reasons.
Introduction
Falls among older adults are common, with a yearly incidence of 33%.1 Falls are associated with significant morbidity, mortality,2 and cost (over $19 billion annually in the US3). Despite guidelines4 and quality measures,5 screening for fall risk remains inconsistent in the primary care setting.6 The ED offers an ideal additional site to capture high risk patients.7 Despite numerous guidelines recommending screening for fall risk in the ED,7,8 ED-specific data are more scant.9 Several small prospective cohort studies have suggested that patients presenting to the ED have an increased risk of future falls as compared to baseline community dwelling adults.9–11
One challenge to implementing ED-based fall prevention is the significant resource requirement to perform in-person screening in the ED.12,13 An alternative approach to active falls screening is the use of electronic health record (EHR) data, to evaluate targets for potential intervention. Identifying fall risk based on EHR data is a priority in geriatric emergency medicine research,14 which stems from the more general goal of using EHR data to evaluate clinical outcomes as we transition towards a learning healthcare system in which clinical data is used to improve patient care.15 A foundational step in examining falls within EHR data is creating a definition which captures fall patients adequately in large datasets without the need for manual chart review. In prior studies, diagnosis codes, such as the ICD-9 codes and the injury subcodes, have been used as an identifier of falls in large datasets.16,17 While this is a standard procedure for many conditions within health services research, it may miss many patients in the ED, where visits for falls may result in other diagnosis codes reflecting the injury sustained such as fractures, contusions, etc. without mention of the mechanism of injury. A growing body of literature supports the value of classifying ED visits based not only on diagnosis codes but chief complaint, which better captures the reason patients present to the ED and allows for definitions to be applied to patients at the beginning of their ED stay as opposed to only retrospectively.18
The goal of this study was to examine the effect of adding chief complaint data to an ICD-9 diagnosis code- based definition to identify fall patients. We hypothesized that chief complaint-based data would identify additional fall visits as compared to the ICD-9 code-based definition, and, furthermore, that these additionally captured visits would differ with regards to rates of admission and mortality.
Methods
Study Setting and Population
We performed a retrospective observational study using patient EHR data at a single academic medical center ED with level 1 trauma center accreditation and over 50,000 patient visits per year. The study was designed in accordance with the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) statement and was IRB-approved.19 All visits at which patients were 65 years of age or older were included in the analysis. This age cutoff was chosen because the CDC recommends initiation of routine fall screening for individuals aged 65 and older.20 Visits were excluded from analysis if they were either transfers to our ED from other hospitals or resulted in transfer out to another ED, as coding information for these episodes of care was likely incomplete within our EHR. Data were collected from 1/1/2013- 9/30/2015, during which time all patient visits were coded using ICD-9 codes.
Measurements
Two separate definitions to identify patients who fell were applied to the study population: an ICD-9 diagnosis code-based and a chief complaint-based definition. These definitions were used to identify four groups for analysis: 1) all falls identified combining both definitions, 2) those falls identified by the ICD-9 strategy alone, 3) those falls identified by chief complaint alone, and 4) a group representing visits captured by the chief complaint definition which were missed by the ICD-9 definition.
Because the primary purpose of this study was to ascertain whether chief complaint data could identify ED patients who fell, but were not identified using existing claims data, a liberal claims-based falls definition was adopted to maximize sensitivity for falls as opposed to specificity. We examined several published diagnosis code-based definitions of falls16,17 and selected the approach used by Bohl et al.17 Falls were identified by both ICD-9 codes associated with injuries commonly sustained during fall (800–848, 850–854, and 920–924) or e-codes identifying a fall mechanism (E880, E881, E884, E885, or E888). We chose this broad definition to intentionally bias the study towards the null hypothesis: by selecting a coding-based definition which casts a wide net, additional cases identified via chief complaint data were unlikely to have been picked up by more specific definitions. Diagnosis codes are stored in two distinct areas of the EHR: the “encounter diagnoses” are selected by healthcare providers while “hospital account diagnoses” are determined by professional coders and used to submit for insurance reimbursement (also known as the “billing diagnosis”). We searched both encounter and hospital account codes to extract all relevant diagnosis codes. The EHR stores numerous codes for each visit; in our database, the maximum number of encounter codes was 46 and maximum number of hospital account codes was 102. Our methodology recorded all diagnoses for an admission, and as such, may have captured inpatient falls (although these are unlikely events).
In our EHR, chief complaint is stored as a string (text) variable chosen at the time of registration from a predefined list of complaints. Although up to seven chief complaints were stored for each encounter, less than 2% of encounters had more than two complaints listed. Chief complaints were categorized as fall related if they contained the text “fall.” In practice, given the predefined list for selection, this included only two possible chief complaints: “Fall” and “Falls.”
Mortality and admission status were extracted from the EHR, where they exist as discreet fields. Several additional data elements were extracted for exploratory data analysis with the goal of describing patient populations and identifying factors which may relevant to likelihood of capture by ICD-9 versus chief complaint definition. These included patient demographics (age, gender, race/ethnicity, and insurance status) and factors affecting mode of presentation to the ED (arrival mode and Emergency Severity Index (ESI) triage category). The ESI is a widely-used triage system for ED patients, which categorizes patients into five levels, from 1 for the most acute to 5 for the least acute, and has been validated for use in the geriatric population.21 We also reported measures of baseline morbidity: The Elixhauser comorbidity count,22 a count of distinct comorbidities, was calculated using baseline diagnosis data in the EHR. Similarly, we report the Center for Medicare and Medicaid Services’ hierarchical condition categories (HCC) scores, which are used for baseline risk adjustment. Both the Elixhauser count and the HCC scores allowed us to compare the various populations for differences in comorbidities.
Data Analysis
Data were extracted from the EHR and analyzed using Stata® 13.1 (StataCorp, College Station, TX). Means, medians, and confidence intervals were generated using Stata’s mean and proportion commands. We reported these means and 95% confidence intervals for each group and used these confidence intervals where we report significant differences between mutually exclusive groups of visits (i.e., falls captured by the ICD-9 definition versus falls missed by that definition).
Results
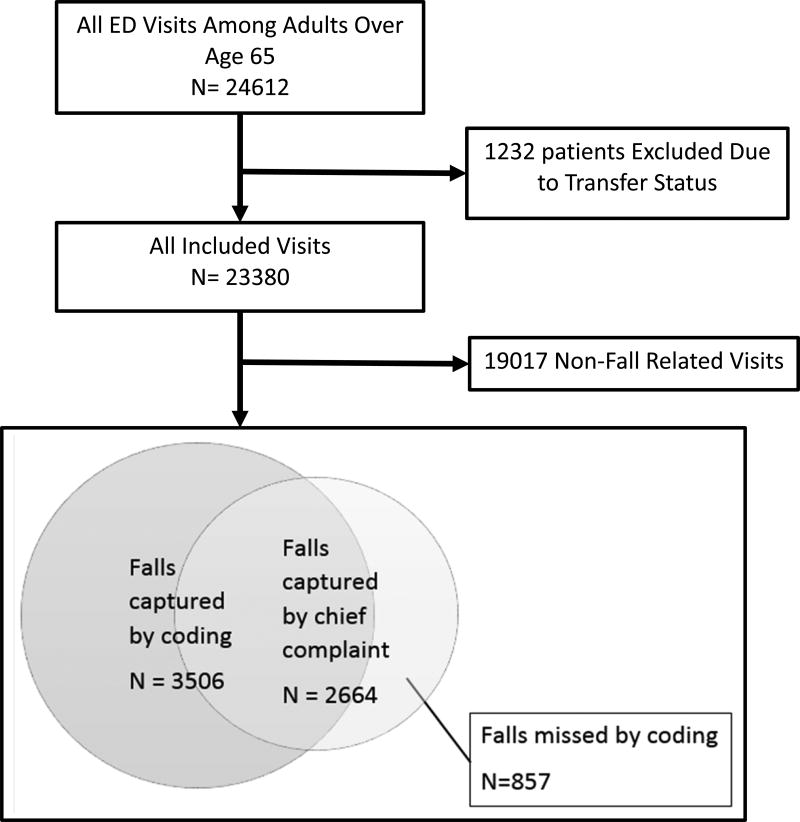
After selecting for older adult ED visits meeting study criteria, 23,880 patient visits were included in the analysis; Figure 1 describes patient attribution in the study. Using the most inclusive definition (either ICD-9 code OR chief complaint data indicating a fall), 4,363 ED visits were fall-related. Among these visits, 3,506 (80.4%) met the ICD-9 definition for a fall-related visit, while 2,664 (61.1%) met the chief complaint definition. 857 (19.6%) of fall visits were missed when only applying the ICD-9 definition.
Figure 1.
Patient Attribution
Table 1 displays extracted patient characteristics and outcomes stratified by fall definition. Demographic variables as well as mode of arrival and ESI triage acuity were similar between all fall groups. As compared to fall visits captured by the ICD-9 definition, those missed were associated with higher mean Elixhauser comorbidity counts at 3.1 (95%CI 2.9–3.2) vs. 2.5 (95%CI 2.4–2.6) and higher mean HCC scores at 1.6 (95%CI 1.5–1.7) vs. 1.3(95%CI 1.3–1.4)
Table 1.
Patient Characteristics and Outcomes, stratified by fall definition group
| All Older Adult ED Visits |
All Falls Captured Combined |
All Falls Captured by Coding |
All Falls Captured by Chief Complaint |
Falls captured by Chief complaint, missed by coding |
|
|---|---|---|---|---|---|
| N (%) | 23880 | 4363 (18.3) | 3506 (14.7) | 2664 (11.2) | 857 (3.6) |
| Age | 76.5 (76.4–76.6) | 78.7 (78.4–78.9) | 78.2 (77.9–78.5) | 80.5 (80.2–80.8) | 80.5 (79.9–81.1) |
| Gen (% Female) | 55.6 (54.9–56.1) | 61.0 (59.6–62.5) | 61.8 (60.2–63.4) | 62.4 (60.6–64.2) | 57.6 (54.3–60.9) |
| Race | |||||
| Unknown | 0.5 (0.4–0.6) | 0.5 (0.3–0.8) | 0.5 (0.3–0.8) | 0.4 (0.3–0.8) | 0.4 (0.1–1.1) |
| White | 91.5 (91.1–91.8) | 94.7 (94.0–95.3) | 94.8 (94.0–95.5) | 94.7 (93.7–95.5) | 94.2 (92.4–95.6) |
| Black | 4.0 (3.7–4.2) | 1.8 (1.5–2.3) | 1.6 (1.2–2.0) | 1.7 (1.2–2.2) | 2.9 (2.0–4.3) |
| Other | 0.2 (0.2–0.3) | 0.1 (0.1–0.3) | 0.1 (0.1–0.3) | 0.1 (0.0–0.3) | 0.1 (0.0–0.8) |
| Asian | 1.9 (1.8–2.1) | 1.1 (0.8–1.4) | 1.1 (0.8–1.5) | 1.1 (0.8–1.6) | 0.9 (0.5–1.9) |
| Hispanic | 1.6 (1.5–1.8) | 1.5 (1.2–1.9) | 1.5 (1.2–2.0) | 1.7 (1.3–2.3) | 1.4 (0.8–2.5) |
| North American Native | 0.3 (0.2–0.3) | 0.3 (0.2–0.5) | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) | 0.1 (0.0–0.8) |
| Insurance Status | |||||
| Medicaid/BadgerCare | 0.6 (0.5–0.7) | 0.4 (0.2–0.6) | 0.4 (0.2–0.7) | 0.3 (0.2–0.6) | 0.2 (0.1–0.9) |
| Medicare | 78.1 (77.6–78.6) | 76.2 (74.9–77.4) | 75.7 (74.3–77.1) | 77.9 (76.3–79.5) | 78.1 (75.2–80.7) |
| Commercial/Worker’s Comp | 11.8 (11.4–12.2) | 10.9 (10.0–11.9) | 11.0 (10.0–12.1) | 9.3 (8.2–10.4) | 10.6 (8.7–12.9) |
| Unknown | 9.5 (9.2–9.9) | 12.5 (11.6–13.6) | 12.9 (11.8–14.0) | 12.5 (11.3–13.8) | 11.1 (9.1–13.4) |
| Mode of Arrival | |||||
| Family or Self | 55.8 (55.1–56.4) | 35.0 (33.6–36.4) | 36.4 (34.8–38.0) | 27.6 (25.9–29.3) | 29.2 (26.2–32.3) |
| EMS | 43.9 (43.2–44.5) | 64.9 (63.4–66.3) | 63.4 (61.8–65.0) | 72.3 (70.6–74.0) | 70.7 (67.6–73.7) |
| Police | 0.3 (0.3–0.4) | 0.1 (0.1–0.3) | 0.1 (0.1–0.3) | 0.1 (0.0–0.3) | 0.1 (0.0–0.8) |
| ESI Triage Acuity Score | |||||
| 1 | 1.2 (1.0–1.3) | 1.9 (1.5–2.4) | 2.1 (1.7–2.6) | 1.4 (1.0–1.9) | 1.0 (0.5–2.0) |
| 2 | 33.0 (32.4–33.6) | 25.8 (24.6–27.2) | 26.5 (25.1–28.1) | 25.3 (23.7–27.0) | 23.0 (20.3–26.0) |
| 3 | 60.0 (59.3–60.6) | 64.8 (63.4–66.2) | 63.4 (61.8–65.0) | 68.0 (66.2–69.8) | 70.3 (67.2–73.6) |
| 4 | 5.6 (5.3–5.9) | 7.5 (6.7–8.3) | 7.9 (7.0–8.8) | 5.3 (4.5–6.2) | 5.6 (4.3–7.4) |
| 5 | 0.3 (0.2–0.4) | 0.0 (0.0–0.2) | 0.0 (0.0–0.2) | No Observation | No Observation |
| Mean Elixhauser Count | 2.8 (2.8–2.8) | 2.6 (2.5–2.7) | 2.5 (2.4–2.6) | 2.8 (2.7–2.9) | 3.1 (2.9–3.2) |
| Mean HCC score | 1.6(1.59–1.63) | 1.4(1.3–1.4) | 1.3(1.3–1.4) | 1.4(1.4–1.5) | 1.6(1.5–1.7) |
| 90-day mortality | 9.0 (8.7–9.4) | 9.3 (8.4–10.2) | 9.2 (8.3–10.2) | 10.3 (9.2–11.5) | 9.3 (7.6–11.5) |
| 30-day mortality | 4.9 (4.7–5.2) | 5.2 (4.6–5.9) | 5.3 (4.6–6.1) | 5.9 (5.0–6.8) | 5.0 (3.7–6.7) |
| Admission Rate | 50.7 (50.1–51.4) | 52.1 (50.6–53.6) | 54.4 (52.7–56.0) | 51.9 (50.0–53.8) | 42.9 (39.7–46.3) |
95% Confidence intervals are included in parentheses. Numbers represent percentages for all categorical variables and means for all continuous variables. ESI is the emergency severity index. HCC is the hierarchical condition category.
Overall, 30- and 90- day mortality was similar among all groups. Admission rate did vary by fall definition: 42.9% (95% CI 39.7–46.3) of encounters missed by the ICD-9 definition resulted in admission vs. 54.4% (95% CI 52.7–56.0) of encounters captured by ICD-9 definition. Patients missed by the ICD-9 definition did not significantly differ from those captured with regards to mortality. Given that falls missed by the ICD-9 definition were significantly more likely to be discharged, we further evaluated mortality among discharged patients, displayed in Table 2. Among these visits, the ICD-9 definition performed more poorly, missing 23.4% of falls as compared to the more inclusive definition. Within this population, there were no significant differences in mortality by group.
Table 2.
Mortality (by visit) among discharged patients, by fall definition group
| All Older Adult ED Visits Resulting in Discharge |
All Falls Captured Combined |
All Falls Captured by Coding |
All Falls Captured by Chief Complaint |
Falls missed by coding |
|
|---|---|---|---|---|---|
| N | 11716 | 2085 | 1598 | 1280 | 487 |
| 90-day mortality | 4.1 (3.8–4.5) | 5.8 (4.9–6.9) | 5.4 (4.4–6.7) | 7.4 (6.1–9.0) | 7.0 (5.0–9.6) |
| 30-day mortality | 1.4(1.2–1.7) | 2.1 (1.6–2.8) | 1.9 (1.4–2.7) | 3.1 (2.3–4.2) | 2.7 (1.6–4.5) |
95% confidence intervals in parentheses.
Discussion
In this single center retrospective study, we found that identifying fall-related ED visits from EHR data by combining ICD-9 diagnosis code and chief complaint resulted in 24.4% more potential fall encounters than using an ICD-9 diagnosis code-based strategy alone. We further found that the missed patients differed captured patients with regards to admission rates (i.e., missed patients were less likely to be admitted), but not mortality. Further, visits missed by the ICD-9 definition were associated with higher baseline patient comorbidity as assessed by both Elixhauser comorbidity count and HCC score. The ability to capture fall events based on EHR records will provide baseline data and targeting ability for future fall risk screening efforts in the ED.
Within the scope of falls research, these findings suggest that previous diagnosis code-based definitions of falls may significantly underestimate the true burden of disease. Furthermore, it appears that code-based definitions miss a significant number of fall patients who are discharged home as opposed to admitted to the hospital. Our study used text retrieval to find falls within the chief complaint field; while this does not represent a sophisticated language-based analysis (such as natural language processing), it points to the potential for such strategies to identify information from other text-based sources such as notes and radiology reports, likely with further ability to extract similarly useful information for defining research cohorts.
The use of code-based definitions to identify research cohorts is a longstanding practice in health services research, with well documented advantages and deficiencies.23 This practice can be problematic when applied to the ED setting, as discharge diagnoses often have poor concordance with ED patients’ reason for visit, need for admission, or further advanced care.24 Previous studies have examined the relatively poor performance of diagnosis codes in the ED generally,25 and for identifying common conditions seen in the ED such as concussion26 or sepsis.27 Code-based definitions are likely to perform particularly poorly in applications have this property; delirium, frailty, elder abuse, and other syndromes are similarly difficult to classify. In these cases, diagnosis codes are unlikely to estimate the true burden of disease accurately. The ICD-9 system utilizes “E” codes to document external causes of injuries (included in our definition), and ICD-10 keeps this system with analogous external cause of injury codes now represented with “V,” “W,” “X,” and “Y” prefixes. In theory, these codes should allow capture of causes of injury; unfortunately, depending on practice location, these codes are reported variably,28 and the transition from ICD-9 to ICD-10 has not resulted in a change in reporting requirements for these external cause codes.29 As limitations of using diagnosis code-based definitions to define research cohorts in the ED have been more widely recognized, there have also been calls to use chief complaint-based data to evaluate ED quality of care.18 Chief complaint offers a valuable additional source of data for identifying patients for research purposes.
The purpose of our study was to identify additional falls missed by diagnosis code-based definitions (as opposed to creating or validating a new definition). As such, we chose to compare chief complaint data to a previously used coding-based definition which utilized ICD-9 data. We reviewed several ICD-9-based definitions of falls, and intentionally selected a liberal definition, which likely lacked specificity for fall visits. The purpose of this choice was to intentionally bias the study towards the null hypothesis: by using a code- based definition with a wide net, we likely picked up fewer additional cases with a chief complaint-based definition than if we had compared to a more specific coding approach. Given this structure, we avoided analyzing and commenting on falls “missed” by the chief complaint definition, which may represent either true misses, or non-fall related visits included in our broad code-based definition.
Since the collection of our data, ICD-10 coding has replaced ICD-9 coding as the standard in the US. While this represents an advance in many areas, ICD-10 codes are conceptually similar to their ICD-9 predecessors, and we would not expect the underlying limitations (i.e. using diagnosis to identify mechanism) to change with regards to fall identification simply because the diagnoses are more accurate or detailed. Given that the purpose of this study was to detect falls missed by code-based definitions (as opposed to creating a new definition), we did not compare either definition to a “gold standard” fall definition. While neither definition is likely to be perfect, it is reasonable to assume that the vast majority of patients with a chief complaint of fall did indeed suffer a fall. As such, our main conclusion, that code-based definitions alone do not capture all falls, is likely unaffected.
Of note, our data is intentionally presented at the visit level, as opposed to patient level. We felt this was most appropriate for examining our primary outcome of per visit classification. Demographic and other data were also reported at this level for consistency. Some data elements, such as demographics and mortality, are more generally reported at the patient level and should not be interpreted as such within the setting of this study. For instance, reported per visit 30- and 90-day mortality for all older adults on a visit level does not correspond to patient level mortality in this population, as a single patient presenting four times in the 90 days leading up to death represents four separate visits within the database.
Our results suggest that the inclusion of chief complaint-based data in fall definitions can increase capture of patients in whom diagnosis codes alone do not reflect falls. Though an increased capture rate of patients who likely fell is a positive for study design, we did not formally evaluate the sensitivity and specificity of our definition, and any increase in capture rate likely increases the chance of false positives in a given definition. Furthermore, our additionally identified fall patients had a higher discharge rate than those not identified and likely represent a population with less severe injuries; the decision to use chief complaint data to increase patient identification for a given indication must be informed by consideration of how additionally identified patients will shape a study or sample cohort with regards to person-oriented outcomes being studied.30
From a broader standpoint, these findings highlight the value of chief complaint for the identification of clinically distinct groups of patients in the ED setting. Most ED care focuses on workups applied to undifferentiated patients and then applying a diagnosis, and thus ED-based research often focuses on cohorts of patients defined based on shared characteristics before specific diagnoses are assigned. Future studies using EHR data to define patient groups may benefit from incorporating chief complaint information, especially in settings such as fall, where populations are primarily defined by symptomatic or mechanistic factors which do not translate well to a single diagnosis or group thereof. This is particularly relevant at a time when EHR data is being harnessed and studied on a large scale in databases such as the American College of Emergency Physician’s Clinical Emergency Data Registry (CEDR). These findings are of interest not only to researchers, but to clinicians, educators, and policymakers, who when interpreting studies performed on older adults, particularly in the ED setting, need to be aware of the limitations inherent in applying health services research methodologies from other specialties to this population.
Conclusion
Examining chief complaint data revealed a subset of falls missed by an ICD-9 code-based definition, suggesting that the practice of defining falls based on coding underestimates the true burden of disease. Furthermore, patients missed by an ICD-9 code-based definition were less likely to have been admitted than those captured, identifying a potential bias among studies identifying falls based on diagnosis codes alone. These findings call attention to the value of using chief complaint information identify fall patients in the ED setting, whether it be for research, clinical care, or policy reasons.
Acknowledgments
This project was supported by grant number K08HS024558 from the Agency for Healthcare Research and Quality and K08DK111234 from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality nor the National Institutes of Health.
Footnotes
Prior Presentations: None
Conflict of Interest: None
Author Contributions: Patterson: study concept and design, data acquisition, analysis and interpretation, drafting and revision of manuscript. Smith: study design, data acquisition, analysis and interpretation, revision of manuscript. Repplinger: data analysis and interpretation, revision of manuscript. Pulia: data analysis and interpretation, revision of manuscript. Svenson: data analysis and interpretation. Kim: data analysis and interpretation. Shah: Study design, data analysis and interpretation, revision of manuscript.
References
- 1.Stalenhoef PA, Crebolder HFJJ, Knottnerus JA, et al. Incidence, risk factors and consequences of falls among elderly subjects living in the community: A criteria-based analysis. Eur J Pub Health. 1997;7:328–34. [Google Scholar]
- 2.Web-based Injury Statistics Query and Reporting System. [Accessed December 12, 2015];Centers for Disease Control and Prevention (online) 2015 Available at: http://www.cdc.gov/injury/wisqars/.
- 3.Stevens JA, Corso PS, Finkelstein EA, et al. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–5. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kenny R, Rubenstein LZ, Tinetti ME, et al. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services. 2016 Physician Quality Reporting System (PQRS) Measures Groups Specifications Manual. 2016. [Google Scholar]
- 6.Landis SE, Galvin SL. Implementation and assessment of a fall screening program in primary care practices. J Am Geriatr Soc. 2016;62:2408–14. doi: 10.1111/jgs.13137. [DOI] [PubMed] [Google Scholar]
- 7.Weigand JV, Gerson LW. Preventive care in the emergency department: should emergency departments institute a falls prevention program for elder patients? A systematic review. Acad Emerg Med. 2001;8:823–6. doi: 10.1111/j.1553-2712.2001.tb00214.x. [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg M, Carpenter CR, Bromley M, et al. Geriatric emergency department guidelines. Ann Emerg Med. 2014;63:e7–25. doi: 10.1016/j.annemergmed.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Carpenter CR, Avidan MS, Wildes T, et al. Predicting geriatric falls following an episode of emergency department care: a systematic review. Acad Emerg Med. 2014;21:1069–82. doi: 10.1111/acem.12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tiedemann A, Sherrington C, Orr T, et al. Identifying older people at high risk of future falls: development and validation of a screening tool for use in emergency departments. Emerg Med J. 2013;30:918–22. doi: 10.1136/emermed-2012-201783. [DOI] [PubMed] [Google Scholar]
- 11.Carpenter C, Scheatzle M, D'Antonio J, et al. Identification of Fall Risk Factors in Older Adult Emergency Department Patients. Acad Emerg Med. 2009;16:211–9. doi: 10.1111/j.1553-2712.2009.00351.x. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter CR, Griffey RT, Stark S, et al. Physician and Nurse Acceptance of Technicians to Screen for Geriatric Syndromes in the Emergency Department. West J Emerg Med. 2011;12:489–95. doi: 10.5811/westjem.2011.1.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donaldson MG, Khan KM, Davis JC, et al. Emergency department fall-related presentations do not trigger fall risk assessment: a gap in care of high-risk outpatient fallers. Arch Gerontol Geriatr. 2005;41:311–7. doi: 10.1016/j.archger.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 14.Carpenter CR, Shah MN, Hustey FM, et al. High Yield Research Opportunities in Geriatric Emergency Medicine: Prehospital Care, Delirium, Adverse Drug Events, and Falls. J Gerontol A Biol Sci Med Sci. 2011;66A:775–83. doi: 10.1093/gerona/glr040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olsen L, Aisner D, McGinnis JM, et al. The learning healthcare system : workshop summary. Washington, DC: National Academies Press; [Accessed April 1, 2017]. Roundtable on Evidence-Based Medicine. Available at https://www.nap.edu/catalog/11903/the-learning-healthcare-system-workshop-summary. [PubMed] [Google Scholar]
- 16.Kim SB, Zingmond DS, Keeler EB, et al. Development of an algorithm to identify fall-related injuries and costs in Medicare data. Inj Epidemiol. 2016;3:1. doi: 10.1186/s40621-015-0066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bohl AA, Phelan EA, Fishman PA, et al. How are the costs of care for medical falls distributed? The costs of medical falls by component of cost, timing, and injury severity. Gerontologist. 2012;52:664–75. doi: 10.1093/geront/gnr151. [DOI] [PubMed] [Google Scholar]
- 18.Griffey RT, Pines JM, Farley HL, et al. Chief Complaint-Based Performance Measures: A New Focus for Acute Care Quality Measurement. Ann Emerg Med. 2014;65(4):387–95. doi: 10.1016/j.annemergmed.2014.07.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 20. [Accessed Febuary 1, 2016];STEADI Initiative for Health Care Providers | STEADI - Older Adult Fall Prevention | CDC Injury Center. 2016 Available at http://www.cdc.gov/steadi/
- 21.Baumann MR, Strout TD. Triage of geriatric patients in the emergency department: validity and survival with the Emergency Severity Index. Ann of Emerg Med. 2007;49:234–40. doi: 10.1016/j.annemergmed.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 23.O'Malley KJ, Cook KF, Price MD, et al. Measuring Diagnoses: ICD Code Accuracy. Health Serv Res. 2016;40:1620–39. doi: 10.1111/j.1475-6773.2005.00444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raven MC, Lowe RA, Maselli J, et al. Comparison of presenting complaint vs discharge diagnosis for identifying" nonemergency" emergency department visits. JAMA. 2013;309:1145–53. doi: 10.1001/jama.2013.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howell SC, Wills RA, Johnston TC. Should diagnosis codes from emergency department data be used for case selection for emergency department key performance indicators? Aust Health Rev. 2014;38:38–43. doi: 10.1071/AH13026. [DOI] [PubMed] [Google Scholar]
- 26.Bazarian JJ, Veazie P, Mookerjee S, et al. Accuracy of mild traumatic brain injury case ascertainment using ICD-9 codes. Acad Emerg Med. 2006;13:31–8. doi: 10.1197/j.aem.2005.07.038. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim I, Jacobs IG, Webb SA, et al. Accuracy of International classification of diseases, 10th revision codes for identifying severe sepsis in patients admitted from the emergency department. Crit Care Resusc. 2012;14:112–8. [PubMed] [Google Scholar]
- 28.McKenzie K, Enraght-Moony EL, Walker SM, et al. Accuracy of external cause-of-injury coding in hospital records. Inj Prev. 2009;15:60–4. doi: 10.1136/ip.2008.019935. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services. [Accessed January 10, 2017];ICD-10-CM Classification Enhancements. 2016 Available at https://www.cms.gov/Medicare/Coding/ICD10/Downloads/ICD-10QuickRefer.pdf.
- 30.Hoffman JR, Carpenter CR. Guarding Against Overtesting, Overdiagnosis, and Overtreatment of Older Adults: Thinking Beyond Imaging and Injuries to Weigh Harms and Benefits. J Am Geriatr Soc. 2017 doi: 10.1111/jgs.14737. [DOI] [PubMed] [Google Scholar]