Abstract
OBJECTIVES
The purpose of this study was to determine the impact of different aortic clamping strategies on the incidence of cerebral embolic events during coronary artery bypass grafting(CABG).
METHODS
From 2012–2015, 142 patients with low-grade aortic disease (epiaortic ultrasound grade I /II) undergoing primary isolated CABG were studied. Those undergoing off-pump CABG were randomized to a partial clamp (n=36) or clampless facilitating device (CFD, n=36) strategy. Those undergoing on-pump CABG were randomized to a single (n=34) or double (n=36) clamp strategy. Transcranial Doppler ultrasonography (TCD) was performed to identify high intensity transient signals (HITS) in the middle cerebral arteries during periods of aortic manipulation. Neurocognitive testing was performed at baseline and 30-days postoperatively. The primary endpoint was total number of HITS detected by TCD. The Mann-Whitney test was performed to compare groups.
RESULTS
In the off-pump group, median total HITS were higher in the CFD group (30.0, IQR 22–43) compared to the partial clamp group (7.0, IQR 0–16) (p<0.0001). For the CFD group, median number of HITS for patients with one CFD was 12.5 (IQR 4–19) compared to 36 (IQR 25–47) for patients with >1 CFD (p=0.001). For the on-pump group, median total HITS were 10.0 (IQR 3–17) in the single-clamp group compared to 16.0 (IQR 4–49, p=0.10) in the double-clamp group. There were no differences in neurocognitive outcomes.
CONCLUSIONS
For patients with low-grade aortic disease, the use of CFDs resulted in more cerebral embolic events compared to partial clamping during off-pump CABG. A single-clamp strategy during on-pump CABG did not significantly reduce embolic events compared to a double-clamp strategy.
INTRODUCTION
Despite advances in no aortic-touch multi-arterial revascularization, extracorporeal perfusion techniques, and off-pump approaches to minimize adverse neurologic events, they remain a leading cause of morbidity associated with coronary artery bypass surgery (CABG). Adverse neurological events are frequently attributed to atheroembolism resulting from aortic manipulation1 which can occur with any event including aortic clamping, cannulation insertion and removal, and the initiation of bypass. Thus, it would seem intuitive that minimizing aortic manipulation would result in less cerebral embolism. Although this is one of the potential benefits of off-pump CABG, off-pump approaches frequently utilize some degree of aortic manipulation for construction of proximal aortocoronary anastomoses2,3.
Transcranial Doppler Ultrasonography (TCD) has been utilized to detect high intensity transient signals (HITS) in the middle cerebral arteries. This methodology is highly sensitive for cerebral microembolization, but the association with clinical outcomes and neurocognitive dysfunction has not been demonstrated. Most of the studies have been observational in nature and thus subject to bias and confounding; whereas others do not examine the spectrum of proximal aortic strategies with different revascularization options. Thus, the purpose of this randomized trial was to compare the impact of different aortic manipulation strategies on the number of cerebral embolic events during CABG.
METHODS
Trial Design and Oversight
This trial was a randomized, single center trial with seven participating surgeons with expertise in both off-pump (each surgeon having performed at least 100 off-pump cases) and on-pump CABG as well as the use of clampless facilitating devices (CFD) for construction of proximal aortocoronary anastomoses. Data collection and management were handled by the Cardiothoracic Center for Clinical Research at Emory University. The Institutional Review Board of Emory University reviewed and approved the study. The trial was monitored by an independent data and safety monitoring board.
Study Population
Patients scheduled for elective or urgent, first-time multivessel sternotomy CABG were eligible for enrollment. All patients underwent a routine and standardized preoperative evaluation by the attending surgeon and a mid-level provider including carotid artery ultrasound. Exclusion criteria included a history of preoperative stroke, preoperative or concomitant carotid endarterectomy, stenting, or known hemodynamically (>80%) significant stenosis, known left ventricular or left atrial thrombus, planned concomitant cardiac surgical procedure, salvage or emergency CABG, reoperative cardiac surgery, CABG with no planned aortocoronary proximal anastomoses, or the presence of preoperative intra-aortic balloon pump, and unwillingness or inability to provide consent. All patients provided written informed consent.
Randomization and Treatment
The study was designed to study and compare the effects of different strategies of construction of proximal anastomoses; it was not designed to compare off- versus on-pump CABG. The decision to perform off- vs. an on-pump CABG was based on the discretion of the operating surgeon. Randomization occurred intraoperatively after completion of sternotomy and epiaortic ultrasonography. Only patients with low grade ascending aortic disease (Grade I–II, Table 1) by epiaortic ultrasound were randomized regardless of whether an off- versus on-pump approach was selected by the operating surgeon4. Specifically, patients selected for off-pump CABG were randomized 1:1 to have proximal aorto-coronary anastomoses performed with a partial-occluding clamp or with a clampless facilitating device (CFD) (Heartstring Device, Maquet Cardiovascular LLC, San Jose, CA). Patients selected for on-pump CABG were randomized 1:1 to have proximal aorto-coronary anastomoses performed with a single-clamp or double-clamp (cross-clamp for cardioplegic arrest and partial- clamp for proximal anastomoses). A randomized block design was employed with blocks of 8; after epiaortic ultrasound confirmed grade I–II aortic disease, randomization assignment was revealed via an opaque envelope by the research coordinator. Patients that were determined intraoperatively to have Grade III–V ascending aortic disease by epiaortic ultrasound were excluded from randomization and the study. At an alpha level of 0.05, there would be 80% power to detect a treatment difference, if it exists, of 40 high intensity transient signals (HITS) with 31 patients per group using the Mann-Whitney test. With an attrition rate of 10% due to dropouts and possible technical problems, the plan was to recruit 34 patients in each group.
Table 1.
Epiaortic Ultrasound Grading System Used at Emory University
| Ultrasound Grade of Ascending Aorta |
Severity (atheroma thickness) |
Description |
|---|---|---|
| 1 | Normal | Intimal thickness < 2mm |
| 2 | Mild | Mild (focal or diffuse) intimal thickening of 2–3mm |
| 3 | Moderate | Atheroma < 3–5mm (no mobile/ulcerated components) |
| 4 | Severe | Atheroma > 5mm (no mobile/ulcerated components) |
| 5 | Complex | Grade 2, 3, or 4 atheroma plus mobile or ulcerated components |
Surgical Technique
All patients underwent sternotomy. Routine left internal mammary artery harvest was performed in all cases. Saphenous vein grafts were harvested using endoscopic techniques. Patients undergoing on-pump CABG underwent standard ascending aortic and right atrial cannulation for cardiopulmonary bypass. In patients randomized to a single-clamp strategy, proximal aortocoronary anastomoses were performed prior to release of the cross-clamp. In patients randomized to a double-clamp strategy, the cross-clamp was released after distal anastomoses, followed by application of a partial-clamp for construction of proximal anastomoses.
In patients undergoing off-pump CABG, distal anastomoses were performed using cardiac positioning and stabilizing devices. In patients randomized to partial-clamp, proximal aorto-coronary anastomoses were performed using a partial- clamp on the ascending aorta. In patients randomized to the CFD group, proximal anastomoses were performed using the Heartstring device.
Transcranial Doppler Ultrasonography
All patients underwent TCD evaluation to detect cerebral embolic signals during all periods of aortic manipulation using the Compumedics DWL system and the QL software (Compumedics, Germany). The TCD monitoring measurements were as follows for the on-pump group: 1) cannulation; 2) initiation of cardiopulmonary bypass; 3) aortic cross-clamping; 4) removal of aortic cross-clamp; 5) application of a partial-clamp (double-clamp group); 6) removal of partial-clamp (double-clamp group); 7) removal of aortic cannula. For the off-pump group, TCD monitoring measurements were as follows: 1) placement and removal of each CFD; or 2) placement and removal of the partial-clamp. The DWL system is a fully digital system that uses an automated event detector to identify HITS and is powered by the Doppler M-Mode. The Doppler M-Mode simultaneously receives and analyzes Doppler signals from a predefined range of depths. This allows emboli detection to be verified when an embolus passes through various depths. Microemboli traveling along an insonated vessel will appear as HITS on the TCD spectrum. The system uses a 2.0 MHz probe with a power range of 20–100mW. Initially, an adequate temporal window was confirmed by locating intracranial arterial signals. The right middle cerebral artery was insonated at a depth between 50–65mm. The middle cerebral artery was verified through visualization of the depth and flow direction. The spectra from each period of insonation was saved to the hard drive of the computer. The number and timing of HITS were monitored and recorded by dedicated research coordinators who were trained and experienced in TCD (e-video). Differentiation between solid and gaseous HITS was not performed because the overall clinical accuracy of dual frequency and frequency modulation analyses were not able to accurately separate gas from solid emboli5–7. All TCD data were reviewed and adjudicated by a staff neurologist at Emory University with expertise in TCD ultrasonography who was blinded to the treatment group. False positive recordings that were recorded as HITS by the software were identified by our neurologist and excluded in the analysis.
Neurocognitive Assessment
Neurocognitive function was measured preoperatively and 30-days postoperatively. Selection of the test battery likely to be sensitive to cognitive deficits in a cardiac surgery population was guided by previous studies of neuropsychological outcomes following cardiac surgery8,9 as well as research in our own laboratory10. For this assessment, CNS Vital Signs (CNSVS, Morrisville, NC) computerized neurocognitive testing was utilized for the majority of patients. The neuropsychological testing was changed from The Repeatable Battery for Neuropsychological Status (RBANS) testing to CNSVS after the first 25 randomized patients in order to improve standardization of testing through a computerized administration. Eliminating the hand-written RBANS test reduced potential variations in test administration among nurse coordinators. Neuropsychological testing was administered by clinical coordinators and scored either by computer (CNSVS) or neuropsychological technicians (RBANS) under the supervision of an experienced neuropsychologist. The CNSVS scoring algorithm detects normatively rare scores, which could reflect actual poor cognitive performance, but could also be due to poor effort, subject distractibility, or other factors that potentially invalidate the scores. As we could not distinguish between these causes of normatively out-of-range scores, we excluded all such potentially invalid scores from analyses.
The change from RBANS to CNSVS required us to exclude the neuropsychological data on individual RBANS subtests from the initial 25 subjects as scores were not on a comparable scale as CNSVS subtests. This reduced the sample size on which sub-test neuropsychological data was available and lowered statistical power. Nonetheless, the improved standardization of test administration likely increased the reliability of available data. The RBANS and CNSVS both include a total score reflecting overall neuropsychological performance which is scaled comparably across the two batteries. We were able to include either the RBANS or CNSVS total score in a single analysis of overall neuropsychological performance across groups.
Statistical Analysis
Transcranial Doppler Ultrasonography Outcomes
For power analysis the expected number of HITS in each group was estimated to be 50 for CFD, 90 for partial-clamp, 100 for single-clamp, and 160 for double-clamp based on pilot data11 for off-pump CABG as well as previously published reports for on-pump CABG12. For the off-pump group, given a significance level of 0.05, we would have 80% power to detect a treatment difference of 40 HITS with 31 patients per group using the Mann-Whitney test. Assuming an attrition rate of 10% due to dropouts and technical problems, 34 patients were needed in both the CFD and partial-clamp groups. For the on-pump group, assuming a significance level of 0.05, we would have 80% power to detect a treatment difference of 50 HITS with 31 patients per group. Assuming an attrition rate of 10% due to dropouts and technical problems, 34 patients would be needed in both the single- and double-clamp groups.
In the two separate studies, CFD and partial clamp for off-pump CABG and single and double-clamp for on-pump CABG, the same data analyses were performed. Numeric variables were summarized using the mean ± standard deviation (or median [interquartile range], as appropriate). Categorical variables were summarized as count [percentage]. Group averages were compared using the student’s t-test (or Mann-Whitney test, as appropriate). Group proportions were compared using the chi-square test (or Fisher's exact test, as appropriate). To assess the difference in the average number of HITS between groups, the Mann-Whitney test was conducted. To compare graphically HITS distributions, box plots were drawn after log transforming the number of HITS. Log transformation compresses the scale for high values and stretches the scale for low values and provides a better visual comparison between two right-skewed distributions. Comparative analysis of the total number of HITS between CFD and partial clamp, as well as between single-clamp and double-clamp, were intention-to-treat. Secondary questions comparing, for example, one CFD and more than one CFD were as-treated. Tests of hypotheses were two-sided, and a significance level of 0.05 was used throughout. All data analyses were performed using SAS 9.4.
Neurocognitive Testing
Invalid CNSVS scores on given variable were excluded from analysis. All planned comparisons were conducted on pre-treatment and post-treatment raw and age-adjusted scaled scores, as well as change scores (pre-treatment score subtracted from post-treatment score).
RESULTS
Enrollment and Patient Characteristics
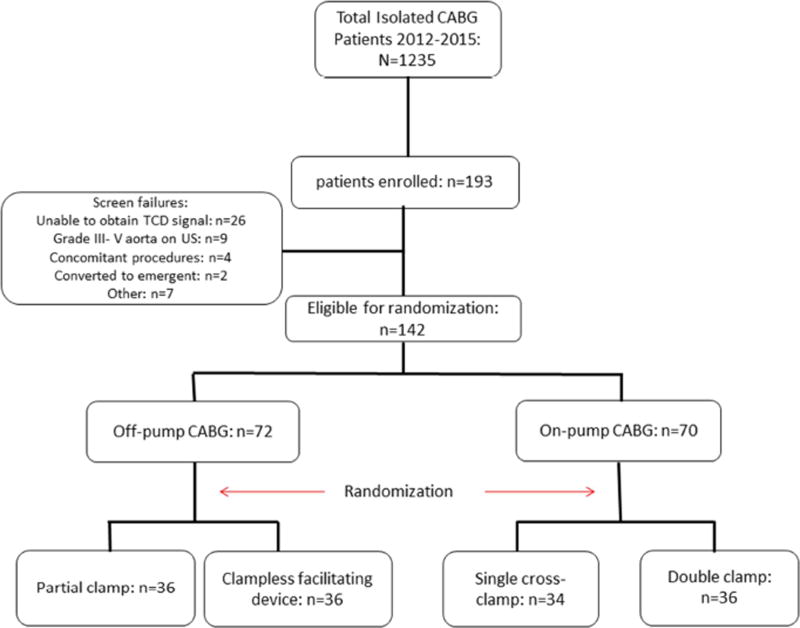
Between 2012 and 2015, 193 patients were enrolled and 142 patients underwent randomization. For the patients enrolled, the main reasons for exclusion were the inability to obtain a TCD signal over the MCA and a Grade III-V aorta on epiaortic ultrasound (Figure 1). In the off-pump group, 72 patients were randomized to have proximal aortocoronary anastomoses performed using either a CFD or a partial-clamp. In the on-pump group, 70 patients were randomized to either a single cross-clamp or double-clamp strategy for construction of aortocoronary proximal anastomoses. Baseline characteristics were similar between groups (Table 2). For randomized patients in the on-pump group, all patients received the treatment that they were assigned. For all patients in the single-clamp group, there was no additional clamping after release of the cross-clamp. For all patients in the double-clamp group, patients received only one application of the cross-clamp and only one application of the partial-clamp. For the off-pump group, 2 patients that were randomized to partial-clamp received CFDs. Two patients that were randomized to the CFD group received a partial-clamp. Thirty-day postoperative follow-up was complete in 129 patients (91%).
Figure 1.
Consort diagram of trial enrollment, randomization, and treatment received.
Table 2.
Patient Perioperative Characteristics
| Off-pump CABG | On-Pump CABG | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| CFD (n=36) |
Partial Clamp (n=36) |
P value |
Single Clamp (n=34) |
Double Clamp (n=36) |
P value |
|
| Age | 60.8 ± | 60.6 ± 9.2 | 0.93 | 62.3 ± 7.8 | 61.1 ± 8.6 | 0.54 |
| Female | 8 (22.2%) | 10 (27.8%) | 0.59 | 6 (17.6%) | 5 (13.9%) | 0.67 |
| Caucasian | 28 | 21 (58.3%) | 0.08 | 25 (73.5%) | 26 (72.2%) | 0.90 |
| Diabetes | 18 | 22 (61.1%) | 0.34 | 13 (38.2%) | 14 (38.9%) | 0.96 |
| NSTEMI | 17 | 13 (36.1%) | 0.34 | 7 (21.2%) | 10 (28.6%) | 0.48 |
| CCS Angina 3/4 | 19 | 20 (57.1% | 0.73 | 21 (70.0%) | 20 (62.5%) | 0.53 |
| NYHA III/IV | 0 | 2 (5.9%) | 0.22 | 2 (6.7%) | 4 (12.5%) | 0.53 |
| EF | 49.5 ± | 51.3 ± 14.4 | 0.61 | 52.6 ± 11.5 | 52.3 ± 12.1 | 0.93 |
| Renal insufficiency | 2 (5.6%) | 4 (11.1%) | 0.53 | 4 (11.8%) | 5 (13.9%) | 0.83 |
| Dyslipidemia | 30 | 32 (88.9%) | 0.50 | 32 (94.1%) | 29 (80.6%) | 0.10 |
| Hypertension | 31 | 34 (94.4%) | 0.27 | 27 (79.4%) | 26 (72.2%) | 0.48 |
| Smoker | 21 | 15 (41.7%) | 0.16 | 21 (61.8%) | 14 (38.9%) | 0.06 |
| Previous_PCI | 11 | 11 (30.6%) | 1.00 | 13 (38.2%) | 5 (13.9%) | 0.02 |
| COPD | 3 (8.3%) | 2 (5.6%) | 0.75 | 4 (11.8%) | 1 (2.8%) | 0.17 |
| PVD | 1 (2.8%) | 2 (5.6%) | 0.68 | 1 (2.9%) | 2 (5.6%) | 0.68 |
| Number of Diseased | 3.1 ± 0.7 | 3.0 ± 0.7 | 0.52 | 3.3 ± 0.8 | 3.5 ± 0.8 | 0.27 |
| Distal Anastomoses | 3.2 ± 0.7 | 3.0 ± 0.8 | 0.15 | 3.4 ± 0.7 | 3.5 ± 0.8 | 0.42 |
| Proximal Anastomoses | 1.8 ± 0.6 | 1.6 ± 0.6 | 0.11 | 2.1 ± 0.8 | 2.1 ± 0.8 | 0.98 |
CCS – Canadian Cardiovascular Society; CFD – clampless facilitating device; COPD – chronic obstructive pulmonary disease; NYHA – New York Heart Association; PCI – percutaneous coronary intervention; PVD – peripheral vascular disease
Clinical Outcomes
There was no 30-day mortality, postoperative myocardial infarction, or deep sternal infections in any group. Superficial sternal infections occurred in 3 (8.3%) patients in the partial-clamp group and 2 (5.6%) in the double-clamp group. Two postoperative strokes occurred in the single-clamp group compared to none in the other groups for an overall stroke rate of 1.4%. Both of these strokes occurred in extubated, stable patients after an initial normal postoperative neurologic exam on postoperative day one. The number of HITS in these two patients were not outliers compared to the other results from other patients (10 and 43 HITS). Postoperative atrial fibrillation occurred in 7 (19.4%) for CFD, 10 (27.8%) for partial-clamp, 6 (17.7%) for single-clamp, and 8 (22.2%) for double-clamp. The number of patients who received blood transfusions intra- or postoperatively was 2 (5.6%) for CFD, 4 (11.1%) for partial-clamp, 5 (14.7%) for single-clamp, and 6 (16.7%) for double-clamp. The overall incidence of postoperative renal failure was 0 for CFD, 1 (2.8%) for partial-clamp, 0 for single-clamp, and 1 (2.8%) for double-clamp. Thirty-day hospital readmission occurred in 3 (8.6%) for CFD, 2 (5.7%) for partial-clamp, 0 for single-clamp, and 3 (8.3%) for double-clamp.
Transcranial Ultrasound Detected Cerebral Embolic Events
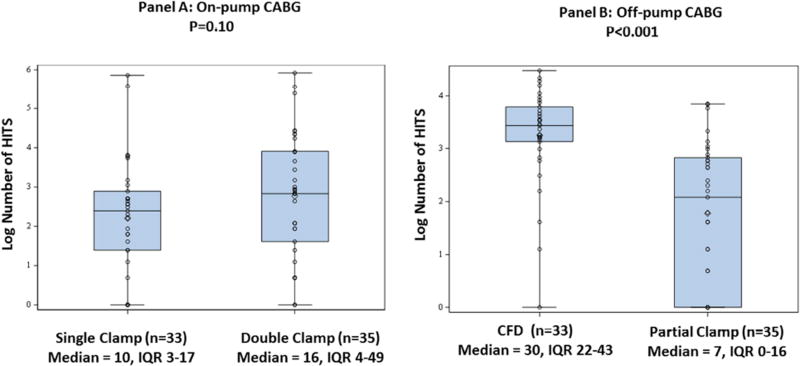
For the on-pump CABG group, TCD data was complete for 33/34 (97%) single-clamp patients and 35/36 (97%) double-clamp patients. In the intention-to-treat analysis, the median number of HITS detected during all periods of aortic manipulation was 10 (IQR 3–17) for the single-clamp group versus 16 (4–49) for the double-clamp group (p=0.10) (Figure 2a).
Figure 2.
ITT Analysis of HITS Data. Panel A: On-pump CABG: Single versus double clamp; Panel B: Off-pump CABG: Clampless facilitating device versus partial clamp. The number of HITS was log-transformed to compress the scale for high values and stretch the scale for low values, allowing a better visual comparison between two right-skewed distributions.
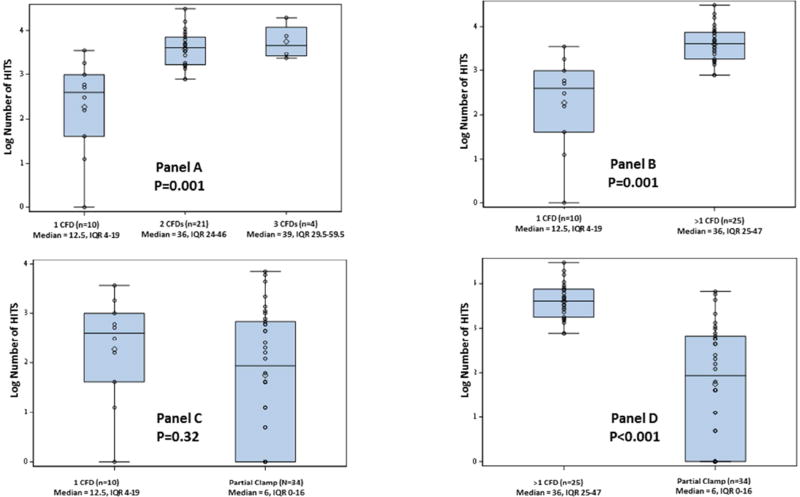
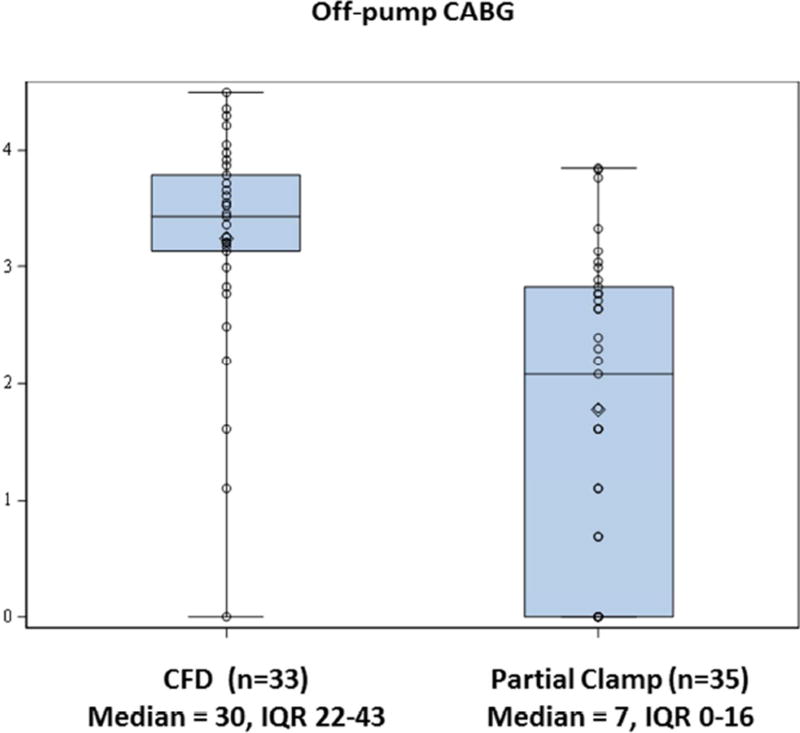
For the off-pump group, TCD data was complete for 35/36 (97%) partial-clamp patients and 33/36 (92%) CFD patients. The median number of HITS detected during all periods of aortic manipulation was 30 (IQR 22–43) for the CFD group versus 7 (IQR 0–16) for the partial-clamp group (p<0.001) (Figure 2b). For patients undergoing off-pump CABG with CFDs for construction of proximal anastomoses, the effect on HITS was positively related to the number of devices used (Figure 3a–d).
Figure 3.
As-treated Analysis of HITS Data in Off-pump CABG. Panel A: Number of clampless facilitating devices used on high intensity transient signals; Panel B: 1 clampless facilitating device vs more than 1 clampless facilitating device; Panel C: 1 clampless facilitating device vs partial clamp; Panel D: More than 1 clampless facilitating device vs partial clamp. The number of HITS was log-transformed to compress the scale for high values and stretch the scale for low values, allowing a better visual comparison between two right-skewed distributions.
Neurocognitive function
Exclusion of invalid CNSVS scores unfortunately reduced sample sizes available for some analyses. Loss of data due to invalid scores was comparable across groups, so this factor did not introduce a systematic bias. Utilizing available valid data, there were no statistically significant between group differences on any of the CNSVS domain scores preoperatively (Appendix). The groups did differ significantly in the pre-surgery CNSVS or RBANS Total Score, with the double-clamp group showing a higher score than the other patient groups. Hence, the preoperative total score was used as a covariate in analyses of the corresponding postoperative scores in the on-pump group. In the analysis of both raw and age-adjusted (as well as covariate adjustment for the on-pump group) postoperative and change scores, no comparisons approached statistical significance.
DISCUSSION
Because of the large number of patients that would be required to demonstrate a difference in a postoperative stroke, a randomized trial with stroke as the primary outcome was impractical. In this study, the number of HITS detected during TCD ultrasonography was utilized as a surrogate for cerebral embolism and was the primary outcome.
Wolf and coworkers used TCD to detect cerebral microembolization in 42 patients undergoing off-pump CABG13. There was no difference in total microemboli between the CFD group and the partial-clamp group, but there were significantly more solid microemboli in the partial-clamp group. Liu and associates also utilized TCD in an prospective observational study and found significantly higher microemboli in patients undergoing on-pump compared to off-pump CABG (median number of HITS 430 vs. 2, p<0.001)12. In a randomized study, Motallebzadeh and colleagues reported 1,605 embolic signals in on-pump compared to 9 in off-pump patients with a partial-clamp14. Other studies have been relatively consistent with the above reports15,16.
The main findings of this study can be summarized as follows: For patients undergoing CABG with low-grade aortic disease determined by epiaortic ultrasonography, 1) there was no difference in cerebral embolic events for on-pump patients undergoing a single-clamp technique compared to a double-clamp technique; 2) more cerebral embolic events occurred when CFDs were used compared to a partial-clamp for off-pump CABG patients; and 3) the effect of using CFDs on cerebral embolic events was directly related to the number of devices used. Each insertion and removal of the device, much like a partial-clamp, is associated with a level of cerebral microembolization. These results also suggest that the use of CFDs is another form of aortic manipulation and may not completely eliminate the risk of cerebral embolism. This study also contradicts prior reports which have shown a benefit using CFDs in lieu of partial-clamping in all off-pump patients.
Observational analyses17, including one from our own institution18, have shown a benefit from minimizing or avoiding aortic manipulation. Emmert and colleagues found a significant reduction in stroke (0.7% vs. 2.3%) with the use of the CFDs compared to a partial-clamp in off-pump patients19.
The discrepancies noted between the aforementioned studies and current one can be explained by several differences. First, the ubiquitous use of epiaortic ultrasound in this trial helped to significantly reduce selection bias and confounding based on the burden of aortic disease. Therefore, patients that were selected to on-pump or off-pump based on the discretion of the operating surgeon and then randomized to the aortic manipulation strategy were more likely to have a similar level of atheroembolic risk compared to observational analyses that neither account for selection bias nor burden of aortic disease. The benefit of CFDs compared to partial-clamping that has been observed in other studies may be partially related to their use in patients with varying levels of advanced aortic disease and surgeon selection. In our institution, patients that were identified to have advanced aortic disease (Epiaortic U/S grade 3–5) were not eligible for randomization because equipoise does not exist in our practice about how to manage these patients-we do not clamp the aorta and either use CFDs or in situ arterial grafts alone or as inflow for other conduits. Furthermore, there may have been more HITS in the CFD group compared to the partial-clamp group because there were simply more measurement occasions since 25 CFD patients had more than one CFD used (4 measurement occasions versus 2 in the partial clamp group). In addition, because of the intricacies associated with TCD analysis, a dedicated neurologist with expertise in TCD reviewed and adjudicated our TCD findings. Similarly, based on his analysis (AA) and previous reports5,6, we did not feel that we could accurately separate gaseous from solid emboli in this study. Finally, randomizing a large number of patients in this study minimizes confounding that may exist in observational retrospective and prospective cohort studies despite the use of advanced statistical analyses such as propensity-score matching.
Similar to other studies12,14,20, we failed to find a correlation between neurocognitive testing and cerebral microembolization. It is possible that cerebral microemboli that are detected by TCD do not result in persistent neurocognitive dysfunction, and that properties such as size and composition are more important that actual number21.
Study Limitations
The main study limitation was the use of TCD as a surrogate for cerebral adverse events. Its limitations are well known and include no proven correlation with adverse neurologic clinical events, difficulty with data capture during surgery, difficulty differentiating artifacts from microembolic events, and difficulty distinguishing gaseous from solid microemboli. Diffusion weighted MRI would have strengthened this study but was cost-prohibitive. Use of a dedicated neuropsychometrist to perform neurocognitive testing may have improved the ability to detect subtle differences in cognitive impairment between groups.
The sample size calculations were derived from TCD data from previously published reports and preliminary data at our own institution (for off-pump CABG)11,12. However, the number of HITS observed in this study was far lower than anticipated in any of the groups. This raises the possibility of a Type II error in the on-pump comparison because the study was not powered to detect a smaller effect size. The main reason that HITS were likely lower in all groups in our study is that our TCD recordings were reviewed and adjudicated by neurologist with expertise in TCD. Many signals that were labeled as HITS by the computer software were in fact false positive readings.
CONCLUSIONS
There was no significant difference with the use of two clamps compared to one for patients undergoing on-pump CABG and there was no advantage of using CFDs compared to a partial-clamp for patients undergoing off-pump CABG. Therefore, for off-pump patients with grade I–II aortic disease requiring aortocoronary proximal anastomoses, our recommendation is to utilize partial-clamping, especially when multiple proximal anastomoses are performed. For patients undergoing on-pump CABG, either a single- or a double-clamp strategy can be performed in patients with grade I–II aortic disease, depending on surgeon preference.
Supplementary Material
E-Video. Video of actual recording obtained with TCD measurement during clamp removal. The sounds interspersed during the pulse wave recordings are recorded as HITS by the computerized software program.
Central Picture.
Off-pump CABG: Median HITS with clampless facilitating device versus partial clamp
CENTRAL MESSAGE.
Patients with low-grade aortic disease undergoing off-pump CABG had more embolic events with CFDs than with partial clamping. On-pump patients had comparable results with single or double clamping.
PERSPECTIVE STATEMENT.
Aortic clamping during CABG surgery is associated with cerebral atheroembolism which is likely responsible for increased periprocedural stroke risk in patients undergoing CABG. The findings of this study support the use of traditional clamping methods during on- or off-pump CABG for patients with low-grade aortic disease.
Acknowledgments
Funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health; NIH Award Number 5K23HL105892-05.
Supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1TR000454. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ABBREVIATIONS
- CABG
coronary artery bypass grafting
- TCD
transcranial Doppler ultrasonography
- HITS
high intensity transient signals
- CFD
clampless facilitating device
- RBANS
The Repeatable Battery for Neuropsychological Status
- ANOVA
one-way analysis of variables
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the 96th Annual Meeting of The American Association for Thoracic Surgery, Baltimore, Maryland, May 17th, 2016
Conflict of Interest:
Michael E. Halkos, MD – Maquet Cardiovascular – consultant
None of the other authors have any relevant disclosures or conflicts of interest
This clinical trial is registered with clinicaltrials.gov # NCT01502683.
References
- 1.Filsoufi F, Rahmanian PB, Castillo JG, Bronster D, Adams DH. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann Thorac Surg. 2008;85(3):862–870. doi: 10.1016/j.athoracsur.2007.10.060. [DOI] [PubMed] [Google Scholar]
- 2.Diegeler A, Borgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med. 2013;368(13):1189–1198. doi: 10.1056/NEJMoa1211666. [DOI] [PubMed] [Google Scholar]
- 3.Lamy A, Devereaux PJ, Yusuf S. Off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. 2013;369(2):196. doi: 10.1056/NEJMc1306329. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein SA, Evangelista A, Abbara S, et al. Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging: endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2015;28(2):119–182. doi: 10.1016/j.echo.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Darbellay GA, Duff R, Vesin JM, et al. Solid or gaseous circulating brain emboli: are they separable by transcranial ultrasound? J Cereb Blood Flow Metab. 2004;24(8):860–868. doi: 10.1097/01.WCB.0000126235.54306.FA. [DOI] [PubMed] [Google Scholar]
- 6.Markus HS, Punter M. Can transcranial Doppler discriminate between solid and gaseous microemboli? Assessment of a dual-frequency transducer system. Stroke. 2005;36(8):1731–1734. doi: 10.1161/01.STR.0000173399.20127.b3. [DOI] [PubMed] [Google Scholar]
- 7.Banahan C, Rogerson Z, Rousseau C, Ramnarine KV, Evans DH, Chung EM. An in vitro comparison of embolus differentiation techniques for clinically significant macroemboli: dual-frequency technique versus frequency modulation method. Ultrasound in medicine & biology. 2014;40(11):2642–2654. doi: 10.1016/j.ultrasmedbio.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammon JW, Stump DA, Butterworth JF, et al. Coronary artery bypass grafting with single cross-clamp results in fewer persistent neuropsychological deficits than multiple clamp or off-pump coronary artery bypass grafting. Ann Thorac Surg. 2007;84(4):1174–1178. doi: 10.1016/j.athoracsur.2007.04.100. discussion 1178–1179. [DOI] [PubMed] [Google Scholar]
- 9.Hammon JW, Stump DA, Butterworth JF, et al. Single crossclamp improves 6-month cognitive outcome in high-risk coronary bypass patients: the effect of reduced aortic manipulation. J Thorac Cardiovasc Surg. 2006;131(1):114–121. doi: 10.1016/j.jtcvs.2005.08.057. [DOI] [PubMed] [Google Scholar]
- 10.Puskas JD, Stringer A, Hwang SN, et al. Neurocognitive and neuroanatomic changes after off-pump versus on-pump coronary artery bypass grafting: long-term follow-up of a randomized trial. J Thorac Cardiovasc Surg. 2011;141(5):1116–1127. doi: 10.1016/j.jtcvs.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 11.El Zayat H, Puskas JD, Hwang S, et al. Avoiding the clamp during off-pump coronary artery bypass reduces cerebral embolic events: results of a prospective randomized trial. Interact Cardiovasc Thorac Surg. 2012;14(1):12–16. doi: 10.1093/icvts/ivr004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu YH, Wang DX, Li LH, et al. The effects of cardiopulmonary bypass on the number of cerebral microemboli and the incidence of cognitive dysfunction after coronary artery bypass graft surgery. Anesth Analg. 2009;109(4):1013–1022. doi: 10.1213/ane.0b013e3181aed2bb. [DOI] [PubMed] [Google Scholar]
- 13.Guerrieri Wolf L, Abu-Omar Y, Choudhary BP, Pigott D, Taggart DP. Gaseous and solid cerebral microembolization during proximal aortic anastomoses in off-pump coronary surgery: the effect of an aortic side-biting clamp and two clampless devices. J Thorac Cardiovasc Surg. 2007;133(2):485–493. doi: 10.1016/j.jtcvs.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Motallebzadeh R, Bland JM, Markus HS, Kaski JC, Jahangiri M. Neurocognitive function and cerebral emboli: randomized study of on-pump versus off-pump coronary artery bypass surgery. Ann Thorac Surg. 2007;83(2):475–482. doi: 10.1016/j.athoracsur.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Scarborough JE, White W, Derilus FE, et al. Combined use of off-pump techniques and a sutureless proximal aortic anastomotic device reduces cerebral microemboli generation during coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;126(5):1561–1567. doi: 10.1016/s0022-5223(03)01039-0. [DOI] [PubMed] [Google Scholar]
- 16.Abu-Omar Y, Balacumaraswami L, Pigott DW, Matthews PM, Taggart DP. Solid and gaseous cerebral microembolization during off-pump, on-pump, and open cardiac surgery procedures. J Thorac Cardiovasc Surg. 2004;127(6):1759–1765. doi: 10.1016/j.jtcvs.2003.09.048. [DOI] [PubMed] [Google Scholar]
- 17.Misfeld M, Brereton RJ, Sweetman EA, Doig GS. Neurologic complications after off-pump coronary artery bypass grafting with and without aortic manipulation: meta-analysis of 11,398 cases from 8 studies. J Thorac Cardiovasc Surg. 2011;142(2):e11–17. doi: 10.1016/j.jtcvs.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 18.Moss E, Puskas JD, Thourani VH, et al. Avoiding aortic clamping during coronary artery bypass grafting reduces postoperative stroke. J Thorac Cardiovasc Surg. 2015;149(1):175–180. doi: 10.1016/j.jtcvs.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Emmert MY, Seifert B, Wilhelm M, Grunenfelder J, Falk V, Salzberg SP. Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2011;142(6):1499–1506. doi: 10.1016/j.jtcvs.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 20.Van Dijk D, Jansen EW, Hijman R, et al. Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomized trial. JAMA. 2002;287(11):1405–1412. doi: 10.1001/jama.287.11.1405. [DOI] [PubMed] [Google Scholar]
- 21.van Dijk D, Kalkman CJ. Why are cerebral microemboli not associated with cognitive decline? Anesth Analg. 2009;109(4):1006–1008. doi: 10.1213/ANE.0b013e3181b5af06. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
E-Video. Video of actual recording obtained with TCD measurement during clamp removal. The sounds interspersed during the pulse wave recordings are recorded as HITS by the computerized software program.