Abstract
This study investigates the association between exposure to prospectively-substantiated childhood maltreatment between 0 to 14 years of age and lifetime cannabis use, abuse and dependence reported at 21 years. Data were taken from 2526 (51.6% female) participants in the Mater Hospital-University of Queensland Study of Pregnancy, a pre-birth, prospective, cohort study. Prospectively-substantiated cases of childhood maltreatment, reported to the government child protection agencies between 0 and 14 years of age, were linked to CIDI DSM-IV self-report data from the 21-year follow-up. Exposure to any childhood maltreatment, and childhood neglect in particular, predicted subsequent cannabis abuse with adjusted odds ratios (AORs) of 1.79 and 2.62, respectively. Any childhood maltreatment, physical abuse, emotional abuse and neglect predicted cannabis dependence with AORs of 2.47, 2.81, 2.44 and 2.68, respectively. The associations for an early age of onset of cannabis abuse and dependence were significant and consistent for maltreated children. In addition, frequency of maltreatment substantiations predicted cannabis abuse, dependence and an early age of onset of these disorders. The AORs for cannabis ever use without any DSM-IV cannabis disorder were 1.78 for any maltreatment and 2.15 for emotional abuse. Any childhood maltreatment and neglect predicted lifetime ever cannabis use, as well as cannabis use disorder. There was little evidence for any interaction between gender and different forms of childhood maltreatment and its association with cannabis use disorders. Physical abuse, emotional abuse and neglect, as well as multiple episodes of maltreatment independently predicted cannabis use disorders.
Keywords: Childhood abuse, neglect, cannabis use disorders, longitudinal study
1. Introduction
Childhood maltreatment including sexual, physical, emotional abuse and neglect (Gilbert et al., 2009) and substance use disorders, including cannabis abuse and dependence, are public health problems experienced by youth (Tonmyr et al., 2010) in both developed (Atakan, 2008) and developing (Longman-Mills et al., 2013) regions of the world (Feigin, 2016). Although there is some evidence for an association between childhood maltreatment and adolescent cannabis use, little is known about the independent effects of specific forms of childhood maltreatment, particularly neglect, as well as the frequency or intensity of maltreatment.
There is emerging evidence, largely from retrospective studies of an association between childhood maltreatment and adolescent cannabis abuse or dependence, particularly when the maltreatment occurs at an early age (Aas et al., 2014; Baiden et al., 2014; Compton et al., 2004; Duncan et al., 2008; Longman-Mills et al., 2013). For example, self-reported experiences of sexual abuse have been associated with higher rates of cannabis use in adolescents (Longman-Mills et al., 2013), with a twofold likelihood of cannabis abuse and dependence in sexually abused children, even after controlling for offspring gender, alcohol use disorders and conduct disorder (Duncan et al., 2008). This association has also been observed in clinical patients with diagnosed mental health morbidities (Aas et al., 2014; Baiden et al., 2014; Compton et al., 2004). Similarly, physical (Baiden et al., 2014; Compton et al., 2004) and emotional (Aas et al., 2014) abuse have been associated with cannabis use (Baiden et al., 2014), abuse (Aas et al., 2014) and dependence (Compton et al., 2004) in patients aged between 12 and 29 years with mental health disorders (Baiden et al., 2014) such as bipolar disorders (Aas et al., 2014) and schizophrenia (Compton et al., 2004). The temporal sequence and directionality of the association between experiences of maltreatment and cannabis use is uncertain because of the cross-sectional design of these studies. People with early cannabis use disorders may experience higher levels of maltreatment and may have higher rates of subsequent mental health disorders. More generally, previous studies have reported an inconsistent association both for physical (Longman-Mills et al., 2013) and emotional (Baiden et al., 2014; Longman-Mills et al., 2013) abuse, and have not considered childhood neglect as a potential predictor (Aas et al., 2014; Baiden et al., 2014; Longman-Mills et al., 2013). Also life course impacts of adverse exposures can change overtime depending on resilience, recovery (Dekel and Bonanno, 2013) and severity of the exposures, and may bias the findings, particularly in retrospective reports. In addition, the use of retrospective reports of childhood maltreatment limits the validity of the association between childhood maltreatment and cannabis abuse or dependence, including the age of onset of these disorders.
In a few prospective studies, sexual and physical abuse (Werner et al., 2016) predicted cannabis use (Hayatbakhsh et al., 2009; Mills et al., 2016), abuse, and/or dependence in adolescents (Rogosch et al., 2010), young adults (Mills et al., 2016), and adults (Werner et al., 2016). As well, a composite score of substantiated neglect, sexual, physical, and emotional abuse (Rogosch et al., 2010; Mills et al., 2016) predicted subsequent cannabis use disorders. The severity of childhood maltreatment (Oshri et al., 2011) including frequency of maltreatment (Molnar et al., 2001) may account for the relationship between childhood maltreatment and cannabis use disorders. However, these results are largely based upon unsubstantiated self-reports of childhood maltreatment. With one exception (Mills et al., 2016), previous studies have also not addressed a range of types of childhood maltreatment, especially emotional abuse and neglect (Hayatbakhsh et al., 2009), although a few have included them in a cumulative score rather than independently (Rogosch et al., 2010). Consequently, little is known about the independent effect of different types of maltreatment (Teicher and Parigger, 2015) and the impact of the number of episodes on outcomes (Jackson et al., 2014). In addition, the link between childhood maltreatment and an early onset of cannabis use disorders has not been well established in a prospective population sample, controlling for the possible overlap between childhood maltreatment and the age of onset of cannabis use. The only report on this topic is for reported sexual and physical abuse (Hayatbakhsh et al., 2009; Sartor et al., 2013; Werner, et al., 2016), as well as combined forms of substantiated maltreatment (Mills et al., 2016). None of these studies examined the independent effect of each form of substantiated childhood maltreatment, while adjusting for other concurrent forms of maltreatment (Hayatbakhsh et al., 2009; Sartor et al., 2013; Werner et al., 2016; Mills et al., 2016).
The association between childhood maltreatment and cannabis use disorders may be complex, with a possibility that both may share common risk factors. For example, childhood maltreatment is commonly perpetrated by disadvantaged parents such as teenage mothers (Thornberry et al., 2014) who disproportionately experience prenatal and postnatal substance use disorders (Smith et al., 2007). In addition, gender (Baiden et al., 2014), poverty (Reinarman, 2011; Slack et al., 2004; Thornberry et al., 2014), poor educational achievement (Slack et al., 2004), and being single/never married (Degenhardt et al., 2008; Messman-Moore et al., 2000) may also be associated with exposure to childhood maltreatment (Baiden et al., 2014; Fluke et al., 2003; Slack et al., 2004; Smith et al., 2007; Thornberry et al., 2014) as well as cannabis use disorders (Choquet et al., 2008; Degenhardt et al., 2008; Horwood et al., 2010; Reinarman, 2011; Wallace et al., 2003). However, few studies have controlled for these potential confounding factors and/or covariates. Furthermore, exposure to traumatic events and associated posttraumatic stress disorder may be related to cannabis use disorders (Kevorkian et al., 2015). For example, the association between posttraumatic stress disorder and cannabis use disorders (i.e., lifetime, current and daily) is reportedly persistent even above and beyond the effects of socio demographic characteristics, lifetime substance use disorders, concurrent mental health problems and lifetime traumatic events such as physical assault, combat experience and automobile accidents (Cougle, Bonn-Moller, Vujanovic, Zvolensky, Hawkins, 2011).
Another concern relates to cannabis use measurement. Abuse and dependence are separate categories in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) (American Psychiatric Association, 2000) and International Classification of Diseases, 10th Edition (ICD-10) (Hasin, Hatzenbuehler, Keyes and Ogburn, 2006). However, they are merged into a single diagnostic category in the 5th version of DSM (DSM-5) (American Psychiatric Association, 2013). Nonetheless, DSM-5 criteria may underestimate the prevalence of DSM-IV lifetime cannabis use disorders with 40% of cases with DSM-IV cannabis use disorders remaining undetected when assessed by using DSM-5 (Mewton et al., 2013).
This study therefore examines the independent association between specific forms of substantiated childhood maltreatment and cannabis use as well as abuse or dependence, controlling for relevant confounders. It extends prior work using data from the same birth cohort on the effect of multiple combinations of childhood maltreatment on cannabis use (Mills et al., 2016). Unlike the earlier study, we specifically examined lifetime cannabis use, abuse and dependence separately, and adjusted for the effect of maternal smoking at pregnancy, as well as 6 months postpartum, on each form of substantiated maltreatment, while adjusting for other concurrent types of childhood maltreatment. We specifically investigated the effect of maternal cigarette smoking during pregnancy because it is a risk factor for offspring neurobehavioral and cognitive disorders (e.g., ADHD, externalizing, etc.) (Huizink and Mulder, 2006), psychotic symptoms (Zammit et al., 2009), drug dependence (Weissman, Warner, Wickramaratne and Kandel, 1999), alcohol and cannabis use (D’Onofrio et al., 2012). In addition, the number of incidents of childhood maltreatment substantiations was used as a severity marker. Finally, unlike the earlier study by Mills et al., this study also investigated the effects of increasing levels of cannabis use from subthreshold levels of cannabis use through to clinically evident disorders as measured by DSM-IV. We also investigated whether maltreatment had an effect on the age of onset of cannabis use disorders, and whether multiple episodes of child abuse and neglect predicted worse cannabis use, abuse and dependence outcomes.
2. Methods
2.1. Participants
The data of this study were collected from the Mater Hospital-University of Queensland Study of Pregnancy (MUSP), a cohort of expectant mothers and their children, identified consecutively at the time of their first antenatal clinic visit from 1981 to 1983 at Brisbane’s Mater Hospital. The number of mothers initially approached was 8556. Some 8458 pregnant women accepted the invitation to participate in the study. A total of 7223 gave birth to a live, singleton baby at the study hospital, who neither died nor was adopted out before the discharge. Starting from that point, the study focused on mother-child pairs up to the 21 year offspring follow-up. There were follow-ups at 3–5 days and 6 months postpartum, as well as at 5, 14 and 21 years of the index child’s age. The details of MUSP are presented elsewhere (Najman et al., 2015). The MUSP dataset was linked to agency-reported cases of childhood maltreatment of children 14 years of age and below. For the purpose of this study, the target age group is extended to the age of 21 years and their follow-up includes details of cannabis use disorders. The sample focused on 2526 young adults (females = 51.6%), who had data on cannabis use disorders at the 21-year follow-up (Figure 1). The mean age of the participants was 20.6 years. The MUSP has been approved by the Human Ethics Review Committee of The University of Queensland and the Mater Hospital. Parents provided consent before 14 years, and participants provided informed consent at latter phases of data collection. Ethical approval was obtained separately from the Human Ethics Review Committee of The University of Queensland for linking substantiated child maltreatment data to the 21-year follow-up data.
Figure 1.
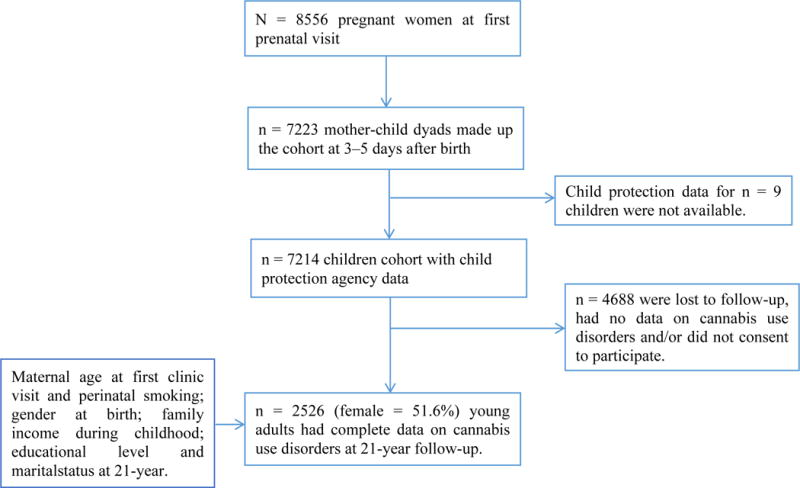
Flow of the study
2.2. Measures
2.2.1. Childhood maltreatment
State-wide child protection records were used to identify suspected cases of childhood maltreatment. Referrals from community members and mandatory reports from general practitioners were sources of information for childhood maltreatment. This birth cohort (n = 7223), comprised 789 (11%) notifications of any childhood maltreatment, of which 663 were for abuse and 500 for neglect. Child protection data were not available for 9 participants. Those cases where the Department of Families, Youth and Community Care Queensland had “reasonable cause to believe that the child had been, was being, or was likely to be abused or neglected” were defined as substantiated cases of childhood maltreatment. In terms of the categories of maltreatment, substantiated sexual abuse was recorded when the suspected child was confirmed for, “exposing a child to or involving a child in inappropriate sexual activities”. Physical abuse was defined as “any non-accidental physical injury inflicted by a person who had care of the child”. Emotional abuse included “any non-accidental physical injury inflicted by a person who had care of the child”. Finally, neglect was defined as a “failure to provide conditions that were essential for the healthy physical and emotional development of a child”, including both physical and emotional neglect (Steering Committee for the Review of Commonwealth/State Service Provision (SCRCSSP)). Queensland government child protection agency workers determined substantiations of childhood maltreatment.
These data were confidentially and anonymously linked to the MUSP longitudinal database (Strathearn et al., 2009). In this study, substantiated cases of childhood maltreatment were restricted to those occurring between 0 and 14 years of age to ensure childhood maltreatment preceded cannabis use disorders. Child maltreatment events were dichotomized and coded as substantiated maltreatment vs. no maltreatment. Specific categories (Lau et al., 2005) and co-occurring (Senn and Carey, 2010) forms of childhood maltreatment included substantiated sexual abuse, physical abuse, emotional abuse and neglect, as well as one or more combinations of the preceding maltreatment types. This classification appears to have greater predictive validity in predicting developmental outcomes (Lau et al., 2005; Senn and Carey, 2010). To disentangle the specific effects of each form of maltreatment, a composite variable was created. For example, a variable that excluded substantiated sexual abuse was created from one or more combinations of physical abuse, emotional abuse and neglect to adjust for sexual abuse and so on. Each composite variable was used to adjust for a specific model that examined the association between each subtype of childhood maltreatment and cannabis use disorders accordingly. The study also investigated the effect of frequency of childhood maltreatment substantiations on later outcomes.
2.2.2. Cannabis use, abuse, dependence and age of onset of cannabis use disorders
The study assessed lifetime cannabis abuse (ICD-10: 305.2) and dependence (ICD-10: 304.3) of the participants using the Composite International Diagnostic Interview (CIDI-Auto) Version 2.1 (Composite International Diagnostic Interview (CIDI-AUTO), 1997) at the 21-year follow-up. The age of onset of cannabis abuse (ICD-10: 305.2) or dependence (ICD-10: 304.3) was also recorded for those who reported either in their lifetime. Responses were coded to provide lifetime cannabis abuse and dependence based on the DSM-IV (American Psychiatric Association, 2000). The DSM-IV has been validated for cannabis abuse in a population-based adolescent sample (Legleye et al., 2013) and these diagnoses are broadly compatible with the ICD-10 (Hasin et al., 2006) and DSM-5 (Compton, Dawson, Goldstein and Grant, 2013) classifications. Participants were considered to have cannabis abuse diagnosis, if they endorsed any one or more of the four DSM-IV cannabis abuse criteria. Similarly, they were considered to have the diagnosis of cannabis dependence, if they endorsed three of the seven symptoms for cannabis dependence. To test the association between childhood maltreatment and an early age of onset of cannabis abuse and dependence, we restricted the analyses to those who reported cannabis abuse and dependence, and stratified the participants by age when they first reported cannabis abuse and dependence into the following categories; after and before 15 years of age. As there is no standard cutoff of age for early initiation of cannabis abuse, we chose the lowest fourth quartile of the age distribution to represent an early age of onset of cannabis abuse and dependence. In addition, participants were asked about the frequency of cannabis use in the previous month (never, every day, every few days, once or so, and not in the last month) and the age they started cannabis use (in years). The former was combined with DSM-IV disorders (i.e., abuse or dependence) to yield a categorical variable: never used, ever used with no DSM-IV disorders and use with DSM-IV disorders. This variable was used to examine whether childhood maltreatment predicted a greater tendency of episodic use or persistent cannabis use disorder. Additional models to test the temporal association between childhood maltreatment and cannabis use disorders by restricting the analyses to those who reported cannabis abuse and dependence were also performed. In addition, we assessed the effect of childhood maltreatment on age of onset of use as a continuous measure in participants who reported smoking cannabis (see the section on supplementary analyses).
2.2.3. Confounders/covariates
Both maternal and child related confounders/covariates were included in the analyses. Maternal age at pregnancy (in years) was obtained at first prenatal clinic visit. This was dichotomized as 20+ vs. 13–19 years for logistic regressions and used as a continuous measure for the multiple regressions. We also included data on maternal prenatal and postnatal cigarette smoking, obtained at the first prenatal clinic visit and 6 months postpartum. Mothers were asked how frequently they smoked cigarettes in the previous week at pregnancy and 6 months postpartum and recoded as follows: no-smoker = 0; once or so = 1; every few days = 2; and every day = 3. They were also asked how many cigarettes they smoked per day. The responses were recoded as follows: nil = 0; 1–9 = 1; 10–19 = 2; 20–29 = 3; 30–49 = 4; and 50+ = 5. A dichotomized composite variable for both prenatal and postpartum cigarette smoking was created from the frequency and number of cigarettes smoked and coded as ‘non-smokers” and “light to heavy smokers”. Family income was measured from pregnancy through to 5 years. The mean family income at each phase was taken and those mothers whose income was consistently below the poverty line over the first 5 years of their child’s life were coded as consistent poverty versus adequate income, using thresholds of the poverty level from 1981–1983 (Najman et al., 2004). Additionally, gender at birth (male/female), educational level attained (complete post-secondary/incomplete post-secondary school) and marital status (married-living together-separated-divorced-widowed/never married) were collected at the 21-year follow-up and included in the analyses as covariates.
2.3. Statistical analysis
Descriptive statistics including chi-squared analyses were used to describe the study variables and bivariate correlations of the selected confounders/covariates, predictors and outcomes. A series of unadjusted and hierarchical multivariable logistic regressions were done specifying cannabis abuse, dependence, early age of onset of cannabis abuse and dependence as dependent variables. We chose hierarchical regression analyses to determine the predictive stability of childhood maltreatment with adjustment for potential confounders of different levels and overlapping forms of maltreatment. Each form of childhood maltreatment was sequentially entered into the first model (Model 1) followed by maternal (Model 2) and young adults’ socio-demographic variables (Model 3) as well as the overlapping forms of childhood maltreatment variables (Model 4). Those who did not use or did not meet the DSM-IV cannabis abuse and/or dependence criteria were the reference groups in these models. We assessed the effect on severity of use with a three-category dependent variable ranging from never used through ever used but no disorder to abuse or dependence using unadjusted and simultaneously adjusted multinomial logistic regression models. The maximum likelihood ratio was used to test for model fit and significance. Additional analyses using the same models were done to account for possible overlap between exposure to childhood maltreatment and early onset cannabis abuse and dependence, controlling for those who reported cannabis abuse and dependence before the age of 14 years. The analyses were done for males and females separately, as well as the combined sample. Given that preliminary analyses showed gender differences in cannabis use disorders, interaction terms were computed for gender and all forms of childhood maltreatment and added to the final models. Odds ratios (ORs) with 95% confidence intervals (95% CIs) were used to present the findings. A higher odds ratio means a higher risk of cannabis use disorders.
2.3.1. Missing values
Weighted analyses using inverse probability weighting (Hogan et al., 2004) from the complete cases (Schafer and Graham, 2002) were done to determine whether missing values affected the reliability of findings from complete cases in three steps. This approach is used to account for possible biases arising from higher rates of non-random missingness. Binary logistic regressions of the selected predictors, including gender, maternal age and cigarette smoking status, and family income against missing values were carried out to identify those variables associated with higher rates of missing values. These variables were also used to generate weights. Multivariable logistic regression analysis was then undertaken to determine the independent predictors of missing values and to generate weights for the study sample. Finally, the weighted sample that involved the final adjusted regression model was done to determine whether missing values had affected the findings for each outcome. Results presented in the main paper involved findings derived from both the unweighted and weighted data analyses. Statistical analyses were done using STATA (StataCorp LP: College Station, Texas, 2015) and SPSS (IBM Corp: Armonk, NY, 2013) for windows setting the level of significance at p-value of 0.05.
2.3.2. Supplementary analyses
In order to examine the association between childhood maltreatment and age of onset of cannabis abuse, supplementary analyses using age of onset of cannabis abuse as a continuous outcome were carried out.
3. Results
There were 2526 participants who had complete data on lifetime cannabis abuse at the 21-year follow-up, representing 35.0% of the baseline cohort. Over 7 in 10 (n = 1834) participants ever used cannabis. Of these, 27.5% (n = 336) and 12.2% (n = 159) males and females were cannabis abusers, respectively. Similarly, 14.7% (n = 180) and 8.0% (n = 105) males and females had cannabis dependence disorder, respectively (Table S1). In the birth cohort, there were 789 notifications for any childhood maltreatment. This was substantiated for any maltreatment for 4.8% (n = 121) participants remaining in the study, of which 1.8% (n = 42) children experienced two or more episodes of childhood maltreatment substantiations. The rates of any substantiated childhood maltreatment were higher for teen age mothers (χ2 = 27.62 (df = 1); p <0.0001), maternal smoking both at pregnancy and postpartum (χ2 = 26.65 (df = 1); p <0.0001), family poverty over the first 5 years of age (χ2 = 5.46 (df = 1); p = 0.019), incomplete high school χ2 = 4.23 (df = 1); p = 0.040) and being never married (χ2 = 5.72 (df = 1); p = 0.017) at 21 years. The rates of late childhood and adolescence substantiations were higher for teenage mothers (χ2 = 13.74 (df = 1); p <0.0001), maternal smoking both at pregnancy and postpartum (χ2 = 16.83 (df = 1); p <0.0001) and family poverty over the first 5 years of age (χ2 = 5.49 (df = 1); p = 0.019). The rates of more frequent substantiations were higher for teenage mothers (χ2 = 28.02 (df = 2); p <0.0001), maternal smoking both at pregnancy and postpartum (χ2 = 26.12 (df = 2); p <0.0001) and family poverty over the first 5 years of age (χ2 = 16.78 (df = 2); p = 0.019).
The results are presented for cannabis abuse and cannabis dependence separately. A total of 19.6% (n = 495) participants met 1 or more of the DSM-IV diagnostic criteria for lifetime cannabis abuse at the 21-year follow-up. Of those who met a diagnosis of cannabis abuse, 34.5% (n = 171) had cannabis abuse symptoms before the age of 15. More than one half of those participants, 57.4% (n =284), who used cannabis also had cannabis dependence, meeting 3 or more of the DSM-IV diagnostic criteria. Interestingly, 29.4% (n = 743) participants used cannabis without manifesting any DSM-IV disorders. The age of onset of cannabis dependence was before 15 years for 25.0% (n = 72) of the participants. Maternal prenatal and postpartum cigarette smoking and incomplete post-high school at 21-year were more likely associated with later cannabis use disorders. Males had higher rates of cannabis abuse (χ2 = 93.37 (df = 1); p <0.0001), an early age of onset of cannabis abuse (χ2 = 99.19 (df = 1); p <0.0001) and cannabis dependence (χ2 = 28.62 (df = 1); p <0.0001). Those participants who had had incomplete high school (χ2 = 87.9 (df=1); p <0.0001) had higher rates of cannabis abuse. Levels of cannabis abuse and dependence were also higher for those who were exposed to any form of childhood maltreatment including physical abuse, emotional abuse and neglect, as well as for those substantiated for two or more episodes of substantiations to maltreatment (Table 1).
Table 1.
Prevalence and bivariate association of childhood maltreatment and cannabis abuse and dependence at 21-year, Brisbane, Australia.
| Childhood maltreatment | Cannabis abuse
|
Cannabis dependence
|
||||
|---|---|---|---|---|---|---|
| No; number (%) | Yes; number (%) | χ2 (df = 1) (p-value) | No; number (%) | Yes; number (%) | χ2 (df = 1) (p-value) | |
| Any maltreatmenta | ||||||
| No | 1946 (80.9) | 459 (19.1) | 8.32 (0.004) | 2141 (89.3) | 257 (10.7) | 15.59 (<0.0001) |
| Yes | 85 (70.2) | 36 (29.8) | 94 (77.7) | 27 (22.3) | ||
| Sexual abuse | ||||||
| No | 1998 (80.3) | 489 (19.7) | 0.45 (0.504) | 2208 (88.8) | 278 (11.2) | 0.68 (0.410) |
| Yes | 33 (84.6) | 6 (15.4) | 33 (84.6) | 6 (15.4) | ||
| Physical abuse | ||||||
| No | 1997 (80.7) | 478 (19.3) | 6.23 (0.013) | 2201 (89.0) | 273 (11.0) | 5.56 (0.018) |
| Yes | 34 (66.7) | 17 (33.3) | 40 (78.4) | 11 (21.6) | ||
| Emotional abuse | ||||||
| No | 1991 (80.7) | 476 (19.3) | 6.09 (0.014) | 2194 (89.0) | 272 (11.0) | 5.00 (0.025) |
| Yes | 40 (67.8) | 19 (32.8) | 47 (79.7) | 12 (20.3) | ||
| Neglect | ||||||
| No | 1999 (80.7) | 479 (19.3) | 9.27 (0.002) | 2205 (89.0) | 272 (19.0) | 9.27 (0.002) |
| Yes | 32 (66.7) | 16 (33.3) | 36 (75.0) | 12 (25.0) | ||
| Age at substantiations | ||||||
| No | 1964 (80.8) | 468 (19.2) | 5.16 (0.023) | 2167 (89.1) | 264 (10.9) | 9.84 (0.002) |
| 5–14 years | 67 (71.3) | 27 (28.7) | 74 (78.7) | 20 (21.3) | ||
| Frequency of substantiations* | ||||||
| No | 1946 (80.9) | 459 (19.1) | 11.16 (0.004) | 2147 (89.3) | 257 (10.7) | 10.74 (0.005) |
| Only once | 59 (74.7) | 20 (25.3) | 64 (81.0) | 15 (19.0) | ||
| Twice or more | 26 (61.9) | 16 (38.1) | 30 (71.4) | 12 (28.6) | ||
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
χ2 (df = 2).
In binary logistic regression analyses, all forms of childhood maltreatment, except sexual abuse, were strongly associated with cannabis abuse (unadjusted OR = 1.95–2.91). Exposure to any childhood maltreatment was associated with 1.79 times the odds of cannabis abuse even after adjusting for socio-demographic variables. Similarly, neglect was strongly associated with higher odds of cannabis abuse (AOR = 2.62) after adjusting for all variables and other forms of childhood maltreatment (Table 2). Any maltreatment, emotional abuse and neglect were associated with increased odds of an early age of onset of cannabis abuse in binary logistic regression models. After hierarchically adjusting for all confounders/covariates, childhood maltreatment (AOR = 2.77), emotional abuse (AOR = 3.59) and neglect (AOR = 3.48) were strongly associated with an early age of onset of cannabis abuse (Table 3). All forms of childhood maltreatment, except sexual abuse, were associated with cannabis dependence in the binary logistic regressions. The statistical significance of any childhood maltreatment (AOR = 2.47), physical abuse (AOR = 2.81), emotional abuse (AOR = 2.44) and neglect (AOR = 2.68) remained stable after adjusting for all confounders/covariates and other forms of maltreatment in multivariable hierarchical logistic regressions (Table 4). Any types of maltreatment (AOR = 3.72), physical abuse (AOR = 5.09) and neglect (AOR = 4.92) were associated with an early age of onset of cannabis dependence, after adjusting for all covariates/confounders and overlapping forms of childhood maltreatment (Table 5).
Table 2.
Hierarchical logistic regression estimates of childhood maltreatment predicting cannabis abuse at 21-year, Brisbane, Australia.
| Childhood maltreatment | Category | Unadjusted OR (95%CI)
|
Adjusted OR (95%CI)
|
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| Any maltreatment | No | 1 | 1 | 1 | 1 |
| Any maltreatmenta,b | Yes | 1.95 (1.19–3.17)** | 1.79 (1.08–2.97)* | 1.79 (1.08–2.96)* | – |
| Sexual abuse | Yes | 0.79 (0.27–2.31) | 0.93 (0.31–2.78) | 0.93 (0.31–2.79) | 0.97 (0.32–2.89) |
| Physical abuse | Yes | 2.01 (0.97–4.17) | 1.83 (0.86–3.89) | 1.81 (0.85–3.85) | 1.85 (0.87–3.93) |
| Emotional abuse | Yes | 2.29 (1.16–4.54)* | 1.96 (0.97–3.98) | 1.95 (0.96–3.96) | 1.98 (0.98–4.02) |
| Neglect | Yes | 2.91 (1.34–6.31)** | 2.58 (1.15–5.75)* | 2.58 (1.16–5.77)* | 2.62 (1.17–5.86)* |
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
Model did not adjust for other forms of childhood maltreatment.
Model 1: Unadjusted child maltreatment and cannabis abuse.
Model 2: Model 1 + gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age.
Model 3: Adjusted for Models 1 + 2 + educational level and marital status at 21 years.
Model 4: Adjusted for Models 1 + 2 + 3 + any substantiated childhood maltreatment excluding the variable of interest to avoid the effect of overlapping maltreatment.
p <0.05;
p <0.01.
Table 3.
Hierarchical logistic regression estimates of childhood maltreatment predicting early age of onset of cannabis abuse at 21-year, Brisbane, Australia.
| Childhood maltreatment | Category | Unadjusted OR (95%CI)
|
Adjusted OR (95%CI)
|
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| Any maltreatment | No | 1 | 1 | 1 | 1 |
| Any maltreatmenta,b | Yes | 3.36 (1.67–6.76)*** | 2.77 (1.35–5.69)** | 2.77 (1.35–5.68)** | – |
| Sexual abuse | Yes | – | – | – | – |
| Physical abuse | Yes | 2.97 (1.03–8.63)* | 2.39 (0.81–7.08) | 2.36 (0.79–7.00) | 2.51 (0.84–7.44) |
| Emotional abuse | Yes | 4.42 (1.79–10.88)*** | 3.50 (1.39–8.79)** | 3.48 (1.39–8.74)** | 3.59 (1.43–9.01)** |
| Neglect | Yes | 3.89 (1.32–11.50)* | 3.28 (1.09–9.91)* | 3.30 (1.09–9.97)* | 3.48 (1.15–10.52)* |
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
Model did not adjust for other forms of childhood maltreatment.
Model 1: Unadjusted child maltreatment and cannabis abuse.
Model 2: Model 1 + gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age.
Model 3: Adjusted for Models 1 + 2 + educational level and marital status at 21 years.
Model 4: Adjusted for Models 1 + 2 + 3 + any substantiated childhood maltreatment excluding the variable of interest to avoid the effect of overlapping maltreatment.
p <0.05;
p <0.01;
p <0.0001.
Table 4.
Hierarchical logistic regression estimates of childhood maltreatment predicting cannabis dependence at 21-year, Brisbane, Australia.
| Childhood maltreatment | Category | Unadjusted OR (95%CI)
|
Adjusted OR (95%CI)
|
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| Any maltreatment | No | 1 | 1 | 1 | |
| Any maltreatmenta,b | Yes | 2.69 (1.58–4.61)**** | 2.48 (1.43–4.30)*** | 2.47 (1.43–4.29)*** | – |
| Sexual abuse | Yes | 1.12 (0.33–3.77) | 1.21 (0.35–4.14) | 1.22 (0.36–4.19) | 1.30 (0.38–4.47) |
| Physical abuse | Yes | 3.03 (1.39–6.58)** | 2.79 (1.26–6.18)* | 2.72 (1.23–6.01)* | 2.81 (1.27–6.22)* |
| Emotional abuse | Yes | 2.70 (1.26–5.81)* | 2.39 (1.09–5.20)* | 2.36 (1.80–5.15)* | 2.44 (1.12–5.33)* |
| Neglect | Yes | 2.93 (1.22–7.01)** | 2.54 (1.05–6.19)* | 2.57 (1.05–6.25)* | 2.68 (1.09–6.52)* |
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
Model did not adjust for other forms of childhood maltreatment.
Model 1: Unadjusted child maltreatment and cannabis dependence.
Model 2: Model 1 + gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age.
Model 3: Adjusted for Models 1 + 2 + educational level and marital status at 21 years.
Model 4: Adjusted for Models 1 + 2 + 3 + any substantiated childhood maltreatment excluding the variable of interest to avoid the effect of overlapping maltreatment.
p <0.05;
p <0.01;
p <0.01;
p <0.0001.
Table 5.
Hierarchical logistic regression estimates of childhood maltreatment predicting early age of onset of cannabis dependence at 21-year, Brisbane, Australia.
| Childhood maltreatment | Category | Unadjusted OR (95%CI)
|
Adjusted OR (95%CI)
|
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| Any maltreatment | No | 1 | 1 | 1 | |
| Any maltreatmenta,b | Yes | 4.21 (1.83–9.69)*** | 3.72 (1.59–8.75)** | 3.72 (1.58–8.73)** | – |
| Sexual abuse | Yes | – | – | – | – |
| Physical abuse | Yes | 5.59 (1.89–16.54)** | 4.86 (1.62–14.61)** | 4.83 (1.60–14.55)** | 5.09 (1.69–15.39)** |
| Emotional abuse | Yes | 3.61 (1.07–12.19)* | 3.16 (0.92–10.81) | 3.14 (0.92–10.77) | 3.39 (0.99–11.68) |
| Neglect | Yes | 5.14 (1.49–17.69)*** | 4.54 (1.29–15.90)* | 4.56 (1.30–15.96)* | 4.92 (1.40–17.25)* |
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
Model did not adjust for other forms of childhood maltreatment.
Model 1: Unadjusted child maltreatment and cannabis dependence.
Model 2: Model 1 + gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age.
Model 3: Adjusted for Models 1 + 2 + educational level and marital status at 21 years.
Model 4: Adjusted for Models 1 + 2 + 3 + any substantiated childhood maltreatment excluding the variable of interest to avoid the effect of overlapping maltreatment.
p <0.05;
p <0.01;
p <0.0001.
Further fully adjusted analyses using weighted data to account for possible selection bias did not affect the findings of complete case analyses. For example, the AORs of cannabis abuse were 1.80 and 2.63 for any childhood maltreatment and neglect, respectively. Likewise, the association between any maltreatment, physical abuse, emotional abuse and neglect, and cannabis dependence was consistent (Table 6).
Table 6.
Adjusted odds ratio (95%CI) estimates of childhood maltreatment predicting cannabis use disorders at 21-year for weighted data, Brisbane, Australia.
| Childhood maltreatment | Category | Cannabis abuse | Cannabis dependence |
|---|---|---|---|
|
|
|
|
|
| Any maltreatment | No | 1 | 1 |
| Any maltreatmenta,b | Yes | 1.80 (1.08–2.99)* | 2.48 (1.43–4.43)*** |
| Sexual abuse | Yes | 0.99 (0.33–2.99) | 1.31 (0.38–4.53) |
| Physical abuse | Yes | 1.86 (0.87–3.96) | 2.82 (1.27–6.24)* |
| Emotional abuse | Yes | 1.99 (0.98–4.05) | 2.45 (1.12–5.35)* |
| Neglect | Yes | 2.63 (1.18–5.89)* | 2.68 (1.10–6.54)* |
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
Model did not adjust for other forms of childhood maltreatment.
Adjusted for gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age, educational level and marital status at 21 years, and for respective composite variables to avoid the effect of overlapping maltreatment.
p <0.05;
p <0.001.
In terms of frequency, more substantiated events were associated with higher odds of cannabis use disorders. Finally, fully adjusted analyses using weighted data also revealed similar findings with AORs of 1.52, 2.09, 1.88 and 2.71 for cannabis abuse, early age of onset of cannabis abuse, cannabis dependence and early age of onset of cannabis dependence, respectively (Table 7). Childhood maltreatment had a similar association with age of onset of cannabis use in participants who ever smoked cannabis (i.e., n = 1834), measured as a continuous variable (Table S2).
Table 7.
Adjusted logistic regression estimates of number of substantiations predicting cannabis abuse, early age of onset of cannabis abuse and dependence, Brisbane, Australia.
| Frequency of maltreatment |
|
Adjusted OR (95%CI)a
|
|
|
|---|---|---|---|---|
| Cannabis abuse | Early age of onset of cannabis abuse | Cannabis dependence | Early age of onset of cannabis dependence | |
| Number of substantiationsb | ||||
| Once only | 1 | 1 | 1 | 1 |
| Two or more times | 1.51 (1.06–2.16)* | 1.97 (1.36–2.84)**** | 1.87 (1.27–2.74)*** | 2.67 (1.55–4.59)**** |
| Number of substantiationsc | ||||
| Once only | 1 | 1 | 1 | 1 |
| Two or more times | 1.52 (1.06–2.19)* | 2.09 (1.31–3.36)**** | 1.88 (1.28–2.76)*** | 2.71 (1.57–4.68)**** |
Adjusted for gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age, educational level and marital status at 21 years.
Models did not adjust for other forms of childhood maltreatment.
The analyses involved weighted data.
p <0.05;
p <0.001;
p <0.0001.
Additional analyses of the associations between childhood maltreatment and cannabis abuse and dependence after controlling for those participants who reported cannabis abuse (n = 17) and dependence (n = 15) outcomes before 14 years of age showed similar findings in all models (data not shown). The gender–any childhood maltreatment interaction term was significant (interaction term = 0.11, p < 0.0001). However, the inclusion of the interaction term in the respective fully adjusted models controlling for the main effect of gender did not change the size and direction of the association between childhood maltreatment and cannabis use disorders (Table S3).
In unadjusted and adjusted multinomial models, childhood maltreatment was also associated with cannabis use with and/or without any DSM-disorder. All forms of childhood maltreatment were associated with increased odds of cannabis use without any disorder in unadjusted multinomial logistic regression models. After adjusting for all confounders/covariates, childhood maltreatment (AOR = 1.78) and emotional abuse (AOR = 2.15) were strongly associated with cannabis use without any disorder. Similar patterns of unadjusted associations were also reported for subtypes of childhood maltreatment, except sexual abuse, and cannabis use with any disorder. Exposure to any maltreatment (AOR = 2.00) and neglect (AOR = 3.21) were associated with cannabis use with any disorder, after adjusting for all confounders/covariates (Table 8).
Table 8.
Unadjusted and adjusted multinomial logistic regression odds ratio estimates of childhood maltreatment predicting cannabis use with and/or without DSM-IV disorder at 21-year, Brisbane, Australia.
| Childhood maltreatment | Never cannabis use | Ever cannabis use without DSM-IV disorder(95%CI) | Cannabis use with any DSM-IV disorder(95%CI) | ||
|---|---|---|---|---|---|
|
| |||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | ||
|
|
|
|
|||
| Any maltreatmenta, b | 1 | 1.93 (1.29–2.88)*** | 1.78 (1.1.19–2.67)** | 2.26 (1.48–3.46)**** | 2.00 (1.29–3.11)** |
| Sexual abuse | 1 | 2.29 (1.21–4.36)* | 1.58 (0.0.69–3.61) | 1.25 (0.53–2.97) | 1.09 (0.35–3.39) |
| Physical abuse | 1 | 2.44 (1.33–4.47)** | 1.48 (0.70–3.11) | 2.47 (1.27–4.79)** | 1.56 (0.68–3.56) |
| Emotional abuse | 1 | 2.78 (1.60–4.82)**** | 2.15 (1.05–4.39)* | 2.62 (1.42–4.84)** | 2.10 (0.0.95–4.65) |
| Neglect | 1 | 2.43 (1.29–4.57)** | 1.57 (0.64–3.89) | 3.09 (1.61–5.95)*** | 3.21 (1.39–7.35)** |
The reference category is: Not any childhood maltreatment.
Any childhood maltreatment included one or more combination of neglect, sexual, physical or emotional abuse.
Adjusted for gender at birth, maternal age at pregnancy, maternal smoking at pregnancy and 6 months postpartum and family poverty over the first 5 years of age, educational level and marital status at 21 years.
p <0.05;
p <0.01;
p <0.001;
p <0.0001.
On binary logistic regressions of missing values, maternal age at pregnancy (Table S4) as well as all forms of childhood maltreatment was associated with higher rates of missing values. All forms of childhood maltreatment were statistically significant predictors of missing values in multivariable analysis (data not shown).
4. Discussion
We examined the prospective association between specific forms of substantiated childhood maltreatment and subsequent cannabis abuse or dependence while controlling for potential confounders and/or covariates including other types of maltreatment. We also tested the effect of multiple episodes of maltreatment.
This paper extends an earlier study on the effects of substantiated childhood maltreatment on cannabis use disorders using the same dataset in the following ways (Mills et al., 2016). Firstly, we adjusted for maternal pregnancy and postnatal cigarette smoking because this is a risk factor for neurobehavioral and cognitive disorders in their children (e.g., ADHD, externalizing, etc.) (Huizink and Mulder, 2006), as well as psychotic symptoms (Zammit et al., 2009), drug dependence (Weissman et al., 1999), alcohol and cannabis use (D’Onofrio et al., 2012). Secondly, we also adjusted for other concurrent types of childhood maltreatment to further investigate the independent effect of each type of childhood maltreatment. Thirdly, we adjusted for gender-childhood maltreatment interaction term in addition to the main effect of gender. Fourthly, we included analyses of missing values and weighted data to account for attrition, and used the number of incidents of childhood maltreatment substantiations as indicators of severity while examining cannabis use and early age of onset of cannabis use disorders. Fifthly, we explored differences between cannabis use, use disorders and dependence. The previous study collapsed the latter two and did not directly compare cannabis use with and/or without any cannabis DSM-IV disorder. Sixthly, we used DSM-IV age of onset of cannabis use and dependence disorders separately and supplemented the findings with a continuous age of onset. We did this because dichotomizing continuous variables has several disadvantages including the loss of statistical power, as well as the making of variability and non-linearity in the association between the variable of interest and outcome (Altman and Royston, 2006). Moreover, the current paper controlled for those who reported cannabis abuse and dependence before the age of 14 years to account for possible overlap between exposure to childhood maltreatment and early onset cannabis abuse and dependence, whereas Mills et al. reported age of cannabis use from a single self-reported survey item. In addition, Mills and colleagues did not compare age of onset of use and dependence, and did not account for possible overlap between childhood maltreatment and early age of onset of cannabis use. Finally, duplication of the cannabis use variable was eliminated by combining and collapsing cannabis use with DSM-IV disorders yielding three comparable categories: never used, ever used with no DSM-IV disorders, and use with DSM-IV disorders. This was imperative to compare the effects of episodic or subthreshold levels of cannabis use with persistent or clinically evident disorders. Moreover, a continuous age of onset of cannabis use variable has been used in this paper.
We found that substantiated childhood maltreatment was associated with cannabis abuse and dependence including earlier onset of use and dependence. Our further analyses also showed similar findings for cannabis use with and/or without any cannabis use disorder. This was particularly true of each form of maltreatment, except sexual abuse, and when there are multiple forms and episodes of maltreatment. The specific associations may be explained by “differential effects model” (Senn and Carey, 2010) where individual maltreatment type leads to specific detrimental developmental outcomes (Lau et al., 2005; Senn and Carey, 2010) including substance use disorders (Arata et al., 2007). According to the “general effects model” (Senn and Carey, 2010), co-occurring (Arata et al., 2007) and multiple episodes of maltreatment, may also predict later psychopathic conditions through poor coping strategies, behavioral maladaptation (Jackson et al., 2014; Sesar et al., 2010), and substance use disorders including cannabis (Arata et al., 2007). Indeed, an earlier study using the same dataset reported that different types of substantiated childhood maltreatment predicted cannabis use disorders overall (Mills et al., 2016). Our findings build on that body of knowledge by further investigating the effect of childhood maltreatment on the severity of cannabis use as shown by the presence of dependence. The study addresses the main methodological limitation of the field by statistically partitioning the independent effects of specific and multiple forms of childhood maltreatment (Herrenkohl and Herrenkohl, 2009; Higgins and McCabe, 2001). Notably, the analyses that controlled for cannabis use disorders before 14 years of age revealed consistent findings, confirming an independent longitudinal association between childhood maltreatment and cannabis use disorders. Additionally, the prospective evaluation of cannabis use disorders across late childhood period enables us to investigate the chronic developmental impact of childhood maltreatment (Noll et al., 2003; Senn et al., 2008). This is important because the risk of childhood maltreatment in later stages of childhood development (Thornberry et al., 2014) and subsequent substance use is substantial (Thornberry et al., 2010).
The association between childhood maltreatment and cannabis use disorders persisted after adjustment for a range of potential parental and individual confounders. All models controlled for concurrent socio-economic covariates including the level of education and marital status of the young adults while predicting cannabis use disorders. The association between childhood maltreatment and cannabis use disorders may be direct and/or both may have common risk factors. For instance, maternal prenatal and postnatal substance abuse may lead to childhood maltreatment (Smith et al., 2007) through poor child monitoring and protection (Widom and Hiller-Sturmhofel, 2001), which in turn, may predict child substance use (Widom and Hiller-Sturmhofel, 2001) including cannabis. A maternal stressful environment (Kim et al., 2016) including cigarette smoking (Smith et al., 2007) may also lead to childhood maltreatment (Smith et al., 2007), increase behavioral disorganization, disruption, instability (Widom and Hiller-Sturmhofel, 2001), poor impulse control and less academic achievement (Huizink and Mulder, 2006). Exposure to these maternal stresses may be associated with poor neurobehavioral (Huizink and Mulder, 2006; Kim et al., 2016) pathways and cognitive outcomes, with subsequent poor executive functioning (Fontes et al., 2011) including poor educational achievement (Fergusson et al., 2003; Slack et al., 2004) and addiction (Kim et al., 2016), particularly in early cannabis users (Fontes et al., 2011). Future research that considers these intermediate variables may help describe possible pathways that link early childhood adversity and subsequent cannabis use disorders.
Unlike all the other forms of childhood maltreatment, however, sexual abuse was not associated with any cannabis use disorders. In contrast to prior studies (Hayatbakhsh et al., 2009), however, sexual abuse was not significantly associated with cannabis use disorders. For instance, it is possible that sexual abuse is underreported (Martin and Silverstone, 2013) because of inconsistent definitions (Martin and Silverstone, 2013), secrecy (Polonko, 2006) and stigma (Mills et al., 2016). Conversely, the nature and severity of sexual abuse (Hahm et al., 2010; Kendall-Tackett and Becker-Blease, 2004), may mean that it is more likely to be reported and attract an agency response before there is progression to long-term disorders (Kendall-Tackett and Becker-Blease, 2004) involving cannabis use. In addition, restricting our definition of childhood maltreatment to substantiated cases, as well as higher rates of attrition in these cases may underestimated actual levels of maltreatment (Theodore et al., 2005) and so affected the statistical power to detect significant associations, especially for sexual abuse.
Although exploring the mechanism of association between childhood maltreatment and cannabis use disorders is beyond the scope of the current study, cannabis use disorders may result from posttraumatic stress disorder (Hovdestad et al., 2011), or subsequent concurrent symptoms of posttraumatic disorder (Bujarski et al., 2012; Cougle et al., 2011) that persist across the lifespan (deRoon-Cassini et al., 2010). Maltreated individuals (Nomura et al., 2012) may tend to have other unwanted consequences (Harrison et al., 1997), which may also predict cannabis abuse (Atakan, 2008). For example, physical abuse (Stevens et al., 2015), emotional abuse, and neglect (Arata et al., 2007; Hildyard and Wolfe, 2002) may have effect on cognitive, emotional, and behavioral outcomes (Arata et al., 2007; Hildyard and Wolfe, 2002). Consequently, maltreated children may be at risk for early initiation of substance use that may, in turn, lead to later substance use disorders (Rogosch et al., 2010).
Some limitations of the study should also be considered. The use of legally defined cases are likely to underestimate the true prevalence of childhood maltreatment (Theodore et al., 2005) and may account for the observed weak associations, particularly for sexual abuse (Martin and Silverstone, 2013). Maltreated children may have substantially higher rates of early alcohol and tobacco use (Mills et al., 2014), possibly gateways to subsequent cannabis use (Fergusson et al., 2006). Although we could not disentangle this effect (Fergusson et al., 2006; Hall and Lynskey, 2005), a previous study using the same study sample showed self-reported sexual abuse before the age of 16 years led to frequent cannabis use after excluding those participants who reported concurrent use of other illicit drugs and restricting the analysis for those who reported cannabis use only (Hayatbakhsh et al., 2009). Concurrent psychopathologies (Aas et al., 2014) may mediate or moderate the association between childhood maltreatment and cannabis use disorders (Breslau et al., 2003); the observed associations may perhaps have accounted for concurrent mental health disorders and subsequent substance use (Houston et al., 2008). That is, maltreated individuals may have cannabis disorders due to underlying poor mental health and subsequent misuse of drugs (Stewart et al., 2013).Moreover, the potency of cannabis use was not assessed, which may influence patterns of association with cannabis use disorders. Finally, carrying out a substantial number of analyses may have introduced Type I error, although the patterns of results were similar suggesting consistency of the observed findings.
Although there may be many risk factors for cannabis use disorders, our findings revealed strong associations between single and multiple forms of childhood maltreatment and cannabis use disorders that may have specific implications for the prevention of subsequent cannabis abuse and dependence including an early age of onset of these disorders. An early age of onset of cannabis use has both public health and clinical implications (Hall, 2009), as it predicts later abuse and dependence (Hall, 2009; Lansford et al., 2010; Rogosch et al., 2010), and other adverse health, psychosocial (Hall, 2009) and neuropsychiatric disorders, possibly through impaired brain development (Hadland et al., 2015) or distorted neuroendocrine mechanisms (Kim et al., 2016). As such, prevention of childhood maltreatment along with tracking a history of cannabis use disorders would lessen the problem. This may involve community-based prevention in the early childhood period (Daro and Dodge, 2009) along with and appropriate clinical approaches that promote resiliency (Mancini and Bonanno, 2006), and focus on possible causes (Patton et al., 2002) or consequences of cannabis abuse (Horwood et al., 2012). Given similar association of cannabis abuse and dependence with childhood maltreatment, these children may be at higher risk for both episodic and longer-term (i.e., dependence) cannabis use disorders. As such, this study established associations between childhood maltreatment and cannabis use without any diagnosable disorder, implying a higher risk of subthreshold level cannabis use among participants with a history of maltreatment. This was supported by our supplementary analyses showing a strong association between childhood maltreatment and age of onset of cannabis abuse.
Conclusions
Childhood maltreatment was strongly and consistently associated with cannabis abuse and dependence, as well as cannabis use with and/or without any disorder. Emotional abuse, neglect and exposure to more episodes of maltreatment independently predicted cannabis use disorders. There was no evidence for the effect of any interaction between gender and different forms of childhood maltreatment on adulthood cannabis use disorders. Earlier interventions for childhood maltreatment may be a significant public health effort that may also reduce the effect of maltreatment on later cannabis use disorders. However, this requires an evidence-based approach which trades-off the cost and unintended consequences of an intervention against the benefits likely to be derived.
Supplementary Material
Highlights.
Substantiated childhood maltreatment was associated with both subthreshold and persistent cannabis use disorders young adulthood including an early age of onset.
These associations were also strong for more frequent episodes of childhood maltreatment, as well as cannabis use without disorders.
There was no evidence for the effect of any interaction between gender and different forms of childhood maltreatment on cannabis use disorders.
Subthreshold, persistent, early age of onset of, and cannabis use without disorders, were common problems of maltreatment.
These associations were also strong for more frequent episodes of childhood maltreatment.
There was no gender-any childhood maltreatment interaction effect on cannabis use disorders.
Acknowledgments
We would like to extend our acknowledgments to the Mater-University of Queensland Study of Pregnancy mother-child pairs, the research team, National Health and Medical Research Council and Australian Research Council for subsequent funding of the Mater-University of Queensland Study of Pregnancy. We are also grateful to the International Postgraduate Scholarships of the Australian government and The University of Queensland for sponsoring the principal author of the study.
Funding
The Mater-University of Queensland Study of Pregnancy was funded by the National Health and Medical Research Council and Australian Research Council (NHMRC grant #1009460) and the principal investigator is in receipt of Australian government International Postgraduate Research and The University of Queensland Centennial Scholarships. Dr Strathearn was funded by the U.S. National Institute of Drug Abuse (2R01DA026437). The funding sourceshad no rolesin study design, data collection, data analysis, data interpretation or writing of the report.
Footnotes
Conflicts of Interest
The authors report no conflict of interests.
References
- Aas M, Etain B, Bellivier F, Henry C, Lagerberg T, Ringen A, et al. Additive effects of childhood abuse and cannabis abuse on clinical expressions of bipolar disorders. Psychol Med. 2014;44(08):1653–1662. doi: 10.1017/S0033291713002316. [DOI] [PubMed] [Google Scholar]
- Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332(7549):1080. doi: 10.1136/bmj.332.7549.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. American Psychiatric Pub; Arlington, VA: 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) American Psychiatric Pub; Washington, DC: 2013. [Google Scholar]
- Arata CM, Langhinrichsen-Rohling J, Bowers D, O’Brien N. Differential correlates of multi-type maltreatment among urban youth. Child Abuse and Negl. 2007;31(4):393–415. doi: 10.1016/j.chiabu.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Atakan Z. Cannabis use by people with severe mental illness–is it important? Advances in Psychiatric Treatment. 2008;14(6):423–431. [Google Scholar]
- Baiden P, Stewart SL, Dunnen WD. Childhood abuse and cannabis use among adolescents with mental health needs in Ontario, Canada. J Substance Use. 2014;19(1–2):18–24. [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psych. 2003;60(3):289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Bujarski SJ, Feldner MT, Lewis SF, Babson KA, Trainor CD, Leen-Feldner E, et al. Marijuana use among traumatic event-exposed adolescents: posttraumatic stress symptom frequency predicts coping motivations for use. Addictive Behaviors. 2012;37(1):53–59. doi: 10.1016/j.addbeh.2011.08.009. [DOI] [PubMed] [Google Scholar]
- Choquet M, Hassler C, Morin D, Falissard B, Chau N. Perceived parenting styles and tobacco, alcohol and cannabis use among French adolescents: Gender and family structure differentials. Alcohol and Alcoholism. 2008;43(1):73–80. doi: 10.1093/alcalc/agm060. [DOI] [PubMed] [Google Scholar]
- Compton MT, Furman AC, Kaslow NJ. Preliminary evidence of an association between childhood abuse and cannabis dependence among African American first-episode schizophrenia-spectrum disorder patients. Drug and Alcohol Dependence. 2004;76(3):311–316. doi: 10.1016/j.drugalcdep.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Compton WM, Dawson DA, Goldstein RB, Grant BF. Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug and Alcohol Dependence. 2013;132(1):387–390. doi: 10.1016/j.drugalcdep.2013.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cougle JR, Bonn-Miller MO, Vujanovic AA, Zvolensky MJ, Hawkins KA. Posttraumatic stress disorder and cannabis use in a nationally representative sample. Psychol Addicit Behaviors. 2011;25(3):554–558. doi: 10.1037/a0023076. [DOI] [PubMed] [Google Scholar]
- D’Onofrio BM, Rickert ME, Langström N, Donahue KL, Coyne CA, Larsson H, et al. Familial confounding of the association between maternal smoking during pregnancy and offspring substance use and problems. Arch Gen Psych. 2012;69(11):1140–1150. doi: 10.1001/archgenpsychiatry.2011.2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daro D, Dodge KA. Creating community responsibility for child protection: Possibilities and challenges. The Future of Children/Center for the Future of Children. The David and Lucile Packard Foundation. 2009;19(2):67–93. doi: 10.1353/foc.0.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the World Mental Health Surveys. PLoS Med. 2008;5(7):e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekel S, Bonanno GA. Changes in trauma memory and patterns of posttraumatic stress. Psychol Trauma: Theory, Research, Practice and Policy. 2013;5(1):26–34. [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabilitation Psychol. 2010;55(1):1–11. doi: 10.1037/a0018601. [DOI] [PubMed] [Google Scholar]
- Duncan AE, Sartor CE, Scherrer JF, Grant JD, Heath AC, Nelson EC, et al. The association between cannabis abuse and dependence and childhood physical and sexual abuse: evidence from an offspring of twins design. Addiction. 2008;103(6):990–997. doi: 10.1111/j.1360-0443.2008.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feigin V. Global, regional, and national incidence, prevalence, and years lived with disability for 310 acute and chronic diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. The Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Cannabis use and other illicit drug use: testing the cannabis gateway hypothesis. Addiction. 2006;101(4):556–569. doi: 10.1111/j.1360-0443.2005.01322.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Beautrais AL. Cannabis and educational achievement. Addiction. 2003;98(12):1681–1692. doi: 10.1111/j.1360-0443.2003.00573.x. [DOI] [PubMed] [Google Scholar]
- Fluke JD, Yuan YYT, Hedderson J, Curtis PA. Disproportionate representation of race and ethnicity in child maltreatment: Investigation and victimization. Children and Youth Services Review. 2003;25(5):359–373. [Google Scholar]
- Fontes MA, Bolla KI, Cunha PJ, Almeida PP, Jungerman F, Laranjeira RR, et al. Cannabis use before age 15 and subsequent executive functioning. The British J Psych. 2011;198(6):442–447. doi: 10.1192/bjp.bp.110.077479. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. The Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Hadland SE, Knight JR, Harris SK. Medical marijuana: review of the science and implications for developmental behavioral pediatric practice. J Developmental and Behavioral Pediatrics: JDBP. 2015;36(2):115–123. doi: 10.1097/DBP.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahm HC, Lee Y, Ozonoff A, Van Wert MJ. The impact of multiple types of child maltreatment on subsequent risk behaviors among women during the transition from adolescence to young adulthood. J Youth and Adolescence. 2010;39(5):528–540. doi: 10.1007/s10964-009-9490-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W. The adverse health effects of cannabis use: What are they, and what are their implications for policy? Int J Drug Policy. 2009;20(6):458–466. doi: 10.1016/j.drugpo.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Hall WD, Lynskey M. Is cannabis a gateway drug? Testing hypotheses about the relationship between cannabis use and the use of other illicit drugs. Drug and Alcohol Review. 2005;24(1):39–48. doi: 10.1080/09595230500126698. [DOI] [PubMed] [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe TJ. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse and Negl. 1997;21(6):529–539. doi: 10.1016/s0145-2134(97)00013-6. [DOI] [PubMed] [Google Scholar]
- Hasin D, Hatzenbuehler ML, Keyes K, Ogburn E. Substance use disorders: Diagnostic and Statistical Manual of Mental Disorders, (DSM‐IV) and International Classification of Diseases, (ICD‐10) Addiction. 2006;101(s1):59–75. doi: 10.1111/j.1360-0443.2006.01584.x. [DOI] [PubMed] [Google Scholar]
- Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, O’Callaghan MJ, Williams GM. Childhood sexual abuse and cannabis use in early adulthood: Findings from an Australian birth cohort study. Arch Sexual Behavior. 2009;38(1):135–142. doi: 10.1007/s10508-007-9172-5. [DOI] [PubMed] [Google Scholar]
- Herrenkohl RC, Herrenkohl TI. Assessing a child’s experience of multiple maltreatment types: Some unfinished business. J Family Violence. 2009;24(7):485–496. doi: 10.1007/s10896-009-9247-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins DJ, McCabe MP. Multiple forms of child abuse and neglect: Adult retrospective reports. Aggression and Violent Behavior. 2001;6(6):547–578. [Google Scholar]
- Hildyard KL, Wolfe DA. Child neglect: developmental issues and outcomes. Child Abuse and Negl. 2002;26(6):679–695. doi: 10.1016/s0145-2134(02)00341-1. [DOI] [PubMed] [Google Scholar]
- Hogan JW, Roy J, Korkontzelou C. Handling drop‐out in longitudinal studies. Statistics in Medicine. 2004;23(9):1455–1497. doi: 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- Horwood LJ, Fergusson DM, Coffey C, Patton GC, Tait R, Smart D, et al. Cannabis and depression: an integrative data analysis of four Australasian cohorts. Drug and Alcohol Dependence. 2012;126(3):369–378. doi: 10.1016/j.drugalcdep.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Horwood LJ, Fergusson DM, Hayatbakhsh MR, Najman JM, Coffey C, Patton GC, et al. Cannabis use and educational achievement: Findings from three Australasian cohort studies. Drug and Alcohol Dependence. 2010;110(3):247–253. doi: 10.1016/j.drugalcdep.2010.03.008. [DOI] [PubMed] [Google Scholar]
- Houston JE, Murphy J, Adamson G, Stringer M, Shevlin M. Childhood sexual abuse, early cannabis use, and psychosis: testing an interaction model based on the National Comorbidity Survey. Schiz Bull. 2008;34(3):580–585. doi: 10.1093/schbul/sbm127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovdestad WE, Tonmyr L, Wekerle C, Thornton T. Why is childhood maltreatment associated with adolescent substance abuse? a critical review of explanatory models. International J Mental Health and Addiction. 2011;9(5):525–542. [Google Scholar]
- Huizink AC, Mulder EJ. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neuroscience and Biobehavioral Reviews. 2006;30(1):24–41. doi: 10.1016/j.neubiorev.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Jackson Y, Gabrielli J, Fleming K, Tunno AM, Makanui PK. Untangling the relative contribution of maltreatment severity and frequency to type of behavioral outcome in foster youth. Child Abuse and Negl. 2014;38(7):1147–1159. [Google Scholar]
- Kendall-Tackett K, Becker-Blease K. The importance of retrospective findings in child maltreatment research. Child Abuse and Negl. 2004;28(7):723–727. doi: 10.1016/j.chiabu.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Kevorkian S, Bonn-Miller MO, Belendiuk K, Carney DM, Roberson-Nay R, Berenz EC. Asociations among trauma, postraumatic stress disorder, cannabis use, and cannabis use disorders in a nationally representative epidemiologic sample. Psychol Addict Behaviors: J Society Psychol Adddict Behaviors. 2015;29(3):633–638. doi: 10.1037/adb0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S, Kwok S, Mayes LC, Potenza MN, Rutherford HJ, Strathearn L. Early adverse experience and substance addiction: dopamine, oxytocin, and glucocorticoid pathways. Annals of the New York Academy of Sciences. doi: 10.1111/nyas.13140. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE. Does physical abuse in early childhood predict substance use in adolescence and early adulthood? Child Maltreatment. 2010;15(2):190–194. doi: 10.1177/1077559509352359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AS, Leeb RT, English D, Graham JC, Briggs EC, Brody KE, Marshall JM. What’s in a name? A comparison of methods for classifying predominant type of maltreatment. Child Abuse and Negl. 2005;29(5):533–551. doi: 10.1016/j.chiabu.2003.05.005. [DOI] [PubMed] [Google Scholar]
- Legleye S, Piontek D, Kraus L, Morand E, Falissard B. A validation of the Cannabis Abuse Screening Test (CAST) using a latent class analysis of the DSM‐IV among adolescents. Int J Methods Psych Research. 2013;22(1):16–26. doi: 10.1002/mpr.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longman-Mills S, González W, Meléndez M, García M, Gómez J, Juárez C, et al. Exploring child maltreatment and its relationship to alcohol and cannabis use in selected Latin American and Caribbean countries. Child Abuse and Negl. 2013;37(1):77–85. doi: 10.1016/j.chiabu.2012.11.002. [DOI] [PubMed] [Google Scholar]
- Mancini AD, Bonanno GA. Resilience in the face of potential trauma: Clinical practices and illustrations. J Clinic Psychol. 2006;62(8):971–986. doi: 10.1002/jclp.20283. [DOI] [PubMed] [Google Scholar]
- Martin EK, Silverstone PH. How much child sexual abuse is “below the surface,” and can we help adults identify it early? Frontiers in Psych. 2013;4:1–10. doi: 10.3389/fpsyt.2013.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ, Siegfried NJ. The revictimization of child sexual abuse survivors: An examination of the adjustment of college women with child sexual abuse, adult sexual assault, and adult physical abuse. Child Maltreatment. 2000;5(1):18–27. doi: 10.1177/1077559500005001003. [DOI] [PubMed] [Google Scholar]
- Mewton L, Slade T, Teesson M. An evaluation of the proposed DSM-5 cannabis use disorder criteria using Australian national survey data. J Studies on Alcohol and Drugs. 2013;74(4):614–621. doi: 10.15288/jsad.2013.74.614. [DOI] [PubMed] [Google Scholar]
- Mills R, Alati R, Strathearn L, Najman JM. Alcohol and tobacco use among maltreated and non‐maltreated adolescents in a birth cohort. Addiction. 2014;109(4):672–680. doi: 10.1111/add.12447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R, Kisely S, Alati R, Strathearn L, Najman J. Self-reported and agency-notified child sexual abuse in a population-based birth cohort. J Psych Research. 2016;74:87–93. doi: 10.1016/j.jpsychires.2015.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R, Kisely S, Alati R, Strathearn L, Najman JM. Child maltreatment and cannabis use in young adulthood: a birth cohort study. Addiction. 2016;112:494–501. doi: 10.1111/add.13634. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najman JM, Aird R, Bor W, O’Callaghan M, Williams GM, Shuttlewood GJ. The generational transmission of socioeconomic inequalities in child cognitive development and emotional health. Social Sci and Med. 2004;58(6):1147–1158. doi: 10.1016/s0277-9536(03)00286-7. [DOI] [PubMed] [Google Scholar]
- Najman JM, Alati R, Bor W, Clavarino A, Mamun A, McGrath JJ, et al. Cohort profile update: The Mater-University of Queensland study of pregnancy (MUSP) Int J Epidemiol. 2015;44(1):78–78f. doi: 10.1093/ije/dyu234. [DOI] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Putnam FW. A prospective investigation of the impact of childhood sexual abuse on the development of sexuality. J Consulting and Clinic Psychol. 2003;71(3):575–586. doi: 10.1037/0022-006x.71.3.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura Y, Hurd YL, Pilowsky DJ. Life-time risk for substance use among offspring of abusive family environment from the community. Substance Use and Misuse. 2012;47(12):1281–1292. doi: 10.3109/10826084.2012.695420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Rogosch FA, Burnette ML, Cicchetti D. Developmental pathways to adolescent cannabis abuse and dependence: Child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychol Addict Behaviors. 2011;25(4):634–644. doi: 10.1037/a0023151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325(7374):1195–1198. doi: 10.1136/bmj.325.7374.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonko KA. Exploring assumptions about child neglect in relation to the broader field of child maltreatment. J Health and Human Services Administration. 2006;29(3):260–284. [PubMed] [Google Scholar]
- Reinarman C. Commentaries on Pedersen (2011): Does cannabis cause poverty too? Moving beyond the malevolence paradigm. Addiction. 2011;106(9):1644–1645. doi: 10.1111/j.1360-0443.2011.03554.x. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychol. 2010;22(04):883–897. doi: 10.1017/S0954579410000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartor CE, Waldron M, Duncan AE, Grant JD, McCutcheon VV, Nelson EC, et al. Childhood sexual abuse and early substance use in adolescent girls: the role of familial influences. Addiction. 2013;108(5):993–1000. doi: 10.1111/add.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147. [PubMed] [Google Scholar]
- Senn TE, Carey MP. Child maltreatment and women’s adult sexual risk behavior: Childhood sexual abuse as a unique risk factor. Child Maltreatment. 2010;15(4):324–335. doi: 10.1177/1077559510381112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clinical Psychol Review. 2008;28(5):711–735. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sesar K, Šimić N, Barišić M. Multi-type childhood abuse, strategies of coping, and psychological adaptations in young adults. Croatian Medical J. 2010;51(5):406–416. doi: 10.3325/cmj.2010.51.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slack KS, Holl JL, McDaniel M, Yoo J, Bolger K. Understanding the risks of child neglect: An exploration of poverty and parenting characteristics. Child Maltreatment. 2004;9(4):395–408. doi: 10.1177/1077559504269193. [DOI] [PubMed] [Google Scholar]
- Smith DK, Johnson AB, Pears KC, Fisher PA, DeGarmo DS. Child maltreatment and foster care: Unpacking the effects of prenatal and postnatal parental substance use. Child Maltreatment. 2007;12(2):150–160. doi: 10.1177/1077559507300129. [DOI] [PubMed] [Google Scholar]
- Steering Committee for the Review of Commonwealth/State Service Provision (SCRCSSP) Report on Government Services. Canberra: Australian Capital Territory: AusInfo; 2000. [Google Scholar]
- Stevens KI, Schneiderman JU, Negriff S, Brinkmann A, Trickett PK. The whole picture: Child maltreatment experiences of youths who were physically abused. Child Abuse and Negl. 2015;43:30–41. doi: 10.1016/j.chiabu.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SL, Baiden P, den Dunnen W. Prescription medication misuse among adolescents with severe mental health problems in Ontario, Canada. Substance Use and Misuse. 2013;48(5):404–414. doi: 10.3109/10826084.2013.765482. [DOI] [PubMed] [Google Scholar]
- Strathearn L, Mamun AA, Najman JM, O’Callaghan MJ. Does breastfeeding protect against substantiated child abuse and neglect? A 15-year cohort study. Pediatrics. 2009;123(2):483–493. doi: 10.1542/peds.2007-3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Parigger A. The ‘Maltreatment and Abuse Chronology of Exposure’(MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One. 2015;10(2):e0117423. doi: 10.1371/journal.pone.0117423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodore AD, Chang JJ, Runyan DK, Hunter WM, Bangdiwala SI, Agans R. Epidemiologic features of the physical and sexual maltreatment of children in the Carolinas. Pediatrics. 2005;115(3):e331–e337. doi: 10.1542/peds.2004-1033. [DOI] [PubMed] [Google Scholar]
- Thornberry TP, Henry KL, Ireland TO, Smith CA. The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. J Adolescent Health. 2010;46(4):359–365. doi: 10.1016/j.jadohealth.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Matsuda M, Greenman SJ, Augustyn MB, Henry KL, Smith CA, Ireland TO. Adolescent risk factors for child maltreatment. Child Abuse and Negl. 2014;38(4):706–722. doi: 10.1016/j.chiabu.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonmyr L, Thornton T, Draca J, Wekerle C. A review of childhood maltreatment and adolescent substance use relationship. Current Psych Reviews. 2010;6(3):223–234. [Google Scholar]
- Wallace JM, Jr, Brown TN, Bachman JG, Laveist TA. The influence of race and religion on abstinence from alcohol, cigarettes and marijuana among adolescents. J Studies on Alcohol. 2003;64(6):843–848. doi: 10.15288/jsa.2003.64.843. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne PJ, Kandel DB. Maternal smoking during pregnancy and psychopathology in offspring followed to adulthood. J Am Acad Child and Adolescent Psych. 1999;38(7):892–899. doi: 10.1097/00004583-199907000-00020. [DOI] [PubMed] [Google Scholar]
- Werner K, McCutchen V, Agrawal A, Sartor C, Nelson E, Heath A, Bucholz K. The association of soecific traumatic experiences with cannabis initiation and transition to problem use: Differences between African-American and Eurpean-American women. Drug and Alcohol Dependence. 2016;168:162–169. doi: 10.1016/j.drugalcdep.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Hiller-Sturmhofel S. Alcohol abuse as a risk factor for and consequence of child abuse. Alcohol Research and Health. 2001;25(1):52–52. [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI-AUTO) Geneva: 1997. [Google Scholar]
- Zammit S, Thomas K, Thompson A, Horwood J, Menezes P, Gunnell D, et al. Maternal tobacco, cannabis and alcohol use during pregnancy and risk of adolescent psychotic symptoms in offspring. The British J Psych. 2009;195(4):294–300. doi: 10.1192/bjp.bp.108.062471. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


