Abstract
The purpose of this study is to review the trends in hip arthroscopy using data from a statewide database, focusing on utilization rates, patient demographics and complication rates. The Statewide Planning and Research Cooperative System (SPARCS) database for New York State was queried for cases of hip arthroscopy from 1998 to 2012. Patient demographics and procedural details were collected. Patients were subsequently reviewed for complications and readmissions within 30 and 90 days. In total, 12 194 hip arthroscopy procedures were performed by 295 surgeons in 137 centers between 1998 and 2012. There was a 95-fold increase in the annual frequency of hip arthroscopy procedures between 1998 (n = 24) and 2012 (n = 2296). Thirty-day complication rates were 0.2% (n = 19), whereas the 90-day complication rate was 0.3% (n = 30). The all-cause 30-day readmission rate was 0.5% (n = 66), whereas the 90-day rate was 1.6% (n = 200). The number of surgeons performing hip arthroscopy increased 7-fold over the observation period. However, only 14.9% (n = 44) of surgeons performed more than 30 procedures annually. Lower volume surgeons (<102 cases/year) demonstrated significantly higher 90-day readmission rates, compared with higher volume surgeons (>163 cases/year, P < 0.0060); however, complication rates and readmission rates did not differ based on surgeon volume. Our findings confirm our hypothesis, demonstrating a significant increase in utilization of hip arthroscopy in the State of New York. We did not identify an associated increase in annual complication rates as hypothesized with increasing utilization, although there was an association of higher readmission rates among lower volume surgeons. Further study is needed to define rates of failure requiring revision hip arthroscopy or conversion to arthroplasty, and to clarify the relationship between complication rates and surgeon volume and case complexity.
Level of Evidence: III, retrospective cohort series.
INTRODUCTION
Improvement in surgical equipment and advancement of surgical techniques have allowed for improved arthroscopic access to the hip joint. Simultaneously, an improved recognition of femoroacetabular impingement (FAI) and resultant labral pathology has led to widespread utilization of hip arthroscopy in recent years (FAI) [1, 2]. A review of insurance plan data identified an increase in annual rates of 365% from 2004 to 2009 in the United States [3]. Similarly, amongst American Board of Orthopaedic Surgical (ABOS) Part II Candidates, an even larger increase of nearly 600% was noted from 2006 to 2010 [4]. Although these studies have provided evidence of the increasing utilization, there is limited evidence to establish the frequency of hip arthroscopy in a population-based setting.
With increasing utilization, improved understanding of the associated procedural risks and subsequent complications is required to improve the process of obtaining informed consent. Few studies have reviewed large sample data to accurately quantify the incidence of associated procedural complications in the United States, beyond those previously reported in smaller series’ or from European centers [5, 6]. Similarly, there is a lack of information on the relationship between complications or readmissions with surgical volume, as identified in other subspecialties in orthopedics [7–11].
The aim of this study was to determine the frequency of hip arthroscopy from a statewide database, to more accurately reflect national utilization. We also sought to report the associated 30- and 90-day complication rates requiring readmission and utilization of healthcare resources. Finally, we sought to determine surgeon and hospital volume during the study period. We hypothesized that annual hip arthroscopy rates would significantly increase over the study duration, with a corresponding increase in complication rates reflecting widespread utilization.
MATERIALS AND METHODS
The Statewide Planning and Research Cooperative System (SPARCS) database was utilized for data collection. This is a comprehensive, all-payer data reporting system maintained by the New York State Department of Health (NYSDOH), serving as a census of admissions and ambulatory procedures within the state. All licensed hospitals or hospital extension clinics/treatment centers are required to submit inpatient and outpatient data to SPARCS. The enabling legislation for SPARCS is located under Section 28.16 of the Public Health Law (PHL). The regulations pertaining to SPARCS are under Section 400.18 of Title 10 (Health) of the Official Compilation of Codes, Rules and Regulations of the State of New York (NYCRR). Data must be submitted on a monthly basis, with 100% of facility’s SPARCS data submitted within 180 days of the patient discharge/visit.
Data is submitted to the Department of Health via the Health Commerce System (HCS) website. This is a secure website, with all entered data abiding by the New York State Department of Health's data security standards. Access to the database was granted via request (Request #1107-04) from the Data Governance Committee of the NYSDOH. The database was then used to identify any hip arthroscopic procedures performed in an outpatient setting. While the SPARCS database has been established and operational since 1982, hip arthroscopy and associated CPT-4 (Current Procedural Terminology, Fourth Revision) and ICD-9-CM (International Classification of Disease, Ninth Revision, Clinical Modification) codes were not routinely utilized until much later. As a result, this study was restricted to a retrospective review of data from 1998 to 2012.
Patients undergoing outpatient hip arthroscopy were identified by both the initial subset of CPT-4 codes for hip arthroscopy (29860–29863), and using the more recently adopted CPT-4 hip arthroscopy codes, introduced in 2011 (29914–29916) (Table I). Due to the changes in coding over the observation period, a summative analysis combining new and old codes into similar procedural groups was performed to better depict the percentage of performed procedures over the study period. Osteoplasty without labral repair included all procedures with either code 29862, 29914 or 29915 (or a combination of these) without a concomitant code 29916. Osteoplasty with labral repair included all procedures with either 29862, 29914, 29915 (or a combination of these) combined with code 29916. Labral repair without osteoplasty included procedures with code 29916 without any or all combinations of codes 29862, 29914 and 29915. Finally, the group where no osteoplasty or labral repair was performed consisted of procedures without 29862, 29914, 29915 and 29916, largely reflective of isolated synovectomy, loose body removal or diagnostic arthroscopy.
Table I.
Hip arthroscopy CPT codes
| Code | Procedure listing |
|---|---|
| 29860 | Hip Arthroscopy, diagnostic, with or without synovial biopsy |
| 29861 | Hip Arthroscopy, removal of loose body or foreign body |
| 29862 | Hip Arthroscopy, chondroplasty, abrasion arthroplasty and/or resection of labrum |
| 29863 | Hip Arthroscopy, synovectomy |
| 29914 | Hip Arthroscopy, with femoroplasty |
| 29915 | Hip Arthroscopy, with acetabuloplasty |
| 29916 | Hip Arthroscopy, with labral repair |
After identification of the cohort, demographic data was collected including patient age, sex, race, insurance status, discharge disposition and year of surgery. ICD-9 diagnostic codes associated with each procedure were collected in order to determine surgical indications for each arthroscopic procedure. Operative details were otherwise not available given the administrative nature of the database. Unique patient identifiers were then utilized to search for potential in-state readmissions anywhere in the state within 30 and 90 days of the index procedure, screening for a pre-determined list of associated procedural complications to ensure readmission was related to the arthroscopic procedure. The list of procedural complications was derived from a more extensive list of ‘Hospital Acquired Conditions’ on the Center for Medicare & Medicaid Services website (https://www.cms.gov/medicare/medicare-fee-for-service-payment/hospitalacqcond/hospital-acquired_conditions.html). All-cause readmission rates were also reported, which include admissions that were unrelated to surgical procedure or associated complications. Hospital identification numbers and physician license numbers were also available from the SPARCS database and were collected to determine the number of participating surgeons and centers over the study period. Physician identification codes were utilized to determine the nature of fellowship training of participating surgeons, as identified through the NYS Physician Profile website, supplemented with an exhaustive web engine search.
Descriptive statistics were calculated, including means and standard deviations for all continuous variables, and frequency counts and percentages for discrete variables. Rates of readmission were calculated for both 30 and 90 days of the index procedure.
RESULTS
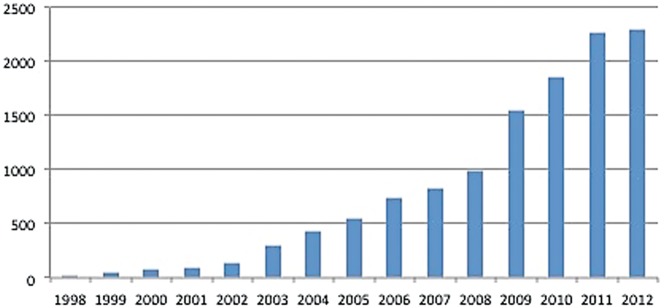
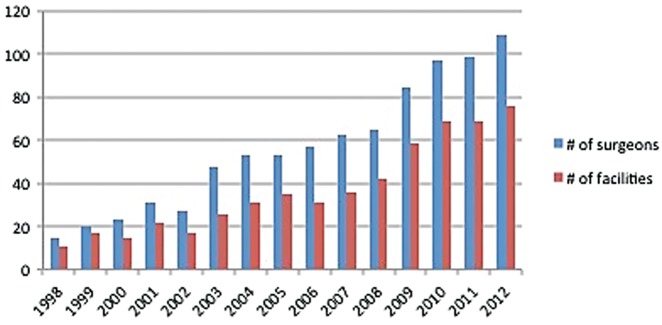
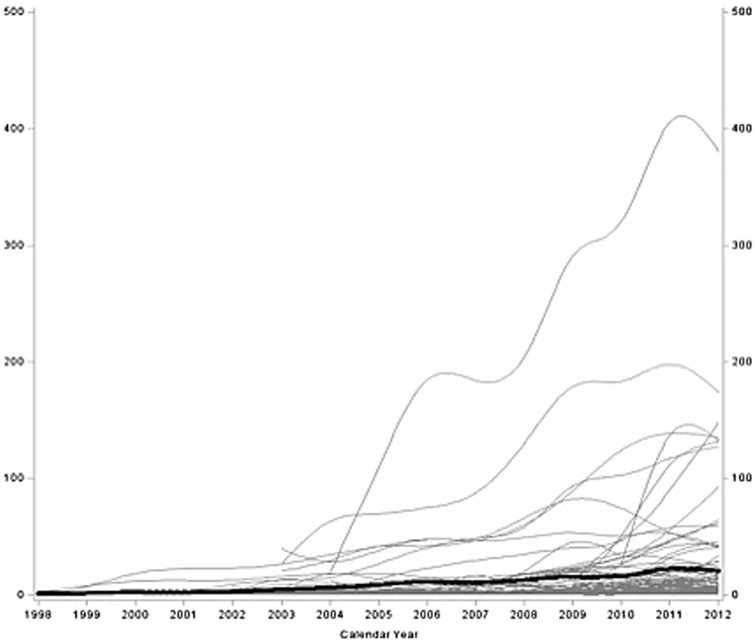
A total of 12 194 hip arthroscopy procedures were performed in the state of New York between 1998 and 2012. General patient characteristics were recorded (Table II). The annual volume of procedures increased steadily over the study period (Fig. 1). Overall, there was a 95-fold increase in the annual frequency of hip arthroscopy from 24 procedures in 1998–2296 procedures in 2012. The frequency of hip arthroscopy increased 650% from 2003 to 2012. These procedures were performed by 295 surgeons in 137 centers. Similar to the trends noted in overall procedural frequency, a comparable increase was identified in the number of participating surgeons and centers per year (Fig. 2).
Table II.
Patient demographics
| (N = 12 194) | |
|---|---|
| Patient characteristics | n (%) |
| Age | |
| Mean age, years ± SD | 36.6 ± 13.2 |
| Median age, years | 37 |
| Sex, n(%) | |
| Male | 5362 (44.0%) |
| Female | 6832 (56.0%) |
| Race, n(%) | |
| White | 9074 (74.4%) |
| Black | 397 (3.3%) |
| Asian | 117 (1.0%) |
| Other | 1629 (13.4%) |
| Missing | 977 (8.0%) |
| Race and Ethnicity, n(%) | |
| White | 8888 (72.9%) |
| Black | 372 (3.1%) |
| Hispanic | 420 (3.4%) |
| Asian | 117 (1.0%) |
| Other | 1429 (11.7%) |
| Missing | 968 (7.9%) |
| Insurance status, n(%) | |
| Medicare | 390 (3.2%) |
| Medicaid | 323 (2.7%) |
| Private | 10 122 (83.0%) |
| Worker's compensation | 880 (7.2%) |
| Other | 477 (3.9%) |
| Missing | 2 (0.0%) |
Fig. 1.
Annual volume of hip arthroscopy procedures in the state of New York.
Fig. 2.
Surgeon and Center volume performing hip arthroscopic procedures per year.
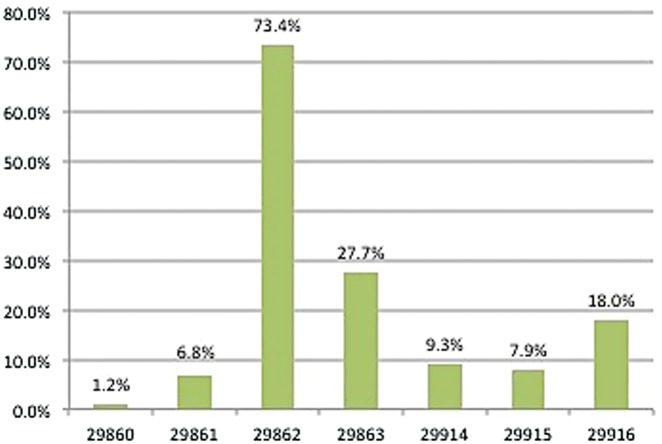
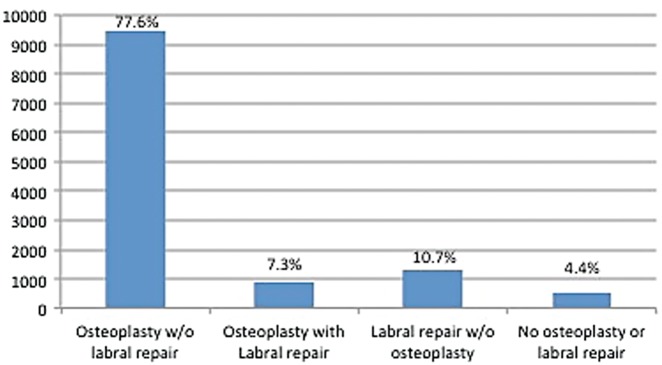
CPT code frequency was also analyzed (Fig. 3). Looking at procedural codes, more than one hip procedure (CPT code) was performed in 36% (n = 4442) of cases. As described earlier, codes were then grouped into classes of procedures. Osteoplasty without labral repair was performed in 78% (n = 9511) of cases. Osteoplasty with labral repair was performed in 7% (n = 904) of cases. Labral repair without osteoplasty was performed in 11% (n = 1341) of cases. Finally, isolated synovectomy, loose body removal or diagnostic arthroscopy was performed in 4% (n = 488) of cases (Fig. 4).
Fig. 3.
Frequency of CPT codes for all identified cases.
Fig. 4.
Frequency of procedures performed.
For this cohort, the 30-day complication rate was 0.2% (n = 19), while the 90-day complication rate was also 0.3% (n = 30). Complications were reported separately as either medical (i.e. pneumonia, urinary tract infection), or surgical (i.e. septic arthritis, mechanical complication) (Table III). The all-cause readmission rate within 30 days was 0.5% (n = 66), while the 90-day all-cause readmission rate was 1.6% (n = 200). Annual complications and readmission rates are reported in Table IV. Further analyzing complications and readmissions before and after 2003, where hip arthroscopy utilization significantly increased, there were no statistically significant differences in the rates of these (Table V).
Table III.
Complications identified at 30 and 90 days
| 30-day complications | 90-day complications | ||
|---|---|---|---|
| (n = 12 194) | (n = 12 194) | ||
| n(%) | n(%) | ||
| Medical | AMI | 1(0.01%) | – |
| Intracranial Injury | 1(0.01%) | 1(0.01%) | |
| Catheter-associated UTI | 3(0.02%) | – | |
| Ileus | 0(0.00%) | – | |
| Pneumonia | 3(0.02%) | – | |
| PE | 1(0.01%) | 3(0.02%) | |
| DVT | 3(0.02%) | 6(0.05%) | |
| Sepsis/Septicemia/Shock | 0(0.00%) | 1(0.01%) | |
| Surgical | Major bleed | 1(0.01%) | 2(0.02%) |
| Wound infection | 5(0.04%) | – | |
| Septic arthritis (hip) | 2(0.02%) | 3(0.02%) | |
| Dislocation | 1(0.01%) | 1(0.01%) | |
| Fracture | 0(0.00%) | 0(0.00%) | |
| AVN | 4(0.03%) | 4(0.03%) | |
| Mechanical Complication | 1(0.01%) | 3(0.02%) | |
| Hardware breakage | 0(0.00%) | 1(0.01%) | |
| Other complications NOS | 1(0.01%) | 1(0.01%) |
Several cases had multiple complications listed.
Table IV.
Annual 30- and 90-day complication and readmission rates
| 30-day complication | 90-day complication | 30-day readmission | 90-day readmission | N | |
|---|---|---|---|---|---|
| Year | n(%) | n(%) | n(%) | n(%) | |
| 1998 | 0(0.00%) | 0(0.00%) | 0(0.00%) | 1(4.17%) | 24 |
| 1999 | 0(0.00%) | 1(2.33%) | 0(0.00%) | 1(2.33%) | 43 |
| 2000 | 0(0.00%) | 0(0.00%) | 0(0.00%) | 4(4.71%) | 85 |
| 2001 | 1(0.99%) | 1(0.99%) | 2(1.98%) | 4(3.96%) | 101 |
| 2002 | 0(0.00%) | 1(0.75%) | 0(0.00%) | 1(0.75%) | 134 |
| 2003 | 0(0.00%) | 0(0.00%) | 3(0.98%) | 6(1.96%) | 306 |
| 2004 | 2(0.46%) | 2(0.46%) | 4(0.93%) | 11(2.55%) | 431 |
| 2005 | 0(0.00%) | 0(0.00%) | 4(0.73%) | 10(1.82%) | 549 |
| 2006 | 0(0.00%) | 1(0.14%) | 3(0.41%) | 7(0.95%) | 739 |
| 2007 | 1(0.12%) | 2(0.24%) | 8(0.97%) | 19(2.31%) | 822 |
| 2008 | 0(0.00%) | 1(0.10%) | 3(0.30%) | 16(1.61%) | 995 |
| 2009 | 3(0.19%) | 3(0.19%) | 11(0.71%) | 33(2.13%) | 1548 |
| 2010 | 4(0.22%) | 5(0.27%) | 8(0.43%) | 23(1.24%) | 1854 |
| 2011 | 5(0.22%) | 7(0.31%) | 10(0.44%) | 32(1.41%) | 2267 |
| 2012 | 3(0.13%) | 6(0.26%) | 10(0.44%) | 32(1.39%) | 2296 |
Table V.
Complication rates before and after 2003, where annual hip arthroscopy utilization rates significantly increased
| 30-day complication | 90-day complication | 30-day readmission | 90-day readmission | N | |
|---|---|---|---|---|---|
| Pre-2003 | 1(0.26%) | 3(0.78%) | 2(0.52%) | 11(2.84%) | 387 |
| 2003 and onward | 18(0.15%) | 27(0.23%) | 64(0.54%) | 189(1.60%) | 11 807 |
| Fisher’s Exact Test | P = 0.458 | P = 0.067 | P = 1.000 | P = 0.066 |
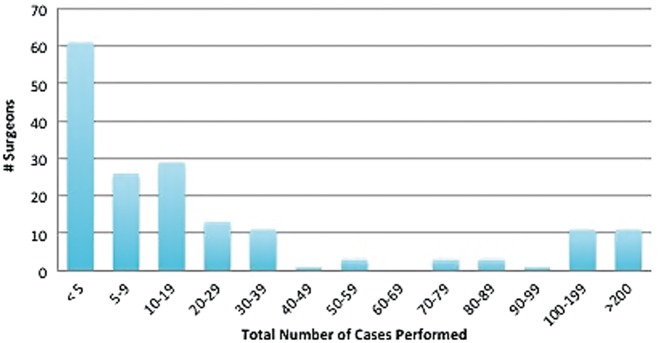
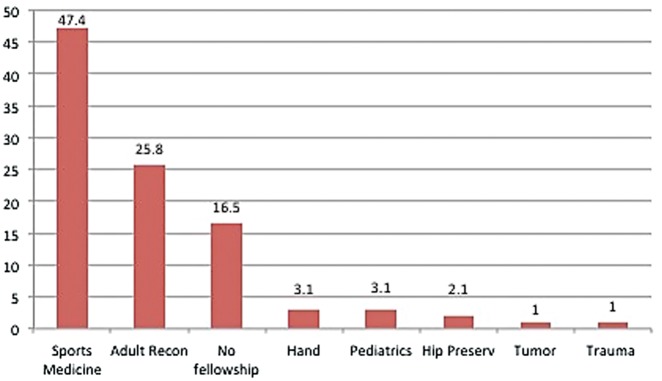
A scatterplot was created to analyze each surgeon’s respective volume by year (Fig. 5). The trendline demonstrates the average surgeon volume, which was approximately 10 cases over the 14-year study period. Surgeon volume demonstrated a bimodal distribution (Fig. 6) with the majority of surgeons performing less than 5 hip arthroscopies per year. It should be noted that 41.3% of surgeons (n = 122) of the initial cohort were identified as having performed only 1 hip arthroscopy over the study period. Only 14.9% of surgeons (n = 44) performed 30 or more procedures over the studied period. Fellowship training was reviewed for all surgeons who performed 5 or more hip arthroscopy procedures over the observed period (n = 97) (Fig. 7), as this group performed the majority of procedures over the observed period (86.1%).
Fig. 5.
Surgeon volume per year with trendline (thick line) representing average surgeon volume.
Fig. 6.
Caseload distribution among Surgeons.
Fig. 7.
Fellowship training of surgeons performing hip arthroscopy.
Additionally, we evaluated the influence of surgeon volume on 30-day and 90-day complication and readmission rates. This was done using previously established annual hip arthroscopy volume cutoffs, defined by using stratum-specific likelihood-ratios to analyze revision surgery data following hip arthroscopy [12]. Utilizing these volume strata, there did not appear to be any effect of surgeon volume on the rates of 30-day (P = 0.3724) or 90-day complications (P = 0.8006), or 30-day readmission rates (P = 0.0802). However, there was a significant difference in the rates of 90-day readmission, with lower volume surgeons (<102 cases/year), identified as having higher readmission rates (2.23%) compared with higher volume surgeons (164–339 cases/year, 0.85%, P = 0.0002; >340 cases/year, 0.58%, P = 0.0060) (Table VI).
Table VI.
Complication and readmission rates stratified by surgeon volume
| Surgeon annual hip arthroscopy volume | 30-day complication | 90-day complication | 30-day readmission | 90-day readmission | N |
|---|---|---|---|---|---|
| <102 | 11(0.15%) | 20(0.28%) | 52(0.72%) | 161(2.23%) | 7204 |
| 102–163 | 5(0.35%) | 5(0.35%) | 7(0.49%) | 20(1.39%) | 1440 |
| 164–339 | 2(0.11%) | 3(0.17%) | 6(0.34%) | 15(0.85%) | 1766 |
| ≥340 | 1(0.15%) | 2(0.29%) | 1(0.15%) | 4(0.58%) | 686 |
| Fisher’s exact test | P = 0.385 | P = 0.791 | P = 0.102 | P<0.001 |
P-values denote chi-square comparison of rates, with significant differences identified in 90-day readmission rates. Further comparisons identified a significantly higher readmission rate in the group performing less than 102 cases per/year, compared to those performing 164–339 cases/year (P < 0.001) and those performing >340 cases/year (P = <0.001).
DISCUSSION
Using the SPARCS database, a significant increase in the utilization of hip arthroscopy was identified in New York State, with a 95-fold increase in the annual frequency of hip arthroscopy procedures performed between 1998 and 2012. Additionally, we identified a relatively low rate of procedural complications requiring readmission (0.2%) and 30-day all-cause readmission rates (0.5%). Lower volume surgeons (<102 cases/year) demonstrated significantly higher 90-day readmission rates, compared with higher volume surgeons (>163 cases/year, P < 0.0060).
Previous studies have attempted to quantify the recent increase in hip arthroscopy, but using different methodology. The American Board of Orthopaedic Surgery (ABOS) Part II database, which studies the trends among newly graduating orthopaedic surgeons, has been queried on two occasions. Colvin et al. identified an increase in the number of candidates submitting hip arthroscopy cases from 1.24% in 1999–7.39% in 2009 [13]. Similarly, Bozic et al. noted a 600% increase in submitted hip arthroscopy cases from 2006 to 2010 [4]. However, the conclusions drawn from both studies were limited by the fact that the ABOS database reflects the practice patterns of newly graduating orthopaedic surgeons during their board collection period and does not reflect the practices of more experienced surgeons.
Other forms of large aggregate insurance data have also been used to assess hip arthroscopy trends. Montgomery et al. reviewed CPT codes from a national database of orthopaedic insurance records. They noted a 365% increase in hip arthroscopy between 2004 and 2009 (1.20 cases per 10 000 patients to 5.58 cases per 10 000) [3]. These trends were also echoed in a recent review of a large cross-sectional population utilizing the PearlDiver database, where a 250% increase in rates of hip arthroscopy was noted from 2007 to 2011 [14].
In our study, we utilized a population-based database, allowing for quantification of the rates of hip arthroscopy utilization in a cohort that more accurately reflects national trends. Similar to the aforementioned studies, surgical rates increased 95-fold, with a corresponding increase in the number of surgeons performing hip arthroscopy, as well as the number of associated surgical centers. The reason for this is likely multi-factorial, relating to improved recognition of FAI and associated labral pathology, as well as improvements in surgical equipment and surgical technique.
Complication rates associated with hip arthroscopy have been extensively studied, particularly as they relate to the ‘learning-curve’ associated with hip arthroscopy [15–18]. A recent systematic review has shown a major complication rate of 0.58% and minor complication rate of 7.0% [6]. This is consistent with outcomes reported from single institutions or from additional systematic reviews [19–21]. However, many of the included studies are smaller case series and large sample data is lacking, with few population-based studies reporting complication or readmission rates. The only study identified was that by Malviya et al., where hospital administrative data in the National Health Service in England was utilized to review 6395 cases, where a 30-day readmission rate of 0.5% was identified [5].
Similar to these results, the use of the SPARCs statewide database, and associated unique patient identifiers, allowed longitudinal tracking of patients to determine rates of medical/surgical complications and readmission in this study. The all-cause readmission rate within 30 days was 0.5%, consistent with that reported by Malviya et al. Additionally, the overall procedural complication rate requiring readmission, reflective of ‘major’ complications in prior studies (e.g. deep infection, PE, abdominal compartment syndrome) was 0.2%, consistent with figures previously reported in systematic analyses [6, 19]. Further conclusions regarding rates of minor complications were not feasible due to the limitation that data is only available for admissible complications.
Novel to this study, surgeon volume was also reviewed, with the number of surgeons performing hip arthroscopy increasing from less than 20 in 1998 to over 100 in 2012. However, only 15% of the total cohort of surgeons performed more than 30 procedures annually. Surgeon volume did not appear to affect complication rates, however 90-day readmission rates were significantly higher in the lower volume groups. This is potentially an area of further study to determine the associated cost with readmission. This may provide data supporting that these procedures should only be done by higher volume surgeons, although these volume cutoffs require further validation.
In addition to surgeon volume, we also reviewed fellowship training. The majority of surgeons performing hip arthroscopy completed a sports medicine (47.4%), adult reconstruction (25.8%) or hip preservation fellowship (2.1%). However, of the procedures performed in the study period, surgeons without fellowship training performed nearly 25% of all cases. While these trends are interesting, limited conclusions can be drawn from this data as fellowship training was not available for all surgeons. Further study is needed to determine the role of surgeon training and volume on outcomes, as has been demonstrated in other areas of orthopaedic surgery [7, 9–11].
Limitations
There are several limitations to the present study. As with any study utilizing data from an administrative database, we are lacking information on clinical indications for surgery. As a result, we cannot draw any further conclusions aside from the observed trends in objective data. Second, new FAI CPT codes were introduced in 2011 and as a result, our methodology needed to be adjusted for the years 2011 and 2012. Along these lines, the complexity of procedures performed was not discernible from the earlier sets of CPT codes (before 2011), and further study is warranted to assess the relationship between increasing case complexity and complication rates. We intentionally excluded CPT code 29999 (unlisted procedure, arthroscopy), as we wanted to ensure that only hip arthroscopy cases were included in the analysis. Finally, we were only able to identify the complications that resulted in an in-state readmission. We, therefore, have likely underreported readmissions or complications that were admitted out of state, or that did not require readmission, including superficial wound infections or nerve palsies, which are often among the most common complications [22]. Additionally, we are unable to appropriately identify long-term complications, including avascular necrosis, proximal femur fractures or revision surgery. This study also does not allow for assessment of associated patient-reported outcomes following treatment.
CONCLUSIONS
Our findings confirm our hypothesis, demonstrating an increasing utilization for hip arthroscopy in the State of New York. We did not identify an associated increase in annual rates of complications as hypothesized with increasing utilization, although there was an association of higher readmission rates among lower volume surgeons. Our findings are comparable to other studies in the literature, however further study is needed to define levels of competency and rates of failure requiring revision hip arthroscopy or conversion to arthroplasty. Additionally, further research is needed to clarify the relationship between complication rates and surgeon volume and case complexity.
ACKNOWLEDGEMENTS
This study utilizes data gathered by the New York State Department of Health, available via a publicly accessible database (Statewide Planning and Research Cooperative System - SPARCS). Our institution IRB has been granted access to this data set and a corresponding copy of the approval is included with submission of this manuscript.
FUNDING
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01AR066069. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Kelly BT, Williams RJ, Philippon MJ.. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med 2003; 31: 1020–37. [DOI] [PubMed] [Google Scholar]
- 2. Ganz R, Parvizi J, Beck M. et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20. [DOI] [PubMed] [Google Scholar]
- 3. Montgomery SR, Ngo SS, Hobson T. et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013; 29: 661–5. [DOI] [PubMed] [Google Scholar]
- 4. Bozic KJ, Chan V, Valone FH. et al. Trends in hip arthroscopy utilization in the United States. J Arthroplasty 2013; 28: 140–3. [DOI] [PubMed] [Google Scholar]
- 5. Malviya A, Raza A, Jameson S. et al. Complications and survival analyses of hip arthroscopies performed in the national health service in England: a review of 6,395 cases. Arthrosc J Arthrosc Relat Surg 2015; 31: 836–42. [DOI] [PubMed] [Google Scholar]
- 6. Harris JD, McCormick FM, Abrams GD. et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy 2013; 29: 589–95. [DOI] [PubMed] [Google Scholar]
- 7. Lyman S, Jones EC, Bach PB. et al. The association between hospital volume and total shoulder arthroplasty outcomes. Clin Orthop Relat Res 2005; 432: 132–7. [DOI] [PubMed] [Google Scholar]
- 8. Lyman S, Koulouvaris P, Sherman S. et al. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am 2009; 91: 2321–8. [DOI] [PubMed] [Google Scholar]
- 9. Laucis NC, Chowdhury M, Dasgupta A. et al. Trend toward high-volume hospitals and the influence on complications in knee and hip arthroplasty. J Bone Joint Surg Am 2016; 98: 707–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shervin N, Rubash HE, Katz JN.. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res 2007; 457: 35–41. [DOI] [PubMed] [Google Scholar]
- 11. Katz JN, Losina E, Barrett J. et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Jt Surg Am 2001; 83: 1622–9. [DOI] [PubMed] [Google Scholar]
- 12. Degen RM, Pan TJ, Nawabi DH. et al. Survivorship of primary hip arthroscopy in New York State: a population-based study. AOSSM Annual Meeting, Colorado Springs, CO, 2016.
- 13. Colvin AC, Harrast J, Harner C.. Trends in hip arthroscopy. J Bone Jt Surg 2012; 94: e23. [DOI] [PubMed] [Google Scholar]
- 14. Sing DC, Feeley BT, Tay B. et al. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthrosc J Arthrosc Relat Surg 2015; 31: 2307–13.e2. [DOI] [PubMed] [Google Scholar]
- 15. Lee Y-K, Ha Y-C, Hwang D-S. et al. Learning curve of basic hip arthroscopy technique: CUSUM analysis. Knee Surg Sport Traumatol Arthrosc 2013; 21: 1940–4. [DOI] [PubMed] [Google Scholar]
- 16. Hoppe DJ, de Sa D, Simunovic N. et al. The learning curve for hip arthroscopy: a systematic review. Arthroscopy 2014; 30: 389–97. [DOI] [PubMed] [Google Scholar]
- 17. Dietrich F, Ries C, Eiermann C. et al. Complications in hip arthroscopy: necessity of supervision during the learning curve. Knee Surg Sports Traumatol Arthrosc 2014; 22: 953–8. [DOI] [PubMed] [Google Scholar]
- 18. Gupta A, Redmond JM, Hammarstedt JE. et al. Safety measures in hip arthroscopy and their efficacy in minimizing complications: a systematic review of the evidence. Arthrosc J Arthrosc Relat Surg 2014; 30: 1342–8. [DOI] [PubMed] [Google Scholar]
- 19. Kowalczuk M, Bhandari M, Farrokhyar F. et al. Complications following hip arthroscopy: a systematic review and meta-analysis. Knee Surg Sport Traumatol Arthrosc 2013; 21: 1669–75. [DOI] [PubMed] [Google Scholar]
- 20. Oak N, Mendez-Zfass M, Lesniak BP. et al. Complications in hip arthroscopy. Sports Med Arthrosc 2013; 21: 97–105. [DOI] [PubMed] [Google Scholar]
- 21. Chan K, Farrokhyar F, Burrow S. et al. Complications following hip arthroscopy: a retrospective review of the McMaster experience (2009-2012). Can J Surg 2013; 56: 422–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clarke MT, Arora A, Villar RN.. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res 2003; 406: 84–8. [DOI] [PubMed] [Google Scholar]